Abstract
Problem and its significance
Perceived benefits of rapid response teams (RRTs) impact their sustained use. Perceived benefits are particularly important for RRT sustainment when limited RRT data is shared with organizational members. Nurse leaders' perceived benefits of RRTs likely influence their support for RRTs, crucial for sustained RRT use. Little is, however, known of nurse leaders' perception of the benefits of RRTs. This study will examine and compare nurse leaders, RRT members, and RRT users perceived benefits of RRTs.
Study design
Qualitative, semi-structured interviews were conducted as part of a larger mixed-methods study examining RRT sustainability. Interviews were conducted at four community hospitals and nurse leaders, RRT members, and RRT users were targeted for interviews.
Sampling method
Purposive and snowball sampling was used. Recruitment strategies included email and list-serve announcements, on-site presentations, direct personal contact, and a study flyer.
Important findings
All participants reported perceived benefits from RRTs to the organization, to staff members, and to patients. Variations were, however, observed between nurse leaders, RRT members, and RRT users.
Important conclusions
Nurse leaders' perceptions were focused on macro-level benefits, whereas RRTMs focused on the learning and teaching aspects RRTs offer, and RRTUs on the psychological support RRTs provided.
Introduction
Organizational members' perceived benefits of RRTs facilitate the sustained use of RRTs. Understanding the perceived benefits of RRTs is important because perceived benefits of programs, even in the absence of actual benefits, is associated with their continued use by staff members and long-term sustainability. Research studies have explored the benefits of rapid response teams (RRTs) as perceived by physicians and nurses. Little is, however, known of how nurse leaders' perceive the benefits of RRTs and how their perceptions compare with those of RRT members (RRTMs) and RRT users (RRTUs). Yet, nurse leaders' support is an important aspect of successful RRT implementation and use; their support is most likely influenced by their perception of RRT benefits. Also, nurses' views are underrepresented because of the small number of nurse participants in various studies of perceived RRT benefits. Because studies have also been conducted in single institutions, nurses' views are also often limited to a single hospital context. This study improves on these limitations by exploring and comparing the views of nurse leaders, RRTMs and RRTUs from four different organizations. Understanding the perceptions of nurse leaders, RRTMs, and RRTUs is important for several reasons. Staff members' perception of RRT benefits may be a reflection of what staff value the most, which can potentially be used as a leverage by nurse leaders to enhance adherence to calling criteria and guiding training efforts by staff development experts. Knowledge of the perceived benefits reported may also steer the mobilization of the necessary resources to support RRT programs to ensure their sustainment, and guide RRT marketing and advertising to staff members and patients and families and RRT program-related quality improvement efforts.
Background
Rapid response teamsare teams that have been implemented as a way for organizations to quickly respond to patients on acute care units who show signs or symptoms of acute clinical deterioration or when a pre-determined objective (such as a heart rate less than 40/minute) or subjective (such as nurse is worried) RRT calling criteria are met (Arashin, 2010; Winters et al. 2013). Depending on organizational policies, an RRT can be initiated by staff members, and patients or their family members. RRT member functions include the rapid assessment and care of the patient in crisis guided by RRT policies and protocols and initiating RRT order sets when available. RRT members may, for example, order laboratory tests and X-rays, start or titrate oxygen therapy, and initiate the transfer of the patient to the critical care unit.
RRTs have the potential to improve both patient and organizational outcomes (see Table 1). Improved patient outcomes associated with RRT implementation include decreased cardiac arrest rates outside of Intensive Care Units (ICUs) (Chan et al., 2010), lowered unanticipated ICU admissions (Salamonson, Van Heere, Everett, & Davidson, 2006; Garretson et al., 2006)and decreased hospital mortality rates (Cretikos et al., 2006; Garretson et al., 2006). Organizational outcomes include enhanced quality and safety of care (Berwick, Calkins, McCannon, & Hackbarth, 2006; Sarani et al., 2009; Williams, Newman, Jones, & Woodard, 2011), enhanced nurse satisfaction (Metcalf et al., 2008) and staff collaboration (Williams et al., 2011), and enhanced physician and nurses' skills and knowledge about managing severely ill patients (Azzopardi, Kinney, Moulden, & Tibbals, 2011; Williams et al., 2011).
Table 1.
Patient and Organizational Outcomes Reported.
| Patient Outcomes | Organizational Outcomes |
|---|---|
| Decreased cardiac arrest rates outside of ICU* | Improved quality and safety of care |
| Decreased unanticipated ICU* admissions | Enhanced nurse satisfaction |
| Decreased hospital mortality rates | Enhanced staff collaboration |
| Enhanced physician and nurses' skills and knowledge about managing severely ill patients |
Note.
ICU = Intensive Care Unit
The perceived effectiveness of RRTs can impact their use on hospitals. Even in the absence of objective evidence of effectiveness, the perception of benefit of a program such as RRTs can support the ongoing use and sustainability of the program (Scheirer, 2005; Commins & Elias, 1991; Goodman & Steckler, 1989). The continuation of programs is also likely when they are valued by staff members and considered as needed. Furthermore, when staff perceive programs to foster their own goals and aspirations, they are more likely to support a program.
The sustained use of RRTs in hospitals is largely dependent on staff members' ability to recognize the need for an RRT and their willingness to activate an RRT call. These staff members may not be aware that organizational data on the effectiveness of the RRT program, (e.g., patient mortality rates, unanticipated intensive care unit [ICU] admissions, and cardiac arrest rates outside of the ICU) are being collected, and the results may not be communicated to them on a regular basis. Thus, staff decisions to call the RRT may depend largely on their perception of RRT benefits, to themselves and their patients, when activating RRT calls rather than on objective measures of effectiveness. Several studies support the linkage between the perception of RRT benefits and RRT activation. Sarani et al. (2009) reported that the physicians and nurses who perceived RRTs to improve patient safety were more likely to activate and call the RRT than those who did not perceive these benefits. More recently, Davies, DeVita, Ayinla, & Perez (2014) found that as the perception of benefit from RRT activation increased, adherence rates to activation criteria increased.
Nursing staff perceive several benefits from having a RRT program available in the hospital (see Table 2). Perceived benefits include: improved staff morale and teamwork, redistribution of nurses' workload, and the escalation of care of patients who were acutely deteriorating on patient care units (Benin, Borgstrom, Jenq, Roumanis, & Horwitz, 2012; Astroth, Woith, Stapleton, Joseph-Degitz, & Jenkins, 2013). Other perceived benefits also include the immediate attention and early intervention that the RRT provided, having a backup system that was always available, particularly when staff was worried about the patient, because it gave them peace of mind and a sense of security; and access to medical experts who knew how to manage emergency situations (Salamonson et al., 2006). RRTs are perceived to also bring valuable expertise, facilitate patient transfers to the ICU, and the rapid care of patients in crisis on nursing units. (Shapiro, Donaldson, & Scott, 2010).
Table 2.
Reported Perceived Benefits of RRTs.
| Perceived Benefits of RRTs | |
|---|---|
| Escalation and rapid care of patients in crisis | Having a backup system that is always available, especially when staff is worried |
| Facilitation of patient transfer to ICU | Improved staff morale and teamwork |
| Immediate attention and early intervention | Redistribution of nurses' workload |
| Access to critical care experts | Nurses gain peace of mind and a sense of security |
Note. * ICU = Intensive Care Unit
Unfortunately, studies that have reported the perceived benefits of RRTs have focused predominantly on examining the perceptions of physicians and Registered Nurses (RNs) (Azzopardi et al., 2014; Davies et al., 2014) or only RNs (Shapiro et al., 2010; Salamonson et al., 2006). One study examined the perceptions of benefit of administrators, but only eight administrators were included in the study (Benin et al., 2012). Little research has been conducted to examine and compare the perceptions of nurse leaders with RRT members and RRT users. Furthermore, studies were limited to single institutions (Davies et al., 2014; Benin et al., 2012; Azzopardi et al., 2011) and, due to low response rates, small numbers of nurses participated with numbers ranging from 16 (Davies et al., 2014) to 18 (Benin et al., 2014). Thus, the view of nurses may not have been fully captured in these studies. As part of a larger two-phased, mixed-methods study examining RRT sustainability, interviews were conducted with various staff members to understand the perceived benefits of RRTs (Stolldorf & Jones, 2015; Stolldorf, Havens, & Jones, 2015; Stolldorf, Mion, & Jones, 2015). In the first phase, the sustainability of RRTs was measured using a survey methodology. In the second phase, multiple-case studies were conducted with a sample of four hospitals that participated in the first phase of the study to understand the factors and contexts and processes associated with RRT sustainability. This paper leveraged data obtained from that study with the purpose to understand the benefits of RRTs as perceived by nurse leaders, RRT members (RRTMs), and RRT users (RRTUs).
Methods
Design
Qualitative, semi-structured interviews were conducted. A semi-structured interview guide was designed and used, but adapted at the time of the interview to fit with the type of individual interviewed (i.e., nurse leader, RRTM, or RRTU).
Setting and Sample
This study was conducted at four community hospitals that participated in a statewide collaborative to implement and sustain RRTs. Hospitals varied in size of 200 to 300 licensed and staffed beds and, at the time of the study, their RRTs have been in place for at least 4 years.
Individuals from three specific groups were targeted for interviews because of their knowledge and experience and their potential to share information about RRTs from different organizational perspectives. These groups included organizational leaders, RRT members who previously or currently respond to RRT calls, and RRT end-users who were affiliated with patient care areas where RRT calls could be activated and may or may not previously have activated a RRT call. Given the qualitative design, an a priori sample size was not set. Instead, sample size was determined by when data saturation (i.e., the point at which no new information or themes emerged from the data) was reached (Polit & Beck, 2012). Other factors considered to affect the sample size of this study included the narrow scope of the study and the knowledge and experiences of those interviewed. In the presence of these factors, a small number of participants could be considered sufficient to achieve data saturation (Polit & Beck, 2012). The researcher also anticipated that the number of leaders involved in RRT implementation and sustainment efforts might be limited which would further limit the sample size for this group.
To identify potential participants, purposive and snowball sampling was used. Organizational leaders were asked at the time of the first on-site visit, to identify potential participants and knowledgeable about RRTs. When permitted, organizations' RRT logs were reviewed to identify potential participants, both RRTMs and RRTUs. In cases where a list-serve was available for any one of the targeted participant groups, the recruitment letter was distributed via the list-serv. At the end of each interview, all participants were asked to identify potential participants. All potential participants identified were subsequently contacted by the researcher and provided with the recruitment letter and consent form. Recruitment strategies included email and list-serve announcements, on-site presentations at relevant meetings, direct personal contact, and a study flyer. A small incentive was offered to enhance participation (Krueger & Casey, 2009: Polit & Beck, 2004).
Data Collection
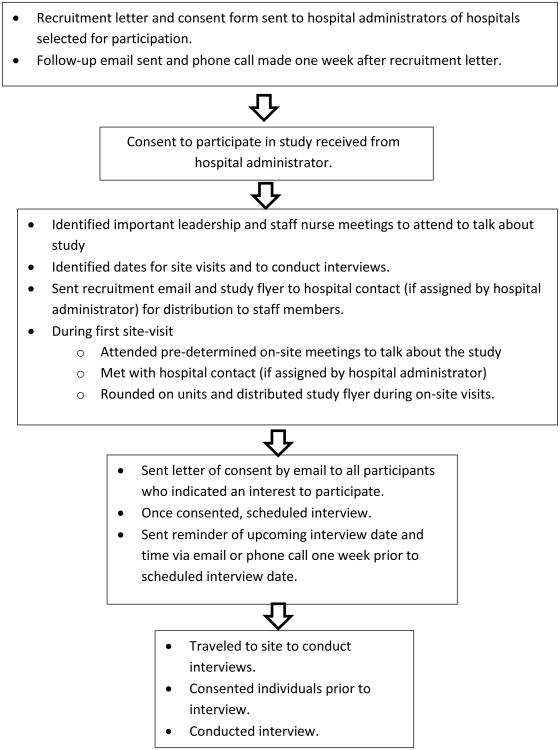
Data were collected through semi-structured, in-person interviews, however, in case of scheduling conflicts, telephone interviews were conducted. For practical reasons, interview dates were pre-determined in collaboration with hospital administration and occurred at a time that was convenient for each participant. Interviews lasted 30-45 minutes and were audiotaped and transcribed. All participants provided oral consent prior to the beginning of the interview. Please see Figure 1 for details about data collection procedures.
Figure 1.
Data Collection Procedures
Ethical Considerations
Institutional review board approval was received prior to the start of the study. Each participant received an informed consent form prior to the interview and verbal consent was obtained at the beginning of each interview. Steps to protect the identity of participants included the use of pseudonyms to replace the name of a participant and the group (i.e., leadership, RRTM, or RRU) and the hospital they represented. To allow for a comparison of findings across groups of participants, pseudonyms consisted of a color code for each hospital (e.g., blue) and a number code for each group with the hospital's pseudonym to include the number 1 for the leadership group (e.g., Blue 1), the number 2 for the RRT member group (e.g., Blue 2), and the number 3 for RRT users (e.g., Blue 3). Individuals within groups were assigned their hospital's pseudonym, their group within the hospital's code, and a letter of the alphabet (e.g., Blue 1.A).
Data Analysis
Data analysis commenced once the accuracy of the transcribed interviews were verified and the data were imported into the computer software program ATLAS ti. (Version 4.2., Berlin, 1999). Miles and Huberman's (1994) steps in data analysis (i.e., data reduction, data display, and conclusion drawing or verification) guided the analysis process. Data reduction consisted of an initial content analysis of the data (Grbich, 2007), that is, a process to systematically code and categorize the data. Data were coded in collaboration with faculty advisors and a qualitative research expert at a local research instituted. To facilitate comparison across groups and across hospitals, following the content analysis data were compressed and displayed in tabular format (i.e., data display) (Miles & Huberman, 1994). The constant comparison method was used to look for patterns in the data (i.e., pattern-matching logic) between the various groups. The researcher sought to determine whether similar patterns were found in the different groups, with regard to the perceived benefits of RRTs for the organization, patients, and staff members.
Results
Semi-structured interview questions elicited responses from participants about what benefits they perceived RRTs offered to the hospital, to staff members, and to patients.
Sample
A total of 50 interviews were conducted with organizational leaders, RRT members, and RRT end-users. The number of participants interviewed is reported by hospital and by group in Table 3. Despite extensive recruitment efforts and support from hospital staff, no physicians affiliated with the four hospitals agreed to participate and no additional nurse participants volunteered to participate. Yet, because of the small scope of the study and the knowledge of those who participated in interviews, data saturation was reached and no new themes emerged from the interviews across the four hospitals.
Table 3.
Participants by Hospital and by Group.
| Hospital A | Hospital B | Hospital C | Hospital D | Total | |
|---|---|---|---|---|---|
| Leadership | 3 | 8 | 5 | 3 | 19 |
| RRT Members | 6 | 1 | 2 | 2 | 11 |
| RRT Users | 4 | 5 | 6 | 6 | 20 |
|
| |||||
| Total | 14 | 12 | 13 | 11 | 50 |
Organizational leaders that participated in interviews included nurse managers of units where RRTs could be activated, nurse leaders involved in the implementation and monitoring of the RRT program, nurses overseeing quality improvement initiatives related to the RRT program, and nurse educators who oversaw RRT program related educational initiatives. RRT members that were interviewed included nurses working in critical care units or the emergency department. The RRT end-user group consisted of nurses who worked on units where RRTs could be activated and included both clinical nurse leaders, charge nurses, and bedside nurses from these units. At the one facility where the researcher had access to RRT logs to collect RRTM and RRTU names and contact information, the response rate to the email invitation to participate in the study was 20%. At all other sites, an administrator distributed study recruitment materials through list serves and postings on bulletin boards. Next, the responses of the three groups of participants, namely leadership, RRT members, and RRT end-users, are reported and compared for each category of benefits (i.e., the organization, staff members, and patients) (see Table 4).
Table 4.
Perceived benefits by Group.
| Benefits Reported | Groups Interviewed | ||
|---|---|---|---|
|
| |||
| Leadership | RRTM | RRTU | |
| Organizational Benefits | |||
| Promoting positive patient outcomes such as decreased length of stay and unanticipated ICU admission. | +++ | ++ | ++ |
| Promoting organizational outcomes such as quality of care and patient safety | +++ | +++ | +++ |
| Enhance patient perception of care | +++ | +++ | +++ |
| Reduce cost | +++ | ++ | ++ |
| Improve patient and staff satisfaction | +++ | - | - |
|
| |||
| Staff Benefits | |||
|
| |||
| Getting expert help | +++ | +++ | +++ |
| RRTU learning: Gaining knowledge, skills, and expertise | ++ | +++ | ++ |
| Supporting end-users | +++ | +++ | +++ |
|
| |||
| Patient Benefits | |||
|
| |||
| Early recognition and intervention | +++ | ++ | ++ |
| Better patient care | ++ | ++ | +++ |
| Enhanced patient safety | ++ | ++ | +++ |
Notes. (+) = Degree to which theme emerged during interviews with a higher number of (+) indicating the topic was mentioned more often in interviews compared to other groups. (-) = Theme did not emerge during interviews. ICU = Intensive Care Unit; RRTM = Rapid Response Team Member; RRTU = Rapid Response Team End-user.
Perceived Benefits of RRTs to the Organization
Participants in each of the three groups perceived RRTs to benefit the organizations that have implemented these teams. Most participants highlighted organizational benefits in terms of RRTs promoting positive patient (i.e., reduced cardiac arrest rates outside of critical care) and organizational outcomes (i.e., quality of care, patient safety) and enhancing the community's perception of the hospital.
Promoting positive patient and organizational outcomes
The majority of participants noted positive patient and organizational outcomes. However, all leaders mentioned RRTs promoting positive patient outcomes, compared to just over half of RRTMs and RRTUs. These outcomes include reduced ICU admissions and patients' length of stay, and improved patient safety as reflected by reduced patient morbidity and mortality following RRT adoption and implementation. As one nurse leader noted, “Our codes have went [sic] down; our ventilator days have went [sic] down so again the patient safety falls into that.” This viewpoint was shared by RRTMs who perceived the availability of an RRT to reduce the risk of ICU admissions and risk of increased length of stay of patients because further deterioration was prevented. As one participant observed, “… once you put someone on a ventilator, once you code somebody, leaving the hospital becomes … dramatically comes down.” Similarly, a RRTU noted that, “… we have less codes, less deaths because of that, better patient outcomes, better satisfaction from the families knowing that somebody's there because the families can use that too.”
Some participants perceived RRTs to reduce the risk for litigation because “… if ever something were to go to lawsuit or to the courts, it definitely will probably give us some support and say we did initiate this [RRT] and the outcomes from that.”
Enhancing community perceptions
Participants in all three groups agreed that the presence of an RRT in the organization help to enhance community members' perception of the hospital because patients who experienced a RRT intervention while in the hospital were likely to share their experiences with others in the community. Participants perceived the ability for patients and families to call an RRT sends a message that, “ … the facility cares about patients and their families and that the patients are going to get the care they expect to get.” Participants in both the leadership and RRTU group noted that the availability of RRTs enhanced patient perception of the care they received. Specifically, participants noted that positive patient experiences with RRTs would enhance patients' outlook on the hospital and the care they received which would increase their comfort to return for care to the same facility. One nurse leader observed that when RRTs intervene early and patients get well, “… they [patients] talk so they get that out to the public, how the hospital took care of them, how their nurses on that floor took care of them … they fixed me up kind of thing.” Similarly, a RRTU noted that patients feel more comfortable and safe coming to the hospital for care because having the ability to intervene early by calling an RRT “… gives you a better reputation of helping people. You have that good reputation of being able to provide care and that means a lot to the community. They kind of feel safe.”
Reducing cost, improving satisfaction
All three groups also reported a perception that RRTs reduced cost and improved the cost-effectiveness of care because of reduced cardiac arrest rates and the need for subsequent critical care. As one nurse leader noted, “… if you see a change and you can get to it before it gets too acute, then you can save on length of stay or you can cut the cost in patient days for the patients staying longer.” An RRTM also observed, “They decrease diverse events or more serious events overall. I think they're a cost reducer.”
A large number of nurse leaders reported RRTs improving nurse and patient/family satisfaction; however, this was rarely mentioned by RRTMs and RRTUs. As one leader observed: “They're [patient] going to be appreciative that there's a lot of staff coming to take care of them quickly. So their satisfaction scores would be increased I would think for the patient that got RRT.”
Perceived Benefits of RRTs to Staff Members
When participants were asked about the benefits of RRTs for staff members, several themes emerged. These include getting expert help, gaining knowledge, skills, and expertise, and supporting end-users, including their psychological well-being.
Getting expert help
Nearly half of the participants in each of the three groups (i.e., leadership, RRTMs, and RRTUs) noted that the RRT provided end-users with expertise. One participant describes the benefit as “You've got Critical Care Nurses that responds, and Respiratory Therapists that are more trained to handle cardiac and respiratory distress issues.” Another participant noted “So even though the patient doesn't always go to the unit they can help you solve problems … give you advice because they are from the units [ICU] and they take care of emergencies more than we [RRTU] do.”
Nurse leaders in particular, believe that staff members benefit because they know that an experienced critical care nurse is available when they have questions, someone that they can have confidence in, and that they can get a second opinion when they need one. They perceive RRTUs benefit by the facility having a RRT because, “A med-surgnurse does not know a lot about how to treat someone with a heart attack. So, they get somebody that is maybe more knowledgeable about what is going on with the patient and can help him out.”
Learning, gaining knowledge, skills, and expertise
Participants in each of the three groups noted RRTU's learning as an important benefit from RRT implementation. One participant thought that RRT calls were a, “… teach-back moment at the point of care. Most of the critical care nurses … are very informative, and they are explaining as their doing. It gives them [RRTUs] some critical thinking skills, as well as the opportunity to learn.” Participants noted that learning occurs during RRT calls through instruction and observation. Some RRTMs noted they use RRT calls as learning opportunities for RRTUs through teaching and explaining and that they have seen evidence of learning through RRTUs improved preparation for the team's arrival following the call (e.g., having intravenous fluids and the crash cart on hand should it be needed).
One participant compared RRTs to a “live lab” and noted the following about RRT calls: It's not a simulation, it's the real thing, and even if they're not talking and doing a didactic teaching, the nurses are watching them and they're watching how they do an assessment, and they watch the communication. They hear the communication with the physician, so it is a very rich learning environment for the next event, next patient.
Gaining knowledge, skills, and expertise was also noted as a benefit; however, compared to leadership and RRTUs, RRTMs were more likely to report this as a benefit. RRTMs perceived that RRTUs gain the knowledge, skills, and expertise of RRT members who intervene on behalf of the RRTU to prevent further patient deterioration. As one RRTM noted, “I think it's having somebody that's there to help you that has the knowledge…. It's somebody to share that [knowledge] with and you can look to their knowledge and you're still helping and you're learning too.”
Supporting end-users
Nearly half of all participants in each group reported that RRTs provide support for RRTUs. RRTUs reported that knowing that the RRT is available when needed is comforting to them and they feel supported. As one participant noted, “To me I feel like, I feel more comfortable knowing that I have a specialized person there”.
Participants in all three groups highlighted the mental or psychological support that the availability of RRTs offers to RRTUs. However, this was reported more often by RRTUs than by any of the other groups. Participants perceived that RRTs give RRTUs, in particular, a sense of security and help them to reduce their work stress. This stress was believed to be reduced because a critical care expert stepped in to help manage the patient in crisis, skills RRTUs are less familiar with or lacking.
As one RRTU noted:
I feel more comfortable knowing that I have a specialized person there. It makes you more confident. It makes you more -- feel better that your patients are going to be taken care of, that nothing's going to go wrong; everything's going to be okay. For a nurse that's a big deal.
As one leadership participant noted:
Security knowing that there's someone there. Their [RRTUs] days are hard enough and stressful enough with the caseload they have, and you have your set of patients and you know you have someone that's getting unstable and you're trying to allot your time. Having that safety net, that expert to come and help you identify a problem, helps with their whole work flow and their ease.
Perceived Benefits of RRTs to Patients
Participants in each of the three groups reported several benefits to patients. These included early recognition and intervention, better patient care, and enhanced patient safety.
Early recognition and intervention
Although noted more often by nurse leaders than RRTMs and RRTUs, early recognition and intervention was noted as an important benefit of RRT implementation. As a nurse leader noted, “They [patients] are assessed by an advanced care professional, so occasionally they're able to intervene before a crisis happens.” Another nurse leader noted, “We're going to catch things sooner. If it's a STEMI or anything like that, the EKG is going to show. You got access to Respiratory if some kind of changes happen to the respiratory status.”
Timeliness of care was thought to be important because the RRT promoted early recognition of patient problems and interventions to address them. For example an RRTM noted, “They [patients] get treaty quicker. They get quicker labs, better respiratory [sic] and that gives better outcomes rather than processing out into a full code blue.”
One RRTU noted:
I think they get a much more rapid treatment than waiting on a physician to maybe come from their office. The Rapid Response Team has standing orders that they can initiate so sometimes you can have several things done before the physician even gets there. You can have blood work. You can have a chest x-ray. You can have blood gases. That's certainly beneficial and they can transfer to the ICU… then that's a much more earlier intervention for the patient.
Better patient care
Because RRTs can intervene earlier and provide additional care or transfer the patient to higher levels when needed, participants believed that RRTs enhance the care provided to patients on acute care units. Although participants in each of the three groups perceived better care, it was noted more often by RRRUs than nurse leaders or RRTMs. Nurse leaders perceived RRTs to enhance patient care because early RRT interventions help to reduce complications. As one nurse leader noted, “Well I think you're delivering better patient care and it could be the difference of getting somebody through a respiratory distress versus being on a ventilator that requires many more days.” RRTMs perceived enhancing patient care as in integral part of their role: “I [RRTM] would say patient care. I mean it still comes down to that's why you're here and what you're doing.” Because of the timeliness of care and the expertise of RRTMs, RRTUs perceived RRTs to also enhanced patient care, “Quicker care, more precise. The more knowledge of nurses you have the faster you're going to get the care that you need and the better, more effective.”
As another RRTU noted:
Better care, just better care … like rapid response to maybe low blood pressures or low O2 Sats or level of consciousness drop or just trouble breathing just any problems that they may have to be more adequately cared for. When the patient is in the correct level of care in the hospital and when you feel that you're satisfied that the patient is at the right place, at the right time, or everybody is notified and safety.
Enhanced patient safety
Although participants in all three groups believed that the safety of patients is enhanced, it was noted far more by RRTUs than by nurse leaders or RRTMs. Patient safety is believed to be enhanced in several ways. First, in the words of a RRTU: “Because it's [RRTs] for their safety, for improved care, for improved outcomes.” Second, as evident by one RRTU's response, safety is enhanced by providing the right level of care to the patient when in crisis:
I think it helps save lives 100% … because we get them where they need to go when they need to go. Because the patient can change just like that and if you don't have a CCU bed, you've got a CCU nurse that can stay with them and manage them until we get them upstairs[CCU].
Third, RRTs are perceived to enhance patient safety because complications and trauma to the patient are prevented. As a RRTM noted, “Snatching them before they code…. we've been able to reverse whatever is going on …they get to stay in the room …they saved from a longer protracted problem …” Similarly, a RRTU noted that RRTs, “… would minimize trauma for the patient, both mentally and physically. Because if they're scared then that's a mental trauma and if they feel confident that staff knows what they're doing then that minimizes that.”
Discussion
Participants in all three groups perceived RRTs to hold benefits for the organization, for staff, and for patients. However, some differences were observed between the benefits reported by nurse leaders, RRTMs, and RRTUs.
Nurse leaders' perceptions of benefit of RRT implementation were more at the macro-level of the organization than at the micro-system or intervention level. Nurse leaders perceived RRTs to improve patient outcomes such as length of stay and reduced ICU admissions. Compared to staff nurses, nurse leaders are more likely to receive information on RRT call trends and outcomes on a regular basis, increasing their awareness of the impact of RRTs on the outcomes such as length of stay and ICU admission rates. Nurse leaders are also more likely to be cognizant of patient/family and nurse satisfaction, measures that are key indicators of the hospital's and unit's performance and the nursing work environment. Therefore, nurse leaders' awareness of staff nurses' work stress and their need for additional support and guidance for caring for higher acuity patients and patients with acute, critical needs may be more pronounced.
RRTMs focused more on the learning opportunity RRTs offer as a perceived benefit. Following RRT calls, RRTMs often conduct debriefing and provide feedback to RRTUs. These are ideal opportunities for learning and to enhance the knowledge and skills of RRTUs and better prepare them for subsequent RRT calls. The impact of these learning opportunities on RRTU behavior was observed and was reflected in improved RRTU responses to RRT calls. For example, following the RRT call, RRTUs were more likely to anticipate and gather the necessary supplies and equipment (i.e., crash cart, oxygen, intravenous infusion supplies) to be used during the RRT call. RRTMs are often highly trained individuals with critical care expertise. Therefore it is not surprising that they believed that their knowledge, skills, and expertise are of great benefit to RRTUs during RRT calls.
RRTUs highlighted the psychological support that RRTs offer far more than the other two groups. Because a critical care expert can intervene on their behalf, the opportunity to activate a RRT call gives them a sense of security and support and reduces their work stress. RRTUs also perceived more so the opportunity RRTs offer to provide better care to their patients in crisis. RRTMs, as critical care experts, augment the skills of RRTUs by providing early intervention and more precise, effective care to patients in crisis. RRTUs also focused more on the safety aspect of care that RRTs offered. Care can be escalated and patients can be transferred quicker, and critical care nurses can manage the patient in crisis on the floor while waiting for an ICU bed to become available.
Most of the findings of this study are in alignment with previous studies. The perception of benefit to the organization, staff members, and patients align with previous reports (Azzopardi et al., 2011; Berwick et al., 2006; Cretikos et al., 2006; Garretson et al., 2006; Metcalf et al., 2008; Salamonson et al., 2001; Williams et al., 2011). However, some perceived benefits reported in this study have not been noted previously. Specifically, the perceived benefit that RRTs reduce the hospital's risk for litigation, that RRTs reduce the cost of care, and that RRTs enhanced a community's perception of RRTs have not previously been reported. It should be noted that these are only perceived and not actual benefits. Future research should explore if these perceived benefits translate into actual benefits.
Limitations
Some limitations of the study should be noted. Despite all recruitment efforts, only a select few RRTMs participated in the study. Therefore, the views of RRTMs are underrepresented. Although physician recruitment was attempted, only one physician was recruited and, due to the lack of physician respondents, their data were subsequently excluded from the analysis. A higher number of participants within each group within individual hospitals would also have enhanced the robustness of the data and would have increased the trustworthiness of the findings. Conducting in-person interviews increase the risk of respondent bias, however, this risk was reduced by asking neutral questions and maintaining a neutral tone of voice and expression during interviews, and, ensuring participants of the confidentiality of their responses.
Recommendations for Practice, Policy, and Future Research
The study offers some recommendations for practice, policy, and future research. Organizational policies should include the sharing of RRT trends and outcomes with not only nurse leaders but also staff members. A better understanding of patient/family satisfaction may be gained by asking RRT specific questions in survey about patient/family members/knowledge about the availability of RRTs, their RRT experiences and satisfaction with these teams, and the impact of these teams on returning to the organization for future care. Post-RRT call surveys should be conducted to evaluate staff nurses'satisfaction with RRT call experiences. Organizations should also capitalize on the learning opportunities that RRTs offer. RRT policies should include debriefing sessions and staff feedback as part of the RRT call. Unit and RRT staffing should facilitate the availability of RRT staff to conduct these debriefings and to provide feedback.
The potential psychological support that RRTs offer to RRTUs should be further explored. The need for support may be indicative of larger, underlying problems that RRTUs face, such as high patient-to-staff ratios and high patient acuities. The availability of a dedicated RRT nurse who can round on units and collaborate with staff nurses in the care of high-risk, high-acuity patients may help to offset RRTUs work stress and enhance their feelings of support. Therefore, the recruitment of a dedicated RRT nurse who respond to RRT calls and round on units in between calls should be considered.
Future research should examine and compare perceived benefits of RRTs with actual, observed benefits. This study was limited to community hospitals and a comparison of perceived benefits between hospitals was not conducted. Future studies should explore the relationship between organizational characteristics and the perceived benefits of nurse leaders, RRTMs, and RRTUs. The structure of the RRTs of hospitals included in this study was somewhat similar: (a) a critical care nurse and respiratory therapists as primary team members with other organizational members responding as necessary; and, (b) a critical care nurse who may or may not have patients assigned to their care whilst also serving as RRT nurse responder. In future studies, the relationship between RRT characteristics and perceived benefits should be explored.
Conclusion
Variation and similarities were found between nurse leaders, RRTMs, and RRTUs' perceived benefits of RRTs. Differences may be indicative of organizations' information sharing processes, differences in the priorities of nurse leaders, RRTMs, and RRTUs, and the challenges nurses face in their daily work environment. Future research should examine and compare actual versus perceived benefits and the relationship between perceived benefits and organizational and RRT characteristics.
Acknowledgments
Grant Support: Partial funding for the project was provided by the National Institute of Nursing Research Grant Number 5 T32 NR 008856.
Appendix A. Semi-Structured Interview Guide*
Questions related to RRT benefits for the organization, patients, and staff members
Broad, opening questions
Let's start.
Think back to when you first learned about RRTs. What were your first thoughts or impressions about the RRT initiative in your hospital?
Why did your organization make the decision to adopt RRTs?
Main questions
Project effectiveness
-
What, if any, do you think are the benefits of RRTs to patients?
To staff?
To the organization as a whole?
How do you think these benefits have affected the use of RRTs since the implementation of RRTs? Please explain.
Concluding questions
Is there anything else that you believe has been helpful in the current and ongoing use of RRTs in your hospital? Please explain.
Thank you very much for participating. The data collected from this interview will be used to shed some light on how RRT sustainability can be fostered in future in hospitals that have adopted these teams.
- Are you willing to be contacted should further clarification be needed on some of what was discussed today?
- Consent given to be contacted again: Yes/No
- Contact information (if not already on file)
Footnotes
Note. This is an abbreviated version of the original interview guide used in the main research study. The questions reported here include only those relevant to the examination of RRT benefits and introductory and concluding questions that helped to set the stage for the main questions and for closing out the interview.
References
- Arashin KA. Using the synergy model to guide the practice of rapid response teams. Dimensions of Critical Care Nursing. 2010;29(3):120–124. doi: 10.1097/DCC.0b013e3181d24b76. [DOI] [PubMed] [Google Scholar]
- Astroth KS, Woith WM, Stapleton SJ, Joseph-Degitz RJ, Jenkins SH. Qualitative exploration of nurses' decisions to activate rapid response teams. Journal of Clinical Nursing. 2013;22(19-20):2876–2882. doi: 10.1111/jocn.12067. [DOI] [PubMed] [Google Scholar]
- Azzopardi P, Kinney S, Moulden A, Tibballs J. Attitudes and barriers to a Medical Emergency Team system at a tertiary paediatric hospital. Resuscitation. 2011;8(2):167–174. doi: 10.1016/j.resuscitation.2010.10.013. [DOI] [PubMed] [Google Scholar]
- Benin AL, Borgstrom CP, Jenq GY, Roumanis SA, Horwitz LI. Defining impact of a rapid response team: qualitative study with nurses, physicians and hospital administrators. Postgraduate Medical Journal. 2012;88(1044):575–582. doi: 10.1136/postgradmedj-2012-000390rep. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berwick DM, Calkins DR, McCannon CJ, Hackbarth AD. The 100,000 lives campaign: setting a goal and a deadline for improving health care quality. The Journal of the American Medical Association. 2006 Jan 18;295(3):324–327. doi: 10.1001/jama.295.3.324. [DOI] [PubMed] [Google Scholar]
- Commins WW, Elias MJ. Institutionalization of mental health programs in organizational contexts: the case of elementary schools. Journal of Community Psychology. 1991;19:207–220. [Google Scholar]
- Chan PS, Jain R, Nallmothu BK, Berg RA, Sasson C. Rapid response teams. A systematic review and meta-analysis. Archives of Internal Medicine. 2010;170(1):18–26. doi: 10.1001/archinternmed.2009.424. Downloaded from www.archinternmed.com at the University of North Carolina- Chapel Hill on February 22, 2010. [DOI] [PubMed] [Google Scholar]
- Cretikos M, Chen J, Hillman K, Bellomo R, Finfer S, Flabouris A. The objective medical emergency team activation criteria: a case-control study. Resuscitation. 2007;73:62–72. doi: 10.1016/j.resuscitation.2006.08.020. [DOI] [PubMed] [Google Scholar]
- Davies O, DeVita MA, Ayinla R, Perez X. Barriers to activation of rapid response system. Resuscitation. 2014;85(11):1557–1561. doi: 10.1016/j.resuscitation.2014.07.013. [DOI] [PubMed] [Google Scholar]
- Garretson S, Rauzi MB, Meister J, Schuster J. Rapid response teams: a proactive strategy for improving patient care. Nursing Standard. 2006;21(9):35–40. doi: 10.7748/ns2006.11.21.9.35.c6408. [DOI] [PubMed] [Google Scholar]
- Goodman RM, Steckler A. A model for the institutionalization of health promotion programs. Family & Community Health. 1989;11(4):63–78. [Google Scholar]
- Grbich D. Qualitative Data Analysis An Introduction. Los Angeles: Sage; 2007. [Google Scholar]
- Krueger RA, Casey MA. Focus groups A practical guide for applied research. 4th. Washington: Sage; 2009. [Google Scholar]
- Metcalf R, Scott S, Ridgway M, Gibson D. Rapid Response Team Approach to Staff Satisfaction. Orthopaedic Nursing. 2008;27(5):266–271. doi: 10.1097/01.NOR.0000337274.32799.89. [DOI] [PubMed] [Google Scholar]
- Miles MB, Huberman AM. Qualitative data analysis. 2nd. Thousand Oaks: Sage; 1994. [Google Scholar]
- Polit DF, Beck CT. Nursing research: principles and methods. 7th. Philadelphia: Lippincott Williams & Wilkins; 2004. [Google Scholar]
- Polit DF, Beck CT. Nursing research: generating and assessing evidence for nursing practice. 9th. Philadelphia: Lippincott Williams & Wilkins; 2012. [Google Scholar]
- Pluye P, Potvin L, Denis J, Pelletier J, Mannoni C. Program sustainability begins with the first events. Evaluation and program planning. 2005;28:123–127. doi: 10.1016/j.evalprogplan.2004.10.003. [DOI] [Google Scholar]
- Salamonson Y, Kariyawasam A, vanHeere B, O'Connor C. The evolutionary process of medical emergency team (MET) implementation: Reduction in unanticipated ICU transfers. Resuscitation. 2001;49(2):135–141. doi: 10.1016/s0300-9572(00)00353-1. [DOI] [PubMed] [Google Scholar]
- Sarani B, Sonnad S, Bergey MR, Phillips J, Fitzpatrick MK, Chalian AA, Myers JS. Resident and RN perceptions of the impact of a medical emergency team on education and patient safety in an academic medical center. 2009 doi: 10.1097/ccm.0b013e3181b09027. [DOI] [PubMed] [Google Scholar]
- Scheirer MA. Is sustainability possible? A review and commentary of empirical studies of program sustainability. American Journal of Evaluation. 2005;26:320–347. doi: 10.1177/1098214005278752. [DOI] [Google Scholar]
- Shapiro SE, Donaldson NE, Scott MB. Rapid Response Teams seen through the eye of the nurse. American Journal of Nursing. 2010;110(6):28–34. doi: 10.1097/01.NAJ.0000377686.64479.84. [DOI] [PubMed] [Google Scholar]
- Stolldorf DP, Jones CB. The deployment of rapid response teams in U.S. Hospitals. Joint Commission Journal on Quality and Patient Safety. 2015 doi: 10.1016/s1553-7250(15)41024-4. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stolldorf DP, Mion L, Jones CB. The sustainability of Rapid Response Teams: Are we there yet? BJM Open. 2015 Revise and resubmit. [Google Scholar]
- Stolldorf DP, Havens DS, Jones CB. Sustaining innovations in complex healthcare environments. A look at Rapid Response Teams. Journal of Patient Safety. 2015 doi: 10.1097/PTS.0000000000000239. Under Review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DJ, Newman A, Jones CB, Woodard EK. Nurses' perceptions of how rapid response teams affect the nurse, the team, and the system. Journal of Nursing Care Quality. 2011;26(1) doi: 10.1097/NCQ.06013e318209f135. Advanced online publication. [DOI] [PubMed] [Google Scholar]
- Winters BD, Pham JC, Hunt EA, Guallar E, Berenholtz S, Pronovost PJ. Rapid response systems: A systematic review. Critical care medicine. 2007;35(5):1238–1243. doi: 10.1097/01.CCM.0000262388.85669.68. [DOI] [PubMed] [Google Scholar]
- Winters BD. Rapid response systems: going beyond cardiac arrest and mortality. Critical Care Medicine. 2013;41(3):911–912. doi: 10.1097/CCM.0b013e3182770fec. [DOI] [PubMed] [Google Scholar]