Abstract
Background
Left ventriculography (LVG) is a gold standard examination of left ventricular function, although it also involves a small but significant risk of complications. However, it was recently reported to be overused in the USA in comparison to an alternative imaging modality. In this study, our aim was to analyze the real-world use of LVG in Taiwan.
Methods
This cohort study analyzed the data in the Taiwan National Health Insurance Bureau database for patients undergoing coronary angiography from 1996-2008. The most recent imaging modalities were used to evaluate left ventricular function including echocardiography and single-photon emission computed tomography (SPECT) within 30-day. The primary outcome was the concomitant use of LVG during coronary angiography.
Results
Of 8653 patients who underwent coronary angiography, LVG was performed on 4634 (53.6%) of those study participants. The frequency of LVG use was lower in the groups indicating left ventricular function evaluation, including acute myocardial infarction, heart failure and shock (49.5 vs. 57.1%, p < 0.001). In the population that had undergone a recent left ventricular assessment, the use of LVG was lower (52.2% vs. 54.7%, p = 0.03). Multivariate analysis found that 30-day imaging tests are not a predictor for use of LVG.
Conclusions
In Taiwan, about one half of those patients whose data we reviewed actually received coronary angiography and LVG at the same time. Ultimately, we found that there was no overuse of LVG in those patients with recent alternative imaging modality performed.
Keywords: Angiography, Coronary, Ventriculography
INTRODUCTION
Left ventriculography (LVG) has been developed and in use for more than 50 years.1,2 It is an imaging technique used to evaluate left ventricular systolic function, regional wall motion, and mitral regurgitation, and is often performed along with other cardiac catheterization examinations. However, the LVG procedure requires cardiac catheterization and contrast medium, which involves the associated risks of renal injury and allergic reaction. Many new noninvasive techniques have been developed and could also be used to evaluate left ventricular function. So LVG may be unnecessary or redundant if another functionally equivalent tool was recently used instead. Nevertheless, under certain critical heart conditions necessitating coronary angiography, the LVG can immediately evaluate heart function. We performed this study for the purpose of examining the real-world use of LVG in Taiwan.
MATERIALS AND METHODS
Data source
The data was analyzed from the National Health Insurance Research Dataset (NHIRD), published by the National Health Research Institute (NHI) in Taiwan, which provided a database of 1,000,000 cases randomly selected from people insured in 2005. Medical claims data during the period 1996-2008 were available for all insureds. The NHI program has been implemented in Taiwan since 1995, offering a comprehensive, unified, and universal health insurance program for all Taiwan citizens. Those citizens who have established a registered domicile for at least 4 months in the Taiwan area are in the position to be enrolled in NHI. This coverage provides outpatient service, inpatient care, Chinese medicine, dental care, childbirth, physical therapy, preventive health care, home care, as well as rehabilitation for chronic mental illness. The coverage rate was 96.16% of the entire Taiwan population in 2000 and further increased to 99% by the end of 2004. The NHI medical claims database also includes ambulatory care, hospital inpatient care, dental services, and prescription drugs. Therefore, the NHIRD is one of the largest and most complete nationwide population-based datasets in Taiwan and there were no statistically significant differences in age, sex, and average insured payroll-related amount between the sample group and all enrollees.3
Because these were secondary data, each patient’s original identification number has been encrypted by a consistent procedure to protect privacy, so that linkage of claims relating to the same patient is feasible within the NHI Research Database.
Study sample
This study population included all adults hospitalized for coronary angiography from January 1, 1996 to December 31, 2008. If a patient had received coronary angiography several times during the study period, the first episode was selected. Coronary angiography was defined by reimbursement for any of the following treatment codes: 18020B or 18021B.
The ejection fraction measurement
LVG during coronary angiography was defined as a claim for 18026B occurring on the same day of the coronary angiography. The alternative left ventricular ejection fraction (LVEF) measurement was defined as echocardiography (codes: 18005B, 18006B, 18007B), stress and redistribution myocardial perfusion study with single-photon emission computed tomography (SPECT) (codes: 26025B). We calculated the frequency of two alternative ejection fraction measurements on the same days and in the prior 30 and 90 days before coronary angiography.
Inpatient diagnosis
The inpatient claims were used to determine the International Classification of Diseases, Ninth Edition (ICD-9) diagnoses for diabetes (codes: 250.0-250.3, 250.7), hypertension (codes: 401-405), heart failure (codes: 428, 429.3, 402.01, 402.11, 402.91, and 425), renal failure (codes: 582, 583, 585, 586, and 588), shock (codes: 458 and 785.5), acute myocardial infarction (codes: 410 and 412), ischemic heart disease (codes: 410-414), and ischemic stroke (codes: 433-434, 436) as major diagnoses for admission.
Statistical analysis
We determined the frequency of LVG stratified by inpatient diagnoses and a prior measurement of ejection fraction. The Chi-square test was used to evaluate for categorical variables, and two-sample t tests were used to evaluate differences in continuous variables. The adjusted odds ratio was derived by multivariate logistic regression to identify the determinants of LVG. A 2-sided p value < 0.05 was considered statistically significant. All analyses were conducted using SAS 9.3 (SAS, Cary, NC, USA).
RESULTS
We identified a total of 8653 patients with baseline clinical characteristics in Table 1. This included 89.8% patients with ischemic heart disease, 26.0% patients with heart failure, 4.6% patients with shock, and 50.1% patients who underwent an imaging study to evaluate ventricular function within a 30-day period. Among all patients who underwent coronary angiography, LVG was performed in 4634 (53.6%).
Table 1. Characteristics of patients with and without left ventriculography .
| Total | LVG | No LVG | p value | |
| N (%) | 8653 | 4634 (53.6) | 4019 (46.4) | |
| Age (y), mean ± SD | 63.2 ± 13.0 | 65.1 ± 13.1 | < 0.001 | |
| Male gender, n (%) | 5546 (64.1) | 2936 (63.4) | 2610 (64.9) | 0.13 |
| 30-day image use (%) | 4099 (50.1) | 2139 (48.9) | 1960 (51.4) | 0.03 |
| Diagnosis, n (%) | ||||
| IHD | 7770 (89.8) | 4201(90.7) | 3569 (88.8) | 0.005 |
| Ischemic stroke | 1071 (12.4) | 591 (12.8) | 480 (11.9) | 0.25 |
| Heart failure | 2252 (26.0) | 1204 (26.0) | 1048 (26.1) | 0.92 |
| Hypertension | 6286 (72.6) | 3334 (71.9) | 2952 (73.5) | 0.12 |
| Diabetes | 3181(36.8) | 1599 (34.5) | 1582 (39.4) | < 0.001 |
| Renal failure | 1263 (14.6) | 567 (12.2) | 696 (17.3) | < 0.001 |
| Myocardial infarction | 2340 (27.0) | 1039 (22.4) | 1301 (32.4) | < 0.001 |
| Shock | 394 (4.6) | 156 (3.4) | 238 (5.9) | < 0.001 |
CI, confidence interval; IHD, ischemic heart disease; LVG, left ventriculography.
Potential indications for LVG
We identified patients who may have potential indications for LVG due to critical heart conditions (Figure 1). These included those hospitalized with a diagnosis of heart failure (n = 2252), acute myocardial infarction (n = 2340), or shock (n = 394). Overall, 4051 (46.8%) patients undergoing coronary angiography had at least one of three indications. However, the frequency of LVG use was lower in the group (49.5 vs. 57.1%, p < 0.001). The frequency of LVG use was significantly lower in patients with a diagnosis of acute myocardial infarction or shock as compared to those patients without similar diagnoses (44.4 vs. 56.9 and 39.6 vs. 54.2%, both p < 0.001). In patients with heart failure, the percentage of use of LVG is not statistically different (53.5 vs. 53.6%, p = 0.92).
Figure 1.
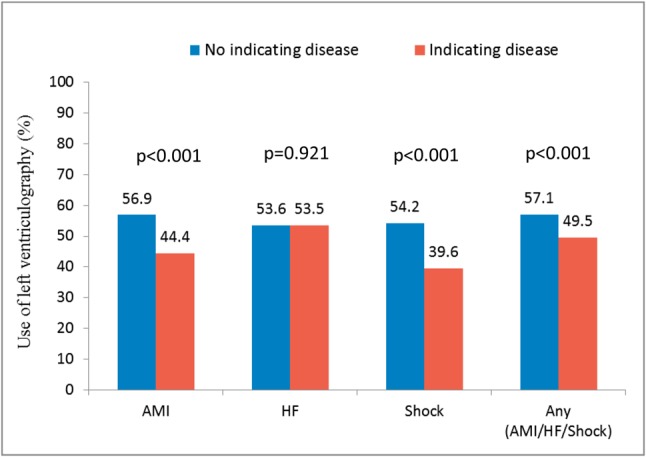
Frequency of left ventriculography for indicating diseases. AMI, acute myocardial infarction; HF, heart failure. In the above chart, I would use “Not” indicating disease instead of “No” indicating disease.
Prior assessment of left ventricular function
The 30-day alternative imaging modality to evaluate left ventricular function (LVF) includes echocardiography and SPECT. Overall, 43.7% of patients undergoing LVG had already received an alternative LVEF measurement within the prior 30 days and the rate increased to 55.3% when the date extended to 90 days (Figure 2). Those patients with a recent LVF measurement by alternative techniques were less likely to undergo LVG (52.2 vs. 54.7%, p = 0.03). If echocardiography had been used in the most recent 30 days, patients were less likely to receive LVG (50.3 vs. 56.5% p < 0.001). However, the use of LVG increased in patients undergoing recent SPECT (59.9 vs. 52.2%, p < 0.01) (Figure 3).
Figure 2.
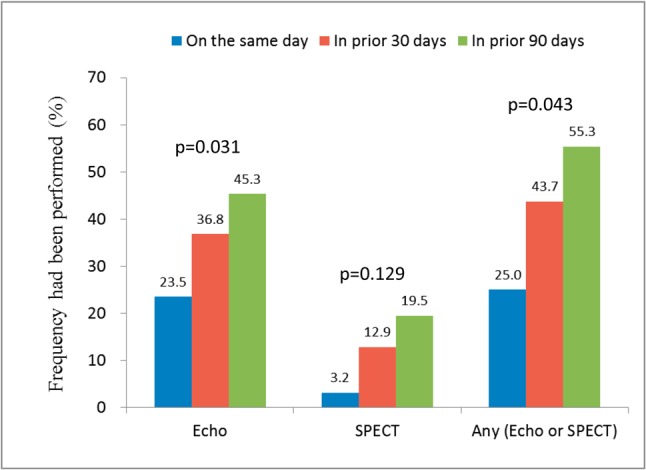
Frequency of imaging study already performed on the patients receiving left ventriculography. Echo, echocardiography; SPECT, single-photon emission computed tomography.
Figure 3.
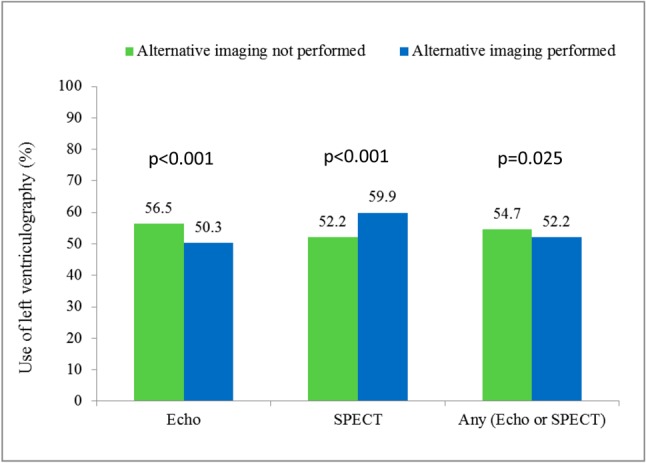
Frequency of left ventriculography if a patient had recently undergone the alternative imaging study in the prior 30 days before coronary angiography. Echo, echocardiography; SPECT, single-photon emission computed tomography.
Factors associated with use of LVG
We calculated the adjusted odds ratio (AOR) of LVG use in different subgroups (Table 2). After multivariate analysis, only ischemic heart disease, ischemic stroke, and heart failure were positively associated with LVG. Patient age, shock, acute myocardial infarction, renal failure, and diabetes were negatively associated with LVG.
Table 2. Multivariate correlates of left ventriculography .
| AOR | 95% CI | p value | |
| Age | 0.99 | 0.98-0.99 | < 0.001 |
| Male gender | 0.93 | 0.84-1.02 | 0.11 |
| 30-day image use | 0.98 | 0.90-1.08 | 0.72 |
| IHD | 1.29 | 1.11-1.49 | < 0.001 |
| Ischemic stroke | 1.17 | 1.02-1.34 | 0.02 |
| Heart failure | 1.15 | 1.04-1.28 | 0.009 |
| Hypertension | 0.98 | 0.89-1.09 | 0.74 |
| Diabetes | 0.87 | 0.79-0.95 | 0.003 |
| Renal failure | 0.72 | 0.63-0.82 | < 0.001 |
| Myocardial infarction | 0.65 | 0.58-0.72 | < 0.001 |
| Shock | 0.69 | 0.55-0.86 | < 0.001 |
AOR, adjusted odds ratio; CI, confidence interval; IHD, ischemic heart disease; LVG, left ventriculography.
DISCUSSION
In the present study, we have three major findings. First, LVG was performed in 53.6% of patients during coronary angiography. Second, the frequency of LVG use was lower in the groups indicating for left ventricular function evaluation. Third, in the population that had undergone a recent 30-day ejection fraction assessment by another modality, the use of LVG was significantly lower.
The LVG was introduced approximately 50 years ago and it represented a superior modality to image left ventricular systolic function and regional wall motion compared with other techniques available at the same time.1,4-6 However, the LVG has many limitations. It is an invasive examination requiring arterial cannulation and use of a cardiac catheterization laboratory. Additionally, it can only provide the 2-dimensional assessment of a single chamber and a single valve at one time. Besides, the quality of LVG is difficult to optimize. Ventricular arrhythmia and inadequate opacification of the ventricular cavity can cause unsatisfactory resulting images. According to Deligonul et al., even when utilized by experienced operators using biplane imaging, only 20% of imaging quality was considered “excellent”.7 Moreover, performing LVG is not completely safe; it carries a risk of ventricular arrhythmia, heart block, thromboembolic event, and extra contrast injection. The contrast volume is usually 30-45 mL, which is nearly equal to the total contrast used in diagnostic coronary angiography.7-9 Studies have validated that total contrast dose is an independent risk factor for the development of contrast-induced nephropathy and this complication could increase mortality.10,11 In Taiwan, we found LVG was performed in 53.6% patients during coronary angiography.
With the development and widespread use of new diagnostic imaging techniques, such as echocardiography, nuclear scintigraphy, and magnetic resonance imaging, the use of LVG could be replaced by new modalities. Despite this, the use of LVG appears to be routine, even when its use overlaps with other recently obtained imaging tests.12,13 According to study of Witteles et al., LVG was overused in the USA. They found that LVG was performed on more than 80% of patients undergoing coronary angiography and most of its use was not indicated.13 Our study evaluated the use of LVG in Taiwan. First, clinicians in Taiwan tended to perform fewer LVGs in the elderly and those suffering from conditions of shock, acute myocardial infarction, renal failure, and diabetes. Second, the use of LVG is reasonable for patients with a higher acuity of illness necessitating coronary angiography because it could provide an on-site assessment of left ventricular function and regional wall motion. However, we found the LVG is less frequently used in patients with acute myocardial infarction and shock. Third, although the LVG was less frequently performed when recent echocardiographic imaging had assessed LVEF, it was more frequently used in those patients who had recently received nuclear scintigraphy.
LIMITATIONS OF THE STUDY
There were several limitations in this study. It is possible that some of the prior LVEF assessments were not of sufficient diagnostic quality and that LVG was therefore a reasonable test. However, in recent years, rates of non-diagnostic studies with echocardiography and nuclear scintigraphy are low. Second, we did not evaluate the influence of additional imaging tests, such as magnetic resonance imaging and coronary computed tomography angiography. However, given that the rate these tools were used was much lower in most clinical conditions, this would not alter the fundamental findings of the study. Third, nuclear medicine doctors might not routinely calculate left ventricular ejection fraction. Furthermore, some physicians could not be convinced of the accuracy of left ventricular function assessment by SPECT, which might partially explain why the frequency of LVG use is higher in those patients who recently underwent nuclear scintigraphy.
CONCLUSION
In an analysis of NHIRD with 8653 patients undergoing coronary angiography in Taiwan from 1996 to 2008, we found that LVG was concomitantly performed in 53.6%. Compared with the USA data, the LVG was not overused in patients who had received recent LVEF measurement in Taiwan. However, the LVG was less frequently performed in certain patient(s) indicating for it such as acute myocardial infarction and shock. Therefore, it would be of value for the education of physicians and their clinical practice guidelines to include the definition of adequate use of LVG.
Acknowledgments
The authors thank those generous people at the Statistical Analysis Laboratory, Department of Internal Medicine, and Kaohsiung Medical University Hospital for their assistance.
This study is based in part on data from the National Health Insurance Research Database provided by the Bureau of National Health Insurance, Department of Health and managed by National Health Research Institutes (Registered number 98178). The interpretation and conclusions contained herein do not represent those of the Bureau of National Health Insurance, Department of Health or National Health Research Institutes.
CONFLICT OF INTEREST STATEMENT
All authors have no financial interests related to the material in the manuscript.
REFERENCES
- 1. Dodge HT, Sandler H, Ballew DW, Lord JD., Jr. The use of biplane angiocardigraphy for the measurement of left ventricular volume in man. Am Heart J. 1960;60:762–776. doi: 10.1016/0002-8703(60)90359-8. [DOI] [PubMed] [Google Scholar]
- 2. Arvidsson H. Angiocardiographic determination of left ventricular volume. Acta Radiol. 1961;56:321–339. doi: 10.3109/00016926109172827. [DOI] [PubMed] [Google Scholar]
- 3. National Health Insurance Research Database. NIH. (Accessed at http://w3.nhri.org.tw/nhird/en/Background.html) [Google Scholar]
- 4. Dodge HT, Hay RE, Sandler H. An angiocardiographic method for directly determining left ventricular stroke volume in man. Circ Res. 1962;11:739–745. doi: 10.1161/01.res.11.4.739. [DOI] [PubMed] [Google Scholar]
- 5. Dodge HT, Sandler H, Baxley WA, Hawley RR. Usefulness and limitations of radiographic methods for determining left ventricular volume. Am J Cardiol. 1966;18:10–24. doi: 10.1016/0002-9149(66)90191-3. [DOI] [PubMed] [Google Scholar]
- 6. Arvidsson H. Angiocardiographic determination of left ventricular volume and its apllications. Radiologe. 1967;7:200–205. [PubMed] [Google Scholar]
- 7. Deligonul U, Jones S, Shurmur S, Oskarsson H. Contrast cine left ventriculography: comparison of two pigtail catheter shapes and analysis of factors determining the final quality. Cathet Cardiovasc Diagn. 1996;37:428–433. doi: 10.1002/(SICI)1097-0304(199604)37:4<428::AID-CCD12>3.0.CO;2-B. [DOI] [PubMed] [Google Scholar]
- 8. Shammas NW, Lee JK, Daubert JP, Pomerantz RM. Complete heart block complicating retrograde left ventricular catheterization: case report and review. Cathet Cardiovasc Diagn. 1994;31:122–126. doi: 10.1002/ccd.1810310206. [DOI] [PubMed] [Google Scholar]
- 9. Goldenberg I, Shupak A, Shoshani O, Boulos M. Left ventriculography complicated by cerebral air embolism. Cathet Cardiovasc Diagn. 1995;35:331–334. doi: 10.1002/ccd.1810350411. [DOI] [PubMed] [Google Scholar]
- 10. McCullough PA, Wolyn R, Rocher LL, et al. Acute renal failure after coronary intervention: incidence, risk factors, and relationship to mortality. Am J Med. 1997;103:368–375. doi: 10.1016/s0002-9343(97)00150-2. [DOI] [PubMed] [Google Scholar]
- 11. Rihal CS, Textor SC, Grill DE, et al. Incidence and prognostic importance of acute renal failure after percutaneous coronary intervention. Circulation. 2002;105:2259–2264. doi: 10.1161/01.cir.0000016043.87291.33. [DOI] [PubMed] [Google Scholar]
- 12. Santolucito PA, Tighe DA, Lessard D, et al. Changing trends in the evaluation of ejection fraction in patients hospitalized with acute myocardial infarction: the Worcester Heart Attack Study. Am Heart J. 2008;155:485–493. doi: 10.1016/j.ahj.2007.10.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Witteles RM, Knowles JW, Perez M, et al. Use and overuse of left ventriculography. Am Heart J. 2012;163:617–623 e1. doi: 10.1016/j.ahj.2011.12.018. [DOI] [PubMed] [Google Scholar]


