Abstract
Acute cholecystitis and other clinical problems requiring gallbladder removal or drainage have conventionally been treated with surgery, endoscopic retrograde cholangiopancreatography or percutaneous transhepatic drainage of the gallbladder and/or extrahepatic bile duct. Patients unable to undergo these procedures due to functional status or anatomical anomalies are candidates for endoscopic ultrasound (EUS)-guided gallbladder drainage with stent placement. The aim of this review was to evaluate the technical feasibility and efficacy of EUS-guided placement of the recently developed lumen-apposing self-expandable metallic stent (LASEMS). A literature review was performed to identify the studies describing this technique. In this review article we have summarized case series or reports describing EUS-guided LASEMS placement. The indications, techniques, limitations and complications reported are discussed. A total of 78 patients were included across all studies described thus far in the literature. Studies have reported near 100% technical and clinical success rates in selected cases. No major complications were reported. EUS-guided gallbladder drainage and LASEMS placement can be a safe and effective alternative approach in the management of selected patients.
Keywords: Endoscopic ultrasound, gallbladder drainage, lumen-apposing stent, AXIOS
Introduction
Acute cholecystitis and other biliary pathologies are commonly treated with modalities such as surgical intervention, percutaneous transhepatic gallbladder drainage (PTGBD), or endoscopic retrograde cholangiopancreatography (ERCP) depending upon the patient’s condition. In some cases, a modality such as surgery is unsuitable for patients of advanced age or with underlying comorbidities [1]. Non-surgical gallbladder drainage (GBD) is carried out by percutaneous and endoscopic drainage procedures for these patients. Though PTGBD is the most established second-line therapy for GBD in many cases, it may be inappropriate for some patients. Furthermore, patient discomfort and post-procedure pain have been associated with percutaneous drainage catheters. Catheter dislodgment or migration is a fairly common complication occurring in up to 12% of patients [2-5].
Endoscopic ultrasound (EUS)-guided GBD is recently gaining favor as an attractive alternative for managing acute cholecystitis in high-risk patients. EUS-GBD presents the endoscopist with the advantage of avoidance of external drainage and the potential for minimal risk of post-ERCP pancreatitis or cholangitis [6]. Currently, endoscopic GBD techniques include trans-papillary nasogallbladder drainage (ENGBD), transpapillary gallbladder stenting, and EUS-GBD. Ongoing advances in these EUS techniques and accessories have led to the development of various types of stents, most recently the lumen-apposing self-expandable metallic stent (LASEMS). Conventional stents still have a chance of migration or leakage that can lead to serious adverse events, a less likely complication with the new lumen-apposing stent (AXIOS; Xlumena Inc, Mountain View, Calif) (Fig. 1, 2). AXIOS is a fully covered nitinol stent with bilateral anchor flanges and a silicone covering that prevents potential bile leakages and tissue ingrowth. The anchors maintain attachment to gastric/duodenal and gallbladder walls, allowing fistula forming and maturation and therefore lowering the likelihood of stent migration [7-12].
Figure 1.
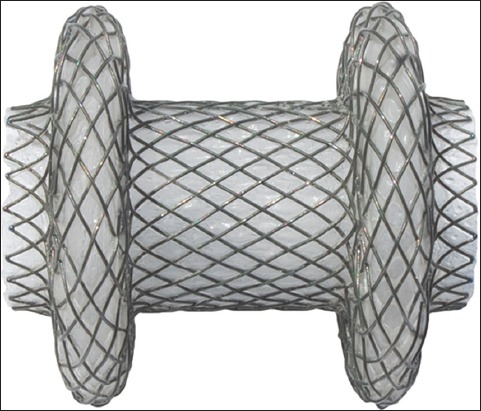
AXIOS stent
Figure 2.
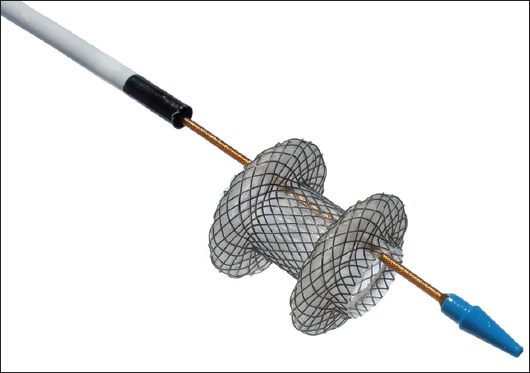
AXIOS Stent delivery system
Few authors have recently described successful use of the LASEMS in EUS-GBD. In the present review the indications, techniques, success rates, limitations, and complications reported with EUS-GBD using the LASEMS are described.
Materials and methods
An extensive English language literature search was conducted using PubMed, Medline, and Google to identify peer-reviewed original and review articles using the keywords ‘endoscopic ultrasound’, ‘lumen-apposing self-expandable metallic stent’, ‘gallbladder’, and ‘biliary drainage’. Only articles in humans were selected. The references of pertinent studies were manually searched to identify additional relevant studies. The indications, procedural details, technical and clinical success rates, complications, and limitations were considered as part of the inclusion criteria. Search results yielded mostly small sample sized prospective studies including case reports and case series, which limited statistical analysis in the form of meta-analysis.
Results
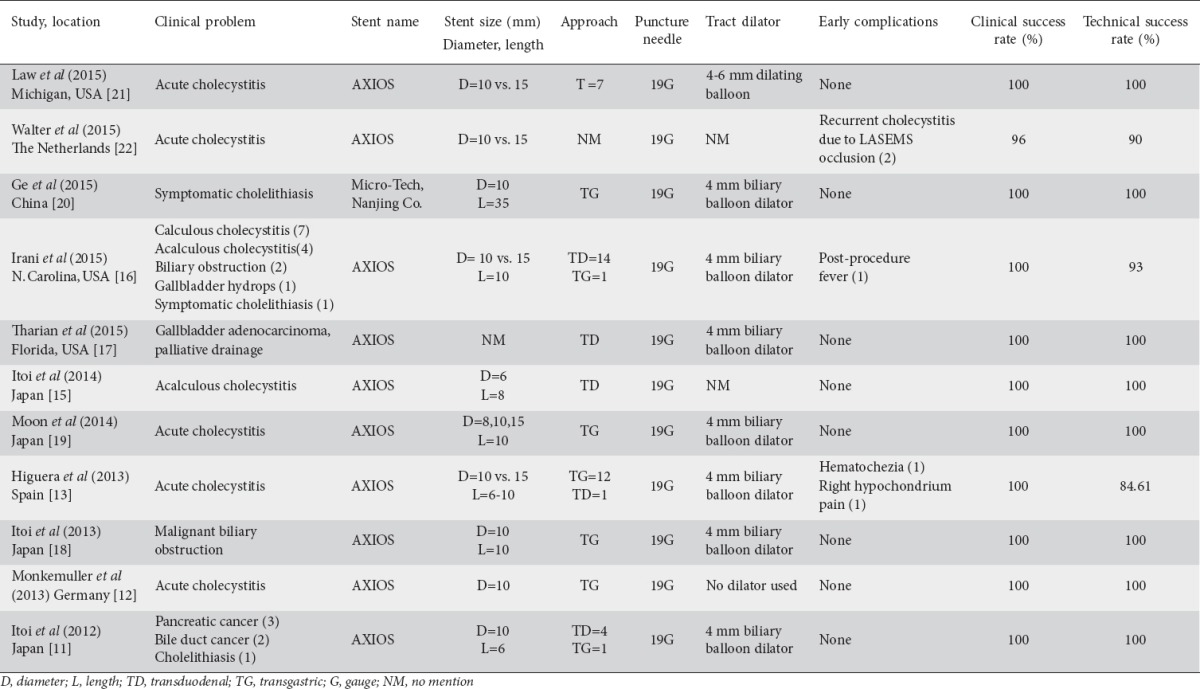
Eleven original articles published were considered appropriate to be included in the review article. Of these, five were case reports from China [20], Florida, USA [17], Japan [15,18], and Germany [12] while the other six were case series from North Carolina, USA [16], Japan [11,19], Spain [13], the Netherlands [22], and Michigan, USA [21]. The total number of patients included across all studies was 78. All cases have been summarized in Tables 1 and 2.
Table 1.
Patient characteristics in lumen-apposing self-expandable metallic stent cases

Table 2.
Summary of reports describing endoscopic ultrasound-guided gallbladder drainage with lumen-apposing self-expandable metallic stent (LASEMS)
Indications
Usual indications for EUS-GBD were acute cholecystitis or other biliary obstruction caused by malignancy or cholelithiasis outside of the cystic duct not amenable to treatment by invasive procedures such as surgery due to the patient’s poor clinical status.
Etiology
The clinical problems varied among patients, however calculous or acalculous cholecystitis comprised 52/78 (67%) of cases. Other etiologies warranting EUS with GBD and placement of a LASEMS included symptomatic cholelithiasis and palliative GBD in the setting of malignancy.
Technique
An oblique/forward-viewing therapeutic linear array echoendoscope was used in most cases. Punctures were performed with a 19-gauge needle under direct EUS visualization from the distal gastric antrum or duodenal bulb to access the gallbladder body, avoiding any vessels. After stylet removal, bile was aspirated and sent for culture, and cholecystography was performed by injection of contrast medium. A 0.035-inch guidewire was then passed and the tract dilated by use of a cystotome and, in most cases, a 4-mm biliary balloon dilator. Finally, the AXIOS stent was inserted under direct fluoroscopic and EUS control. Sometimes, at the discretion of the endoscopist, a 10-mm balloon dilator could be inflated within the AXIOS lumen to achieve more rapid deployment and prevent potential dislodgement. Standard or ultraslim endoscopes were then introduced into the gallbladder to aspirate pus and sludge or for stone removal or to lavage with saline. A second tubular self-expandable metallic stent (SEMS) could be inserted through the AXIOS lumen to prevent dislodgement in the case of doubts about the proper anchoring of the distal flange, especially in patients with very thick gallbladder walls [13,14].
In the articles reviewed, a transgastric approach via the antral wall was performed in 20/48 (42%) patients while a transduodenal approach was performed in 28/48 (50%) cases. Most studies did not mention the reason for a transgastric vs. transduodenal approach however, in Walter et al [22], the duodenal approach was the preferred method of access as it was hypothesized that duodenal access may lead to less tissue overgrowth over time. Walter et al [22] hypothesized that duodenal access allows for a more stability of the tract to the gallbladder and that a gastric approach may lead to more tissue overgrowth due to frequent peristalsis resulting in more risk for tissue reaction.
In all cases a 19-gauge EUS fine-needle was used and puncture was performed under direct EUS visualization from the distal gastric antrum or duodenal bulb to access the gallbladder body. A 0.035-inch guidewire was passed and the tract dilated by sequential use of, in most cases, a 4-mm biliary balloon dilator. The LASEMS was inserted under direct fluoroscopic and EUS control. The AXIOS stent was used in 77/78 (98%) patients.
Technical and clinical success rate
The combined clinical success rate was 99.6% in all case reports and series with most studies measuring success as clinical improvement and alleviation of pain symptoms. The combined technical success rate was 97%. Studies that reported lower technical success rates were Higuera et al [13], Irani et al [16], and Walter et al [22]. In Higuera et al [13], the insertion of the AXIOS stent was successful in 11 of 13 patients and the two cases that failed were due to: 1) uncontrolled stent release and complete deployment into the gastric lumen; and 2) cobblestone gallbladder preventing deep insertion and progression of the guide-wire. In Irani et al [16], one patient experienced intra-procedural migration of the distal flange of the stent into the peritoneum. In Walter et al [22], technical failures occurred in 3 of 30 patients (10%). The 3 cases of LASEMS placement that were unsuccessful were remedied by the placement of an additional stent to allow for successful endoscopic GBD. Walter et al [22] argued that there may be more technical failures with the placement of LASEMS that are not reported due to the remediation of the problem by adding an additional stent. For example, in Higuera et al [13], technical failures were reported in 11 of 13 patients (85%), however four patients required a second fully covered tubular SEMS inserted through the LASEMS to ensure stent patency and stability. If these additional stent cases were included in technical failures of LASEMS, the technical success rate of the study would decrease to 46%.
Complications
No major acute complications were reported after insertion of LASEMS. Minor early complications were only reported in Irani et al [13] and Higuera et al [16]. In Irani et al [13], one patient reported post-procedural fever while in Higuera et al [16] one patient experienced hematochezia without anemia post-operatively while the other reported hypochondrium pain that was alleviated by analgesics. No report of stent migration was reported in any case. The only study included that reported side effects of LASEMS over a longer term (3 months) was the study by Walter et al [22]. In this study, patients did not undergo stent removal until 3 months and this resulted in significant tissue overgrowth in 3 patients. Two of 27 (7%) patients developed recurrent cholecystitis due to LASEMS obstruction.
Limitations
Thus far, clinically successful cases have been published with few complications reported, but this may be due to a publication bias as the procedure is fairly new. As more technically and clinically relevant cases are published, further data may be assessed regarding the potential uses of LASEMS. Furthermore, technical success rates may be over-estimated, as some studies did not take into account that use of additional stents to ensure patency of LASEMS may be considered a technical failure.
Discussion
Laparoscopic cholecystectomy is the treatment of choice in patients with acute cholecystitis [1,2]; however, the procedure may be unsuitable for patients with poor surgical performance. PTGBD is currently the treatment of choice for these patients who do not respond to conservative treatment [3,4]; however, this procedure has several drawbacks including bleeding and catheter dislodgement in up to 12% of patients [5]. EUS-GBD can be a safe and minimally invasive alternative approach to surgery in selected patients who fail PTGBD. EUS-guided placement of a LASEMS recently has been used to avoid drawbacks of previously used plastic and tubular stents. In the past, plastic stents have limited bile flow and conventional tubular SEMS have carried a high risk of migration and biliary leak. The new LASEMS avoids these drawbacks by means of distal anchor flanges that ensure both lumen apposition and drainage. In the majority of patients in our review, the AXIOS stent was utilized with few minor acute complications and 99.6% clinical success.
Though no major complications have been reported using LASEMS in this review, potential serious complications of this technique do exist. Major complications include air or bile leakage into the peritoneal cavity as a result of stent insertion, perforation, and bleeding. Other complications include stent migration, obstruction, tissue overgrowth, and recurrent cholecystitis [22]. In Walter et al [22], long-term complications were observed and included tissue overgrowth and stent obstruction in 2 patients, however no cases resulted in stent migration. This may be due in part to the lumen-apposing feature of the new LASEMS. In patients in whom placement of LASEMS proves technically difficult or in whom tissue overgrowth is anticipated, additional tubular, SEMS may be placed to ensure patency and stability of fistula tract and to improve GBD [21,22]. Furthermore, in order to improve technical success, refinements of the current LASEMS and accessories may improve the results of EUS-GBD. The LASEMS used in the studies included in this review did not include a new delivery system with electrocautery on the tip, which allows puncture and release of the stent in a single-step procedure, which decreases the number of accessories to be exchanged and potentially reduces the frequency of complications. This newly developed device (Hot Axios, Xlumena, Mountain View, California, USA) may be used for GBD but is a challenging procedure and thus must be performed by appropriately trained gastroenterologists. As reported by Law et al [21], LASEMS may also be used as a secondary intervention for the purposes of internalizing GBD in patients following placement of a percutaneous cholecystostomy. Placement of a LASEMS in patients with an indwelling percutaneous drain offers more technical challenges. The LASEMS mounted onto a cautery-tipped delivery system could greatly simplify EUS-guided transmural LASEMS placement [22].
The majority of the studies included (10/11) reported short-term complications of LASEMS placement and short-term removal. No major adverse events were reported with stent removal and timing of stent removal ranged from removal during the same admission as insertion to weeks following discharge. In Walter et al [22], long-term results were reported for LASEMS insertion and removal. In this study, more than half of patients did not have stent removal due to poor clinical condition or patient refusal. In these patients, no LASEMS-related complications were observed for a mean stent dwelling time of about one year. Long-term stenting without stent-related complications has been reported in the literature and leaving the LASEMS permanently in place avoids the risks and discomfort associated with a repeat procedure for stent removal. Furthermore, many patients are high risk for surgery and though percutaneous drainage is intended to be a bridge to surgical intervention, many patients remain high-risk candidates and therefore never receive the intervention. To reduce the risk of recurrent cholecystitis in these patients, permanent drainage is desirable. The advantage of EUS-GBD compared with PTGBD is that long-term stenting does not require an external drainage catheter, which likely may increase patients’ comfort and quality of life.
This is the first review article reporting clinical and technical results of the LASEMS stent selectively designed for GBD. It shows that the lumen-apposing stent may be, in the future, a feasible and safe alternative to PTGBD in selected patients. In the cases described in the literature, all the patients progressed adequately in a short period of time without significant complications related to the procedure. Preliminary reports appear promising and large multi-center prospective studies are needed in the future to further determine its safety and efficacy. With further experience and the development of more sophisticated accessories, the arena of EUS-GBD and stent placement is likely to expand and the technique has the potential to not only treat biliary pathology but also to facilitate a mode of communication between non-adhering intra-abdominal organs for delivery of further therapy.
Concluding remarks
The technical and clinical success of the LASEMS has proven thus far in clinical case reports and prospective studies to be a safe and feasible alternative to currently accepted methods of GBD. In the future, larger prospective, randomized control trials are needed to validate these preliminary findings.
Biography
Mount Sinai Health Systems New York, USA; The Brooklyn Hospital Center Academic Affiliate of The Icahn School of Medicine at Mount Sinai Clinical Affiliate of The Mount Sinai Hospital, Brooklyn, New York; MD Anderson Cancer Center Academic and Clinical Affiliate of the University of Texas, Houston, USA
Footnotes
Conflict of Interest: None
References
- 1.Kiviluoto T, Siren J, Luukonen P, et al. Randomised trial of laparoscopic cholecystectomy for acute and gangrenous cholecystitis. Lancet. 1998;351:321–325. doi: 10.1016/S0140-6736(97)08447-X. [DOI] [PubMed] [Google Scholar]
- 2.Borzellino G, Saverland S, Minicozzi AM. Laparoscopic cholecystectomy for severe acute cholecystitis:a meta-analysis of results. Surg Endosc. 2008;22:8–15. doi: 10.1007/s00464-007-9511-6. [DOI] [PubMed] [Google Scholar]
- 3.Kalloo AN, Thuluvath PJ, Pasricha RJ. Treatment of high-risk patients with symptomatic cholelithiasis by endoscopic gallbladder stenting. Gastrointest Endosc. 1994;40:608–610. doi: 10.1016/s0016-5107(94)70263-2. [DOI] [PubMed] [Google Scholar]
- 4.Johlin FC, Jr, Neil GA. Drainage of the gallbladder in patients with acute acalculous cholecystitis by transpapillary endoscopic cholecystostomy. Gastrointest Endosc. 1993;39:645–651. doi: 10.1016/s0016-5107(93)70216-3. [DOI] [PubMed] [Google Scholar]
- 5.Itoi T, Sofuni A, Itokawa F, et al. Endoscopic transpapillary gallbladder drainage in patients with acute cholecystitis in whom percutaneous transhepatic approach is contraindicated or anatomically impossible. Gastrointest Endosc. 2008;68:455–460. doi: 10.1016/j.gie.2008.02.052. [DOI] [PubMed] [Google Scholar]
- 6.Baron TH, Topazian MD. Endoscopic transduodenal drainage of the gallbladder:implications for endoluminal treatment of gallbladder disease. Gastrointest Endosc. 2007;65:735–737. doi: 10.1016/j.gie.2006.07.041. [DOI] [PubMed] [Google Scholar]
- 7.Binmoeller KF, Shah J. A novel lumen-apposing stent for transluminal drainage of nonadherent extraintestinal fluid collections. Endoscopy. 2011;43:337–342. doi: 10.1055/s-0030-1256127. [DOI] [PubMed] [Google Scholar]
- 8.Pannala R, Petersen BT, Gostout CJ, Topazian MD, Levy MJ, Baron TH. Endoscopic transpapillary gallbladder drainage:10-year single center experience. Minerva Gastroenterol Dietol. 2008;54:107–113. [PubMed] [Google Scholar]
- 9.Mutignani M, Iacopini F, Perri V, et al. Endoscopic gallbladder drainage for acute cholecystitis:Technical and clinical results. Endoscopy. 2009;41:539–546. doi: 10.1055/s-0029-1214727. [DOI] [PubMed] [Google Scholar]
- 10.Itoi T, Coelho-Prabhu N, Baron TH. Endoscopic gallbladder drainage for management of acute cholecystitis. Gastrointest Endosc. 2010;71:1038–1045. doi: 10.1016/j.gie.2010.01.026. [DOI] [PubMed] [Google Scholar]
- 11.Itoi T, Binmoeller KF, Shah J, et al. Clinical evaluation of a novel lumen-apposing metal stent for endosonography-guided pancreatic pseudocyst and gallbladder drainage (with videos) Gastrointest Endosc. 2012;75:870–876. doi: 10.1016/j.gie.2011.10.020. [DOI] [PubMed] [Google Scholar]
- 12.Monkemuller K, Zabielski M, Didowacz-Grollmann A, von Gruchalla C, Neumann H, Vormbrock K. Endoluminal trans-gastric endoscopic anastomosis of the gallbladder using an anchoring self-expanding metal stent. Endoscopy. 2013;45:164–166. doi: 10.1055/s-0032-1325776. [DOI] [PubMed] [Google Scholar]
- 13.de la Serna-Higuera C, Perez-Miranda M, Gil-Simon P, et al. EUS-guided transenteric gallbladder drainage with a new fistula-forming, lumen-apposing metal stent. Gastrointest Endosc. 2013;77:303–308. doi: 10.1016/j.gie.2012.09.021. [DOI] [PubMed] [Google Scholar]
- 14.Itoi T, Binmoeller K. EUS-guided choledochoduodenostomy by using a biflanged lumen-apposing metal stent. Gastrointest Endosc. 2014;79:715. doi: 10.1016/j.gie.2013.11.021. [DOI] [PubMed] [Google Scholar]
- 15.Itoi T, Itokawa F, Kurihara T, et al. Transgastric large gallstone extraction through a lumen-apposing metal stent in a patient with acute cholecystitis. Gastrointest Endosc. 2014;79:547. doi: 10.1016/j.gie.2013.12.010. [DOI] [PubMed] [Google Scholar]
- 16.Irani S, Baron T, Grimm I, et al. EUS-guided gallbladder drainage with a lumen-apposing metal stent (with video) Gastrointest Endosc. 2015;82:1110–1115. doi: 10.1016/j.gie.2015.05.045. [DOI] [PubMed] [Google Scholar]
- 17.Tharian B, Varadarajulu S, Hawes R. Drainage of obstructed gallbladder with use of lumen-apposing metal stent. Gastrointest Endosc. 2016;83:460–461. doi: 10.1016/j.gie.2015.08.016. [DOI] [PubMed] [Google Scholar]
- 18.Itoi T, Binmoeller K, Fumihide I, et al. Endoscopic ultrasonography-guided cholecystogastrostomy using a lumen-apposing metal stent as an alternative to extrahepatic bile duct drainage in pancreatic cancer with duodenal invasion. Dig Endosc. 2013;25:137–141. doi: 10.1111/den.12084. [DOI] [PubMed] [Google Scholar]
- 19.Moon J, Choi H, Kim D, et al. A newly designed fully covered metal stent for lumen apposition in EUS-guided drainage and access:a feasibility study (with videos) Gastrointest Endosc. 2014;79:990–995. doi: 10.1016/j.gie.2014.02.015. [DOI] [PubMed] [Google Scholar]
- 20.Ge N, Wang S, Sun S, et al. Endoscopic ultrasound-assisted cholecystogastrostomy by a novel fully covered metal stent for the treatment of gallbladder stones. Endosc Ultrasound. 2015;2:152–155. doi: 10.4103/2303-9027.156749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Law R, Grimm IS, Stavas JM, Baron TH. Conversion of percutaneous cholecystostomy to internal transmural gallbladder drainage using an endoscopic ultrasound-guided, lumen-apposing metal stent. Clin Gastroenterol Hepatol. 2016;14:476–480. doi: 10.1016/j.cgh.2015.10.026. [DOI] [PubMed] [Google Scholar]
- 22.Walter D, Teoh AY, Itoi T, et al. EUS-guided gall bladder drainage with a lumen-apposing metal stent:a prospective long-term evaluation. Gut. 2016;65:6–8. doi: 10.1136/gutjnl-2015-309925. [DOI] [PubMed] [Google Scholar]


