Abstract
Objective
This pilot randomized controlled trial evaluated a novel trauma-informed model of Mindfulness Based Stress Reduction (TI-MBSR) as a phase-I trauma intervention for female survivors of interpersonal violence (IPV).
Method
A community-based sample of women (Mean Age = 41.5, SD = 14.6) with a history of IPV were randomly assigned to an 8-week TI-MBSR intervention (n = 23) or a wait-list control group (n = 22). Symptoms of PTSD and depression, as well as anxious and avoidant attachment, were assessed pre- and post-intervention.
Results
Relative to the control group, participation in TI-MBSR was associated with statistically and clinically significant decreases in PTSD and depressive symptoms, as well as significant reductions in anxious attachment. Retention in the intervention was high, with most participants completing at least 5 of the 8 sessions for the intervention. Minutes of mindfulness practice per week significantly predicted reductions in PTSD symptoms.
Conclusion
TI-MBSR appears to be a promising and feasible phase I intervention for female survivors of interpersonal trauma.
Keywords: MBSR, mindfulness, interpersonal violence, trauma, post-traumatic stress disorder, Stage I RCT
Interpersonal violence (IPV) can have lasting adverse effects across the lifespan on both mental and physical health outcomes (Felitti et al., 1998), as well as on relationships (Pearlman & Saakvitne, 1995). Here we define IPV as the intentional use of physical or sexual violence against another person within the context of a relationship. This includes physical or sexual violence committed by a family member, intimate partner, friend, or acquaintance. In the U.S. at least one in three women have experienced episodes of IPV, including sexual assault and physical violence, in their lifetime, and most female survivors of IPV experience violence for the first time before the age of 25 (Black et al., 2011). The consequences of IPV can be lifelong and far reaching. For example, in one of the largest scale, population-level assessments of IPV, adult survivors of IPV lost approximately 8 million days of paid work in 2003 as a consequence of episodes of violence (Centers for Disease Control and Prevention, 2003). At least 30% of female survivors answering a survey through the National Institute on Injury Prevention reported psychological impacts from past violence, including symptoms of post-traumatic stress-disorder (PTSD) or depression, as well as increased needs for health care, housing services, and legal services (Black et al., 2011).
Epidemiologic data indicate that women tend to experience a higher incidence of lifetime IPV than men as well as experience a higher incidence of revictimization (Lilly & Valdez, 2012; Tang & Freyd, 2012), gender differences which have been found consistently across varying socioeconomic strata, geographic locations, and cultures (Tang & Freyd, 2012). Recurrent experiences of IPV may be one reason among many why women have twice the rate of PTSD as men (Iverson, et al., 2013, Kessler et al., 1995, 2005), exhibit PTSD symptoms for four times as long as men, report significantly poorer quality of life, and develop more comorbid psychiatric disorders (Breslau et al., 1998; Holbrook, Hoyt, Stein, & Sieber, 2001; Institute of Medicine, 2012; Seedat, Stein, & Carey, 2005).
IPV and Psychological Trauma
IPV commonly results in psychological trauma, defined as the appraisal of threat to bodily integrity or sanity which overwhelms an individual’s ability cope and thus to integrate their emotional experience (Allen, 2005; Pearlman & Saakvitne, 1995, Saakvitne, Gamble, Pearlman, & Tabor Lev, 2000). Traumatization includes psychological (APA, 2013; Rothschild, 2000; Siegel, 2003) and neurophysiological processes, including changes to the central, autonomic, and neuroendocrine systems integral to regulating arousal (Yehuda & LeDoux, 2007; Sherin & Nemeroff, 2011). From a psychological perspective, trauma entails loss and alterations to one’s sense of self-efficacy, way of life, and relationships. This often results in feelings of fear and grief which become inseparable from memories of the traumatic event (Iverson, et al., 2013; Titchener, 1986). Mental health outcomes associated with traumatic experiences like IPV can range across the diagnostic span, including major depressive disorder, substance use disorders, anxiety disorders, and PTSD (Follette, Palm, & Rasmussen Hall, 2004). Individuals who have faced repeated IPV, emotional abuse, and neglect from childhood onward often have the most severe psychological symptoms (Allen, 2013; Allen, Coyne, & Huntoon, 1998; Iverson, et al., 2013).
Additionally, IPV can have a profound effect on relational capacity, profoundly affecting the attachment style of adult survivors (Ainsworth, Blehar, Waters, & Wall, 1978; Allen, 2013). According to attachment theory, secure attachments help individuals regulate emotional distress, whereas insecure attachments render people susceptible to affective dysregulation (Mikulincer & Shaver, 2008). Building on the work of Bowlby (1958, 1988), Ainsworth and colleagues described two primary insecure attachment styles as avoidant/dismissive and anxious/resistant (Ainsworth, Blehar, Waters, & Wall, 1978). Individuals who develop an avoidant attachment style exhibit outwardly compliant, polite, and submissive behavior towards significant others that masks their internally dysregulated emotional state. In contrast, individuals who develop an anxious attachment style exhibit relational ambivalence, vacillating between attempts to draw in significant others with endearing attention-seeking behaviors and attempts to attract attention through emotional outbursts of crying or anger.
Exposure to traumatic incidents, such as IPV, in childhood or adulthood can disrupt attachments and lead to insecure attachment styles (Allen, 2005, 2013). For survivors of IPV with anxious attachment styles, emotional distress is often experienced as intolerable, resulting in desperate attempts to obtain security from adult attachment figures (e.g., romantic partner or close friend), typically in off-putting ways that actually undercut the emotional needs of the survivor. IPV survivors with avoidant attachment styles may attempt to suppress their negative emotions, which later erupt explosively as a result of intensified autonomic arousal (Gross, 2002) and the post-suppression rebound effect (Wetzlaff & Wegner, 2000).
The disrupted attachments, tremendous losses, absence of control, violations of safety, and betrayal of trust experienced by survivors of recurrent IPV can impede quality of life and impair relationships (Allen, 2013; Giller, 1999; Saakvitne, Gamble, Pearlman, & Tabor Lev, 2000). Conscious and unconscious attempts to manage affective and physiological states can lead to behaviors that, though initiated as escapist or protective strategies, can become self-destructive (i.e. cutting, substance abuse, controlling relational behaviors) and deleterious to forging and maintaining relations with family, romantic partners, and friends, among others (Allen, 2013; Courtois & Ford, 2013).
Rationale for the Modification of the MBSR model for Survivors of IPV
Mindfulness-based interventions such as Mindfulness-Based Stress Reduction (MBSR) (Kabat-Zinn, 1982, 1990, 2006) are now being offered in some community settings to survivors of violence, including individuals exposed to IPV. Although this is an understudied area, emerging research suggests that mindfulness-based interventions may hold promise for survivors of violence (Dutton, Bermudez, Matas, Majid, & Myers, 2013; Gallegos, Cross, & Pigeon, 2015; Kimbrough, Magyari, Langenberg, Chesney, & Berman, 2010; Smith, 2009). Going beyond the rationalist philosophy of cognitive-behavioral tradition (Beck, 1970), mindfulness-based interventions teach participants to change their relationship to their thoughts, rather than changing thought content itself. In other words, mindfulness training aims to enhance capacity for metacognitive awareness (Teasdale et al., 2002), leading to the recognition that negative thoughts, emotions, and sensations linked with past traumas are inherently ephemeral and not necessarily veridical reflections of present reality (Segal, Teasdale, & Williams, 2004). In spite of this sound theoretical rationale and the growing use of MBSR and other mindfulness-based interventions for trauma, few controlled trials of this therapeutic approach have been conducted.
The purpose of the present study was to provide a Stage I (Onken, Carroll, Shoham, Cuthbert, & Riddle, 2014) randomized-controlled pilot trial (RCT) of a trauma-informed MBSR intervention (TI-MBSR) in a community setting for female survivors of IPV. Rather than test a standard version of MBSR, this study aimed to develop and test a version of MBSR tailored to the clinical needs and issues of women suffering from IPV. The tailoring of MBSR and other mindfulness-based interventions for particular clinical issues has yielded promising results in studies of patients with substance use disorders (Bowen et al., 2014; Garland et al., 2014), major depressive disorder (Piet & Hougaard, 2011), and binge eating disorder (Kristeller & Wolever, 2011), among others. The TI-MBSR intervention tested in the current study was tailored by pairing mindfulness practices with trauma-specific psychoeducation to facilitate awareness of and exposure to conditioned trauma responses, without avoidance or reactivity to those experiences. Mindful breathing and body scanning techniques were taught as a way to titrate autonomic nervous system activation, enabling participants to attain an optimal level of arousal for processing traumatic memories and emotions without suppression, dissociation, or flooding. Through this synergy of mindfulness and psychoeducation, IPV survivors are taught to develop self-compassion (Neff, 2003) and insight into their maladaptive trauma coping behaviors, which may reduce shame while allowing for the possibility adaptive behavioral change.
The primary aim of this study was to evaluate the feasibility of developing a clinical trial comparing acute (pre-post) efficacy of TI-MBSR as a Phase-I intervention to a wait-list control condition in reducing the psychological sequelae of IPV. We hypothesized that participation in TI-MBSR would be associated with significantly greater improvements in post-traumatic stress symptoms, symptoms of depression and anxiety, and measures of anxious and avoidant attachment.
Method
Participants
A community-based sample (N=45) of self-identified female survivors of IPV was recruited through flyers and advertisements placed throughout the community to attend an 8-week mindfulness course for survivors of interpersonal trauma. Participants were screened according to study inclusion criteria: female gender, age 18 or older, a history of IPV, comprehension of spoken and written English, and having their own transportation to and from study activities. IPV was defined as physical or sexual abuse by a family member or intimate partner during the life course. In the interest of study safety, individuals were excluded if they were currently experiencing IPV, or if they screened positive for current suicidality or substance dependence as determined via the Mini-International Neuropsychiatric Interview (MINI) (Lecrubier et al., 1997).
Procedure
A randomized waitlist controlled design was implemented to assess preliminary efficacy of the TI-MBSR intervention. Participants meeting eligibility criteria completed the informed consent process as well as the pre-intervention questionnaires, and were then randomly allocated to 8 weeks of TI-MBSR or a waitlist control condition (allocation ratio 1:1). During screening structured interview questions were given by a trained clinical interviewer asking whether or not participants felt that they continued to experience trauma-related symptoms related to past experience of interpersonal violence, as this was required to meet inclusion criteria for the study. Participants were also queried regarding the proximity of their last incident of IPV, as well as the types of IPV they had experienced. Pre- and post-measures of post-traumatic stress and depression symptoms, as well as relational attachment, were completed in the offices of a local university.
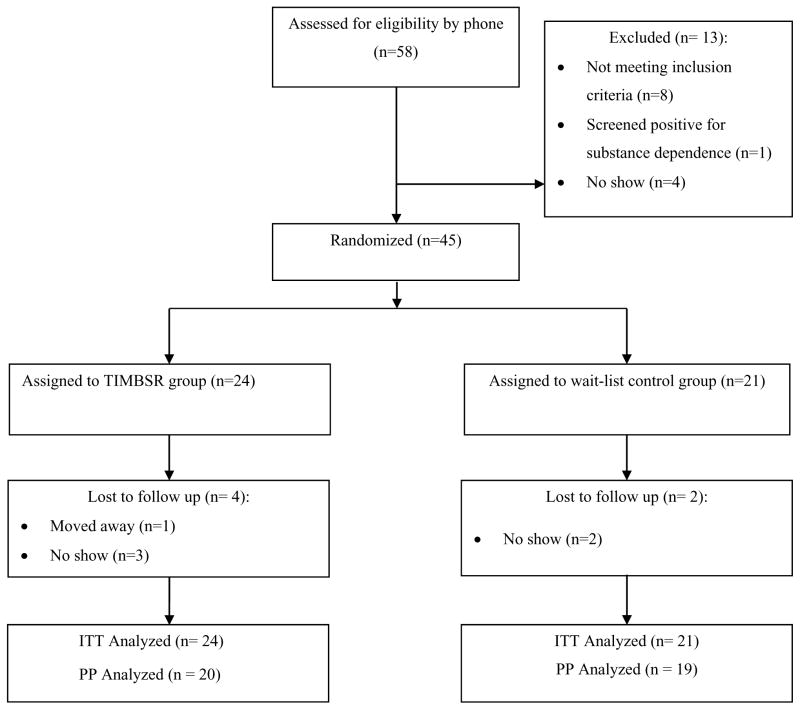
Of the 45 women, 24 were randomly assigned to TI-MBSR and 21 to a wait-list control condition. Participants were informed of group allocation by phone. The intervention was provided by a Licensed Clinical Social Worker, with formal training in both trauma-informed and mindfulness-based treatment approaches, including MBSR. Following the initial 8-week intervention period, both groups completed follow-up questionnaires. The wait-list group was offered the 8-week intervention following the completion of the second round of questionnaires. Outcome assessments were conducted by a research assistant who was blinded to treatment allocation. See Figure 1 for the study flow chart. Participants were paid $160 for completing the study. Study procedures were approved by the Smith College Institutional Review Board.
Figure 1.
CONSORT Study Flow Diagram.
TI-MBSR Intervention
The manualized TI-MBSR intervention took place over eight consecutive weeks, with each weekly session lasting approximately two to two and one-half hours long. Each session consisted of guided meditations, gentle movement exercises, didactic lecture, and group discussion, closely aligning with the practices offered in the same timeline for the standard MBSR model (Kabat-Zinn & Santorelli, 2011). The standard MBSR program is a group based program which focuses on developing mindful awareness through various meditation practices (Grossman, Niemann, Schmidt, & Walach, 2004). Mindfulness skills are taught in a structured 8-week group format. Each session lasts approximately two hours with one all-day meditation retreat that takes place in week six of the intervention. MBSR emphasizes experiential learning; in keeping with the standard model, in TI-MBSR participants were asked to practice mindfulness 30–45 minutes a day guided by an audio CD, as well as complete additional reading via course handouts. The skills taught in the program focus are designed to cultivate a sustained, focused awareness of mental states, physical sensations, perceptions, thoughts, and imagery. MBSR teaches observation of body sensations and thoughts without evaluation, and acceptance of experiences, whether negative, positive, or neutral, without suppression or rumination (Kabat-Zinn, 2005). In contrast to cognitive behavioral therapy (Beck, 1970) which teaches individuals to change the content of their thoughts, MBSR teaches participants to change their relationship to their thoughts. Through this process, MBSR participants may increase their capacity for metacognition (Teasdale, et al., 2002) or mentalization (Allen, 2005), in which thoughts, sensations, and emotions are experienced as ephemeral mental events and not veridical truths.
The TI-MBSR treatment manual detailed modifications of the original MBSR protocol designed to target clinically-salient issues for female survivors of IPV. No original content from the original MBSR protocol was cut in the modification - instead, additional psychoeducational content was embedded within each session. One exception was the elimination of the full day retreat portion of the original model, generally held on a weekend day following class 6. Table 1 outlines the practices and psychoeducational components added to the original MBSR model. The treatment fidelity measure was completed by the therapist, who ensured fidelity by using a checklist to document each intervention component as it was delivered during the session. Using this approach, adherence to the manual was 100%.
Table 1.
Modifications to the MBSR protocol to address trauma secondary to IPV. Note – not every session was modified from the original MBSR protocol. Additionally, it should be noted that no content was removed from the original MBSR protocol.
| Modification | Aim | Source |
|---|---|---|
| Session 1 – Introduction to neurophysiology of trauma | Provide a framework with which to understand trauma related symptomology, as well as a rationale for using mindfulness skills to cope with symptoms stemming from survival of past traumatic experience | (Allen, 1995; Foa & Kozak, 1986; Pearlman & Saakvitne, 1995; Rosthchild, 2000; Siegel, 2003, van der Kolk, McFalane, & Weisaeth, 2007) |
| Session 2 – Discussion of reactivity as related to survival of trauma and symptoms as adaptations. | Provide a framework for understanding coping behaviors from a strengths-based perspective; identify coping behaviors and the underlying anxieties resulting in such behaviors | (Pearlman & Saakvitne, 1995; Follette, Palm, & Rasmussen Hall, 2004; van der Kolk, McFalane, & Weisaeth, 2007; Herman, 1997) |
| Session 2 – Social Brain vs. Survival Brain | Discuss the relationship between higher-order more cognitive and relational aspects of thinking and more survival (primitive) aspects of thinking, and how these higher-order and primitive forms of cognition relate to the fight, flight, or freeze response | (Siegel, 2003) |
| Session 2 - Trauma survivors and Perceptions | Discuss the perceptions exercise from the perspective of being a trauma survivor; foster the recognition that the individual made attempts to cope with anxiety or other symptoms stemming from the initial overwhelming traumatic experience | (Foa & Kozak, 1986; Follette, Palm, & Rasmussen Hall, 2004; Garland, Gaylord, & Fredrickson, 2011; van der Kolk, McFalane, & Weisaeth, 2007) |
| Session 2 – Brief introduction to physiological processing | Recognize the physiological symptoms of trauma reactivity in the body | (Ogden, 2006; Rothschild, 2000) |
| Session 3 – Introduction to meditation of physiological experience | Notice bodily reactions to particular triggers; learn to regulate physiological arousal through mindful breathing, paced breathing, grounding (coming into the present moment and into the body using mindfulness of physical sensations), and resourcing (remembering healthy coping resources to aid in present-moment awareness, e.g., remembering the face of a family member important to the participant) | (Rothschild, 2000; Siegel, 2003) |
| Session 3 – Observation of Suppression, Repression, Avoidance, and Denial | Discuss the adverse consequences of suppressing thoughts and/or emotions; gain awareness of thought suppression through meditation | (Follette, Palm, & Rasmussen Hall, 2004; Freud, 1936) |
| Session 4 – Seeing Our Patterns | Introduce the idea of patterns of relating with others; develop insight into how one’s current emotional attachments are based on past relationships and psychological adaptations developed following previous traumatic experiences | (Allen, 2005; Benjamin, 2004; Follette, Palm, & Rasmussen Hall, 2004; Pearlman & Saakvitne, 1995) |
| Session 4 – The Trauma Triangle | Introduce the idea of the victim/victimizer/bystander relationship with a discussion of the different roles/dynamics that participants recognize themselves taking in their relationships | (Herman, 1997; Miller, 1994; Staub, 2002) |
| Session 5 – Review of patterns of relating and the trauma triangle, integrating reacting vs. responding | Review of materials from classes 2 & 4 | (Benjamin, 2004; Follette, Palm, & Rasmussen Hall, 2004; Herman, 1997; Pearlman & Saakvitne, 1995; Staub, 2002; van der Kolk, McFalane, & Weisaeth, 2007) |
| Session 7 – Mindful/Present Parenting | Discuss mindfulness as it applies to parenting; provide psychoeducation on how meditation practices might be integrated into everyday experiences with one’s children | (Kabat-Zinn & Kabat-Zinn, 1997; Saakvitne K. W., 2005) |
TI-MBSR was designed to be a Phase 1 model of trauma treatment for survivors of IPV. The International Society for Traumatic Stress Studies endorses a phased approach to interventions for complex trauma (Cloitre et al., 2012). Hermann (1997) identified the following successive phases of trauma treatment with associated tasks: establishing safety (Phase I), remembrance and mourning (Phase II), and reconnection with ordinary life (Phase III). In Phase I, goals and tasks seek to engender a sense of safety by attending to the survivor’s current social-relational context, the therapeutic environment (including psychoeducation about diagnosis and symptoms), and the therapeutic relationship. Congruent with Hermann’s Phase I, Allen (2001; 2005) argues that the goal of containment of traumatic thoughts and emotions, both internal and external (i.e., self-guided and containment by others), is the first task and primary goal of trauma treatment. Allen (2001) emphasizes the primary importance of learning to regulate one’s emotional responses in trauma treatment. From this perspective, until containment skills are developed, the processing of traumatic events and memories can be overwhelming, often leading to dangerous abreactions and an increase in symptoms for survivors of trauma. TI-MBSR aligns with both Allen and Herman’s initial phase of trauma recovery, by aiming to establish a sense of safety and affect regulation through training in mindfulness skills and psychoeducation. The development of the TI-MBSR model as a Phase I intervention was intended to allow for the intervention to be offered in spaces where more vulnerable sharing of traumatic narrative may not clinically appropriate or safe (e.g., criminal justice settings).
Measures
PTSD symptoms
The total score of the PTSD Checklist-Civilian Version (PCL-C) (Weathers, Litz, Herman, Huska, & Keane, 1994) was used to assess PTSD symptoms for participants. This 17-item self-report measure was selected due to its excellent reliability, validity, and generalizability to a wide variety of populations (Elhai, Gray, Kashdan, & Franklin, 2005; Elhai, Gray, Docherty, Kashdan, & Kose, 2007). Responses are rated on a five point Likert scale (1 = not at all, 5 = extremely), with a total score computed by summing scores on each item. The PCL demonstrates convergent validity through its high correlation with the Clinician Administered PTSD Scale (r = .92; Weathers et al., 1994), and high internal consistency (Cronbach’s α = .87 in this sample). According to the cutoffs established by Harrington and Newman (2007) via receiver–operator characteristic curve (ROC) analysis, a score of 44 or higher on the PCL-C may be considered diagnostic for PTSD among treatment-seeking individuals.
Depressive symptoms
The Beck Depression Inventory, Second Edition (BDI-II) (Beck, Steer, & Brown, 1996) was used to assess depressive symptoms. This 21-item self-report measure was selected for its excellent psychometric properties (Cronbach’s α = .92 in this sample) and common usage within MBSR studies measuring outcomes for depression (Kabat-Zin, 1982; Smith, 2010; Dutton, Bermudez, Matas, Majid, & Myers, 2013; Grossman, Neimann, Schmidt, & Walach, 2004). Responses are rated on a four point Likert scale, with a total score computed by summing scores on each item.
Anxious and Avoidant Attachment
The Relationship Structures Questionnaire (RSQ) (Fraley, Heffernan, Vicary, & Brumbaugh, 2011) was used to assess attachment patterns in multiple close relationships. Nine items are used to assess avoidant and anxious attachment styles for mother, father, romantic partner, and best friend, including items such as “I usually discuss my problems with this person” and “I’m afraid this person might abandon me.” Internal consistency in the present study sample was high (Cronbach’s α = .88). Responses are rated on a seven point Likert scale (1= strongly disagree, 7 = strongly agree), with a total scores computed separately for the anxious and avoidant subscales. 9.
Statistical Analysis
Study sample size was determined a priori based on a power analysis conducted with G-Power software using medium effect size estimates (e.g., Cohen’s f) derived from earlier trials demonstrating therapeutic effects of mindfulness training on psychological distress (Goyal et al., 2014). According to this model, a total sample size of 35 was required to gain medium effect size estimates. Approximately 87% (n=39) of the total enrolled sample (N=45) completed post-intervention assessments, with 20 participants completing the TI-MBSR intervention and 19 completing the post-intervention measures from the wait-list control group; attrition did not significantly differ between groups, nor was it predicted by baseline values of study variables.
We evaluated pre-post changes in measures of PTSD symptoms (PCL-C), depression (BDI-II), and anxious and avoidant attachment (RSQ). For hypothesis testing, we conducted intention-to-treat (ITT) analyses. To analyze patterns of missing data, we performed Little’s MCAR test (Little, 1988). The pattern of missing data was consistent with being missing completely at random; thus, maximum likelihood estimation was employed to handle missing data. To reduce potential bias resulting from listwise deletion or last-observation carried forward techniques, ITT analysis was conducted using a linear mixed model approach, which is considered preferable to other methods of dealing with missing data (Singer & Willett, 2003). Denominator degrees of freedom were obtained by a Satterthwaite approximation. ITT models were estimated with maximum likelihood methods, which estimate the variance-covariance matrix for all available data, including data from cases assessed at only one time point. In analysis models, we treated Group (TI-MBSR vs. wait-list) and Time (pre- vs. post-intervention) as fixed effects. Analyses focused on the Group X Time interaction term as the parameter of interest. Binomial McNemar tests (McNemar, 1947; Adedokun & Burgess, 2012) were used to determine whether there was a significant difference in the proportion of participants in the TI-MBSR versus the control group who surpassed the validated cutoff on the PCL-C for PTSD (Harrington & Newman, 2007) at baseline but no longer surpassed the threshold for PTSD at post-treatment.
Results
Participants
Table 2 presents sample characteristics. The women ranged in age from 19–69 years (M age = 41.5, SD = 14.6). A majority of the women self-identified as white (73%). Income levels varied; however a majority reported earning less than $20,000/year. Most participants (89%) had completed at least some college.
Table 2.
Demographic Comparisons between TIMBSR and Wait-list Control group completers
| Category | TIMBSR n = 24 | Control n = 21 |
|---|---|---|
| Age | ||
| 19–29 | 5 (20.8%) | 7 (33.3%) |
| 30–39 | 7 (29.2%) | 4 (19%) |
| 40–49 | 3 (12.5%) | 2 (9.5%) |
| 50–59 | 2 (8.3%) | 6 (28.6%) |
| 60–69 | 5 (20.8%) | 2 (9.5%) |
| Did not disclose | 2 (8.3%) | 0 (0%) |
| Race/Ethnicity | ||
| Of white European descent | 19 (79.2%) | 14 (66.7%) |
| Of African Descent | 2 (8.3%) | 2 (9.5%) |
| Indigenous to North/South America | 1 (4.2%) | 2 (9.5%) |
| Hispanic | 0 (0%) | 1 (4.8%) |
| Of Asian descent | 0 (0%) | 0 (0%) |
| Other | 2 (8.3%) | 1 (4.8%) |
| Would rather not disclose | 0 (0%) | 1 (4.8%) |
| Income | 0 (0%) | 0 (0%) |
| Less than 20,000/yr | 12 (50%) | 12 (57.1%) |
| 20,000 – 39,999 | 5 (20.8%) | 5 (23.8%) |
| 40,000 – 59,999 | 4 (16.7%) | 4 (19%) |
| 60,000 – 79,999 | 1 (4.2%) | 0 (0%) |
| 80,000 and up | 2 (8.3%) | 0 (0%) |
| Relationship Status | ||
| Married | 7 (29.2%) | 3 (14.3%) |
| Divorced | 6 (25%) | 6 (28.6%) |
| Never Married | 1 (4.2%) | 4 (19%) |
| Partnered, living together, but not married | 6 (25%) | 6 (28.6%) |
| Widowed | 1 (4.2%) | 0 (0%) |
| Single | 3 (12.5%) | 2 (9.5%) |
| Education Level | ||
| 8th–11th grade | 0 (0%) | 1 (4.8%) |
| High School Diploma | 4 (16.7%) | 0 (0%) |
| Some college | 5 (20.8%) | 6 (28.6%) |
| Two year degree | 5 (20.8%) | 6 (28.6%) |
| Bachelors degree | 5 (20.8%) | 5 (23.8%) |
| Masters degree | 5 (20.8%) | 3 (14.3%) |
| PhD | 0 (0%) | 0 (0%) |
| Employment status | ||
| Currently employed | 11 (45.8%) | 25 (71.4%) |
| Not currently employed | 13 (54.2%) | 6 (28.6%) |
Table 3 presents clinical information related to exposure to IPV. The average number of lifetime types of IPV-related traumatic experience was 2.1 (SD = 1.7, range 1 – 6). Participants reported a wide range of symptom severity, from individuals with subclinical symptoms of traumatic stress and depression, to those who met full diagnostic criteria for mental disorders. Of those intervention or wait-list group pre- and post-survey completers, 38% of participants screened positive for PTSD per a validated cutpoint on the PCL-C (Harrington & Newman, 2007) at the time of the pre-intervention survey. No statistically significant, between-groups differences were found at pre-intervention assessment for age, gender, race, income, exposure to traumatic violence, psychiatric symptoms, or attachment style.
Table 3.
Clinical information related to trauma exposure.
| Category | TIMBSR n = 20 | Control n = 19 |
|---|---|---|
| Time since last traumatic incident | ||
| Less than on month ago | 0 (0%) | 1 (5.3%) |
| Two to six months ago | 2 (10.0%) | 0 (0.0%) |
| Six months to one year ago | 4 (20.0%) | 3 (15.8%) |
| 1 to 2 years ago | 6 (30.0%) | 5 (26.3%) |
| 3 to 5 years ago | 4 (20.0%) | 5 (26.3%) |
| Over 5 years ago | 4 (20.0%) | 5 (26.3%) |
| Number of types of traumatic experiences per trauma questionnaire | ||
| Mean (SD) | 1.92 (1.6) | 2.43 (1.8) |
| PTSD diagnosis per PCL-C cut off | ||
| Positive for PTSD | 7 (35%) | 5 (26%) |
| Negative for PTSD | 13 (65%) | 14 (74%) |
The number of women completing surveys at both pre- and post-intervention were 19 for the intervention group and 20 for the wait-list control group. The average number of participants per group session was 17/19. For those that attended at least the first session in the intervention group, 53% (n = 10) completed all eight sessions of the intervention, 26% (n = 5) completed 7 sessions, 11% (n = 2) completed 6 sessions, and 5% (n = 1) completed 5 sessions. One participant attended only the first class and did not return.
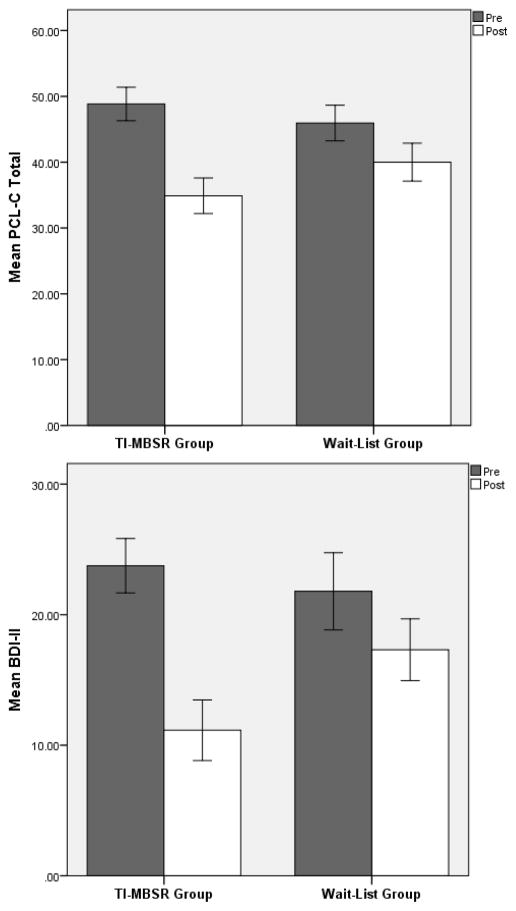
PTSD symptoms
Linear mixed models revealed a significant Group X Time interaction effect on PCL-C, F(1,39.63) = 9.51, p = .004, d = .94, indicating that the TI-MBSR group reported significantly greater reductions in post-traumatic stress than the wait-list control group (Figure 2). Though inspection of PCL-C means (Table 4) revealed that participants in the TI-MBSR group exhibited significantly greater decreases in PTSD symptoms than the control group by the post-treatment assessment, in addition to examining PTSD decreases dimensionally we compared participants categorically based on the diagnostic cutoff on the same measure. There was a significant reduction in the proportion of participants in the TI-MBSR group surpassing the cutoff for PTSD, binomial McNemar p = .008, whereas there was not a significant reduction among control group participants, binomial McNemar p = .25 (80% and 40% reduction, respectively).
Figure 2.
Changes in PTSD (PCL-C) and depressive symptoms (BDI-II) over the course of the study for the Trauma-Informed Mindfulness Based Stress Reduction (TI-MBSR) and wait-list control groups. Error bars represent ±1 S.E.
Table 4.
Averages (SD) and effect sizes for TIMBSR and Wait-list Control group completers
| Category | TIMBSR n = 19 | Control n = 20 | Between-Group Effect Size (Δ) Cohen’s d |
|---|---|---|---|
|
| |||
| Measure | Mean (SD) | Mean (SD) | |
| PTSD-pre | 49 (11) | 46 (12) | |
| PTSD-post | 35 (12) | 40 (13) | |
| PTSD change | .94 | ||
| Depression-pre | 24 (9) | 22 (13) | |
| Depression-post | 11 (10) | 17 (10) | |
| Depression change | .86 | ||
| Anxious Attachment-pre | 3.7 (1.3) | 2.8 (1.1) | |
| Anxious Attachment-post | 3.2 (1.7) | 3.1 (1.4) | |
| Anxious Attachment change | .85 | ||
| Avoidant Attachment-pre | 3.9 (0.8) | 3.5, (1.0) | |
| Avoidant Attachment-post | 3.8 (1.4) | 3.4 (1.1) | |
| Avoidant Attachment change | .11 | ||
Depressive symptoms
There was a significant Group x Time interaction on depression, BDI-II, F(1,38.69) = 8.35, p = .006, d = .86, such that the TI-MBSR group reported significantly greater decreases in depression than the wait-list control group (Figure 2). According to validated clinical cutoffs on the BDI, the TI-MBSR group shifted from moderate to minimal levels of depression by the end of treatment.
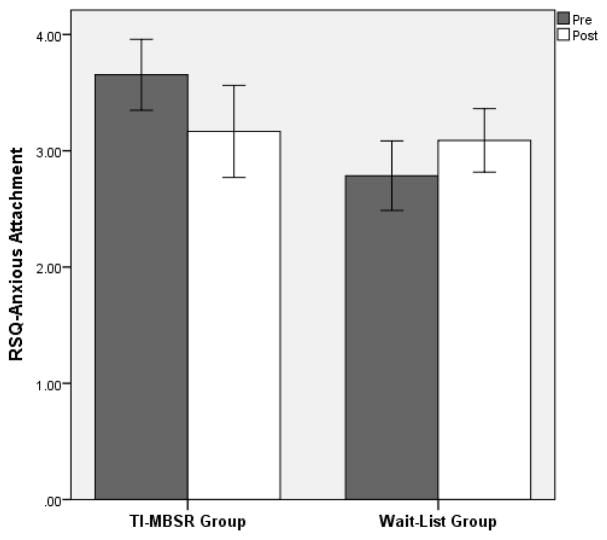
Anxious and avoidant attachment
With regard to anxious attachment scores on the RSQ, the Group x Time interaction was significant, F(1,35.18) = 4.94, p = .033, d = .85, such that the TI-MBSR group reported significantly greater decreases in anxious attachment than the wait-list control group (Figure 3). However, the Group X Time interaction was not found to be significant for avoidant attachment scores on the RSQ.
Figure 3.
Changes in anxious attachment (RSQ) over the course of the study for the Trauma-Informed Mindfulness Based Stress Reduction (TI-MBSR) and wait-list control groups. Error bars represent ±1 S.E.
Mindfulness practice and relation to therapeutic change
The mean number of TI-MBSR sessions attended by participants who completed the intervention was 7.0 (SD = 1.7). Participants self-reported practicing mindfulness skills for an average of 190.5 minutes per week (SD = 99.7). This was measured through weekly homework tracking forms, as well as through inquiry at the time of post-intervention survey completion. Minutes of mindfulness practice per week significantly predicted residualized change in PCL-C scores, β = −.33, p = .004, such that individuals who engaged in more extensive mindfulness practice experienced greater decreases in PTSD symptoms than those who practiced for fewer minutes per week. Mindfulness practice was not significantly correlated with changes in depression or attachment style.
Discussion
Study findings indicate that female survivors of IPV who were randomly assigned to participate in an eight-week TI-MBSR program exhibited significantly decreased levels of post-traumatic stress symptoms, depressive symptoms, and anxious attachment compared to a wait-list control condition. Moreover, attrition was low and individuals appeared willing to engage in mindfulness practice at home between sessions. These results suggest that TI-MBSR is promising and feasible Phase-I intervention for female survivors of IPV.
The version of MBSR tested in this study was modified to specifically target cognitive, affective, and autonomic mechanisms underpinning psychological traumatization related to IPV. To that end, participants were taught mindfulness skills, including attention regulation and non-reactive observation of thoughts, emotions, and somatic states. By enhancing attentional regulatory capacity, it was hoped that participants would become more skillful at modulating their own arousal, thereby countering post-traumatic stress while facilitating naturalistic processing of traumatic memories and schemas of helplessness. Psychoeducation on the physiological and emotional impact of trauma was also provided to normalize participant experience and provide insight. The synergy of mindfulness skills and trauma-specific psychoeducation was intended to help participants begin to reclaim an empowered sense of self from the aftermath of past traumas.
In that regard, participation in TI-MBSR was associated with robust reductions in post-traumatic stress symptoms. The large effect size of TI-MBSR on post-traumatic stress for this population is notable, given the limited literature on the efficacy of MBSR for survivors of IPV. The observed effect size of TI-MBSR in this pilot trial exceed those of other mindfulness-based interventions for trauma in prior research: two non-experimental, observational studies of MBSR with survivors of IPV found medium effect sizes for post-traumatic stress symptoms (Kimbrough, Magyari, Langenberg, Chesney, & Berman, 2010; Smith, 2010), a quasi-experimental study of MBSR for combat veterans found a small effect size (Kearney, McDermott, Malte, Martinez, & Simpson, 2012), and another quasi-experimental study of Mindfulness-Based Cognitive Therapy for veterans identified a medium effect size for post-traumatic symptoms (King et al., 2013). Moreover, in the present study, participation in TI-MBSR was associated with a significant reduction in the proportion of individuals surpassing the cutoff on the PCL-C for having PTSD diagnosis. These substantial effects on post-traumatic stress are remarkable given that participants were not asked to disclose details about their index traumas nor were they guided to actively process their traumatic memories directly during the TI-MBSR treatment. Significant therapeutic effects of TI-MBSR for depression were also observed. The large effect size found for decreases in depression for the intervention group as compared to wait-list control was either greater than or comparable to other studies with MBSR as an intervention for survivors of IPV (Kimbrough, Magyari, Langenberg, Chesney, & Berman, 2010) and combat-related violence (Kearney, McDermott, Malte, Martinez, & Simpson, 2012). Though smaller in magnitude, participants in the waitlist control group also evidenced symptom improvements, which may have stemmed from measurement reactivity or regression to the mean over time.
Though mechanistic measures were not included in the present study, we offer the following speculative account of how TI-MBSR may have reduced the psychological sequelae of IPV. Hypothetically, TI-MBSR might facilitate therapeutic exposure (Holzel et al., 2011), thereby reducing reactivity to trauma-related thoughts and emotions during mindfulness practice and increasing distress tolerance. Furthermore, In TI-MBSR, participants are taught to recognize when they are dissociating or exhibiting excessive sympathetic arousal to difficult mental contents, and to use techniques like mindful breathing or the body scan to modulate fight/flight/freeze responses. Through such techniques, which have been shown to induce parasympathetic responses (Jain et al., 2007), participants may have learned to titrate their arousal to counter post-traumatic stress symptoms. For IPV survivors suffering from uncontrollable autonomic arousal, the experience of enhanced self-regulatory capacity might have also increased self-efficacy. Furthermore, mindfulness coupled with psychoeducation on trauma may have enhanced self-compassion, thereby reducing shame and consequent symptoms of depression. Lastly, it is possible that mindfulness practice may have facilitated a reframing of past traumas, thereby facilitating post-traumatic growth in the wake of IPV (Garland, Farb, Goldin, & Fredrickson, 2015). To be clear, these hypothetical mechanisms were not directly assessed in the present study. Future studies should biobehavioral research methods to probe the effects of TI-MBSR on cognitive, affective, and psychophysiological mechanisms implicated in IPV.
Importantly, statistically significant reductions were found for measures of anxious attachment for the TI-MBSR group compared to the wait-list control group. To our knowledge, this is the first finding in the literature of a mindfulness-based intervention positively impacting attachment style in the context of a RCT. This finding is remarkable, given the relatively brief duration of intervention. The intentional focus on present-moment relational experiences taught in the TI-MBSR intervention may have contributed to changes in anxious attachment. Participants were encouraged to practice non-reactive, present-moment awareness while engaged in relationships, both in session (during group discussions) and in their day-to-day lives. This practice of mindful awareness was aimed at differentiating current from past relational experiences and decreasing preoccupation with past attachments. Present-moment awareness of current relationships, coupled with increased self-regulatory capacity, may allow survivors with an anxious attachment style to engage adaptively in their adult relationships. In contrast, avoidant attachment was not found to be significantly different for participants in the TI-MBSR group as compared to the wait-list control. Though future moderation analyses are needed, study findings may provide some indication that the TI-MBSR model may have greater therapeutic impact on individuals with anxious attachment styles than those with avoidant attachment styles.
This study had a number of limitations. Most notably, the use of a wait-list control condition limits our ability to determine the therapeutically active components of the TI-MBSR intervention. The clinical outcomes observed might be due to a range of non-specific therapeutic factors, such as attention by a caring professional, social support, or the expectancy effects. Additionally, participants might have been in concurrent psychotherapy outside of the study, which may have influenced outcomes. That said, the fact that time spent in mindfulness practice was correlated with improvements in post-traumatic stress symptoms suggests that mindfulness training may have played a key role in producing therapeutic change. In addition, the study was limited by lack of a follow-up measurement point. Although participation in TI-MBSR was associated with significant changes in post-traumatic stress and depressive symptoms, the duration of these changes are unknown. All therapeutic change was measured via self-report, which may be biased and may not accurately measure clinical outcomes. Also, the study lacked quantitative measurement of treatment fidelity: therapist adherence and competence was not evaluated. Lastly, the study was limited by its small sample size, which may detract from the generalizability of study findings, as well as constrain statistical power. That said, significant effects were obtained despite the modest sample. Future studies might profitably employ a three-arm dismantling design with 6- and 12-month follow-ups, randomizing women with IPV to TI-MBSR, traditional MBSR, or a social support group to disentangle the differential therapeutic effects of trauma-informed content from standard mindfulness skills and non-specific therapeutic factors.
We found that TI-MBSR was feasible to implement with few resources and acceptable to participants with low incomes. TI-MBSR can be offered in most settings, even those with comparatively limited resources - for example, in prison settings where there are high rates of IPV and traumatization among incarcerated women. Given that MBSR has begun to be implemented in such settings (Samuelson, Carmody, Kabbat-Zinn, & Bratt, 2007; Himelstein, 2011; Perkins, 1998), more research is needed to determine if it would be beneficial to modify the mindfulness training programs already being offered by integrating specific psychoeducation on trauma and therapeutic techniques informed by the trauma literature.
In sum, TI-MBSR appears to be a promising Phase-I intervention for female survivors of IPV. Clinically significant improvements in post-traumatic stress and depressive symptoms were observed, and anxious attachment significantly decreased following this relatively brief intervention. More treatment development research is needed to elucidate the mechanisms and long-term effects of this therapeutic approach.
Acknowledgments
This research was supported by a 1440 Grant from the Mind & Life Institute awarded to AK and ELG. Additionally, it was supported through the Smith College School for Social Work’s Clinical Research Institute awarded to AK. ELG was also supported by NIDA Grant R34DA037005 in preparing this manuscript.
Contributor Information
Amber Kelly, Quinnipiac University.
Eric L. Garland, University of Utah.
References
- Adedokun OA, Burgess WD. Analysis of paired dichotomous data: A gentle introduction to the MdNemar test in SPSS. Journal of Multidisciplinary Education. 2012;8:125–131. [Google Scholar]
- Ainsworth MD, Blehar MC, Waters E, Wall S. Patterns of attachment: A psychological study of the strange situation. Hillsdale: Erlbaum; 1978. [Google Scholar]
- Allen J. Traumatic relationships and serious mental disorders. New York: John Wiley & Sons, Inc; 2001. [Google Scholar]
- Allen J. Coping with trauma: A guide to self-understanding. 2. Washington, DC: American Psychoanalytic Press; 2005. [Google Scholar]
- Allen J. Mentalizing in the development and treatment of attachment trauma. London: Karnac; 2013. [Google Scholar]
- Allen JG, Coyne L, Huntoon J. Complex posttraumatic stress disorder in women from a psychometric perspective. Journal of Personality Assessment. 1998;70:277–298. doi: 10.1207/s15327752jpa7002_7. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4. Washington: American Psychiatric Association; 2000. Text Revision. [Google Scholar]
- American Psychiatric Association. Disgnostic and statistical manual of mental disorders. 5. Washington, DC: Author; 2013. [Google Scholar]
- Beck AT. Cognitive therapy: Nature and relation to behavior therapy. Behavior Therapy. 1970:184–200. [Google Scholar]
- Beck AT, Rush AJ, Shaw BF, Emery G. Cognitive therapy of depression. New York: Guilford Press; 1979. [Google Scholar]
- Beck AT, Steer RA, Brown GK. Manual for the beck depression inventory-II. San Antionio: Psychological Corporation; 1996. [Google Scholar]
- Benjamin J. Beyond doer and done to: An intersubjective view of thirdness. Psychoanalytic Quarterly. 2004;72:5–42. doi: 10.1002/j.2167-4086.2004.tb00151.x. [DOI] [PubMed] [Google Scholar]
- Black MC, Basile KC, Breiding MJ, Smith SG, Walters ML, Merrick MT, Stevens MR. The national intimate partner and sexual violence survey: 2010 summary report. Atlanta: National Center for Injury Prevention and Control, Division of Violence Prevention; 2011. [Google Scholar]
- Bowen S, Witkiewitz K, Clifasefi SL, Grow J, Chawla N, Hsu SH, Larimer ME. Relative efficacy of Mindfulness-Based Relapse Prevention, standard relapse prevention, and treatment as usual for substance use disorders: A randomized clinical trial. JAMA Psychiatry. 2014;71:547–556. doi: 10.1001/jamapsychiatry.2013.4546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowlby J. The nature of the child’s tie to his mother. International Journal of PsychoAnalysis. 1958;39:350–373. [PubMed] [Google Scholar]
- Bowlby J. A secure base. New York: Basic Books; 1988. [Google Scholar]
- Breslau NR, Kessler RC, Cilcoat HD, Schultz LR, Davis GC, Andreski P. Trauma and posttraumatic stress disorder in the community - the 1996 Detroit area survey of trauma. Archives of General Psychiatry. 1998;55:626–632. doi: 10.1001/archpsyc.55.7.626. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Costs of intimate partner violence against women in the United States. Atlanta: National Centers for Injury Prevention and Control; 2003. [Google Scholar]
- Cloitre M, Courtois CA, Ford JD, Green BL, Alexander P, Briere J, van der Hart O. The ISTSS expert consensus treatment guidelines for complext PTSD in adults. International Society for Traumatic Stress Studies, Complex Trauma Task Force; 2012. [Google Scholar]
- Committee on the assessment of ongoing effects in the treatment of post-traumatic stress disorder; Institute of medicine. Treatment for posttraumatic stress disorder in military and veteran populations: Initial assessment. Washington, DC: National Academy of Sciences; 2012. [Google Scholar]
- Courtois CA, Ford JD. Treating complex traumatic stress disorders in children and adults. New York, NY: Guilford Press; 2013. [Google Scholar]
- Dutton MA, Bermudez D, Matas A, Majid J, Myers NL. Mindfulness-based stress reduction for low-income, predominantly African American women with PTSD and a history of intimate partner violence. Cognitive and behavioral practice. 2013;20:23–32. doi: 10.1016/j.cbpra.2011.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elhai JD, Gray MJ, Docherty AR, Kashdan TB, Kose S. Structural validity of the posttraumatic stress disorder checklist among college students with a trauma history. Journal of Interpersonal Violence. 2007;22:1471–1478. doi: 10.1177/0886260507305569. [DOI] [PubMed] [Google Scholar]
- Elhai JD, Gray MJ, Kashdan TB, Franklin CL. Which instruments are most commonly used to assess traumatic event exposure and posttraumatic effects?: A survey of traumatic stress professionals. Journal of Traumatic Stress. 2005;18:541–545. doi: 10.1002/jts.20062. [DOI] [PubMed] [Google Scholar]
- Felitti MD, Vincent J, Anda MD, Robert F, Norenbert MD, Williamson MS, James S. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The Adverse Childhood Experiences (ACE) Study. American Journal of Preventative Medicine. 1998;14:245–258. doi: 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- Foa EB. Prolonged explosure therapy: Past, present, and future. Depression and anxiety. 2011;28:1043–1047. doi: 10.1002/da.20907. [DOI] [PubMed] [Google Scholar]
- Follette VM, Palm KM, Rasmussen Hall ML. Acceptance, mindfulness, and trauma. In: Hayes SC, Follette VM, Linehan MM, editors. Mindfulness and Acceptance: Expanding the Cognitive-Behavioral Tradition. New York: The Guilford Press; 2004. pp. 192–208. [Google Scholar]
- Fraley RC, Heffernan ME, Vicary AM, Brumbaugh CC. The experiences in close relationships-relationship structures questionnaire: A method for assessing attachment orientations across relationships. Psychological Assessment. 2011;23 doi: 10.1037/a0022898. [DOI] [PubMed] [Google Scholar]
- Freud A. The ego and the mechanisms of defense. New York: International Universities Press; 1936. [Google Scholar]
- Gallegos AM, Cross W, Pigeon WR. Mindfulness-Based Stress Reduction for Veterans Exposed to Military Sexual Trauma: Rationale and Implementation Considerations. Military Medicine. 2015;180:684–689. doi: 10.7205/MILMED-D-14-00448. [DOI] [PubMed] [Google Scholar]
- Garland EL, Manusov EG, Froeliger B, Kelly A, Williams JM, Howard MO. Mindfulness-oriented recovery enhancement for chronic pain and prescription opioid misuse: Results from an early-state randomized controlled trial. Journal of Consulting and Clinical Psychology. 2014;82:448–459. doi: 10.1037/a0035798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giller E. What is psychological trauma?. Annual Conference of the Maryland Mental Hygiene Administration, “Passages to Prevention: Prevention Across Life’s Spectrum,”; Sidran Institute; 1999. [Google Scholar]
- Goyal M, Singh S, Sibinga EM, Gould NF, Rowland-Seymour A, Sharma R, Berger Z. Meditation programs for psychological stress and well-being: A systematic review and meta-analysis. JAMA Internal Medicine. 174:357–368. doi: 10.1001/jamainternmed.2013.13018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grossman P, Niemann L, Schmidt S, Walach H. Mindfulness-based stress reduction and health benefits: A meta-analysis. Journal of Psychosomatic Research. 2004;57:35–43. doi: 10.1016/S0022-3999(03)00573-7. [DOI] [PubMed] [Google Scholar]
- Harrington T, Newman E. The psychometric utility of two self-report measures of PTSD among women substance abusers. Addictive Behaviors. 2007;32:2788–2798. doi: 10.1016/j.addbeh.2007.04.016. [DOI] [PubMed] [Google Scholar]
- Herman J. Trauma and recovery: The aftermath of violence -- from domestic abuse to political terror. New York: Basic Books; 1997. [Google Scholar]
- Himelstein S. Meditation research: The state of the art in correctional settings. International Journal of Offender Therapy and Comparative Criminology. 2011;55:646–661. doi: 10.1177/0306624X10364485. [DOI] [PubMed] [Google Scholar]
- Holbrook TL, Hoyt DB, Stein MB, Sieber WJ. Perceived threat to life predicts posttraumatic stress disorder after major trauma: Risk factors and functional outcome. Journal of Trauma0Injury Infection & Cricial Care. 2001;51:287–283. doi: 10.1097/00005373-200108000-00010. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine. Treatment for posttraumatic stress disorder in military and veteran populations: Initial assessment. Washington, DC: National Academy of Sciences; 2012. [PubMed] [Google Scholar]
- Iverson KM, Dick A, McLaughlin KA, Smith BN, Bell ME, Gerber MR, Mitchell KS. Exposure to interpersonal violence and its associations with psychiatric morbidity in a U.S. national sample: A gender comparison. Psychology of Violence. 2013;3:273–287. doi: 10.1037/a0030956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kabat-Zin J. An outpatient program in behavioral medicine for chronic pain based on the practices of mindfulness meditation. General Hospital Psychiatry. 1982;4:33–47. doi: 10.1016/0163-8343(82)90026-3. [DOI] [PubMed] [Google Scholar]
- Kabat-Zinn J. Full catastrophe living: Using the wisdom of your body and mind to face stress, pain, and illness. New York: Dell; 1990. [Google Scholar]
- Kabat-Zinn J. Mindfulness-based interventions in context: Past, present, and future. Clinical Psychology. 2006;10:144–156. [Google Scholar]
- Kabat-Zinn J, Santorelli S. MBSR in mind body medicine: A 7-day residential setting. Mount Madonna, CA: 2011. [Google Scholar]
- Kearney D, McDermott K, Malte C, Martinez M, Simpson TL. Association of participation in a mindfulness program with measures of PTSD, depression, and quality of life in a veteran sample. Journal of Clinical Psychology. 2012;68:101–116. doi: 10.1002/jclp.20853. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Burglund O, Demler R, Jin KR, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distrubtions of DSM-IV disorders in the national comorbidity survey replication. Archives of General Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Sonnega E, Bromet M, Hughes M, Nelson CB. Posttraumatic stress disorder in the national comorbidity survey. Archives of General Psychiatry. 1995;52:1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- Kimbrough E, Magyari T, Langenberg P, Chesney M, Berman B. Mindfulness intervention for child abuse survivors. Journal of Clinical Psychology. 2010;66:17–33. doi: 10.1002/jclp.20624. [DOI] [PubMed] [Google Scholar]
- King AP, Erickson TM, Giardino ND, Favorite T, Rauch SA, Robinson E, Liberzon I. A pilot study of group Mindfulness-Based Cognitive Therapy (MBCT) for combat veterans with posttraumatic stress disorder (PTSD) Depression and Anxiety. 2013;00:1–8. doi: 10.1002/da.22104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kristeller JL, Wolever RQ. Mindfulness-based eating awareness training for treatment binge eating disorder: The conceptual foundation. Eating Disorders: The Journal of Treatment and Prevention. 2011;19:49–61. doi: 10.1080/10640266.2011.533605. [DOI] [PubMed] [Google Scholar]
- Lecrubier Y, Sheehan DV, Weiller E, Amorim P, Bonora I, Harnett Sheehan K, Dunbar GC. The Mini International Neuropsychiatric Interview (MINI). A short Diagnotistic structured overview: reliability and validity according to the CIDI. European Psychiatry. 1997;12:224–231. [Google Scholar]
- Lilly MM, Valdez CE. Interpersonal trauma and PTSD: The roles of gender and a lifespan perspective in predicting risk. Psychological Trauma: Research, Practice, and Policy. 2012;4:140–144. [Google Scholar]
- Little RJ. A test of missing completely at random for multivariate data with missing values. Journal of the American Statistical Association. 1988;83:1198–1202. [Google Scholar]
- McNemar Q. Note on the sampling error of the difference between correlated proportions or percentages. Psychometricka. 1947;12:153–157. doi: 10.1007/BF02295996. [DOI] [PubMed] [Google Scholar]
- Mikulincer M, Shaver PR. The attachment behavioral system in adulthood: Activation, psychodynamics, and interpersonal processes. In: Zanna MP, editor. Advances in experimental social psychology. Vol. 35. San Diego: Academic Press; 2003. pp. 53–152. [Google Scholar]
- Miller D. Women who hurt themselves: A book of hope and understanding. New York: Basic Books; 1994. [Google Scholar]
- Neff K. Self-compassion: An alternative conceptualization of a healthy attitude toward oneself. Self and Identity. 2003;2:85–101. [Google Scholar]
- Ogden P, Minton K, Pain C. Trauma and the body; A sensorimotor approach to psychotherapy. New York: WW Norton & Company; 2006. [Google Scholar]
- Onken LS, Carroll KM, Shoham V, Cuthbert BN, Riddle M. Reenvisioning clinical science: Unifying the discipline to improve public health. Clinical Psychological Science. 2014;2:22–34. doi: 10.1177/2167702613497932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearlman LA, Saakvitne KW. Trauma and the therapist. New York: Norton; 1995. [Google Scholar]
- Perkins R. The efficacy of mindfulness-based techniques in the reduction of stress in a sample of incarcerated women. 1998 (Order No. 9905418), Available from ProQuest Dissertations & Theses Full Text. (304425591) [Google Scholar]
- Rothschild B. The body remembers: The psychophysiology of trauma and trauma treatment. New York: W. W. Norton & Company; 2000. [Google Scholar]
- Saakvitne KW. Parenting resource handbook: Support for survivor parents: Breaking the cycle of abuse one day at a time. Holyoke: The Consortium; 2005. [Google Scholar]
- Saakvitne KW, Gamble S, Pearlman LA, Tabor Lev B. Risking connection: A training curriculum for working with survivors of childhood abuse. Baltimore: Sidran Press; 2000. [Google Scholar]
- Samuelson M, Carmody J, Kabbat-Zinn J, Bratt MA. Mindfulness-based stress reduction in Massachusetts correctional facilities. The Prison Journal. 2007;87:254–268. [Google Scholar]
- Santorelli SF, Kabat-Zinn J. Mindfulness-based stress reduction professional training resource manual: Integrating mindfulness meditation into medicine and society. Worcester: Center for Mindfulness in Medicine, Healthcare, and Society; 2006. [Google Scholar]
- Seedat S, Stein DJ, Carey PD. Post-traumatic stress disorder in women: Epidemiological and treatment issues. CNS Drugs. 2005;19:411–427. doi: 10.2165/00023210-200519050-00004. [DOI] [PubMed] [Google Scholar]
- Segal ZV, Teasdale JD, Williams MG. Mindfulness-Based Cognitive Therapy: Theoretical Rationale and Empirical Status. In: Hayes SC, Follette VM, Linehan MM, editors. Mindfulness and acceptance: Expanding the cognitive-behavioral tradition. New York: The Guilford Press; 2004. pp. 45–65. [Google Scholar]
- Sherin JE, Nemeroff CB. Post-traumatic stress disorder: the neurobiological impact of psychological trauma. Diologues on Clinical Neuroscience. 2011;13:263–278. doi: 10.31887/DCNS.2011.13.2/jsherin. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siegel DJ. An interpersonal neurobiology of psychotherapy: The developing mind and the resolution of trauma. In: Soloman MF, Siegel DJ, editors. Healing Trauma: Attachment, Mind, Body, and Brain. New York: WW Norton & Company; 2003. pp. 1–56. [Google Scholar]
- Singer J, Willett J. Applied longitudinal data analysis: Modeling change and event occurrence. New York: Oxford University Press; 2003. [Google Scholar]
- Smith JD. Doctoral dissertation. FIELDING GRADUATE UNIVERSITY; 2010. Mindfulness-based stress reduction (MBSR) for women with PTSD surving domestic violence. [Google Scholar]
- Staub E. The psychology of bystanders, perpetrators, and heroic helpers. In: Newman LS, Erber R, editors. Understanding genocide: The social psychology of the Holocaust. New York: Oxford University Press; 2002. pp. 11–42. [Google Scholar]
- Tang SS, Freyd JJ. Betrayal trauma and gender differences in posttraumatic stress. Psychological Trauma: Theory, Practice, and Policy. 2012;4:469–478. [Google Scholar]
- Teasdale JD, Moore RD, Hayhurst H, Pope M, Williams S, Segal ZV. Megacognitive awareness and prevention of relapse into depression: Empirical evidence. Journal of Consulting and Clinical Psychology. 2002;70:275–287. doi: 10.1037//0022-006x.70.2.275. [DOI] [PubMed] [Google Scholar]
- van der Kolk BA, McFalane AC, Weisaeth L. Traumatic stress: The effects of overwhelming experience on mind, body, and society. New York: The Guilford Press; 2007. [Google Scholar]
- Weathers FW, Litz BT, Herman DS, Huska JA, Keane TM. The PTSD checklist: reliability, validity, & diagnostic utlity. Paper presented at the Annual Convention of the International Society for Traumatic Stress Studies; San Antonio, TX. 1994. [Google Scholar]
- Weaver TL, Clum GA. Psychological distress associated with interpersonal violence: A meta-analysis. Clinical Psychology Review. 1995;15:115–140. [Google Scholar]
- Yehuda R, LeDoux J. Response variation following trauma: A translational neuroscience approach to understanding PTSD. Neuron. 2007;56:19–32. doi: 10.1016/j.neuron.2007.09.006. [DOI] [PubMed] [Google Scholar]