Abstract
Background
he Multicenter Automatic Defibrillator Implantation Trial (MADIT) II showed that use of a prophylactic implantable cardioverter defibrillator (ICD) improved the survival of patients with poor left ventricular ejection fraction after myocardial infarction. The major concerns about primary ICD prevention in Asian countries are the long-term survival and the incidence of sudden cardiac death. Whether long-term outcomes within the Taiwanese population are comparable to the MADIT II trial remains unclear.
Methods
We retrospectively reviewed the clinical records of 1909 inpatients who had both myocardial infarction and heart failure in the discharge diagnoses from Jan. 2001 through Dec. 2006, and 313 patients without ICD implantation who satisfied the MADIT II criteria were included for survival analysis.
Results
After 4.60 ± 4.31 years of follow-up, 152 (49%) patients had died. Of these patients, 68 (45%) died of sudden cardiac death, similar to the conventional group (patients without ICD implantation) in the MADIT II study (51%). The Kaplan-Meier curve showed that survival during the first two years in this cohort was inferior to the conventional group of the MADIT II population. After two years, the survival curve was similar to the conventional group but still inferior to the defibrillator group in the MADIT II study. Multivariate Cox regression analysis showed old age and blood urea nitrogen > 25 mg/dL were independent predictors of mortality. A history of percutaneous coronary intervention was associated with lower mortality.
Conclusions
The long-term outcomes of Taiwanese patients who are eligible within MADIT II criteria are similar to the conventional group in the MADIT II study.
Keywords: Heart failure, Implantable cardioverter defibrillator, Myocardial infarction, Sudden cardiac death
INTRODUCTION
The Multicenter Automatic Defibrillator Implantation Trial (MADIT) II revealed that prophylactic implantable cardioverter defibrillators (ICD) improved the survival of patients who had left ventricular ejection fraction (LVEF) less than 30% with no history of ventricular tachyarrhythmia after myocardial infarction (MI).1 Accordingly, the ACCF/AHA guideline suggests ICD implantation in this population of patients.2 However, cost effectiveness is still one of the most important issues of primary ICD prevention. Whether the long-term survival and the incidence of sudden cardiac death of Asian patients are comparable to the MADIT II patients is still unclear. Two previous studies reported by Tanno et al. and Siu et al. showed that Asian patients with a previous history of MI and heart failure might have a better prognosis than the MADIT II patients.3,4 These results challenge the application of primary ICD therapy for different ethnic patients who are eligible within the MADIT II criteria. A previous report of the Taiwan Acute Coronary Syndrome Full Spectrum Registry has shown that outcomes in the Taiwanese population may differ from outcomes found in non-Taiwanese populations.5 Therefore, we sought to investigate the long-term survival of the MADIT II population in Taiwan to learn more about the prognosis of Taiwanese heart failure patients.
MATERIALS AND METHODS
This study was approved by the institutional review board of Chang Gung Memorial Hospital. We retrospectively reviewed clinical records of 1909 inpatients who were admitted for myocardial infarction from Jan. 2001 through Dec. 2006. The inclusion criteria of the MADIT II study were applied to patient selection: patients who were equal to or older than 21 years old, and patients who had LVEF less than 30% in echocardiography or left ventricular angiography were included. The exclusion criteria included: 1) patients who had indication of secondary ICD prevention or already had ICD implantation during enrollment; 2) patients who were New York Heart Association (NYHA) functional class IV; or 3) patients who had advanced cerebral disease or other terminal medical diseases. Day 1 of enrollment was defined as the 31st day after acute MI or the day of stable discharge from the hospital if the patient had remained in the hospital for a period exceeding than 31 days. Patients who were persistently unstable and/or unable to be discharged from the hospital were excluded from this study. During this period, 313 patients (230 males) who fulfilled these criteria were included in this study. We followed the definitions of the MADIT II trial,1 in that sudden cardiac death was defined as abrupt consciousness loss within one hour after the onset of acute cardiac symptoms, or death occurred within 1 day after patient was last seen alive. Non-cardiac death was defined as an alternative definite death by a cause other than cardiac diseases.
Statistical analysis
Survival curves were created by use of the Kaplan-Meier survival analysis in this study. An unpaired Student’s t-test was used to compare difference between two groups of continuous variables. Additionally, the χ2 test or Fisher’s exact test was used to test differences of categorical variables among more than 2 groups. Multivariate Cox proportional hazard regression backward analyses were conducted for predictors of survival. Statistical analysis was performed using SPSS statistical software for Windows Version 13.0 (SPSS Inc., Chicago, Illinois, USA). A p value < 0.05 was considered statistically significant, except that comparisons of continuous variables between this cohort and either group of the MADIT II study were performed using the two separate unpaired t-tests, in which a p value < 0.025 was considered significant.
RESULTS
After 4.60 ± 4.31 years of follow-up, 152 (49%) of the study patients had died. Of these patients, 68 (45%) died of sudden cardiac death, 43 (28%) of non-sudden cardiac death, 30 (20%) passed from non-cardiac death and 11 (7%) due to unknown causes. Nine patients (3%) received ICD implantation due to sustained ventricular tachycardia and/or ventricular fibrillation during the follow-up period. Eight of these 9 ICD patients were still alive at the end of the follow-up date, except one died of septic shock. The Kaplan-Meier curves of comparison between this cohort and the MADIT II study are shown in Figure 1. The survival of the Taiwanese cohort during the first two years was inferior to the conventional group (patients without ICD implantation) of the MADIT II population. After two years, the survival curve was similar to the conventional therapy group. The results indicated that the long-term outcomes of the Taiwanese MADIT II patients were comparable to the conventional therapy group of the MADIT II study. The benefit of primary ICD prevention of Taiwan patients might be similar to the MADIT II study.
Figure 1.
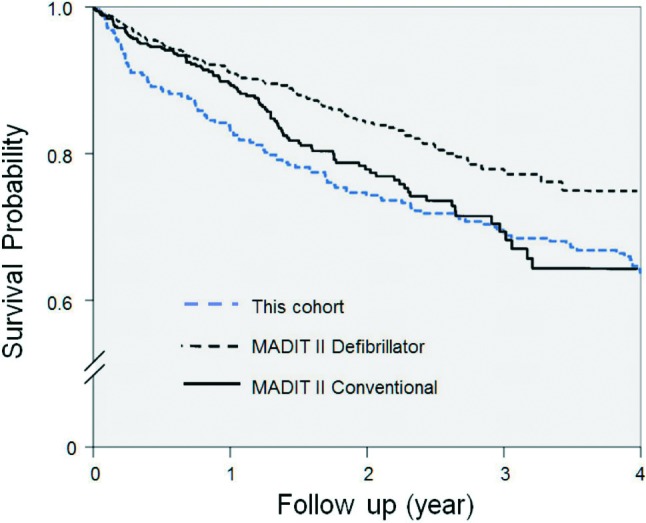
Kaplan-Meier curves of probability of survival in patients of the Taiwanese MADIT II eligible cohort. The curve of this cohort was similar to the conventional group in the MADIT II study during long-term follow-up. MADIT, multicenter automatic defibrillator implantation trial.
Comparisons of the clinical characteristics among this Taiwanese cohort and both groups of the MADIT II study are shown in the Table 1. The age of this Taiwanese cohort (67 ± 13 years) during enrollment was older than both groups of the MADIT II population (the conventional therapy group, 65 ± 10 years; the defibrillator group, 64 ± 10 years; both p < 0.025). This Taiwanese cohort had a lower rate both for current or former cigarette smoking, and for receiving percutaneous coronary angioplasty and/or coronary bypass surgery. However, this cohort had a higher prevalence of patients with blood urea nitrogen (BUN) more than 25 mg/dL and atrial fibrillation.
Table 1. Clinical characteristics .
| Characteristics | This cohort (n = 313) | MADIT II conventional (n = 490) | MADIT II defibrillator (n = 742) |
| Age | 67 ± 13* | 65 ± 10 | 64 ± 10 |
| Male sex (%) | 73* | 85 | 84 |
| NYHA functional class (%) | |||
| I | 31 | 39 | 35 |
| II | 27 | 34 | 35 |
| III | 42 | 23 | 25 |
| IV | 0 | 4 | 5 |
| Hypertension (%) | 57 | 53 | 53 |
| Diabetes (%) | 47* | 38 | 33 |
| Current or former cigarette smoker (%) | 38* | 82 | 80 |
| Coronary angioplasty (%) | 23* | 42 | 45 |
| Coronary bypass (%) | 6* | 56 | 58 |
| Atrial fibrillation (%) | 17* | 8 | 9 |
| BUN > 25 mg/dl (%) | 46* | 32 | 29 |
| QRS interval ≥ 0.12 sec | 33* | 51 | 50 |
| Non-specific conduction defect | 13* | 26 | 22 |
| Right bundle branch block | 9 | 7 | 9 |
| Left bundle branch block | 11* | 18 | 19 |
| LVEF (%) | 24 ± 5 | 23 ± 6 | 23 ± 5 |
| Medications (%) | |||
| Amiodarone | 7 | 10 | 13 |
| ACEi or ARB | 79 | 72 | 68 |
| Beta-blockers | 65 | 70 | 70 |
| Calcium-channel blockers | 5 | 9 | 9 |
| Class I antiarrhythmic agents | 1 | 2 | 3 |
| Digitalis | 13* | 57 | 57 |
| Diuretics | 63* | 81 | 72 |
| Statins | 25* | 64 | 67 |
ACEi, angiotensin-converting enzyme inhibitors; ARB, angiotensinogen receptor blockers; BUN, blood urea nitrogen; LVEF, left ventricular ejection fraction; NYHA, New York Heart Association.
* p < 0.025 in comparison among this cohort and both groups of the MADIT II study.
Comparisons of clinical characteristics between the survivors and non-survivors are shown in Table 2. The age of the survivors was significantly younger than the age of non-survivors (65 ± 12 years vs. 69 ± 13 years, p = 0.003). Significantly more patients in the survivor group received coronary angioplasty than the non-survivors (32% vs. 14%, p < 0.001). The non-survivors had a higher prevalence of elevated BUN (the percentage of BUN > 25 mg/dL was 59% vs. 40% in the conventional group in the MADIT II study, p = 0.001). Notwithstanding these several exceptions, other parameters were not different between the survivor and the non-survivor groups.
Table 2. Comparison between survivors and non-survivors .
| Characteristics | Survivors (n = 161) | Non-survivors (n = 152) | p value |
| Age (years) | 65 ± 12 | 69 ± 13 | 0.003 |
| Male sex (%) | 75 | 72 | 0.66 |
| NYHA functional class (%) | 0.48 | ||
| I | 30 | 31 | |
| II | 30 | 26 | |
| III | 40 | 43 | |
| Hypertension (%) | 58 | 57 | 0.83 |
| Diabetes (%) | 45 | 51 | 0.29 |
| Current or former cigarette smoker (%) | 40 | 36 | 0.38 |
| Coronary angioplasty (%) | 32 | 14 | < 0.001 |
| Coronary bypass (%) | 6 | 6 | 0.90 |
| Atrial fibrillation (%) | 17 | 16 | 0.82 |
| BUN > 25 mg/dL (%) | 40 | 59 | 0.001 |
| QRS interval ≥ 0.12 sec | 33 | 33 | 1.00 |
| Non-specific conduction defect | 14 | 13 | 0.90 |
| RBBB | 9 | 9 | 0.96 |
| LBBB | 11 | 11 | 0.86 |
| LVEF (%) | 24 ± 5 | 23 ± 5 | 0.19 |
| Medications (%) | |||
| Amiodarone | 6 | 9 | 0.41 |
| ACEi or ARB | 81 | 78 | 0.59 |
| Beta-blockers | 69 | 61 | 0.18 |
| Calcium-channel blockers | 5 | 5 | 0.97 |
| Class I antiarrhythmic agents | 0 | 3 | 0.06 |
| Digitalis | 13 | 15 | 0.60 |
| Diuretics | 64 | 62 | 0.76 |
| Statins | 28 | 22 | 0.27 |
ACEi, angiotensin-converting enzyme inhibitors; ARB, angiotensinogen receptor blockers; BUN, blood urea nitrogen; LVEF, left ventricular ejection fraction; NYHA, New York Heart Association.
Multivariate Cox proportional hazard regression analysis also showed that older age and BUN > 25 mg/dL were the independent predictors of mortality (Table 3). A history of percutaneous transluminal coronary intervention was associated with lower risk of mortality.
Table 3. Multivariate Cox proportional hazard model with LR backward selection .
| Predictors | HR | 95% CI of HR | p value |
| Age (per year) | 1.03 | 1.01-1.05 | 0.001 |
| PCI | 0.50 | 0.30-0.83 | 0.007 |
| BUN > 25 mg/dL | 1.81 | 1.25-2.62 | 0.002 |
BUN, blood urea nitrogen; CI, confidence interval; HR, hazard ratio; LR, logistic regression; PCI, percutaneous transluminal coronary intervention.
DISCUSSION
We had several significant findings in this study. First, the survival curve of Taiwanese patients who were eligible through incorporation of the MADIT II criteria was similar to the conventional therapy group in the MADIT II study. This finding implies that MADIT II-eligible patients in Taiwan do not have better outcomes than the conventional MADIT II population. Second, the sudden death and non-sudden cardiac death risk for the Taiwanese group was similar to the MADIT II population. The percentage of sudden cardiac death (45%) in all mortality was close to the conventional therapy group (no ICD implantation) in the MADIT II study (51%). Third, old age and BUN > 25 mg/dL were the independent predictors of mortality in this Taiwanese cohort. Percutaneous transluminal coronary intervention was associated with lower mortality. The scope of this study is not only to report the outcome of domestic MADIT II-eligible patients in Taiwan but also risk stratification. This study suggests that Taiwanese MADIT II-eligible patients have a comparable mortality rate and risk of sudden cardiac death as Caucasians. Primary ICD prevention might be considered in patients who are eligible within the MADIT II criteria.
Although this study showed that the Taiwanese cohort and the MADIT II patients had comparable outcomes, two previous studies have reported that Asian patients with a prior history of MI and heart failure had a better prognosis than MADIT II patients.3,4 There were several disparities among patients enrolled in this study and these two previous studies: Tanno et al. enrolled patients who received cardiac catheterization and Siu et al. enrolled patients who were referred for cardiac rehabilitation after ST-elevation MI. The patients in these two earlier reports differed from the population in the MADIT II study in that most of them had received coronary revascularization within the past 3 months at the time of enrollment. Patients who underwent recent cardiac catheterization and were referred for cardiac rehabilitation may have had a generally better clinical condition, and thus had lower mortality. The better outcome was also compatible with the finding of better outcome of patients who received percutaneous coronary intervention in this study. This is consistent with the idea that patients who were able to receive coronary intervention were in a generally better clinical condition, and the intervention reduced the incidence of cardiac event. In a previous report, Zheng et al. indicated that Asians had a lower overall sudden cardiac death rate than white people.6 However, two other reports showed that Asian and white patients had a similar survival rate after acute MI.7,8 Our interpretation of the discrepancy is that Asian people may have a lower incidence of MI, but the clinical outcomes after MI are similar to white people. Therefore, undertaking ICD implantation in Asian patients who satisfy MADIT II criteria might be still appropriate. However, primary ICD prevention is expensive, and cost effectiveness is still an important issue. Previous studies indicated that primary ICD prevention had acceptable cost-effectiveness in the MADIT II patients.9,10 Compared with conventional medical therapy, ICD implantation resulted in a US dollar figure cost-effectiveness of $34,000 to $70,200 per quality-adjusted life year.10 For most Asian patients, the cost of primary ICD prevention might be still higher than an acceptable threshold. Moreover, public medical insurance in most Asian countries does not reimburse the expense of most primary ICD prevention for heart failure patients. To achieve improved cost-effectiveness in the future, it will be important to look more closely at risk factor stratification.
Multivariate analyses with Cox regression showed that older age and BUN > 25 mg/dL were independent predictors of mortality. In this study, the patient population was older (67 ± 13 years vs. 65 ± 10 years) and had a higher rate of BUN > 25 mg/dl (46% vs. 32%). These facts may explain the lower survival rate in our study during the first two years compared to the MADIT II study. These results may also support earlier ICD implantation for patients with MI and heart failure because of a trend towards higher mortality in the initial 2 years after MI. However, this theory requires further supporting evidence.
Previous reports have shown that patients with chronic kidney diseases had a higher risk of death and cardiovascular events.11,12 Additionally, patients with chronic kidney diseases had a high mortality rate during the first year after developing acute MI.12,13 However, a previous study showed that ICD implantation was associated with a survival benefit among patients with mild to moderate kidney disease, but was not beneficial to patients with severe renal failure.14 In this study, we did not collect creatinine and estimated glomerular filtration rate (eGFR), which is a more appropriate indicator of renal function. When the MADIT II study was conducted from 1997 through 2002,1 the concept of eGFR as a better indicator of kidney function was not generally accepted. Until the early 2000’s, many papers about eGFR were published,15 but the impact of these articles had not yet convinced the broader general medical community of the need for eGFRs use as a reliable marker. Thereafter, when the true value of eGFR as an effective gauge later became apparent, it was then ordinarily used as a better indicator of kidney function than BUN/creatinine. Therefore, further risk stratification should be considered in ICD implantation for patients with impaired renal function, especially to exclude those patients with advanced renal diseases.
In this Taiwanese cohort, fewer patients received coronary angioplasty and coronary bypass surgery than in the MADIT II study, likely because of ethnical-cultural differences, health insurance coverage and a greater number of patients with impaired renal function. A previous report indicated that Asian patients had delayed coronary revascularization during hospitalization for heart diseases.16,17 Older Asian patients commonly fear invasive procedures, and therefore the rate of coronary revascularization was reduced. In Taiwan, the National Health Insurance covered regular bare coronary stents only when the balloon angioplasty was suboptimal. Therefore, some patients paid out of their pockets for stents, especially drug-eluting ones.
In this study, 8 of 9 patients who received ICD implantation during the follow-up period survived, except one who died of septic shock. Even though the mortality rate was low, the patient number was too small to achieve statistical significance. Therefore, further study is required for cost-effectiveness of primary ICD prevention in Taiwanese heart failure patients.
Study limitations
There were several limitations in this study. The enrolled population characteristics were different from patients in the MADIT II study. We enrolled patients one month after acute MI. Some patients did not received coronary revascularization due to clinical, economic, cultural, or personal reasons. The coronary revascularization, especially the rate of coronary bypass surgery, was significantly lower. And day 1 was defined at the 31st day - if the patients discharged stably. However, most of the MADIT II patients had longer duration from development of acute MI to the date of enrollment (57% patients > 6 months). These factors may contribute to the inferior survival rate compared to the MADIT II study in the first two years. The causes of death in some patients remained unknown in this study. Some patients were not reachable during the outpatient follow-up, and the outcomes of these patients might also influence the analyzed results. In this study, we did not collect serum creatinine and eGFR, which is a more appropriate indicator of renal function. To analyze the relationship between survival in the MADIT II eligible patients and renal function, further studies are required.
CONCLUSIONS
The survival rate of Taiwanese patients who are eligible within MADIT II criteria is similar to the conventional therapy group in the MADIT II study. The sudden death percentage in our cohort was similar to patients in the MADIT II study. Old age and BUN > 25 mg/dL were found to be independent predictors of mortality in this cohort, and a history of percutaneous coronary intervention was associated with lower mortality.
REFERENCES
- 1.Moss AJ, Zareba W, Hall WJ, et al. Prophylactic implantation of a defibrillator in patients with myocardial infarction and reduced ejection fraction. N Engl J Med. 2002;346:877–883. doi: 10.1056/NEJMoa013474. [DOI] [PubMed] [Google Scholar]
- 2.Epstein AE, DiMarco JP, Ellenbogen KA, et al. ACC/AHA/HRS 2008 Guidelines for Device-Based Therapy of Cardiac Rhythm Abnormalities: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the ACC/AHA/NASPE 2002 Guideline Update for Implantation of Cardiac Pacemakers and Antiarrhythmia Devices): developed in collaboration with the American As-sociation for Thoracic Surgery and Society of Thoracic Surgeons. Circulation. 2008;117:e350–e408. doi: 10.1161/CIRCUALTIONAHA.108.189742. [DOI] [PubMed] [Google Scholar]
- 3.Siu CW, Pong V, Ho HH, et al. Are MADIT II criteria for implantable cardioverter defibrillator implantation appropriate for Chinese patients? J Cardiovasc Electrophysiol. 2010;21:231–235. doi: 10.1111/j.1540-8167.2009.01609.x. [DOI] [PubMed] [Google Scholar]
- 4.Tanno K, Miyoshi F, Watanabe N, et al. Are the MADIT II criteria for ICD implantation appropriate for Japanese patients? Circ J . 2005;69:19–22. doi: 10.1253/circj.69.19. [DOI] [PubMed] [Google Scholar]
- 5.Shyu KG, Wu CJ, Mar GY, et al. Clinical characteristics, management and in-hospital outcomes of patients with acute coronary syndrome. Observations from the Taiwan ACS Full Spectrum Registry. Acta Cardiol Sin. 2011;27:135–144. [Google Scholar]
- 6.Zheng ZJ, Croft JB, Giles WH, et al. Sudden cardiac death in the United States, 1989 to 1998. Circulation. 2001;104:2158–2163. doi: 10.1161/hc4301.098254. [DOI] [PubMed] [Google Scholar]
- 7.Blackledge HM, Newton J, Squire IB. Prognosis for South Asian and white patients newly admitted to hospital with heart failure in the United Kingdom: historical cohort study. BMJ. 2003;327:526–531. doi: 10.1136/bmj.327.7414.526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mukhtar HT, Littler WA. Survival after acute myocardial infarction in Asian and white patients in Birmingham. Br Heart J. 1995;73:122–124. doi: 10.1136/hrt.73.2.122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Al-Khatib SM, Anstrom KJ, Eisenstein EL, et al. Clinical and economic implications of the Multicenter Automatic Defibrillator Implantation Trial-II. Ann Intern Med. 2005;142:593–600. doi: 10.7326/0003-4819-142-8-200504190-00007. [DOI] [PubMed] [Google Scholar]
- 10.Sanders GD, Hlatky MA, Owens DK. Cost-effectiveness of implantable cardioverter-defibrillators. N Engl J Med. 2005;353:1471–1480. doi: 10.1056/NEJMsa051989. [DOI] [PubMed] [Google Scholar]
- 11.Go AS, Chertow GM, Fan D, et al. Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med. 2004;351:1296–1305. doi: 10.1056/NEJMoa041031. [DOI] [PubMed] [Google Scholar]
- 12.Chertow GM, Normand SL, Silva LR, McNeil BJ. Survival after acute myocardial infarction in patients with end-stage renal disease: results from the cooperative cardiovascular project. Am J Kidney Dis. 2000;35:1044–1051. doi: 10.1016/s0272-6386(00)70038-2. [DOI] [PubMed] [Google Scholar]
- 13.Herzog CA, Ma JZ, Collins AJ. Poor long-term survival after acute myocardial infarction among patients on long-term dialysis. N Engl J Med. 1998;339:799–805. doi: 10.1056/NEJM199809173391203. [DOI] [PubMed] [Google Scholar]
- 14.Goldenberg I, Moss AJ, McNitt S, et al. Relations among renal function, risk of sudden cardiac death, and benefit of the implanted cardiac defibrillator in patients with ischemic left ventricular dysfunction. Am J Cardiol. 2006;98:485–490. doi: 10.1016/j.amjcard.2006.03.025. [DOI] [PubMed] [Google Scholar]
- 15.Stevens LA, Coresh J, Greene T, Levey AS. Assessing kidney function -- measured and estimated glomerular filtration rate. N Engl J Med. 2006;354:2473–2483. doi: 10.1056/NEJMra054415. [DOI] [PubMed] [Google Scholar]
- 16.Carlisle DM, Leake BD, Shapiro MF. Racial and ethnic differences in the use of invasive cardiac procedures among cardiac patients in Los Angeles County, 1986 through 1988. Am J Public Health. 1995;85:352–356. doi: 10.2105/ajph.85.3.352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Feder G, Crook AM, Magee P, et al. Ethnic differences in invasive management of coronary disease: prospective cohort study of patients undergoing angiography. BMJ. 2002;324:511–516. doi: 10.1136/bmj.324.7336.511. [DOI] [PMC free article] [PubMed] [Google Scholar]


