Abstract
Radical surgery for tracheal tumors is typically completed under basal anesthesia. Thus, endotracheal intubation and mechanical ventilation are required. However, these procedures may influence the surgical operation and meanwhile prolong the surgical duration and postoperative recovery. In this article we describe the application of video-assisted transthoracic surgery (VATS) resection of a tracheal mass and reconstruction of trachea a non-intubated patient with spontaneous breathing.
Keywords: Tracheal mass, video-assisted transthoracic surgery (VATS), non-intubated, surgery, spontaneous respiration
Introduction
The application of video-assisted transthoracic surgery (VATS) for tracheal diseases has been reported in literature, showing satisfactory effectiveness (1,2). However, these surgical procedures typically require endotracheal intubation, chest intubation, and mechanical ventilation. Some recent articles have reported the use of segmentectomy or lobectomy in non-intubated patients with spontaneous breathing (3-5). They found that these lung surgeries were feasible and safe. In our center we have completed segmentectomy or lobectomy in more than 250 non-intubated patients with spontaneous breathing. Thus, we have accumulated rich experiences in dealing with the relevant complications and unexpected situations. In addition, repeated intubation is needed for patients undergoing surgeries for tracheal neoplasms. In order to minimize the injuries caused by endotracheal intubation and mechanical ventilation and speed up the postoperative recovery, we performed the VATS resection of a tracheal mass and reconstruction of trachea in a non-intubated patient with spontaneous breathing.
Case presentation
Subjects
A 44-year-old non-smoking female patient developed progressively worsening shortness of breath with decreased body weight in the past 2 months. She had progressive dyspnea and intermittent orthopnea. Chest computed tomography (CT) showed a tracheal mass located at the T2 and T3 vertebrae, about 3 cm away from the carina. The mass could be clearly seen under contrast-enhanced CT, with a size of 2.0 cm × 1.6 cm × 1.2 cm (Figure 1). Bronchofiberscopy showed that there was a lobulated mass inside the trachea, and the tumor almost complete blocked the trachea (Figure 2). Since the shortness of breath and dyspnea were gradually worsening, bronchofiberscopic resection of tracheal tumor was performed to alleviate the respiratory symptoms (Figure 3). The postoperative pathology confirmed that the lesion was a mucoepidermoid carcinoma. A second postoperative chest CT indicated that the residual tumor inside the trachea had invaded the entire posterior wall of trachea (Figure 4). In order to achieve satisfactory effectiveness of radical treatment, we further discussed the disease condition and treatment protocol with the patient and her family and with other colleagues in our department and then decided to carry out VATS resection of tracheal mass and reconstruction of trachea under non-intubated anesthesia with spontaneous breathing.
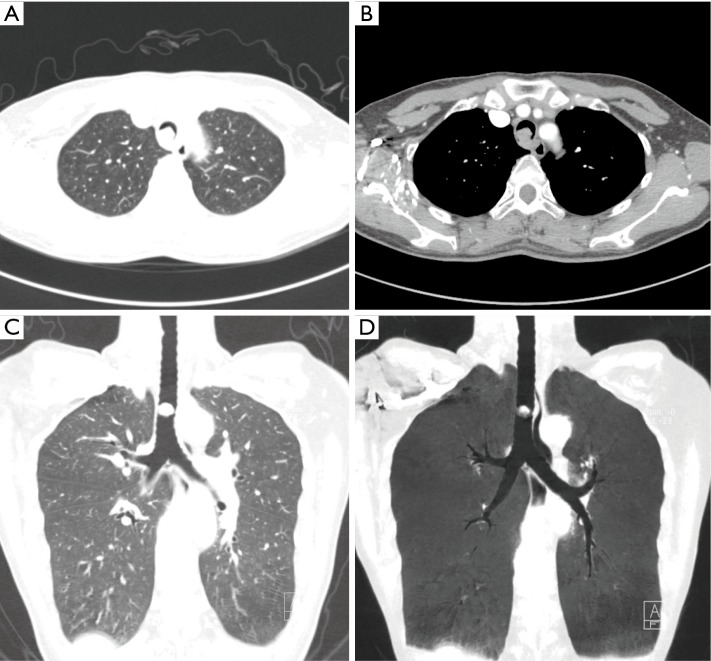
Figure 1.
Preoperative computed tomography (CT) indicated a mass sized 1.2 cm × 1.3 cm on the right posterior wall of the mid-lower trachea (6 cm away from carina). The mass protruded into the tracheal lumen, resulting in airway blockage and stenosis.
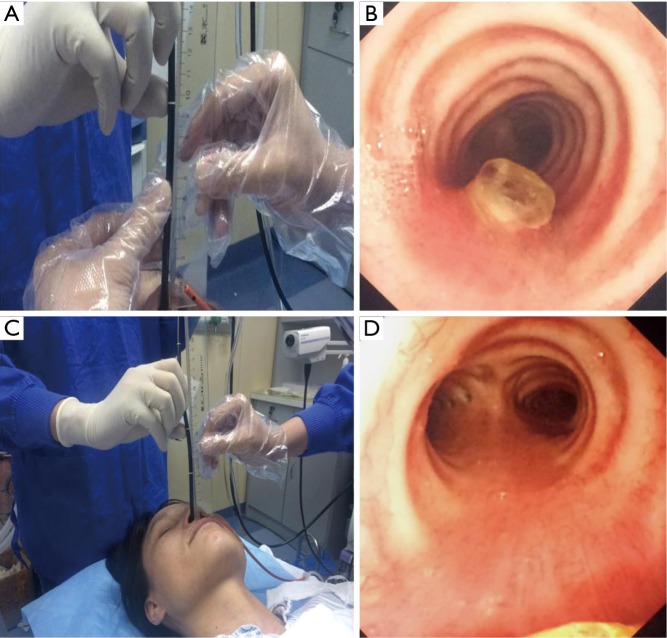
Figure 2.

Preoperative fibrobronchoscopy showed a mass sized 1.2 cm × 1.3 cm on the right posterior wall of the trachea (about 8 cm away from glottis). The mass had a gray-yellow surface, with congestive basal part. It protruded into the tracheal lumen, resulting in airway blockage and stenosis.
Figure 3.
After bronchoscopic intervention, a second preoperative bronchoscopy showed that most of the primary tumor had been resected, and the residual tumor had invaded the posterior wall of trachea. The distal and proximal ends of the residual tumor and the surgical resection range were evaluated again.
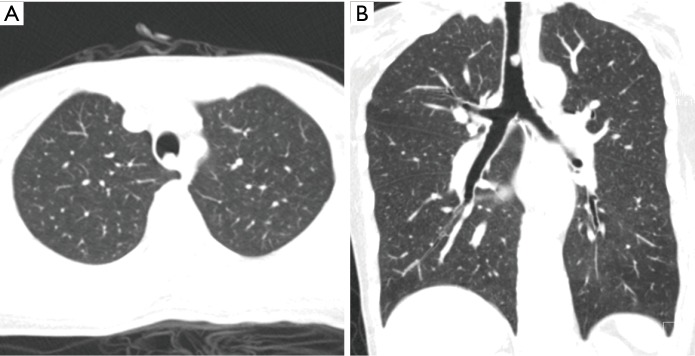
Figure 4.
A second postoperative chest computed tomography (CT) following bronchoscopic electrocautery indicated that the residual tumor was located in the mid-lower section of the trachea and 6 cm away from the carina. It had invaded the entire posterior wall of trachea, and the posterior wall of trachea was remarkably thickened.
Anesthesia
Epidural anesthesia was applied in this patient. After local anesthesia, a thoracic epidural catheter was inserted into the T7/8 intercostal space, via which 2 mL of 2% lidocaine was slowly injected for testing the anesthetic effectiveness. After the testing, 3 mL of 0.5% ropivacaine was injected into the catheter. Sufentanil (10 µg) and propofol (80 mg) were used during the induction of anesthesia. During the surgery, anesthesia was maintained using remifentanil (0.03–0.05 µg/kg per min) and propofol (0.2 mg/kg per min). Also, 40% oxygen was delivered using a laryngeal mask at a rate of 3.5 mL/min. Spontaneous breathing was maintained throughout the surgery. The depth of anesthesia was measured using the EEG bispectral index during the surgery. Finally, devices for tracheal intubation, VATS endobronchial intubation, and mechanical ventilation were also prepared to prevent emergency situation (e.g., airway obstruction) and ensure the surgical safety.
Surgical process
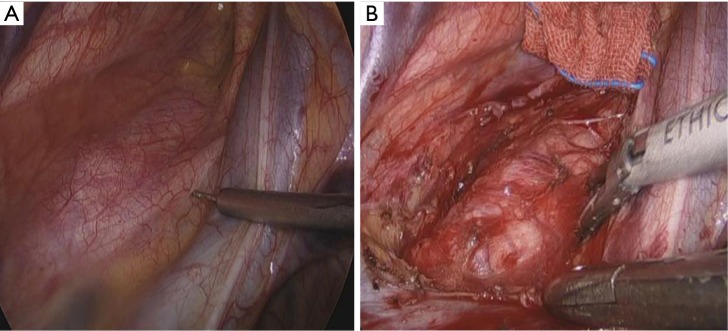
The patient was placed in a left lateral decubitus position. A 1-cm observation port was made in the 6th intercostal space at right anterior axillary line for the placement of 30° thoracoscopy. In addition, two incisions (2 cm and 0.5 cm in length, respectively) were made in the 3rd intercostal space at anterior axillary line and in the 7th intercostal space at posterior axillary line as the operation ports. Intercostal nerve block (from the second intercostal space to the seventh intercostal space) using 1% lidocaine was performed; meanwhile, 2 mL of 0.5% bupivacaine was used for vagus nerve block (Figure 5A). During the surgery, we found that the collapse of the operated lung was good; then, the lung was lifted forwards to achieve good surgical field. The trachea section from the level of suprasternal notch to the level of carina was separated (Figures 5,6,7,8), and the mass borders and the resection scope were further confirmed using bronchofiberscopy during the surgery. The tracheal mass was completely removed about 1.0 cm away from the outer margin of the tumor (Figures 9,10). Intra-operative frozen section analysis showed that the surgical margin was negative. After the reconstruction of the tracheal stump by continuous suture using 2–0 Prolene sutures, we carried out anastomotic leak test using sterile saline (Figures 11,12,13,14,15). After it was confirmed that there was no anastomotic leak or intrathoracic active bleeding, we closed the chest incisions, while two chest tubes (up and down) were remained in the thoracic cavity for drainage. The anesthesia time and surgery time were 105 minutes and 180 minutes, respectively. The intraoperative blood loss was controlled within 30 mL, and the intraoperative SpO2 was maintained between 97–100%. Blood gas analysis showed that the patient had no non-respiratory acidosis. The intraoperative EtCO2 was between 40 and 48 mmHg. The patient’s vital signs remained stable throughout the operation.
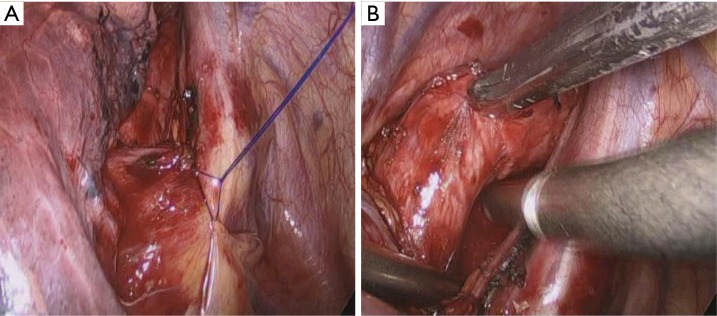
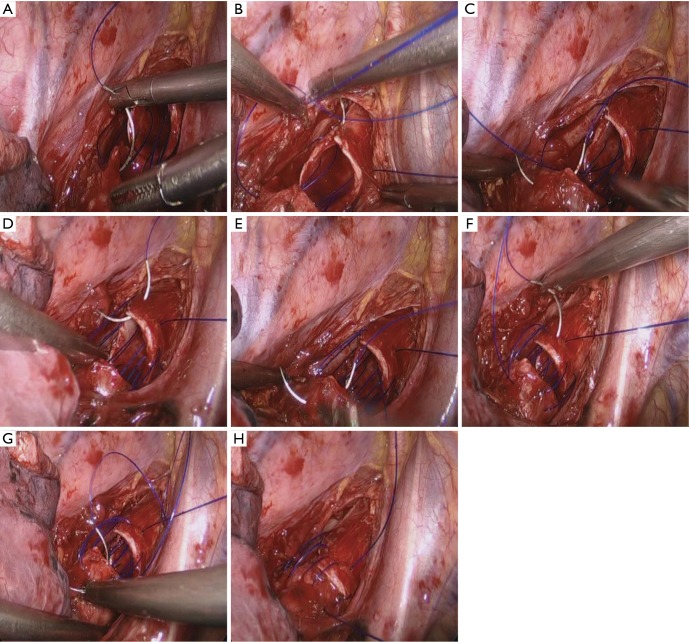
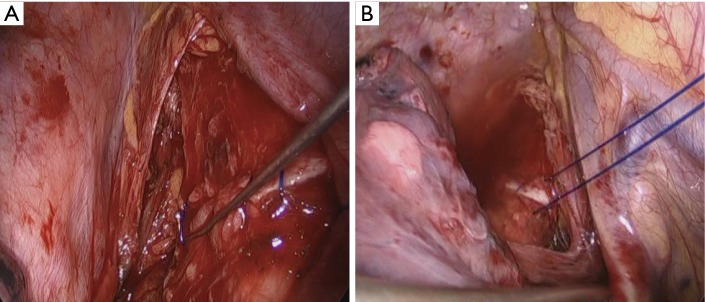
Figure 5.
Nerve blockage and surgical process. (A) Right thoracic vagus blocks were performed before surgery; (B) cut open the mediastinal pleura to dissociate the thoracic trachea.
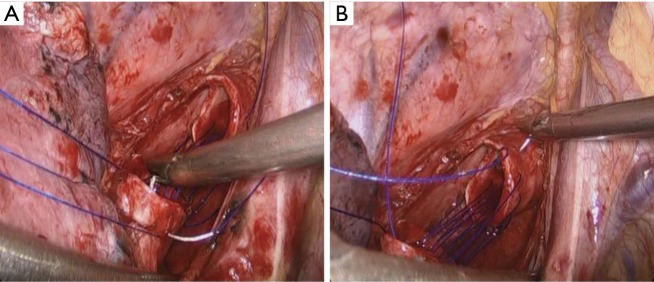
Figure 6.
Suspension of thoracic vagus nerve to protect the nerve; dissociate the tissues behind the thoracic trachea.
Figure 7.
Blunt dissociation of the posterior segment of trachea; dissociate the thoracic trachea using right-angled forceps.
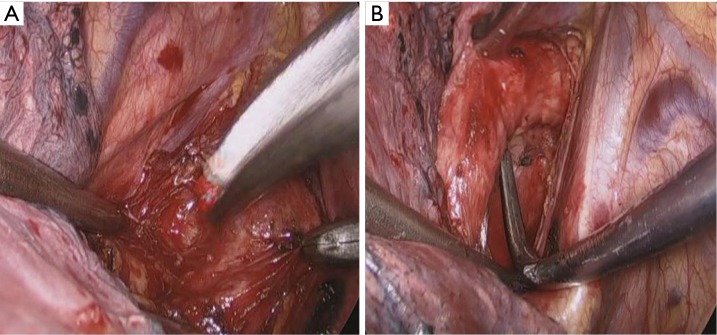
Figure 8.
Dissociate the thoracic trachea using right-angled forceps; suspend the dissociated thoracic trachea using a retraction cord.
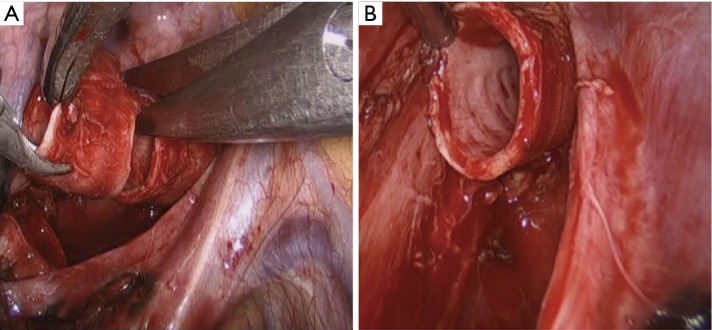
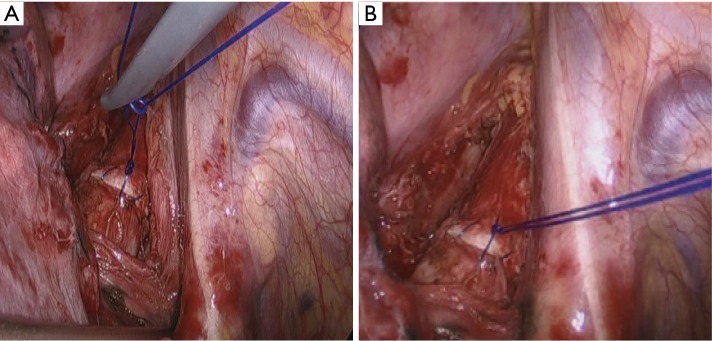
Figure 9.
Divide at the distal end of tracheal mass and at the distal end of tracheal ring.
Figure 10.
Divide at the distal end 1cm away from the lower edge of the mass.
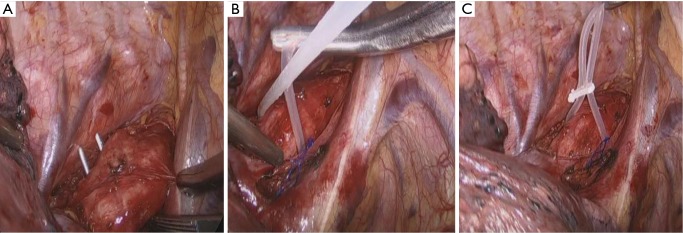
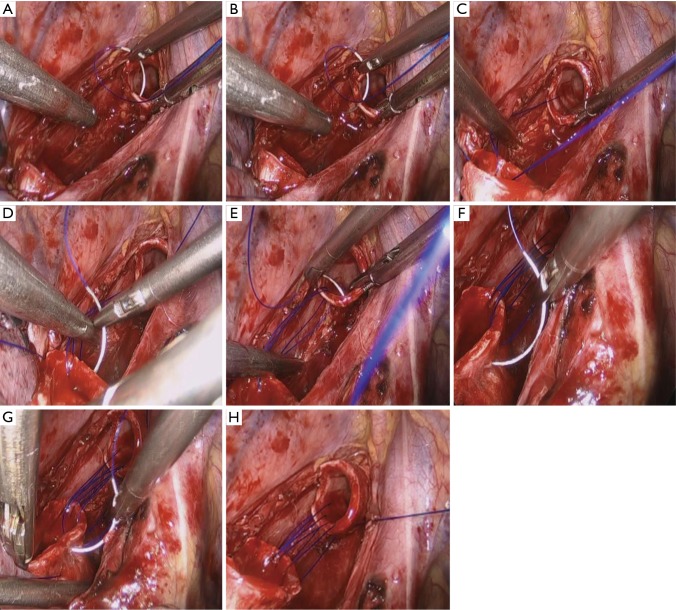
Figure 11.
After the tumor was resected, the posterior wall of the trachea was continuously closed using the Prolene sutures.
Figure 12.
The lateral wall of the trachea was continuously closed using the Prolene sutures.
Figure 13.
The anterior wall of the trachea was continuously closed using the Prolene sutures.
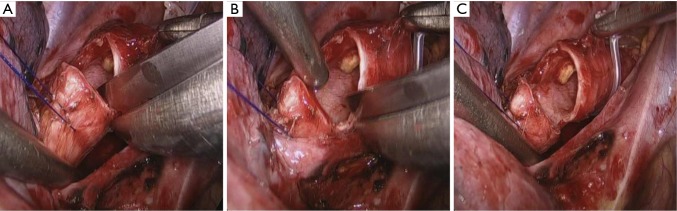
Figure 14.
The sutures were retracted stepwise using a nerve hook to tighten the anastomosis, reduce tension, and prevent the sutures to cut the anastomosis.
Figure 15.
Anastomotic leak testing; knots were tied and fixed after the anastomosis was confirmed to be leak-free.
Under non-intubated anesthesia with spontaneous breathing, the procedure was performed on July 8th 2015 (Figure 16).
Figure 16.

VATS resection of a tracheal mass and reconstruction of trachea under non-intubated anesthesia with spontaneous (6). VATS, video-assisted transthoracic surgery. Available online: http://www.asvide.com/articles/910
Postoperative outcome
Postoperative chest X-ray showed that the operated lung was well re-expanded and there was no sign of pneumothorax. The patient had no postoperative symptoms such as nausea and vomiting but complained of mild pain at the chest tube insertion site. Non-steroidal anti-inflammatory drugs and ambroxol were administered to alleviate the symptom. The patient began to eat and drink 6 hours after surgery. She was able to walk slowly 10 hours after surgery. The patient did not experience any surgery-related complication. The chest tubes were withdrawn on the second postoperative day, and the patient was discharged on the fifth postoperative day. During the 3-month follow-up, the patient had good general conditions and did not complain of any respiratory symptom.
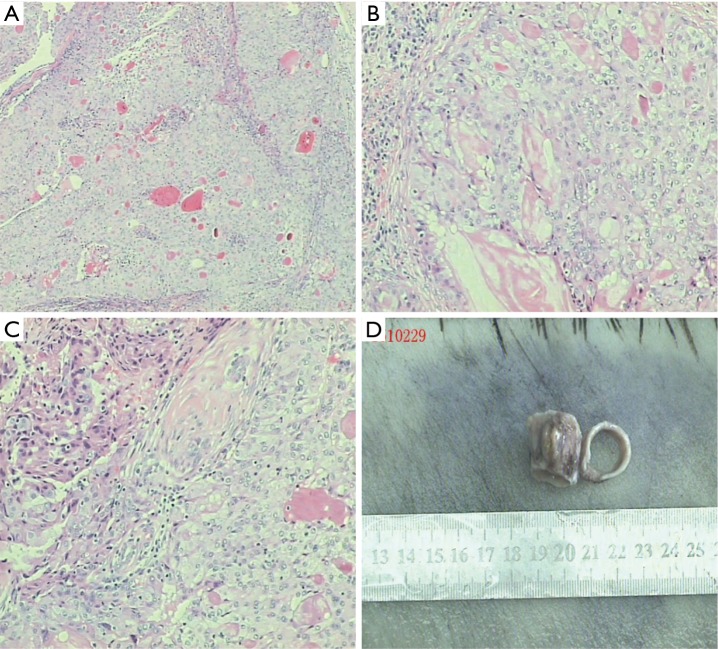
Postoperative diagnosis
The mass was pathologically diagnosed as intermediate-grade mucoepidermoid carcinoma of the trachea invading the bronchial wall. The mass was sized 1.2 cm × 1.0 cm × 0.6 cm, and it had protruded into the tracheal lumen (Figure 17).
Figure 17.
Pathology result: two parts inside the bronchus: 1.5 cm in length and 1.8 cm in diameter; and 0.6 cm in length and 1.5 cm in diameter. A 1.2 cm × 1.0 cm × 0.6 cm mass could be seen on the surface. The mass protruded into the tracheal lumen, with gray-yellow cutting surface and moderate texture (magnification, ×100).
Immunohistochemical findings: CK7 (+), Napsin A (−), TTF1 (−), Calponin (−), P63 (−), CK5/6 (−), P40 (−), and Ki67 (about 15%).
Special staining: Mayer’s dyeing (+).
Genetic testing: EGFR exon 19 deletion.
Discussion
According to our experiences, VATS procedures in non-intubated patients with spontaneous breathing have many advantages: first, the anesthesia effectiveness of this procedure is similar to the traditional anesthesia. The anesthesia depth and vital signs were maintained stably throughout the surgery, and the patient did not wake up during surgery. Second, no muscle relaxant is required during the anesthesia, thus avoiding the slow recovery of lung function and its relevant airway complications due to the use of muscle relaxant. In addition, inflammatory cytokines such as TNF-α can increase the permeability of the blood vessels and cause tissue edema. As shown in our previous study, the inflammatory cytokine levels were significantly lower in non-intubated patients than in intubated patients (7).
In our current case, the non-intubation technique under spontaneous breathing brought more benefits to the patient: it decreased the risk of hemorrhage and airway edema following tracheal intubation; meanwhile, the trachea had larger range of motion and the surgical field was clearer in the absence of tracheal intubation. Spontaneous breathing during surgery helped to maintain good hemodynamic status and blood oxygen saturation.
However, not all patients are suitable for non-intubated anesthesia under spontaneous breathing. This technique should be avoided in patients with the following conditions for safety considerations: (I) low blood volume, hemodynamic instability, or dysfunction of blood coagulation; (II) American Society of Anesthesiologists (ASA) score >3; (III) heart failure, abnormal anatomical structures, or spinal cord and peripheral nerve diseases; (IV) pulmonary insufficiency (FEV1 <60% expected value) and/or poorly controlled asthma; (V) severe pleural adhesions; (VI) BMI >25 kg/m2; and (VII) low cardiac output due to aortic stenosis, hypertrophic cardiomyopathy, severe arrhythmia, mitral stenosis, or complete atrioventricular block. Meanwhile, devices for endotracheal intubation, thoracoscopic intubation, and mechanical ventilation should also be prepared during the surgery to ensure the safety of patients. Active intervention along with endotracheal intubation or thoracoscopic intubation should be performed in case the following conditions occur during the surgery: (I) the SpO2 cannot be maintained above 90%; (II) obvious carbon dioxide retention, along with the development of respiratory acidosis; and (III) sudden bleeding that cannot be stopped quickly (7).
In this article we described the application of VATS resection of a mass and reconstruction of trachea in a non-intubated patient with spontaneous breathing. As shown by the surgical outcomes and intraoperative conditions, this anesthesia and surgical technique is feasible for patients who are unsuitable for tracheal intubation. However, the surgical team must have rich experiences in non-intubated anesthesia with spontaneous breathing and are able to properly deal with surgery-related complications.
Acknowledgements
None.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.Grillo HC. Development of tracheal surgery: a historical review. Part 1: Techniques of tracheal surgery. Ann Thorac Surg 2003;75:610-9. 10.1016/S0003-4975(02)04108-5 [DOI] [PubMed] [Google Scholar]
- 2.Nakanishi K, Kuruma T. Video-assisted thoracic tracheoplasty for adenoid cystic carcinoma of the mediastinal trachea. Surgery 2005;137:250-2. 10.1016/j.surg.2004.06.010 [DOI] [PubMed] [Google Scholar]
- 3.Al-Abdullatief M, Wahood A, Al-Shirawi N, et al. Awake anaesthesia for major thoracic surgical procedures: an observational study. European journal of cardio-thoracic surgery: official journal of the European Association for Cardio-thoracic Surgery 2007;32:346-50. [DOI] [PubMed]
- 4.Hung MH, Cheng YJ, Chan KC, et al. Nonintubated uniportal thoracoscopic surgery for peripheral lung nodules. Ann Thorac Surg 2014;98:1998-2003. 10.1016/j.athoracsur.2014.07.036 [DOI] [PubMed] [Google Scholar]
- 5.Pompeo E, Mineo D, Rogliani P, et al. Feasibility and results of awake thoracoscopic resection of solitary pulmonary nodules. Ann Thorac Surg 2004;78:1761-8. 10.1016/j.athoracsur.2004.05.083 [DOI] [PubMed] [Google Scholar]
- 6.Li S, Liu J, He J, et al. VATS resection of a tracheal mass and reconstruction of trachea under non-intubated anesthesia with spontaneous. Asvide 2016;3:155. Available online: http://www.asvide.com/articles/910 [DOI] [PMC free article] [PubMed]
- 7.Liu J, Cui F, Li S, et al. Nonintubated video-assisted thoracoscopic surgery under epidural anesthesia compared with conventional anesthetic option: a randomized control study. Surg Innov 2015;22:123-30. 10.1177/1553350614531662 [DOI] [PubMed] [Google Scholar]