Abstract
Objective
To estimate the associations between the duration of active pushing during the second stage of labor and maternal and neonatal outcomes.
Methods
We performed an observational study in which data were obtained by trained abstractors from maternal and neonatal charts of deliveries at 25 hospitals over a 3-year period. In this secondary analysis, women with no prior cesarean delivery who had a term, singleton, cephalic gestation and reached complete dilation were analyzed. The duration of pushing, defined as the time from initiation of pushing to either vaginal delivery or the decision to proceed with a cesarean, was determined. The primary maternal outcome was cesarean delivery and the primary neonatal outcome was a composite that included: mechanical ventilation, proven sepsis, brachial plexus palsy, clavicular fracture, skull fracture, other fracture, seizures, hypoxic ischemic encephalopathy, or death. Nulliparous and parous women were analyzed separately in univariable and then multivariable analyses.
Results
Fifty three thousand two hundred eighty five women were analyzed. In both nulliparous and parous women, longer duration of pushing was associated with increased odds of both cesarean delivery and the neonatal adverse outcome composite. Nevertheless, even after 4 hours of pushing, approximately 78% of nulliparous women who continued with active pushing had a vaginal delivery and over 97% did not have the composite adverse neonatal outcome. Similarly, after more than 2 hours of pushing, approximately 82% of parous women who continued active pushing delivered vaginally and over 97% did not have the adverse neonatal outcome.
Conclusion
A longer duration of pushing is associated with an increased relative risk, but small absolute difference in risk, of neonatal complications. Approximately 78% of nulliparous women delivered vaginally even after 4 hours of pushing.
As the cesarean rate has continued to climb, there has been increasing interest in determining best practices in labor and how they might be used to prevent unnecessary cesarean deliveries. One area of focus has been the duration of the second stage. Recently, in a document entitled “Safe prevention of the primary cesarean delivery” which was a joint document from ACOG and SMFM, the authors noted that arrest of the second stage should not be diagnosed until 2 and 3 hours in parous and nulliparous women without epidural analgesia have elapsed, respectively, and that “longer durations may be appropriate on an individualized basis.”1
Nevertheless, there remains uncertainty about this recommendation for several reasons. First, many studies of the duration of the second stage may not have been large enough to be able to discern the extent to which this duration is associated with differences in infrequent, but clinically important, neonatal outcomes. Second, it is not entirely clear in many of the studies what the “duration” actually represents, as it has been difficult from large administrative databases to distinguish active pushing from delayed pushing (i.e., after complete dilation but before pushing has begun) or from the time after which a decision for cesarean has been made but before the delivery has occurred.1-5
Thus, the association between the duration of active pushing and obstetric outcomes remains uncertain. The Assessment of Perinatal Excellence study (APEX) was an observational study of over 100,000 women in which trained research personnel abstracted detailed labor data. The objective of the present analysis was to use this detailed and large dataset to estimate whether a longer duration of active pushing, independent of delayed pushing, was associated with a higher frequency of adverse maternal and neonatal outcomes.
Materials and Methods
Between 2008 and 2011, investigators at 25 medical centers of the Eunice Kennedy Shriver National Institute of Child Health and Human Development Maternal-Fetal Medicine Units (MFMU) Network performed an observational study (i.e., the APEX study). Patient characteristics, intrapartum events, and pregnancy outcomes were collected on all deliveries at these hospitals on randomly selected days representing one third of deliveries over a three-year period. Trained and certified research personnel abstracted all charts. For this study, all centers obtained institutional review board approval and a waiver of informed consent. Full details of the technique of data collection have been described previously.6,7
Women were considered eligible for this secondary analysis if they had no prior cesarean, had a singleton, cephalic gestation at ≥ 37 weeks, and reached complete dilation. The duration of active pushing, defined as the duration between the initiation of pushing and either vaginal delivery or the decision to proceed with cesarean delivery was determined. Not included in the duration of active pushing was the duration of delayed pushing, which was defined as the time between the identification of complete dilation and the initiation of active pushing.
In order to facilitate clinical translation of the results, women were grouped according to their duration of active pushing in 60-minute increments: < 1 hour, 1 to < 2 hours, 2 to < 3 hours, 3 to < 4 hours, and ≥ 4 hours. Patient characteristics and outcomes were compared in univariable analysis between the groups after stratification by parity. The primary maternal outcome was cesarean delivery, although other outcomes such as post-partum hemorrhage (defined as > 500 cc and > 1000 cc estimated blood loss at vaginal and cesarean delivery, respectively) and 3rd or 4th degree perineal laceration were assessed as well. The primary neonatal outcome was an adverse event composite that included any of the following events: mechanical ventilation, proven sepsis (i.e., clinical evidence of infection in combination with positive blood, urine, or cerebrospinal fluid culture), brachial plexus palsy (i.e., a diagnosis of brachial plexus palsy noted after delivery that involved the nerves of the brachial plexus with partial or complete paralysis affecting an upper extremity), clavicular fracture, skull fracture, other fracture, seizures, hypoxic ischemic encephalopathy (HIE), or death (within 120 days of delivery).
The chi-square test, Cochrane-Armitage trend test, and nonparametric Kruskal-Wallis test were utilized as appropriate. Multivariable analysis with binary logistic regression was used to assess which outcomes remained independently associated with duration of active pushing after adjustment for potential confounding factors. Covariates entered into the multivariable regression were those baseline characteristics that had been assessed in univariable analysis. Odds ratios with 95% confidence intervals were estimated from the regression equations. Multivariable analyses were performed for all maternal outcomes and for the primary neonatal composite. Individual neonatal outcomes could not be examined in multivariable analysis given the infrequency of their occurrence. The duration of active pushing was entered into the regression equation as a categorical variable using the groups defined by the duration categories above. Also entered into the regression was the list of patient characteristics. Lastly, the duration of delayed pushing as a categorical covariate (using the same time intervals that had been used to categorize durations of active pushing) was adjusted for in all multivariable equations. All tests were two sided and P < .05 was used to define statistical significance. There were no adjustments for multiple comparisons, and analyses were performed using SAS. No imputation for missing data was performed (Table 1).
Table 1.
Frequency of missing data for each variable field.
| Patient characteristics and outcomes | N = 53,285 |
|---|---|
| Maternal | |
| Age (years) | 0 |
| BMI (kg/m2) at delivery | 1072 (2.0) |
| Race/ethnicity | 0 |
| Private insurance | 432 (0.8) |
| Cigarette use during pregnancy | 51 (0.1) |
| Hypertensive disease of pregnancy | 8 (0.02) |
| Diabetes mellitus | 17 (0.03) |
| GBS status | 0 |
| Oligohydramnios | 13 (0.02) |
| Premature rupture of membranes | 601 (1.1) |
| Epidural | 6,047 (11.4) |
| Episiotomy | 16 (0.03) |
| Duration of delayed pushing | 1756 (3.3) |
| Route of delivery | 1 (0.00) |
| Postpartum hemorrhage | 1891 (3.6) |
| 3rd/4th degree laceration | 23 (0.04) |
| Neonatal | |
| Composite adverse outcome | 323 (0.6) |
| Mechanical ventilation ≥1 day | 9 (0.02) |
| Confirmed sepsis | 10 (0.02) |
| Brachial plexus palsy | 3 (0.01) |
| Fracture | |
| Clavicular | 6 (0.01) |
| Skull | 3 (0.01) |
| Other | 4 (0.01) |
| Seizure | 10 (0.02) |
| Hypoxic ischemic encephalopathy | 371 (0.7) |
| Death | 0 |
All data presented as n (%)
Results
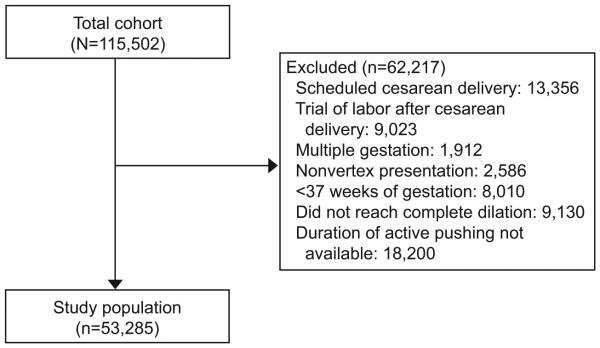
Of the 115,502 women in the APEX study, 53,285 women met inclusion criteria for this analysis (Figure 1). Forty-nine percent (N = 26,028) were nulliparous and 51% (N = 27,257) were parous. Few (5.7%) nulliparous women and no parous woman actively pushed for more than 3 hours (Table 2). Women who pushed for longer durations of time were more likely to be older, non-Hispanic white, have diabetes mellitus, and have received epidural analgesia.
Figure 1.
Flow chart detailing composition of the study population.
Table 2.
Patient characteristics of the study population stratified by parity and by duration of active pushing
| Nulliparous | Parous | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Patient characteristics |
< 60m N=15148 |
60-119m N = 6613 |
120-179m N=2796 |
180-239m N=1011 |
≥ 240m N = 460 |
P | < 60m N = 25645 |
60-119m N = 1145 |
120-179m N=467 |
P |
| Age (years) | 24.7 (5.9) |
26.6 (5.9) |
28.0 (5.8) |
28.2 (5.9) |
27.8 (6.2) | <0.001 | 29.3 (5.6) |
30.7 (5.6) |
30.0 (5.7) |
<0.001 |
| BMI (kg/m2) | 30.0 (5.7) | 30.1 (5.6) |
30.0 (5.4) |
30.1 (5.2) |
30.4 (5.5) | 0.072 | 30.8 (5.9) |
31.5 (6.2) |
31.4 (5.3) |
<0.001 |
| Race/ ethnicity |
<0.001 | <0.001 | ||||||||
| NHW | 6928 (45.7) |
3798 (57.4) |
1713 (61.3) | 599 (59.3) |
266 (57.8) |
11360 (44.3) |
535 (46.7) | 191 (40.9) |
||
| NHB | 3431 (22.7) |
771 (11.7) | 223 (8.0) |
84 (8.3) |
61 (13.3) | 4989 (19.5) | 160 (14.0) | 90 (19.3) |
||
| Hispanic | 3045 (20.1) |
1066 (16.1) |
381 (13.6) |
164 (16.2) |
67 (14.6) | 6981 (27.2) | 296 (25.9) | 141 (30.2) |
||
| Asian | 844 (5.6) |
566 (8.6) |
257 (9.2) |
88 (8.7) |
34 (7.4) |
1091 (4.3) |
94 (8.2) |
23 (4.9) |
||
| Other | 900 (5.9) |
412 (6.2) |
222 (7.9) |
76 (7.5) |
32 (7.0) |
1224 (4.8) |
60 (5.2) |
22 (4.7) |
||
| Private insurance |
7694 (51.1) |
4214 (64.4) |
1978 (71.8) | 704 (70.5) |
289 (63.4) |
<0.001 | 12059 (47.4) |
636 (55.9) | 205 (44.2) |
<0.001 |
| Cigarette use during pregnancy |
1357 (9.0) |
437 (6.6) |
146 (5.2) |
47 (4.7) |
27 (5.9) |
<0.001 | 2530 (9.9) |
81 (7.1) |
40 (8.6) |
0.006 |
| HDP* | 1580 (10.4) |
697 (10.5) | 264 (9.4) |
130 (12.9) |
59 (12.8) | 0.017 | 1681 (6.6) |
68 (5.9) |
34 (7.3) |
0.58 |
| Diabetes mellitus** |
622 (4.1) |
333 (5.0) |
138 (4.9) |
53 (5.2) | 24 (5.2) | 0.003 | 1605 (6.3) | 83 (7.3) |
39 (8.4) |
0.006 |
| GBS status | <0.001 | 0.11 | ||||||||
| Positive | 3539 (23.4) |
1476 (22.3) |
602 (21.5) |
212 (21.0) | 88 (19.1) | 5696 (22.2) | 244 (21.3) | 90 (19.3) |
||
| Negative | 10170 (67.1) |
4628 (70.0) |
2001 (71.6) | 711 (70.3) |
351 (76.3) |
16209 (63.2) |
752 (65.7) | 317 (67.9) |
||
| Unknown | 1439 (9.5) | 509 (7.7) |
193 (6.9) |
88 (8.7) |
21 (4.6) |
3740 (14.6) | 149 (13.0) | 60 (12.9) |
||
| Oligo- hydramnios |
632 (4.2) |
243 (3.7) | 91 (3.3) |
36 (3.6) |
18 (3.9) |
0.12 | 696 (2.7) |
34 (3.0) |
6 (1.3) |
0.14 |
| pPROM or PROM |
357 (2.4) |
168 (2.6) |
77 (2.8) |
35 (3.5) |
16 (3.6) |
0.11 | 326 (1.3) |
16 (1.4) |
9 (1.9) |
0.45 |
| Epidural | 12,644 (90.5) |
6100 (95.9) |
2629 (97.6) | 965 (98.3) |
425 (96.8) |
<0.001 | 18186 (85.5) |
1028 (94.4) |
397 (91.5) |
<0.001 |
| Episiotomy | 2266 (15.0) |
1305 (19.7) |
613 (21.9) |
210 (20.8) |
79 (17.2) |
<0.001 | 1517 (5.9) |
142 (12.4) |
42 (9.0) |
<0.001 |
| Duration of delayed pushing (min) |
10 (1, 30) |
14 (3, 46) |
15 (3, 51) |
13 (2, 49) |
10 (0, 40) |
<0.001 | 4 (0, 12) |
7 (0, 24) |
4 (0, 17) |
<0.001 |
All data presented as means (standard deviation), median (interquartile range), or N (%)
m = minutes; BMI = body mass index at delivery; NHW = non-Hispanic white; NHB = non-Hispanic black; HDP = hypertensive disease of pregnancy; GBS = Group B streptococcus; pPROM = preterm premature rupture of the membranes; PROM = premature rupture of membranes
includes chronic hypertension, gestational hypertension, and preeclampsia;
includes pregestational and gestational diabetes mellitus
As the duration of the active pushing increased, the chance of a cesarean delivery or an operative vaginal delivery increased as well (Table 3). The risk of a postpartum hemorrhage and third or fourth degree lacerations also increased with longer duration of active pushing. Even at more than four hours of pushing, however, the chance of vaginal delivery for a nulliparous woman was approximately 78%; at more than two hours of pushing, the chance of a vaginal delivery for a parous woman was approximately 82%.
Table 3.
Association between duration of active pushing and maternal and neonatal outcomes
| Nulliparous | Parous | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Obstetric outcomes |
< 60m N=15148 |
60-119m N = 6613 |
120-179m N=2796 |
180-239m N=1011 |
≥ 240m N = 460 |
P* | < 60m N = 25645 |
60-119m N = 1145 |
120-179m N=467 |
P* |
| Maternal | ||||||||||
| Route of delivery |
<0.001 | <0.001 | ||||||||
| Cesarean | 447 (3.0) |
543 (8.2) |
499 (17.9) |
245 (24.2) |
103 (22.4) |
136 (0.5) |
97 (8.5) |
85 (18.2) |
||
| OVD | 1201 (7.9) |
881 (13.3) |
768 (27.5) |
355 (35.1) |
151 (32.8) |
814 (3.2) |
151 (13.2) |
87 (18.6) |
||
| SVD | 13500 (89.1) |
5189 (78.5) |
1528 (54.7) |
411 (40.7) |
206 (44.8) |
24695 (96.3) |
897 (78.3) |
295 (63.2) |
||
| ȀPPH | 150 (1.0) |
87 (1.4) |
68 (2.5) |
37 (3.7) |
15 (3.3) |
<0.001 | 157 (0.6) |
17 (1.5) |
16 (3.5) |
<0.001 |
| 3rd/4th degree laceration |
752 (5.0) |
563 (8.5) |
391 (14.0) |
154 (15.3) |
75 (16.3) |
<0.001 | 236 (0.9) |
41 (3.6) |
24 (5.1) |
<0.001 |
| Neonatal | ||||||||||
| CAO | 193 (1.3) |
97 (1.5) |
61 (2.2) |
26 (2.6) |
11 (2.4) |
<0.001 | 270 (1.1) |
25 (2.2) |
13 (2.8) |
<0.001 |
| Mechanical ventilation ≥ 1 day |
80 (0.5) |
43 (0.7) |
21 (0.8) |
4 (0.4) |
3 (0.7) |
0.39 | 91 (0.4) |
7 (0.6) |
3 (0.6) |
0.10 |
| Confirmed sepsis |
23 (0.2) |
7 (0.1) |
3 (0.1) |
1 (0.1) |
0 | 0.25 | 26 (0.1) |
0 | 1 (0.2) |
0.97 |
| Brachial plexus palsy |
16 (0.1) |
9 (0.1) |
8 (0.3) |
5 (0.5) |
0 | 0.009 | 20 (0.1) |
2 (0.2) |
0 | 0.83 |
| Fracture | ||||||||||
| Clavicular | 39 (0.3) | 12 (0.2) | 10 (0.4) | 4 (0.4) | 0 | 0.86 | 108 (0.4) | 4 (0.4) | 2 (0.4) | 0.84 |
| Skull | 1 (0.0) | 2 (0.0) | 1 (0.0) | 2 (0.2) | 0 | 0.009 | 1 (0.0) | 0 | 0 | 0.81 |
| Other | 0 | 3 (0.1) | 2 (0.1) | 3 (0.3) | 0 | <0.001 | 9 (0.0) | 2 (0.2) | 1 (0.2) | 0.006 |
| Seizure | 18 (0.1) | 12 (0.2) | 13 (0.5) | 3 (0.3) | 5 (1.1) | <0.001 | 13 (0.1) | 2 (0.2) | 2 (0.4) | <0.001 |
| HIE | 51 (0.3) | 25 (0.4) | 15 (0.6) | 8 (0.8) | 5 (1.1) | 0.001 | 35 (0.1) | 7 (0.6) | 5 (1.1) | <0.001 |
| Death | 1 (0.0) | 0 | 0 | 0 | 0 | 0.49 | 1 (0.0) | 0 | 0 | 0.81 |
All P values derived from the Cochran-Armitage trend test with the exception of “route of delivery” (which is derived from chi-square) All data presented as n(%)
m = minutes; OVD = operative vaginal delivery; SVD = spontaneous vaginal delivery; PPH = postpartum hemorrhage; HIE = hypoxic ischemic encephalopathy; CAO = composite adverse outcome
The composite adverse neonatal outcome also increased in frequency with a longer duration of pushing. Statistically significant increases were noted in several individual components of the composite outcome, including brachial plexus palsy, seizures, and HIE. The absolute difference in risk, however, was small – in all cases approximately 1% or less.
The results from the multivariable analyses largely mimic those of the univariate analyses (Tables 4 and 5). Women, regardless of parity, generally had higher odds of experiencing cesarean delivery, operative vaginal delivery, postpartum hemorrhage, 3rd or 4th degree laceration, and the neonatal composite adverse outcome with longer durations of pushing. The associations between duration of pushing and the various outcomes also were similar when “center” was evaluated in the multivariable regressions as a potential confounder (data not shown).
Table 4.
Multivariable analysis for the association of duration of active pushing with maternal and neonatal outcomes in nulliparous women.
| Obstetric outcomes | 60-119 min* | 120-179 min* | 180-239 min* | ≥ 240 min* |
|---|---|---|---|---|
| Cesarean** | 2.9 (2.5, 3.3) | 8.9 (7.7, 10.3) | 16.7 (13.7, 20.3) | 14.7 (11.2, 19.3) |
| OVD** | 1.7 (1.6, 1.9) | 5.0 (4.5, 5.6) | 8.6 (7.3, 10.1) | 7.9 (6.2, 9.9) |
| PPH | 1.5 (1.1, 2.0) | 3.1 (2.3, 4.3) | 4.0 (2.7, 6.0) | 3.8 (2.1, 6.9) |
| 3rd/4th degree laceration |
1.6 (1.4, 1.8) | 2.7 (2.3, 3.1) | 2.9 (2.4, 3.6) | 3.5 (2.6, 4.6) |
| Neonatal CAO | 1.3 (0.98, 1.7) | 2.0 (1.4, 2.7) | 2.1 (1.4, 3.3) | 2.2 (1.2, 4.2) |
All data presented as odds ratios (95% confidence intervals)
Multivariable analysis adjusted for the following covariates: age, body mass index, race/ethnicity, private insurance, cigarette use during pregnancy, hypertensive disease of pregnancy, diabetes mellitus, Group B streptococcus status, oligohydramnios, premature rupture of membranes, epidural analgesia, duration of delayed pushing
referent = active pushing < 60 minutes;
referent = spontaneous vaginal delivery
min = minutes; AP = active pushing; OVD = operative vaginal delivery; PPH = postpartum hemorrhage; CAO = composite adverse outcome
Table 5.
Multivariable analysis for the association of duration of active pushing with maternal and neonatal outcomes in parous women.
| Obstetric outcomes |
60-119 min* | 120-179 min* |
|---|---|---|
| Cesarean** | 14.1 (10.6, 18.9) | 44.4 (32.4, 60.9) |
| OVD** | 4.4 (3.6, 5.4) | 8.2 (6.3, 10.6) |
| PPH | 2.2 (1.3, 3.8) | 5.6 (3.2, 9.6) |
| 3rd/4th degree laceration |
3.1 (2.1, 4.4) | 5.5 (3.5, 8.6) |
| CAO | 1.8 (1.2, 2.9) | 2.7 (1.5, 4.8) |
All data presented as odds ratios (95% confidence intervals) Multivariable analysis adjusted for the following covariates: age, body mass index, race/ethnicity, private insurance, cigarette use during pregnancy, hypertensive disease of pregnancy, diabetes mellitus, Group B streptococcus status, oligohydramnios, premature rupture of membranes, epidural analgesia, duration of delayed pushing
referent = active pushing < 60 minutes;
referent = spontaneous vaginal delivery min = minutes; AP = active pushing; OVD = operative vaginal delivery; PPH = postpartum hemorrhage; CAO = composite adverse outcome
Discussion
In this analysis, we have assessed the relationship between the duration of active pushing and obstetric outcomes. We have found that it is quite uncommon that nulliparous women push more than three hours or parous women push more than two hours. This is consistent with contemporary data from the Consortium of Safe Labor.8 It does appear that a longer duration of pushing is statistically associated with a rise in the frequency of maternal and neonatal adverse outcomes. Nevertheless, even when nulliparous women exceed 4 hours of pushing or parous women exceed 2 hours of pushing, they continue to have a relatively high chance of vaginal delivery and low chance of neonatal adverse outcomes.
This analysis generally supports the conclusions of other investigators, particularly with regard to maternal outcomes. For example, Rouse et al utilized data on 4126 women from a randomized trial of fetal pulse oximetry and showed that the duration of the second stage was associated with higher odds of chorioamnionitis, uterine atony, and 3rd or 4th degree pelvic laceration.2 That study, as well as others, did not demonstrate an increased risk of neonatal adverse outcomes with longer second stage duration2-5, although the sample sizes may not have been sufficiently large to demonstrate differences even if they were to exist. In contrast, in the present study, which included over 50,000 women, a statistical rise in adverse neonatal outcomes also was seen as the duration of the second stage increased.
This analysis extends the findings of prior studies by specifically analyzing only the duration of active pushing, and not a more ill-defined second stage that may or may not include delayed pushing or the duration between when a cesarean delivery has been decided upon and when it has been performed. The exclusion of the latter interval is particularly important, as “prolonged” second stages that include this duration may not reflect the length of the second stage itself, but prolonged time in effecting a cesarean delivery. The study has additional strengths, including its large sample size, its geographically and demographically diverse population, and data that are derived from direct chart abstraction by trained research personnel.
Nevertheless, the limitations of this study with regard to translation to clinical practice should be noted. These are observational data, and it cannot be known whether the relationships are causal or whether avoiding a longer second stage would necessarily avert adverse outcomes. It is possible, for example, that a higher chance of postpartum hemorrhage is not directly due to longer pushing per se, but is more likely in women who require that duration of time to deliver. If this were the case, earlier intervention would not lessen the risk of the complication. Also, we do not know the orientation of the vertex as pushing began or as the second stage progressed. And, the findings should not be interpreted to set a single standard with regard to the optimal duration of pushing for all women. Indeed, this study demonstrates that there is a not a single time at which obstetric outcomes suddenly become worse. Accordingly, for any individual woman, the weighing of risks and benefits will have to account for a variety of individual factors such as the estimated fetal weight, the assessment of fetal status, the extent of descent in the pelvis, and the presence of continued descent with pushing.
The prevention of unnecessary cesarean deliveries and the reduction of maternal and neonatal morbidity remain important goals. There is no one risk-free solution regarding labor management or route of delivery, and maternal and neonatal risks are sometimes in conflict. These data should give providers confidence that in the significant majority of women, overall outcomes remain good even after “prolonged” durations of active pushing.
Supplementary Material
Acknowledgements
Supported by grants from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) [HD21410, HD27869, HD27915, HD27917, HD34116, HD34208, HD36801, HD40500, HD40512, HD40544, HD40545, HD40560, HD40485, HD53097, HD53118] and the National Center for Research Resources [UL1 RR024989; 5UL1 RR025764]. Comments and views of the authors do not necessarily represent views of the NICHD.
The authors thank Cynthia Milluzzi, R.N. and Joan Moss, R.N.C., M.S.N. for protocol development and coordination between clinical research centers; Madeline M. Rice, Ph.D. and Elizabeth Thom, Ph.D. for protocol and data management and statistical analysis; and Brian M. Mercer, M.D. and Catherine Y. Spong, M.D. for protocol development and oversight.
Footnotes
Financial Disclosure
The authors did not report any potential conflicts of interest.
Dr. Rouse, Associate Editor of Obstetrics & Gynecology, was not involved in the review or decision to publish this article.
References
- 1.Caughey AB, Cahill AG, Guise JM, Rouse DJ. Safe prevention of the primary cesarean delivery. Am J Obstet Gynecol. 2014;210:179–93. doi: 10.1016/j.ajog.2014.01.026. [DOI] [PubMed] [Google Scholar]
- 2.Rouse DJ, Weiner SJ, Bloom SL, et al. Second-stage labor duration in nulliparous women: relationship to maternal and perinatal outcomes. Am J Obstet Gynecol. 2009;201(357):e1–7. doi: 10.1016/j.ajog.2009.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Le Ray C, Audibert F, Goffinet F, Fraser W. When to stop pushing: effects of duration of second-stage expulsion efforts on maternal and neonatal outcomes in nulliparous women with epidural analgesia. Am J Obstet Gynecol. 2009;201(361):e1–7. doi: 10.1016/j.ajog.2009.08.002. [DOI] [PubMed] [Google Scholar]
- 4.Cheng YW, Hopkins LM, Caughey AB. How long is too long: does a prolonged second stage of labor in nulliparous women affect maternal and neonatal outcomes? Am J Obstet Gynecol. 2004;191:933–8. doi: 10.1016/j.ajog.2004.05.044. [DOI] [PubMed] [Google Scholar]
- 5.Cheng YW, Hopkins LM, Laros RK Jr, Caughey AB. Duration of the second stage of labor in multiparous women: maternal and neonatal outcomes. Am J Obstet Gynecol. 2007;196(585):e1–6. doi: 10.1016/j.ajog.2007.03.021. [DOI] [PubMed] [Google Scholar]
- 6.Grobman WA, Bailit JL, Rice MM, et al. Can differences in obstetric outcomes be explained by differences in the care provided? The MFMU Network APEX study. Am J Obstet Gynecol. 2014;211(147):e1–147. doi: 10.1016/j.ajog.2014.03.017. e16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bailit JL, Grobman WA, Rice MM, et al. Risk-adjusted models for adverse obstetric outcomes and variation in risk-adjusted outcomes across hospitals. Am J Obstet Gynecol. 2013;209(446):e1–446. doi: 10.1016/j.ajog.2013.07.019. e30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Laughon SK, Berghella V, Reddy UM, et al. Neonatal and Maternal Outcomes With Prolonged Second Stage of Labor Obstet Gynecol. 2014;124:57–67. doi: 10.1097/AOG.0000000000000278. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.