Abstract
Tetralogy of Fallot (ToF) can be challenging for clinicians to both diagnose and treat, given the multiple heart defects that are by definition associated with the illness. This study investigates the value of real-time three- dimensional echocardiography (RT-3DE) in evaluating the pre-and postoperative right ventricular systolic function of patients with tetralogy of Fallot. A total of 41 ToF patients were divided into two groups: the child group (CG) and the adult group (AG) according to age. The right ventricular end-diastolic volume (RVEDV), right ventricular end-systolic volume (RVESV), and the right ventricular ejection fraction (RVEF) of ToF patients were measured before surgery, 7 days, and 3 months after the surgery. The correlation between the preoperative Nakata index and RVEF was then analyzed. Compared with the RVEDV and RVESV prior to surgery, those of the postoperative 7-day and 3-month were not statistically significant (p > 0.05). However, RVEF decreased, and the difference was statistically significant (p < 0.05). The differences in RVEDV, RVESV, and RVEF between postoperative 3-month and 7-day were not significant (p > 0.05). Compared with the pre-and postoperative RVEDV and RVESV of CG, those of AG increased. However, RVEF decreased, and the differences were statistically significant (p < 0.05). Our study indicated that the correlation between preoperative Nakata index and RVEF was good. Ultimately, we did confirm that RT-3DE can quantitatively evaluate the right ventricular volume and systolic function of ToF patients, thereby providing clinical significance in determining postoperative efficacy and prognosis evaluation.
Keywords: Echocardiography, Right, Tetralogy of Fallot, Three-dimensional, Ventricular function
INTRODUCTION
Tetralogy of Fallot (ToF) is the most common cyanotic congenital heart disease.1 This disease can occur both in males and females, and the occurrence rate in males is slightly higher than that in females. ToF is characterized by four main anatomic features as follows: right ventricular outflow tract obstruction (RVOTO), ventricular septal defect (VSD), overriding aortic root, and right ventricular hypertrophy. The manifestation of ToF in patients varies depending on the severity of RVOTO, which range from mild to severe (i.e., pulmonary atresia). The level of obstruction may affect the infundibulum, pulmonary valve, trunk, and branches.
The prognosis for patients diagnosed with ToF is very poor, and surgery is the primary clinical treatment method. If left untreated, ToF can be fatal. Given the continuous improvements in levels of preoperative diagnosis, surgical technique, and postoperative care, the success rate of total correction of ToF has significantly improved. Successfully completing a total correction may significantly improve the middle-phase quality of life of ToF patients.2 Despite the advantages of total correction of ToF, the postoperative right ventricular dysfunction is still the leading cause of death in patients.2 The right ventricular functions of most patients, even without any clinical symptoms, have declined to various degrees.4 Thus, early and accurate assessment of right ventricular function for ToF patients is important.
Right ventricular ejection fraction (RVEF) is a conventional parameter to evaluate right ventricular systolic function (RVSF), and is based on right ventricular (RV) volumetric variables. With the more complex geometrical shape of the right ventricular cavity, exhibiting a crescent shape, a large funnel portion and prominent trabecular muscles, and also with inflow and outflow tracts not on the same plane, its complex geometric appearance limits the evaluation value of traditional 2D and M-mode echocardiography towards the right ventricular function.5 ToF patients normally have a thickened right ventricular wall and enlarged right heart, and these pathological changes lead to a much more complex geometric appearance of the right ventricle. Therefore, determining an accurate and quantitative assessment of right ventricular volume and systolic function in ToF patients has become more challenging. Cardiac magnetic resonance imaging (CMRI) is recognized as the “gold standard” in evaluating the right ventricular volume and function,6 but its limitations including the time consuming nature of the procedure, high expense, and claustrophobic effect restrict its widespread clinical application. Real-time three-dimensional echocardiography (RT-3DE) does not depend on the geometric assumptions of the heart and can quantitatively and accurately assess the right ventricular volume and systolic function.7 Studies have shown that RT-3DE is highly correlated with CMRI in the evaluation of right ventricular volume and systolic function.8
In the past, the assessment of the right ventricular function via RT-3DE would normally involve the use of a TomTec quantitative analysis software where the product’s accuracy and feasibility have been confirmed by recent studies.5,7,9 The QLAB quantitative analysis software was commonly used in the evaluation of the left ventricular function, and related literature about its use in the assessment of right ventricular function are rare. In this study, the General Imaging 3D Quantification (GI 3DQ) short-axis analysis was performed to manually scan each short axis view of the right ventricle following a principle similar to that of the TomTec analysis software and CMRI measurement method. Moreover, its accuracy has also been confirmed in previous studies.8 As such, the present study aimed to investigate the feasibility and reproducibility of RT-3DE by using the GI 3DQ short-axis analysis in evaluating RV volumes and RVEF before and after the short-term follow-up of total correction to explore the clinical significance of RT-3DE in evaluating the RVSF of ToF.
MATERIALS AND METHODS
Objectives
A total of 41 ToF patients were selected who underwent total correction from November 2012 to August 2013 in the Department of Cardiac Surgery, Henan Provincial People’s Hospital. These patients were composed of 23 males and 18 females whose ages ranged from 0.5 to 43 years old. Based on patient ages, the ToF patients were divided into the child group (age < 18 years old, with 29 patients) and the adult group (age ≥ 18 years old, with 12 patients). All patients had varying degrees of cyanosis, and their peripheral oxygen saturation (SpO2) ranged from 0.63 to 0.85. All patients underwent 2D and 3D echocardiography. The inclusion criteria were as follows: the subjects were suited for the complete preoperative and postoperative data, and the images were clear. The exclusion criteria were as follows: ToF patients accompanied by other heart diseases, such as pulmonary atresia, that would affect the right ventricular volume and the surgical program. This study was conducted in accordance with the declaration of Helsinki, and with the approval from the Ethics Committee of Henan Provincial People’s Hospital. Written informed consent was obtained from all participants.
2DE
An iE33 ultrasound system (Philips Medical Systems, Andover, Massachusetts, USA) with an X5-1 RT 3D probe was used in the 2DE, and the probe frequency was 1 MHz to 3 MHz. The patient lied in the left-side supine position, and a check was performed when the child patient was quiet or in a sleeping state. 2DE was performed to screen the combined cardiac malformation and to measure the left and right pulmonary arteries before surgery. The preoperative Nakata index was then calculated (Nakata index = total cross-sectional using areas near the first branch of the left and right pulmonary arteries/body surface area).
RT-3DE image acquisition and analysis
An iE33 ultrasound system (Philips Medical Systems, Andover, Massachusetts, USA), with an X5-1 RT 3D probe was used in the 3DE, and the probe frequency was 1 MHz to 3 MHZ. The patient lied in the left-side supine position and was connected to the electrocardiogram. To avoid affecting image quality arising from patient movement, the images should be collected when the child is in a quiet or sleeping state, and the adult should hold their breath at the end of expiration. The probe was placed at the cardiac apex, and the full volume imaging mode was started when the four-chamber view (FCV) exhibited the complete envelope of right heart chambers. The full volume images of the heart were then collected. The images were stored and burned into discs. The images of the preoperative, 3-day, postoperative 7-day and 3-month were collected.
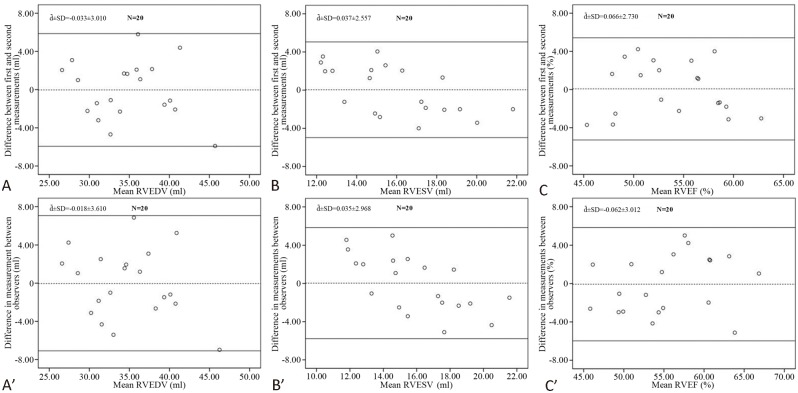
The QLAB 9.0 quantitative analysis software was used to offline-analyze the full volume data of RT-3DE. The GI 3DQ mode was initiated to ensure the end diastole and end systole, then the short axis addition method was performed. After the FCV had been selected, a line was drawn from the middle point of the tricuspid annulus to the RV apex to decide the RV length. Then, RV is cropped into short-axis multiplanar slices, whereafter the outline of each endocardial border of the short axis view was manually traced gradually to obtain right ventricular end-diastolic volume (RVEDV) and right ventricular end-systolic volume (RVESV), where RVEF = (RVEDV-RVESV)/RVEDV, as shown in Figure 1.
Figure 1.
RT-3DE measured the right ventricular volume of ToF. A to D were, respectively: four-chamber view, ventricular short axis view, right ventricular coronal view and right ventricular volume diagram. RT-3DE, real-time three-dimensional echocardiography; ToF, tetralogy of Fallot.
To assess the consistency of the measured values between observers and within the same observer, 20 ToF patients were randomly selected, and the same observer performed repeated analyses at least every other week. Two observers analyzed the results individually to measure the inter-observer difference. During the repeated measurements, the observers did not know each other’s measurements or their own previous measurements.
Statistical analysis
In our study, SPSS 17.0 statistical software was used. All measurement data were obtained using the normality test, and the ones that met the normal distribution were expressed as ± s, whereas the others were expressed as M (QR). RVEDV and RVESV were statistically analysed after their values were corrected using their body surface area (BSA), BSA (m2) = body weight (kg)0.425 × height (cm)0.725 × 71.84 × 10-4. Comparison between different time intervals before and after surgery was accomplished by use of the paired t-test. On the one hand, when homogeneity of variance was assumed, we used the independent sample t test for comparison between AG and CG; on the other hand, the non-parametric test was performed. The correlation analysis of the preoperative Nakata index and RVEF was performed using Pearson’s correlation analysis. The consistency test of the measured right ventricular values between the different observers and within the same observer was conducted using the Bland-Altman plot analysis method, and p < 0.05 was considered as a statistically significant difference.
RESULTS
Objectives
The clinical and preoperative ultrasonographic data of ToF patients are shown in Table 1. There were 41 ToF patients who successfully underwent the total correction procedure. Among them, 24 patients underwent intraoperative pulmonary valve annulus-crossing patch to expand the right ventricular outflow tract (58.54%), and 17 patients underwent simple expansion of the right ventricular outflow tract and pulmonary arterial patch (41.46%). Improvements were observed in the cyanosis of all patients postoperatively as well as in 5 patients of residual ventricular septal defect, including 3 adult patients, with sizes ranging from 1.5 mm to 4 mm. Up to 27 patients exhibited an upflow rate of the pulmonary valve > 2.5 m/s, including 19 with a flow rates from 2.5 m/s to 3 m/s and 8 with flow rates from 3 m/s to 3.5 m/s. A total of 39 patients (95.1%) exhibited different degrees of combined pulmonary valve regurgitation, in which 28 of those patients were mild (the diastolic reverse flow was restricted inside the pulmonary valve annulus), 9 patients were moderate (the pulmonary artery exhibited the diastolic reverse flow but did not exceed the level of pulmonary arterial branch), and 2 patients were severe (the pulmonary arterial branch exhibited the diastolic reverse flow).
Table 1. Preoperative clinical and ultrasound data of ToF patients .
| Variable | Value |
| Age | |
| Median (y) | 2.5 |
| Range (y) | 0.5-43 |
| ≥ 18 y | 12 (29.27%) |
| BSA | |
| Median (m2) | 0.46 |
| Range (m2) | 0.33-1.74 |
| SpO2 | |
| Median | 0.76 |
| Range | 0.63-0.83 |
| Symptoms | |
| Dyspnea | 41 (100%) |
| Squtting | 26 (63.41%) |
| Physical signs | |
| Cyanosis | 41 (100%) |
| Clubbing fingers and toes | 23 (56.10%) |
| Associated cardiac anomalies | |
| Patent foramen ovale | 9 (21.95%) |
| Patent ductus arteriosus | 2 (0.05%) |
| Persistent left superior vena cava | 2 (0.05%) |
| Aortopulmonary collateral arteries | 20 (48.78%) |
ToF, tetralogy of Fallot; SpO2, peripheral oxygen saturation.
Analysis of right ventricular values
The comparison of right ventricular values before and after the surgery in ToF patients is shown in Table 2. The 3D images for all patients were clear enough for quantitative analysis. Compared with the preoperative RVEDV and RVESV, postoperative 7-day and 3-month readings exhibited no statistically significant difference (p > 0.05). However, the RVEF decreased, and the difference was statistically significant (p < 0.05). The comparison of RVEDV, RVESV, and RVEF between the postoperative 3-month and 7-day exhibited no significant difference (p > 0.05).
Table 2. Comparison of RT-3DE-measured values before and after the surgery (x ± s) .
| Observation time | Cases (n) | RVEDV (ml) | RVESV (ml) | RVEF(%) |
| Preoperative 3-d | 41 | 38.78 ± 5.82 | 18.15 ± 2.82 | 53.07 ± 3.91# |
| Postoperative 7-d | 41 | 39.10 ± 5.68 | 19.151 ± 3.02 | 50.94 ± 3.89* |
| Postoperative 3-m | 41 | 38.42 ± 5.91 | 18.94 ± 3.03 | 50.59 ± 3.67* |
The above data were all corrected by body surface area, * compared with the preoperative, p < 0.05; # compared with the postoperative 7-day, p < 0.05. RT-3DE, real-time three-dimensional echocardiography; RVEDV, right ventricular end-diastolic volume; RVEF, right ventricular ejection fraction; RVESV, right ventricular end-systolic volume.
The comparison of CG and AG before and after surgery is shown in Table 3. Compared with the pre- and postoperative RVEDV and RVESV of CG, those of AG increased. However, RVEF decreased, and the difference was statistically significant (p < 0.05).
Table 3. Comparison of RT-3DE-measured values of CG and AG (x ± s) .
| Group | Observation time | RVEDV (ml) | RVESV(ml) | RVEF(%) |
| CG (N = 29) | Preoperative 3-d | 37.27 ± 6.19 | 17.09 ± 2.60 | 53.87 ± 4.07 |
| Postoperative 7-d | 37.49 ± 5.91 | 17.97 ± 2.77 | 51.87 ± 3.92 | |
| Postoperative 3-m | 36.86 ± 6.31 | 17.75 ± 2.81 | 51.58 ± 3.65 | |
| AG (N = 12) | Preoperative 3-d | 42.42 ± 2.30# | 20.70 ± 1.25# | 51.15 ± 2.74* |
| Postoperative 7-d | 42.98 ± 2.22# | 22.01 ± 0.99# | 48.70 ± 2.85* | |
| Postoperative 3-m | 42.20 ± 1.85# | 21.82 ± 0.71# | 48.20 ± 2.48# |
The above data were all corrected by body surface area, compared with CG, * p < 0.05; # p < 0.01. AG, adult group; CG, child group; RT-3DE, real-time three-dimensional echocardiography; RVEDV, right ventricular end-diastolic volume; RVEF, right ventricular ejection fraction; RVESV, right ventricular end-systolic volume.
Correlation analysis
The preoperative Nakata indexes of 41 ToF patients ranged from 135.93 mm2/m2 to 211.55 mm2/m2 with an average of (163.76 20.44) mm2/m2. The correlation between preoperative RVEF and the Nakata index was good (r = 0.678, p = 0.000) as noted in Figure 2.
Figure 2.
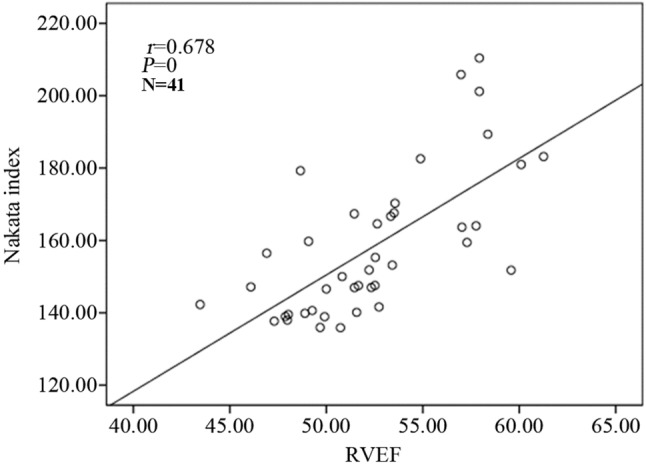
Correlation of RVEF with Nakata index. RVEF, right ventricular ejection fraction.
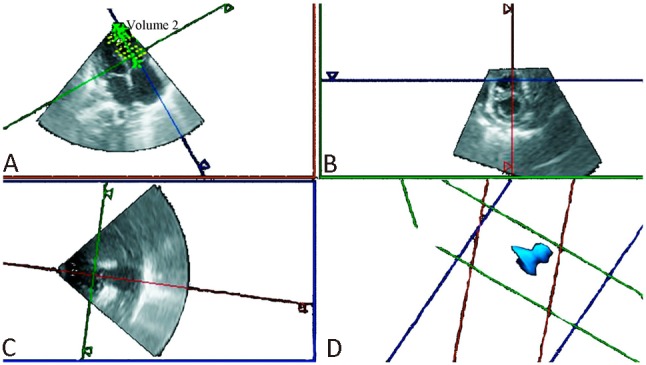
Bland-Altman plot method analysis
The intra-observer variability of RVEDV, RVESV, and RVEF by the same observer showed a mean bias of -0.033 ml, 0.037 ml, and 0.066%, respectively, and a 95% confidence interval for agreement from 5.867 ml to -5.933 ml, 5.049 ml to -4.975 ml, and 5.417% to -5.285%, respectively, which indicated high agreement.
Comparison of RVEDV, RVESV, and RVEF between the two observers showed minimal differences (-0.018 ml, 0.035 ml, and -0.062%, respectively) and high agreement, 95% confidence interval for agreement from 7.058 ml to -7.094 ml, 5.852 ml to -5.782 ml, and 5.842% to -5.966%, respectively (Figure 3).
Figure 3.
Bland-Altman plots showing interobserver (A, B, C) and intraobserver (A′, B′, C′) differences and limits of agreement of RV variables measured by RT-3DE: The solid line represents the mean difference between the measurements analyzed by one observer or by two observers, and the dashed lines represent the 95% confidence interval for agreement, đ ± SD: mean ± standard deviation. RT-3DE, real-time three-dimensional echocardiography; RV, right ventricular; SD, standard deviation.
DISCUSSION
In this study, we investigated the feasibility and reproducibility of RT-3DE by using GI 3DQ short-axis analysis in evaluating RVSF before total correction of ToF and after short-term follow-ups. To our knowledge, this study is the first to evaluate RVSF in ToF patients including AG by using GI 3DQ short-axis analysis. Inter-and intra-observer agreement of assessment of RV end-diastolic volume, end-systolic volume, and EF with RT-3DE showed small differences, fair limits, and high agreement.
RT-3DE of RV
Right ventricular volume and function have important clinical significance in the development, therapeutic judgment, and prognostic evaluation of most heart disease treatment programs;10-12 therefore, these factors are given increased attention by clinicians. Several evaluations of the accuracy and feasibility of RT-3DE technology used to investigate the right ventricular volume and function of most diseases have been conducted.5,7-9 Studies on ToF patients predominantly focused on the middle-and long-term follow-up after total correction, whereas studies on the preoperative and recent follow-up are limited. A previous study13 found that the preoperative RVSF of ToF patients exhibited different degrees of reduction; therefore, the accurate and quantitative assessments of right ventricular volume and systolic function before and after ToF surgery are equally important.
This study showed the feasibility and repeatability of RT-3DE in assessing RVSF. Among the 41 ToF patients in this study, the preoperative RVEF of 11 patients was less than 50%, thereby indicating that the preoperative RVSF already had various degrees of damage, which were related to the increasing pressure of systemic circulation, chronic hypoxia, and increased right ventricular afterload of these ToF patients. These pathological changes can lead to right ventricular myocardial hypertrophy, myocardial rearrangement, and various degrees of interstitial and perivascular fibrosis.14 The RVEF observed in the postoperative 7-day and 3-month testing of ToF patients exhibited a statistically significant difference compared with preoperative RVEF; this indicated that the short-term RVSF of post-total correction was greatly impacted. The reasons for this impact may be the following: (1) the excision of right ventricular hypertrophic myocardium directly caused right ventricular myocardial injury; and (2) the application of extracorporeal circulation in total correction could lead to myocardial ischemia-reperfusion injury.15
In the present study, compared with the RVEDV and RVESV of CG, those of AG increased. However, RVEF decreased before and after the surgery, and the differences were statistically significant. In addition, the proportion of patients with postoperative residual ventricular septal defects was larger, thereby indicating that the course of disease had a significant relationship with right ventricular volume and systolic function and that an early surgery might improve the prognosis of ToF patients, which was consistent with the findings of Bakhtiary.16
Previous studies have found that for post-ToF patients who exhibited no clinical symptoms, RVEF < 47% could be used as an indicator for pulmonary valve replacement surgery17 and that the prolonged QRS duration was significantly associated with RVEF reduction.18 When RVEF was < 45%, the physical component summary and physical functioning scores would decline, that is, the quality of life decreases.19 Thus, RVEF in the post-ToF follow-up is important. In this study, RVEF in the short-term post-ToF follow-up was > 45%, and no arrhythmia or other complications occurred during the follow-up. To a certain extent, this confirms the reliability of the results of previous studies. Moreover, we hope that continuing follow-ups will provide more valuable information that can be used for early clinical intervention.
In this study, 95.1% of the ToF patients exhibited various degrees of postoperative pulmonary valve regurgitation, thereby indicating that pulmonary valve regurgitation is a common postoperative complication and is related to the weakening of the pulmonary valve annulus supporting tissue. This is due to right ventricular infundibulum expansion caused by the annulus-crossing patch and excision of hypertrophic myocardium.20 A previous study21 has shown that pulmonary valve regurgitation could lead to the overload of the right ventricular volume followed by the right ventricular systolic dysfunction, and this effect is the long-term risk factor of right ventricular failure after total correction of ToF. The present study found that the difference in the short-term postoperative right ventricular volume was not statistically significant compared with the preoperative right ventricular volume, In addition, the comparison of RVEDV, RVESV, and RVEF between the postoperative 3-month and 7-day exhibited no significant difference, thereby indicating that pulmonary valve regurgitation had less effect on the short-term postoperative right ventricular volume and systolic function, which was consistent with the findings of Spiewak.22 Other researchers showed that23 pulmonary regurgitation combined with pulmonary stenosis was a long-term right ventricular protective factor after the ToF radical surgery, and the degree of right ventricular dilatation was relatively alleviated than simple pulmonary regurgitation. Thus, it could delay the pulmonary valve replacement. In this study, 27 patients were noted to have faster postoperative pulmonary branch velocity, while the short-term follow-up revealed that the right ventricular volume did not change significantly. Because of the short postoperative follow-up time, this conclusion needs to be confirmed in further studies.
The developmental condition of the pulmonary artery is a main factor in surgical prognosis. The Nakata index could well reflect the developmental condition of the pulmonary artery, thereby exhibiting its important clinical value. This study pointed out that preoperative RVEF showed a positive correlation with the Nakata index, that is, RVSF decreases as the developmental condition of the pulmonary artery worsens. Therefore, preoperative RVSF is closely related to pulmonary development and has a specific reference value in terms of postoperative efficacy determination and prognosis evaluation.
Strengths and limitations
Several strengths and limitations of this study must be addressed. To date, there are few studies that link RVEF with the Nakata index in preoperative ToF patients. Additionally, the use of the Bland-Altman plot method with limits of agreement for evaluating RV measurements provided a robust examination of agreement.
The image acquisition and analysis times of RT-3DE were long. Given the small sample size of this study, CG could not be further refined by the ages of the patients, and the postoperative follow-up time was short. On the other hand, in the study, RVSF was evaluated in both the pre-operative and post-operative states, but was not correlated with any clinical outcomes, for example long-term survival, heart failure, exercise capacity, or quality of life. Long-term follow-up data still need to be collected, and further research is necessary to assess the prognostic value of the parameter. In addition, the results of this study were not compared with the gold standard to validate RT-3DE; thus, evaluating the accuracy of this method in assessing the right ventricular systolic functions of the ToF patients was not possible.
CONCLUSIONS
The process of RT-3DE by using GI 3DQ short-axis analysis could quantitatively evaluate right ventricular volume and systolic function in patients before total correction of ToF and after short-term follow-ups. The Bland-Altman drawing method analysis results showed that the measurements of RVEDV, RVESV and RVEF between observers and within the same observer exhibited good reproducibility. Preoperative RVEF showed a positive correlation with the Nakata index, indicating that preoperative RVSF is closely related to pulmonary development. Although pulmonary valve regurgitation is a common postoperative complication, it had less effect on the short-term postoperative right ventricular volume and systolic function. Accordingly, further studies are required to assess the prognostic value.
Acknowledgments
This study was supported by basic and advanced research program of Science and Technology Department of Henan Province (132300410039); Henan provincial medical research program (201, 303, 121).
REFERENCES
- 1.Rahman F, Salman M, Akhter N, et al. Pattern of congenital heart diseases. Mymensingh Med J. 2012;21:246–250. [PubMed] [Google Scholar]
- 2.Pilla CB, Pereira CA, Fin AV, et al. Health-related quality of life and right ventricular function in the midterm follow-up assessment after tetralogy of Fallot repair. Pediatr Cardiol. 2008;29:409–415. doi: 10.1007/s00246-007-9145-4. [DOI] [PubMed] [Google Scholar]
- 3.Barron DJ. Tetralogy of Fallot:controversies in early management. World J Pediatr Congenit Heart Surg . 2013;4:186–191. doi: 10.1177/2150135112471352. [DOI] [PubMed] [Google Scholar]
- 4.Van Aerschot I, Iserin L. Follow-up of tetralogy of Fallot after repair. Presse Med. 2011;40:740–747. doi: 10.1016/j.lpm.2011.02.030. [DOI] [PubMed] [Google Scholar]
- 5.van der Zwaan HB, Geleijnse ML, Mcghie JS, et al. Right ventricular quantification in clinical practice:two-dimensional vs. three-dimensional echocardiography compared with cardiac magnetic resonance imaging. Eur J Echocardiogr. 2011;12:656–664. doi: 10.1093/ejechocard/jer107. [DOI] [PubMed] [Google Scholar]
- 6.Galea N, Carbone I, Cannata D, et al. Right ventricular cardiovascular magnetic resonance imaging:normal anatomy and spectrum of pathological findings. Insights Imaging. 2013;4:213–223. doi: 10.1007/s13244-013-0222-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Simpson J, Miller O, Bell A, et al. Image orientation for three-dimensional echocardiography of congenital heart disease. Int J Cardiovasc Imaging. 2012;28:743–753. doi: 10.1007/s10554-011-9893-3. [DOI] [PubMed] [Google Scholar]
- 8.Morikawa T, Murata M, Okuda S, et al. Quantitative analysis of right ventricular function in patients with pulmonary hypertension using three-dimensional echocardiography and a two-dimensional summation method compared to magnetic resonance imaging. Am J Cardiol. 2011;107:484–489. doi: 10.1016/j.amjcard.2010.09.047. [DOI] [PubMed] [Google Scholar]
- 9.Peacock AJ, Crawley S, Mclure L, et al. Changes in right ventricular function measured by cardiac magnetic resonance imaging in patients receiving pulmonary arterial hypertension-targeted therapy:the EURO-MR study. Circ Cardiovasc Imaging. 2014;7:107–114. doi: 10.1161/CIRCIMAGING.113.000629. [DOI] [PubMed] [Google Scholar]
- 10.Davlouros PA, Niwa K, Webb G, Gatzoulis MA. The right ventricle in congenital heart disease. Heart. 2006;92 Suppl 1:i27–i138. doi: 10.1136/hrt.2005.077438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sun X, Ellis J, Kanda L, Corso PJ. The role of right ventricular function in mitral valve surgery. Heart Surg Forum. 2013;16:E170–E176. doi: 10.1532/HSF98.20121080. [DOI] [PubMed] [Google Scholar]
- 12.Tong K, Zhang J, Wang J, et al. Quantification of left and right ventricular systolic function in patients with dilated cardiomyopathy using real-time three-dimensional echocardiography. Zhong Nan Da Xue Xue Bao Yi Xue Ban. 2012;37:561–566. doi: 10.3969/j.issn.1672-7347.2012.06.004. [DOI] [PubMed] [Google Scholar]
- 13.Ye JJ, Shu Q, Liu XW, et al. Noninvasive perioperative evaluation of right ventricular function in children with tetralogy of Fallot. Artif Organs. 2014;38:41–47. doi: 10.1111/aor.12189. [DOI] [PubMed] [Google Scholar]
- 14.Starr JP. Tetralogy of Fallot:yesterday and today. World J Surg. 2010;34:658–668. doi: 10.1007/s00268-009-0296-8. [DOI] [PubMed] [Google Scholar]
- 15.Schuuring MJ, Bolmers PP, Mulder BJ, et al. Right ventricular function declines after cardiac surgery in adult patients with congenital heart disease. Int J Cardiovasc Imaging. 2012;28:755–762. doi: 10.1007/s10554-011-9892-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bakhtiary F, Dahnert I, Leontyev S, et al. Outcome and incidence of re-intervention after surgical repair of tetralogy of Fallot. J Card Surg. 2013;28:59–63. doi: 10.1111/jocs.12030. [DOI] [PubMed] [Google Scholar]
- 17.Geva T. Indications for pulmonary valve replacement in repaired tetralogy of fallot:the quest continues. Circulation. 2013;128:1855–1857. doi: 10.1161/CIRCULATIONAHA.113.005878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bassareo PP, Mercuro G. QRS complex enlargement as a predictor of ventricular arrhythmias in patients affected by surgically treated tetralogy of Fallot:a comprehensive literature review and historical overview. ISRN Cardiol. 2013;2013:782508. doi: 10.1155/2013/782508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lu JC, Cotts TB, Agarwal PP, et al. Relation of right ventricular dilation,age of repair,and restrictive right ventricular physiology with patient-reported quality of life in adolescents and adults with repaired tetralogy of fallot. Am J Cardiol. 2010;106:1798–1802. doi: 10.1016/j.amjcard.2010.08.021. [DOI] [PubMed] [Google Scholar]
- 20.Kim H, Sung SC, Kim SH, et al. Early and late outcomes of total repair of tetralogy of Fallot:risk factors for late right ventricular dilatation. Interact Cardiovasc Thorac . 2013;17:956–962. doi: 10.1093/icvts/ivt361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Menon SC, Kaza AK, Puchalski MD. Effect of ventricular size and function on exercise performance and the electrocardiogram in repaired tetralogy of Fallot with pure pulmonary regurgitation. Ann Pediatr Cardiol. 2012;5:151–155. doi: 10.4103/0974-2069.99617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Spiewak M, Malek LA, Petryka J, et al. Stable right ventricular size and function during short-term follow-up in patients with pulmonary regurgitation after tetralogy of Fallot repair. Clin Radiol. 2013;68:1206–1211. doi: 10.1016/j.crad.2013.06.020. [DOI] [PubMed] [Google Scholar]
- 23.Maskatia SA, Spinner JA, Morris SA, et al. Effect of branch pulmonary artery stenosis on right ventricular volume overload in patients with tetralogy of Fallot after initial surgical repair. Am J Cardiol. 2013;111:1355–1360. doi: 10.1016/j.amjcard.2013.01.278. [DOI] [PubMed] [Google Scholar]