Abstract
Purpose
Infected aneurysm of the aorta and adjacent arteries is rarely occurring and can be fatal without surgical intervention. Within the medical community, the most efficacious treatment strategy to address infected aortic aneurysm remains controversial. In this study, we have reviewed our treatment experience with 109 patients.
Methods
We included in our study all consecutive patients treated for primary infected aortic aneurysm at our facility between 1995 and 2011. Aneurysm-related mortality was defined as the presence of in-hospital and late mortality related to infection or postoperative complications.
Results
The median patient age was 72 years (range, 35-88), and 87 (80%) were male. Pathogen was isolated in 101 patients, and the most common microorganism identified was non-typhoid Salmonella in 61 (60%), followed by Staphylococcus aureus in 16 (16%) and Streptococci species in 7 (7%). Eighty-five (78%) patients underwent surgical treatment. Surgery included open repair with in-situ graft replacement in 77 (71%) and endovascular repair in 8 (7%). The aneurysm-related mortality rate was 67% in medically treated and 21% in surgically treated patients, with a median follow-up duration of 31.5 months (range 1-189). Additionally, risk factors for aneurysm-related mortality included old age, chronic lung disease, psoas muscle abscess, short duration of preoperative antibiotics, no operation, and probably endovascular repair.
Conclusions
Non-typhoid Salmonella was the most common pathogen found in our study group patients with infected aortic aneurysm. It appears that prolonged preoperative antibiotic treatment followed by open in-situ graft replacement remains the preferred and most effective treatment strategy.
Keywords: Infected aortic aneurysm, Outcome, Pathogen, Surgery
INTRODUCTION
Primary infected aortic aneurysm is a rare and life-threatening disease,1-15 and has an extremely high mortality rate without surgery. Several studies have investigated the risk factors for mortality associated with this disease. Such studies have observed that hospital survival duration was poor in patients with old age, ruptured aneurysm, suprarenal location, extensive infection, or where aorto-enteric fistula has formed.1-15 However, the probity of this information is limited by the small case numbers involved in these studies, and short follow-up durations.1-15 In addition, there was a significant number of patients who experienced late mortality that was related to aneurysm.1-15
Infected aortic aneurysm is common in Taiwan.4,5,12-14 We have reported that with timely surgical intervention and prolonged intravenous antibiotics, surgery with in-situ graft replacement provides a good outcome.4,16,17 Here, we sought to review our treatment experience with 109 consecutive patients of primary infected aortic aneurysm and find the specific predictors of aneurysm-related mortality. This overview herein provided is an update adding new patients to our previously reported patients.4,16-22
MATERIALS AND METHODS
Patients
This was a retrospective, observational cohort study of prospectively collected data. We included 109 consecutive patients with primary infected aortic aneurysms from 1995 to 2011. National Taiwan University Hospital is a 2200-bed tertiary care hospital. It serves an urban population of 2 million, providing both first-line and tertiary services and facilities. It serves also as a referral center for other hospitals in the country with a population of 23 million people. All data were collected by retrospective chart review. The local institutional medical ethics committee approved the study and waived the need for informed consent.
Diagnosis
The diagnosis of infected aortic aneurysm was made by a combination of clinical evidence of infection, imaging evidence of infected aorta, and/or pathological evidence of inflammation.4,16-22 We excluded patients with iatrogenic or traumatic aneurysms. Clinically, infected aortic aneurysm was usually preceded by infected aorta or aortitis. Infected aorta was diagnosed with clinical evidence of infection (fever and leukocytosis) and peri-aortic soft tissue infiltration demonstrated by either computed tomography or magnetic resonance imaging.4 In order to ascertain the responsible micro-organism, blood and tissue cultures were taken and then repeated for purposes of confirmation. In patients who underwent open surgery, the diagnosis of infected aneurysm was further confirmed by the presence of infection or frank pus during operation, and the presence of acute suppurative inflammation and/or aggregation of bacteria upon pathological examination. Tissue culture and pathological confirmation were not available in patients without open surgery.
Medical treatment
Intravenous antibiotic was administered once the diagnosis of infected aortic aneurysm was confirmed, as previously described.4,16-22 For patients with Salmonella species infections, intravenous ceftriaxone (1000-2000 gm Q12h) was used. For patients with non-salmonella infections, the particular antibiotic chosen was based on culture result and sensitivity test. In patients with good response to antibiotic treatment (no fever, no localized pain, and declining white cell count), surgical intervention was considered after the infection was controlled.
Surgical treatment
The surgical techniques employed and postoperative management undertaken were based on the particular treatment to address the diagnosed type of infected aortic aneurysm in each case.4,16-20,22 Open surgical repair consisted of wide debridement of necrotic tissue, copious saline irrigation, and in-situ repair with a Dacron graft through either thoracotomy, thoracoabdominal incision or midline laparotomy. Since April 2005, we began applying the endovascular repair technique on patients with infected aortic aneurysms.22
Once the diagnosis of infected aortic aneurysm was made, surgical repair was advised in all patients; the ultimate choice of open or endovascular repair was mainly based on the surgeon’s preference. Patients who underwent open or endovascular repair were unselected and surgery was performed even in the urgent condition of uncontrolled infection or unknown pathogen. Since 2007, endovascular repair was preferred in the majority of cases. However, surgical intervention was determined to be inappropriate in some patients because of old age, severe medical co-morbidities, or simply patient preference.21 However, no patients were denied surgery due to the surgeon factor.
Data collection
Data on age, sex, medical co-morbidities, pathogen, operation status, location of infection, surgical procedure, and clinical outcome were collected retrospectively from medical records. Immunodeficiency was defined as having acquired human immunodeficiency virus infection, use of corticosteroid and chemotherapeutic agents for malignancy or autoimmune diseases, or use of immunosuppressive agents for organ transplantation.23 Major postoperative complications included shock, neurologic, pulmonary, infectious, and gastrointestinal complications. The National Death Index, hospital computerized records, or telephone follow-up were used to verify the outcomes of patients.
We defined aneurysm-related mortality as the presence of in-hospital mortality, late mortality related to the infection, or late mortality caused by major postoperative complications such as stroke, respiratory failure and renal failure. Patient mortality which occurred more than 12 months after operation and was caused by a diagnosis not related to infected aortic aneurysm was not considered to be aneurysm-related.18-22 Follow-up duration was calculated from the day when the diagnosis was made and treatment was initiated to the last date of follow-up information.
Statistical analysis
Categorical variables were reported as the percentage of patients in the subgroup. The distributions of continuous variables were examined by the Shapiro-Wilk test. Continuous variables with skewed distribution were presented as medians with interquartile range. Comparison between groups was performed using the Chi-square test, Fisher’s exact test, and the Mann-Whitney test. A p-value below 0.05 was considered significant. The actuarial survival curve was plotted using the Kaplan-Meier method.
RESULTS
Patients
There were 87 males (80%) and 22 females enrolled in our study, with a median age of 72 years (range, 35-88). Patient characteristics are listed in Table 1. The medical co-morbidities present in these patients included diabetes mellitus in 25 (23%), hypertension in 45 (41%), cerebrovascular disease in 16 (15%), chronic lung disease in 11 (10%), chronic renal insufficiency in 20 (18%), and immunodeficiency in 17 (16%) patients. At presentation, 92 (84%) patients were febrile, and 69 (63%) patients had localized pain. Three (3%) patients presented with shock.
Table 1. Patient data stratified by aneurysm-related mortality: comparison between groups by Chi-square test, Fisher’s exact test, and Mann-Whitney test.
| All | Aneurysm-related mortality | Surgical | Aneurysm-related mortality | |||||
| patients | No | Yes | p | patients | No | Yes | p | |
| Case number | 109 | 75 | 34 | 85 | 67 | 18 | ||
| Median age in years (IQR) | 72 (61-80) | 70 (59-76) | 78.5 (69-83) | 0.001 | 71 (61-78) | 69 (60-76) | 78 (68-83) | 0.04 |
| Male gender | 87 (80%) | 57 (76%) | 30 (88%) | 0.2 | 67 (79%) | 51 (76%) | 16 (89%) | 0.24 |
| Co-morbidities | ||||||||
| Diabetes mellitus | 25 (23%) | 17 (23%) | 8 (24%) | 0.92 | 18 (21%) | 15 (22%) | 3 (17%) | 0.6 |
| Hypertension | 45 (41%) | 28 (37%) | 17 (50%) | 0.21 | 35 (41%) | 25 (37%) | 10 (56%) | 0.16 |
| Cerebrovascular disease | 16 (15%) | 10 (13%) | 6 (18%) | 0.56 | 13 (15%) | 9 (13%) | 4 (22%) | 0.46 |
| Chronic lung disease | 11 (10%) | 4 (5%) | 7 (21%) | 0.03 | 9 (11%) | 4 (6%) | 5 (28%) | 0.02 |
| Chronic renal insufficiency | 20 (18%) | 11 (15%) | 9 (27%) | 0.14 | 15 (18%) | 9 (13%) | 6 (33%) | 0.05 |
| Immunodeficiency | 17 (16%) | 12 (16%) | 5 (15%) | 1 | 12 (14%) | 10 (15%) | 2 (11%) | 1 |
| Clinical presentation | ||||||||
| Fever | 92 (84%) | 65 (87%) | 27 (79%) | 0.33 | 72 (85%) | 57 (85%) | 15 (83%) | 1 |
| Pain | 69 (63%) | 50 (67%) | 19 (56%) | 0.28 | 58 (68%) | 46 (69%) | 12 (67%) | 0.87 |
| Pathogen* | ||||||||
| Staphylococcus aureus | 16 (16%) | 8 (11%) | 8 (27%) | 0.08 | 11 (14%) | 8 (13%) | 3 (18%) | 0.69 |
| Non-typhoid Salmonella | 61 (60%) | 47 (66%) | 14 (47%) | 0.07 | 50 (62%) | 41 (64%) | 9 (53%) | 0.4 |
| Ciprofloxacin-sensitive | 52 (85%) | 42 (89%) | 10 (71%) | 0.19 | 42 (52%) | 5 (12%) | 3 (33%) | 0.14 |
| Image findings | ||||||||
| Pseudoaneurysm | 104 (95%) | 72 (96%) | 32 (94%) | 0.65 | 84 (99%) | 66 (99%) | 18 (100%) | 1 |
| Psoas abscess | 8 (7%) | 3 (4%) | 5 (15%) | 0.11 | 7 (8%) | 3 (5%) | 4 (22%) | 0.03 |
| Location | ||||||||
| Aortic arch | 14 (13%) | 10 (13%) | 4 (12%) | 11 (13%) | 8 (12%) | 3 (17%) | ||
| Descending thoracic | 24 (22%) | 14 (19%) | 10 (29%) | 17 (20%) | 14 (21%) | 3 (17%) | ||
| Suprarenal abdominal | 14 (13%) | 9 (12%) | 5 (15%) | 9 (11%) | 6 (9%) | 3 (17%) | ||
| Infrarenal abdominal | 59 (54%) | 44 (59%) | 15 (44%) | 50 (59%) | 41 (61%) | 9 (50%) | ||
| Suprarenal location | 51 (47%) | 32 (43%) | 19 (56%) | 0.2 | 36 (42%) | 27 (40%) | 9 (50%) | 0.2 |
| Surgery | 85 (78%) | 67 (89%) | 18 (53%) | < 0.001 | ||||
| Median duration of preoperative antibiotic in days (IQR) | 8 (2-21) | 14 (3-26) | 3 (0-7) | 0.005 | ||||
| Operation procedure | 0.06 | |||||||
| Open repair | v | v | 77 (91%) | 63 (94%) | 14 (78%) | |||
| Endovascular repair | 8 (9%) | 4 (6%) | 4 (22%) |
IQR, interquartile range. * Culture-negative in 8 patients.
Location of infection
The sites of infection were aortic arch in 14 (13%), descending thoracic aorta in 24 (22%), suprarenal abdominal aorta in 14 (13%), and infrarenal abdominal aorta or iliac arteries in 59 (54%) patients (Table 1). Two patients had multiple infected aortic aneurysms: one in both the proximal thoracic and the suprarenal abdominal aorta, and another in both the distal thoracic and the infrarenal abdominal aorta. Imaging studies showed aortitis in 5 patients, and 104 (95%) patients had formation of pseudoaneurysm or a saccular aneurysm. Eight (7%) patients with infrarenal infection had concomitant psoas muscle abscess.
Pathogen
All but 8 patients had a positive blood or tissue culture. Of the 101 pathogens isolated, the most common responsible microorganism was non-typhoid Salmonella species in 61 (60%), followed by Staphylococcus aureus in 16 (16%), Streptococci species in 7 (7%), Escherichia coli in 6 (6%), Klebsiella pneumoniae in 6 (6%), Mycobacterium tuberculosis in 4 (4%), and Bacteroides specie in 1 patient (1%). Of the 61 non-typhoid Salmonella isolates, 9 (15%) were ciprofloxacin-resistant. Of the 16 Staphylococcus aureus isolates, 8 were oxacillin-resistant (50%).
Hospital outcome
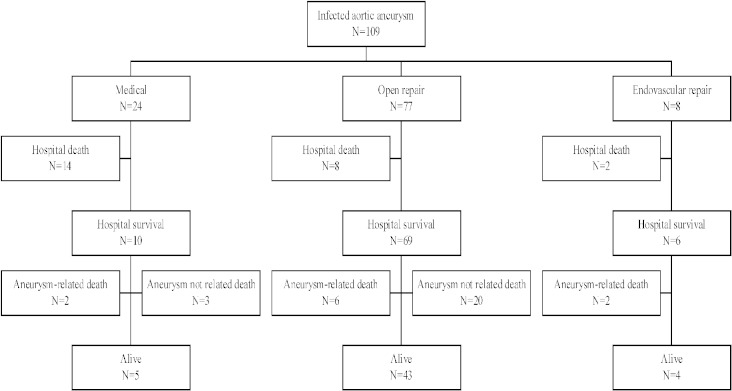
Twenty-four (22%) patients had medical treatment alone, while 85 (78%) of the patients underwent combined medical treatment and surgical repair (clinical outcomes are shown in Figure 1). The different types of surgical interventions included open repair with situ graft replacement in 77 patients (71%) and endovascular repair in 8 patients (7%). The overall in-hospital mortality rate was 22% (24/109): 58% (14/24) for medically treated patients, and 12% (10/85) for patients who underwent surgical repair. The in-hospital mortality rate was 10% (8/77) for patients who underwent open repair and 25% (2/8) for patients who underwent endovascular repair.
Figure 1.
Clinical outcomes of 109 patients with primary infected aortic aneurysms.
Of the total 14 in-hospital deaths which occurred in medically treated patients in our study, 14 patients died due to aneurysm rupture (100%). The causes of 8 in-hospital deaths in patients who underwent open repair were aneurysm rupture in 4 (50%) and persistent infection in 4 patients (50%). The causes of 2 in-hospital deaths in patients who underwent endovascular repair were ischemic bowel disease in 1, and early graft infection with massive gastrointestinal bleeding in 1 patient.
The risk factors of in-hospital mortality were old age in years (median with range: 70, range 59 to 77, versus 80.5, range 75 to 84, p < 0.001 by Mann-Whitney test), non-Salmonella infection (39% versus 62%, p = 0.04 by Fisher’s exact test), and no operation (12% versus 58%, p < 0.001 by Fisher’s exact test).
Aneurysm-related mortality
Eighty-five patients were followed-up through use of an outpatient clinic, with a median follow-up duration of 31.5 months (range, 1-189). A total of 10 patients died of late aneurysm-related causes after subsequent to hospital discharge discharge (Figure 1).
Of the 10 medically treated patients who passed from aneurysm-related causes, 2 patients (20%) died of late aneurysm rupture. Of the 69 patients who underwent open repair, 6 patients (9%) died of complications arising during or after surgery, with recurrent infection in 4 and major postoperative complications in 2 patients. Of the 6 patients who underwent endovascular repair, 2 patients (33%) died; one passed due to recurrent infection and 1 from major postoperative complication (renal failure). Among all mortal patients, aneurysm-related mortality occurred up to 8 months after discharge.
After combining the in-hospital (n = 24) and late (n = 10) mortalities, a total of 34 (31%) patients died of aneurysm-related mortality: 67% (16/24) in medically treated patients, 18% (14/77) in patients who underwent open repair and 50% (4/8) in patients who underwent endovascular repair. Aneurysm rupture (59%) and persistent or recurrent infection (38%) remained the major causes of death. The Kaplan-Meier survival curves in 3 treatment groups were plotted in Figure 2.
Figure 2.
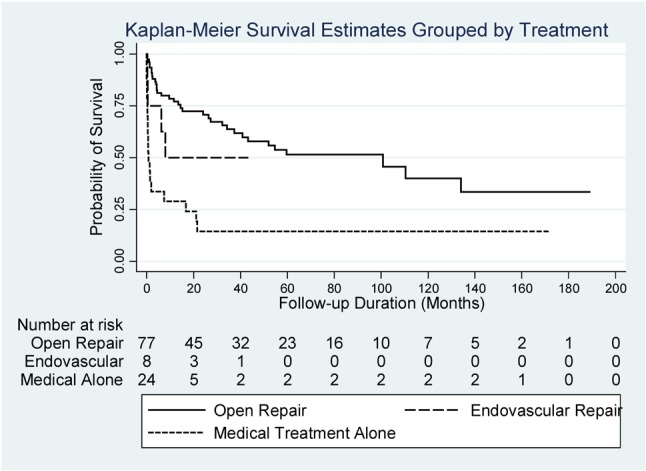
Infected aortic aneurysm: Kaplan-Meier survival curves of medically treated patients, patients who underwent open repair and patients who underwent endovascular repair.
For all of the patients in our study, patients with aneurysm-related mortality were older in age, and had a higher incidence of chronic lung disease, psoas muscle abscess, and no operation. Patient data stratified by aneurysm-related mortality are shown in Table 1. For patients who underwent surgical repair, patients with aneurysm-related mortality were older in age, and had a higher incidence of chronic lung disease, psoas muscle abscess, and short duration of preoperative antibiotic treatment. Open repair was associated with a higher rate of survival than endovascular repair, with a borderline statistical significance (p = 0.06 by Fisher’s exact test).
DISCUSSION
In this study, we investigated the predictive factors of early and late mortality in patients with primary infected aortic aneurysms. The in-hospital mortality was found to be 22% in the total cohort and 12% in patients who underwent surgical repair. For patients who passed due to aneurysm-related causes, the mortality rate was 31% in the total cohort, 67% (16/24) in medically treated patients, and 21% in patients who underwent surgical repair. In this study, we found that there was a significantly high risk of mortality in patients with old age, chronic lung disease, psoas muscle abscess, no operation and (probably) endovascular repair.
Infected aortic aneurysms are rare and account for only 0.7% to 1.3% of all aortic aneurysms.2,3 Medical treatment alone is insufficient in most cases because of the high risk of aneurysm rupture.21,24 The recommended treatment policy is open repair including surgical resection of the infected aorta, extensive debridement of infected tissue, and aortic reconstruction with either in-situ graft or extra-anatomic bypass. In the literature, the reported data assessing risk factors for surgery is minimal.1-15 This study is the first and the largest case series to date to assess the risk factors for early and late mortality.
Location of infection
In this study, the suprarenal location of infection was not associated with mortality. Although the surgical mortality risk was traditionally thought to be low in patients with infrarenal abdominal infection,3,12 the survival advantage was countered by the fact that the association of psoas muscle abscess and ciprofloxacin resistance in infrarenal infection was not rare. We have reported that the presence of psoas muscle abscess and infection caused by ciprofloxacin-resistant Salmonella was associated with poor outcome.19,25
Psoas muscle abscess
Psoas muscle abscess is uncommon. It can be divided into two groups: primary or secondary. In Taiwan, the most common etiological source of secondary psoas muscle abscess was urinary tract infection caused by an enteric micro-organism.26 We have demonstrated that psoas muscle abscess was associated with high incidence of emergency operation, prosthetic graft infection, in-hospital mortality and aneurysm-related mortality in infected aortic aneurysms.19 The results of medical treatment for psoas muscle abscess have been dismal, with an extremely high mortality rate (44%) even with aggressive drainage.26 In this study, the aneurysm-related mortality rate of 57% in patients with associated psoas muscle abscess was very close to the mortality rate in patients with primary psoas muscle abscess.26 In this study, psoas muscle abscess was identified as one of the major risk factors for aneurysm-related mortality in patients with infected aortic aneurysm. Therefore, careful preoperative evaluation using imaging studies to ascertain the presence of psoas muscle abscess is of paramount importance for risk stratification before treatment.
Endovascular repair
Endovascular repair for degenerative aortic aneurysms is well established, but its role in patients with infected aortic aneurysms remains controversial. There are an increasing number of reports associated with endovascular repair of thoracic and abdominal infected aortic aneurysms.27-32 The majority of reports with promising results were from small case series and early follow-up data.27-32 Endovascular repair was performed in selected patients.30,31 However, major concerns still remained because of the lack of long-term follow-up data and lingering doubt about stent graft placement in an infected bed. Several reports have described a high incidence of recurrent infection and late mortality after endovascular repair.22,27-29,32 Recurrent sepsis and death could occur up to 7 years after a successful endovascular repair.28
In this study, we reported 8 unselected patients who underwent endovascular repair. The in-hospital mortality rate of 25% and the aneurysm-related mortality rate of 50% were not satisfactory. The role and efficacy of endovascular repair in infected aortic aneurysms remains unclear. Because a prospective study comparing endovascular or open repair in a rare disease seems implausible, open repair remains a preferred and durable treatment strategy in patients with infected aortic aneurysms.
Study limitation
There were several limitations in this study. First, this study was retrospective and patient selection bias existed. Because of the nature of a retrospective study, there was no consistent approach applied to these patients and the duration of preoperative antibiotic use was also variable. It could very well be that patients with severe conditions might just decline surgical intervention. Second, the median follow-up duration of 31.5 months was not long enough to identify all cases of late aneurysm-related mortality, especially for patients who underwent endovascular repair. Third, the number of patients who underwent endovascular repair was small and limited our ability to reach a statistically meaningful conclusion. Therefore, an extended-period and multi-institutional study comparing the outcome of open and endovascular repair would be recommended.
CONCLUSIONS
Non-typhoid Salmonella was the most common pathogen found in our study of patients with infected aortic aneurysm. A further review of available medical courses of treatment suggests that prolonged preoperative antibiotic treatment followed by open in-situ graft replacement remains a preferred and durable treatment strategy.
REFERENCES
- 1.Moneta GL, Taylor LM, Jr., Yeager RA, et al. Surgical treatment of infected aortic aneurysm. Am J Surg. 1998;175:396–399. doi: 10.1016/S0002-9610(98)00056-7. [DOI] [PubMed] [Google Scholar]
- 2.Müller BT, Wegener OR, Grabitz K, et al. Mycotic aneurysms of the thoracic and abdominal aorta and iliac arteries:experience with anatomic and extra-anatomic repair in 33 cases. J Vasc Surg. 2001;33:106–113. doi: 10.1067/mva.2001.110356. [DOI] [PubMed] [Google Scholar]
- 3.Oderich GS, Panneton JM, Bower TC, et al. Infected aortic aneurysm: aggressive presentation, complicated early outcome, but durable results. J Vasc Surg. 2001;34:900–908. doi: 10.1067/mva.2001.118084. [DOI] [PubMed] [Google Scholar]
- 4.Hsu RB, Tsay YG, Wang SS, Chu SH. Surgical treatment for primary infected aneurysm of descending thoracic aorta, abdominal aorta and iliac arteries. J Vasc Surg. 2002;36:746–750. doi: 10.1067/mva.2002.126557. [DOI] [PubMed] [Google Scholar]
- 5.Luo CY, Ko WC, Kan CD, et al. In situ reconstruction of septic aortic pseudoaneurysm due to Salmonella or Streptococcus microbial aortitis: long-term follow-up. J Vasc Surg. 2003;38:975–982. doi: 10.1016/s0741-5214(03)00549-4. [DOI] [PubMed] [Google Scholar]
- 6.Fillmore AJ, Valentine RJ. Surgical mortality in patients with infected aortic aneurysms. J Am Coll Surg. 2003;196:435–441. doi: 10.1016/S1072-7515(02)01607-1. [DOI] [PubMed] [Google Scholar]
- 7.Ting AC, Cheng SW, Ho P, et al. Surgical treatment of infected aneurysms and pseudoaneurysms of the thoracic and abdominal aorta. Am J Surg. 2005;189:150–154. doi: 10.1016/j.amjsurg.2004.03.020. [DOI] [PubMed] [Google Scholar]
- 8.Woon CYL, Sebastian MG, Tay KH, Tan SG. Extra-anatomic revascularization and aortic exclusion for mycotic aneurysms of the infrarenal aorta and iliac arteries in an Asian population. Am J Surg. 2008;195:66–72. doi: 10.1016/j.amjsurg.2007.01.032. [DOI] [PubMed] [Google Scholar]
- 9.Dubois M, Daenens K, Houthoofd S, et al. Treatment of mycotic aneurysms with involvement of the abdominal aorta: single-centre experience in 44 consecutive cases. Eur J Vasc Endovasc Surg. 2010;40:450–456. doi: 10.1016/j.ejvs.2010.07.017. [DOI] [PubMed] [Google Scholar]
- 10.Brossier J, Lesprit P, Marzelle J, et al. New bacteriological patterns in primary infected aorto-iliac aneurysms: a single-centre experience. Eur J Vasc Endovasc Surg. 2010;40:582–588. doi: 10.1016/j.ejvs.2010.07.020. [DOI] [PubMed] [Google Scholar]
- 11.Vallejo N, Picardo NE, Bourke P, et al. The changing management of primary mycotic aortic aneurysms. J Vasc Surg. 2011;54:334–340. doi: 10.1016/j.jvs.2010.12.066. [DOI] [PubMed] [Google Scholar]
- 12.Yu SY, Hsieh HC, Ko PJ, et al. Surgical outcome for mycotic aortic and iliac aneurysm. World J Surg. 2011;35:1671–1678. doi: 10.1007/s00268-011-1104-9. [DOI] [PubMed] [Google Scholar]
- 13.Sugimoto M, Banno H, Idetsu A, et al. Surgical experience of 13 infected infrarenal aortoiliac aneurysms: preoperative control of septic condition determines early outcome. Surgery. 2011;149:699–704. doi: 10.1016/j.surg.2010.12.015. [DOI] [PubMed] [Google Scholar]
- 14.Lai CH, Luo CY, Lin PY, et al. Surgical consideration of in situ prosthetic replacement for primary infected abdominal aortic aneurysms. Eur J Vasc Endovasc Surg. 2011;42:617–624. doi: 10.1016/j.ejvs.2011.07.005. [DOI] [PubMed] [Google Scholar]
- 15.Uchida N, Katayama A, Tamura K, et al. In situ replacement for mycotic aneurysms on the thoracic and abdominal aorta using rifampicin-bonded grafting and omental pedicle grafting. Ann Thorac Surg. 2012;93:438–442. doi: 10.1016/j.athoracsur.2011.07.050. [DOI] [PubMed] [Google Scholar]
- 16.Hsu RB, Tsay YG, Wang SS, Chu SH. Management of aortic aneurysm infected with salmonella. Br J Surg. 2003;90:1080–1084. doi: 10.1002/bjs.4170. [DOI] [PubMed] [Google Scholar]
- 17.Hsu RB, Chen RJ, Wang SS, Chu SH. Infected aortic aneurysms:clinical outcome and risk factor analysis. J Vasc Surg. 2004;40:30–35. doi: 10.1016/j.jvs.2004.03.020. [DOI] [PubMed] [Google Scholar]
- 18.Hsu RB, Lin FY. Infected aneurysm of the thoracic aorta. J Vasc Surg. 2008;47:270–276. doi: 10.1016/j.jvs.2007.10.017. [DOI] [PubMed] [Google Scholar]
- 19.Hsu RB, Lin FY. Psoas abscess in patients with an infected aortic aneurysm. J Vasc Surg. 2007;46:230–235. doi: 10.1016/j.jvs.2007.04.017. [DOI] [PubMed] [Google Scholar]
- 20.Hsu RB, Lin FY. Surgery for infected aneurysm of the aortic arch. J Thorac Cardiovasc Surg. 2007;134:1157–1162. doi: 10.1016/j.jtcvs.2007.07.009. [DOI] [PubMed] [Google Scholar]
- 21.Hsu RB, Chang CI, Wu IH, Lin FY. Selective medical treatment of infected aneurysms of the aorta in high risk patients. J Vasc Surg. 2009;49:66–70. doi: 10.1016/j.jvs.2008.08.004. [DOI] [PubMed] [Google Scholar]
- 22.Hsu RB, Chang CI, Chan CY, Wu IH. Infected aneurysms of the suprarenal aorta. J Vasc Surg. 2011;54:972–978. doi: 10.1016/j.jvs.2011.04.024. [DOI] [PubMed] [Google Scholar]
- 23.Hsu RB, Tsay YG, Chen RJ, Chu SH. Risk factors for primary bacteremia and endovascular infection in patients without acquired immunodeficiency syndrome who have nontyphoid salmonellosis. Clin Infect Dis. 2003;36:829–823. doi: 10.1086/367932. [DOI] [PubMed] [Google Scholar]
- 24.Soravia-Dunand VA, Loo VG, Salit IE. Aortitis due to salmonella: report of 10 cases and comprehensive review of the literature. Clin Infect Dis. 1999;29:862–868. doi: 10.1086/520450. [DOI] [PubMed] [Google Scholar]
- 25.Hsu RB, Lin FY, Chen RJ, et al. Antimicrobial drug resistance in salmonella-infected aortic aneurysms. Ann Thorac Surg. 2005; 80:530–536. doi: 10.1016/j.athoracsur.2005.02.046. [DOI] [PubMed] [Google Scholar]
- 26.Huang JJ, Ruaan MK, Lan RR, Wang MC. Acute pyogenic iliopsoas abscess in Taiwan:clinical features,diagnosis,treatments and outcome. J Infect. 2000;40:248–255. doi: 10.1053/jinf.2000.0643. [DOI] [PubMed] [Google Scholar]
- 27.Lew WK, Rowe VL, Cunningham MJ, Weaver FA. Endovascular management of mycotic aortic aneurysms and associated aortoaerodigestive fistulas. Ann Vasc Surg. 2009;23:81–89. doi: 10.1016/j.avsg.2008.08.008. [DOI] [PubMed] [Google Scholar]
- 28.Clough RE, Black SA, Lyons OT, et al. Is endovascular repair of mycotic aortic aneurysms a durable treatment option? Eur J Vasc Endovasc Surg. 2009;37:407–412. doi: 10.1016/j.ejvs.2008.11.025. [DOI] [PubMed] [Google Scholar]
- 29.Sörelius K, Mani K, Björck M, et al. Endovascular repair of mycotic aortic aneurysms. J Vasc Surg. 2009;50:269–274. doi: 10.1016/j.jvs.2009.01.001. [DOI] [PubMed] [Google Scholar]
- 30.Kan CD, Yen HT, Kan CB, Yang YJ. The feasibility of endovascular aortic repair strategy in treating infected aortic aneurysms. J Vasc Surg. 2012;55:55–60. doi: 10.1016/j.jvs.2011.07.077. [DOI] [PubMed] [Google Scholar]
- 31.Kritpracha P, Premprabha D, Sungsiri J, et al. Endovascular therapy for infected aortic aneurysms. J Vasc Surg. 2011;54:1259–1265. doi: 10.1016/j.jvs.2011.03.301. [DOI] [PubMed] [Google Scholar]
- 32.Patel HJ, Williams DM, Upchurch GR, Jr., et al. Thoracic aortic endovascular repair for mycotic aneurysms and fistulas. J Vasc Surg. 2010;52:37S–40S. doi: 10.1016/j.jvs.2010.06.139. [DOI] [PubMed] [Google Scholar]