Abstract
Background
Depression and anxiety are common in heart failure (HF) patients and associated with adverse clinical outcomes. However, there are little or no published data that focuses on the relationship between these commonly observed situations and HF classes. The aim of this study was to evaluate the relationship between these psychiatric co-morbidities and HF symptom classes. As a second objective of our study, the associations between patient characteristics and depression severity were also assessed.
Methods
Our study enrolled a total of 420 HF study participants. The severity of depressive and anxiety symptoms was evaluated by Beck’s depression and anxiety. The measured total scores were used to grade depression severity and anxiety as minimal/mild and moderate/severe.
Results
According to NYHA Functional Classification, 228 patients (51%) had class I symptoms, 101 (23%) had class II symptoms, 31 (7%) had class III symptoms, and class IV symptoms were noted in the remaining 60 patients (19%). The mean Beck’s depression and anxiety scores were 12.4 ± 11.1 and 13.4 ± 9.0, respectively. While no association between HF symptom classes and anxiety severity was observed, a significant positive relation between HF symptom class and depression score was found.
Conclusions
The results of our study suggested that HF symptom class was positively associated with severity of depression. On the other hand, there was no association between HF symptom class and anxiety score in a wide population of heart failure patients.
Keywords: Anxiety, Depression, Heart failure
INTRODUCTION
Heart failure (HF) is commonly seen in the present era and associated with increased morbidity and mortality. Currently, the total number of HF patients around the world is estimated to be around 23 million.1 Nevertheless, as the world population ages, with an increasing rate of coronary event treatment, this number is expected to increase even moreso. Despite advances in treatment, mortality remains high and the 5-year survival rate of patients with HF is approximately 20%.2 Additionally, frequent hospitalizations, mandatory dietary restrictions and other social life and socialization problems experienced may negatively affect the quality of life.
In recent years, it has been suggested that psychosocial risk factors are associated with cardiovascular diseases as well as worsening of disease prognosis.3 One of these factors is depression and it is common in patients with HF, with a prevalence ranging between 11-51%.1-6 Depression rates can be much higher among patients screened with questionnaires or with more advanced HF. Additionally, depression is associated with worse outcomes such as increased morbidity, mortality, HF related hospitalizations and impaired quality of life; therefore, assessment and behavioral intervention efforts are needed based on profiling of patient factors early in the HF process.5,7,8
In the literature, there is a paucity of studies which have investigated the consequence of the anxiety symptoms in HF patients, and conflicting results were obtained regarding the relationship between this behavioral entity and HF severity and prognosis.9-14 Therefore, the general or specific associations between these common situations and HF symptom class are still obscure.
By undertaking this cross-sectional study, we aimed to test the relation between HF symptom class and the prevalence of psychiatric co-morbidities. As a second objective of our study, we assessed the associations between the characteristics of patients and depression severity.
MATERIALS AND METHODS
Study population
A total of 420 consecutive adult outpatients with a diagnosis of HF for at least three months were recruited into the study between October 2012 and September 2013. Patients who had developed conditions that are strongly associated with the development of HF and showed at least NYHA class I symptoms were included.15 These conditions included common structural heart diseases due to known left ventricular hypertrophy and previous myocardial infarction or acute coronary syndrome, hypertension, lipid disorders, obesity, diabetes mellitus, tobacco and other known cardiotoxic agents. The study protocol was approved by the local ethics committee and informed consent was obtained from all patients. The study complied with the declaration of Helsinki. Patients were excluded if they were using or used psychiatric drug, refused to participate, had cognitive impairments, a history of psychiatric disorder or life-threatening diseases (e.g. cancer).
Procedures
Socio-demographic and clinical risk factors including gender, hypertension, diabetes, hyperlipidemia, smoking, coronary artery disease (CAD), marital status, number of child, employment status, income level, educational level, time to HF diagnosis, previous HF hospitalizations, etiology of HF (ischemic vs. non-ischemic), medications, New York Heart Association (NYHA) class, and co-morbidities were assessed for all patients. In addition, laboratory, echocardiographic and electrocardiographic (ECG) findings were recorded (Table 1 and Table 2).
Table 1. Clinical and demographic characteristics of the study patients .
| Variable | All patients | Minimal-mild depression | Moderate-severe depression | Odds ratios (95% CI) | p value |
| Age, (years) | 57.9 ± 14.4 | 55.5 ± 14.2 | 63.2 ± 13.2 | - | < 0.001 |
| Male gender, n (%) | 201 (45) | 124 (46) | 69 (49) | 1.1 (0.7-1.7) | 0.6 |
| Dyslipidemia, n (%) | 112 (25) | 69 (26) | 40 (28) | 1.1 (0.7-1.8) | 0.57 |
| Diabetes mellitus n (%) | 140 (31) | 71 (26) | 64 (45) | 2.3 (1.5-3.5) | < 0.001 |
| Hypertension n (%) | 248 (55) | 134 (50) | 109 (77) | 3.4 (2.1-5.4) | < 0.001 |
| Smoking n (%) | 182 (41) | 117 (44) | 57 (40) | 0.9 (0.6-1.3) | 0.5 |
| Family history of CAD, n (%) | 87 (19) | 66 (25) | 20 (14) | 0.5 (0.3-0.9) | 0.01 |
| Previous MI n (%) | 91 (20) | 45 (17) | 46 (33) | 2.4 (1.5-3.9) | < 0.001 |
| Previous CABG, n (%) | 58 (13) | 25 (9) | 33 (23) | 3.0 (1.7-5.2) | < 0.001 |
| CAD, n (%) | 249 (56) | 140 (52) | 106 (75) | 2.8 (1.8-4.3) | < 0.001 |
| Ischemic HF, n (%) | 233 (52) | 62 (23) | 125 (88) | 26 (14-47) | < 0.001 |
| HF duration(years) | 6.6 ± 5.3 | 6.3 ± 4.9 | 7.2 ± 5.8 | - | 0.11 |
| Hospitalization* | 1.8 ± 2.3 | 1.3 ± 2.0 | 2.5 ± 2.5 | - | < 0.001 |
| NYHA class | - | < 0.001 | |||
| Class 1, n (%) | 228 (51) | 213 (79)# | 5 (3.5)# | ||
| Class 2, n (%) | 101(23) | 41 (15)# | 59 (42)# | ||
| Class 3, n (%) | 31 (7) | 11 (4)# | 20 (14)# | ||
| Class 4, n (%) | 60 (19) | 3 (1)# | 57 (40)# | ||
| LVEF (%) | 54.2 ± 12.4 | 57.5 ± 9.6 | 47.5 ± 14.6 | - | < 0.001 |
| BDI score | 12.4 ± 11.1 | 5.5 ± 4.7 | 25.5 ± 7.3 | - | < 0.001 |
| BAI score | 13.4 ± 9.0 | 12.1 ± 8.1 | 15.8 ± 10.1 | - | < 0.001 |
BAI, Beck Anxiety Inventory; BDI, Beck Depression Inventory; CABG, coronary artery bypass grafting; CAD, coronary artery disease; HF, heart failure; LVEF, left ventricular ejection fraction; MI, myocardial infarction; NYHA, New York Heart Association.
* Number of hospitalizations in the last year. # Denotes significant column proportions by Chi-Square test.
Table 2. Demographic, socioeconomic, medical and laboratory characteristics of the study patients .
| Variable | All patients | Minimal-mild depression | Moderate-severe depression | Odds ratios (95% CI) | p value |
| Education level, n (%) | - | 0.02 | |||
| Primary | 315 (70) | 191 (71)# | 116 (82)# | ||
| Secondary | 49 (11) | 31 (12) | 15 (11) | ||
| High school | 40 (9) | 31 (12) | 9 (6) | ||
| University | 16 (4) | 15 (6)# | 1 (1)# | ||
| Condition, n (%) | - | 0.01 | |||
| Unmarried | 11 (2) | 11 (4)# | 0 (0)# | ||
| Married | 338 (76) | 218 (81) | 110 (78) | ||
| Widow | 71 (16) | 39 (15) | 31 (22) | ||
| Number of child | 3.4 ± 2.1 | 3.2 ± 2.2 | 3.6 ± 2.0 | - | 0.06 |
| Career, n (%) | - | 0.03 | |||
| Unemployed | 1 (0.2) | 0 (0) | 1 (1) | ||
| Worker | 54 (12) | 41 (15)# | 11 (8)# | ||
| Officer | 9 (2) | 6 (2) | 3 (2) | ||
| Retired | 129 (29) | 72 (27)# | 54 (38)# | ||
| Housewife | 189 (42) | 119 (44) | 65 (46) | ||
| Other | 38 (8) | 30 (11) | 7 (5) | ||
| Income level*, n (%) | - | 0.12 | |||
| < 500 | 18 (4) | 12 (4) | 5 (3) | ||
| 500-1000 | 247 (55) | 148 (55) | 95 (67) | ||
| 1000-1500 | 121 (27) | 84 (31) | 31 (22) | ||
| > 1500 | 34 (8) | 24 (9) | 10 (7) | ||
| Beta blocker, n (%) | 244 (55) | 131 (49) | 108 (77) | 3.4 (2.2-5.4) | < 0.001 |
| ACEI/ARB, n (%) | 238 (53) | 127 (47) | 106 (75) | 3.4 (2.1-5.3) | < 0.001 |
| Spiranolacton, n (%) | 18 (4) | 4 (1.5) | 14 (10) | 7.2 (2.4-22.5) | < 0.001 |
| Digoxin, n (%) | 14 (3) | 5 (2) | 9 (6) | 3.6 (1.2-11.0) | 0.02 |
| Diuretic, n (%) | 103 (23) | 36 (13) | 66 (47) | 5.7 (3.5-9.2) | < 0.001 |
| Statin, n (%) | 73 (16) | 49 (18) | 23 (16) | 0.9 (0.5-1.5) | 0.62 |
| Hemoglobin, g/dl | 13.7 ± 5.2 | 13.7 ± 1.7 | 12.9 ± 1.8 | - | < 0.001 |
| Blood glucose, mg/dl | 133 ± 80 | 125 ± 73.1 | 146 ± 87 | - | 0.02 |
| Urea, mg/dl | 37.6 ± 17.9 | 33.8 ± 12 | 45.1 ± 24 | - | < 0.001 |
| Creatinine, g/dl | 1.02 ± 0.32 | 0.9 ± 0.2 | 1.1 ± 0.4 | - | < 0.001 |
| TSH, mIU/ml | 1.76 ± 1.5 | 1.7 ± 1.6 | 1.7 ± 1.3 | - | 0.8 |
ACEI/ARB, angiotensin converting enzyme inhibitor/angiotensin receptor blocker; TSH, thyroid stimulating hormone.
* Income level (Turkish Lira) < 500, low; 500-1000, low-intermediate; 1000-1500, intermediate-high; > 1500, high (1 Turkish Lira ≈ 0.33 Euro and 0.44 dollar). # Denotes significant column proportions by Chi-Square test.
The Beck Depression Inventory (BDI) and the Beck Anxiety Inventory (BAI) were used to measure the frequency and severity of patient depression and anxiety. BDI is a Likert-type scale that includes 21 symptoms and attitudes, behavioral changes, and somatic symptoms.16 The Turkish version is a reliable and valid tool that is used extensively.17 Each symptom is rated between 0-3 points and the final score ranges from 0 to 63, with higher scores representing more severe depression, where a cut-off score of ≥ 17 on each scale represents a clinically significant level of depression.16-18 Measured total scores were used to grade the severity as minimal/mild (0-16) and moderate/severe (17-63). Participants were classified into 2 groups according to severity of depression. BAI is a Likert-type scale that includes 21 evaluation sentences on a 4-point intensity scale and the final score ranges from 0 to 63.19 This scale is used to measure the level and severity of anxiety symptoms, and a cut-off point of 16 or greater was used to determine the presence of significant anxiety.18,19 Measured total scores were used to grade the severity as minimal/mild (0-15) and moderate/severe (16-63). BDI and BAI were applied to all study participants upon admission to measure the frequency and severity of depressive and anxiety symptoms of persons. The questionnaire was self-administered in an outpatient clinic.
Statistical analysis
Continuous variables were presented as mean ± standard deviation and categorical variables as numbers and percentages. A cut-off point of 17 or greater was used to determine the presence of moderate to severe depression and 2 groups were created as minimal/mild and moderate/severe. The Kolmogorov-Smirnov test was used to assess the distribution of continuous variables. Also, the Student’s t-test was used to compare normally distributed continuous variables, and the Mann-Whitney U test was used for variables without normal distribution. Categorical variables were compared using chi-square or Fisher’s exact tests and odds ratios with confidence intervals were calculated for 2 × 2 contingency tables. Correlations analyses were performed by use of Spearman’s correlation analysis. The differences between BDI and BAI scores in HF patients according to NYHA symptom class were detected with variance analysis (ANOVA). A P value of less than 0.05 was always required for statistical significance. Data were analyzed with the SPSS software version 20.0 for Windows (SPSS Inc., Chicago, Illinois, USA).
RESULTS
A total of 420 consecutive adult outpatients with a diagnosis of heart failure for at least three months were included in the study. The mean age was 57.9 × 14.4 years. Two hundred and one patients (45%) were male, 219 patients (55%) were female, 248 (55%) had hypertension, 140 (31%) had diabetes, and 249 (56%) had CAD. According to NYHA classification, 228 patients (51%) had class I symptoms, 101 (23%) had class II symptoms, 31 (7%) had class III symptoms, and class IV symptoms were found in the remaining 60 patients (19%). The mean left ventricular ejection fraction of the entire patient population was 54.2 × 12.4 % (Table 1).
The prevalence of depression was 33.5% (n = 141), and these patients had moderate/severe depressive symptoms. The mean Beck’s depression score was 12.4 ± 11.1. There was a significant positive correlation between NYHA functional class and BDI scores (p < 0.001) and the severity of depression increased with severity of HF symptom class (Figure 1). There was no significant difference between male and female regarding clinically significant depression [72 (33%) vs. 69 (36%), p > 0.05]. It was found that there was a significant positive correlation between age and depressive symptoms (p < 0.001). Patients with moderate/severe depression were older than patients with milder symptoms (63 ± 13 years vs. 55 ± 14 years, p < 0.001). Depressive symptoms were also significantly associated with increased cardiac hospitalization. In contrast, we observed no relationship between HF duration and severity of depression (7.2 ± 5.8 years vs. 6.3 ± 4.9 years, p = 0.09) (Table 1).
Figure 1.
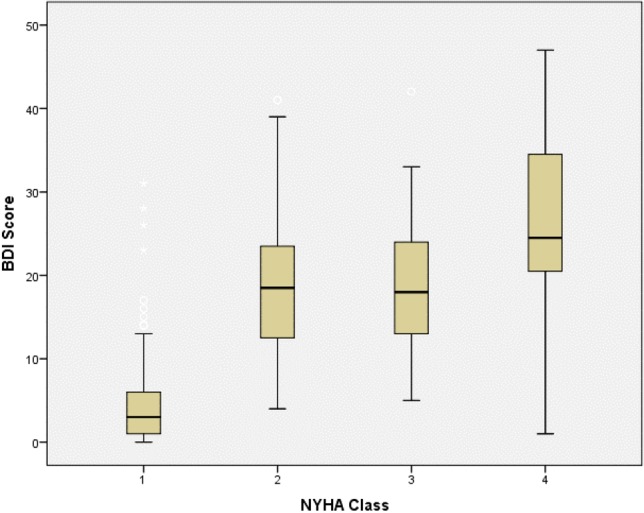
Distribution of BDI scores according to NYHA class. BDI, Beck Depression Inventory; NYHA, New York Heart Association.
While primary school educated patients were more likely to have more severe depression than otherwise, income level was not significantly associated with depression. Depression increased significantly with marriage (12.0 ± 11.1) and widow status (15.4 ± 11.1) than in unmarried status (4.6 ± 3.8) (p = 0.004) (Table 2). Clinical, demographic, socioeconomic, medical and laboratory characteristics of our study group according to depression severity is shown in Table 1 and Table 2.
The prevalence of moderate/severe anxiety was 33% (n = 138). The mean Beck’s anxiety score was 13.4 ± 9.0. No significant association was found between NYHA class and anxiety severity (p = 0.31). Age, education level, marital status, income level, and cardiac hospitalization were not significantly associated with anxiety severity (p = 0.06, 0.28, 0.98, 0.22, and 0.81, respectively). Women were more anxious than men (11.8 ± 8.6 vs. 15.1 ± 9.1, p < 0.05).
DISCUSSION
HF is a major and growing public health problem worldwide, and causes increased mortality and morbidity. It is associated with severe disease burden impacting both the population and patients. In the current study, we examined the associations between HF and severity of depression and anxiety. Most studies on the role of psychosocial risk factors in HF have focused on depression, which in several studies have shown that depression is associated with increased morbidity and mortality, including frequent and longer hospitalizations and worsening quality of life.20-23
It has been reported that the prevalence of depression and anxiety in HF patients is high, ranging between 30-50%.5,24,25-28 Unfortunately, the rates of recognizing and treating anxiety and depression in HF patients are quite low.24,29 In the current study, it was demonstrated that depressive symptoms were significantly associated with higher cardiac hospitalization rate. This finding confirmed previous studies which indicated a known relationship between increased HF related hospitalizations due to the presence of depression in HF patients.20-23
It was reported that the prevalence of depression in HF patients varied according to gender, age and NYHA classes, and it might be more common in women and in young patients.5 In the present study, we found that there was no significant difference between men and women. In contrast to previous studies, there was a significantly positive correlation between age and depression score, in that patients with moderate-severe depression were older.
The majority of previous studies have indicated that there was significant correlation between NHYA class and depressive symptoms, and the prevalence of depression increased with higher NYHA class.20,30,31 Azevodo et al. showed that there was a linear association between depressive symptoms and HF stages in women, on the other hand, in men, only stage C was associated with a higher score.32 We also found that the severity of depression increased with NYHA functional class.
Another psychosocial risk factor in HF patients is anxiety, but little is known about the role of anxiety. Previous studies showed conflicting results regarding the consequence of anxiety in HF patients. In some studies, it was determined that symptoms of anxiety were related to impaired quality of life, increased HF related hospitalizations10,26,33 and mortality.11,34 On the other hand, other studies showed that there were no significant association between anxiety and cardiac events. We also assessed the relationships among NYHA class, HF related hospitalization and symptom of anxiety and there was no significant association. It has also been previously reported that anxiety was common in women.35 Likewise, we also found that women were more anxious than men.
Previous studies have demonstrated that marital status affected depression and anxiety; married persons tend to be more depressed, whereas unmarried persons tend to exhibit anxiety.36,37 In this study, there was no significant association between marital status and anxious symptoms which is inconsistent with the findings of previous studies; in earlier investigations, BDI score was significantly higher in married group which was consistent with the literature. In contrast to the relationship between depression and age, we found no significant association between age and anxiety score. We also found that income level and education level were not linked to anxiety severity.
Limitations
The findings of the present study should be evaluated with some limitations. First, low educational level of the participants may influence the measurement reliability due to difficulty in answering the BDI and BAI questionnaire. Second, some factors in the BDI and BAI (e.g. dyspnea, fatigue, and insomnia) are common HF symptoms; therefore, the scores may not represent true depression or anxiety severity in patients with severe HF symptoms. Third, HF treatment and the timing of evaluation may influence the values of BDI and BAI.
CONCLUSION
We believe this is the first investigation to examine the relationship between the severity of depression and anxiety and HF symptom class. We demonstrated that depression and anxiety were common in outpatients with chronic HF. Depressive symptoms were significantly associated with NYHA class whereas symptoms of anxiety were not linked to symptom class. In particular, with increasing NYHA class, the presence of depression should be kept in mind. Furthermore, the coinciding of symptoms of anxiety and depression should be considered in HF patients, and routine screening for depression and anxiety should be of crucial importance in high-risk patients.
DECLARATION OF CONFLICTING INTERESTS
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
FUNDING
The authors received no financial support for the research, authorship, and/or publication of this article.
REFERENCES
- 1. McMurray JJ, Petrie MC, Murdoch DR, et al. Clinical epidemiology of heart failure: public and private health burden. Eur Heart J. 1998;19(Suppl):9–16. [PubMed] [Google Scholar]
- 2. McMurray JJ, Adamopoulos S, Anker SD, et al. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2012;33:1787–1847. doi: 10.1093/eurheartj/ehs104. [DOI] [PubMed] [Google Scholar]
- 3. Perk J, De Backer G, Gohlke H, et al. European Guidelines on cardiovascular disease prevention in clinical practice (version 2012). The Fifth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of nine societies and by invited experts) Eur Heart J. 2012;33:1635–1701. doi: 10.1093/eurheartj/ehs092. [DOI] [PubMed] [Google Scholar]
- 4. Guallar-Castillon P, Magarinos-Losada MM, Montoto-Otero C, et al. Prevalence of depression and associated medical and psychosocial factors in elderly hospitalized patients with heart failure in Spain. Rev Esp Cardiol. 2006;59:770–778. [PubMed] [Google Scholar]
- 5. Rutledge T, Reis VA, Linke SE, et al. Depression in heart failure a meta-analytic review of prevalence, intervention effects, and associations with clinical outcomes. J Am Coll Cardiol. 2006;48:1527–1537. doi: 10.1016/j.jacc.2006.06.055. [DOI] [PubMed] [Google Scholar]
- 6. O'Connor CM, Jiang W, Kuchibhatla M, et al. Antidepressant use, depression, and survival in patients with heart failure. Arch Intern Med. 2008;168:2232–2237. doi: 10.1001/archinte.168.20.2232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kato N, Kinugawa K, Yao A, et al. Relationship of depressive symptoms with hospitalization and death in Japanese patients with heart failure. J Card Fail. 2009;15:912–919. doi: 10.1016/j.cardfail.2009.06.442. [DOI] [PubMed] [Google Scholar]
- 8. Cully JA, Johnson M, Moffett ML, et al. Depression and anxiety in ambulatory patients with heart failure. Psychosomatics. 2009;50:592–598. doi: 10.1176/appi.psy.50.6.592. [DOI] [PubMed] [Google Scholar]
- 9. Jenner RC, Strodl ES, Schweitzer RD. Anger and depression predict hospital use among chronic heart failure patients. Aust Health Rev. 2009;33:541–548. doi: 10.1071/ah090541. [DOI] [PubMed] [Google Scholar]
- 10. Jiang W, Kuchibhatla M, Cuffe MS, et al. Prognostic value of anxiety and depression in patients with chronic heart failure. Circulation. 2004;110:3452–3456. doi: 10.1161/01.CIR.0000148138.25157.F9. [DOI] [PubMed] [Google Scholar]
- 11. Rozanski A, Blumenthal JA, Kaplan J. Impact of psychological factors on the pathogenesis of cardiovascular disease and implications for therapy. Circulation. 1999;99:2192–2217. doi: 10.1161/01.cir.99.16.2192. [DOI] [PubMed] [Google Scholar]
- 12. Volz A, Schmid J-P, Zwahlen M, et al. Predictors of readmission and health related quality of life in patients with chronic heart failure: a comparison of different psychosocial aspects. J Behav Med. 2010;34:1–10. doi: 10.1007/s10865-010-9282-8. [DOI] [PubMed] [Google Scholar]
- 13. Moser DK, Worster PL. Effect of psychosocial factors on physiologic outcomes in patients with heart failure. J Cardiovasc Nurs. 2000;14:106–115. doi: 10.1097/00005082-200007000-00008. [DOI] [PubMed] [Google Scholar]
- 14. Konstam V, Salem D, Pouleur H, et al. Baseline quality of life as a predictor of mortality and hospitalization in 5,025 patients with congestive heart failure. Am J Cardiol. 1996;78:890–895. doi: 10.1016/s0002-9149(96)00463-8. [DOI] [PubMed] [Google Scholar]
- 15. Yancy CW, Jessup M, Bozkurt B, et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2013;128:e240–e327. doi: 10.1161/CIR.0b013e31829e8776. [DOI] [PubMed] [Google Scholar]
- 16. Beck AT, Ward CH, Mehdelson M, et al. An inventory for measuring depresssion. Arch Gen Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 17. Hisli N. Reliability and validity of Beck depression inventory among university students [in Turkish] Psikoloji Dergisi. 1989;7:3–13. [Google Scholar]
- 18. Hekimoglu L, Altun ZO, Kaya EZ, et al. Psychometric properties of the Turkish version of the 42 item Depression Anxiety Stress Scale (DASS-42) in a clinical sample. Int J Psychiatry Med. 2012;44:183–198. doi: 10.2190/PM.44.3.a. [DOI] [PubMed] [Google Scholar]
- 19. Beck AT, Epstein N, Brown G, et al. An inventory for measuring clinical anxiety: psychometric properties. J Consult Clin Psychol. 1988;56:893–897. doi: 10.1037//0022-006x.56.6.893. [DOI] [PubMed] [Google Scholar]
- 20. Jiang W, Kuchibhatla M, Clary GL, et al. Relationship between depressive symptoms and long-term mortality in patients with heart failure. Am Heart J. 2007;154:102–108. doi: 10.1016/j.ahj.2007.03.043. [DOI] [PubMed] [Google Scholar]
- 21. Konstam V, Moser DK, De Jong MJ. Depression and anxiety in heart failure. J Card Fail. 2005;11:455–463. doi: 10.1016/j.cardfail.2005.03.006. [DOI] [PubMed] [Google Scholar]
- 22. Sullivan M, Simon G, Spertus J, et al. Depression-related costs in heart failure care. Arch Intern Med. 2002;162:1860–1866. doi: 10.1001/archinte.162.16.1860. [DOI] [PubMed] [Google Scholar]
- 23. Faller H, Steinbuchel T, Störk S, et al. Impact of depression on quality of life assessment in heart failure. Int J Cardiol. 2010;142:133–137. doi: 10.1016/j.ijcard.2008.12.093. [DOI] [PubMed] [Google Scholar]
- 24. Cully JA, Jimenez DE, Ledoux TA, et al. Recognition and treatment of depression and anxiety symptoms in heart failure. Prim Care Companion J Clin Psychiatry. 2009;11:103–109. doi: 10.4088/pcc.08m00700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Brenes GA. Anxiety and chronic obstructive pulmonary disease: prevalence, impact, and treatment. Psychosom Med. 2003;65:963–970. doi: 10.1097/01.psy.0000097339.75789.81. [DOI] [PubMed] [Google Scholar]
- 26. Jiang W, Alexander J, Christopher E, et al. Relationship of depression to increased risk of mortality and rehospitalization in patients with congestive heart failure. Arch Intern Med. 2001;161:1849–1856. doi: 10.1001/archinte.161.15.1849. [DOI] [PubMed] [Google Scholar]
- 27. Kunik ME, Roundy K, Veazey C, et al. Surprisingly high prevalence of anxiety and depression in chronic breathing disorders. Chest. 2005;127:1205–1211. doi: 10.1378/chest.127.4.1205. [DOI] [PubMed] [Google Scholar]
- 28. MacMahon KM, Lip GY. Psychological factors in heart failure: a review of the literature. Arch Intern Med. 2002;162:509–516. doi: 10.1001/archinte.162.5.509. [DOI] [PubMed] [Google Scholar]
- 29. Serafini G, Pompili M, Innamorati M, et al. The impact of anxiety, depression, and suicidality on quality of life and functional status of patients with congestive heart failure and hypertension: an observational cross-sectional study. Prim Care Companion J Clin Psychiatry. 2010;12(6):pii:PCC.09m00916. doi: 10.4088/PCC.09m00916gry. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Sherwood A, Blumenthal JA, Trivedi R, et al. Relationship of depression to death or hospitalization in patients with heart failure. Arch Intern Med. 2007;167:367–373. doi: 10.1001/archinte.167.4.367. [DOI] [PubMed] [Google Scholar]
- 31. Gottlieb SS, Kop WJ, Ellis SJ, et al. Relation of depression to severity of illness in heart failure (from Heart Failure and a Controlled Trial Investigating Outcomes of Exercise Training [HF-ACTION]) Am J Cardiol. 2009;103:1285–1289. doi: 10.1016/j.amjcard.2009.01.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Azevedo A, Bettencourt P, Friões F, et al. Depressive symptoms and heart failure stages. Psychosomatics. 2008;49:42–48. doi: 10.1176/appi.psy.49.1.42. [DOI] [PubMed] [Google Scholar]
- 33. Moser DK. Psychosocial factors and their association with clinical outcomes in patients with heart failure: why clinicians do not seem to care. Eur J Cardiovasc Nurs. 2002;1:183–188. doi: 10.1016/S1474-5151(02)00033-6. [DOI] [PubMed] [Google Scholar]
- 34. Deepa R, Shanthirani CS, Pradeepa R, et al. Is the ‘rule of halves’ in hypertension still valid? — evidence from the Chennai Urban Population Study. J Assoc Physicians India. 2003;51:153–157. [PubMed] [Google Scholar]
- 35. Sadock BJ, Sadock VA. Kaplan & Sadock’s clinical psychiatry. Lippincott Williams & Wilkins; 2005. pp. s.211– s.246. [Google Scholar]
- 36.Şentürk A, Levent BA, Tamam L. The psychopathology in patients with chronic renal failure treated with hemodialysis. J Exp Clin Med. 2000;17:163–172. [Google Scholar]
- 37. Türkçapar H, Güriz O, Özel A, et al. Relationship between depression and anger in patients with antisocial personality disorder. Turkish J Psychiatry. 2004;15:119–124. [PubMed] [Google Scholar]


