Abstract
The video-assisted thoracoscopic surgery (VATS) approach for combined lobectomy and segmentectomy in the same lung is an infrequent procedure, rarely reported in the literature. Currently, Most of the surgeons still use 2–3 thoracic incisions for thoracoscopic anatomic resections. However, the uniportal approach is gaining worldwide acceptance in the recent years. The main advances of uniportal VATS during the last years are related to improvements in surgical technique by implementing new technology. The experience acquired with the uniportal technique allows expert uniportal VATS surgeons to explore new approaches in order to minimize even more the surgical invasiveness. Recently the aim to avoid the intercostal nerve damage created by the transthoracic incision has led to the creation of a novel procedure entitled uniportal VATS subxiphoid approach. Here we report the first case of a lobectomy combined with anatomic segmentectomy performed through a uniportal subxiphoid approach.
Keywords: Subxiphoid approach, uniportal VATS, segmentectomy, lobectomy, uniportal subxiphoid
Introduction
The video-assisted thoracoscopic surgery (VATS) approach for combined lobectomy and segmentectomy is an infrequent procedure, rarely reported in the literature. There is no doubt that VATS is currently a better choice than thoracotomy for segmentectomies. However, anatomical segmental resections are more demanding procedures because they require a better knowledge of the distal lung anatomy (1). These lung sparing procedures are usually indicated for deeply located benign lesions, metastasis or early stage lung cancer such as ground glass opacities (GGO). Several studies recently published have shown that segmentectomies can be performed safely without compromising oncologic results in this group of patients (2).
Most of the surgeons doing segmentectomies implement a thoracoscopic approach through a transthoracic utility incision of 4–6 cm, with one to three additional ports in different positions (3). However, the anatomic resection can be performed by opening only one intercostal space, through a single utility incision. Since 2011, when the first uniportal VATS lobectomy was published (4), the single incision technique has been stablished as the approach of choice in many thoracic departments all over the world (5,6). Since then, a growing number of articles are available in the literature showing the feasibility, safety and good outcomes of this procedure for major pulmonary resections (7,8). Recently the aim to avoid the intercostal nerve damage created by the transthoracic ports has led to the creation of a novel procedure described in 2014 for lobectomy through a single subxiphoid incision (9). Here we report the first case of a lobectomy combined with anatomic segmentectomy performed through a uniportal subxiphoid approach (10).
Clinical case
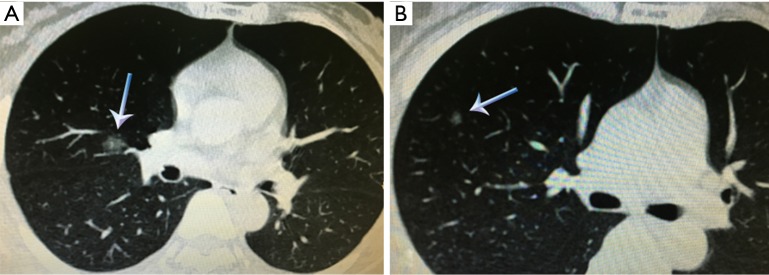
A 53-year-old female was admitted to our department for surgery. The patient suffered from cough, and a CT scan revealed two GGO lesions located in the Middle lobe and anterior segment of RUL (S3) respectively (Figure 1). Pulmonary function tests were normal. The patient was proposed for uniportal VATS subxiphoid middle lobectomy and anterior anatomic segmentectomy of the right upper lobe.
Figure 1.
CT scan showing the GGO lesions located on the middle lobe (A) and on the anterior segment of the right upper lobe (B).
Surgical technique (Figure 2)
Figure 2.
Subxiphoid uniportal video-assisthed thoracoscopic middle lobectomy and anterior anatomic segmentectomy (10). Available online: http://www.asvide.com/articles/904
The procedure was performed under general anesthesia and double lumen endotracheal intubation. The patient was positioned in lateral position with 60 degrees of inclination. The surgeon and scrub nurse were located in front of the patient and the assistant in the opposite side. A 3-cm midline vertical incision was made below the sterno-costal triangle, (longitudinal incision is made when the infrasternal angle is <70°). The rectus abdominis was divided and the xiphoid process was partially resected in order to have more space for instrumentation. Upon finding the infra-sternal angle between the xiphoid process and the subcostal margin, the right pleura was opened by finger dissection via the infra-sternal angle above the level of the diaphragm. The pericardial fatty tissue was removed and a wound protector was placed. The use of a wound protector helps the insertion of the camera and instruments, without the need of a sternal lifter. A 10-mm, 30-degrees video camera and double articulated instruments combined with several specific longer VATS instruments were used through the same subxiphoid incision. The lung was free of adhesions and a middle lobectomy and anterior anatomic segmentectomy of the right upper lobe (S3) were performed. The mean postoperative time was 70 minutes. A single chest tube was placed at the end of the operation through the subxiphoid incision.
Postoperative pain was managed with PCA (Patient-controlled analgesia) pump as required with sufentanyl citrate 1 mL: 50 mcg and regular medication with flurbiprofen 50 mg every 4 hours alternated with paracetamol 1 gr every 4 hours.
The postoperative course of the patient was uneventful, the chest tube was removed on the second postoperative day and the patient was discharged home on the 4th postoperative day with no complications. The final pathology revealed the GGO located on the middle lobe as a 1.2-cm adenocarcinoma in situ and no malignancy was found in the anterior segment lesion of the RUL.
Discussion
The subxiphoid approach is a variant of uniportal VATS approach without opening the intercostal space. It has been employed during the last years for thoracic minor procedures such as thymectomies, pulmonary metastasectomies, pneumothorax (11,12).
However, this technique was recently introduced for major pulmonary resections in selected patients. After reviewing the literature, we have found few cases reporting about the subxiphoid approach incision for lobectomy (9) showing similar values to transthoracic uniportal VATS with regards to chest drain duration, hospital stay, operating time, rate of conversion and complications (8). Based on our previous experience with the uniportal VATS technique, we started to perform the subxiphoid approach for lobectomy with the potential advantage of decreased postoperative pain, better cosmesis and easier specimen retrieval compared to the transthoracic approach (13). Segmental anatomic resections are more complex procedures and require a perfect knowledge of the distal lung anatomy (14). The increased use of low-dose CT for screening will result in more diagnosed lung cancer in the early stage (15) therefore segmentectomy is being performing more frequently. For GGO lesions, anatomic segmentectomy should be sufficient for complete removal without risk of recurrence, and conserves an important amount of normal lung tissue in order to maintain better lung function (16).
To attempt the subxiphoid approach it is mandatory to have a previous experience in uniportal VATS lobectomies and a skilled assistant. As it happens with the transthoracic uniportal approach, bimanual instrumentation is crucial to achieve a good anatomic hilar dissection through a single incision (Figure 3). The view is caudal-cranial and anterior to posterior. The access for the view of the posterior mediastinum is difficult. Particularly challenging and difficult to accomplish is the need to apply traction to the lung in order to assess the lesions as well as the complete resection of subcarinal lymph node dissection. Moreover, this technique has several limitations such as the control of major bleeding and the performance of a complete oncologic lymph node dissection. When an emergent conversion to open surgery is necessary, an extension of the subxiphoid incision is unlikely to be useful and an additional thoracotomy must be performed. Despite these disadvantages, this novel approach has potential for widespread use after the developing of new technology, wireless cameras, instruments adapted to this approach or single port robotic technology also adapted to the subxiphoid approach (17).
Figure 3.

Surgical photo showing bimanual instrumentation through the subxiphoid incision.
Further studies are necessary to certify the feasibility and compare clinical outcomes of the subxiphoid versus other transthoracic approaches, in order to show the clear benefits from this technique.
Acknowledgements
None.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.Gonzalez-Rivas D, Mendez L, Delgado M, et al. Uniportal video-assisted thoracoscopic anatomic segmentectomy. J Thorac Dis 2013;5 Suppl 3:S226-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Watanabe A, Ohori S, Nakashima S, et al. Feasibility of video-assisted thoracoscopic surgery segmentectomy for selected peripheral lung carcinomas. Eur J Cardiothorac Surg 2009;35:775-80; discussion 780. 10.1016/j.ejcts.2009.01.013 [DOI] [PubMed] [Google Scholar]
- 3.Atkins BZ, Harpole DH, Jr, Mangum JH, et al. Pulmonary segmentectomy by thoracotomy or thoracoscopy: reduced hospital length of stay with a minimally-invasive approach. Ann Thorac Surg 2007;84:1107-12; discussion 1112-3. 10.1016/j.athoracsur.2007.05.013 [DOI] [PubMed] [Google Scholar]
- 4.Gonzalez D, Paradela M, Garcia J, et al. Single-port video-assisted thoracoscopic lobectomy. Interact Cardiovasc Thorac Surg 2011;12:514-5. 10.1510/icvts.2010.256222 [DOI] [PubMed] [Google Scholar]
- 5.Ng CS, Rocco G, Wong RH, et al. Uniportal and single-incision video-assisted thoracic surgery: the state of the art. Interact Cardiovasc Thorac Surg 2014;19:661-6. 10.1093/icvts/ivu200 [DOI] [PubMed] [Google Scholar]
- 6.Ng CS, Lau KK, Gonzalez-Rivas D, et al. Evolution in surgical approach and techniques for lung cancer. Thorax 2013;68:681. 10.1136/thoraxjnl-2012-203157 [DOI] [PubMed] [Google Scholar]
- 7.Wang BY, Liu CY, Hsu PK, et al. Single-incision versus multiple-incision thoracoscopic lobectomy and segmentectomy: a propensity-matched analysis. Ann Surg 2015;261:793-9. 10.1097/SLA.0000000000000712 [DOI] [PubMed] [Google Scholar]
- 8.Gonzalez-Rivas D, Paradela M, Fernandez R, et al. Uniportal video-assisted thoracoscopic lobectomy: two years of experience. Ann Thorac Surg 2013;95:426-32. 10.1016/j.athoracsur.2012.10.070 [DOI] [PubMed] [Google Scholar]
- 9.Liu CC, Wang BY, Shih CS, et al. Subxiphoid single-incision thoracoscopic left upper lobectomy. J Thorac Cardiovasc Surg 2014;148:3250-1. 10.1016/j.jtcvs.2014.08.033 [DOI] [PubMed] [Google Scholar]
- 10.Gonzalez-Rivas D, Yang Y, Lei J, et al. Subxiphoid uniportal video-assisthed thoracoscopic middle lobectomy and anterior anatomic segmentectomy. Asvide 2016;3:149. Available online: http://www.asvide.com/articles/904 [DOI] [PMC free article] [PubMed]
- 11.Suda T, Ashikari S, Tochii S, et al. Single-incision subxiphoid approach for bilateral metastasectomy. Ann Thorac Surg 2014;97:718-9. 10.1016/j.athoracsur.2013.06.123 [DOI] [PubMed] [Google Scholar]
- 12.Liu CY, Lin CS, Liu CC. Subxiphoid single-incision thoracoscopic surgery for bilateral primary spontaneous pneumothorax. Wideochir Inne Tech Maloinwazyjne 2015;10:125-8. 10.5114/wiitm.2015.48572 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ismail NA, Elsaegh M, Dunning J. Novel Techniques in Video-assisted Thoracic Surgery (VATS) Lobectomy. Surg Technol Int 2015;26:206-9. [PubMed] [Google Scholar]
- 14.Shiraishi T, Shirakusa T, Iwasaki A, et al. Video-assisted thoracoscopic surgery (VATS) segmentectomy for small peripheral lung cancer tumors: intermediate results. Surg Endosc 2004;18:1657-62. [DOI] [PubMed] [Google Scholar]
- 15.Zhao SJ, Wu N. Early detection of lung cancer: Low-dose computed tomography screening in China. Thorac Cancer 2015;6:385-9. 10.1111/1759-7714.12253 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shao G, Ren W, Feng Z, et al. The role of video-assisted thoracoscopic surgery in management of the multiple ground-glass nodules. Indian J Cancer 2015;52 Suppl 2:e75-9. 10.4103/0019-509X.172518 [DOI] [PubMed] [Google Scholar]
- 17.Gonzalez-rivas D, Yang Y, Calvin NG. Advances in Uniportal video-assisted thoracoscopic surgery: pushing the envelope. Thorac Surg Clinics 2016. (In press). DOI: . 10.1016/j.thorsurg.2015.12.007 [DOI] [PubMed] [Google Scholar]