Abstract
Background
Diabetes mellitus (DM) is a major public health problem in Taiwan and is associated with poor outcomes in patients with coronary artery disease. However, the role of DM in outcomes for patients with acute coronary syndrome (ACS) has not been clearly defined in Taiwan. This study utilized the Taiwan ACS registry, and characterized the clinical features, risk factors, hospital therapies, hospital outcomes, and events within one year post-discharge to identify the effect of DM on adverse cardiovascular outcomes in ACS patients.
Methods
A total of 3183 patients were enrolled from a Taiwan nationwide registry, from October 2008 to January 2010. We compared these ACS patients with and without DM in terms of baseline demographics, clinical presentation, risk factors, medical treatment, intervention, and outcomes in the following 12 months. The primary endpoint was a composite outcome that included death, re-myocardial infarction and stroke within a 12-month period. The secondary endpoint consisted of the combined results of death, re-myocardial infarction, stroke, re-vascularization, and re-hospitalization over 12 months.
Results
Overall, 2766 (86.8%) ACS patients were analyzed in this study. Of that total, 1000 (36%) of them were diabetes patients. Over the course of one year of follow-up, the DM patients had higher probabilities of all-cause death (10.1% vs. 6.06%, p < 0.05), for both primary outcomes (15.7% vs. 10.93%, p < 0.05) and secondary outcomes (51.6% vs. 42.41%, p < 0.05). Logistic regression analysis showed that patients in the DM group were at a higher risk of all-cause death and the primary outcomes, after adjusting the confounding variables (odds ratio was 1.9 and 1.6 respectively, p < 0.01). For those patients suffering from primary outcomes, the mean survival time was 34.7 ± 10.4 days in the Non-DM group and 33.3 ± 11.8 days in the DM group (p < 0.05). The log rank test showed the two survival curves were significantly distinctive (p < 0.05). Cox regression analysis showed the odds ratio for all-cause death and the primary outcomes were 1.66 and 1.5, respectively (p < 0.05).
Conclusions
Compared to patients without DM, ACS patients with diabetes had significantly worse outcomes in terms of all-cause death and the combined results for death, re-infarction and stroke.
Keywords: Acute coronary syndrome, Diabetes mellitus, Myocardial infarction
INTRODUCTION
Diabetes mellitus (DM) is a major health problem in Taiwan. According to nationwide health insurance data, the prevalence rate was about 6-7%, with a more than 70% increase in the total diabetic population in Taiwan from 2000-2009.1-3 Diabetes is usually associated with cardiovascular risk factors such as smoking, male sex, hypercholesterolemia and hypertension and is considered to be a coronary artery disease (CAD) equivalent.4-7 In Taiwan, DM is strongly associated with cardiovascular diseases and CAD is the most common cause of death in DM patients.8
Several earlier trials found a close relationship between acute coronary syndrome (ACS) and DM, including the Drug Eluting Stents Evaluation: a randomized trial (DESERT) and the Drug Eluting Stenting for Patients with Diabetes Mellitus Trial (DIABETES).9,10 These studies show that in patients with ACS, DM is associated with more stent thrombosis, target lesion revascularization, re-infarction, and major adverse cardiac events. However, less is known about how DM influences outcome in ACS patients in Taiwan.
The Taiwan ACS registry is a nationwide study to assess real-world clinical practices and outcomes for patients with ACS in Taiwan. The study period started from the time of admission and continued for one year post-discharge. To our knowledge, information about the outcomes for patients with ACS as it relates to DM status and treatment practices in Taiwan has been limited. Our main purpose was to document the risk factors, complications, disease severity, therapeutic interventions, hospital outcomes, and events over a period of one year to identify the risks DM poses for ACS patients.
MATERIALS AND METHODS
Study design
The study used a prospective, national, multicenter, and observational design. We enrolled patients ≥ 20 years of age between October 2008 and January 2010 who presented with symptoms of ACS, and were admitted within 24 hours at any of the 39 hospitals in Taiwan participating in the study. ACS was defined by a wide range of symptoms including ST elevation myocardial infarction (STEMI), non-ST elevation myocardial infarction (NSTEMI) and unstable angina (UA) based on electrocardiogram ST changes and cardiac enzyme elevation. Each participating hospital recruited between 50-200 consecutive eligible patients. To ensure that the ACS population was well presented, the Scientific Committee of the Taiwan Society of Cardiology selected the participating hospitals. We compared DM and non-DM patients in term of baseline demographics, clinical presentation, risk factors, medical treatment, interventions, in-hospital outcomes, and outcomes over the following twelve months. DM status was determined by previous medical records, self-reporting, or newly diagnosed DM during admission. For this cohort study of ACS patients with or without DM, we used data from the Taiwan ACS registry to examine adverse outcomes, including death, re-myocardial infarction (re-MI), stroke, repeat revascularization, and re-hospitalization. The primary endpoints included death, re-MI and stroke happening in the hospital or in the one year following discharge. The secondary endpoints included death, re-MI, stroke, repeat revascularization and re-hospitalization occurring either in the hospital or in the one year following discharge.
The study was carried out in accordance with the local regulatory guidelines and international guidelines for good epidemiological practices.11 Ethics committee approval was obtained at each trial site, and written informed consent was obtained from each patient.
Statistical analysis
In this study, continuous variables are shown as means ± standard deviation (SD) or medians with inter-quartile ranges (IQRs); categorical variables are shown as absolute numbers and percentages. The independent t-test or Mann-Whitney U test was used for comparison of continuous variables. For categorical variables, we applied Pearson’s chi-square test or Fisher’s exact test. A p value of less than 0.05 was considered significance for all factors. The one-year follow-up event analysis is presented with Kaplan-Meier survival curves and log rank test. Cox regression models were used to calculate the hazard ratio (HR) for all-cause death and primary outcome, adjusting for age, sex, Killip class, hypertension, dyslipidemia, serum creatinine, smoking, family history of CAD, prior CAD, prior stroke, previous heart failure, angiotensin converting enzyme inhibitor (ACEI), angiotensin II receptor blocker (ARB), statin, aspirin and clopidogrel. All analyses were conducted using SPSS software, version 20.0 (SPSS Inc., Chicago, IL, USA).
RESULTS
Clinical characteristics
We enrolled a total of 3183 patients from 20 medical centers and 19 regional hospitals in Taiwan between October 2008 and January 2010. We excluded patients without any record of DM status, patients lost to follow-up after discharge, patients whose data were incorrect or not sufficiently clear, and patients who were misdiagnosed on admission if their discharge diagnosis excluded ACS. Overall, 2766 (86.8%) patients were analyzed in this study. A majority of patients, 2173 (78.6%), were male, with an average age of 62.9 ± 13.4 years. The number of patients diagnosed with DM was 1000 (36.2%). Of these DM patients, 69.8% were male, a significantly lower proportion than in the non-DM group (83.52%, p < 0.001). The average age of the DM patients was 65.1 ± 11.9 years, significantly higher than the age of non-DM patients, (61.7 ± 14.0 years, p < 0.001). Compared with the non-DM group, the DM patients had significantly higher Killip class grade (III/IV), and higher rates of hypertension, dyslipidemia, prior CAD, prior percutaneous coronary intervention (PCI), prior coronary artery bypass graft (CABG), prior stroke, prior peripheral artery disease (PAD), previous heart failure, dialysis, NSTEMI, and UA (DM group: 26.91%, 77.21%, 51%, 34.3%, 51.32%, 10.26%, 12.7%, 4%, 8.3%, 7.7%, 41.1% and 15.2%; non-DM group: 16.59%, 57.76%, 33.75%, 19.99%, 43.23%, 4.91%, 7.42%, 1.42%, 3.57%, 1.76% , 30.86% and 11.61%, Table 1). The DM patients also had lower rates of STEMI and smoking compared with the non-DM group (DM group: 49.49% and 43.7%, respectively; non-DM group: 63.98% and 57.3%, respectively). Systolic blood pressure was 140.52 ± 33.41 mmHg for DM patients and 138.42 ± 32.4 mmHg for non-DM patients (p = 0.11). Diastolic blood pressure was 79.8 ± 21.23 mmHg for DM patients and 82.3 ± 20.57 mmHg for non-DM patients (p = 0.003). The average heart rate, serum creatinine and TG level were significantly higher in the DM group, while height, high-density lipoprotein and low-density lipoprotein level were significantly lower in the DM group. The average length of hospital stay for DM patients was significantly longer (DM: 10.0 ± 14.0 days), than for the non-DM patients (7.2 ± 7.2 days, p < 0.001).
Table 1. Baseline characteristics of patients with and without DM .
| Variables | All (N = 2766) | DM (N = 1000) | Non-DM (N = 1766) | p-value |
| Age (year) (mean ± SD) | 62.9 ± 13.3 | 65.1 ± 11.9 | 61.7 ± 14 | < 0.001 |
| Sex, male (%) | 2173 (78.6) | 698 (69.8) | 1475 (83.5) | < 0.001 |
| Killip Class ≥ III | 447 (20.2) | 208 (26.9) | 239 (16.6) | < 0.001 |
| Hypertension (%) | 1785 (64.8) | 769 (77.2) | 1016 (57.8) | < 0.001 |
| Dyslipidemia (%) | 1101 (40) | 508 (51) | 593 (33.8) | < 0.001 |
| Smoking (%) | 1598 (58.7) | 488 (49.5) | 1110 (64) | < 0.001 |
| Prior CAD (%) | 696 (25.2) | 343 (34.3) | 353 (20) | < 0.001 |
| Prior PCI (%) | 483 (46.8) | 234 (51.3) | 249 (43.2) | 0.01 |
| Prior CABG (%) | 75 (7.3) | 47 (10.3) | 28 (4.9) | 0.001 |
| Prior MI (%) | 278 (27.1) | 131 (28.7) | 147 (25.8) | 0.30 |
| Prior stroke (%) | 258 (9.3) | 127 (12.7) | 131 (7.4) | < 0.001 |
| Prior PAD (%) | 65 (2.3) | 40 (4) | 25 (1.4) | < 0.001 |
| Previous heart failure (%) | 146 (5.3) | 83 (8.3) | 63 (3.6) | < 0.001 |
| Family history (%) | 485 (23) | 163 (22.2) | 322 (23.4) | 0.55 |
| Blood pressure (mmHg) (mean ± SD) | ||||
| SBP | 139.2 ± 32.8 | 140.5 ± 33.4 | 138.4 ± 32.4 | 0.11 |
| DBP | 81.4 ± 20.8 | 79.8 ± 21.2 | 82.3 ± 20.6 | 0.003 |
| Heart rate (bpm) (mean ± SD) | 81.9 ± 22 | 86.6 ± 23.6 | 79.3 ± 20.5 | < 0.001 |
| Rapid troponin (mean ± SD) | 6 ± 28.5 | 5.3 ± 20.3 | 6.5 ± 32.3 | 0.52 |
| Height (cm) (mean ± SD) | 164 ± 7.8 | 162.9 ± 8 | 164.6 ± 7.7 | < 0.001 |
| Weight (kg) (mean ± SD) | 68.4 ± 12.7 | 67.8 ± 12.9 | 68.7 ± 12.6 | 0.07 |
| BMI (kg/m2), median (IQR) | 25.2 (4.8) | 25.1 (4.9) | 25.2 (4.7) | 0.78 |
| Waist circumference (cm), median (IQR) | 90 (11) | 91 (12.8) | 89 (11) | 0.004 |
| Serum creatinine (mg/dl) (mean ± SD) | 1.6 ± 1.8 | 2 ± 2.2 | 1.4 ± 1.6 | < 0.001 |
| Dialysis (%) | 108 (3.9) | 77 (7.7) | 31 (1.8) | < 0.001 |
| White cell count (mean ± SD) | 10.5 ± 4.5 | 10.6 ± 4.9 | 10.4 ± 4.3 | 0.28 |
| Cholesterol (mg/dl) (mean ± SD) | 178.5 ± 46.6 | 173.8 ± 49.4 | 181.2 ± 44.7 | < 0.001 |
| HDL (mg/dl) (mean ± SD) | 39.6 ± 24 | 37.7 ± 19.7 | 40.6 ± 26 | 0.006 |
| LDL (mg/dl) (mean ± SD) | 112.3 ± 37.4 | 105.6 ± 37.7 | 115.9 ± 36.7 | < 0.001 |
| TG (mg/dl) (mean ± SD) | 142.8 ± 105.6 | 164.5 ± 126.6 | 130.7 ± 89.8 | < 0.001 |
| STEMI (%) | 1449 (52.4) | 437 (43.7) | 1012 (57.3) | < 0.001 |
| NSTEMI (%) | 956 (34.6) | 411 (41.1) | 545 (30.9) | < 0.001 |
| Unstable angina (%) | 357 (12.9) | 152 (15.2) | 205 (11.6) | 0.007 |
| Length of hospital stay (day) (mean ± SD) | 8.2 ± 10.3 | 10 ± 14 | 7.2 ± 7.2 | < 0.001 |
a. Chi-square test or Fisher’s exact test. b. Independent t test or Mann-Whitney U test.
Hypertension is defined as systolic pressure ≥ 140 mmHg or diastolic pressure ≥ 90 mmHg; dyslipidemia is defined as elevated total or LDL cholesterol levels, or low levels of HDL cholesterol; smoking is defined as current and former smokers; coronary artery disease is defined as known coronary stenosis > 50%.
BMI, body mass index; CABG, coronary artery bypass graft; CAD, coronary artery disease; DBP, diastolic blood pressure; HDL, high density lipoprotein cholesterol; IQR, interquartile range; LDL, low density lipoprotein cholesterol; MI, myocardial infarction; NSTEMI, non-ST-segment elevation myocardial infarction; PAD, peripheral artery disease; PCI, percutaneous coronary intervention; SBP, systolic blood pressure; SD, standard deviation; STEMI, ST-segment elevation myocardial infarction; TG: triglyceride.
With regard to treatment received in the hospital (Table 2), the CABG rate was significantly higher in the DM group (4.4% versus 2.77%, p < 0.05), but the PCI rate was significantly higher in the non-DM group (82.23% versus 87.93%, p < 0.05). DM patients took less aspirin, clopidogrel, and ACEI, but more ARB (DM: 89%, 92.6%, 43.5%, 16.5%; Non-DM: 93.15%, 95.36%, 52.38%, 10.08%, respectively, where p < 0.05). There was no difference between the two groups for the use of renin-angiotensin blocker which include ACEI and ARB. The primary PCI rate for STEMI was higher in the non-DM group (82.2% versus 87.9%, p < 0.001).
Table 2. Hospital therapies .
| Variables | All (N = 2766) | DM (N = 1000) | Non-DM (N = 1766) | p-value |
| Aspirin (%) | 2535 (91.6) | 890 (89) | 1645 (93.1) | < 0.001 |
| Clopidogrel (%) | 2610 (94.4) | 926 (92.6) | 1684 (95.4) | 0.003 |
| ACEI (%) | 1360 (49.2) | 435 (43.5) | 925 (52.4) | < 0.001 |
| ARB (%) | 343 (12.4) | 165 (16.5) | 178 (10.1) | < 0.001 |
| Renin-angiotensin blocker (%) | 1630 (58.93) | 567 (56.7) | 1063 (60.2) | 0.07 |
| B-blocker (%) | 1264 (45.7) | 465 (46.5) | 799 (45.2) | 0.52 |
| Statin (%) | 1370 (49.5) | 497 (49.7) | 873 (49.4) | 0.89 |
| Thrombolysis (%) | 47 (2.5) | 15 (2.4) | 32 (2.5) | 0.88 |
| Primary PCI (%) | 1316 (90.8) | 390 (89.2) | 926 (91.5) | < 0.001 |
| PCI (%) | 2371 (85.9) | 819 (82.2) | 1552 (87.9) | < 0.001 |
| CABG (%) | 93 (3.4) | 44 (4.4) | 49 (2.8) | 0.02 |
a. Chi-square test or Fisher's exact test. b. Independent t test or Mann-Whitney U test.
ACEI, angiotensin converting enzyme inhibitor; ARB, angiotensin II receptor blocker; CABG, coronary artery bypass graft; PCI, percutaneous coronary intervention; renin-angiotensin blocker includes ACEI and ARB.
Survival analysis
Our primary endpoint was a composite outcome of death, re-myocardial infarction and stroke over 12 months. Of the 2766 patients in our study, 2715 remained “valid” for survival analysis after excluding 48 cases that were missed and 3 where outcomes were unclear. A total of 299 (11.0%) patients suffered from the primary outcomes (death, re-MI, and stroke); 2416 patients were free from primary outcomes after one year. The total number of patients subjected to survival analysis was 2715.
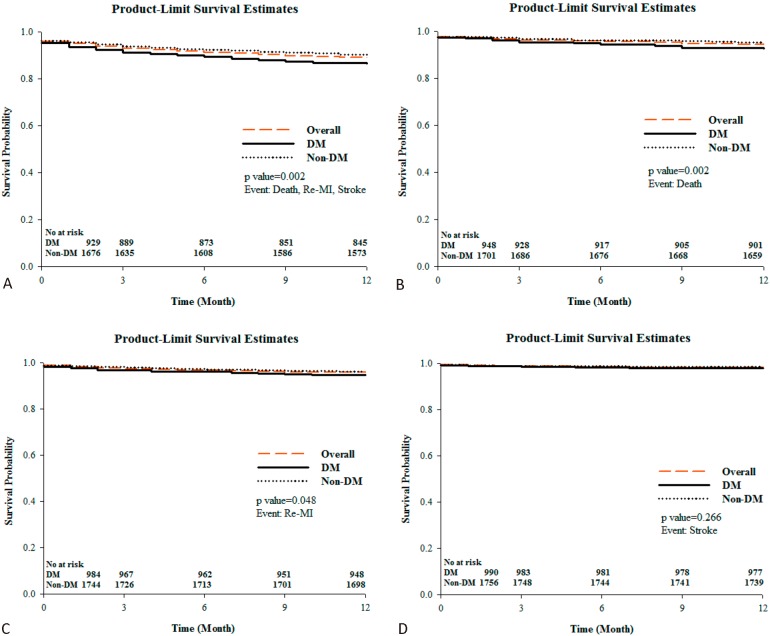
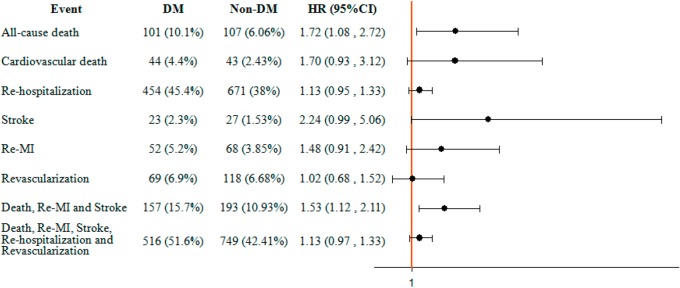
Figure 1A-D shows the Kaplan-Meier curves of DM and non-DM patients diagnosed with any of the primary outcomes, death, re-MI, and stroke within 12 months. For DM patients, the survival probability of primary outcomes, death and re-MI were significantly lower than in non-DM patients (see analysis of survival time in Table 3). The average duration from onset of ACS to the first event was 34.7 ± 10.4 days in the Non-DM group and 33.3 ± 11.8 days for the DM group (p < 0.05). The log rank test showed that the survival curves for DM and non-DM patients were significantly distinctive (p < 0.05). Figure 2 shows the results of Cox regression model analysis. Results showed the odds ratio for all-cause death and primary outcome was higher in DM patients compared with Non-DM patients (1.66 vs. 1.5, where p < 0.05).
Figure 1.
(A) Kaplan-Meier curves of DM and non-DM patients with primary cardiovascular events over 12 months. (B) Kaplan-Meier curves of DM and non-DM patients for death events over 12 months. (C) Kaplan-Meier curves of DM and non-DM patients for Re-MI events over 12 months. (D) Kaplan-Meier curves of DM and non-DM patients on stroke events over 12 months. DM, diabetes mellitus; MI, myocardial infarction. The resulting Kaplan-Meier curves for events free survival. (A) primary cardiovascular events (Death, MI and stroke). (B) Death. (C) Re-myocardial infarction. (D) Stroke.
Table 3. Mean survival time .
| Group | n (events) | Mean ± SD | 95% CI | p-valuea | |
| Lower | Upper | ||||
| DM | 975 (132) | 33.3 ± 12.0 | 32.5 | 34.0 | 0.002 |
| Non-DM | 1740 (167) | 34.7 ± 10.3 | 34.2 | 35.1 | |
| Overall | 2715 (299) | 34.2 ± 11.0 | 33.8 | 34.6 |
a. Log Rank test.
CI, confidence interval; DM, diabetes mellitus; SD, standard deviation.
The average time from onset of ACS to the first event was 34.7 ± 10.3 days in the non-DM group and 33.3 ± 12.0 days for DM group (p = 0.002).
Figure 2.
Effect of DM on cardiovascular events over 12 months. * Adjusted for age, sex, Killip class, hypertension, dyslipidemia, serum creatinine, smoking, family history of CAD, prior CAD, prior stroke, previous HF, ACEI, ARB, statin, aspirin, clopidogrel. CAD, coronary artery disease; CI, confidence interval; DM, diabetes mellitus; HF, heart failure; HR, hazard ratio; MI, myocardial infarction. The results show that all cause death and composites of primary outcomes (death, MI and stroke) increase in DM patients with ACS in 12 months of follow up.
Logistic regression
Univariable analysis showed the crude odds ratio for all-cause death, cardiovascular death, and the primary and secondary outcomes were higher in the DM group (odds ratio: 1.74, 1.84, 1.52, 1.36 and 1.45). After adjusting for confounding variables, multivariable analysis showed the DM group had higher probability of all-cause death and the primary outcome, with an odds ratio of 1.88 vs. 1.58, p < 0.01. Table 4 shows the results of logistic regression.
Table 4. Multivariable-adjusted odd ratios .
| Outcomes | Crude OR (95% CI) | p-value | Adjusted OR (95% CI) | p-value |
| All-cause death | 1.7 (1.3-2.3) | < 0.001 | 1.9 (1.2-3.0) | 0.006 |
| Cardiovascular death | 1.8 (1.2-2.8) | 0.005 | 1.9 (0.9-3.5) | 0.06 |
| Stroke | 1.5 (0.9-2.7) | 0.15 | 2.3 (0.9-5.2) | 0.053 |
| Re-MI | 1.4 (0.9-2.0) | 0.10 | 1.3 (0.8-2.2) | 0.25 |
| Death, Re-MI and stroke | 1.5 (1.2-1.9) | < 0.001 | 1.6 (1.2-2.2) | 0.005 |
| Re-hospitalization | 1.4 (1.2-1.6) | < 0.001 | 1.1 (0.9-1.4) | 0.24 |
| Revascularization | 1.0 (0.8-1.4) | 0.83 | 1.0 (0.7-1.5) | 0.95 |
| Death, Re-MI, Stroke, Re-hospitalization and revascularization | 1.4 (1.2-1.7) | < 0.001 | 1.2 (0.9-1.5) | 0.14 |
Adjusted for age, sex, Killip class, hypertension, dyslipidemia, serum creatinine, smoking, family history of CAD, prior CAD, prior stroke, previous HF, ACEI, ARB, Statin, Aspirin, clopidogrel.
CAD, coronary artery disease; CI, confidence interval; HF, heart failure; MI, myocardial infarction; OR, odds ratio.
Univariable analysis showed the crude odds ratio for all-cause death, cardiovascular death, primary and secondary outcomes were all higher in the DM group (odds ratio: 1.7, 1.8, 1.5, and 1.4). Multivariable analysis also indicated higher all-cause death and the primary outcome in the DM group (Odds ratio: 1.9 vs. 1.6, p < 0.01).
DISCUSSION
After reviewing several large worldwide ACS registries, the estimated prevalence of diabetes among ACS patients was about 20-30%.4,12-20 In our registry of Taiwanese patients with ACS, the prevalence of diabetes was about 36%, a little higher than that percentage found in other large registries.
Comparing the prevalence of diabetes in the STEMI and NSTEMI groups in our study, 43% of patients in NSTEMI group had diabetes, significantly higher than the 30.2% patients with diabetes in the STEMI group (p < 0.05). In worldwide ACS registries such as the global registry of acute coronary events (GRACE), patients with diabetes comprised 28% of the NSTEMI group and 21% of the STEMI group.4,12-14 Can rapid risk stratification of unstable angina patients suppress adverse outcomes with early implementation of the ACC/AHA guidelines registry (CRUSADE),15 the patients with diabetes were 33% in NSTEMI group and 22% in STEMI group. In the Acute Coronary Treatment and Intervention Outcomes Network registry (ACTION),16-20 36% of patients diagnosed with NSTEMI had diabetes, while 24% of the STEMI group had diabetes. Compared with these worldwide registries, the Taiwan ACS registry had higher DM prevalence no matter whether NSTEMI or STEMI patients were being compared.
Like other studies4,12-20, the diabetes patients in our study had more traditional cardiovascular risk factors than the non-DM patients, such as hypertension (77.2% vs. 57.8%, p < 0.001), dyslipidemia (51.0% vs. 33.8%, p < 0.001) and poorer renal function (2.0 ± 2.2 vs. 1.42 ± 1.6, p < 0.001). Also, these diabetes patients were associated with a greater likelihood of stroke (12.7% vs. 7.4%, p < 0.001) and peripheral artery diseases (4.0% vs. 1.42%, p < 0.001).
Several previous studies have reported worse ACS outcomes among patients with diabetes.22-26 In these studies, diabetes was an independent predictor for mortality, for both short and long-term outcomes. In our study, diabetic patients were at a higher risk of all-cause death (10.1% vs. 6.1%, p < 0.05) and the primary outcomes (15.7% vs. 11.0%, p < 0.05) when compared with non-DM patients after multivariable adjustment analysis. The adjustment factors included age, sex, Killip class, hypertension, dyslipidemia, serum creatinine, smoking, family history of CAD, previous CAD, prior stroke, previous heart failure, and evidence-based medications including ACEI, ARB, statin, aspirin and clopidogrel, which would influence the outcomes (Figure 2). These findings may help to better document the effect of DM on the prognosis for ACS patients in Taiwan.
In our study, patients with diabetes were less likely to be treated in accordance with standardized therapy. Furthermore, they received less aspirin, and less clopidogrel. Also, the rate of primary PCI for STEMI was lower in diabetic patients (Table 2). This result was consistent with previous studies of Taiwanese patients with ACS.21,25-27 Thus in the real-world ACS practice in Taiwan, the use of evidence-based medication was suboptimal.25-27 Treatment was strongly associated with the prognosis of the patients who suffered cardiac events. The suboptimal usage of these medications and treatment might explain the poorer outcomes. This is apparent not just in our study, but in other investigations where authors have analyzed the data from several large worldwide registries28 and concluded that ACS patients with diabetes continue to be treated more conservatively than other patients, despite evidence that they would derive similar or even greater benefits from aggressive treatment. This real world underutilization of evidence-based therapies for diabetes patients with ACS may contribute to worse outcome. In Taiwan, there is a need to close the gap between real-world practices and standardized therapies, especially for diabetes patients.
LIMITATIONS
Our study was a post-hoc analysis based on data from the Taiwan ACS registry. Several parameters such as glucose levels, HbA1c data or glycemic control strategies were not available due to the original study design. We therefore cannot know the relationship between the severity and duration of diabetes and ACS outcomes. In addition, some patients may suffer from transient hyperglycemia due to acute illness and these patients might also be enrolled in our DM group. Lastly, our study shows outcomes over only 1 year and it could be useful to follow up the patients for a longer time to get more information.
CONCLUSION
ACS patients with diabetes had significantly worse outcomes regarding all-cause death and the combined results for death, re-MI and stroke, compared to patients without DM. Patients with DM are also given less aggressive treatment, which may be a factor in the worse outcomes.
REFERENCES
- 1. Jiang YD, Chang CH, Tai TY, et al. Incidence and prevalence rates of diabetes mellitus in Taiwan: analysis of the 2000-2009 national wide health insurance database. J Formos Med Assoc. 2012;111:599–604. doi: 10.1016/j.jfma.2012.09.014. [DOI] [PubMed] [Google Scholar]
- 2. The Taiwan declaration on diabetes . http://www.diabetes.org.tw/wddte_wdd4.jsp . 2007 [Google Scholar]
- 3. Chou P, Chen HH, Hsiao KJ. Community-based epidemiological study on diabetes in Pu-Li, Taiwan. Diabetes Care. 1992;15:81e9. doi: 10.2337/diacare.15.1.81. [DOI] [PubMed] [Google Scholar]
- 4. GRACE Investigators. Rationale and design of the GRACE (Global Registry of Acute Coronary Events) Project: a multinational registry of patients hospitalized with acute coronary syndromes. Am Heart J. 2001;141:190–199. doi: 10.1067/mhj.2001.112404. [DOI] [PubMed] [Google Scholar]
- 5. Goldberg RB. Cardiovascular disease in diabetic patients. Med Clin North Am. 2000;84:81–93. doi: 10.1016/s0025-7125(05)70208-x. [DOI] [PubMed] [Google Scholar]
- 6. Savage MP, Krolewski AS, Kenien GG, et al. Acute myocardial infarction in diabetes mellitus and significance of congestive heart failure as a prognostic factor. Am J Cardiol. 1988;62:665–669. doi: 10.1016/0002-9149(88)91199-x. [DOI] [PubMed] [Google Scholar]
- 7. Zuanetti G, Latini R, Maggioni AP, et al. Influence of diabetes on mortality in acute myocardial infarction: data from the GISSI-2 study. J Am Coll Cardiol. 1993;22:1788–1794. doi: 10.1016/0735-1097(93)90758-s. [DOI] [PubMed] [Google Scholar]
- 8. Tseng CH. Mortality and causes of death in a national sample of diabetic patients in Taiwan. Diabetes Care. 2004;27:1605–1609. doi: 10.2337/diacare.27.7.1605. [DOI] [PubMed] [Google Scholar]
- 9. De Luca G, Dirksen MT, Spaulding C, et al. Impact of diabetes on long-term outcome after primary angioplasty: insights from the DESERT cooperation. Diabetes Care. 2013;36:1020–1025. doi: 10.2337/dc12-1507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Jimenez-Quevedo, Sabate M, Angiolillo DJ, et al. Long-term clinical benefit of sirolimus-eluting stent implantation in diabetes patients with de novo coronary stenosis: long-term results of the DIABETES trial. EHJ. 2007;28:1946–1952. doi: 10.1093/eurheartj/ehm197. [DOI] [PubMed] [Google Scholar]
- 11.International Epidemiological Association guidelines. http://www.ieaweb.org/index.php?option=com_content&view=article&id=15%3Agood-epidemiological-practice-gep&catid=20%3Agood-epidemiological-practice-gep&Itemid=43&limitstart=1 [Google Scholar]
- 12. Eagle KA, Goodman SG, Avezum Á, et al. Practice variation and missed opportunities for reperfusion in ST-segment-elevation myocardial infarction: findings from the Global Registry of Acute Coronary Events (GRACE) Lancet. 2002;359:373–377. doi: 10.1016/S0140-6736(02)07595-5. [DOI] [PubMed] [Google Scholar]
- 13. Goldberg RJ, Currie K, White K, et al. Six-month outcomes in a multinational registry of patients hospitalized with an acute coronary syndrome (the Global Registry of Acute Coronary Events [GRACE]) Am J Cardiol. 2004;93:288–293. doi: 10.1016/j.amjcard.2003.10.006. [DOI] [PubMed] [Google Scholar]
- 14. Franklin K, Goldberg RJ, Spencer F, et al. Implications of diabetes in patients with acute coronary syndromes. The Global Registry of Acute Coronary Events. Arch Intern Med. 2004;164:1457–1463. doi: 10.1001/archinte.164.13.1457. [DOI] [PubMed] [Google Scholar]
- 15. Diercks DB, Owen KP, Kontos MC, et al. Gender differences in time to presentation for myocardial infarction before and after a national women’s cardiovascular awareness campaign: a temporal analysis from the Can Rapid Risk Stratification of Unstable Angina Patients Suppress ADverse Outcomes with Early Implementation (CRUSADE) and the National Cardiovascular Data Registry Acute Coronary Treatment and Intervention Outcomes Network-Get with the Guidelines (NCDR ACTION Registry-GWTG) Am Heart J. 2010;160:80–87. doi: 10.1016/j.ahj.2010.04.017. [DOI] [PubMed] [Google Scholar]
- 16. Forman DE, Chen AY, Wiviott SD, et al. Comparison of outcomes in patients aged < 75, 75-84, ≥ 85 years with ST-elevation myocardial infarction (from the ACTION Registry-GWTG) Am J Cardiol. 2010;106:1382–1388. doi: 10.1016/j.amjcard.2010.07.008. [DOI] [PubMed] [Google Scholar]
- 17. Guzman LA, Li S, Wang TY, et al. Differences in treatment patterns and outcomes between Hispanics and non-Hispanic whites treated for ST-segment elevation myocardial infarction: results from the NCDR ACTION Registry-GWTG. J Am Coll Cardiol. 2012;59:630–631. doi: 10.1016/j.jacc.2011.10.882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Mathews R, Peterson ED, Chen AY, et al. In-hospital major bleeding during ST-elevation and non-ST-elevation myocardial infarction care: derivation and validation of a model from the ACTION Registry(R)-GWTG. Am J Cardiol. 2011;107:1136–1143. doi: 10.1016/j.amjcard.2010.12.009. [DOI] [PubMed] [Google Scholar]
- 19. Chin CT, Chen AY, Wang TY, et al. Risk adjustment for in-hospital mortality of contemporary patients with acute myocardial infarction: the acute coronary treatment and intervention outcomes network (ACTION) registry-get with the guidelines (GWTG) acute myocardial infarction mortality model and risk score. Am Heart J. 2011;161:113–122. doi: 10.1016/j.ahj.2010.10.004. [DOI] [PubMed] [Google Scholar]
- 20. Peterson ED, Roe MT, Chen AY, et al. The NCDR ACTION Registry-GWTG: transforming contemporary acute myocardial infarction clinical care. Heart. 2010;96:1798–1802. doi: 10.1136/hrt.2010.200261. [DOI] [PubMed] [Google Scholar]
- 21. Chiang FT, Shyu KG, Wu CJ, et al. Predictors of one-year outcomes in the Taiwan acute coronary syndrome full spectrum registry . J Formos Med Assoc. 2014;112:794–802. doi: 10.1016/j.jfma.2013.08.001. [DOI] [PubMed] [Google Scholar]
- 22. Brener SJ, Mehran R, Dressler O, et al. Diabetes mellitus, myocardial reperfusion and outcome in patients with acute ST elevation myocardial infarction treated with primary angioplasty; insights from HORIZON AMI. Am J Cardio. 2012;109:1111–1116. doi: 10.1016/j.amjcard.2011.11.046. [DOI] [PubMed] [Google Scholar]
- 23. Frye RL, August P, Brooks MM, et al. A randomized trial of therapies for type 2 diabetes and coronary artery disease. N Engl J Med. 2009;360:2503–2515. doi: 10.1056/NEJMoa0805796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Lee TT, Feinberg L, Baim DS, et al. Effect of diabetes mellitus on five-year clinical outcomes after single-vessel coronary stenting (a pooled analysis of coronary stent clinical trials) Am J Cardiol. 2006;98:718–721. doi: 10.1016/j.amjcard.2006.03.059. [DOI] [PubMed] [Google Scholar]
- 25. Shyu KG, Wu CJ, Mar GY, et al. Clinical characteristics, management and in-hospital outcomes of patients with acute coronary syndrome-observation from the Taiwan ACS full spectrum registry. Acta Cardio Sin. 2011;27:135–144. [Google Scholar]
- 26. Chua SK, Shyu KG, Hung HF, et al. Gender and age differences in short- and long-term outcomes following primary percutaneous coronary intervention for ST-Elevation myocardial infarction. Acta Cardiol Sin. 2014;30:274–283. [PMC free article] [PubMed] [Google Scholar]
- 27. Lin TH, Lai WT, Hsin HT, et al. Effects of clopidogrel on mortality, cardiovascular and bleeding outcomes in patients with chronic kidney disease - Data from Taiwan acute coronary syndrome full spectrum registry. PLoS One. 2013;8(8): e71917. doi: 10.1371/journal.pone.0071917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Temporal changes in the management and outcome of Canadian diabetic patients hospitalized for non-ST-elevation acute coronary syndromes. Am Heart J. 2011;162:347–355. doi: 10.1016/j.ahj.2011.05.020. [DOI] [PubMed] [Google Scholar]