Abstract
Background
Sudden death is a rare but real threat to hospital-based physicians and surgeons. The association between sudden death and blood pressure (BP) fluctuations in healthcare providers has not been documented. We hypothesized that work-shift loading may lead to variable BP surges in hospital-based healthcare staff, which might contribute to their development of cardiovascular disease.
Methods
Our intention is to ask 150 healthcare staff (doctors, medical technicians, and nurses) working in the coronary catheterization lab, intensive care unit, and the medical wards, respectively, to volunteer for the study. Their changes in BP would automatically be recorded every 60 minutes on an ambulatory BP monitoring machine for 24 hours during a normal workday. All events and activities would be recorded in a diary, which would allow us to coordinate BP changes with the work being done during the shift. All cardiovascular outcomes would be followed-up for a five-year duration.
Conclusions
We herein report the rationale and design of this first multicenter trial in Taiwan to explore the BP behavior associated with long work shifts in healthy hospital-based healthcare providers.
Keywords: Ambulatory blood pressure, Health-care staff, Occupation, Work shift
INTRODUCTION
While rare, sudden death on the job for healthcare workers is not unheard of, who most often succumb to cardiovascular disease (CVD). In addition to traditional risk factors documented for sudden cardiac death, only observational studies have been done for occupational risk factors, such as shift work. Shift work refers to work patterns that extend beyond the conventional 8-hour work day and that potentially disrupt workers’ normal biological or social diurnal rhythms, or both.1 Several studies have reported the adverse impacts of shift work on health. A meta-analysis2 of 17 studies showed a 40% higher relative risk of CVD both in male and female shift workers than in more traditional 8 ante meridiem (a.m.) -5 post meridiem (p.m.) daytime workers. The number of years rotating night shifts worked by American nurses was associated with an increase in the risk of developing CVD.1 This link has been increasingly highlighted most recently because shift work is common in several services, especially healthcare and other public-service systems.
Moreover, shift workers comprise a substantial segment of the working population.3 One of the associated health problems experienced by healthcare staffers is a rise in blood pressure (BP) during night work, which is a recognized occupational risk factor for CVD.4-7 Plausible explanations for this include partial adjustments of the circadian rhythms of arterial BP and modifications of sympathetic nervous system responses. In the case of shift workers, this can turn into insufficient nocturnal decreases in BP and relative increases during a sleep period after night shifts compared with daytime workers, who sleep at night. This “non-dipper” status, nevertheless, may be reversible after a day off.3 Another notable observation is the elevated risk of developing hypertension.8-10 Furthermore, the relationships between elevated BP, metabolic syndrome, and shift workers have been disclosed by other studies.11-13 Therefore, we hypothesized that increased BP variability during shift work is pivotal in the future occurrence of CVD.
Despite being caretakers of the larger public’s well-being, the health and well-being of shift-working healthcare providers are routinely neglected. In Taiwan, these healthcare providers work overtime in a highly demanding environment and have a high burnout rate.14 Hence, we focused on this population in our study. We investigated the hypothesis that shift work contributes to increased BP variability in BP, which translates into a higher risk for CVD.
MATERIALS AND METHODS
Trial design and objectives
The AMBITIOUS trial is a prospective, multicenter, observational, nonblinded trial that will be conducted using the healthcare staffs of six medical centers or regional hospitals in Taiwan. Its primary objective is to evaluate the effect of shift work on BP variability. The secondary objective is to test whether increased BP variability correlates with a higher incidence of CVD after long-term follow-up.
Selection and description of candidates
We plan to recruit 150 healthy healthcare workers from the catheterization laboratories, medical intensive care units, and medical wards in 6 hospitals. The included cardiovascular doctors and technicians working in the catheterization laboratories will be required to take part in providing emergency coronary or endovascular interventions during overnight duties. The doctors in the intensive care units work either only during the daytime or only during the night shift (from 6 p.m. to 8 a.m.). Medical doctors in the wards are in their first, second, or third year of medical residency and work night shifts for 7 to 8 days per month on average. The exclusion criteria are: (1) the presence of hypertension or taking an antihypertensive medication, (2) a history of structural heart disease, (3) a history of congenital heart disease, (4) the presence of acute illness, and (5) unwillingness to participate. The baseline characteristics, personal habits, and medication use at the start of participant enrollment will be recorded, as will the participants’ medical histories and their family members’ medical histories. BP measurement in all patients will follow the European Society of Cardiology recommendations.15 Baseline information will be recorded from renal and liver function tests, lipid profile analyses, and blood sugar tests. The research ethics committee of our hospital has approved the study, and informed consent will be obtained from all participants.
BP monitoring and device description
An ambulatory blood pressure monitoring (ABPM) device (WatchBP Office; Microlife AG, Widnau, Switzerland), which measures BP using oscillometry and has been clinically validated, will be used in our study.16 The device will be programmed to measure BP every 30 minutes from 7 a.m. until 10 p.m., and every 60 minutes from 10 p.m. until 7 a.m. The device will also be worn from 8 a.m. on a non-duty day (day 1) until 8 a.m. the next morning (day 2) (at least 48 hours apart from the last duty day), and from 8 a.m. (day 1) to 5 p.m. (day 2) on a duty day. To be considered satisfactory, an ABPM must provide at least 18 hours of readings during a non-duty day and 24 hours of readings during a duty day, with no more than a 2-hour interruption.
Study flow and procedures
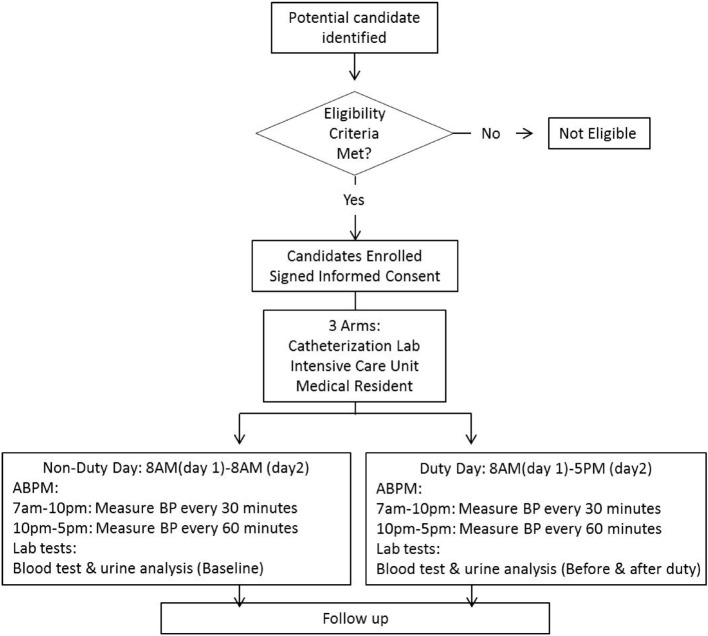
The flow chart of the study is shown in Figure 1. After providing written informed consent, candidates meeting the eligibility criteria will be enrolled from February 2014. Non-duty and on-duty day ABPM recordings from each candidate will include systolic BP (SBP), diastolic BP (DBP), and heart rate. On-duty diaries will be required. They will include the duration of duty, meal times, sleeping hours, any symptoms of illness, and whether an urgent task will be performed while on duty. Optional blood tests and urinary studies will be done before and after the ABPM recordings, if our participants agree before meals.
Figure 1.
Flow chart of participant selection in AMBITIOUS study. ABPM, ambulatory blood pressure monitoring; AM, ante meridiem; BP, blood pressure; Lab, laboratory; PM, post meridiem.
Follow up and interhospital coordination
The participants will be followed-up for at least 5 years. Any cardiovascular events and a new diagnosis of hypertension during the follow-up period will be recorded by telephone contact. The chief of the study coordinators is responsible for the organization of the study and for conducting a monthly meeting. The committee will be comprised of physicians with expertise in general cardiology and hypertension.
Data definition of ambulatory BP
The sleeping and waking periods will be based on the participants’ diaries. The recordings of SBP, DBP, and pulse pressure, during both waking and sleeping hours, after which the information will be analyzed. The nocturnal fall of SBP and DBP will also be analyzed. Abnormal SBP and DBP values for 24 hours, the waking period, and the sleeping period will be > 130/80 mm Hg, > 135/ 85 mm Hg, and > 120/70 mm Hg, respectively.5,15,17,18
Estimation of study sample size
Our case number was estimated based on one previous clinical study analyzing 10,538 subjects (age 54.4 ± 14.5, 47% males) referred for assessment of their hypertension between 1982 and 2002 in Dublin, Ireland, with 24 hour ambulatory blood pressure monitoring of adequate quality obtained off treatment.18 The average follow-up period was 5.8 years. Twenty-four hour blood pressure standard deviation values showed an inverse relationship with cardiovascular (CV) mortality (β = 0.024, Z = 3.22, p = 0.03). The prevalence rate of primary endpoints, such as CV or non-CV death, was 839/10499 = 8% (0.08). If we calculated the estimated sample size in our current study: size number will be (Z2*P * (1 - P)/d2). At the same time, due to limited study resources in this multicenter clinical trial, d was suggested to use as 10% (0.1). Finally, under a designated 5 year follow-up, the estimated sample size will be 3.22 * 3.22 * 0.08 * 0.92 * 100 = 76. We thus set the sample size as 150 for all and 50 for individual group in this relatively pilot study.
Statistical analysis
An independent, blinded research team will perform data management. If the coefficient of variation remains correlated with mean BP, a transformation, defined as the variation independent of the mean (VIM), will be derived using the formula [standard deviation (SD)]/meanx, with x estimated from the curve fitting. 17,18 Within-individual variability in SBP, DBP, and pulse pressure will be expressed as the SD and coefficient of variation (SD/mean) of readings taken over the total duration of monitoring. First, we will use average successive variability (ASV, the average absolute difference between successive values), which is affected less by trends. Second, variability over and above any linear time-trend in BP will be calculated with the residual SD: the square root of the total squared deviation of data points from a linear regression of BP values against time, divided by (n - 2), where n is the number of readings.17,18
Analyses will also be done based on whether or not the participant was on duty. We also plan to assess the mean BP and variability in both conditions. Analysis will be stratified by daytime versus nighttime; the morning surge (highest SBP from 0900 hour to 1100 hour minus the lowest from 0600 hour to 0800 hour) will also be calculated. Furthermore, to establish to what extent differences in mean BP and variability account for the effect of duty events on BP change, duty events will also be recorded in the diary. Apart from “shift work”, several other predictors may affect the BP variability. The association of these BP variability variables with cardiovascular outcomes will be assessed in Cox regression models adjusted for age, sex, BMI, smoking status, diabetes, previous cardiovascular disease, and 24-hour systolic or diastolic BP values.
The baseline health backgrounds of study participants will be compared using χ2 analysis. Independent-samples t-tests will be used to compare mean values of parametric continuous variables (expressed as mean ± SD). For nonparametric analysis, we will use Mann-Whitney U tests to evaluate the difference in levels between groups. All reported p-values will be 2-sided, and significance will be set at p < 0.05. SPSS for Windows version 17.0 (SPSS Inc., Chicago, IL, USA) will be used for all statistical analyses.
DISCUSSION
This report describes the rationale and design of the first multicenter trial in Taiwan to test the hypothesis that nocturnal work shifts have a negative effect on health because they increase BP variability, which can lead to an increase in CVD risks.
The exact mechanisms that link shift work and greater cardiovascular mortality remain unclear. Multiple biological, social, and behavioral factors appear to be responsible, however.6 One generally accepted mechanism is adaptive alterations by the autonomic nervous system, i.e., changes in circadian rhythm, BP, and heart rate.19,20 For example, several epidemiology observational studies report non-dipping of nocturnal BP during night work in healthy individuals17,18 and a higher SBP following the duty day, which is probably related to an elevated tone in the sympathetic nervous system, to behavioral factors associated with stress management, or to both.7,19,20
In this study, we will survey a younger population of healthcare workers in Taiwan, none of whom have obvious cardiovascular disease or risk factors. They are all clinical staff and are required to work extended hours and to share night duties. Given the unique characteristics of Taiwan’s healthcare employees, and the lack of local epidemiologic data, it is important to explore the effects of shift work load as an occupational risk factor for CVD. Therefore, we designed this study to investigate the interplay between different types of shift-work loadings and alterations of BP. Our findings should provide valuable local epidemiological data to increase our understanding of this potential hazard. It will also help us identify whether shift work imposes a high risk of developing hypertension, which staff populations are most at risk, and which aspects of shift work are the culprits. This kind of information will help promote occupational health; this has been an issue ignored for a long time in Taiwan, and will benefit future working-hour and shift-work-frequency policies.
In conclusion, by investigating the correlation of shift work with a higher variability in and a greater incidence of CVD in Taiwan’s healthcare workers, the present study will help healthcare employers recognize and eliminate the causes of occupationally induced hypertension and related CVD.
Acknowledgments
This study received partial funding through grants by the Taiwan Society of Cardiology, Taipei, Taiwan from 2012-2014. IRB number in National Cheng Kung University Hospital: B-ER-101-179.
DISCLOSURE
This is a physician-initiated clinical trial. Therefore, the authors are fully responsible for the concept, design, and conduct of this study, as well as all analyses performed, and reporting of the trial design and results. In addition, any relevant conflicts of interest in relation to this study have been disclosed by all authors and investigators. The study is funded by the Taiwan Society of Cardiology.
This research was also supported in part by the Headquarters of University Advancement at the National Cheng Kung University, which is sponsored by the Ministry of Education, Taiwan, Republic of China (ROC). The research was also granted from Health Promotion Program: Blood Pressure Control from Health Promotion Administration, Ministry of Health and Welfare, Taiwan, ROC and the grant from NSC101-2314-B-006-075-MY2, sponsored by the Ministry of Science and Technology, Taiwan, ROC. The investigator (Ping-Yen Liu) was granted by “A Landmark Project to Promote Innovation & Competitiveness of Clinical Trials by the Excellent Clinical Trial and Research Center in National Cheng Kung University Hospital, Mi-nistry of Health and Welfare, Taiwan”.
REFERENCES
- 1.Kawachi I, Colditz GA, Stampfer MJ, et al. Prospective study of shift work and risk of coronary heart disease in women. Circulation. 1995;92:3178–3182. doi: 10.1161/01.cir.92.11.3178. [DOI] [PubMed] [Google Scholar]
- 2.Bøggild H, Knutsson A. Shift work, risk factors and cardiovascular disease. Scand J Work Environ Health. 1999;25:85–99. doi: 10.5271/sjweh.410. [DOI] [PubMed] [Google Scholar]
- 3.Gordon NP, Cleary PD, Parker CE, Czeisler CA. The prevalence and health impact of shiftwork. Am J Public Health. 1986;76:1225–1228. doi: 10.2105/ajph.76.10.1225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stiefel P, Gimenez J, Miranda ML, et al. Ambulatory blood pressure monitoring in physicians working in a hospital: is there an increase in the number of subjects with high workplace blood pressures? Int J Cardiol. 1994;45:183–189. doi: 10.1016/0167-5273(94)90164-3. [DOI] [PubMed] [Google Scholar]
- 5.Fialho G, Cavichio L, Povoa R, Pimenta J. Effects of 24-h shift work in the emergency room on ambulatory blood pressure monitoring values of medical residents. Am J Hypertens. 2006;19:1005–1009. doi: 10.1016/j.amjhyper.2006.03.007. [DOI] [PubMed] [Google Scholar]
- 6.Schnall PL, Schwartz JE, Landsbergis PA, et al. A longitudinal study of job strain and ambulatory blood pressure:results from a three-year follow-up. Psychosom Med. 1998;60:697–706. doi: 10.1097/00006842-199811000-00007. [DOI] [PubMed] [Google Scholar]
- 7.Adams SL, Roxe DM, Weiss J, et al. Ambulatory blood pressure and Holter monitoring of emergency physicians before, during, and after a night shift. Acad Emerg Med. 1998;5:871–877. doi: 10.1111/j.1553-2712.1998.tb02816.x. [DOI] [PubMed] [Google Scholar]
- 8.Nedić O, Belkić K, Filipović D, Jocić N. Job stressors among female physicians: relation to having a clinical diagnosis of hypertension. Int J Occup Environ Health. 2010;16:330–340. doi: 10.1179/107735210799160165. [DOI] [PubMed] [Google Scholar]
- 9.Kales SN, Tsismenakis AJ, Zhang C, Soteriades ES. Blood pressure in firefighters, police officers, and other emergency responders. Am J Hypertens. 2009;22:11–20. doi: 10.1038/ajh.2008.296. [DOI] [PubMed] [Google Scholar]
- 10.Landsbergis PA, Schnall PL, Belkić KL, et al. Work conditions and masked (hidden) hypertension-insights into the global epidemic of hypertension. SJWEH Suppl. 2008;(6):41–51. [Google Scholar]
- 11.Esquirol Y, Perret B, Ruidavets JB, et al. Shift work and cardiovascular risk factors: new knowledge from the past decade. Arch Cardiovasc Dis. 2011;104:636–668. doi: 10.1016/j.acvd.2011.09.004. [DOI] [PubMed] [Google Scholar]
- 12.Li Y, Sato Y, Yamaguchi N. Shift work and the risk of metabolic syndrome: a nested case-control study. Int J Occup Environ Health. 2011;17:154–160. doi: 10.1179/107735211799030960. [DOI] [PubMed] [Google Scholar]
- 13.Phan WL, Wang JY, Liu CC, et al. Systolic blood pressure as an independent predictor of metabolic syndrome in male adolescents. Acta Cardiol Sin. 2012;28:111–117. [Google Scholar]
- 14.Chief Investment Office Wealth Management Research. (2012) Prices and earnings: a comparison of purchasing power around the globe. Retrieved from http://www.ubs.com/pricesandearnings [Google Scholar]
- 15.Mancia G, Fagard R, Narkiewicz K, et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC) J Hypertens. 2013;31:1281–1357. doi: 10.1097/01.hjh.0000431740.32696.cc. [DOI] [PubMed] [Google Scholar]
- 16.Ragazzo F, Saladini F, Palatini P. Validation of the Microlife WatchBP O3 device for clinic, home, and ambulatory blood pressure measurement, according to the international protocol. Blood Press Monit. 2010;15:59–62. doi: 10.1097/MBP.0b013e32833531ca. [DOI] [PubMed] [Google Scholar]
- 17.Rothwell PM, Howard SC, Dolan E, et al. Prognostic significance of visit-to-visit variability, maximum systolic blood pressure, and episodic hypertension. Lancet. 2010;375:895–905. doi: 10.1016/S0140-6736(10)60308-X. [DOI] [PubMed] [Google Scholar]
- 18.Bilo G, Dolan E, O’Brien E, Parati G. Blood pressure variability as a predictor of cardiovascular mortality:results of Dublin outcome study. J Hypertens. 2010;28:e209 (abstract). [Google Scholar]
- 19.Schnall P, Landsbergis P, Baker D. Job strain and cardiovascular disease. Annu Rev Public Health. 1994;15:381–411. doi: 10.1146/annurev.pu.15.050194.002121. [DOI] [PubMed] [Google Scholar]
- 20.Yamasaki F, Schwartz JE, Gerber LM, et al. Impact of shift work and race/ethnicity on the diurnal rhythm blood pressure and catecholamines. Hypertension. 1998;32:417–423. doi: 10.1161/01.hyp.32.3.417. [DOI] [PubMed] [Google Scholar]