Abstract
Background:
Tuberculosis (TB) is a global public health crisis. 25% of world’s TB cases are found in India. Ayurveda, an ancient medical science may offer some solution to this problem. Hence, a systematic review was carried out to assess the role of Ayurveda for the management of TB.
Methodology:
A systematic review was carried out using published literature obtained through “PubMed” until April 2015. The key words used for literature search include “Ayurveda, role and TB.”
Results and Discussion:
It was observed that a couple of single and compound drugs have been used for the management of TB. However, none of the studies could reflect the true anti-TB activities of any drug, both single and compound. Two of the studies revealed in vitro anti-TB properties of some herbs which can potentially be brought into the realm of a clinical trial to test their efficacy in a human subject. Most of these Ayurvedic therapeutic preparations studied in different clinical settings primarily reflected their adjunct properties for the management of TB. These studies revealed that Ayurvedic therapeutics was able to reduce associated symptoms and the adverse drug effects of ATDs (anti-TB drugs). Furthermore, some of the preparations showed potential hepato-protective properties that can be simultaneously administered with ATDs.
Conclusion:
Distressingly research on the role of Ayurveda in the management of TB is very scanty and mostly limited to adjunct or supportive therapy. Being a global public health crisis, it is highly recommended to carry out clinical trials on TB patients using Ayurvedic drugs and therapeutic regimens.
KEY WORDS: Adjunct therapy, Ayurveda, Herbal Drugs, Rajayakshma, Tuberculosis
INTRODUCTION
Tuberculosis (TB) is an infectious disease caused by Mycobacterium tuberculosis or the other members of Mycobacterium complex such as Mycobacterium africanum and Mycobacterium bovis, known to affect the humans. Since the times immemorial, it has affected many civilizations around the world and has been a major reason for many death tolls during the earlier days. It remains as the number one killer infectious disease among the adult population in developing countries even today. The WHO’s 1990 global disease burden report ranked TB in the seventh position and expected to continue the same until 2020 in terms of morbidity [1]. It is a global public health crisis. In India, TB continues to be a devastating health crisis with more than 3, 00,000 deaths, 2.2 million new cases with an economic loss of $23bn (£14.9bn; €20.3bn) each year [2]. In spite of noticeable progress achieved TB always offers newer challenges such multidrug-resistant TB (MDR-TB), extensively drug-resistant TB (XDR-TB) along with debilitating side effects of anti-TB drugs. In India, TB in the community is managed by a centrally sponsored TB control program known as Revised National TB Control Programme (RNTCP). The main target of this program is 85% cure rate and 70% case detection rate. Since 2007, India has achieved this global target of cure rate and case detection rate. Furthermore, RNTCP has 100% coverage rate under DOTS. Although India has achieved the global targets but the problem does not end there owing to a multiplicity of problems [3]. Despite being a centrally sponsored program and free treatment and diagnostic services people still visit private practitioners at their first point of contact when a symptom arises. Studies report that around 50-80% of the patients visit private practitioners for TB treatment [4]. Currently, Ayurvedic drugs are not a part of RNTCP. However, private practitioners use various types of Ayurvedic medicines, both general practitioners and chest physicians, to support TB management [5]. This ancient medical science can offer some solutions to these problems hence a systematic review was carried out to assess the role of Ayurveda for the management of TB.
Ayurvedic Concept of Pulmonary TB (PTB)
PTB is aptly compared with Rajayakshma in Ayurveda. Rajayakshma is primarily attributable to Dhatukshaya (tissue emaciation or loss). This process universally initiates the process of pathogenesis in Rajayakshma patients. In addition, there is inevitable metabolic dysfunction (Dhatwagninasana), in which rasa (tissue fluid), rakta (blood), mamsa (muscle), meda (adipose tissue), and sukra (generative tissue) are lost. This leads to ultimate deterioration of immunity or ojokshaya. As per Ayurvedic concepts, an unusual metabolic change occur leading to loss of various dhatus (tissue) such as Ojokshaya, sukra, meda dhatus to rasa dhatu preceding each other, which is known as Pratilomakshaya [6].
METHODOLOGY
A systematic search strategy was adopted using “PubMed (US National Library of Medicine, USA)” for the main search process. The key words used for the purpose of PUBMED search include “Ayurveda, role and TB.” No limits were adopted such as; journals, years of publication, language, types of articles, or authors, but the articles published in English language only were included for the purpose of review. This was done purposefully to obtain a comprehensive list of articles published until April 2015 without the above-mentioned limits. In the second stage, the total articles obtained from searching the database using the above search criteria was pooled together, and articles were initially screened by reading the “title” and thereafter the “abstracts.” Studies not satisfying the inclusion criteria were excluded at these stages. The remaining articles were screened in the final stage by reading the full-text and those not meeting inclusion criteria were excluded. The Figure 1 gives an idea about the flow of information through different phases of this systematic review as per Preferred Reporting Items for Systematic review and Mata Analysis (PRISMA) guidelines (http://www.prisma-statement.org/).
Figure 1.
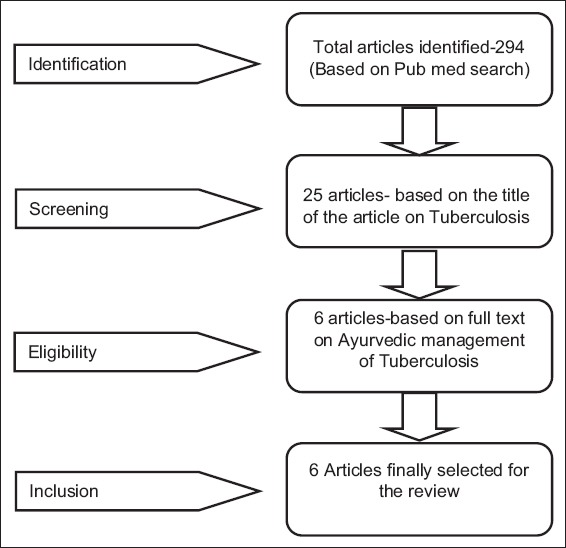
Flow of information through different phases of this systematic review (As per PRISMA guidelines)
RESULTS
In this section, the results are mentioned in two phases. In the first phase studies related to the Ayurvedic management of TB as an adjunct therapy are delineated and in the next part the studies related to Ayurvedic drugs showing in-vitro anti-TB properties are described.
Ayurvedic Management of TB (Adjunct and Supportive)
Four different studies conducted in different clinical settings in India evaluated the properties of some of the Ayurvedic therapeutics as adjunct to anti-TB treatment. Table 1 summarizes the properties of some of the Ayurvedic therapeutics as adjunct to anti-TB drugs. Vyas et al. conducted a single blind controlled trial to evaluate the adjunct properties of Rasayana compound among 133 TB patients receiving “Cat-1” therapy under RNTCP. The Rasayana used in this study is composed of Amalaki (Emblica officinalis Gaertn.)-Pericarp, 1 part, Guduchi (Tinospora cordifolia willd.)-Stem, 1 part, Ashwagandha (Withania somnifera L.)-Root, 1 part, Yashtimadhu (Glycyrrhiza glabra Linn.)-Root, 1 part, Pippali (Piper longum Linn.)-Fruit, ½ parts, Sariva (Hemidesmus indicus R.Br.)-Root, ½ Parts, Kustha (Saussurea lappa Falc.)-Root, ½ parts, Haridra (Curcuma longa Linn.)-Rhizome, ½ parts and Kulinjan (Alpinia galangal Linn.)-Rhizome, ¼ parts and administered in capsule form. They conducted the study at OPD level at three different hospitals; (1) Institute of Post Graduate Training and Research in Ayurveda (IPGT and RA), Hospital, Gujarat Ayurveda University, Jamnagar, (2) District TB Centre and Hospital, Jamnagar, and (3) Guru Govind Singh Hospital, P. N. Marg, Jamnagar. The study was carried out for 60 days, and the capsule was administered at a dose of 450 mg. Only sputum smear-positive patients from Category I of PTB or extra PTB and age group of >13 years were selected for the study, rest excluded from the study. The study found that the compound is helpful in alleviating the associated symptoms of PTB in the treatment group (TG) compared to the control group (CG). The results were statistically significant (P < 0.001). The Rasayana compound was found to decrease cough (83%), fever (93%), dyspnea (71.3%), hemoptysis (87%), and increase body weight (7.7%) [7]
Table 1.
Ayurvedic management of TB as an adjunct therapy

Dornala and Dornala conducted a study to evaluate the clinical efficacy of Bhringarajasava as Naimittika Rasayana in PTB. The study was conducted at the Out Patient Department (OPD) of the State TB Training and Demonstration Centre, S.R. Nagar, Hyderabad, Andhra Pradesh, India among 60 PTB patients who were already under directly observed treatment short course (DOTS). Each patient was administered 30 ml of Bhringarajasava with an equal quantity of water, ½ an hour after food, thrice a day during the intensive phase of treatment, and followed up to 6-8 months based on treatment category. Bhringarajasava is a liquid formulation composed of Bhringaraja (Eclipta prostrate Linn.), as active ingredient along with Haritaki (Terminalia chebula Retz.), Pippali (Piper longum Linn.), Jatiphala (Myristica fragrance Houtt.), Lavanga (Sygizium aromaticum Linn.), Twak (Cinnamomum zeylanicum), Ela (Elatteria cardamomum), Tamalapatra (Cinnamomum tamala), Nagakesara (Messua ferrea), and Gudam (old cane jaggery). The investigators evaluated the role of Bhringarajasava in 15 subjective parameters and 3 objective parameters. The role of this formulation on these subjective parameters is as follows; the improvement is mentioned in both TG and in CG; Amsaparsabhitapah (pain in costal and scapular region) - 35% in CG and 100% in TG, Samtapakarapadayoh (burning sensation in palms and Soles) - 50% in CG and 75% in TG and complete relief in Cat-III, patients, Jwara (Pyrexia) - <75% in CG and 100% in TG, Bhaktadwesha (Anorexia)-mild in CG and complete in TG, Swasa (Dyspnea) - <65% in CG and >90% in TG, Kasa (Cough) - moderate relief in CG and progressive relief, later occasional-nonproductive and easy expectoration in TG after 15 days of treatment, Shonita darshanam (Hemoptysis) - the relief is not statistically significant among CG and were given another drug but encouraged results were observed in TG, Swarabheda (Hoarseness of voice) - the relief is not statistically significant among CG but encouraged results were observed in TG, Anilath shula (pain in visceral organs) - complete relief in TG, Sankochamsaparshyoh (shoulder and scapular emaciation) - very encouraging in TG patients over the CG, Daha (burning sensation) - complete relief in TG, Atisara (Diarrhea) - no manifestation among TG, Pittaraktasyachagama (Hematemesis) - manifested in 2 patients and controlled immediately, Sirasaha paripoonata (Heaviness in the head) - relieved in 10 days among TG and in CG after 3-4 months, Kantadwamsa (Tracheal shift) - observed only in one case with fibrosed and consolidated lung. The role in objective parameters is as follows; Wight loss-in CG there was further weight loss but in TG there was no weight loss and is statistically significant, Sputum Conversion-sputum conversion was found among TG after intensive phase but in CG 10 patients out of 30 again put on intensive phase, Skiagram (chest X-ray [CXR]) - Density of the opacity in the CXR was less than on previous studies, with lessening of the cavities and resolution of fibrotic changes noted in the TG patients [8].
Debnath et al. conducted a study to assess the use of adjunct therapy of Ayurvedic medicine with anti-tubercular drugs in the therapeutic management of PTB. It primarily aimed to evaluate the toxicity reduction and early restoration by adjunct therapy of Ayurvedic drugs by increasing the bioavailability of ATDs. The study was conducted among 99 newly diagnosed PTB patients from both the sexes aged between 10 and 65 years. The subjects were administered 500 mg of Ashwagandha -2 caps, twice daily and Chyawanprash (as per Indian Pharmacopeia)-10 g, thrice daily for a period of 28 days. The study reported amelioration of symptoms, improvement of body weight, normalization of erythrocyte sedimentation rate, appreciable change in IgA and IgM patterns, and significant increase in bioavailability of isoniazid and pyrazinamide. Bioavailability of isoniazid and pyrazinamide showed 7-10% increased value after 28 days of treatment [9].
Sharma et al. conducted a study to assess the hepato-protective properties of Ayurvedic herbs among patients receiving anti-TB treatment. The study was conducted among three groups of subjects, each with 10 subjects aged 15-70 years, for a period of 90 days with normal liver Anatomy and Physiology confirmed by ultrasonography and biochemical analysis at the time of the investigation. Group-1 received capsule Liv-600, thrice a day composed of 200 mg of hydro alcoholic extract of Berberis aristata, Solanum nigrum, and Aloe vera, Group-2 received freshly prepared decoction of Bhumyamalaki (Phyllanthus fraternus) prepared from 10 g of aerial plant, and the Group-3 received 600 mg of starch powder as placebo. To evaluate, the hepato-protective efficacies of the above drugs the investigators used subjective and objective parameters such as liver function test including serum bilirubin, alanine transaminase (ALT), aspartate aminotransferase (AST), and alkaline phosphatase. No significant elevation in AST and ALT were observed in TG compared to CG, whereas no significant elevation was observed for serum total bilirubin and alkaline phosphatase in both TG and CG [10].
In vitro Drug Trials for Anti-TB Activities
Two studies reported in vitro anti-TB properties of some Ayurvedic herbs. Table 2 summarizes the in vitro anti-TB properties of some of the Ayurvedic Herbs. Komal Kumar et al. conducted a study to evaluate the in vitro anti-TB properties of the leaves of five legumes. These include Kingiodendron pinnatum Rox. Hams., Humboldtia brunonis Wall., Indigofera cassioides Rottl. ex DC, Derris scandens Benth., and Ceasalpinia mimosoides Lamk. Non-polar and polar solvent extracts of leaves of these medicinal legumes were tested against M. TB H37RV, and minimum inhibitory concentrations (MICs) were determined by the agar-based proportion assay. Isoniazid was used as positive control to evaluate the anti-TB activity of the crude extracts of medicinal legumes. Except I. cassioides methanol extracts of the leaves of all the five legumes completely inhibited the growth of M. TB at the concentration of 50 µg/ml. Ethyl acetate extract of two legume leaves, K. pinnatum and D. scandens and chloroform extract of three legume leaves of H. brunonis, C. mimosoides, and D. scandens showed anti-TB activity. However, petroleum ether extract of only I. cassioides showed the activity, similarly, the methanol extract of only H. brunonis leaves showed the activity [11]. Gupta et al. conducted a study to evaluate in vitro anti-TB activity of five medicinal plants viz., Acalypha indica, Adhatoda vasica, Allium cepa, Allium sativum, and Aloe vera. Aqueous extracts of leaves of A. indica, A. vasica, bulbs of A. cepa, cloves of A. sativum, and pure gel of A. vera leaves, were tested in vitro. Percentage inhibition was used to evaluate the activity in L-J (Lowenstein-Jensen) medium which was calculated by mean reduction in a number of colonies on extract containing as compared to extract free controls. Extracts of all the five plants A. vasica, A. indica, A. cepa, A. vera, and A. sativum exhibited anti-TB activity in L-J medium, the proportion of inhibition of these plants extract in respect to that mentioned above is 95, 32, 37, 72, 32%, respectively, for MDR isolate DKU-156 and 68, 86, 79, 72, 85%, respectively, for another MDR isolate JAL-1236, while for sensitive M. TB H37Rv, inhibition was found to be 68, 70, 35, 63, and 41%, at 4% v/v concentration in L-J medium. There was no inhibition against rapid grower Mycobacterium fortuitum (TMC-1529). In BacT/ALERT also extracts of these plants showed significant inhibition against M. TB [12].
Table 2.
Ayurvedic drugs showing in-vitro anti-TB properties

DISCUSSION
It was observed that a couple of single drugs and compound drugs are useful for the management of TB. However, none of the studies could reflect the true anti-TB activities of any drug, both single and compound. Two studies revealed in vitro anti-TB properties of some herbs which can potentially be brought into the realm of a clinical trial to test their efficacy in a human subject. Most of these therapeutic preparations studied at different clinical set ups reflected their adjunct properties for the management of TB. These drugs were able to possibly reduce associated symptoms and the adverse drug effects of ATDs. Some of the preparations showed potential hepato-protective properties that can be used as adjunct to ATDs. The first study primarily focused on the use of a Rasayana drug as an Adjunct with the simultaneous administration of ATDs. It provided better physical and mental well-being to the patients by potentiating therapeutic efficacy of ATDs and also counteracting the unwanted effects caused by ATDs. Rasayana therapy has an anti-oxidant effect along with nutritive value, immune-modulator, immune-protective properties, and free radical scavenging property [7]. In the second study, the authors focused on the role of a Naimittika Rasayana, a unique concept used in chronic diseases described in Ayurveda. It promotes vigor and vitality and instills the ability to hold out disastrous outcomes of diseases as in the case of PTB which has similar untoward effects due to the disease itself and the effects of ATDs as well [13]. Most importantly, the second study delineated an objective parameter, “sputum conversion,” which creates some degree of skepticism. As the authors have mentioned that the TG got sputum conversion after the intensive phase which was not seen among some patients in CG poses a question, whether it is mere coincidence or the Rasayana has really some effect on M. TB. Similarly, the study conducted by Debnath et al. also reflected on the reduction of the bacterial load with the patients who were on adjunct therapy along with ATDs. This requires further investigation to establish and validate the fact. The Debnath et al. study reported a very significant finding of increased bioavailability of isoniazid and pyrazinamide, which is potentially a great hope in today’s situation of drug resistance. Furthermore, TB is associated with social determinants such as poor living condition, overcrowding, poor nutrition, and above all poverty. Again poverty leads to under nutrition, which itself is affected by both scarcity of food and intra-household distribution. A poor nutritional status also affects drug absorption, resulting in sub-therapeutic serum drug levels, which may lead to non-response to drug therapy [14]. Hence, supplementation of these drugs (Ashwagandha and Chyawanprash) along with first line ATDs could improve bioavailability and help in combating the problem of drug resistance and improve curability. Currently at the national level such initiatives are not a part of TB control program which can seriously be thought of looking at the current scenario of widespread drug resistance. Most importantly, in all the studies, the commonest improvement as a result of Ayurvedic intervention is gain in body weight, which is undoubtedly a cardinal improvement in the part of a PTB patient.
Furthermore, the hepatotoxic properties of ATDs are proved. Isoniazid causes liver damage owing to its reactive metabolites generated from Acetyle hydrazine. Rifampicin is an enzyme inducer and promotes the formation of reactive metabolites and thus hepatotoxic in the form of impairment of uptake of bilirubin and acute cellular necrosis [15]. Pyrazinamide has also potential to induce hepatocellular damage [16]. Hence, the adjunct intake of Liv-600 capsule and decoction of Bhumyamalaki could be extremely beneficial in combating hepatotoxicity as a consequence of administration of ATDs. In addition, in the post-trial analysis, it was observed that the effect of freshly prepared decoction of Bhumyamalaki is more effective than Liv-600 composed of three drugs. The activity is attributable to their anti-cholestatic action, reduction in free radical damage and cell protein necrosis as well [10]. Hence, freshly prepared decoction of Bhumyamalaki can be promoted, as a home remedy, at the community level as a hepato-protective agent with the co-administration of ATDS, which appears to be a cost-effective measure to combat hepatotoxicity of ATDs.
In addition to clinical trials, few herbal drugs showed potential anti-TB activities in vitro. The study conducted by Kumar et al. showed anti-TB properties of five different legumes. The leaf extracts of the legumes completely inhibited the growth of M. TB at MIC level of 50 µg/ml. This is acceptable as activity is considered significant if MIC values are below 100 µg/ml for crude extract and moderate when MIC is between 100 to 625 µg/ml [17,18]. The frontline anti-TB drugs have MICs in the range of 0.025-2.0 µg/ml and if the activity of any new entity is to be compared (compound/extract), its activity should also be in the same range. However, since extracts are crude preparations they may be considered active at higher concentrations also [11]. Gupta et al. conducted a study to evaluate the anti-TB properties of some herbs on two MDR M. TB isolates. In addition to some other first line and second line drugs, these MDR isolates were earlier found to be resistant to at least rifampicin and isoniazid. Hence, further studies should be carried out using various fractions of crude extracts of these plants as well as their semi-purified/purified principles responsible for anti-TB activity (specially for MDR and XDR isolates of M. TB) to find out the MIC in suitable broth based media as MICs defined in broth are more accurate [12]. Most importantly in vitro studies could be brought into the arena of the clinical trial to test their efficacy in human subjects in today’s situation of MDR and XDR TB.
Studies reveal that chest physicians are treating TB patients using few Ayurvedic preparations along with ATDs. The chest physicians are of the opinion that these medications act as immune modulators if given along with second line anti-TB drugs [5]. Furthermore, there is a growing interest in identifying the compounds responsible for the anti-mycobacterial activity of traditional medicine and developing them as potential TB drugs [19]. Many drugs of the Indian System of Medicine have come to the realm of national health programs for the management of common ailments, as in national health mission. Similarly, few drugs could also be brought into the same platform and be implemented in the national TB control program [20,21].
CONCLUSION
TB has been a major public health crisis for the developing world including India. Due to increase in MDR and XDR strains of M. TB, there is an urgent need to find newer solutions to combat this problem. Distressingly research on the role of Ayurveda in the management of TB is very scanty and mostly limited to adjunct or supportive therapy. However, the adjunct role of Ayurveda drugs cannot be simply neglected for not qualifying as agents to combat the M. TB rather their role as agents of increasing bioavailability of ATDs and counteracting the adverse drug interactions should be properly utilized. Being a global public health crisis and having the state of current drug resistance, it is highly recommended to carry out clinical trials on TB patients using Ayurvedic drugs and therapeutic regimens. The drugs those proved potent in combating the adverse drug reactions of both the first line and second line anti-TB drugs could be successfully added to the drug regimens of TB for better curability and to reduce drug resistance. Similarly, the drugs which showed potential anti-TB properties in vitro could also be useful in today’s world of drug resistance.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Murray CJ, Lopez AD. The global burden of disease: A comprehensive assessment of mortality and disability from diseases, injuries and risk factors in 1990 and projected to 2020: Summary. W 74 96GL-1/1996. Geneva, Switzerland: WHO; 1996. [Google Scholar]
- 2.Udwadia ZF. Tuberculosis in India: Ancient enemy just gets stronger. BMJ. 2015;350:h1080. doi: 10.1136/bmj.h1080. DOI: 10.1136/bmj.h1080. [DOI] [PubMed] [Google Scholar]
- 3.TBC India. Directorate General of Health Services, Ministry of Health and Family Welfare, Government of India. [Last accessed on 2015 Apr 15]. Available from: http://www.tbcindia.nic.in .
- 4.Uplekar M, Juvekar S, Morankar S, Rangan S, Nunn P. Tuberculosis patients and practitioners in private clinics in India. Int J Tuberc Lung Dis. 1998;2:324–9. [PubMed] [Google Scholar]
- 5.Dholakia Y, Quazi Z, Mistry N. Drug-resistant tuberculosis: Study of clinical practices of chest physicians, Maharashtra, India. Lung India. 2012;29:30–4. doi: 10.4103/0970-2113.92359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Charak A. In: Vidyatini Hindi Commentary, editors. Charak Samhita. Part I and II. Shastri K, Chaturvedi GN, editors. Varanasi: Chaukhamba Sanskrit Series; 1969. [Google Scholar]
- 7.Vyas P, Chandola HM, Ghanchi F, Ranthem S. Clinical evaluation of Rasayana compound as an adjuvant in the management of tuberculosis with anti-Koch’s treatment. Ayu. 2012;33:38–43. doi: 10.4103/0974-8520.100307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dornala SN, Dornala SS. Clinical efficacy of Bhringarajasava as Naimittika Rasayana in Rajayakshma with special reference to pulmonary tuberculosis. Ayu. 2012;33:523–9. doi: 10.4103/0974-8520.110536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Debnath PK, Chattopadhyay J, Mitra A, Adhikari A, Alam MS, Bandopadhyay SK, et al. Adjunct therapy of Ayurvedic medicine with anti tubercular drugs on the therapeutic management of pulmonary tuberculosis. J Ayurveda Integr Med. 2012;3:141–9. doi: 10.4103/0975-9476.100180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sharma YK, Singh H, Mehra BL. Hepatoprotective effects of few Ayurvedic herbs in patients receiving antituberculus treatment. Indian J Tradit Knowl. 2004;3:391–6. [Google Scholar]
- 11.Kumar JK, Devi Prasad AG, Chaturvedi V. Phytochemical screening of five medicinal legumes and their evaluation for in vitro anti-tubercular activity. Ayu. 2014;35:98–102. doi: 10.4103/0974-8520.141952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gupta R, Thakur B, Singh P, Singh HB, Sharma VD, Katoch VM, et al. Anti-tuberculosis activity of selected medicinal plants against multi-drug resistant Mycobacterium tuberculosis isolates. Indian J Med Res. 2010;131:809–13. [PubMed] [Google Scholar]
- 13.Singh RH. Rasāyanā and Vajikarana (promotive therapy) In: Sharma PV, editor. History of Medicine in India. New Delhi, India: Indian National Science Academy; 1992. pp. 242–54. [Google Scholar]
- 14.Byrd RP. Malnutrition and pulmonary tuberculosis. Clin Infect Dis. 2002;35:633–4. doi: 10.1086/342314. [DOI] [PubMed] [Google Scholar]
- 15.Askgaard DS, Wilcke T, Døssing M. Hepatotoxicity caused by the combined action of isoniazid and rifampicin. Thorax. 1995;50:213–4. doi: 10.1136/thx.50.2.213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Khanna BK. Hepatitis during INH, Pyrazinamide and rifampicin therapy. Indian J Tuberc. 1983;30:104. [Google Scholar]
- 17.Kuete V. Potential of Cameroonian plants and derived products against microbial infections: A review. Planta Med. 2010;76:1479–91. doi: 10.1055/s-0030-1250027. [DOI] [PubMed] [Google Scholar]
- 18.Kuete V, Efferth T. Cameroonian medicinal plants: Pharmacology and derived natural products. Front Pharmacol. 2010;1:123. doi: 10.3389/fphar.2010.00123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Trease GE, Evans WC. The Pharmacognosy. 11th ed. London: Brailliar Tiride Land Mac Millian Publishers; 1989. pp. 710–84. [Google Scholar]
- 20.Ministry of Health and Family Welfare. National Health System Resource Center-National Rural Health Mission, Mainstreaming of AYUSH and Revitalization of Local Health Traditions Under NRHM, An Appraisal of the Annual State Programme Implementation Plans 2007-2010 and Mapping of Technical Assistance Needs. New Delhi: Government of India; [Google Scholar]
- 21.Samal J. Role of AYUSH Workforces, Therapeutics and principles in health care delivery with special reference to National Rural Health Mission. Ayu. 2015;36:5–9. doi: 10.4103/0974-8520.169010. [DOI] [PMC free article] [PubMed] [Google Scholar]


