Abstract
Cardiac pseudoaneurysm is an extremely rare condition in children. It can be congenital or acquired and has been primarily described in the left side of the heart. The congenital form of pseudoaneurysm is thought to be related to muscular dysplasia of the muscular layer of the heart. The acquired form is related to myocardial infarction, infective endocarditis or chest trauma. In this report we described a 5-month-old baby with left atrial pseudoaneurysm who was referred to our hospital due to tachycardia and hemodynamic instability. After diagnosis of left atrial pseudoaneurysm, aneurysmectomy was performed and the left atrial wall was successfully repaired by surgery three days after admission. In conclusion, due to life threatening complications such as dissection, arrhythmias, compression of aneurysm and tromboembolic complications, pseudoaneurysm should be treated by surgery.
Keywords: Chest trauma, Left atrial pseudoaneurysm, Supraventricular arrhythmias
INTRODUCTION
Cardiac pseudoaneurysm is an extremely rare condition in childhood. It can be congenital or acquired and has been mostly described in the left side of the heart.1,2 The congenital form of pseudoaneurysm is thought to be related to muscular dysplasia of the muscular layer.2 The acquired form is related to myocardial infarction, infective endocarditis or blunt chest trauma.3 In this report we described a 5-month-old baby with left atrial pseudoaneurysm who was referred to our hospital due to tachycardia and hemodynamic instability.
CASE REPORT
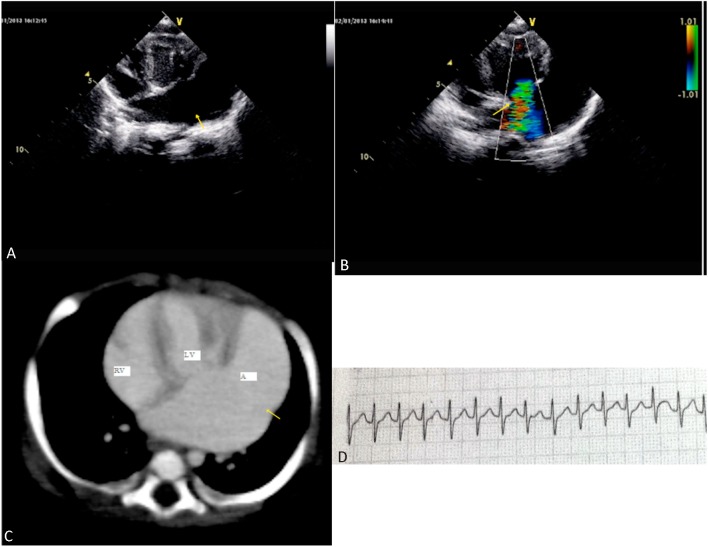
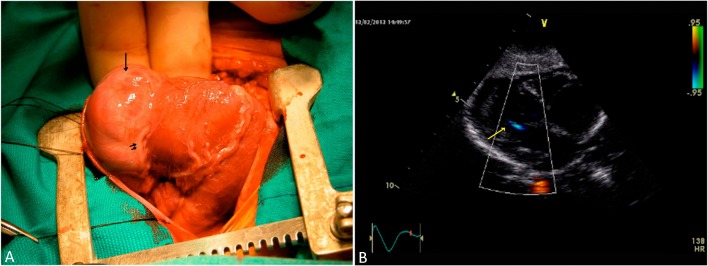
A 5-month-old baby was referred to our hospital due to tachycardia and hemodynamic instability. We learned from the patient’s history that the patient was dropped on the floor from a one-meter-high bed two months ago. The young patient became restless and pale, and refused oral ingestion one day prior to admission. We also learned that fetal echocardiography had been performed in our hospital and it was determined to be normal at the 24th week of gestation. Upon physical examination, the patient was unrestful, with a heart rate of 280 beats/min and blood pressure of 60/30 mmHg. Electrocardiography of the patient revealed supraventricular tachycardia with a heart rate 280 beats/min (Figure 1D). Supraventricular tachycardia persisted despite the intravenous adenosine administration with a repeated dose of 0.1 mg/kg and 0.2 mg/kg. Normal sinus rhythm was obtained following a cardioversion with the 0.5 J/kg. We did not perform echocardiography before cardioversion due to the fact that we learned the patient’s fetal echocardiograph was normal, and also that he was hemodynamically unstable and in bad condition. Echocardiographic examination after cardioversion showed a 4 cm aneurysm arising from the left atrium with a narrow neck, a left ventricular compression with aneurysm and a severe mitral insuffiency (Figure 1A and B). At first glance we considered an aneurysm of the left atrial appendage secondary to pericardial defect after the first echocardiographic examination. Multi-slice chest tomography showed intact pericardial tissue in addition to left atrial aneurysm (Figure 1C). During follow-up, short supraventricular tachycardia episodes were repeated and were brought under control with amiodarone infusion. Due to the huge left atrial aneurysm, left ventricular compression and arrhythmia, the patient was referred for surgical treatment. Intraoperative findings revealed an intact pericardium, and a huge left atrial pseudoaneurysm (Figure 2A). Consequently, aneurysmectomy was performed and the left atrial wall was succesfully repaired by surgery three days after admission. During surgery under cardiopulmonary bypass and cardioplegia, after the standard aortic and bicaval canullation, the left atrial pseudoaneurysm was opened. The circumflex artery was protected and psuedoaneurysm was closed with a 6/0 prolene suture. Biopsy was also taken from the pseudoaneurysm during surgery. The process of weaning from cardiopulmonary bypass was uncomplicated. Biopsy showed that there was no true atrial wall except the pericardial layer. During follow-up, there was no problem after surgery, amiodarone treatment was stopped and the patient was discharged one week after surgery. Postoperative echocardiographic examination showed good ventricular functions and trivial mitral insufficiency (Figure 2B).
Figure 1.
(A) Apical four-chamber view of echocardiography shows huge aneurysm arising from left atrium, (B) Apical four-chamber view of echocardiography shows 3rd degree mitral insufficiency due to aneurysm compression on to the left ventricle, (C) Multi-slice computed tomography shows huge aneurysm formation arising from left atrium (RV: right ventricle, LV: left ventricle, A: aneurysm), (D) Electrocardiography of patient shows supraventricular tachycardia (lead II).
Figure 2.
(A) Intraoperative appearance of aneurysm. Arrow shows aneurysm. Double short arrows shows circumflex artery, (B) Postoperative echocardiography shows mild mitral insufficiency.
DISCUSSION
Cardiac pseudoaneurysm is an extremely rare condition in children and mostly described in the left side of the heart. Its congenital form is thought to be related to muscular dysplasia of the muscular layer.1 The acquired form is related to myocardial infarction, infective endocarditis or blunt chest trauma.2,3 Fetal echocardiography of our patient in the 24th week of gestation was normal. We learned from the patient’s history that he was dropped down from one meter high onto his chest two months ago. During the blunt chest trauma or acceleration/deceleration type chest trauma, the heart compressed between the sternum and the wall of the chest can lead to incomplete myocardial rupture, organized thrombus and hematoma formation, and finally develop the pseudoanerysm. Contrary to a real aneurysm, there is no muscular layer in a pseudoaneurysm. Diagnosis of aneurysm can be easily accomplished by transthoracic, transesophageal echocardiography or 3D echocardiography; but to effectively differentiate from a pseudoaneursym, other imaging techniques such as magnetic resonance imaging (MRI) are required. Due to the absence of predisposing factors, they can be confused with pericardial cysts, left ventricular pseudoaneurysm, and congenital partial absence of pericardium. Three-dimensional echocardiography helps determine diagnosis as it shows the auricular appendage anatomy and its anatomic relationships, as does colour Doppler, which shows filling from the left atrium.
Cardiac MRI can differentiate pseudoaneurysm from the left atrial aneurysm related to pericardial defect.
Aneurysm or pseudoaneurysm arising from the left atrium or the left atrial appendage is a rare cause of atrial arrhythmia in childhood. In our patient, mitral insufficiency was related to compression of aneurysm and it disappeared after surgical treatment.4 Supraventricular arrhythmias may be early signs of left atrial aneurysm or pseudoaneurysm. Wagshal et al. described a case involving incessant atrial tachycardia related to atrial appendage aneurysm. In our patient, supraventricular tachycardia is related to interaction between the left ventricular myocardium and the aneurysm wall.5 Evaluating patients with echocardiography prior to cardioversion can prevent thromboembolic complications in patients with prolonged arrhythmias and related cardiac aneurysm/pseudoaneurysms. In our patient, we did not perform echocardiography before cardioversion because we learned that the patient’s fetal echocardiograph was normal, and also that the patient was hemodynamically unstable and in bad condition.
In conclusion, cardiac pseudoaneurysm is a rare condition and commonly seen during infective endocarditis, after cardiac ischemia, trauma or surgery. Additionally, left atrial pseudoaneurysm related to chest trauma is an extremely rare condition in children and young adults. Therefore, dissection, arrhythmias, compression of aneurysm and thromboembolic complications of pseudoaneurysm, should be considered early surgical treatment.
REFERENCES
- 1. Chowdhury UK, Seth S, Govindappa R, et al. Congenital left atrial appendage aneurysm: a case report and brief review of literature. Heart Lung Circ. 2009;18:412–416. doi: 10.1016/j.hlc.2008.10.015. [DOI] [PubMed] [Google Scholar]
- 2. Wilson D, Kalra N, Brody EA, et al. Left atrial appendage aneurysm - a rare anomaly with an atypical presentation. Congenit Heart Dis. 2009;4:489–493. doi: 10.1111/j.1747-0803.2009.00319.x. [DOI] [PubMed] [Google Scholar]
- 3. Darchis J, de Laguerenne N, Auffray JL, et al. Septic pseudo-aneurysm of the left main trunk in a dialysis patient. Eur J Echocardiogr. 2008;9:334–335. doi: 10.1093/ejechocard/jen012. [DOI] [PubMed] [Google Scholar]
- 4. Lee YH, Hou CJ, Hung CL, Tsai CH. Silent and huge left ventricular pseudoaneurysm with left atrial compression: dedicated spatial resolution and geometry by 3-dimensonal echocardiography. J Am Soc Echocardiogr. 2007;20:772.e5-9. doi: 10.1016/j.echo.2006.12.007. [DOI] [PubMed] [Google Scholar]
- 5. Wagshal AB, Applebaum A, Crystal P, et al. Atrial tachycardia as the presenting sign of a left atrial appendage aneurysm. Pacing Clin Electrophysiol. 2000;23:283–285. doi: 10.1111/j.1540-8159.2000.tb00815.x. [DOI] [PubMed] [Google Scholar]