Summary
Background
Granulosa cell tumours of the ovary are rare, hormonally active, oestrogen-secreting tumours of the ovary existing in two forms: the adult form and the even rarer juvenile form. These tumours present as predominantly solid lesions while the cystic, unilocular presentation is uncommon.
Case Report
We present an 18-year-old unmarried girl who presented with complaints of chronic pain, abdominal distension and presence of facial hair. Radiological examination revealed a large, purely cystic, unilocular lesion without any solid components, debris or septations. Histopathological diagnosis was of a juvenile granulosa cell tumour.
Conclusions
Radiological criteria suggestive of malignant ovarian masses include thick, irregular walls and septae; papillary projections and solid, echogenic foci. Nonetheless, we propose that a malignant ovarian lesion should be included in the differential diagnosis of a unilocular, purely cystic ovarian lesion.
MeSH Keywords: Granulosa Cell Tumor, Ovarian Cysts, Ovarian Neoplasms
Background
Granulosa cell tumours of the ovary are unique, hormonally active, oestrogen-secreting tumours accounting for 1 to 2% of all the ovarian malignancies [1–3]. These are rare tumours with an overall incidence varying from 0.4 to 1.7 cases per 100,000 women [3]. The juvenile form of granulosa cell tumours (5% of the cases) is even rarer as compared to its adult counterpart (remaining 95% of the cases); and usually presenting as predominantly solid mass lesions. We hereby report an unusual case of juvenile granulosa cell tumour presenting as a large, unilocular purely cystic lesion.
Case Report
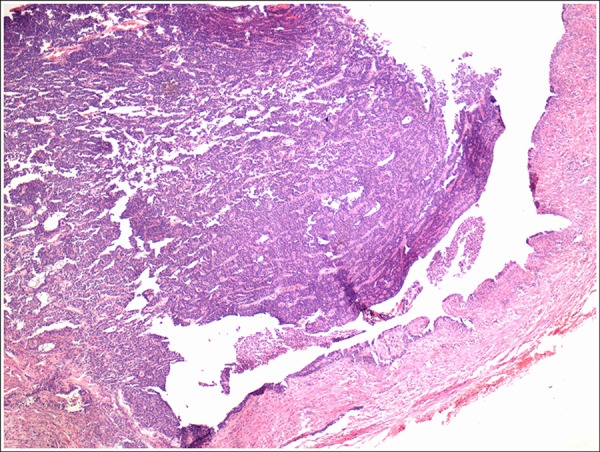
An 18-year-old unmarried girl presented with complaints of chronic pain and distension of the abdomen for the last 2 months and presence of facial hair for 1 year. Her per abdominal examination revealed a large mass, cystic in consistency, most likely arising from the pelvis and reaching up to the xiphisternum. The erect abdominal radiograph revealed a large mass occupying almost the entire abdominal cavity and displacing the bowel loops superiorly (Figure 1). The ultrasound findings suggested a large anechoeic cystic lesion with posterior acoustic enhancement arising from the pelvis. Remainder of the abdomen was normal. There was no obvious evidence of internal echoes or septations within the lesion (Figure 2). Subsequently, a computed tomogram of the abdomen and pelvis was advised which showed a large 85×110×125 cm (AP×TR×CC) lesion of fluid consistency arising from the pelvis (Figure 3). No enhancing soft tissue or septae were noted within the lesion and the left ovary could not be visualised separately from the lesion. Based on imaging features, a diagnosis of a large left ovarian cyst of benign etiology was given. Hormonal analysis was done in our case. The estradiol levels were elevated to 450 pg/mL (reference range 15–350 pg/mL). Preoperative CA-125 and beta-HCG were within the normal reference range. After preoperative investigations, the patient underwent left ovarian cystectomy. A large left ovarian cyst was excised. The cyst wall revealed a few intervening solid areas (Figure 4). Histopathological examination of the solid cell nests showed round to oval cells with moderately pleomorphic nuclei, prominent nucleoli and scanty cytoplasm (Figure 5). Many nuclei showed irregular nuclear margins and a few showed grooves. Call-Exner bodies were noted (Figure 6). A diagnosis of Granulosa cell tumour was thus established.
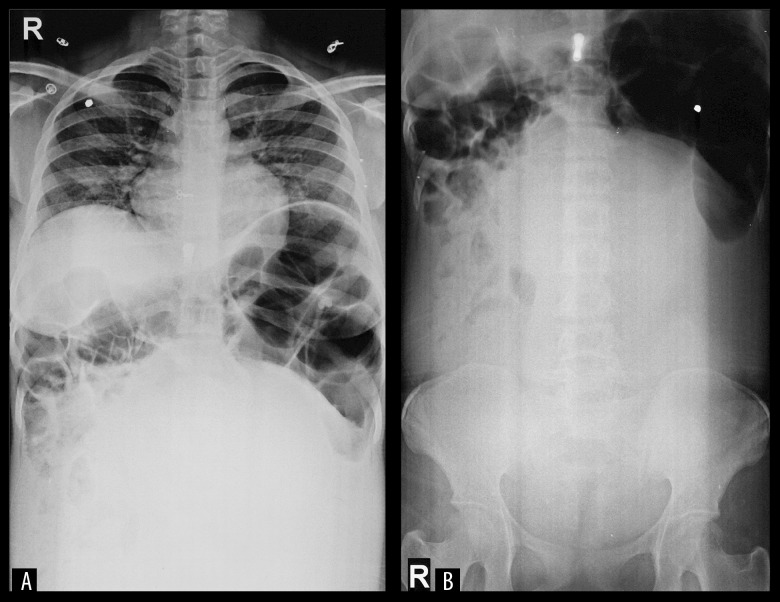
Figure 1.
Plain radiograph of the chest (A) and abdomen (B) reveals a large lesion occupying almost the entire abdominal cavity and pelvis with superior displacement of the bowel loops due to mass effect.
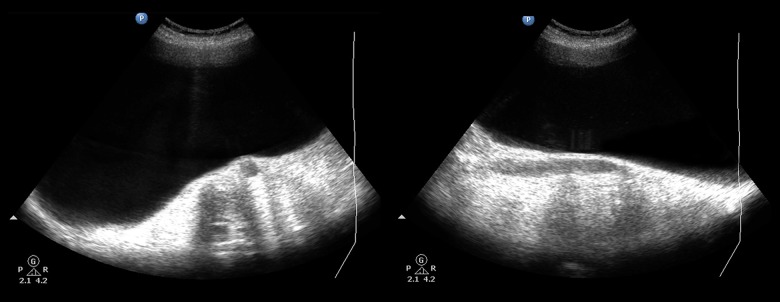
Figure 2.
Ultrasonography revealed a completely anechoeic lesion suggestive of a purely cystic consistency. Note the absence of sepatae or soft tissue component within the lesion.
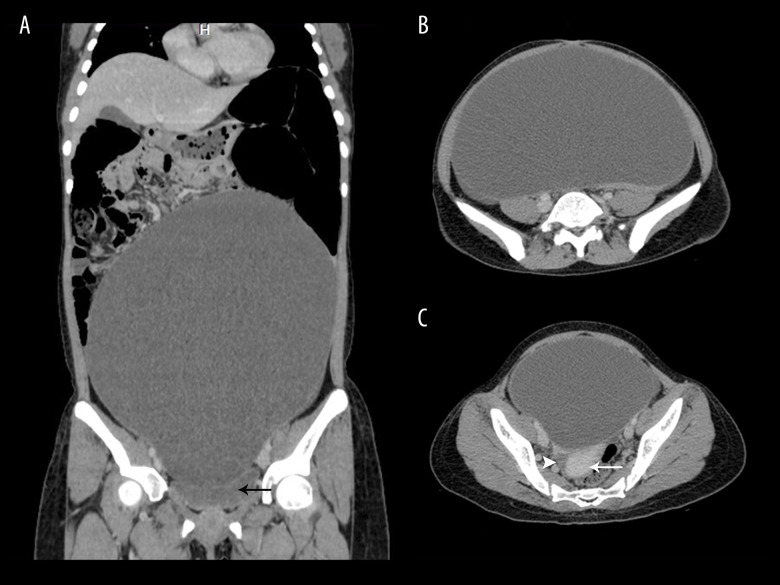
Figure 3.
Contrast-enhanced computed tomography of the abdomen and pelvis, in coronal reformatted (A) and axial (B, C) sections reveal a large, unilocular, purely cystic lesion arising from the pelvis and occupying almost the entire abdominal cavity. Note the absence of enhancing soft tissue or septae within the lesion. Also note the urinary bladder (black arrow), uterus (white arrow) and right ovary (white arrowhead). The left ovary could not be visualised separately from the lesion implying left ovarian origin of the cystic lesion.
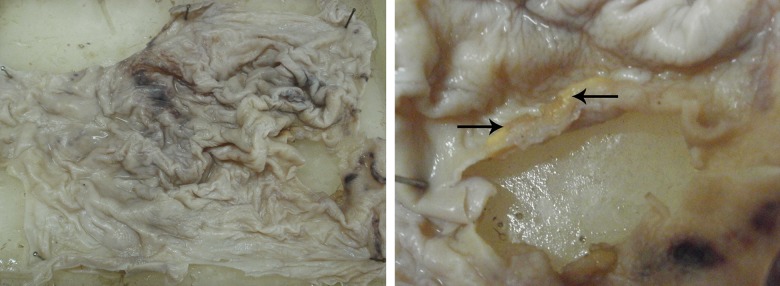
Figure 4.
Gross pathological specimen showing cut surface of the ovarian cystic wall. Note the intervening solid areas (black arrows).
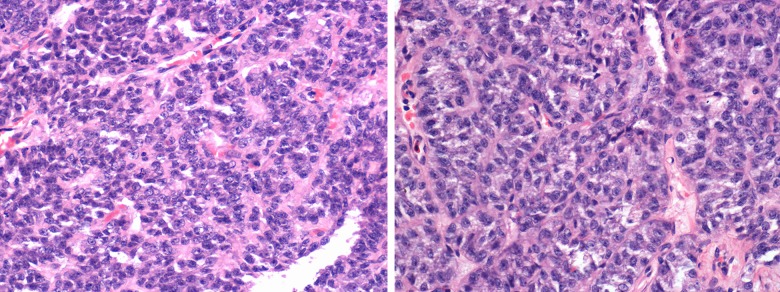
Figure 5.
Photomicrograph, hematoxylin and eosin stained section (×40) shows the cyst lined by cuboidal to columnar epithelium resting on the thick fibrous wall. At places it shows multi-layering of the lining epithelium.
Figure 6.
Photomicrograph, hematoxylin and eosin stained section (×100) through the solid nests of the cyst wall shows round to oval cells with moderately pleomorphic nuclei, prominent nucleoli and scanty cytoplasm. Many nuclei show irregular nuclear margins and a few show grooves. Call-Exner bodies are seen.
Discussion
Ovarian malignancies stand as a leading cause of gynaecological cancer death accounting for around 6% of all cancers diagnosed in females [4]. Based on the cell of origin, ovarian malignancies are classified as epithelial, germ cell and sex cord-stromal tumours. The latter may contain granulosal cells, thecal cells or Sertoli cells. Granulosa cell tumours are subdivided into two types – the adult type (AGCT – 95% of cases) and juvenile type (JGCT – 5% of cases) [1–5]. The mere subclassification into the two types is not based on age alone as either form may occur in any age group. Two thirds of the adult variety occur in post-menopausal women with a peak incidence between 50 and 55 years [6] and less than 1% of AGCT occur in prepuberscent girls [2], while more than a half of the cases of the juvenile form have been reported in the “less than 10 years” age group [2]. Our case was thus unusual since our case of JGCT presented with symptoms at a marginally later age of 18 years.
Around 70% [2] of GCTs secrete estrogen responsible for clinical evidence of precocious puberty in cases of JGCT, while the hyperestrogenic state in the AGCT variety is responsible for endometrial hyperplasia, endometrial carcinoma [6] and abnormal uterine bleeding. Overall however, abdominal mass, distension and pain are the commonest symptoms of GCTs [5–7]. This finding was consistent with our index case as well; whose chief complaints were abdominal pain and distension. On retrospective evaluation, our patient did not have any signs of precocious puberty; however, she did complain of features of virilization which was consistent with the hormonally active tumour.
Unlike its adult counterpart, the juvenile form is considered to be relatively benign with excellent survival rates reaching as high as 97% [2] while the chances of recurrence are higher in the AGCT [7]. Histologically, unlike the AGCT, fewer Call-Exner bodies are seen in JGCT, visualised as grooved, pale, round nucei – the classic feature of GCT. Morphologically and radiologically it is not possible to differentiate between the two varieties. Thus, both clinical and histopathological guidelines are needed to correctly subcategorize granulosa cell tumours into the two types and age cannot be considered the definitive criterion.
Granulosa cell tumours generally present as solid masses with varying amounts of haemorrhage and necrosis responsible for the cystic components. Pure cystic presentation, as in our index case, has been reported very rarely [8–10]. Radiological criteria suggestive of malignant ovarian masses include thick, irregular walls and septae; papillary projections and solid, echogenic foci [11]. None of these criteria were seen in our case. Nonetheless, we propose that a malignant ovarian lesion should be included in the differential diagnosis of a unilocular, purely cystic ovarian lesion.
Conclusions
Radiological criteria suggestive of malignant ovarian masses include thick, irregular walls and septae; papillary projections and solid, echogenic foci. Nonetheless, we propose that a malignant ovarian lesion should be included in the differential diagnosis of a unilocular, purely cystic ovarian lesion.
References
- 1.Ashnagar A, Alavi S, Nilipour Y, et al. Massive ascites as the only sign of ovarian juvenile granulosa cell tumor in an adolescent: a case report and a review of the literature. Case Rep Oncol Med. 2013;2013:386725. doi: 10.1155/2013/386725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kanthan R, Senger J-L, Kanthan S. The multifaceted granulosa cell tumours-myths and realities: a review. ISRN Obstet Gynecol. 2012;2012:878635. doi: 10.5402/2012/878635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Calcaterra V, Nakib G, Pelizzo G, et al. Central precocious puberty and granulosa cell ovarian tumor in an 8-year old female. Pediatr Rep. 2013;5(3):e13. doi: 10.4081/pr.2013.e13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Long JR, Danielson D. Juvenile granulosa cell tumor of the ovary. Applied Radiology. 2008;1:44–48. [Google Scholar]
- 5.Kwon SH. A clinicopathologic study of ovarian granulosa cell tumor. J Women’s Med. 2010;3(1):12–17. [Google Scholar]
- 6.Ukah CO, Ikpeze OC, Eleje GU, Eke AC. Adult granulosa cell tumor associated with endometrial carcinoma: A case report. J Med Case Rep. 2011;5:340. doi: 10.1186/1752-1947-5-340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rusterholz KR, MacDonald W. An unusual case of juvenile granulosa cell tumor of the ovary. Radiology Case Reports. 2009;4:178. doi: 10.2484/rcr.v4i1.178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Choi CH, Pritchard JR. Large cystic granulosa cell tumor: case report. Am J Obstet Gynecol. 1990;163:74–76. doi: 10.1016/s0002-9378(11)90671-1. [DOI] [PubMed] [Google Scholar]
- 9.Nomelini RS, Micheletti AMR, Adad SJ, Murta EFC. Androgenic juvenile granulosa cell tumor of the ovary with cystic presentation: a case report. Eur J Gynaecol Oncol. 2007;28:236–38. [PubMed] [Google Scholar]
- 10.Mulvany NJ, Riley CB. Granulosa cell tumors of unilocular cystic type. Pathology. 1997;29:348–53. doi: 10.1080/00313029700169295. [DOI] [PubMed] [Google Scholar]
- 11.Jeong YY, Outwater EK, Kang HK. Imaging evaluation of ovarian masses. Radiographics. 2000;20:1445–70. doi: 10.1148/radiographics.20.5.g00se101445. [DOI] [PubMed] [Google Scholar]