Abstract
Objective:
Suicidal behavior (suicidal ideation, suicide attempts, and suicide completion) has been increasingly linked with difficulty initiating sleep, maintaining sleep, and early morning awakenings. However, the relationship between suicidal behavior and sleep duration abnormalities is unclear, especially at the population level. The present study used a nationally representative sample to examine the association of suicidal ideation with extreme sleep durations and insomnia symptoms.
Method:
Cross-sectional data from adult respondents (≥ 18 years of age, N = 6,228) were extracted from the 2007–2008 wave of the National Health and Nutritional Examination Survey. Ordinal logistic regression analyses were used to evaluate the relationship of suicidal ideation with sleep duration, global insomnia, and individual insomnia symptoms in models adjusted for sociodemographic, socioeconomic, and health-related covariates.
Results:
Suicidal ideation was associated with abnormalities of sleep duration. This relationship ceased to exist once the model was adjusted for depressive symptoms. As expected, an increased level of suicidal ideation was consistently associated with insomnia. Of the insomnia symptoms, difficulty maintaining sleep was found to be the most predictive of suicidal ideation, followed by difficulty initiating sleep (P< .05).
Conclusions:
Abnormalities of sleep duration and continuity should prompt a clinical assessment for suicide risk.
Clinical Points
■ Increased suicidal ideation was associated with abnormalities of sleep duration.
■ Increased suicidal ideation was positively associated with insomnia.
■ Clinicians should screen for depressive disorder and suicidal ideation in patients complaining of insomnia and abnormalities of sleep duration.
Suicide is the 10th leading cause of death in the United States, claiming more than 36,000 lives per year.1 Suicide is an important concern for psychiatric and health care professionals as well as public policy makers. Suicide is often associated with psychiatric disorders. According to a 2004 meta-analysis,2 the mean percentage of suicides with a psychiatric diagnosis was 87.3%. On average, 43.2% of suicide patients were diagnosed with affective disorders (including depressive and bipolar disorders) and 25.7% with other substance problems.2 While completed suicide is the ultimate cause of death, studies of suicidal ideation can yield valuable information on risk factors for committing suicide. Current suicidal ideation is the best indicator of a recent suicide attempt in psychiatric patients3 as well as eventual suicide.4
Studies5–11 have further demonstrated a link between suicidal behavior and sleep continuity disturbances. A prospective cohort study7 performed with a representative population in Norway reported a strong association between sleeping problems and completed suicide. In a sleep medical center sample, Krakow et al6 found that suicidal ideation was associated with insomnia symptoms. Generally, difficulty initiating sleep, maintaining sleep, and early morning awakening all relate to suicidal behavior. Difficulty initiating sleep has been cited as a predictor of suicidal ideation and planning, while difficulty maintaining sleep has been shown to be a significant predictor of suicide attempts.12 Yang and colleagues5 observed Internet searches for the word insomnia were elevated 1 month prior to a known suicide attempt.
A number of other studies utilizing samples from special populations such as adolescents, prisoners, military personnel, and persons misusing alcohol have demonstrated strong links between insomnia and suicide. Insomnia in adolescents has been found to be related to higher rates of substance abuse, depression, and suicide completion—both overall and when sleep patterns from the week prior to suicide are isolated and analyzed.13 Another study14 found that when suicide completers were compared to matched controls, the completers exhibited greater insomnia over the week prior to suicide. Likewise, self-reported insomnia has been shown to associate with suicidal ideation in military personnel, even after controlling for symptoms of depression, hopelessness, posttraumatic stress disorder diagnosis, anxiety symptoms, and drug and alcohol abuse.15 Prison populations are often plagued by both insomnia and suicide. Existing literature indicates that in prison populations, insomnia is related to both a lifetime history of suicidal ideation and current suicidal ideation.8 Those misusing alcohol also are at a higher risk of both suicide16 and insomnia.17–19 Insomnia symptoms in alcohol misusers have been associated with alcohol consumption, cigarette smoking, psychiatric disturbance, and the subject’s age.20
Clarifying the role of insomnia as a risk factor for suicide is imperative10 and may improve suicide risk assessment, suicide prediction, and future treatments. Factors contributing to the paucity of such research include the use of nonstandard and understudied definitions of insomnia,21,22 nonstandardized instruments for the measurement of insomnia, the reliance on nonrepresentative samples such as the special populations previously mentioned, and a lack of attention to factors related to insomnia (such as sleep duration). Literature from some large-scale studies11,12,23 indicates that self-reported difficulty initiating sleep, maintaining sleep, and early morning awakening significantly relate to suicidal ideation. However, such studies focused on insomnia while neglecting sleep duration. Sleep duration is a relevant variable, as both extremes (short and long) are associated with depression.24,25 Short sleep duration has been associated with insomnia in the general population,26 as well as in those with psychiatric symptoms27 and suicidal ideation.9 Furthermore, data have shown an association between suicidal ideation and increased sleep duration on weekends in Korean adolescents.28,29 Moreover, although extreme sleep duration has been linked to depression, there are few studies that reported the relationship between sleep duration and suicidal ideation, especially at the population level.
Accordingly, the present study examined a nationally representative sample in order to assess the association of sleep duration and suicidal ideation, while concurrently taking into account insomnia (construed as initial, middle, and late), using data from the National Health and Nutritional Examination Survey (NHANES).30 Specifically, the present study examined whether abnormal sleep duration and insomnia symptoms were associated with suicidal ideation among participants in the 2007–2008 NHANES survey. It was hypothesized that extreme sleep durations (short or long) would be significantly associated with suicidal ideation in the respondents. It was also hypothesized that overall insomnia and insomnia symptoms (difficulty falling asleep, difficulty maintaining sleep, and early morning awakenings) would be linked with suicidal ideation, even after adjusting for comorbid depression.
METHOD
Data Source
The participants used in this study were also participants in the 2007–2008 NHANES, a national survey conducted by the Centers for Disease Control and Prevention reporting the health and nutritional characteristics of children and adults.30 As NHANES is a general health survey, it is believed that participants do not exhibit the self-selection bias that may have been present in some previous studies. Participants were administered questionnaires concerning their demographic, socioeconomic, nutritional, and related statuses during in-person interviews conducted in the home. The unweighted response rate for the total sample was 78.4%. Sampling and weighting procedures were performed to ensure generalizability to the entire US population. In order to compensate for underrepresentation, blacks, Hispanics, and adults over age 60 years were oversampled.
Sampling in this survey was performed to ensure generalizability to the entire US population across all ages. Because of the complexity of the survey design coupled with variable probabilities of selection, the data used in the following analyses also were weighted to control for representativeness by following the procedures outlined in the current NHANES Analytic and Reporting Guidelines.31
Measures
Suicidal ideation.
Suicidal ideation was assessed with the survey item, “Over the last 2 weeks, how often have you been bothered by the following problem: thoughts that you would be better off dead or of hurting yourself in some way?” Responses were categorized as “not at all,” “several days,” “more than half the days,” or “nearly every day.” Although this item assesses more passive (versus active) thoughts of the wish to die or self-harm, a previous study32 showed that many of those who endorse this item also endorse recent thoughts of hurting or killing themselves (more active suicidal ideation).
Depressive disorder.
The 9-item Patient Health Questionnaire,33 a well-validated tool for depression screening, was used to screen for depressive disorder. Probable depression diagnosis was evaluated using the standard algorithm, which involved assessing for the presence of depressed mood or anhedonia more than half of the days in the past 2 weeks, as well as the presence of at least 5 symptoms (including suicidal ideation) more than half of the days in the past 2 weeks and a report that these symptoms interfere with functioning. Likely depression was coded as “no” or “yes.”
Sleep duration.
Sleep duration was assessed with the survey item, “How much sleep do you usually get at night on weekdays or workdays?” Responses were coded as whole numbers in hours. These responses were used to generate the following categories: <5 hours, 5 hours, 6 hours, 7 hours, 8 hours, 9 hours, and > 9 hours. These categories were chosen so that independent effects of short and long sleep duration could be examined, as both extremes are associated with depression.24,25
Insomnia symptoms.
Insomnia symptoms were operationalized as difficulty falling asleep, difficulty maintaining sleep, and early daytime awakening, as they represent hallmark symptoms of insomnia.34 Difficulty falling asleep was assessed with the item, “In the past month, how often did you have trouble falling asleep?” Difficulty maintaining sleep was assessed with the item, “In the past month, how often did you wake up during the night and had trouble getting back to sleep?” Early morning awakenings were assessed with the item, “In the past month, how often did you wake up too early in the morning and were unable to get back to sleep?” Responses were coded in whole numbers and categorized as “never,” “rarely: 1 time a month,” “sometimes: 2–4 times a month,” “often: 5–15 times a month,” and “always: 16–30 times a month.”
A global insomnia measure called “overall insomnia” also was developed. Overall insomnia is a severity measure derived from additive scoring of the 3 hallmark symptoms mentioned previously and is continuous in nature, with a potential range of 0–12.
Sociodemographic, socioeconomic, and health covariates.
A number of potential confounders were assessed. These confounders included age, sex, race/ethnicity (non-Hispanic white, Hispanic/Latino, black/African-American, and Asian/other), household income (< $20,000, $20,000–$24,999, $25,000–$34,999, $35,000–$44,999, $45,000–$54,999, $55,000–$64,999, $65,000–$75,000, and > $75,000), education (< 9th grade, 9th to 11th grade, high school graduate, some college, and college graduate), marital status, physical activity, smoking habits, and alcohol use. These variables were specifically chosen because they all are likely confounders.35
Statistical Analyses
Differences in sociodemographic, socioeconomic, and health covariates; depression symptoms; insomnia symptoms; and sleep duration between suicidal ideation groups were assessed using analysis of variance for continuous variables and Pearson χ2 for categorical variables. Continuous variables were expressed in terms of mean ± SD, while categorical variables were expressed as percentages.
The effects of sleep duration and insomnia symptoms on suicidal ideation were assessed using ordinal logistic regression. A total of 3 separate regression models were evaluated. Model 1 evaluated the crude relationships of individual insomnia symptoms and sleep duration (unadjusted). Model 2 evaluated relationships after adjustment for all sociodemographic, socioeconomic, and health covariates (adjusted). Model 3 evaluated relationships after adjustment for all model 2 variables, as well as depression (overcontrolled). Odds ratios and 95% confidence intervals were reported, and a 2-tailed P value < .05 was considered significant for evaluating each independent variable. STATA/IC version 12 (STATA Corp, College Station, Texas) was used to perform all statistical calculations.
RESULTS
Sample Characteristics
For the present study, analyses included adults aged ≥ 18 with complete data on all independent and dependent variables (N = 6,228). Characteristics of the sample are reported in Table 1. All cases were weighted, resulting in a sample that was closely matched to the general population. Suicidal ideation categories were, however, differentially distributed across sociodemographic, socioeconomic, and health variables, justifying their inclusion as covariates.
Table 1.
Characteristics of the Sample (weighted) Combined and Stratified by Suicidal Ideationa
| Variable | Category | Overall Sample | Suicidal Ideation |
||||
| Not at All (n = 5,191) | Several Days (n = 177) | More Than Half the Days (n = 33) | Nearly Every Day (n = 40) | Pb | |||
| Age (y) | Continuous | 45.760 ± 17.224 | 45.642 ± 16.951 | 47.176 ± 19.789 | 42.957 ± 19.452 | 45.530 ± 19.965 | .676 |
| Sex | Male | 0.52 | 0.51 | 0.49 | 0.58 | 0.51 | .889 |
| Female | 0.48 | 0.49 | 0.51 | 0.42 | 0.49 | ||
| Race | Non-Hispanic white | 0.69 | 0.70 | 0.61 | 0.55 | 0.63 | .003 |
| Hispanic/Latino | 0.13 | 0.13 | 0.24 | 0.26 | 0.22 | ||
| Black/African-American | 0.11 | 0.11 | 0.12 | 0.17 | 0.16 | ||
| Asian/other | 0.06 | 0.05 | 0.04 | 0.02 | 0.00 | ||
| Income (US $) | < $20,000 | 0.16 | 0.15 | 0.34 | 0.45 | 0.47 | < .001 |
| 20,000–$24,999 | 0.07 | 0.07 | 0.12 | 0.16 | 0.24 | ||
| 25,000–$34,999 | 0.11 | 0.11 | 0.15 | 0.09 | 0.25 | ||
| 35,000–$44,999 | 0.09 | 0.09 | 0.08 | 0.09 | 0.00 | ||
| 45,000–$54,999 | 0.08 | 0.09 | 0.05 | 0.04 | 0.01 | ||
| 55,000–$64,999 | 0.07 | 0.07 | 0.07 | 0.03 | 0.03 | ||
| 65,000–$75,000 | 0.07 | 0.08 | 0.06 | 0.02 | 0.00 | ||
| > $75,000 | 0.33 | 0.34 | 0.12 | 0.12 | 0.00 | ||
| Education | < 9th grade | 0.07 | 0.06 | 0.16 | 0.22 | 0.23 | < .001 |
| 9th–11th grade | 0.14 | 0.13 | 0.16 | 0.32 | 0.29 | ||
| High school graduate | 0.25 | 0.25 | 0.26 | 0.22 | 0.11 | ||
| Some college | 0.29 | 0.29 | 0.32 | 0.23 | 0.37 | ||
| College graduate | 0.25 | 0.26 | 0.11 | 0.01 | 0.00 | ||
| Marital status | Married | 0.57 | 0.58 | 0.38 | 0.30 | 0.33 | < .001 |
| Widowed | 0.06 | 0.05 | 0.09 | 0.12 | 0.05 | ||
| Divorced | 0.10 | 0.10 | 0.13 | 0.19 | 0.17 | ||
| Separated | 0.02 | 0.02 | 0.04 | 0.09 | 0.14 | ||
| Never married | 0.18 | 0.17 | 0.25 | 0.20 | 0.26 | ||
| Living with partner | 0.07 | 0.07 | 0.11 | 0.11 | 0.05 | ||
| Exercise (min) | Continuous | 166.06 ± 221.64 | 168.59 ± 220.19 | 113.99 ± 213.78 | 156.21 ± 267.98 | 134.29 ± 276.23 | .018 |
| Sedentary activity (min) | Continuous | 334.62 ± 206.86 | 333.86 ± 204.46 | 319.26 ± 235.30 | 345.19 ± 259.41 | 270.91 ± 208.97 | .278 |
| Ever smoked | No | 0.53 | 0.53 | 0.51 | 0.23 | 0.23 | .001 |
| Yes | 0.47 | 0.47 | 0.49 | 0.77 | 0.77 | ||
| Type of smoker | Never smoker | 0.53 | 0.53 | 0.51 | 0.23 | 0.23 | < .001 |
| Current smoker | 0.23 | 0.22 | 0.34 | 0.70 | 0.53 | ||
| Former smoker | 0.24 | 0.25 | 0.15 | 0.07 | 0.24 | ||
| Alcohol use (no. of drinks/d) | Continuous | 2.82 ± 2.76 | 2.81 ± 2.75 | 3.08 ± 2.71 | 3.94 ± 2.83 | 4.43 ± 4.70 | .049 |
| Alcohol use (no. of days ≥ 5 drinks) | Continuous | 2.50 ± 2.37 | 2.48 ± 2.11 | 3.72 ± 3.66 | 1.69 ± 3.05 | 3.38 ± 9.09 | .708 |
| Depression | No | 0.98 | 0.98 | 0.79 | 0.65 | 0.23 | < .001 |
| Yes | 0.02 | 0.02 | 0.21 | 0.35 | 0.77 | ||
| Overall insomnia | Continuous | 3.78 ± 3.23 | 3.77 ± 3.17 | 5.81 ± 4.07 | 4.74 ± 4.21 | 6.33 ± 4.48 | < .001 |
| Difficulty falling asleep | Never | 0.39 | 0.38 | 0.22 | 0.23 | 0.17 | < .001 |
| Rarely | 0.21 | 0.22 | 0.15 | 0.31 | 0.12 | ||
| Sometimes | 0.22 | 0.22 | 0.22 | 0.19 | 0.15 | ||
| Often | 0.11 | 0.11 | 0.21 | 0.04 | 0.23 | ||
| Always | 0.08 | 0.07 | 0.21 | 0.23 | 0.34 | ||
| Difficulty maintaining sleep | Never | 0.36 | 0.36 | 0.19 | 0.37 | 0.24 | < .001 |
| Rarely | 0.20 | 0.20 | 0.09 | 0.11 | 0.16 | ||
| Sometimes | 0.24 | 0.24 | 0.36 | 0.16 | 0.16 | ||
| Often | 0.13 | 0.13 | 0.20 | 0.23 | 0.28 | ||
| Always | 0.08 | 0.08 | 0.16 | 0.13 | 0.16 | ||
| Early morning awakenings | Never | 0.45 | 0.44 | 0.30 | 0.42 | 0.25 | < .001 |
| Rarely | 0.19 | 0.19 | 0.13 | 0.11 | 0.19 | ||
| Sometimes | 0.20 | 0.21 | 0.24 | 0.22 | 0.17 | ||
| Often | 0.10 | 0.10 | 0.21 | 0.18 | 0.15 | ||
| Always | 0.06 | 0.06 | 0.12 | 0.07 | 0.23 | ||
| Sleep duration (h) | < 5 | 0.05 | 0.05 | 0.14 | 0.15 | 0.17 | < .001 |
| 5 | 0.09 | 0.09 | 0.10 | 0.09 | 0.10 | ||
| 6 | 0.23 | 0.23 | 0.21 | 0.24 | 0.18 | ||
| 7 | 0.29 | 0.30 | 0.22 | 0.12 | 0.14 | ||
| 8 | 0.26 | 0.26 | 0.25 | 0.36 | 0.36 | ||
| 9 | 0.05 | 0.05 | 0.04 | 0.04 | 0.00 | ||
| > 9 | 0.02 | 0.02 | 0.04 | 0.01 | 0.06 | ||
Continuous variables are presented as mean ± SD, and categorical variables are presented as %. Univariate tests include 1-way analysis of variance for continuous variables and χ2 tests for categorical variables.
Bolding indicates statistical significance.
Sleep Duration
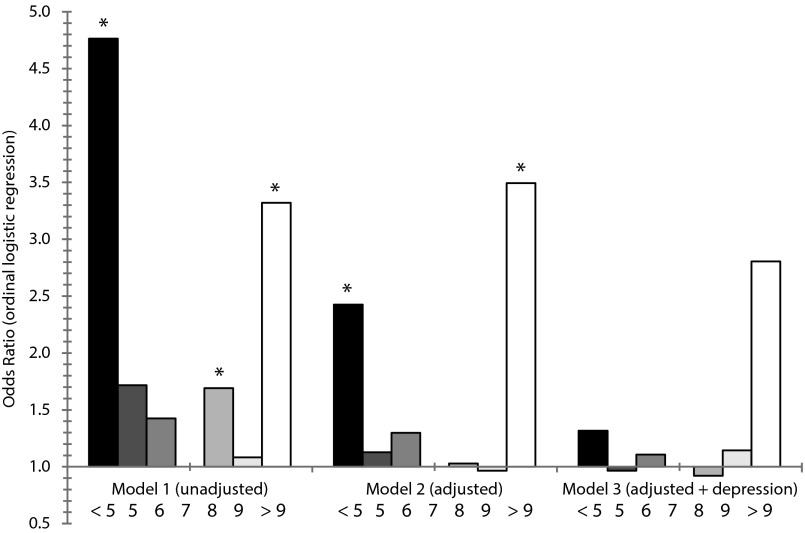
Sleep duration < 5 hours or > 9 hours (vs 7 hours) was associated with higher suicidal ideation in model 1 (unadjusted) and model 2 (adjusted). Sleep duration of 8 hours (vs 7 hours) was associated with higher suicidal ideation in unadjusted analyses only. These results are displayed graphically in Figure 1.
Figure 1.
Sleep Duration Associated With Suicidal Ideation Across 3 Models (reference = 7 h)
*P < .05.
Insomnia Symptoms
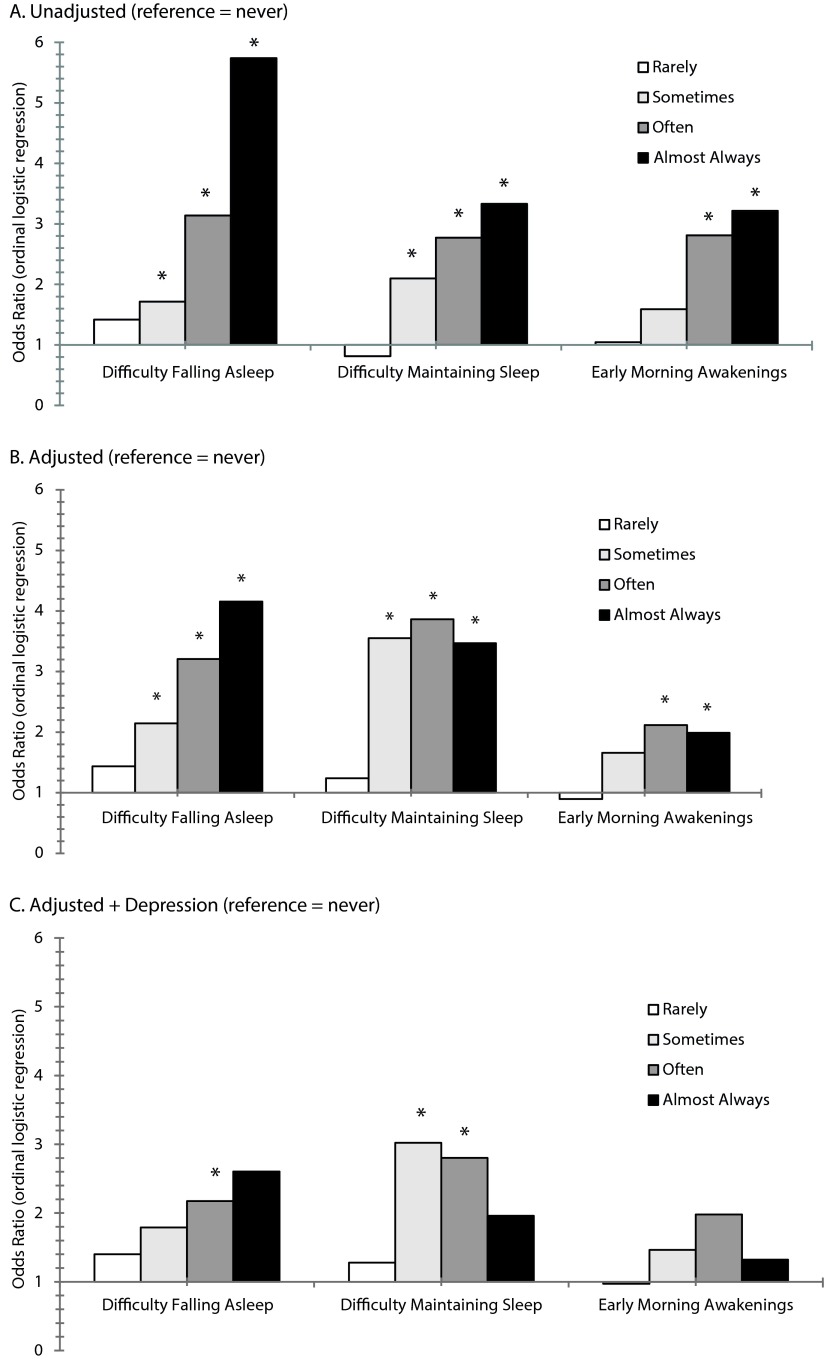
Results from unadjusted, adjusted, and overcontrolled logistic regression analyses are reported in Table 2. In all models, including the unadjusted, adjusted, and overcontrolled model, increased overall insomnia was associated with higher level of suicidal ideation. Regarding specific insomnia symptoms, in both unadjusted (model 1) and adjusted (model 2) analyses, increased suicidal ideation was associated with difficulty falling asleep (sometimes, often, or almost always), difficulty maintaining sleep (sometimes, often, or almost always), and early morning awakenings. In the overcontrolled model (model 3), elevated suicidal ideation was still associated with difficulty falling asleep (although only the “often” category) and difficulty maintaining sleep (although only the “sometimes” and “often” categories). These results are displayed graphically in Figure 2.
Table 2.
Odds Ratios and 95% Confidence Intervals Reflecting Associations Between Suicide Ideation and Sleep Variables Across 3 Modelsa
| Model 1: Unadjusted |
Model 2: Adjusted |
Model 3: Overcontrolled |
||||||||
| Variable | Category | Odds Ratio | 95% CI | P | Odds Ratio | 95% CI | P | Odds Ratio | 95% CI | Pb |
| Sleep duration (h) (reference = 7 h) | < 5 | 4.76 | 2.76–8.21 | < .001 | 2.43 | 1.21–4.86 | .013 | 1.32 | 0.56–3.09 | .527 |
| 5 | 1.72 | 0.93–3.16 | .082 | 1.13 | 0.44–2.89 | .802 | 0.97 | 0.33–2.81 | .950 | |
| 6 | 1.43 | 0.86–2.36 | .167 | 1.30 | 0.67–2.51 | .436 | 1.11 | 0.55–2.22 | .776 | |
| 7 | Reference | Reference | Reference | |||||||
| 8 | 1.69 | 1.02–2.80 | .041 | 1.03 | 0.51–2.09 | .939 | 0.92 | 0.45–1.89 | .823 | |
| 9 | 1.08 | 0.29–4.09 | .908 | 0.97 | 0.16–5.90 | .971 | 1.14 | 0.18–7.18 | .886 | |
| > 9 | 3.32 | 1.55–7.11 | .002 | 3.49 | 1.31–9.32 | .013 | 2.81 | 0.98–8.07 | .056 | |
| Overall insomnia | 1-unit increase | 1.18 | 1.13–1.24 | < .001 | 1.16 | 1.09–1.24 | < .001 | 1.11 | 1.03–1.18 | .003 |
| Difficulty falling asleep (reference = never) | Never | Reference | Reference | Reference | ||||||
| Rarely | 1.42 | 0.83–2.42 | .203 | 1.44 | 0.69–2.99 | .331 | 1.40 | 0.66–2.96 | .376 | |
| Sometimes | 1.72 | 1.04–2.82 | .033 | 2.15 | 1.05–4.39 | .036 | 1.79 | 0.88–3.67 | .110 | |
| Often | 3.14 | 1.91–5.16 | < .001 | 3.21 | 1.62–6.34 | .001 | 2.18 | 1.06–4.48 | .035 | |
| Almost always | 5.74 | 3.48–9.45 | < .001 | 4.16 | 1.81–9.53 | .001 | 2.60 | 0.94–7.22 | .066 | |
| Difficulty maintaining sleep (reference = never) | Never | Reference | Reference | Reference | ||||||
| Rarely | 0.82 | 0.46–1.46 | .491 | 1.24 | 0.57–2.71 | .587 | 1.28 | 0.59–2.77 | .534 | |
| Sometimes | 2.10 | 1.31–3.36 | .002 | 3.55 | 1.80–7.00 | < .001 | 3.02 | 1.45–6.29 | .003 | |
| Often | 2.77 | 1.74–4.42 | < .001 | 3.86 | 1.92–7.79 | < .001 | 2.80 | 1.39–5.64 | .004 | |
| Almost always | 3.33 | 1.99–5.56 | < .001 | 3.47 | 1.64–7.34 | .001 | 1.96 | 0.91–4.24 | .087 | |
| Early morning awakenings (reference = never) | Never | Reference | Reference | Reference | ||||||
| Rarely | 1.04 | 0.61–1.78 | .876 | 0.90 | 0.46–1.76 | .747 | 0.97 | 0.50–1.90 | .931 | |
| Sometimes | 1.59 | 0.99–2.54 | .053 | 1.66 | 0.89–3.09 | .110 | 1.46 | 0.73–2.95 | .288 | |
| Often | 2.81 | 1.77–4.46 | < .001 | 2.12 | 1.03–4.36 | .042 | 1.98 | 0.97–4.03 | .061 | |
| Almost always | 3.22 | 1.93–5.36 | < .001 | 1.99 | 1.00–3.94 | .049 | 1.32 | 0.61–2.86 | .477 | |
Model 1 is unadjusted. Model 2 includes age, sex, race/ethnicity, income, education, marital status, exercise, sedentary activity, smoking, and alcohol use. Model 3 includes all model 2 variables and depressive symptoms.
Bolding indicates statistical significance.
Figure 2.
Insomnia Symptoms Associated With Suicidal Ideation Across 3 Models
*P < .05.
DISCUSSION
Suicidal ideation has been repeatedly linked with insomnia in previous studies,36–38 some above and beyond the effects of depression. Emerging evidence also has associated suicidal ideation with abnormalities of sleep duration.11,12,23 The present study sought to explore this relationship of suicidal ideation with abnormalities of sleep duration at a population level using nationally representative data from a diverse sample of adults aged ≥ 18 years. In addition, this study also concurrently sought to reevaluate the relationship between insomnia symptoms and suicidal ideation among NHANES survey respondents.
As expected, increased suicidal ideation was found in the non-Hispanic white group, as well as in those with lower socioeconomic status. Interestingly, higher suicide symptoms were seen in those who were married, had a relatively more sedentary lifestyle, used psychoactive substances, and reported depressive symptoms. A higher risk of suicidal ideation was associated with extremes of sleep duration with the contours of a U-shaped distribution. Overall, insomnia was consistently found to be associated with increased level of suicidal ideation. Of the 3 types of insomnia, difficulty maintaining sleep was found to be the most predictive of suicidal ideation, followed by difficulty initiating sleep. Early morning awakening, while thought to be a cardinal sign of depression, was not found to be related to suicidal ideation after adjusting for covariates.
The observed relationships between the demographic covariates and suicidal ideation were generally in line with those seen in prior studies. For example, problematic marital relationships may have been associated with suicidal ideation because of associated underlying psychiatric symptoms with and without substance use.39,40 Further, smoking may be related to suicidal ideation due to underlying psychiatric symptoms,41 and the association of alcohol consumption with suicidal ideation is in line with prior literature.16,18
The association of suicidal ideation with sleep duration demonstrated a U-shaped distribution in the unadjusted model as well as the model adjusted for covariates, such that the highest risk is seen in those reporting sleep durations of < 5 and > 9 hours a day. This pattern was similar to the U-shaped distribution of the hazard ratios for mortality and sleep duration seen in prior literature.42–44 Similar U-shaped distributions also have been seen for the association of sleep duration with percent body fat,45 hemoglobin A1C levels,46 Type 2 diabetes, or impaired glucose tolerance,47 as well as for sleep time exchanged for waking activities.48 Although both short and long sleep duration have been associated with depressive disorder,49–52 only 1 study has demonstrated a U-shaped distribution.50 It is therefore plausible that the association of suicidal ideation and sleep duration may have a similar U-shaped distribution as demonstrated in this study.
Both short and long sleep durations were associated with suicidal ideation in the unadjusted model as well as in the model adjusted for most of the covariates. But, sleep duration was no longer a significant variable after adjusting for depression. This finding is consistent with prior literature showing that increased sleep duration on weekends among Korean adolescents was associated with suicidal ideation,28 as well as the relationship of suicidal ideation with abnormalities in sleep duration in veterans misusing alcohol,53 and extends the literature in the general population from short sleep duration9 to short and long sleep duration. This relationship between sleep duration and suicidal ideation is largely explained by underlying depressive symptoms as suggested previously.24,25
While it is true that the variance is explained by depression, this finding shows that sleep duration as a marker for suicidal ideation may have some clinical utility, as patients may be more willing to endorse extreme sleep duration than depressive (or suicidal) symptoms. In addition, the presence of short and long sleep duration may be a predictor of a more chronic course of the associated depressive disorder as demonstrated in a recent study.52
These results also replicate the findings from prior epidemiologic studies wherein the presence of individual insomnia symptoms was associated with a higher intensity of suicidal ideation.12,54–59 In an overfitted model including depression, 2 of the 3 hallmark insomnia symptoms, difficulty falling asleep and difficulty maintaining sleep, were still significantly associated with higher suicidal ideation. However, the strength of the association was attenuated. The attenuation suggests that the risk for suicidal ideation conferred by depression partially subsumes the risk conferred by insomnia symptoms. These findings are consistent with prior literature in which insomnia symptoms such as difficulty falling asleep and nonrestorative sleep have been associated with suicidal ideation, suicide attempts, or death by suicide, as well as their association with depressive symptoms using data from population samples across studies from multiple nations.7,23,54–58 Despite the association of insomnia symptoms with depressive disorder, it is important to note that insomnia symptoms still independently confer a significantly higher risk of suicidal ideation. This association was demonstrated in a recent study59 in which treatment with cognitive-behavioral therapy for insomnia decreased suicidal ideation in patients with insomnia, even after adjusting for severity of depression and other relevant covariates.
Limitations
The present study involves a cross-sectional analysis of survey items. Consequently, the significant association between insomnia and suicidal ideation does not establish a causal relationship between these variables. Second, the NHANES depression questionnaire includes items that refer to subjective symptoms. These survey items are not the “gold-standard” assessments nor are they clinically diagnostic. However, a previous study32 has shown that many of those individuals who endorse this item also endorse recent thoughts of hurting or killing themselves (more active suicidal ideation). Third, no data were available on nightmares or dysfunctional attitudes and beliefs regarding sleep in these respondents. Nightmare as a symptom is important, as its frequency and duration may be independent risk factors for suicide.60,61 Further, nightmares and dysfunctional attitudes and beliefs about sleep may mediate the relationship between insomnia and suicidal ideation as demonstrated previously.62 Finally, the NHANES questionnaire did not adequately assess acute versus chronic insomnia. The data presented reflect acute insomnia symptoms and do not reflect the chronicity of the symptoms. It is arguable whether the present results will hold true over the course of chronic insomnia. Future research may seek to explore this possibility prospectively or retrospectively.
CONCLUSIONS
In a population-weighted, nationally representative sample of American adults, increased suicidal ideation was associated with abnormalities of sleep duration and insomnia symptoms. Further, this relationship persisted after adjustment for a number of potential confounders, including demographics, socioeconomics, and other health risk factors. The relationship of suicidal ideation with insomnia symptoms of difficulty falling asleep and difficulty maintaining sleep persisted after adjustment for variance contributed by likely depression diagnosis (which is highly associated with both insomnia and suicidal ideation). In addition, certain insomnia symptoms (eg, difficulty maintaining sleep) were more strongly associated with suicidal ideation than others (eg, early morning awakenings). Taken together, these findings suggest that abnormalities of sleep duration and insomnia experienced in the general population are associated with increased levels of suicidal ideation. This relationship has clinical and research-related implications. Since abnormalities of sleep duration and insomnia have now been associated with suicidal ideation in multiple epidemiologic studies, clinical assessments for suicide risk should include an evaluation for these symptoms in addition to other known suicide risk factors.
Disclosure of off-label usage:
The authors have determined that, to the best of their knowledge, no investigational information about pharmaceutical agents that is outside US Food and Drug Administration–approved labeling has been presented in this article.
Financial disclosure:
Drs Chakravorty, Siu, Brown, Findley, Perlis, and Grandner and Ms Lalley-Chareczko have no personal affiliations or financial relationships with any commercial interest to disclose relevant to the article.
Funding/support:
This study was supported by Veterans Affairs grant IK2CX000855 (Dr Chakravorty) and National Institutes of Health grants K23HL110216, 12SDG9180007, R01AT003332, and R01MH077900 and the University of Pennsylvania (CTSA UL1RR024134).
Role of the sponsors:
The Centers for Disease Control and Prevention provided public access to the NHANES survey data. The data analysis and preparation of this manuscript were possible due to support from the above-mentioned grant funding sources.
Disclaimer:
The content of this publication does not represent the views of the Department of Veterans Affairs, United States Government, University of Pennsylvania, or any other institution.
Footnotes
CME Background
Articles are selected for credit designation based on an assessment of the educational needs of CME participants, with the purpose of providing readers with a curriculum of CME articles on a variety of topics throughout each volume. Activities are planned using a process that links identified needs with desired results.
To obtain credit, read the article, correctly answer the questions in the Posttest, and complete the Evaluation. The Posttest and Evaluation are available at http://www.cmeinstitute.com/activities/Pages/journal.aspx.
CME Objective
After studying this article, you should be able to:
• Assess patients with sleep disturbances for suicidality
Accreditation Statement
The CME Institute of Physicians Postgraduate Press, Inc., is accredited by the Accreditation Council for Continuing Medical Education to provide continuing medical education for physicians.
Credit Designation
The CME Institute of Physicians Postgraduate Press, Inc., designates this journal-based CME activity for a maximum of 1.0 AMA PRA Category 1 Credit™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Note: The American Academy of Physician Assistants (AAPA) accepts certificates of participation for educational activities certified for AMA PRA Category 1 Credit™ from organizations accredited by ACCME or a recognized state medical society. Physician assistants may receive a maximum of 1.0 hour of Category I credit for completing this program.
Date of Original Release/Review
This educational activity is eligible for AMA PRA Category 1 Credit™ through December 31, 2017. The latest review of this material was December 2015.
Financial Disclosure
All individuals in a position to influence the content of this activity were asked to complete a statement regarding all relevant personal financial relationships between themselves or their spouse/partner and any commercial interest. The CME Institute has resolved any conflicts of interest that were identified. In the past year, Larry Culpepper, MD, MPH, Editor in Chief, has been a member of the speakers/advisory boards for AstraZeneca, Forest, Jazz, Lundbeck, Merck, Shire, Sunovion, and Takeda; has been a stock shareholder of M3 My Mood Monitor; and has received royalties from UpToDate and other financial or material support from Oxford University Press. No member of the CME Institute staff reported any relevant personal financial relationships. Faculty financial disclosure appears with the article.
References
- 1.Heron M. Deaths: leading causes for 2008. Natl Vital Stat Rep. 2012;60(6):1–94. [PubMed] [Google Scholar]
- 2.Arsenault-Lapierre G, Kim C, Turecki G. Psychiatric diagnoses in 3,275 suicides: a meta-analysis. BMC Psychiatry. 2004;4(1):37. doi: 10.1186/1471-244X-4-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mann JJ, Ellis SP, Waternaux CM, et al. Classification trees distinguish suicide attempters in major psychiatric disorders: a model of clinical decision making. J Clin Psychiatry. 2008;69(1):23–31. doi: 10.4088/jcp.v69n0104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brown GK, Beck AT, Steer RA, et al. Risk factors for suicide in psychiatric outpatients: a 20-year prospective study. J Consult Clin Psychol. 2000;68(3):371–377. [PubMed] [Google Scholar]
- 5.Yang AC, Tsai SJ, Huang NE, et al. Association of Internet search trends with suicide death in Taipei City, Taiwan, 2004–2009. J Affect Disord. 2011;132(1–2):179–184. doi: 10.1016/j.jad.2011.01.019. [DOI] [PubMed] [Google Scholar]
- 6.Krakow B, Ribeiro JD, Ulibarri VA, et al. Sleep disturbances and suicidal ideation in sleep medical center patients. J Affect Disord. 2011;131(1–3):422–427. doi: 10.1016/j.jad.2010.12.001. [DOI] [PubMed] [Google Scholar]
- 7.Bjørngaard JH, Bjerkeset O, Romundstad P, et al. Sleeping problems and suicide in 75,000 Norwegian adults: a 20-year follow-up of the HUNT I study. Sleep. 2011;34(9):1155–1159. doi: 10.5665/SLEEP.1228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Carli V, Roy A, Bevilacqua L, et al. Insomnia and suicidal behavior in prisoners. Psychiatry Res. 2011;185(1–2):141–144. doi: 10.1016/j.psychres.2009.10.001. [DOI] [PubMed] [Google Scholar]
- 9.Goodwin RD, Marusic A. Association between short sleep and suicidal ideation and suicide attempt among adults in the general population. Sleep. 2008;31(8):1097–1101. [PMC free article] [PubMed] [Google Scholar]
- 10.McCall WV. Insomnia is a risk factor for suicide: what are the next steps? Sleep. 2011;34(9):1149–1150. doi: 10.5665/SLEEP.1222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chellappa SL, Araújo JF. Sleep disorders and suicidal ideation in patients with depressive disorder. Psychiatry Res. 2007;153(2):131–136. doi: 10.1016/j.psychres.2006.05.007. [DOI] [PubMed] [Google Scholar]
- 12.Wojnar M, Ilgen MA, Wojnar J, et al. Sleep problems and suicidality in the National Comorbidity Survey Replication. J Psychiatr Res. 2009;43(5):526–531. doi: 10.1016/j.jpsychires.2008.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Roane BM, Taylor DJ. Adolescent insomnia as a risk factor for early adult depression and substance abuse. Sleep. 2008;31(10):1351–1356. [PMC free article] [PubMed] [Google Scholar]
- 14.Goldstein TR, Bridge JA, Brent DA. Sleep disturbance preceding completed suicide in adolescents. J Consult Clin Psychol. 2008;76(1):84–91. doi: 10.1037/0022-006X.76.1.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ribeiro JD, Pease JL, Gutierrez PM, et al. Sleep problems outperform depression and hopelessness as cross-sectional and longitudinal predictors of suicidal ideation and behavior in young adults in the military. J Affect Disord. 2012;136(3):743–750. doi: 10.1016/j.jad.2011.09.049. [DOI] [PubMed] [Google Scholar]
- 16.Rossow I. Regional analyses of alcohol and suicide in Norway: some empirical considerations. Suicide Life Threat Behav. 1995;25(3):401–409. [PubMed] [Google Scholar]
- 17.Baekeland F, Lundwall L, Shanahan TJ, et al. Clinical correlates of reported sleep disturbance in alcoholics. Q J Stud Alcohol. 1974;35(4 Pt A):1230–1241. [PubMed] [Google Scholar]
- 18.Dhossche DM, Meloukheia AM, Chakravorty S. The association of suicide attempts and comorbid depression and substance abuse in psychiatric consultation patients. Gen Hosp Psychiatry. 2000;22(4):281–288. doi: 10.1016/s0163-8343(00)00085-2. [DOI] [PubMed] [Google Scholar]
- 19.Foster JH, Peters TJ. Impaired sleep in alcohol misusers and dependent alcoholics and the impact upon outcome. Alcohol Clin Exp Res. 1999;23(6):1044–1051. [PubMed] [Google Scholar]
- 20.Chakravorty S, Grandner MA, Kranzler HR, et al. Insomnia in alcohol dependence: predictors of symptoms in a sample of veterans referred from primary care. Am J Addict. 2013;22(3):266–270. doi: 10.1111/j.1521-0391.2012.12009.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Edinger JD, Bonnet MH, Bootzin RR, et al. American Academy of Sleep Medicine Work Group. Derivation of research diagnostic criteria for insomnia: report of an American Academy of Sleep Medicine Work Group. Sleep. 2004;27(8):1567–1596. doi: 10.1093/sleep/27.8.1567. [DOI] [PubMed] [Google Scholar]
- 22.Ohayon MM. Epidemiology of insomnia: what we know and what we still need to learn. Sleep Med Rev. 2002;6(2):97–111. doi: 10.1053/smrv.2002.0186. [DOI] [PubMed] [Google Scholar]
- 23.Brower KJ, McCammon RJ, Wojnar M, et al. Prescription sleeping pills, insomnia, and suicidality in the National Comorbidity Survey Replication. J Clin Psychiatry. 2011;72(4):515–521. doi: 10.4088/JCP.09m05484gry. [DOI] [PubMed] [Google Scholar]
- 24.Grandner MA, Patel NP, Gehrman PR, et al. Problems associated with short sleep: bridging the gap between laboratory and epidemiological studies. Sleep Med Rev. 2010;14(4):239–247. doi: 10.1016/j.smrv.2009.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Grandner MA, Drummond SP. Who are the long sleepers? towards an understanding of the mortality relationship. Sleep Med Rev. 2007;11(5):341–360. doi: 10.1016/j.smrv.2007.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Grandner MA, Kripke DF. Self-reported sleep complaints with long and short sleep: a nationally representative sample. Psychosom Med. 2004;66(2):239–241. doi: 10.1097/01.psy.0000107881.53228.4d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Vgontzas AN, Fernandez-Mendoza J, Bixler EO, et al. Persistent insomnia: the role of objective short sleep duration and mental health. Sleep. 2012;35(1):61–68. doi: 10.5665/sleep.1586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lee YJ, Cho SJ, Cho IH, et al. Insufficient sleep and suicidality in adolescents. Sleep. 2012;35(4):455–460. doi: 10.5665/sleep.1722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gau SS, Shang CY, Merikangas KR, et al. Association between morningness-eveningness and behavioral/emotional problems among adolescents. J Biol Rhythms. 2007;22(3):268–274. doi: 10.1177/0748730406298447. [DOI] [PubMed] [Google Scholar]
- 30.Centers for Disease Control and Prevention; US Department of Health and Human Services. National Health and Nutrition Examination Survey Data. Hyattsville, MD: National Center for Health Statistics; 2008. [Google Scholar]
- 31.Centers for Disease Control and Prevention. Hyattsville, MD: National Center for Health Statistics; 2006. Analytic and Reporting Guidelines: The National Health and Nutrition Examination Survey (NHANES) [Google Scholar]
- 32.Corson K, Gerrity MS, Dobscha SK. Screening for depression and suicidality in a VA primary care setting: 2 items are better than 1 item. Am J Manag Care. 2004;10(11 Pt 2):839–845. [PubMed] [Google Scholar]
- 33.Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA. 1999;282(18):1737–1744. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- 34.Morin CM, Benca RM. Insomnia nature, diagnosis, and treatment. Handb Clin Neurol. 2011;99:723–746. doi: 10.1016/B978-0-444-52007-4.00004-7. [DOI] [PubMed] [Google Scholar]
- 35.Grandner MA, Patel NP, Gehrman PR, et al. Who gets the best sleep? ethnic and socioeconomic factors related to sleep complaints. Sleep Med. 2010;11(5):470–478. doi: 10.1016/j.sleep.2009.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Buysse DJ, Angst J, Gamma A, et al. Prevalence, course, and comorbidity of insomnia and depression in young adults. Sleep. 2008;31(4):473–480. doi: 10.1093/sleep/31.4.473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jindal RD, Thase ME. Treatment of insomnia associated with clinical depression. Sleep Med Rev. 2004;8(1):19–30. doi: 10.1016/S1087-0792(03)00025-X. [DOI] [PubMed] [Google Scholar]
- 38.McCall WV, Blocker JN, D’Agostino R, Jr, et al. Insomnia severity is an indicator of suicidal ideation during a depression clinical trial. Sleep Med. 2010;11(9):822–827. doi: 10.1016/j.sleep.2010.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Aseltine RH, Jr, Kessler RC. Marital disruption and depression in a community sample. J Health Soc Behav. 1993;34(3):237–251. [PubMed] [Google Scholar]
- 40.Halford WK, Sanders MR, Behrens BC. A comparison of the generalization of behavioral marital therapy and enhanced behavioral marital therapy. J Consult Clin Psychol. 1993;61(1):51–60. doi: 10.1037//0022-006x.61.1.51. [DOI] [PubMed] [Google Scholar]
- 41.Anda RF, Williamson DF, Escobedo LG, et al. Depression and the dynamics of smoking: a national perspective. JAMA. 1990;264(12):1541–1545. [PubMed] [Google Scholar]
- 42.Kripke DF, Garfinkel L, Wingard DL, et al. Mortality associated with sleep duration and insomnia. Arch Gen Psychiatry. 2002;59(2):131–136. doi: 10.1001/archpsyc.59.2.131. [DOI] [PubMed] [Google Scholar]
- 43.Ferrie JE, Shipley MJ, Cappuccio FP, et al. A prospective study of change in sleep duration: associations with mortality in the Whitehall II cohort. Sleep. 2007;30(12):1659–1666. doi: 10.1093/sleep/30.12.1659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hublin C, Partinen M, Koskenvuo M, et al. Sleep and mortality: a population-based 22-year follow-up study. Sleep. 2007;30(10):1245–1253. doi: 10.1093/sleep/30.10.1245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Patel SR, Blackwell T, Redline S, et al. Study of Osteoporotic Fractures Research Group. The association between sleep duration and obesity in older adults. Int J Obes (Lond) 2008;32(12):1825–1834. doi: 10.1038/ijo.2008.198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Nakajima H, Kaneita Y, Yokoyama E, et al. Association between sleep duration and hemoglobin A1C level. Sleep Med. 2008;9(7):745–752. doi: 10.1016/j.sleep.2007.07.017. [DOI] [PubMed] [Google Scholar]
- 47.Chaput JP, Després JP, Bouchard C, et al. Sleep duration as a risk factor for the development of type 2 diabetes or impaired glucose tolerance: analyses of the Quebec Family Study. Sleep Med. 2009;10(8):919–924. doi: 10.1016/j.sleep.2008.09.016. [DOI] [PubMed] [Google Scholar]
- 48.Basner M, Fomberstein KM, Razavi FM, et al. American time use survey: sleep time and its relationship to waking activities. Sleep. 2007;30(9):1085–1095. doi: 10.1093/sleep/30.9.1085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.John U, Meyer C, Rumpf HJ, et al. Relationships of psychiatric disorders with sleep duration in an adult general population sample. J Psychiatr Res. 2005;39(6):577–583. doi: 10.1016/j.jpsychires.2005.01.006. [DOI] [PubMed] [Google Scholar]
- 50.Kaneita Y, Ohida T, Uchiyama M, et al. The relationship between depression and sleep disturbances: a Japanese nationwide general population survey. J Clin Psychiatry. 2006;67(2):196–203. doi: 10.4088/jcp.v67n0204. [DOI] [PubMed] [Google Scholar]
- 51.van Mill JG, Hoogendijk WJ, Vogelzangs N, et al. Insomnia and sleep duration in a large cohort of patients with major depressive disorder and anxiety disorders. J Clin Psychiatry. 2010;71(3):239–246. doi: 10.4088/JCP.09m05218gry. [DOI] [PubMed] [Google Scholar]
- 52.van Mill JG, Vogelzangs N, van Someren EJ, et al. Sleep duration, but not insomnia, predicts the 2-year course of depressive and anxiety disorders. J Clin Psychiatry. 2014;75(2):119–126. doi: 10.4088/JCP.12m08047. [DOI] [PubMed] [Google Scholar]
- 53.Chakravorty S, Grandner MA, Mavandadi S, et al. Suicidal ideation in veterans misusing alcohol: relationships with insomnia symptoms and sleep duration. Addict Behav. 2014;39(2):399–405. doi: 10.1016/j.addbeh.2013.09.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Turvey CL, Conwell Y, Jones MP, et al. Risk factors for late-life suicide: a prospective, community-based study. Am J Geriatr Psychiatry. 2002;10(4):398–406. [PubMed] [Google Scholar]
- 55.Fujino Y, Mizoue T, Tokui N, et al. Prospective cohort study of stress, life satisfaction, self-rated health, insomnia, and suicide death in Japan. Suicide Life Threat Behav. 2005;35(2):227–237. doi: 10.1521/suli.35.2.227.62876. [DOI] [PubMed] [Google Scholar]
- 56.Lee JI, Lee MB, Liao SC, et al. Prevalence of suicidal ideation and associated risk factors in the general population. J Formos Med Assoc. 2010;109(2):138–147. doi: 10.1016/S0929-6646(10)60034-4. [DOI] [PubMed] [Google Scholar]
- 57.Suh S, Kim H, Yang HC, et al. Longitudinal course of depression scores with and without insomnia in nondepressed individuals: a 6-year follow-up longitudinal study in a Korean cohort. Sleep. 2013;36(3):369–376. doi: 10.5665/sleep.2452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Bernert RA, Turvey CL, Conwell Y, et al. Association of poor subjective sleep quality with risk for death by suicide during a 10-year period: a longitudinal, population-based study of late life. JAMA Psychiatry. 2014;71(10):1129–1137. doi: 10.1001/jamapsychiatry.2014.1126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Trockel M, Karlin BE, Taylor CB, et al. Effects of cognitive-behavioral therapy for insomnia on suicidal ideation in veterans. Sleep. 2015;38(2):259–265. doi: 10.5665/sleep.4410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Tanskanen A, Tuomilehto J, Viinamäki H, et al. Nightmares as predictors of suicide. Sleep. 2001;24(7):844–847. [PubMed] [Google Scholar]
- 61.Nadorff MR, Nazem S, Fiske A. Insomnia symptoms, nightmares, and suicide risk: duration of sleep disturbance matters. Suicide Life Threat Behav. 2013;43(2):139–149. doi: 10.1111/sltb.12003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.McCall WV, Batson N, Webster M, et al. Nightmares and dysfunctional beliefs about sleep mediate the effect of insomnia symptoms on suicidal ideation. J Clin Sleep Med. 2013;9(2):135–140. doi: 10.5664/jcsm.2408. [DOI] [PMC free article] [PubMed] [Google Scholar]