Abstract
Mutations in epithelial growth factor receptor (EGFR), as well as in the EGFR downstream target KRAS are frequently observed in non-small cell lung cancer (NSCLC). Chronic obstructive pulmonary disease (COPD), an independent risk factor for developing NSCLC, is associated with an increased activation of EGFR. In this study we determined presence of EGFR and KRAS hotspot mutations in 325 consecutive NSCLC patients subjected to EGFR and KRAS mutation analysis in the diagnostic setting and for whom the pulmonary function has been determined at time of NSCLC diagnosis. Information about age at diagnosis, sex, smoking status, forced vital capacity (FVC) and forced expiratory volume in 1 sec (FEV1) was collected. Chronic obstructive pulmonary disease(COPD) was defined according to 2013 GOLD criteria. Chi-Square, student t-test and multivariate logistic regression were used to analyze the data. A total of 325 NSCLC patients were included, 193 with COPD and 132 without COPD. COPD was not associated with presence of KRAS hotspot mutations, while EGFR mutations were significantly higher in non-COPD NSCLC patients. Both female gender (HR 2.61; 95% CI: 1.56–4.39; p<0.001) and smoking (HR 4.10; 95% CI: 1.14–14.79; p = 0.03) were associated with KRAS mutational status. In contrast, only smoking (HR 0.11; 95% CI: 0.04–0.32; p<0.001) was inversely associated with EGFR mutational status. Smoking related G>T and G>C transversions were significantly more frequent in females (86.2%) than in males (61.5%) (p = 0.008). The exon 19del mutation was more frequent in non-smokers (90%) compared to current or past smokers (36.8%). In conclusion, KRAS mutations are more common in females and smokers, but are not associated with COPD-status in NSCLC patients. EGFR mutations are more common in non-smoking NSCLC patients.
Introduction
Chronic obstructive pulmonary disease (COPD) is associated with lung cancer also after accounting for other respiratory diseases and smoking [1–2]. An increased risk of lung cancer in COPD patients was evident in a meta-analysis [2]. About one third of smokers with COPD died of lung cancer within a follow-up of 14.5 years [3]. On the other hand, 50–70% of the lung cancer patients have COPD according to results of pulmonary function tests at time of diagnosis [4]. In a more recent, large prospective study, the association between COPD and lung cancer was largely explained by smoking [5]. The odds ratio (OR) for patients diagnosed with COPD to develop lung cancer within a period of 6 months was 11.4. However, the OR dropped to 6.8 after correction for smoking [5]. This is consistent with the notion that COPD has been recognized as an independent risk factor for developing lung cancer [6].
KRAS is involved in regulation of cell proliferation [7]. Mutations in KRAS are mostly found in codons 12, 13 and 61 and result in constitutive activation of the protein [8]. KRAS mutations are observed more frequent in smoking patients with adenocarcinoma (5–40%) than in the other subtypes of lung cancer [7, 9]. Mutations in KRAS are associated with poorer prognosis of NSCLC patients [10]. Moreover, a COPD-like airway inflammation can increase lung carcinogenesis in the presence of the p.G12D K-ras activating mutation in a mouse model [11].
EGFR plays a crucial role in wound healing and tissue repair in the lung, especially in the bronchial wall. Overexpression of EGFR was reported in the bronchial mucosa of non-smoking asthmatic individuals compared to normal controls [12]. Moreover, prolonged activation of EGFR leads to metaplasia [13]. Exposure of epithelial cells to cigarette smoke induced aberrant phosphorylation and activation of EGFR and this may subsequently mediate development of lung cancer [14–15]. Mutations in the kinase domain also lead to activation of the EGFR pathway independent of binding to its ligand [16]. These activating EGFR mutations are common in non-small cell lung cancer (NSCLC) with a frequency of about 10–15% in Caucasians [17–18]. EGFR mutations have been associated with non-smoking NSCLC patients [19]. The p.(L858R) in exon 21 (referred to as L858R) and deletions in exon 19 (referred to as exon 19del) of the EGFR gene are the most commonly observed activating mutations [20]. We previously showed a significant association between EGFR mutations and clinical outcome [21]. In vivo studies in mouse models conditionally expressing either the L858R or an exon19del mutant allele of the human EGFR gene have supported the role of these mutations in initiation and development of lung cancer [22].
Smoking is a known risk factor for both COPD and lung cancer [23–24]. KRAS mutations are described as a signature for cigarette smoking [25], while EGFR mutations are more common in non-smokers. We hypothesize that KRAS mutations are positively associated with COPD status in NSCLC patients, while activating EGFR mutations are negatively associated with COPD in NSCLC patients. To study this hypothesis we analyzed NSCLC patients screened for the presence of EGFR and KRAS mutations in a diagnostic setting and investigated whether the presence of EGFR and KRAS mutations in NSCLC patients was related to COPD.
Materials and Methods
Patients
Consecutive patients with advanced NSCLC, diagnosed between November 2008 and July 2012, and for whom KRAS and EGFR mutation analysis was performed in a clinical setting, were selected for this study. In this cohort we further selected patients for whom lung function data were available. All patients had stage IV NSCLC and had one or more visceral metastases at diagnosis. Previously, 165 of the NSCLC patients have been described in a study on EGFR and KRAS mutations in relation to clinical outcome [21]. Patients with NSCLC post lung transplantation were excluded from this study. For all patients, data on gender, smoking status (including pack year if available), age at diagnosis, stage at diagnosis according to the 6th TNM edition, localization of metastases, start date and (different) lines of treatment were collected. Data on lung function was newly collected for all patients included in this study. All procedures and protocols were performed according to the guidelines for good clinical practice and after informed consent was obtained from all patients.
Informed Consent and Ethics
Written informed consent for blood and tumor tissue from all patients was obtained before biobanking. This procedure was approved by the Medical Ethical Committee of the University Medical Center Groningen. This study was conducted in accordance with the provisions of the Declaration of Helsinki and Good Clinical Practice guidelines. For this study, all patient data were anonymized and de-identified prior to analysis. Besides the mutational analysis, pulmonary function tests were performed as part of routine diagnostic approach and the outcome of these tests was documented in the patient file and communicated with patients. Due to the retrospective nature of this study, under Dutch Law for human medical research (WMO), no specific permission was compulsory from the Institutional Review Board.
Pulmonary function testing
Spirometry was performed with a daily-calibrated pneumotachograph (MasterscreenPneumo, Jaeger, Wurzburg, Germany) according to standardized guidelines [26]. Lung function tests are provided after bronchodilatator (salbutamol 100 microgram). Patients were defined as having COPD if the forced expiratory volume in 1 sec (FEV1)/forced vital capacity (FVC) (FEV1/FVC) was <0.70 with fixed bronchial obstruction over time not due to endobronchial tumor obstruction. Staging of COPD was performed according to GOLD criteria [27].
Histology and KRAS/EGFR molecular testing
Tumor samples were obtained either by bronchoscopy, transthoracic lung biopsies and/or from pulmonary resections. Histological subtyping was performed according to 2004 WHO criteria [28]. Mutational analysis was performed as previously described [21].
Statistics
For normally distributed data we show mean and standard deviation (SD) and used a student t-test to determine significant differences. For not normally distributed data median and range are given and Chi-Square test is used to determine significance. Logistic regression was performed to study whether the presence of COPD had any effect on KRAS or EGFR mutational status using sex, age, histology, and smoking as covariates. Statistical analysis was performed using SPSS version 22.0. Nominal P-values less than 0.05 were considered significant. Data are available in S1 Table.
Results
Patient characteristics and KRAS/EGFR mutations
A total of 325 stage IV NSCLC patients were included. Over 80% had adenocarcinoma, 174 (53.5%) were male and 151 (46.5%) female. The mean age at time of diagnosis was 63.6 (±10.5 years). One hundred and five patients (32.3%) had a KRAS mutation. For 1 out of 105 patients with a KRAS mutation, the type of mutation was inconclusive with a positive high resolution melting (HRM) PCR result, but with a wild type sequence based on the Sanger sequencing result. For one patient with an EGFR mutation, the KRAS mutation status was not available. The remaining 219 patients did not have mutations in the KRAS hotspot region. Twenty-nine patients (8.9%) had an EGFR mutation. In five patients, the EGFR mutational status was not available; four of these patients did have a KRAS mutation. The other 291 patients did not have EGFR mutations in the hotspot regions. The mean age of the males was higher than the mean age of the females (66.3 ±9.8 years vs. 60.5 ±10.5 years; p<0.001). Males showed a significant higher number of smoking pack years than females (mean 37.5 ±20.6 pack years vs. 30.1 ±15.7 pack years; p = 0.015).
Patient characteristics in COPD stratified subgroups
Almost 60% (193/325) of the NSCLC patients had COPD. Two third of the COPD cases were males. The distribution of females was almost equal in COPD and non-COPD groups (Table 1). Mean age in the COPD group was higher with 65.6 years (±9.9 years) compared to the non-COPD group with 60.6 (±10.8 years) (p<0.001). We found a significant relationship between smoking and COPD, 62.6% of current or past smokers had COPD, while only 18.2% of non-smokers had COPD (p<0.001). A logistic regression model for COPD using sex, age and smoking as covariates revealed significant associations with age (Hazard ratio [HR] 1.05; 95% confidence interval [CI]: 1.02–1.07; p<0.001) and smoking (HR 8.28; 95% CI: 2.61–26.24; p<0.001), but not with gender (Table 2).
Table 1. NSCLC patient characteristics according to COPD status.
| Characteristics | COPD (%) N = 193 | Non-COPD (%) N = 132 | p-value |
|---|---|---|---|
| Sex | |||
| Female | 77 (51) | 74 (49) | 0.004† |
| Male | 116 (66.7) | 58 (33.3) | |
| Age at diagnosis, Mean (±SD) | 65.6 (±9.9) | 60.6 (±10.8) | <0.001* |
| Histology | |||
| Adenocarcinoma | 154 (59) | 107 (41) | 0.777† |
| Adeno-squamous | 14 (66.7) | 7 (33.3) | |
| NSCLC-NOS | 25 (58.1) | 18 (41.9) | |
| Smoking status# | |||
| Current or past smoker | 184 (62.6) | 110 (37.4) | <0.001† |
| Non-smoker | 4 (18.2) | 18 (81.8) | |
| FEV1%, Mean (±SD) | 72.8 (±18.7) | 90.2 (±19.4) | - |
| FEV1/FVC ratio, Mean (±SD) | 0.58 (±0.09) | 0.76 (±0.05) | - |
| KRAS mutation# | |||
| Yes | 66 (62.9) | 39 (37.1) | 0.404† |
| No | 127 (58) | 92 (42) | |
| EGFR activating mutation# | |||
| Yes | 9 (31) | 20 (69) | 0.001† |
| No | 180 (61.9%) | 111 (38.1) |
* T-test;
†Chi-square test;
#Missing data for smoking (n = 9), KRAS (n = 1) and EGFR (n = 5) status.
Table 2. Logistic regression analysis of patient characteristics associated with COPD, KRAS and EGFR.
| Characteristics | COPD | KRAS | EGFR | ||||||
|---|---|---|---|---|---|---|---|---|---|
| HR | 95% CI | p-value | HR | 95% CI | p-value | HR | 95% CI | p-value | |
| Sex | 0.78 | 0.48–1.29 | 0.33 | 2.61 | 1.56–4.39 | <0.001 | 1.21 | 0.51–2.90 | 0.66 |
| Age | 1.05 | 1.02–1.07 | <0.001 | 0.99 | 0.97–1.01 | 0.39 | 0.98 | 0.95–1.02 | 0.39 |
| Smoking | 8.28 | 2.61–26.24 | <0.001 | 4.10 | 1.14–14.79 | 0.03 | 0.11 | 0.04–0.32 | <0.001 |
| COPD | - | - | - | 1.29 | 0.77–2.18 | 0.34 | 0.44 | 0.18–1.09 | 0.08 |
HR: Hazard ratio; CI: Confidence interval
COPD and tumor KRAS/EGFR hotspot mutations
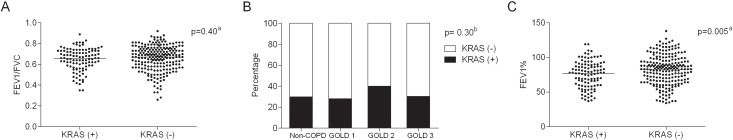
KRAS mutations were observed more often in females compared to males (65/151 (43%) versus 40/173, (23%); p<0.001) and also more often in current or past smokers (34.5%) than in non-smokers (13.6%) (p = 0.045) (Table 3). KRAS mutations were not significantly different between COPD (34.2%) and non-COPD patients (29.8%) (Table 1), sothe presence of KRAS mutations were independent of COPD. Stratification according to FEV1/FVC and GOLD stage did not reveal a significant association with presence of KRAS mutation (Fig 1A and 1B). However, FEV1 percentage as a continuous variable was significantly related to the presence of KRAS mutations (Fig 1C), but not in a multivariate analysis. Putting the variables (sex, age, smoking and COPD) in a logistic regression model confirmed the significant association between KRAS hotspot mutations with female sex (HR 2.61; 95% CI: 1.56–4.39; p<0.001) and smoking (HR 4.10; 95% CI: 1.14–14.79; p = 0.03) (Table 2).
Table 3. NSCLC patient characteristics andKRAS/EGFR mutation*.
| Characteristics | KRAS mutation | Pearson Chi-Square | EGFR mutation | Pearson Chi-Square | ||
|---|---|---|---|---|---|---|
| No (%) | Yes (%) | No (%) | Yes (%) | |||
| Sex | ||||||
| Female | 86 (57) | 65 (43) | <0.001 | 130 (87.8) | 18 (12.2) | 0.07 |
| Male | 133 (76.9) | 40 (23.1) | 161 (93.6) | 11 (6.4) | ||
| Smoking status | ||||||
| Current or past smoker | 192 (65.5) | 101 (34.5) | 0.045 | 270 (93.4) | 19 (6.6) | <0.001 |
| Nonsmoker | 19 (86.4) | 3 (13.6) | 12 (54.5) | 10 (45.5) | ||
* Missing data for smoking (n = 9), KRAS (n = 1) and EGFR (n = 5) status.
Fig 1. KRAS mutations and severity of airflow obstruction.
(A) FEV1/FVC, (B) COPD GOLD classification and (C) FEV1 percentage in KRAS mutant and wildtype patients with NSCLC. aP-value was calculated by student t-test. bP-value was calculated by Chi-square test.
EGFR mutations showed a trend to a higher frequency in females compared to males, (p = 0.073). Ten out of 22 (45.5%) non-smokers had activating EGFR mutations, while only 19 out of 289 (6.5%) of the current or past smokers had an EGFR mutation (p<0.001). EGFR mutations were observed more often in the non-COPD (20/131, i.e. 15.3%) as compared to the COPD group (9/189, i.e. 4.8%)(p = 0.001) (Table 3). Using sex, age, smoking and COPD as covariates in a logistic regression model for EGFR mutations, confirmedsignificant inverse association between smoking (HR 0.11; 95% CI: 0.04–0.32; p<0.001) and EGFR mutational status (Table 2).
COPD and type of KRAS/EGFR mutations
The KRAS p.(G12C) was the most common amino acid change in both male and female with a frequency of approximately 41%. The p.(G12V) and p.(G12D) mutations were the second most frequent mutations in females and males, with a frequency of 20% and 25.6%, respectively (Table 4). Forty-three percent of the KRAS mutations in the current or past smoker group were p.(G12C) mutations, while none of the non-smoking patients had this mutation. In addition, G>T and G>C transversions in KRAS occurred in 86.2% of the females and in 61.5% of the males. The G>A transition was more common in males than in females (p = 0.008)(Table 5). COPD status was not associated with any type of KRAS amino acid changes or nucleotide substitutions.
Table 4. Distribution of different KRAS amino acid changes in advanced NSCLC patients*.
| Characteristics | KRAS amino acid change | Pearson Chi-Square | ||||
|---|---|---|---|---|---|---|
| p.(G12C) (%) | p.(G12V) (%) | p.(G12A) (%) | p.(G12D) (%) | Other (%) | ||
| Sex | ||||||
| Female | 27 (41.5) | 13 (20) | 7 (10.8) | 6 (9.2) | 12 (18.8) | 0.20 |
| Male | 16 (41) | 5 (12.8) | 2 (5.1) | 10 (25.6) | 6 (15.4) | |
| Histology | ||||||
| Adenocarcinoma | 41 (42.7) | 16 (16.7) | 8 (8.3) | 13 (13.5) | 18 (18.8) | 0.26 |
| NSCLC NOS | 2 (25) | 2 (25) | 1(12.5) | 3 (37.5) | 0 | |
| Smoking status | ||||||
| Current or past smoker | 43 (43) | 17 (17) | 7 (7) | 15 (15) | 18 (18) | 0.24 |
| Nonsmoker | 0 | 1 (33.3) | 1 (33.3) | 1 (33.3) | 0 | |
| COPD | ||||||
| Yes | 27 (40.9) | 11 (16.7) | 6 (9.1) | 11 (16.7) | 11 (16.7) | 0.99 |
| No | 16 (42.1) | 7 (18.4) | 3 (7.9) | 5 (13.2) | 7 (18.4) | |
* Missing data for smoking (n = 1) status and type of KRAS mutation (n = 1); p.(G12C) and p.(G12V) (G>T), p.(G12A) (G>C), p.(G12D) (G>A).
Table 5. Distribution of different KRAS nucleotide changes in advanced NSCLC patients*.
| Characteristics | KRAS mutations | Pearson Chi-Square* | ||
|---|---|---|---|---|
| Transversions G>T, G>C (%) | Transitions G>A (%) | Other (%) | ||
| Sex | ||||
| Female | 56 (86.2) | 7 (10.8) | 2 (3.1) | 0.008 |
| Male | 24 (61.5) | 14 (35.9) | 1 (2.6) | |
| Histology | ||||
| Adenocarcinoma | 75 (78.1) | 18 (18.8) | 3 (3.1) | 0.41 |
| NSCLC NOS | 5 (62.5) | 3 (37.5) | 0 | |
| Smoking | ||||
| Current or past smoker | 77 (77) | 20 (20) | 3 (3) | 0.83 |
| Nonsmoker | 2 (66.7) | 1 (33.3) | 0 | |
| COPD | ||||
| Yes | 50 (75.8) | 14 (21.2) | 2 (3) | 0.93 |
| No | 30 (78.9) | 7 (18.4) | 1 (2.6) | |
* Missing data for smoking (n = 1) status and type of KRAS mutation (n = 1).
Of all EGFR mutation positive cases the percentage of patients with an exon 19del was not significantly different between females (11/18) and males (5/11). In non-smokers, 9 out of 10 EGFR mutation positive cases had an exon 19del (Table 6), whereas in current or past smokers only 7 out of 19 patients with an EGFR mutation had an exon 19del.
Table 6. Distribution of different EGFR mutations in advanced NSCLC patients.
| Characteristics | EGFR mutations | Pearson Chi-Square | ||
|---|---|---|---|---|
| Exon 19del (%)* | p.(L858R) (%)† | Other (%)‡ | ||
| Sex | ||||
| Female | 11 (61.1) | 4 (22.2) | 3 (16.7) | 0.69 |
| Male | 5 (45.5) | 3 (27.3) | 3 (27.3) | |
| Histology | ||||
| Adenocarcinoma | 16 (57.1) | 6 (21.4) | 6 (21.4) | 0.20 |
| NSCLC NOS | 0 | 1 (100) | 0 | |
| Smoking | ||||
| Current or past smoker | 7 (36.8) | 6 (31.6) | 6 (31.6) | 0.02 |
| Nonsmoker | 9 (90) | 1 (10) | 0 | |
| COPD | ||||
| Yes | 5 (55.6) | 3 (33.3) | 1 (11.1) | 0.60 |
| No | 11 (55) | 4 (20) | 5 (25) | |
* One patient had an exon 19del and p.(T790M),
†One patient had a p.(L858R) and p.(T790M),
‡ One patient had a p.(G719S) and p.(S768I) and another patient had a p.(G719C) and an exon 20 insertion.
Discussion
In contrast to our hypothesis we showed that COPD is not associated with the presence of KRAS mutations in lung cancer, whereas presence of EGFR mutations was more frequent in non-COPD as compared to COPD lung cancer patients, after correcting for sex and smoking. We found significantly higher mean age in the COPD group as compared to the non-COPD group. This finding is consistent with the fact that the COPD prevalence increases with age [29].
KRAS mutations were identified in 32% of the NSCLC patients, which mainly included adenocarcinoma patients. We observed a relationship between presence of KRAS hotspot mutations and smoking status consistent with previous studies [25, 30], but not with COPD. In other studies no relation between smoking and the presence of KRASmutations have been observed in lung cancer patients[25, 30–32]. These differences may be caused by differences in selecting study groups, ethnicity, number of patients and smoking status. The lack of an association with COPD is in concordance with the results reported ina recent study [33].
Although smoking females were younger and lighter smokers based on pack years than the males, we noticed that KRAS mutations were more common in smoking females than in smoking males with NSCLC. This supports an increased susceptibility of females to cigarette carcinogens as reported previously [34]. Moreover, these results are also consistent with a previous study showing that females had a higher OR for lung cancer at every level of tobacco exposure [35]. This elevated vulnerability to smoking may be caused by the higher expression levels of genes encoding tobacco carcinogen-metabolizing enzymes, such as CYP1A1 and CYP1B1, in normal lung tissue of female smokers in comparison to male smokers [36]. Uppstad and colleagues [37] also showed higher expression of CYP1A1 in cell lines derived from lung adenocarcinoma of female compared to cell lines derived from adenocarcinomas of male patients.
Although we observed the smoking related p.(G12C) KRAS mutation at the same frequency in both genders, smoking related transversions, i.e. G>T and G>C, were significantly more common in females than in males. In a previous study with a sample size of over 2,500 patients, the c.34G>T; p.(G12C) KRAS mutation occurred more frequent in females and current or past smokers, while the c.35G>A; p.(G12D) KRAS mutations were more frequent in never smokers [20]. This suggests again that females are more susceptible of cigarette smoke related KRAS mutations compared to males.
We showed that EGFR activating mutations were more common in females, non-smokers and in non-COPD NSCLC patients. In a recent study, EGFR mutations were seen in 12.8% (51/399) of lung cancer patients without COPD and in 6.3% (7/111) of patients with COPD [38]. Suzukiand colleagues [39]identified EGFR mutations in 32% (56/177) of the non-COPD and in 8% (4/52) of the COPD NSCLC patients. Lim and colleagues[33] found EGFR mutations in 37.3% (91/244) of non-COPD and in 16% (17/106) of COPD patients. They also found an inverse association between the presence of EGFR mutation with severity of airflow obstruction. The finding that EGFR mutations are more common in non-COPD lung cancer patients might indicate that lung cancer development is dependent on activating EGFR mutations in non-COPD patients.Chronic pulmonary diseases, such as severe asthma and COPD, cause an increased activation of the epithelial growth factor receptor (EGFR)[12, 40]. Moreover, COPD is characterized by epithelial inflammatory reactions and many pro-inflammatory chemokines and growth factors are induced by transcription factor Nuclear Factor kB (NFkB). This transcription factor can be activated via physical and chemical stress such as smoke [41]. In addition, increased activation of EGFR by oxidative stress, which is involved in pathogenesis of COPD, or cigarette smoke can occur in human bronchial epithelial cells [14–15, 42]. All together suggesting that EGFR activation in COPD is induced by smoking, oxidative stress and subsequently by inflammation probably via NFkB.
In conclusion, KRAS mutations were more common in females and smokers, but are not associated with COPD-status in NSCLC patients. EGFR mutations are more common in females and non-smoking NSCLC patients.
Supporting Information
(XLSX)
Acknowledgments
We are grateful to the molecular diagnostics team for EGFR and KRAS mutation analysis and help with data collection.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
The authors have no support or funding to report.
References
- 1.Denholm R, Schuz J, Straif K, Stucker I, Jockel KH, Brenner DR, et al. Is previous respiratory disease a risk factor for lung cancer? Am J Respir Crit Care Med. 2014; 190(5):549–59. 10.1164/rccm.201402-0338OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brenner DR, McLaughlin JR, Hung RJ. Previous lung diseases and lung cancer risk: a systematic review and meta-analysis. PLoS One. 2011; 6(3):e17479 10.1371/journal.pone.0017479 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Anthonisen NR, Skeans MA, Wise RA, Manfreda J, Kanner RE, Connett JE. The effects of a smoking cessation intervention on 14.5-year mortality: a randomized clinical trial. Ann Intern Med. 2005; 142(4):233–9. [DOI] [PubMed] [Google Scholar]
- 4.Yao H, Rahman I. Current concepts on the role of inflammation in COPD and lung cancer. Curr Opin Pharmacol. 2009; 9(4):375–83. 10.1016/j.coph.2009.06.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Powell HA, Iyen-Omofoman B, Baldwin DR, Hubbard RB, Tata LJ. Chronic obstructive pulmonary disease and risk of lung cancer: the importance of smoking and timing of diagnosis. J Thorac Oncol. 2013; 8(1):6–11. 10.1097/JTO.0b013e318274a7dc [DOI] [PubMed] [Google Scholar]
- 6.Young RP, Hopkins RJ, Christmas T, Black PN, Metcalf P, Gamble GD. COPD prevalence is increased in lung cancer, independent of age, sex and smoking history. Eur Respir J. 2009; 34(2):380–6. 10.1183/09031936.00144208 [DOI] [PubMed] [Google Scholar]
- 7.Okudela K, Woo T, Kitamura H. KRAS gene mutations in lung cancer: particulars established and issues unresolved. Pathol Int. 2010; 60(10):651–60. 10.1111/j.1440-1827.2010.02580.x [DOI] [PubMed] [Google Scholar]
- 8.Riely GJ, Marks J, Pao W. KRAS mutations in non-small cell lung cancer. Proc Am Thorac Soc. 2009; 6(2):201–5. 10.1513/pats.200809-107LC [DOI] [PubMed] [Google Scholar]
- 9.Saber A, van der Wekken A, Hiltermann TJ, Kok K, Van den Berg A, Groen H. Genomic aberrations guiding treatment of non-small cell lung cancer patients. Cancer Treatment Communications. 2015; 4:23–33. [Google Scholar]
- 10.Sunaga N, Kaira K, Imai H, Shimizu K, Nakano T, Shames DS, et al. Oncogenic KRAS-induced epiregulin overexpression contributes to aggressive phenotype and is a promising therapeutic target in non-small-cell lung cancer. Oncogene. 2013; 32(34):4034–42. 10.1038/onc.2012.402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Moghaddam SJ, Li H, Cho SN, Dishop MK, Wistuba II, Ji L, et al. Promotion of lung carcinogenesis by chronic obstructive pulmonary disease-like airway inflammation in a K-ras-induced mouse model. Am J Respir Cell Mol Biol. 2009; 40(4):443–53. 10.1165/rcmb.2008-0198OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Puddicombe SM, Polosa R, Richter A, Krishna MT, Howarth PH, Holgate ST, et al. Involvement of the epidermal growth factor receptor in epithelial repair in asthma. FASEB J. 2000; 14(10):1362–74. [DOI] [PubMed] [Google Scholar]
- 13.Tyner JW, Kim EY, Ide K, Pelletier MR, Roswit WT, Morton JD, et al. Blocking airway mucous cell metaplasia by inhibiting EGFR antiapoptosis and IL-13 transdifferentiation signals. J Clin Invest. 2006; 116(2):309–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Filosto S, Becker CR, Goldkorn T. Cigarette smoke induces aberrant EGF receptor activation that mediates lung cancer development and resistance to tyrosine kinase inhibitors. Mol Cancer Ther. 2012; 11(4):795–804. 10.1158/1535-7163.MCT-11-0698 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Khan EM, Lanir R, Danielson AR, Goldkorn T. Epidermal growth factor receptor exposed to cigarette smoke is aberrantly activated and undergoes perinuclear trafficking. FASEB J. 2008; 22(3):910–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Piperdi B, Perez-Soler R. Role of erlotinib in the treatment of non-small cell lung cancer: clinical outcomes in wild-type epidermal growth factor receptor patients. Drugs. 2012; 72 Suppl 1:11–9. 10.2165/1163018-S0-000000000-00000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Blons H, Cote JF, Le Corre D, Riquet M, Fabre-Guilevin E, Laurent-Puig P, et al. Epidermal growth factor receptor mutation in lung cancer are linked to bronchioloalveolar differentiation. Am J Surg Pathol. 2006; 30(10):1309–15. [DOI] [PubMed] [Google Scholar]
- 18.Reinmuth N, Jauch A, Xu EC, Muley T, Granzow M, Hoffmann H, et al. Correlation of EGFR mutations with chromosomal alterations and expression of EGFR, ErbB3 and VEGF in tumor samples of lung adenocarcinoma patients. Lung Cancer. 2008; 62(2):193–201. 10.1016/j.lungcan.2008.03.011 [DOI] [PubMed] [Google Scholar]
- 19.Ma ES, Ng WK, Wong CL. EGFR gene mutation study in cytology specimens. Acta Cytol. 2012; 56(6):661–8. 10.1159/000343606 [DOI] [PubMed] [Google Scholar]
- 20.Dogan S, Shen R, Ang DC, Johnson ML, D'Angelo SP, Paik PK, et al. Molecular epidemiology of EGFR and KRAS mutations in 3,026 lung adenocarcinomas: higher susceptibility of women to smoking-related KRAS-mutant cancers. Clin Cancer Res. 2012; 18(22):6169–77. 10.1158/1078-0432.CCR-11-3265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kerner GS, Schuuring E, Sietsma J, Hiltermann TJ, Pieterman RM, de Leede GP, et al. Common and rare EGFR and KRAS mutations in a Dutch non-small-cell lung cancer population and their clinical outcome. PLoS One. 2013; 8(7):e70346 10.1371/journal.pone.0070346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Politi K, Zakowski MF, Fan PD, Schonfeld EA, Pao W, Varmus HE. Lung adenocarcinomas induced in mice by mutant EGF receptors found in human lung cancers respond to a tyrosine kinase inhibitor or to down-regulation of the receptors. Genes Dev. 2006; 20(11):1496–510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Eklund BM, Nilsson S, Hedman L, Lindberg I. Why do smokers diagnosed with COPD not quit smoking?—a qualitative study. Tob Induc Dis. 2012; 10(1):17 10.1186/1617-9625-10-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Molina JR, Yang P, Cassivi SD, Schild SE, Adjei AA. Non-small cell lung cancer: epidemiology, risk factors, treatment, and survivorship. Mayo Clin Proc. 2008; 83(5):584–94. 10.4065/83.5.584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ahrendt SA, Decker PA, Alawi EA, Zhu YR, Sanchez-Cespedes M, Yang SC, et al. Cigarette smoking is strongly associated with mutation of the K-ras gene in patients with primary adenocarcinoma of the lung. Cancer. 2001; 92(6):1525–30. [DOI] [PubMed] [Google Scholar]
- 26.Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A, et al. Standardisation of spirometry. Eur Respir J. 2005; 26(2):319–38. [DOI] [PubMed] [Google Scholar]
- 27.Vestbo J, Hurd SS, Agusti AG, Jones PW, Vogelmeier C, Anzueto A, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med. 2013; 187(4):347–65. 10.1164/rccm.201204-0596PP [DOI] [PubMed] [Google Scholar]
- 28.Travis WD, Brambilla E, Muller-Hermelink HK, Harris CCE. World Health Organization Classification of Tumours Pathology and Genetics of Tumours of the Lung, Pleura, Thymus and Heart. Lyon: IARC Press; 2004. [Google Scholar]
- 29.Mannino DM, Buist AS. Global burden of COPD: risk factors, prevalence, and future trends. Lancet. 2007; 370(9589):765–73. [DOI] [PubMed] [Google Scholar]
- 30.Shigematsu H, Lin L, Takahashi T, Nomura M, Suzuki M, Wistuba II, et al. Clinical and biological features associated with epidermal growth factor receptor gene mutations in lung cancers. J Natl Cancer Inst. 2005; 97(5):339–46. [DOI] [PubMed] [Google Scholar]
- 31.Li M, Liu L, Liu Z, Yue S, Zhou L, Zhang Q, et al. The status of KRAS mutations in patients with non-small cell lung cancers from mainland China. Oncol Rep. 2009; 22(5):1013–20. [DOI] [PubMed] [Google Scholar]
- 32.Riely GJ, Kris MG, Rosenbaum D, Marks J, Li A, Chitale DA, et al. Frequency and distinctive spectrum of KRAS mutations in never smokers with lung adenocarcinoma. Clin Cancer Res. 2008; 14(18):5731–4. 10.1158/1078-0432.CCR-08-0646 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lim JU, Yeo CD, Rhee CK, Kim YH, Park CK, Kim JS, et al. Chronic Obstructive Pulmonary Disease-Related Non-Small-Cell Lung Cancer Exhibits a Low Prevalence of EGFR and ALK Driver Mutations. PLoS One. 2015; 10(11):e0142306 10.1371/journal.pone.0142306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Henschke CI, Yip R, Miettinen OS. Women's susceptibility to tobacco carcinogens and survival after diagnosis of lung cancer. JAMA. 2006; 296(2):180–4. [DOI] [PubMed] [Google Scholar]
- 35.Zang EA, Wynder EL. Differences in lung cancer risk between men and women: examination of the evidence. J Natl Cancer Inst. 1996; 88(3–4):183–92. [DOI] [PubMed] [Google Scholar]
- 36.Mollerup S, Berge G, Baera R, Skaug V, Hewer A, Phillips DH, et al. Sex differences in risk of lung cancer: Expression of genes in the PAH bioactivation pathway in relation to smoking and bulky DNA adducts. Int J Cancer. 2006; 119(4):741–4. [DOI] [PubMed] [Google Scholar]
- 37.Uppstad H, Osnes GH, Cole KJ, Phillips DH, Haugen A, Mollerup S. Sex differences in susceptibility to PAHs is an intrinsic property of human lung adenocarcinoma cells. Lung Cancer. 2011; 71(3):264–70. 10.1016/j.lungcan.2010.09.006 [DOI] [PubMed] [Google Scholar]
- 38.Maki-Nevala S, Ronty M, Morel M, Gomez M, Dawson Z, Sarhadi VK, et al. Epidermal growth factor receptor mutations in 510 Finnish non—small-cell lung cancer patients. J Thorac Oncol. 2014; 9(6):886–91. 10.1097/JTO.0000000000000132 [DOI] [PubMed] [Google Scholar]
- 39.Suzuki M, Wada H, Yoshino M, Tian L, Shigematsu H, Suzuki H, et al. Molecular characterization of chronic obstructive pulmonary disease-related non-small cell lung cancer through aberrant methylation and alterations of EGFR signaling. Ann Surg Oncol. 2010; 17(3):878–88. 10.1245/s10434-009-0739-3 [DOI] [PubMed] [Google Scholar]
- 40.Ganesan S, Unger BL, Comstock AT, Angel KA, Mancuso P, Martinez FJ, et al. Aberrantly activated EGFR contributes to enhanced IL-8 expression in COPD airways epithelial cells via regulation of nuclear FoxO3A. Thorax. 2013; 68(2):131–41. 10.1136/thoraxjnl-2012-201719 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Edwards MR, Bartlett NW, Clarke D, Birrell M, Belvisi M, Johnston SL. Targeting the NF-kappaB pathway in asthma and chronic obstructive pulmonary disease. Pharmacol Ther. 2009; 121(1):1–13. 10.1016/j.pharmthera.2008.09.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.MacNee W. Oxidants/antioxidants and COPD. Chest. 2000; 117(5 Suppl 1):303S–17S. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(XLSX)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.