Abstract
Objective
To describe obstetric health care providers’ responses and counseling approaches to patients’ disclosures of marijuana use during first prenatal visits.
Methods
We performed a content analysis of audio-recorded patient–health care provider first prenatal visits for obstetrics health care providers’ responses to patients’ disclosure of marijuana use. The study was conducted at five urban outpatient clinics located in Pittsburgh, PA.
Results
Among 468 audio-recorded first obstetric encounters, 90 patients (19%) disclosed marijuana use to 47 health care providers; mean number of recoded encounters containing marijuana disclosures for participating health providers was 1.8+1.4.. In 48% of these 90 visits, obstetric health care providers did not respond to marijuana use disclosures or offer counseling. When counseling was offered, it consisted of general statements without specific information on the risks or outcomes related to marijuana use in pregnancy, discussions regarding the need for urine toxicology testing, and warnings that use detected at the time of delivery would initiate child protective services involvement.
Conclusions
Obstetric health care provider responses to disclosure of marijuana use occurred in approximately half of patient encounters when marijuana use was disclosed and focused on legal and procedural consequences with less focus on health or medical implications. Our results suggest a need for health care provider training on potential consequences of perinatal marijuana use and communication skills for counseling patients about perinatal marijuana.
INTRODUCTION
Marijuana is the most commonly used drug during pregnancy in the United States.(1-3) In the 2009 National Survey on Drug Use and Health report, 4.6% of women reported they used marijuana during pregnancy,(4, 5) while population-based studies using biochemical testing noted rates as high as 12%.(6) Our previous work found 29% of pregnant patients were users of marijuana during pregnancy.(7)
Perinatal marijuana use is associated with negative pregnancy, infant, and child outcomes. In a prospective international multicenter cohort study of over 3000 women, multivariate predictive modeling that included other risk factors such as tobacco noted that women who used marijuana were two times more likely to have a spontaneous preterm birth with intact membranes.(8) Other studies found associations between perinatal marijuana use and adverse child neurobehavioral consequences such as cognitive, learning and behavioral problems.(9-11) The Generation R study examined a prospective cohort from fetal life to young adulthood and found prenatal exposure to marijuana was associated with behavioral problems such as aggressive behavior in early childhood.(12) In studies examining childhood depression, perinatal marijuana use is independently associated with more depressive and anxious symptoms in children as young as 10.(13)
With the legalization of recreational marijuana in several states and broadening public acceptance regarding marijuana use, it is imperative to understand how to optimize counseling for women using marijuana during pregnancy. We conducted our literature review in PubMed multiple times from October 2015 through December 2015, using search terms that included obstetric care providers, physician, resident, marijuana, cannabis, counseling, addressing, substance use, pregnancy, pregnant, prenatal drug use, and perinatal drug use, we found no studies focusing on obstetric health care providers’ counseling of pregnant patients about marijuana. A Google search with the same terms also did not elicit any existing research. To address this gap in the literature, we performed a content analysis of audio-recorded patient– health care provider first prenatal visits for obstetric health care providers’ responses to patients’ disclosure of marijuana use.
MATERIALS AND METHODS
This study is a sub-analysis of a larger study focused on patient–health care provider screening communication regarding substance use during pregnancy.(7) The study was approved by the University of Pittsburgh Institutional Review Board (IRB # PR008090530) and also received a National Institutes of Health (NIH) Certificate of Confidentiality. For this sub-analysis, we analyzed audio-recordings of first obstetric visit conversations between pregnant patients and their obstetric health care providers from five urban prenatal, outpatient clinic sites in Pittsburgh, Pennsylvania between 2011-2014.
Participants
Patient and health care provider participants were recruited for enrollment in the study and all participants signed informed consent. Patients were eligible if they were pregnant, 18 years of age or older, spoke English, and attending their first obstetric (OB) visit. Health care providers were eligible if they saw patients for first OB visits at the participating sites. Each study site served racially diverse populations of women with high proportions reliant on medical assistance (between 50-100%). In all five clinics, health care providers receive electronic medical record prompts to inquire about patients’ smoking, alcohol and drug use. All participants were informed they were participating in a study regarding patient–health care provider communication and were not initially made aware of the focus on substance use during pregnancy. Immediately after the audio recorded visits, patient participants were debriefed on the study focus and participated in a post-questionnaire with study staff. Following the post questionnaire, patients were invited to participate in a second phase of the larger study and asked to give a urine sample for toxicology testing. Interested subjects signed a second, separate consent. Results of the urine drug screens were not shared with the patients’ health care provider and were used for the larger study’s assessment of patient substance use disclosure rates(7). In order to minimize the Hawthorne effect (14), health care providers were not debriefed on the study focus until they saw a total of ten patients in the study or were leaving their position at the study sites.
Data Collection & Coding
Recordings were transcribed verbatim and reviewed for accuracy. Two experienced qualitative coders (JC & CH) independently reviewed all transcripts and audio recordings for patient disclosure of marijuana use. Patient marijuana use disclosure was coded as present or absent and categorized as current (any use by patient in last 30 days), past (any use 30 days or more prior to visit) or undetermined timing of marijuana use (unable to determine when last use occurred) Participants were categorized into only one time frame.
Coders independently identified health care providers’ responses, comments, counseling, advice, or any giving of information communicated to the patient about marijuana with almost half of conversations (n = 43; 48%) double-coded to assess inter-rater reliability. Any coding disagreements were discussed and final decisions were made by consensus. Inter-rater agreement was calculated using Cohen’s Kappa using Landis and Koch’s classification.(15) The interrater reliability for the coders was found to be Kappa = 0.73 indicating substantial agreement between coders. (15)
Statistical Analyses
All statistical analyses were conducted using SPSS (Ver 21)®. Descriptive statistics were summarized for demographic data, disclosure, and counseling items. Bivariate analyses were performed using chi-square analyses and risk ratios to examine associations between marijuana counseling responses with health care provider and patient characteristics.
RESULTS
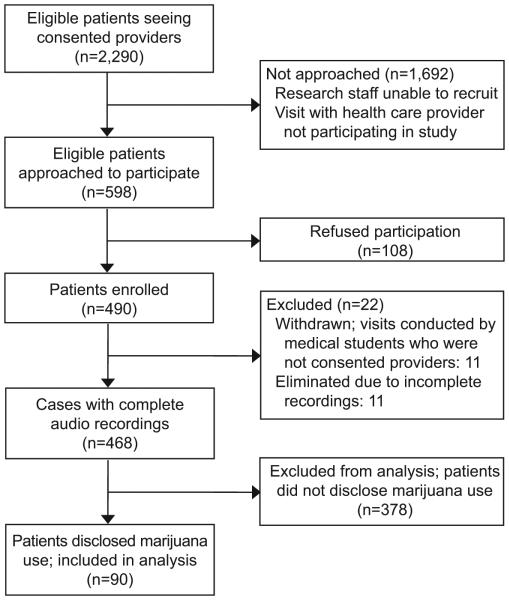
Figure 1 illustrates the study flow diagram. Between February 2011 and November 2014, a total of 2,290 patients presented for a new OB visit at the five participating clinical sites. Due to research staffing limitations and need to ensure consented participation of both patients and obstetric health care providers, a total of 598 of the 2,290 (26%) of these patients were approached for study participation. Of these, 490 patients enrolled and 468 complete recordings were obtained. Among these recorded visits, 90 patients (19%) disclosed marijuana use to their health care provider. We used the 90 recordings containing marijuana use disclosures in this analysis.
Figure 1.
Study flow diagram.
Table 1 describes patient participants’ characteristics. Mean patient age was 25+4.7 with most patients living with a partner. Almost two thirds were African American, less than half had a high school diploma or high school equivalency certificate, and the majority reported personal income of less than $20,000 per year. Forty-seven percent of the patients self-identified as current tobacco smokers.
Table 1.
Patient Characteristics
| Demographic | Category | Total (N=90) |
|---|---|---|
| Age | Mean; SD | 25.0 ± 4.7 |
| <20 | 9 (10.0) | |
| 20-29 | 65 (72.2) | |
| 30-39 | 16 (17.8) | |
| Ethnicity | African American | 58 (64.4) |
| White | 25 (27.8) | |
| Other | 7 (7.8) | |
| Marital Status | Single | 38 (42.2) |
| Living with partner | 44 (48.9) | |
| Married | 4 (4.4) | |
| Divorced/Separated | 4 (4.4) | |
| Highest Level of Education Completed | Grade school | 15 (16.7) |
| GED/High school | 40 (44.4) | |
| Associate’s degree | 11 (12.2) | |
| Some college | 21 (23.3) | |
| Finished college | 2 (2.2) | |
| Graduate school | 1 (1.1) | |
| Yearly income | $0-$4,999 | 35 (38.9) |
| $5,000-$9,999 | 16 (17.8) | |
| $10,000-$14,999 | 15 (16.7) | |
| $15,000-$19,999 | 13 (14.4) | |
| $20,000 + | 9 (10.0) | |
| Refused | 2 (2.2) | |
| Gravid women | Mean; SD Range/Min-Max |
2.9 ± 0.5 2/1-3 |
| Parous women | Mean; SD Range/Min-Max |
1.0 ± 1.2 5/0-5 |
Eighty-one health care providers were consented to participate in the study. Forty-seven participated in audio-recorded visits included in these analyses. Health care provider characteristics are shown in Table 2. A majority of the health care providers were female, white, and obstetrics and gynecology residents. Forty-two percent of the visits were conducted by health care providers that were junior residents (1st or 2nd year), and 24% were conducted by senior residents (3rd and 4th years). The remaining 33% of visits were conducted by non-residents (nurse practitioners, midwives, physician assistant and faculty physician). The mean number of audio-recorded visits across participating health care providers included in this analysis was 1.8+1.4
Table 2.
Health Care Provider Characteristics
| Demographic | Category | N(%) |
|---|---|---|
| Gender | Female | 44 (93.6) |
| Male | 3 (6.4) | |
| Ethnicity | White | 38 (80.9) |
| African American | 2 (4.3) | |
| Asian | 3 (6.4) | |
| Other | 4 (8.5) | |
| Provider Type | OB/Gyn Resident Faculty Ob/Gyn Nurse Midwife Physician Assistant Nurse Practitioner |
35 (74.5) 1 (2.1) 2 (4.3) 1 (2.1) 8 (17.0) |
| Years of Experience | Mean Range/Min-Max |
5.1 ± 5.3 29/0-30 |
Of the 90 visits in which patients disclosed marijuana use, 90% of these disclosures occurred secondary to a health care provider–initiated screening question about illicit drug or marijuana use; the remaining 10% of patients either had a positive urine drug screen documented in their medical record prior to the new obstetric visit or self-disclosed marijuana use when discussing nausea or asked about smoking. Forty-eight (53%) patients disclosed current marijuana use within the last 30 days to their health care provider. Twenty-six patients (29%) described their last use of marijuana as more than 30 days prior to the recorded visit. Sixteen patients (18%) disclosed marijuana use to their health care provider but the timing of their last marijuana use was undetermined. Sixty-four percent (n=58) of patients who disclosed any marijuana use had a positive urine drug screen in the second phase of our study.
Health care provider responses and counseling regarding patient marijuana use were categorized to five domains based on content. The five domains health care providers used were defined as no counseling, punitive, medical, helpful and supportive, and unclear. Definitions for and examples of the five counseling domains are contained in Table 3.
Table 3.
Marijuana Counseling Domains: Definitions and Examples
| Domain | Definition and Example |
|---|---|
| No counseling | No health care provider response to patient’s marijuana use or disclosure; health care provider may assess last use if patient quit since confirming pregnancy but offers no information or counseling regarding marijuana use. |
|
OB: Any smoking, drinking, or drugs? PT: I smoked marijuana a month ago to 2 months ago. OB: And how much did you used to smoke? PT: Marijuana? OB: No, cigarettes. PT: Ah a pack would last me for 2 weeks. OB: Alright Ms. X. So again it is your first time seeing us, um, so we are going to do a number of tests that we do for everybody on their first pregnancy visit. | |
| Punitive | Counseling focused on the legal ramifications of patient’s marijuana use; patient wamed child protective services will be contacted or informing patient that urine drug screening will be performed (at visit; at delivery). |
|
OB: Um, the issue with marijuana specifically is just that it is illegal. So at the time of delivery, they will do a urine drug test because you have a history of using it. If it is positive, at the time of delivery, they will often have you, like force you to talk to the child protective services because it is a risk factor. | |
| Medical | Counseling focused on medical risks of marijuana use such as comparing the negative outcomes of smoking tobacco (small gestational age, preterm birth, asthma); includes discussions regarding nausea and suggestions of using or prescribing medications for nausea in place of marijuana. |
|
OB: We do know it can affect size of the babies and things like that. And we want your baby to develop as healthy as possible. And you know how it alters your mind when you have it, how it makes you feel, so think about what it is doing to the baby that is not even formed quite yet. It gets the effects as well. And we don’t want to do that to the baby. | |
| Helpful and supportive |
Counseling included offering resources such as social work or counseling referrals, providing encouragement and support to quit; health care provider notes intention to follow-up with patient on quit efforts. |
|
OB: If you find yourself in a position where you feel like you can’t stop using…there are lots of avenues that we can help you explore to…keep you clean and sober…So let us know if there is anything we can do to help. | |
| Unclear | Counseling is not specific, health care provider expressed uncertainty of effects of marijuana use during pregnancy, patients advised to quit without providing information on risks or other educational information. |
| OB: Ok, so our goal is to keep you off of everything during pregnancy. |
OB, obstetrician; PT, patient.
In 43 visits (48%), obstetric health care providers offered no counseling or information specific to marijuana use. Specifically, in 21 of these 43 visits, the health care provider did not acknowledge the patient’s disclosure of marijuana use in any manner. In the remaining 22 instances without health care provider counseling, the obstetric health care providers assessed patients’ last use of marijuana or inquired if the patient had quit since confirming the pregnancy, yet offered no other counseling, information or guidance on marijuana use in pregnancy. Among the 42 patients who disclosed use of both marijuana and tobacco, 36 (86%) received tobacco counseling.
In the remaining 47 of the 90 visits containing marijuana use disclosures, health care providers addressed patient’s marijuana use with counseling, advice, information regarding marijuana use during pregnancy. Punitive (n=33) and helpful and supportive (n=34) were the two most commonly used counseling domains. Among punitive counseling, health care providers evenly split their discussions on informing patients they would undergo toxicology testing at delivery (n=27), or at the current visit (n=23), and warning if toxicology testing was positive for marijuana at time of delivery, child protective services would be contacted (n=21). Most helpful and supportive counseling focused on supportive or validating statements (n=26) indicating the health care provider’s belief in the patient’s ability and motivation to quit marijuana. Health care providers seldom offered resources or strategies to assist the women in their attempts to quit marijuana use. In only three visits did health care providers offer referrals to behavioral health counseling or social work; in one visit, the health care provider offered a referral to genetics. Additionally, only four visits contained health care providers’ intention to follow-up with the patient on her quit efforts.
Medical counseling was performed in 26 visits. In this counseling domain, health care providers discussed the evidence-based risks of perinatal marijuana use (n=12) or described that risks were “like smoking cigarettes” (n=10), and offered alternatives to treating nausea or lack of appetite associated with pregnancy (n=11).
Counseling was categorized in the unclear domain in 25 visits. In this domain, health care providers frequently used a general statement advising no substance use exposure (n=13) without providing any specific reasons why not to use marijuana during pregnancy or risks involved with perinatal marijuana use. In seven visits, health care providers admitted they did not know the risks of perinatal marijuana use.
Health care providers most commonly used varied combinations of the five domains with most (77%) using two to three domains in their counseling. In more than half (n=20, 61%) of visits during which health care providers’ counseling contained punitive responses, health care providers would also use supportive or validating statements encouraging patient’s efforts to quit.
Health care provider counseling did differ slightly depending on if the patient disclosed current, past or undetermined timing of last use of marijuana. In our bivariate analyses, no marijuana counseling was more likely to occur when patient’s disclosure specified past use (OR 1.9; CI 1.3-2.9) or did not indicate when last use occurred (OR 1.8 CI 1.2-2.6). Another finding from our bivariate analyses, patients who self-identified their race as black or African American or as “other” were more likely than white/Caucasian patients to admit their marijuana use was current. Compared to nurse midwives and faculty physicians, junior residents, senior residents, nurse practitioners, and physician assistants were more likely to respond to marijuana disclosures with no counseling (p=0.038). Counseling was also less likely to occur if the patient’s self-identified race was white; only 6 of the 25 (24%) white patients who admitted marijuana use received any type of counseling, compared to 36 of the 58 (62%) of African American patients and 5 of the 7 (71%) patients who indicted their race as “other” (p=0.004). Receipt of marijuana counseling was not associated with patient’s gravidity or parity, level of education, or household income, nor with health care providers’ gender or years in practice.
In multivariate analyses with patient race, health care provider type and timing of marijuana use, the only factor that remained significantly associated with whether patients received counseling regarding marijuana was whether patients disclosed current, past or undetermined use. Those who disclosed past use had 6 times the odds of receiving no counseling (OR 5.9; CI 1.7-20.5); those whose timing of use was undetermined had 12 times the odds (OR 12.0; CI 2.4-60.9). Patients who described their race as black or African-American were almost 10 times as likely to have counseling that was punitive (OR 9.7; CI 1.6-59.0) than patients who described their race as white or Caucasian. Race was not associated with the other counseling domains.
DISCUSSION
Our study finds a high rate of absent and insufficient health care provider responses to pregnant women’s disclosure of marijuana use during the first obstetric visit. Additionally, when counseling occurred, discussions focused on potential legal or child protective services implications rather than potential medical or pregnancy consequences. There may be several explanations for our results. Health care providers may, like the general public, have relatively favorable attitudes towards marijuana use compared to other illicit drugs. The United States population has demonstrated increasingly favorable attitudes regarding marijuana use. From 2010 to 2013, Pew Research surveys an 11% increase in the proportion of supporters for marijuana legalization with 52% favoring legalization. Further, the survey noted 48% of Americans tried or used marijuana in their lifetime, up 38% from a decade ago. (16) A survey of family physicians in Colorado found that 30% favored legalization for recreational use and 27% believed there were significant physical benefits to using marijuana. (17)
Lack of counseling may have also been related to lack of knowledge or information regarding risks of perinatal marijuana. When we performed a PubMed and a Google search using the terms “obstetric care providers”, “physician”, “resident”, “marijuana”, “cannabis”, “beliefs”, “attitudes”, “knowledge”, “pregnancy”,“pregnant, “prenatal” or “cannabis marijuana use”, and “perinatal marijuana or cannabis use”, we could find no studies examining either health care providers’ views or knowledge regarding marijuana use in pregnancy. The illegal status of marijuana in Pennsylvania may also influence obstetric health providers’ counseling. The health care provider may feel obligated to inform patients about the legal implications of continued perinatal marijuana use as a fair warning and a motivator to quit before delivery.
There are several limitations to our study. Our population was recruited from urban prenatal clinics in Pittsburgh, which primarily served low-income women on medical assistance and thus may not be representative of other patient populations, obstetric clinical settings, or geographic locations. This may limit generalizability of our findings. Other studies show higher rates of perinatal marijuana use among African American patients and patients of lower socio-economic status.(18-20) Our higher rates of marijuana use may be explained by our patient population. Also, marijuana use remains illegal in Pennsylvania; thus, our findings may not reflect counseling conversations occurring in regions where marijuana is legal for medical or recreational use. Being audio-recorded may have influenced patient disclosure and health care provider counseling of marijuana. Another factor is the majority of our participating obstetric health care providers are residents and most of the recorded encounters occurred when these residents were junior. Thus the counseling, or lack of counseling, may reflect this limited training and experience. Potentially with a broader sample of more experienced obstetric health care providers and a larger representation of other clinician types, we would obtain a different description of perinatal marijuana counseling.
Additionally, recordings collected captured communication between patient and health care providers during the first obstetric visit. Counseling discussions regarding marijuana use may occur in subsequent interactions or discussions with other staff members such as nurses or social workers that were not captured as part of this study. Qualitative coding is also an iterative, interpretive process that could be subject to investigator bias. However, to reduce impact of such bias in the analysis and increase credibility, we used the strategy of triangulating analysts or use of two independent coders.(21) And, while there is not universal agreement or support for qualitative studies to include statistical assessments of inter-rater reliability(21, 22), we felt that given our relatively large number of transcripts and limited number of codes this assessment to represent a reasonable demonstration of the degree of correlation between coders. We used Landis and Koch’s interrater taxonomy for determining quality of inter-rater reliability and have included the interpretive category for the value to help reader’s understand that the Kappa of 0.79 represented substantial levels of agreement.(15) Finally, all observational studies face potential bias from unknown, unmeasured, or poorly measured confounding factors.(23)
To inform future policies regarding perinatal marijuana use, it is imperative to understand the effects of legalization on beliefs, attitudes, behaviors, practices, and concerns regarding marijuana use among pregnant patients and their obstetric health care providers. The American College of Obstetricians and Gynecologists recently issued a committee opinion recommending all obstetric health care providers ask and counsel pregnant patients about perinatal marijuana.(24) There have been efforts in Colorado and Washington where marijuana is legal for recreational use, to make information on the health consequences of perinatal marijuana use available to clinicians. Despite the literature available regarding the negative outcomes associated with marijuana use in pregnancy and the recommendations for counseling, there is no evidence on whether, or how counseling for marijuana use nationally, is occurring with the continuing and growing legalization. We provide suggested components for obstetric health care provider counseling for marijuana (Box 1). Counseling should address the potential medical risks for both mother and fetus, and strategies to assist the patient in quitting. Further, studies are needed to better understand the beliefs, perspectives, knowledge, and concerns of both pregnant patients and obstetric health care providers to develop and tailor effective communication resources and training interventions on perinatal marijuana that address the specific needs and concerns of health care providers and patients in the varying regions across the nation.
Box 1. Suggested Marijuana Counseling.
Implications for Mother and Baby
Small gestational weight, preterm delivery
Respiratory complications (asthma, lung disorders)
Cognitive deficits (attention, memory, learning, and behavioral)
Higher rates of anxiety and depression
Support for Patient
Available medications to help treat nausea and emesis
Safe medications for anxiety and depression in pregnancy
Availability of social work, physicians, or other health care providers to assist with quit plans.
Positive drug screening at delivery may prompt notification of child protective services, depending on state laws or health system policies.
ACKNOWLEDGMENTS
Funded by the National Institute of Drug Abuse (NIDA) 1R01DA026410-01A1, the Pennsylvania Department of Health, and the Magee Womens Hospital Volunteer Service Board, and supported by the National Institutes of Health through Grant Number UL1TR000005. Funders had no role in study design, collection analysis and interpretation of data; writing the report; and the preparation, review, approval or decision to submit the report for publication.
Footnotes
Financial Disclosure
The authors did not report any potential conflicts of interest.
Presented at the International Conference on Communication in Healthcare in New Orleans, Louisiana on October 27, 2015.
Contributor Information
Cynthia L. Holland, Magee-Womens Research Institute; Department of Obstetrics, Gynecology and Reproductive Sciences.
Doris Rubio, Division of General Internal Medicine, Department of Internal Medicine; Center for Research in Health Care; Clinical and Translational Science Institute, University of Pittsburgh.
Keri L. Rodriguez, Center for Health Equity Research & Promotion (CHERP), Veterans Affairs Pittsburgh Healthcare System; Division of General Internal Medicine, Department of Internal Medicine, University of Pittsburgh.
Kevin L. Kraemer, Division of General Internal Medicine, Department of Internal Medicine; Center for Research in Health Care; University of Pittsburgh.
Nancy Day, Department of Psychiatry, University of Pittsburgh.
Robert M. Arnold, Section of Palliative Care and Medical Ethics, Institute to Enhance Palliative Care; Institute for Doctor-Patient Communication; Center for Research in Health Care; Division of General Internal Medicine, Department of Internal Medicine, University of Pittsburgh; Jill A. Tarr, LCSW, ACSW - Magee-Womens Research Institute; Department of Obstetrics, Gynecology and Reproductive Sciences.
Judy C. Chang, Magee-Womens Research Institute; Department of Obstetrics, Gynecology and Reproductive Sciences; Center for Research in Health Care; Division of General Internal Medicine, Department of Internal Medicine, University of Pittsburgh.
References
- 1.Westfall R, Janssen P, Lucas P, Capler R. Survey of medicinal cannabis use among childbearing women: patterns of its use in pregnancy and retroactive self-assessment of its efficacy against 'morning sickness'. Complement Ther Clin Pract. 2006;12(1):27–33. doi: 10.1016/j.ctcp.2005.09.006. [DOI] [PubMed] [Google Scholar]
- 2.Substance Abuse and Mental Health Services Administration (SAMHSA) Results from the 2007 National Survey on Drug Use and Health: National Findings (NSDUH Series H-34, DHHS Publication No. SMA-08-4343. Department of Health and Human Services; Rockville, MD: 2008. [Google Scholar]
- 3.Kuczkowski K. The effects of drug abuse on pregnancy. Curr Opin Obstet Gynecol. 2007;19:578–85. doi: 10.1097/GCO.0b013e3282f1bf17. [DOI] [PubMed] [Google Scholar]
- 4.Substance Abuse and Mental Heatlh Services Administration (SAMHSA) Summary of National Findings. Rockville, MD; 2010. Results from the 2009 National Survey on Drug Use and Health: Volume I. [Google Scholar]
- 5.Havens J, Simmons L, Shannon L, Hansen W. Factors associated with substance use during pregnancy: results from a national sample. Drug Alcohol Depend. 2009;99:89–95. doi: 10.1016/j.drugalcdep.2008.07.010. [DOI] [PubMed] [Google Scholar]
- 6.Chasnoff I, Landress H, Barrett M. The prevalence of illicit drug or alcohol use during pregnancy and discrepancies in mandatory reporting in Pinellas County, Florida. NEJM. 1990;322(17):1202–6. doi: 10.1056/NEJM199004263221706. [DOI] [PubMed] [Google Scholar]
- 7.Chang J, Holland C, Tarr J, Rodriguez K, Kraemer K, Rubio D, et al. Perinatal marijuana use: an observational study examining prevalence, screening, and disclosure. Am J Health Promot. 2015 Epub ahead of print. [Google Scholar]
- 8.Dekker G, Lee S, North R, McCowan L, Simpson N, Roberts C. Risk factors for preterm birth in an International prospective cohort of nulliparous women. PLoS One. 2012;7(7):1–9. doi: 10.1371/journal.pone.0039154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Richardson G, Ryan C, Willford J, Day N, Goldschmidt L. Prenatal alcohol and marijuana exposure: effects on neuropsychological outcomes at 10 years. Neurotoxicol Teratol. 2002;24(3):309–20. doi: 10.1016/s0892-0362(02)00193-9. [DOI] [PubMed] [Google Scholar]
- 10.Goldschmidt L, Day N, Richardson G. Effects of prenatal marijuana exposure on child behavior problems at age 10. Neurotoxicol Teratol. 2000;22(3):325–36. doi: 10.1016/s0892-0362(00)00066-0. [DOI] [PubMed] [Google Scholar]
- 11.Fried P, Watkinson B. Differential effects on facets of attention in adolescents prenatally exposed to cigarettes and marijuana. Neurotoxicol Teratol. 2001;23(5):421–30. doi: 10.1016/s0892-0362(01)00160-x. [DOI] [PubMed] [Google Scholar]
- 12.El Marroun H, Hudziak J, Tiemeire H, Creemers H, Steegers E, Jaddoe V, et al. Intrauterine cannabis exposure leads to more aggressive behavior and attention problems in 18-month-old girls. Drug Alcohol Depend. 2011;118(2-3):470–4. doi: 10.1016/j.drugalcdep.2011.03.004. [DOI] [PubMed] [Google Scholar]
- 13.Gray K, Day N, Leech S, Richardson G. Prenatal marijuana exposure: effect on child depressive symptoms at ten years of age. Neurotoxicol Teratol. 2005;27:439–48. doi: 10.1016/j.ntt.2005.03.010. [DOI] [PubMed] [Google Scholar]
- 14.Gillespie R. A history of the Hawthorne Effect. Cambridge, Massachusetts; Cambridge University Press; 1991. [Google Scholar]
- 15.Landis J, Koch G. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–74. [PubMed] [Google Scholar]
- 16.Pew Research Center Majority now supports legalizing marijuana. 2013 cited; Available from: http://www.people-press.org/2013/04/04/majority-now-supports-legalizing-marijuana/
- 17.Kondrad E, Reid A. Colorado family physicians' attitudes towards medical marijuana use. J Am Board Fam Med. 2013;26(1):52–60. doi: 10.3122/jabfm.2013.01.120089. [DOI] [PubMed] [Google Scholar]
- 18.Hans S. Demographic and psychosocial characteristics of substance-abusing pregnant women. Clin Perinatol. 1999;26(1):55–74. [PubMed] [Google Scholar]
- 19.Noble A, Vega W, Kolody B, Porter P, Hwang J, Merk G, et al. Prenatal substance abuse in California: findings from the Perinatal Substance Exposure Study. J Psychoactive Drugs. 1997;29(1):43–53. doi: 10.1080/02791072.1997.10400169. [DOI] [PubMed] [Google Scholar]
- 20.Yawn B, Thompson L, Lupo V, Googins M, Yawn R. Prenatal drug use in Minneapolis-St Paul, Minn. A 4-year trend. Arch Fam Med. 1994;3(6):520–7. doi: 10.1001/archfami.3.6.520. [DOI] [PubMed] [Google Scholar]
- 21.Patton M. Qualitative Research and Evaluation Methods. 4th Sage Publications, 4th ed; Thousand Oaks, CA: 2015. [Google Scholar]
- 22.Morse J. “Perfectly Healthy but Dead”: The myth of inter-rater reliability. Qual Health Res. 1997;7(4):445–7. [Google Scholar]
- 23.Grimes D, Schulz K. False alarms and pseudo-epidemics: the limitations of observational epidemiology. Obstetrics and gynecology. 2012;120(4):920–7. doi: 10.1097/AOG.0b013e31826af61a. [DOI] [PubMed] [Google Scholar]
- 24.American College of Obstetricians and Gynecologists Marijuana use during pregnancy and lactation. Committee Opinion. 2015;126:234–8. [Google Scholar]