Abstract
Age-related macular degeneration (AMD) is the leading cause of irreversible blindness in elderly people worldwide. Cuticular drusen (CD) is a clinical subtype of AMD, which typically displays an earlier age at onset, and has a strong genetic component. Genetic studies support a role for rare sequence variants in CD susceptibility, and rare sequence variants in the CFH gene have been identified in 8.8% of CD cases. To further explore the role of rare variants in CD, we performed whole exome sequencing (WES) in 14 affected members of six families and 12 sporadic cases with CD. We detected rare sequence variants in CFH and FBLN5, which previously were shown to harbor rare variants in patients with CD. In addition, we detected heterozygous rare sequence variants in several genes encoding components of the extracellular matrix (ECM), including FBLN1, FBLN3/EFEMP1, FBLN5, FBLN6/HMCN1, FBN2, and COL15A1. Two rare pathogenic variants were identified in the COL15A1 gene: one in a sporadic case and another was found to segregate in a family with six affected individuals with CD. In addition, two rare pathogenic variants were identified in the FGL1 gene in three unrelated CD cases. These findings suggest that alterations in the ECM and in the coagulation pathway may play a role in the pathogenesis of CD. The identified candidate genes require further analyses in larger cohorts to confirm their role in the CD subtype of AMD. No evidence was found of rare sequence variants in a single gene that segregate with CD in the six families, suggesting that the disease is genetically heterogeneous.
Introduction
Age-related macular degeneration (AMD, OMIM 603075) is a leading cause of visual impairment and affects 8.7% of elderly people worldwide [1]. An early pathological symptom is the formation of drusen in the macula, the central region of the retina that is necessary for sharp and central vision. AMD is a clinically heterogeneous disorder that displays a broad spectrum of clinical appearances [2–5]. Cuticular drusen (CD, OMIM 126700) is a clinical subtype of AMD, characterized by the presence of at least 50 small (25–75μm) uniformly sized hyperfluorescent drusen, scattered primarily in the macular region on fluorescein angiography (FA) [6]. There is evidence that CD has a strong genetic component; CD often occurs in families and it presents clinically at an earlier age at onset than AMD [7,8]. Also, the most commonly associated environmental factor, smoking, shows a weaker association with CD than with the non-CD type AMD [9]. Genetic studies further support that CD has a strong genetic component by showing significant associations of CD with common variants (minor allele frequency [MAF] ≥ 1%) in the CFH (OMIM 134370), ARMS2 (OMIM 611313) C2 (OMIM 613927)/CFB (OMIM 138470), C3 (OMIM 120700), and APOE (OMIM 107741) genes [7,9]. Moreover, heterozygous mutations in CFH segregate in multiplex CD families [10,11] and a highly penetrant AMD risk variant, p.Arg1210Cys in CFH, was identified in two CD cases [12]. Furthermore, we recently demonstrated that 8.8% of CD cases harbor rare sequence variants (MAF ≤ 1%) in CFH [12]. This evidence supports a strong genetic component in CD, but additional genetic factors that contribute to CD susceptibility are yet to be discovered. Whole exome sequencing (WES) selectively sequences all protein-coding regions of the genome, known as the exome. Protein-coding regions are collectively approximately 30 megabases in size, spread across 180,000 exons that constitute 1% of the human genome [13], and are estimated to harbor 85% of disease-causing mutations [14]. Therefore, WES offers an unprecedented opportunity to study the role of rare sequence variants in protein-coding regions in complex diseases. In the present study, we sought to determine the role of rare sequence variants in CD using WES. We performed WES in 14 affected members of six families and 12 sporadic cases with CD. In addition, we conducted segregation analysis for rare sequence variants that were identified by WES, in affected individuals of six families.
Materials and Methods
Patients
We performed WES in 14 affected members of six families and 12 sporadic cases with the CD subtype of AMD (Figs 1 and 2). All study participants were selected from the European Genetic Database (EUGENDA) and are of Caucasian descent. All participants underwent extensive retinal examinations, which is described elsewhere in detail [12,15]. CD was diagnosed on the basis of the clinical observation of a symmetrically distributed pattern in both eyes of at least 50 scattered, uniformly-sized, small (25–75μm), and hyperfluorescent drusen on FA in each eye, and with a minimum of 20 drusen located outside the Wisconsin age-related maculopathy grading template [16,17]. The EUGENDA study was approved by the local research ethics committees (Commissie Mensgebonden Onderzoek Regio Arnhem-Nijmegen, the Netherlands, and Ethics Committee of the University Hospital Cologne, Germany). The study adhered to the ARVO statement for the use of human subjects in ophthalmic and vision research, and was performed in accordance with the tenets of the Declaration of Helsinki. Written informed consent was obtained from all participants. Peripheral blood samples were collected from all participants, and genomic DNA was isolated using the Chemagic STAR DNA Blood4k kit (PerkinElmer, Waltham, MA, USA).
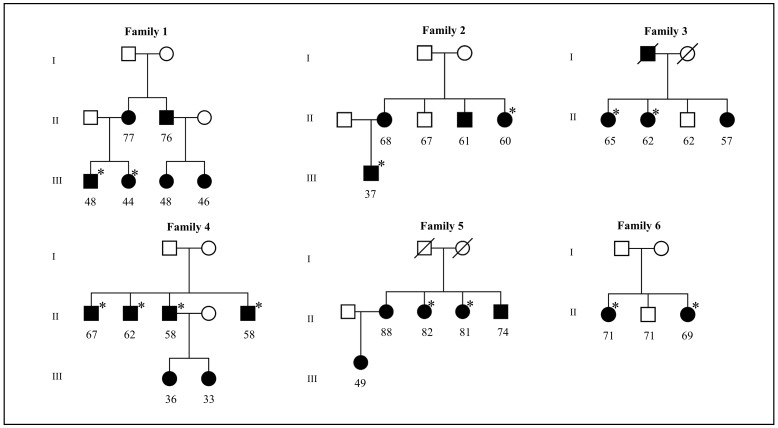
Fig 1. Pedigrees of six cuticular drusen (CD) families in which whole exome sequencing (WES) was performed.
Circle and square symbols indicate female and male individuals, respectively. Symbols with slashes indicate deceased individuals. Black and empty symbols indicate affected and unaffected individuals, respectively. Asterisks indicate the family members for whom exome sequencing was performed. The numbers below the symbols indicate the age at participation of family members.
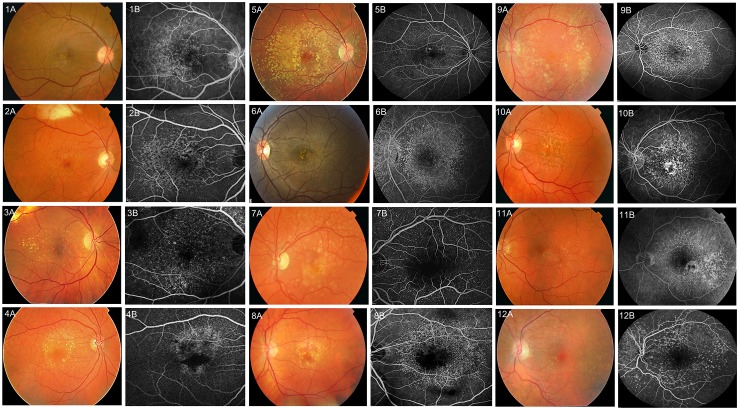
Fig 2. Retinal images of 12 sporadic cuticular drusen (CD) cases for whom exome sequencing (WES) was performed.
Panels A and B represent colour fundus photographs (1A-12A) and fluorescein angiograms (FAs) (1B-12B) of 12 cases respectively. For cases 1–5 retinal images of the right eye are shown, whereas for cases 6–12 retinal images of the left eye are shown. The CD phenotype presents with a large number of small and uniformly sized hyperfluorescent drusen on FA.
Whole exome sequencing
The exomes of all study participants were captured using the SureSelect Human All Exon kit version 2 (50Mb; Agilent Technologies, Santa Clara, CA, USA) using 3μg of genomic DNA. Subsequently, captured libraries were sequenced on SOLiD4 or 5500xl sequencing platforms (Life Technologies, Carlsbad, CA, USA). Reads were aligned to the reference human genome (NCBI hg19) with SOLiD LifeScope version 2.1 or SOLiD BioScope version 1.3 software (Life Technologies). Single nucleotide variants (SNVs) were called using the high-stringency DiBayes algorithm, and small insertions and deletions were detected using the SOLiD small Indel Tool (Life Technologies). The pathogenicity of missense variants were predicted in silico using Polymorphism Phenotyping version 2 (PolyPhen-2) and Sorting Intolerant from Tolerant (SIFT) tools.
The exomes were analyzed for variants in 289 candidate genes for CD and atypical hemolytic uremic syndrome (aHUS), because of their known allelic overlap [15,18,19]. The candidate genes were selected from known CD genes [5,7], known AMD loci [20], genes known to be involved in monogenic macular degeneration (Retnet), and genes encoding components of the complement system, coagulation system, innate immunity, endothelial cells, and the glomerular basement membrane (S1 Table) (Westra et al, in preparation). The exomes of the six families were also analyzed for variants in all genes of the exome that were shared among all affected individuals of all six families.
Sanger sequencing
Sanger sequencing was performed to validate rare sequence variants identified by WES. In families, confirmed rare sequence variants were analyzed for segregation by Sanger sequencing in available family members. Primers were designed with Primer3Plus software (Primer3Plus). PCR was performed, and amplification products were sequenced using an automated sequencer (BigDye Terminator, version 3, 3730 DNA analyzer; Applied Biosystems, Waltham, MA, USA). Sequencing chromatograms were compared to the reference sequence using ContigExpress (Vector NTI Advance, version 11.0, Life Technologies).
Results
Whole exome sequence analysis
WES was performed in 14 affected members of six families and 12 sporadic cases with the CD subtype of AMD. We detected an average of 34,784 sequence variants per exome, with an average coverage of 70-fold. We subsequently focused our analyses on 289 candidate genes (S1 Table) and detected an average of 780 sequence variants in these genes per sporadic case (S2 Table). In the six families, identically annotated sequence variants (referred to as overlapping variants) were selected that were found in all affected individuals of each family. An average of 508 overlapping variants were detected in these candidate genes per family (S2 Table). We next applied rigorous filtering criteria to identify rare, functionally relevant sequence variants in the candidate genes. The sequence variants were selected when they were present on 10 or more (≥10) variant reads, and when they were present in 20 percent or more (≥20%) of the variant reads. We then selected non-synonymous, coding insertion-deletions (indels), and splice acceptor and donor site variants in the candidate genes, and detected an average of 133 variants in each sporadic case, while on average 88 overlapping variants were detected in each family. Finally, we selected rare sequence variants with a minor allele frequency of ≤1% (MAF ≤0.01) in the 1000 Genomes project (1000 Genomes project) and the global MAF listing in the dbSNP database (dbSNP database). These filtering criteria resulted a total of 98 heterozygous rare sequence variants in 12 sporadic cases, with an average of eight rare sequence variants per sporadic case (S2 Table; S3–S14 Tables). A total of nine heterozygous overlapping variants were detected in four families, with an average of two variants in each family. In two families, no overlapping rare variants were identified (S2 Table).
Rare variants in sporadic CD cases
We first examined genes that have previously been described to carry rare variants in macular degeneration, for rare sequence variants in 12 sporadic CD cases. In eight sporadic cases, we detected eight heterozygous rare sequence variants in six macular degeneration genes (CFH; FBLN1, OMIM 135820; FBLN3/EFEMP1, OMIM 601548; FBLN5, OMIM 604580; HMCN1, OMIM 608548; FBN2, OMIM 612570) (Table 1). All rare sequence variants in the CFH (p.Ala173Gly; p.Gln950His/rs149474608), FBLN1 (p.His695Arg/rs13268), EFEMP1 (p.Asp49Ala/rs55849640), FBLN5 (p.Val126Met/rs61734479), HMCN1 (p.Lys2559Asn/rs139899015), and FBN2 (p.Pro326Ser/rs28763954; p.His1381Asn/rs78727187) genes were confirmed by Sanger sequencing. Five of these variants (p.Gln950His (CFH), p.His695Arg (FBLN1), p.Val126Met (FBLN5), p.Lys2559Asn (HMCN1), and p.His1381Asn (FBN2)) are predicted to be damaging by prediction tools SIFT and PolyPhen2. However, three variants (p.Ala173Gly (CFH), p.Asp49Ala (EFEMP1), and p.Pro326Ser (FBN2)) are predicted to be damaging by one of these prediction tools. Evolutionary conservation of altered bases were predicted using the Phylop program. The variants in the FBLN1, EFEMP1, FBLN5, HMCN1, and FBN2 genes are conserved, whereas the c.518C>G (p.Ala173Gly) and c.2850G>T (p.Gln950His) variants in the CFH gene are less conserved (Table 1).
Table 1. Rare missense variants identified in known macular degeneration genes in 12 sporadic CD subtype of AMD cases by WES.
| Gene | Change in | dbSNP | Prediction algorithms | Conservation | # Cases (Fig 2) | |||
|---|---|---|---|---|---|---|---|---|
| Nucleotide | Protein | ID | MAF (%) | SIFT | PolyPhen2 | Phylop (Base level) | ||
| CFH | c.518C>G | p.Ala173Gly | NA | 0 | Deleterious | Benign | 0.3 | 1 (3AB) |
| CFH | c.2850G>T | p.Gln950His | rs149474608 | 0.002 | Deleterious | Damaging | -0.7 | 1 (9AB) |
| FBLN1 | c.2084A>G | p.His695Arg | rs13268 | 0.007 | Deleterious | Damaging | 4.2 | 1 (2AB) |
| FBLN3/EFEMP1 | c.146T>G | p.Asp49Ala | rs55849640 | 0.0004 | Deleterious | Benign | 2.3 | 1 (12AB) |
| FBLN5 | c.376C>T | p.Val126Met | rs61734479 | 0.0008 | Deleterious | Damaging | 4.0 | 1 (10AB) |
| FBLN6/HMCN1 | c.7677G>C | p.Lys2559Asn | rs139899015 | 0 | Deleterious | Damaging | 1.2 | 1 (8AB) |
| FBN2 | c.976G>A | p.Pro326Ser | rs28763954 | 0.003 | Deleterious | Benign | 2.7 | 1 (9AB) |
| FBN2 | c.4141G>T | p.His1381Asn | rs78727187 | 0 | Deleterious | Damaging | 5.9 | 1 (7AB) |
CD, cuticular drusen; AMD, age-related macular degeneration; WES, whole exome sequencing; MAF, minor allele frequency; SIFT, sorting intolerant from tolerant; PolyPhen2, polymorphism phenotyping; Phylop score (< 0, less conserved; 0, neutral; > 0 conserved; a large score indicates high conservation); NA, not applicable
We next sought for genes that were burdened recurrently with rare sequence variants in at least three sporadic cases. We detected two recurrent candidate genes (FGL1, OMIM 605776; COL15A1, OMIM 120325) that harbored rare sequence variants in a total of six sporadic cases (Table 2). Sanger sequencing confirmed variants in the FGL1 (p.Tyr140Phe/rs35431851; p.Trp256Leu/rs2653414), and COL15A1 (p.Phe851Leu/rs35901514) genes, while a variant in the COL15A1 (p.Lys1365Ile) gene was not confirmed by Sanger sequencing (S15 Table). Of the confirmed variants, a rare variant (FGL1, p.Trp256Leu/rs2653414) is detected recurrently in two sporadic cases. Two variants in FGL1 (p.Tyr140Phe; p.Trp256Leu) gene are predicted to be damaging by both SIFT and PolyPhen2. The variant in the COL15A1 gene (p.Phe851Leu) is predicted to be damaging by one of two algorithms. The Phylop program predicted that all three variants in the FGL1 and COL15A1 genes are evolutionarily conserved (Table 2).
Table 2. Recurrent missense variants identified in two of 289 candidate genes in 12 sporadic CD subtype of AMD cases by WES.
| Gene | Change in | dbSNP | Prediction algorithms | Conservation | # Cases (Fig 2) | |||
|---|---|---|---|---|---|---|---|---|
| Nucleotide | Protein | ID | MAF (%) | SIFT | PolyPhen2 | Phylop (Base level) | ||
| FGL1 | c.419T>A | p.Tyr140Phe | rs35431851 | 0.007 | Deleterious | Damaging | 4.6 | 1 (11AB) |
| FGL1 | c.767C>A | p.Trp256Leu | rs2653414 | 0.009 | Deleterious | Damaging | 5.1 | 2 (4AB; 6AB) |
| COL15A1 | c.2551T>C | p.Phe851Leu | rs35901514 | 0.003 | Tolerated | Damaging | 2.8 | 1 (2AB) |
CD, cuticular drusen; AMD, age-related macular degeneration; WES, whole exome sequencing; MAF, minor allele frequency; SIFT, sorting intolerant from tolerant; PolyPhen2, polymorphism phenotyping; Phylop score (< 0, less conserved; 0, neutral; > 0 conserved; a large score indicates high conservation)
Rare variants in CD families
We detected four heterozygous overlapping rare sequence variants in four candidate genes (TFPI, OMIM 152310; TLR1, OMIM, 601194; COL15A1; C1QBP, OMIM 601269) in affected members of family 1 (Table 3). Family 3 harbored three heterozygous overlapping rare sequence variants in three candidate genes (DDR1, OMIM 600408; VWF, OMIM 613160; SLC12A3, OMIM 600968) (Table 3). Families 2 and 6 harbored one heterozygous overlapping rare variant in one candidate gene each (Family 2: ADAMTS20, OMIM 611681; Family 6: ITGA1, OMIM 192968), but both variants were not confirmed by Sanger sequencing (S15 Table). No overlapping rare sequence variants were detected in candidate genes in affected members of families 4 and 5 (S2 Table).
Table 3. Overlapping rare sequence variants identified in seven of 289 candidate genes in affected members of CD families by WES.
| Gene | Change in | dbSNP | Prediction algorithms | Conservation | Family number | |||
|---|---|---|---|---|---|---|---|---|
| Nucleotide | Protein | ID | MAF (%) | SIFT | PolyPhen2 | Phylop (Base level) | ||
| TFPI | c.874G>A | p.Val292Met | rs5940 | 0.008 | Deleterious | Damaging | 0.5 | 1 |
| TLR1 | c.1138C>T | p.Gln380* | NA | 0 | NA | NA | 1.3 | 1 |
| COL15A1 | c.2114C>T | p.Pro705Leu | rs41308900 | 0.007 | Deleterious | Damaging | 1.9 | 1 |
| C1QBP | c.389C>T | p.Thr130Met | rs56014026 | 0.007 | Tolerated | Damaging | 3.4 | 1 |
| DDR1 | c.1093A>T | p.Ile365Phe | rs143367160 | 0.003 | Deleterious | Benign | 1.6 | 3 |
| VWF | c.2771C>T | p.Arg924Gln | rs33978901 | 0.007 | Tolerated | Benign | 1.4 | 3 |
| SLC12A3 | c.2883+1 G>T | Splice-donor | rs199974259 | 0 | NA | NA | 5.2 | 3 |
CD, cuticular drusen; WES, whole exome sequencing; MAF, minor allele frequency; SIFT, sorting intolerant from tolerant; PolyPhen2, polymorphism phenotyping; Phylop score (< 0, less conserved; 0, neutral; > 0 conserved; a large score indicates high conservation); NA, not applicable
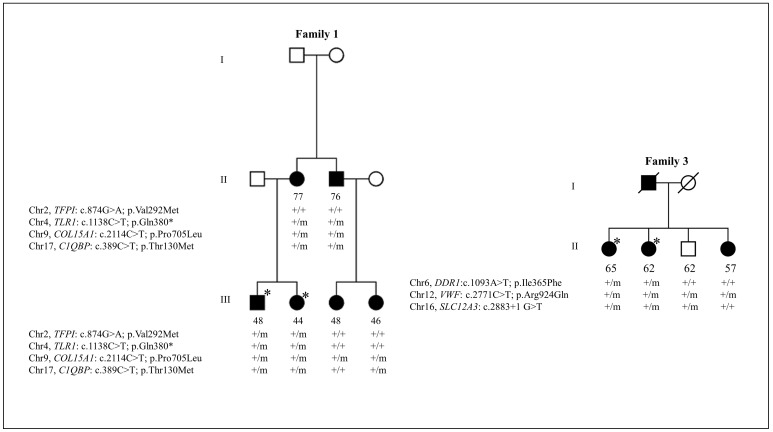
In family 1, all overlapping rare sequence variants (p.Val292Met/rs5940, TFPI; p.Gln380*, TLR1; p.Pro705Leu/rs41308900, COL15A1; p.Thr130Met/rs56014026, C1QBP) in candidate genes were confirmed by Sanger sequencing (Table 3). Two variants, p.Val292Met (TFPI) and p.Pro705Leu (COL15A1), are predicted to be damaging by both SIFT and PolyPhen2, while a variant p.Thr130Met (C1QBP) is predicted to be damaging by one of two algorithms. Evolutionary conservation suggested that variants in the TFPI, TLR1, COL15A1, and C1QBP genes are conserved. We next checked for segregation of all confirmed variants with CD in the additional members of family 1 by Sanger sequencing. Variant p.Pro705Leu in the COL15A1 gene segregated heterozygously with CD in this family, although unaffected family members above age 60 were not available in this family. All other variants were not present in one or two affected members of a family, and thus did not segregate with CD in family 1 (Fig 3).
Fig 3. Segregation analysis of rare sequence variants identified in candidate genes in cuticular drusen (CD) families by whole exome sequencing (WES).
Circles, females; squares, males; empty symbols, unaffected; black symbols, affected; asterisks, exome sequenced individuals; ‘+’ symbol, wild type allele; ‘m’ symbol, mutant type allele. The age at participation is specified below the symbols.
Family 3 harbored three overlapping rare sequence variants (p.Ile365Phe/rs143367160, DDR1; p.Arg924Gln/rs33978901, VWF; c.2883+1G>T/rs199974259, SLC12A3), which were all confirmed by Sanger sequencing. Variant p.Ile365Phe in the DDR1 gene is predicted to be damaging by one of two prediction algorithms, while the p.Arg924Gln variant in the VWF gene is predicted not to be damaging by both SIFT and PolyPhen2 prediction algorithms. All three variants are evolutionarily conserved. These variants subsequently were analyzed for segregation with CD in two additional family members of family 3. Variant p.Ile365Phe in the DDR1 gene did not show segregation, as it was not present in an affected member of the family. The splice donor variant, c.2883+1G>T, in the SLC12A3 gene also did not segregate, as it was found to be present in an unaffected member and was not present in an affected member of the family. The missense variant p.Arg924Gln in the VWF gene is present in three affected members and one unaffected member of the family (Fig 3).
The exomes of the six families were also analyzed for variants in all genes of the exome that were shared among all affected individuals of all six families. We filtered the exome data for rare non-synonymous, coding indels, and splice acceptor and donor site variants with a MAF ≤1% in dbSNP and in our in-house exome database. These filtering criteria did not identify any rare sequence variants in a single gene that segregate with CD in the six families.
Discussion
In the present study, we found rare sequence variants in two genes which previously were shown to harbor rare variants in CD (CFH and FBLN5) [5,11]. In addition, we found heterozygous rare sequence variants (MAF ≤0.01) in several extracellular matrix (ECM) genes, which include FBLN1, FBLN3/EFEMP1, FBLN5, FBLN6/HMCN1, FBN2, and COL15A1, in sporadic cases and families with the CD subtype of AMD by WES (Tables 1 and 2). Two rare pathogenic variants were identified in the COL15A1 gene: one in a sporadic case and another was found to segregate in a family with six affected individuals with CD. In addition, two rare pathogenic variants were identified in the FGL1 gene in three unrelated CD cases.
Variants in the CFH gene are major risk factors for both AMD and CD [10,11,19]. In this study, we identified two missense variants (p.Ala173Gly and p.Gln950His) that were previously identified by Sanger sequencing of the CFH gene in the same patients of the CD subtype of AMD phenotype [12].
The fibulins are ECM proteins that are characterized by tandem arrays of epidermal growth factor (EGF)—like domains, and are widely expressed in basement membranes. A previous study suggests that a single mutation (p.Arg345Trp) in the last EGF domain of FBLN3/EFEMP1 gene causes Doyne honeycomb retinal dystrophy (DHRD; OMIM 126600) [21]. We identified an evolutionarily conserved rare sequence variant (p.Asp49Ala) in the first EGF domain of FBLN3/EFEMP1 gene in a sporadic CD patient. This suggests that variants in the FBLN3/EFEMP1 gene may represent risk factors for the CD phenotype. We also identified a missense variant (p.Val126Met) in the FBLN5 gene, which was previously reported in the Dutch population (AMD cases 1/291; controls 5/91), suggesting that this variant is not rare in the Dutch population [22]. Therefore, the p.Val126Met variant in the FBLN5 gene may not be a causal variant for CD. However, missense variants in the FBLN5 gene have previously been associated with AMD (P < 0.01) and the retinal images of patients showed a peculiar CD phenotype, which suggests that other variants in the FBLN5 gene are a risk factor for both the AMD and CD phenotypes [5,22].
The ECM is an acellular component that provides physical and biochemical support for surrounding cells in all tissues and organs, and constantly undergoes remodeling processes which are indispensible for tissue architecture [23]. A pathological symptom of AMD phenotypes is the formation of drusen between the retinal pigment epithelium (RPE) and Bruch’s membrane (BrM), which is a multilayered ECM structure. The BrM is composed of central elastin fibers sandwiched between layers of collagen [24,25]. The BrM acts as a blood-retinal barrier that regulates the diffusion of nutrients and oxygen from the choroid through the BrM to the RPE, while the metabolic waste diffuses in an opposite direction to the choroid [26]. Several lines of evidence suggest that ageing processes (thickening, calcification, degeneration of collagens and elastic fibers) and alterations in the structural components in the BrM result in loss of normal function of the BrM [27], which may result in accumulation of drusen deposits in AMD patients. Emerging evidence suggests that alterations in specific genes encoding ECM proteins (TIMP3, CTRP5, FBN2, and FBLN 1–6) are implicated in macular degeneration [5,21,28–30]. Recent genome-wide association studies have also identified risk variants in several ECM genes (COL8A1, COL10A1, ADAMTS9, DDR1, TGFBR1, HTRA1, and TIMP3) [20].
The present study identified two evolutionarily conserved rare sequence variants (p.Pro705Leu and p.Phe851Leu) in COL15A1 in 6 affected members of a family and in a sporadic CD patient, respectively. The p.Pro705Leu variant is predicted to be deleterious by both prediction algorithms, while the p.Phe851Leu variant is predicted to be deleterious by one of two prediction algorithms. These prediction algorithms provide a quick functional annotation of variants, but experimental validation is required to properly access the functional consequences of these variants. The COL15A1 gene encodes collagen, type XV, alpha 1, which is widely expressed in basement membranes [31], and in choroidal endothelial cells [32]. Since the choroid plays a vital role in maintenance of BrM, variants in the COL15A1 gene might lead to altered properties of the choroid and/or of BrM, resulting in the formation of drusen in patients with CD.
In this study we also identified two highly conserved rare sequence variants in the FGL1 gene in three of 12 sporadic CD cases (Table 2). Both variants are predicted to be deleterious to the normal function of the protein by prediction algorithms. Fibrinogen and fibrinogen-like protein 1 (FGL1) belong to the fibrinogen superfamily. Fibrinogen is a precursor of fibrin clot formation of the coagulation cascade [33,34]. A proteomic study demonstrated that FGL1 is bound to the fibrin matrix during clot formation, suggesting that FGL1 is involved in the coagulation cascade [35,36]. Interestingly, the molecular composition of drusen consist of fibrinogen as one of several constituents [37]. This suggests that FGL1 variants may be causative in CD, although it is unclear on how the coagulation cascade and variants in FGL1 gene may be implicated in AMD phenotypes.
We found no segregating rare variants among affected members of four of the six CD families in the 289 candidate genes. In all protein-coding regions of the genome, we also found no evidence of rare sequence variants in a single gene that segregate with CD in all families, providing evidence for genetic heterogeneity in the pathogenesis of CD. Alternatively, the disease risk in some individuals of these families may be attributable to a combination of common genetic and environmental factors, and as a consequence rare variants may not completely segregate in these families. In a recent study we identified a clustering of known risk factors in affected members of families with AMD, suggesting that such families may not be explained by rare genetic variants. However, some families cannot be explained by known risk factors, and are more likely to carry rare, highly penetrant variants [38]. Some affected family members in the CD families examined in this study might thus have CD due to the presence of known risk factors, and not merely by rare sequence variants. Therefore, WES based segregation analyses may not always be the best strategy to solve AMD or CD families. However, other studies have successfully identified rare sequence variants in AMD families by WES, e.g. in the CFH and FBN2 genes [28,39].
In summary, WES in sporadic cases and families with the CD subtype of AMD identified rare variants in known CD genes and several genes encoding ECM components. Rare pathogenic variants were recurrently identified in the COL15A1 and FGL1 genes. These findings suggest that alterations in the ECM and in the coagulation pathway may play a role in the pathogenesis of CD. These candidate genes require further analyses in larger cohorts to confirm their involvement in the CD subtype of AMD. No evidence was found of rare sequence variants in a single gene that segregate with CD in the six families, suggesting that the disease is genetically heterogeneous.
Supporting Information
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
Acknowledgments
Sequencing (Sanger and whole-exome sequencing) was performed at the Genome Technology Center, Department of Human Genetics, Radboud University Medical Centre, Nijmegen, the Netherlands.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This study was supported by the Netherlands Organization for Scientific Research (Vidi Innovational Research Award 016.096.309) and the Foundation Fighting Blindness USA (grant C-GE-0811-0548-RAD04). The research leading to these results has received funding from the European Research Council under the European Union's Seventh Framework Programme (FP/2007-2013) / ERC grant agreement n. 310644 (MACULA).
References
- 1.Wong WL, Su X, Li X, Cheung CM, Klein R, Cheng CY, et al. (2014) Global prevalence of age-related macular degeneration and disease burden projection for 2020 and 2040: a systematic review and meta-analysis. Lancet Glob Health 2: e106–116. 10.1016/S2214-109X(13)70145-1 [DOI] [PubMed] [Google Scholar]
- 2.Bird AC, Bressler NM, Bressler SB, Chisholm IH, Coscas G, Davis MD, et al. (1995) An international classification and grading system for age-related maculopathy and age-related macular degeneration. The International ARM Epidemiological Study Group. Surv Ophthalmol 39: 367–374. [DOI] [PubMed] [Google Scholar]
- 3.Swaroop A, Chew EY, Rickman CB, Abecasis GR (2009) Unraveling a multifactorial late-onset disease: from genetic susceptibility to disease mechanisms for age-related macular degeneration. Annu Rev Genomics Hum Genet 10: 19–43. 10.1146/annurev.genom.9.081307.164350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Malek G, Cousins SW (2006) Is our current clinical classification of AMD up to the job? Br J Ophthalmol 90: 1080–1081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stone EM, Braun TA, Russell SR, Kuehn MH, Lotery AJ, Moore PA, et al. (2004) Missense variations in the fibulin 5 gene and age-related macular degeneration. N Engl J Med 351: 346–353. [DOI] [PubMed] [Google Scholar]
- 6.Boon CJF, van de Ven JPH, Hoyng CB, den Hollander AI, Klevering BJ (2013) Cuticular drusen: stars in the sky. Prog Retin Eye Res 37: 90–113. 10.1016/j.preteyeres.2013.08.003 [DOI] [PubMed] [Google Scholar]
- 7.Grassi MA, Folk JC, Scheetz TE, Taylor CM, Sheffield VC, Stone EM (2007) Complement factor H polymorphism p.Tyr402His and cuticular Drusen. Arch Ophthalmol 125: 93–97. [DOI] [PubMed] [Google Scholar]
- 8.Saksens NT, Kersten E, Groenewoud JM, van Grinsven MJ, van de Ven JPH, Sanchez CI, et al. (2014) Clinical characteristics of familial and sporadic age-related macular degeneration: differences and similarities. Invest Ophthalmol Vis Sci 55: 7085–7092. 10.1167/iovs.14-14659 [DOI] [PubMed] [Google Scholar]
- 9.van de Ven JPH, Smailhodzic D, Boon CJF, Fauser S, Groenewoud JM, Chong NV, et al. (2012) Association analysis of genetic and environmental risk factors in the cuticular drusen subtype of age-related macular degeneration. Mol Vis 18:2271–2278. [PMC free article] [PubMed] [Google Scholar]
- 10.van de Ven JPH, Boon CJF, Fauser S, Hoefsloot LH, Smailhodzic D, Schoenmaker-Koller F, et al. (2012) Clinical evaluation of 3 families with basal laminar drusen caused by novel mutations in the complement factor H gene. Arch Ophthalmol 130: 1038–1047. [DOI] [PubMed] [Google Scholar]
- 11.Boon CJF, Klevering BJ, Hoyng CB, Zonneveld-Vrieling MN, Nabuurs SB, Blokland E, et al. (2008) Basal laminar drusen caused by compound heterozygous variants in the CFH gene. Am J Hum Genet 82: 516–523. 10.1016/j.ajhg.2007.11.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Duvvari MR, Saksens NT, van de Ven JPH, de Jong-Hesse Y, Schick T, Nillesen WM, et al. (2015) Analysis of rare variants in the CFH gene in patients with the cuticular drusen subtype of age-related macular degeneration. Mol Vis 21: 285–292. [PMC free article] [PubMed] [Google Scholar]
- 13.Ng SB, Turner EH, Robertson PD, Flygare SD, Bigham AW, Lee C, et al. (2009) Targeted capture and massively parallel sequencing of 12 human exomes. Nature 461: 272–276. 10.1038/nature08250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Choi M, Scholl UI, Ji W, Liu T, Tikhonova IR, Zumbo P, et al. (2009) Genetic diagnosis by whole exome capture and massively parallel DNA sequencing. Proc Natl Acad Sci U S A 106: 19096–19101. 10.1073/pnas.0910672106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Duvvari MR, Paun CC, Buitendijk GH, Saksens NT, Volokhina EB, Ristau T, et al. (2014) Analysis of rare variants in the c3 gene in patients with age-related macular degeneration. PLoS One 9: e94165 10.1371/journal.pone.0094165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.van de Ven JPH, Boon CJF, Smailhodzic D, Lechanteur YTE, den Hollander AI, Hoyng CB, et al. (2012) Short-term changes of Basal laminar drusen on spectral-domain optical coherence tomography. Am J Ophthalmol 154: 560–567. 10.1016/j.ajo.2012.03.012 [DOI] [PubMed] [Google Scholar]
- 17.Klein R, Davis MD, Magli YL, Segal P, Klein BE, Hubbard L (1991) The Wisconsin age-related maculopathy grading system. Ophthalmology 98: 1128–1134. [DOI] [PubMed] [Google Scholar]
- 18.van de Ven JPH, Nilsson SC, Tan PL, Buitendijk GH, Ristau T, Mohlin FC, et al. (2013) A functional variant in the CFI gene confers a high risk of age-related macular degeneration. Nat Genet 45: 813–817. 10.1038/ng.2640 [DOI] [PubMed] [Google Scholar]
- 19.Raychaudhuri S, Iartchouk O, Chin K, Tan PL, Tai AK, Ripke S, et al. (2011) A rare penetrant mutation in CFH confers high risk of age-related macular degeneration. Nat Genet 43: 1232–1236. 10.1038/ng.976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fritsche LG, Chen W, Schu M, Yaspan BL, Yu Y, Thorleifsson G, et al. (2013) Seven new loci associated with age-related macular degeneration. Nat Genet 45: 433–432. 10.1038/ng.2578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stone EM, Lotery AJ, Munier FL, Heon E, Piguet B, Guymer RH, et al. (1999) A single EFEMP1 mutation associated with both Malattia Leventinese and Doyne honeycomb retinal dystrophy. Nat Genet 22: 199–202. [DOI] [PubMed] [Google Scholar]
- 22.Lotery AJ, Baas D, Ridley C, Jones RP, Klaver CC, et al. (2006) Reduced secretion of fibulin 5 in age-related macular degeneration and cutis laxa. Hum Mutat 27: 568–574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Frantz C, Stewart KM, Weaver VM (2010) The extracellular matrix at a glance. J Cell Sci 123: 4195–4200. 10.1242/jcs.023820 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zarbin MA (2004) Current concepts in the pathogenesis of age-related macular degeneration. Arch Ophthalmol 122: 598–614. [DOI] [PubMed] [Google Scholar]
- 25.Nita M, Strzalka-Mrozik B, Grzybowski A, Mazurek U, Romaniuk W (2014) Age-related macular degeneration and changes in the extracellular matrix. Med Sci Monit 20: 1003–1016. 10.12659/MSM.889887 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sivaprasad S, Bailey TA, Chong VN (2005) Bruch's membrane and the vascular intima: is there a common basis for age-related changes and disease? Clin Experiment Ophthalmol 33: 518–523. [DOI] [PubMed] [Google Scholar]
- 27.Chong NH, Keonin J, Luthert PJ, Frennesson CI, Weingeist DM, Wolf RL, et al. (2005) Decreased thickness and integrity of the macular elastic layer of Bruch's membrane correspond to the distribution of lesions associated with age-related macular degeneration. Am J Pathol 166: 241–251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ratnapriya R, Zhan X, Fariss RN, Branham KE, Zipprer D, Chakarova CF, et al. (2014) Rare and common variants in extracellular matrix gene Fibrillin 2 (FBN2) are associated with macular degeneration. Hum Mol Genet. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Weber BH, Vogt G, Pruett RC, Stohr H, Felbor U (1994) Mutations in the tissue inhibitor of metalloproteinases-3 (TIMP3) in patients with Sorsby's fundus dystrophy. Nat Genet 8: 352–356. [DOI] [PubMed] [Google Scholar]
- 30.Hayward C, Shu X, Cideciyan AV, Lennon A, Barran P, Zareparsi S, et al. (2003) Mutation in a short-chain collagen gene, CTRP5, results in extracellular deposit formation in late-onset retinal degeneration: a genetic model for age-related macular degeneration. Hum Mol Genet 12: 2657–2667. [DOI] [PubMed] [Google Scholar]
- 31.Li D, Clark CC, Myers JC (2000) Basement membrane zone type XV collagen is a disulfide-bonded chondroitin sulfate proteoglycan in human tissues and cultured cells. J Biol Chem 275: 22339–22347. [DOI] [PubMed] [Google Scholar]
- 32.Booij JC (2010) Function and pathology of the human retinal pigment epithelium. Thesis avialable: http://hdl.handle.net/11245/2.78270. Accessed 2015.
- 33.Mullins RF, Russell SR, Anderson DH, Hageman GS (2000) Drusen associated with aging and age-related macular degeneration contain proteins common to extracellular deposits associated with atherosclerosis, elastosis, amyloidosis, and dense deposit disease. Faseb j 14: 835–846. [PubMed] [Google Scholar]
- 34.Crabb JW, Miyagi M, Gu X, Shadrach K, West KA, Sakaguchi H, et al. (2002) Drusen proteome analysis: an approach to the etiology of age-related macular degeneration. Proc Natl Acad Sci U S A 99: 14682–14687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rijken DC, Dirkx SP, Luider TM, Leebeek FW (2006) Hepatocyte-derived fibrinogen-related protein-1 is associated with the fibrin matrix of a plasma clot. Biochem Biophys Res Commun 350: 191–194. [DOI] [PubMed] [Google Scholar]
- 36.Yamamoto T, Gotoh M, Sasaki H, Terada M, Kitajima M, Hirohashi S (1993) Molecular cloning and initial characterization of a novel fibrinogen-related gene, HFREP-1. Biochem Biophys Res Commun 193: 681–687. [DOI] [PubMed] [Google Scholar]
- 37.Russell SR, Mullins RF, Schneider BL, Hageman GS (2000) Location, substructure, and composition of basal laminar drusen compared with drusen associated with aging and age-related macular degeneration. Am J Ophthalmol 129: 205–214. [DOI] [PubMed] [Google Scholar]
- 38.Saksens NT, Geerlings MJ, Bakker B, Schick T, Daha MR, Fauser S, et al. (2016) Rare Genetic Variants Associated With Development of Age-Related Macular Degeneration. JAMA Ophthalmol: 1–8. [DOI] [PubMed] [Google Scholar]
- 39.Yu Y, Triebwasser MP, Wong EK, Schramm EC, Thomas B, Reynolds R, et al. (2014) Whole-exome sequencing identifies rare, functional CFH variants in families with macular degeneration. Hum Mol Genet 23: 5283–5293. 10.1093/hmg/ddu226 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.