Abstract
Central-line-associated bloodstream infections (CLABSI) are among the deadliest heathcare-associated infections, with an estimated 12–25% mortality rate. In 2014, the Centers for Medicare and Medicaid Services (CMS) began to penalize hospitals for poor performance with respect to selected hospital-acquired conditions, including CLABSI. A structural factor associated with high-quality nursing care and better patient outcomes is The Magnet Recognition Program®. The purpose of this study was to explore the relationship between Magnet status and hospital CLABSI rates. We used propensity score matching to match Magnet and non-Magnet hospitals with similar hospital characteristics. In a matched sample of 291 Magnet hospitals and 291 non-Magnet hospitals, logistic regression models were used to examine whether there was a link between Magnet status and CLABSI rates. Both before and after matching, Magnet hospital status was associated with better (lower than the national average) CLABSI rates (OR = 1.60, 95% CI: 1.10, 2.33 after matching). While established programs such as Magnet recognition are consistently correlated with high-quality nursing work environments and positive patient outcomes, additional research is needed to determine whether Magnet designation produces positive patient outcomes or rewards existing excellence.
Keywords: magnet hospital, work environment, infection, nursing care, CLABSI, HAC reduction program
On any given day, approximately 1 in 25 patients hospitalized in acute care hospitals in the United States (US) have a healthcare-associated infection (HAI), and in 2011, 75,000 patients with HAIs died during hospitalization (Center for Disease Control [CDC], 2015a; Magill et al., 2014). Infections associated with devices account for 26% of all HAIs (Magill et al., 2014). Central-line-associated bloodstream infections (CLABSI) are among the deadliest HAIs, with an estimated 12–25% mortality rate (Liang & Marschall, 2011; Stevens et al., 2014). CLABSIs increase patient morbidity, prolong hospital stays, and result in billions of dollars in excess healthcare costs (Goudie, Dynan, Brady, & Rettiganti, 2014; Liang & Marschall, 2011; Stevens et al., 2014). While recent reports suggest that CLABSI rates are decreasing overall, there are still an estimated 30,100 infections occurring in acute care hospital facilities each year, and the majority of CLABSIs are estimated to occur outside of intensive care units (CDC, 2015b; Liang & Marschall, 2011).
CLABSIs not only cause significant harm to patients and increase healthcare costs but may also result in additional financial consequences for hospitals. In 2014, the Centers for Medicare and Medicaid Services (CMS) began to penalize hospitals for poor performance with respect to HAIs (CMS, 2014; Rau, 2014). Under Section 3008 of the Affordable Care Act, the Hospital-Acquired Conditions (HAC) Reduction Program was created to incentivize hospitals to reduce the incidence of preventable adverse events at their institutions (Quality Net, n.d.). In the first year of the HAC Reduction Program, CMS cut Medicare payments to 721 hospitals for having high rates of preventable infections and patient injuries. The hospitals in the lowest-performing 25% saw a 1% reduction in Medicare payments (Quality Net, n.d.; Rau, 2014).
Hospitals are ranked based on three quality measures: (a) CLABSI rate; (b) catheter-associated urinary tract infection (CAUTI) rate; and (c) the Agency for Health-care Research and Quality Patient Safety for Selected Indicators (PSI-90) composite score, which includes eight patient safety indicators such as pressure ulcers and postoperative complications. HAC scores range from 1 to 10, and higher scores indicate worse performance. The HAC Score is divided into two domains. Domain 1 consists of the PSI-90 measure, and domain 2 includes both CLABSI and CAUTI rates. However, overlap between domains exists, as CLABSIs are also included as part of the PSI-90. When calculating the HAC Score, domain 1 is weighted at 35%, and domain 2 is weighted at 65% (Cassidy, 2015). Although a hospital's CLABSI rate is only one component of a hospital's HAC Score, poor performance on this measure has the potential to greatly affect a hospital's ranking.
The emphasis placed on CLABSI rates by the HAC Reduction Program increases the penalty for hospitals’ poor performance in this area. As a result, hospital administrators and clinicians are increasingly interested in identifying factors that could lead to lower CLABSI rates. Nurses play an important role in CLABSI prevention, as they have the most direct contact with patients and perform the majority of central line maintenance. In addition, nurses often assist with or guide the insertion of central lines; they are present to intervene if improper technique is observed; and they can advocate for central line removal if it becomes unnecessary. Efforts to reduce CLABSI infections have primarily focused on prevention through the use of multimodal central line “bundles” and checklists (Blot, Bergs, Vogelaers, Blot, & Vandijck, 2014). However, the success of nursing interventions and quality improvement initiatives may vary based on an organization's culture, clinical leadership, and available resources (Dixon-Woods, Bosk, Aveling, Goeschel, & Pronovost, 2011; The Joint Commission, 2012; Krein et al., 2010; Weaver, Weeks, Pham, & Pronovost, 2014).
Despite the importance of nurses to central line insertion and maintenance, as well as evidence that organizational culture is important in the success of quality improvement initiatives to reduce CLABSIs, there is relatively little evidence on the relationship between organizational features of nursing practice and CLABSI rates. One well-established structural marker for nursing excellence is the American Nurses Credentialing Center (ANCC) Magnet Recognition Program® (Aiken, Smith & Lake, 1994; Kelly, McHugh, & Aiken, 2011; Kutney-Lee et al., 2015). Magnet designation recognizes organizations for high-quality patient care, excellent nursing practice, and innovations in professional nursing practice. The framework of the Magnet Recognition Program includes five domains: (a) transformational leadership; (b) structural empowerment; (c) exemplary professional practice; (d) new knowledge, innovations, and improvements; and (e) empirical outcomes (ANCC, 2008). Magnet designation provides a useful indicator with which to examine the links between nursing excellence and CLABSI rates. The purpose of this study was to explore the relationship between Magnet status and CLABSI rates in Magnet and non-Magnet hospitals matched on hospital characteristics using propensity score matching.
Methods
Design and Data Sources
This observational study was a secondary analysis of cross-sectional hospital data from three national sources. The primary data source was Medicare's 2013 Hospital Compare Database of HAIs (Medicare.gov, n.d.a), which we merged with the 2013 American Hospital Association (AHA) Annual Survey (AHA, n.d.) using common hospital identifiers. Magnet status was obtained from the ANCC Magnet Recognition Program (ANCC, 2015a). The sample before matching included 1,995 hospitals: 291 Magnet and 1,704 non-Magnet.
Measures
CLABSI rate
The outcome variable was a hospital's CLABSI rate in 2013, which we obtained from the Hospital Compare Database of HAIs. These rates are established using infection data reported to the CDC's National Healthcare Safety Network (NHSN) for all patients admitted to acute care hospitals (Medicare.gov, n.d.b). CLABSIs are reported to the NHSN via a web-based tool, and infection preventionists manually identify cases in many hospitals.
CLABSI rates are reported as the standardized infection ratio (SIR), which is the observed or actual number of CLABSIs in a facility divided by the expected or predicted number of CLABSIs (Medicare.gov, n.d.b). The expected number of CLABSIs is calculated from baseline data from 2006 through 2008 (CDC, 2015b). The Hospital Compare CLABSI SIR is risk-adjusted to account for the patient care setting, hospital affiliation with a medical school, and bed size of the patient care location (Medicare.gov, n.d.b). The SIR is categorized based on its confidence interval (CI; Medicare.gov, n.d.b). When the lower limit of the CI is >1.0, the rate is considered “worse” than the national average, and when the upper limit is <1.0, the rate is considered “better” than the national average. If a SIR CI includes 1.0, the CLABSI rate is “no different” than the national average (Medicare.gov, n.d.b).
We dichotomized the CLABSI rate as either better or no different/worse because the primary goal for hospitals is to have better CLABSI rates than the national average, and there are many clinical and financial incentives for working towards this goal. Hospital initiatives have greatly reduced the frequency of infections, and a growing number have reported zero CLABSIs (Health Research & Educational Trust, 2011; Margolin, Robinson, D'Andrea, & Doyle, 2011). In many settings, one CLABSI infection is considered too many. Therefore, we focused on the “better than average” category as the most optimal outcome for patient safety and quality of care.
Magnet status
The main independent variable, hospital Magnet status, was established using the ANCC Magnet Recognition Program database. Hospitals were categorized as Magnet or non-Magnet as of the year 2012.
Hospital characteristics
Hospital characteristics were obtained from the 2013 AHA Annual Survey data. These characteristics have been used in previous research on Magnet hospitals (McHugh et al., 2013; Stimpfel, Rosen, & McHugh, 2014). Three categories of hospital size were created based on the number of beds set up and staffed at the hospital (≤100 beds, 101–250 beds, ≥251 beds). Teaching intensity was calculated as the ratio of the number of medical residents and interns per bed. Hospitals were categorized as high-technology if they performed open-heart or major transplant surgery or both. Hospital ownership was established as profit or not-for-profit. We controlled for hospital location using metropolitan, micropolitan, rural, or division core-based statistical area (CBSA). We also calculated the proportion of hospitals’ admissions with Medicaid as the primary payer and used the Herfindahl–Hirschman Index (Henke, Maeda, Marder, Friedman, & Wong, 2013) to measure market competition. Finally, a nurse staffing ratio variable was created by multiplying full-time-equivalent RN staffing by 1,768 and dividing by adjusted patient days to determine average RN hours per adjusted patient day (Spetz, Donaldson, Aydin, & Brown, 2008).
Data Analysis
We used descriptive statistics to compare the hospital characteristics and CLABSI rates of Magnet and non-Magnet hospitals. Using logistic regression, we examined the relationship between Magnet status and hospital CLABSI rates before and after controlling for hospital characteristics.
Propensity score matching
There are non-random differences in hospital characteristics between Magnet and non-Magnet facilities (McHugh et al., 2014). Hospitals with certain characteristics may be more likely to pursue or achieve Magnet status, and some of these characteristics may be highly correlated with quality of care. Propensity score matching permitted an “apples to apples” comparison of two groups balanced on the designated hospital characteristics and differing only by Magnet status (Austin, 2011).
Propensity scores were computed for each hospital based on a logistic regression of Magnet status on the confounding hospital characteristics. Using 1:1 nearest neighbor matching without replacement, 291 non-Magnet hospitals were matched to the full sample of 291 Magnet hospitals based on the propensity scores, eliminating 1,411 non-Magnet hospitals from the analyses. We evaluated the balance of the matched sample using standardized difference in means as well as histograms and jitter plots. Matching analyses were conducted using the MatchIt program in the R statistical software (Ho, Imai, King, & Stuart, 2007, 2011).
Nurse staffing was not included as a characteristic in propensity score matching. We were controlling for antecedent hospital characteristics that would likely lead to a hospital receiving Magnet status. Nurse staffing is not currently a criterion for Magnet recognition (ANCC, 2008). Although, evidence suggests that Magnet hospitals may have better nurse staffing levels when compared to non-Magnet hospitals (Aiken, Smith, & Lake, 1994; McHugh et al., 2013), it is unclear whether better staffing precedes or is the result of Magnet designation. We included nurse staffing in our post-matching logistic regression models as a covariate.
Logistic regression analysis
After matching, we performed doubly robust logistic regressions controlling for hospital characteristics, including nurse staffing. Using the observed covariates in the doubly robust models allowed us to control for any additional residual unobserved differences that may still exist between the matched subsamples (Funk et al., 2011). Descriptive and regression analyses were conducted using STATA® 13.1 (Stata Corp, 2013).
Results
Sample Characteristics Before and After Propensity Score Matching
As can been seen in Table 1, before matching, the most notable differences between Magnet and non-Magnet hospitals were that Magnet hospitals were larger (77.7% vs. 43.6%), high-technology (77.3% vs. 49.2%), major teaching facilities (22.7% vs. 9.7%), and not-for-profit (95.9% vs. 77.1%).
Table 1.
Characteristics of Magnet and Non-Magnet Hospitals Before and After Propensity Score Matching
| All Hospitals (N =1,995)
|
All Non-Magnet Hospitals (n =1,704)
|
All Magnet Hospitals (n = 291)
|
Matched Non-Magnet Hospitals (n = 291)
|
Standardized Difference in Means Between Magnet and Non-Magnet Hospitals
|
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | Before Matching | After Matching | |
| Bed size | ||||||||||
| Large (>250 beds) | 969 | 48.6 | 743 | 43.6 | 226 | 77.7 | 230 | 79.0 | 0.82 | −0.03 |
| Medium (101–250 beds) | 870 | 43.6 | 809 | 47.5 | 61 | 21.0 | 58 | 19.9 | −0.65 | 0.03 |
| Small (≤100 beds) | 156 | 7.8 | 152 | 8.9 | 4 | 1.4 | 3 | 1.0 | −0.64 | 0.03 |
| Technology status | ||||||||||
| High | 1,064 | 53.3 | 839 | 49.2 | 225 | 77.3 | 236 | 81.1 | 0.67 | −0.09 |
| Low | 931 | 46.7 | 865 | 50.8 | 66 | 22.7 | 55 | 18.9 | −0.67 | 0.09 |
| Teaching status | ||||||||||
| Major | 232 | 11.6 | 166 | 9.7 | 66 | 22.7 | 62 | 21.3 | 0.31 | 0.03 |
| Minor | 719 | 36.0 | 620 | 36.4 | 99 | 34.0 | 95 | 32.7 | −0.05 | 0.03 |
| Non-teaching | 1,044 | 52.3 | 918 | 53.9 | 126 | 43.3 | 134 | 46.1 | −0.21 | −0.06 |
| Ownership | ||||||||||
| For-profit | 402 | 20.2 | 390 | 22.9 | 12 | 4.1 | 15 | 5.2 | −0.94 | −0.05 |
| Not-for-profit | 1,593 | 79.9 | 1,314 | 77.1 | 279 | 95.9 | 276 | 94.9 | 0.94 | 0.05 |
| CBSA | ||||||||||
| Division | 533 | 26.7 | 446 | 26.2 | 87 | 29.9 | 83 | 28.5 | 0.08 | 0.03 |
| Metropolitan | 1,262 | 63.3 | 1,074 | 63.0 | 188 | 64.4 | 192 | 66.0 | 0.03 | −0.03 |
| Micropolitan | 186 | 9.3 | 171 | 1.0 | 15 | 5.2 | 15 | 5.2 | −0.22 | 0.00 |
| Rural | 14 | 0.7 | 13 | 0.8 | 1 | 0.3 | 1 | 0.3 | −0.07 | 0.00 |
|
|
||||||||||
| M | SD | M | SD | M | SD | M | SD | |||
|
|
||||||||||
| Market competition (HHI) | 704.6 | 1310.8 | 718.9 | 1341.8 | 621.1 | 1110.5 | 653.5 | 1182.7 | −0.09 | −0.03 |
| % Medicaid | 19.3 | 11.0 | 19.6 | 11.3 | 17.8 | 8.8 | 18.1 | 10.4 | −0.20 | −0.04 |
Note. CBSA, core-based statistical area (US Census): Division (>2.5 million), Metropolitan (50,000–2.5 million), Micropolitan (10,000–50,000), Rural (<10,000); M, mean; SD, standard deviation; HHI, Herfindahl-Hirschman Index.
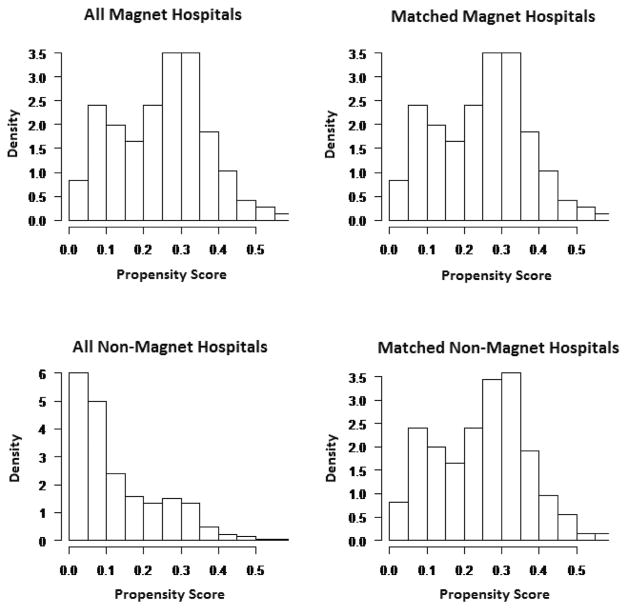
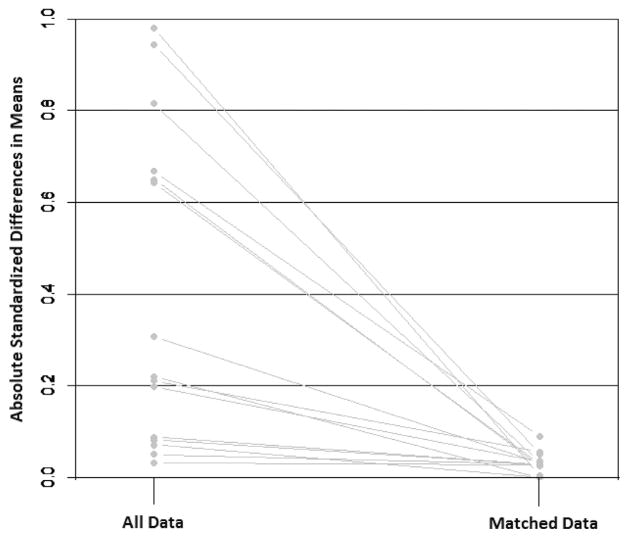
Prior to matching, the propensity scores indicating the likelihood of being a Magnet hospital based on designated hospital characteristics showed that the groups were dissimilar: 0.25 for the Magnet and 0.13 for the non-Magnet hospitals. After matching, the propensity scores for non-Magnet hospitals mirrored that of Magnet hospitals: 0.25. This improvement is illustrated in Figure 1, as the distributions of propensity scores for Magnet and non-Magnet hospitals were more similar after matching. As planned, the matched sample was more balanced with regard to hospital characteristics, which is demonstrated by the standardized differences in means (Table 1). Covariate balance improvement can be appreciated by comparing the standardized differences before and after matching. Whereas many standardized differences were large before matching, after matching they were all below 0.2, which is generally accepted as a threshold for a good match (Stuart, 2010). The similarity of the subsamples was greatly improved with regard to bed size, technology status, teaching status, ownership, market competition, and CBSA. The improvement in balance between the two sub-samples with matching is illustrated in Figure 2. However, for RN hours per adjusted patient day, which was not included in the propensity score, Magnet hospitals had higher RN hours per adjusted patient day than non-Magnet hospitals, both before matching (M =8.3, SD =2.3 vs. M =7.2, SD =2.3) and after matching (M =7.5, SD =2.0).
Figure 1.
Histograms of propensity scores of the Magnet and non-Magnet Hospitals before and after matching. The left side of the figure shows the distribution of propensity scores for all Magnet and all non-Magnet hospitals before matching. The right side shows the distribution of propensity scores for the Magnet and matched non-Magnet hospitals.
Figure 2.
Plot of standardized differences in means of Magnet and non-Magnet hospitals before and after matching. Demonstrated by the standardized differences in means, this figure shows the improved balance between the hospital characteristics of Magnet and non-Magnet hospital samples before and after matching. After matching, each of the individual hospital characteristics had a standardized difference in means below 0.2, considered a threshold for a good match.
Central-Line-Associated Bloodstream Infection Rates
About 29% of all hospitals had “better” CLABSI rates (lower than the national average; Table 2). Over half of Magnet hospitals were better than the average, compared to one-quarter of non-Magnet hospitals (p <0.001). In the matched sample, the percentage of non-Magnet hospitals with better CLABSI rates was 41.6%.
Table 2.
Central-Line-Associated Bloodstream Infection Rates in Magnet and Non-Magnet Hospitals Before and After Matching Using Propensity Scores
| All Hospitals (N =1,995)
|
All Non-Magnet Hospitals (n =1,704)
|
All Magnet Hospitals (n = 291)
|
Matched Non-Magnet Hospitals (n =291)
|
Before Matching
|
After Matching
|
|||||
|---|---|---|---|---|---|---|---|---|---|---|
| CLABSI Rate | n | % | n | % | n | % | n | % | p-value | p-value |
| Better | 581 | 29.1 | 428 | 25.1 | 153 | 52.6 | 121 | 41.6 | <0.001 | 0.008 |
| Worse | 1414 | 70.9 | 1276 | 74.9 | 138 | 47.4 | 170 | 58.4 | ||
Note. CLABSI, central line-associated bloodstream infection; Better, “better” than the national average; Worse, either “no different” or “worse” than the national average. p-values for differences between Magnet and non-Magnet hospitals were calculated using chi-square tests.
The results of the logistic regression models are shown in Table 3. In the unadjusted model for the total sample before matching (291 Magnet and 1,704 non-Magnet hospitals), Magnet hospitals had significantly higher odds of having better-than-average CLABSI rates (OR: 3.30; 95% CI: 2.56, 4.26). After adjusting for hospital characteristics, including nurse staffing, Magnet hospitals had 54% (OR: 1.54; 95% CI: 1.14, 2.09) higher odds of having better CLABSI rates. After matching (291 Magnet and 291 non-Magnet hospitals), Magnet hospitals continued to have significantly higher odds of better-than-average CLABSI rates, both in bivariate models (OR =1.56, 95% CI: 1.12, 2.16) and in doubly robust models controlling for matched structural characteristics plus nurse staffing (OR =1.60, 95% CI: 1.10, 2.33). Of note, the seven small hospitals that were included in the matched subsamples were dropped from the doubly robust logistic regression model, because of complete separation (Albert & Anderson, 1984). That is, none of the seven small hospitals experienced the outcome of being “better” regarding CLABSI rates, and the model allocated these hospitals into one group.
Table 3.
Hospital Magnet Status as Predictor of CLABSI Rates Before and After Matching on Hospital Characteristics
| Bivariate Logistic Regression
|
Logistic Regression, Adjusted Modelsc
|
|||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p | OR | 95% CI | p | |
| Before matchinga | 3.30 | 2.56–4.26 | <0.001 | 1.54 | 1.14–2.09 | 0.005 |
| After matchingb | 1.56 | 1.12–2.16 | 0.008 | 1.60 | 1.10–2.33 | 0.013 |
Note. CLABSI, central line-associated blood stream infection; OR, odds ratio; CI, confidence interval.
N =1995.
n =582 in bivariate model; n =575 in adjusted model (7 small hospitals were dropped from the analysis due to complete separation of the model; none had better-than-average CLABSI rates).
Adjusted models controlled for hospital characteristics: bed size, technology status, teaching status, ownership, Market Competition/Herfindahl–Hirschman Index, % Medicaid, core-based statistical area, and nurse staffing. Magnet and non-Magnet hospitals were not matched on nurse staffing.
Discussion
This is the first study to show a relationship between Magnet designation, an indicator of nursing excellence, and better hospital CLABSI rates. Our principal results indicate that Magnet hospitals were more likely to have lower–than-average CLABSI rates than non-Magnet hospitals, even when important hospital characteristics were controlled by matching. These results add to evidence that Magnet status, while awarded for positive organizational culture, also is a marker for positive empirical outcomes (ANCC, 2015a). Magnet status has been linked to lower patient mortality and failure to rescue, as well as less nurse burnout and job dissatisfaction (Aiken, Havens, & Sloane, 2000; Friese, Xia, Ghaferi, Birkmeyer, & Banerjee, 2015; Kutney-Lee et al., 2015; Lake, Shang, Klaus, & Dunton, 2010; McHugh et al., 2013).
However, it remains unclear from these observational studies whether better outcomes are a result of Magnet recognition, or whether Magnet status recognizes institutions with better outcomes. Kutney-Lee and colleagues conducted a 2-stage panel study and found significant improvements in the nurse work environment and patient outcomes in hospitals seeking Magnet recognition compared to non-Magnet hospitals, suggesting that the Magnet process may be transformative. Likewise, McHugh et al. (2013) found that outcomes before Magnet recognition in hospitals that eventually gained Magnet status were not significantly different from non-Magnet hospitals; this suggests that the better outcomes in Magnet hospitals develop through the process of Magnet recognition and do not precede it. In contrast, Friese et al.'s (2015) findings implied that the Magnet process is not transformative but instead identifies hospitals with already-good outcomes. In a longitudinal study design, they found that Magnet hospitals had better patient outcomes than non-Magnet hospitals, and outcomes were no different before and after obtaining recognition (Friese et al., 2015).
Results of two other studies challenged the positive results in Magnet hospitals. Goode, Blegen, Park, Vaughn, and Spetz (2011) found that non-Magnet hospitals had better outcomes for infections, postoperative sepsis, and postoperative metabolic derangement than Magnet hospitals. Mills and Gillespie (2013) saw no difference in pressure ulcer and failure to rescue rates for matched samples of Magnet and non-Magnet hospitals. However, the clinical significance and generalizability of these studies may be limited by small sample size and variability in measurement of outcomes. Therefore, additional research is needed to understand the nature of the relationship between Magnet recognition and patient outcomes and to determine whether Magnet hospitals develop better outcomes than comparable non-Magnet hospitals as a result of the recognition process or whether better outcomes are present before Magnet recognition.
Patients with central lines are increasingly being found outside ICUs (Liang & Marschall, 2011), increasing opportunities for infection exposure. Nursing care is critical to the prevention of CLABSIs, which requires vigilance and the autonomy to make patient care recommendations. Interventions to reduce CLABSIs have incorporated hand hygiene; aseptic techniques when accessing the line; appropriate timing and technique for changing intravenous tubing, dressings, and accessing ports; and daily review of the necessity of the line (Blot et al., 2014; The Joint Commission, 2012). However, these quality improvement initiatives are most successful in hospitals with favorable organizational environments (Dixon-Woods et al., 2011; Krein et al., 2010; Zingg et al., 2015).
Magnet designation represents, in part, strong leadership, shared governance, and interdisciplinary collaboration: all reflections of a positive organizational culture, which may provide some explanation for the relationship between Magnet status and better CLABSI rates. The present results add to existing evidence that Magnet recognition may be valuable to patients seeking the best institutions for care and to hospital administrators attempting to decrease CLABSI rates in order to improve quality of care and avoid CMS penalties. Currently, less than 8% of all registered hospitals in the US have achieved Magnet status (ANCC, 2015a). While financial and other resource constraints may prevent some hospitals from pursuing Magnet status, there are a variety of ways for hospitals to become Magnet-like. The ANCC Pathway to Excellence Program® (ANCC, 2015b), a credentialing program recognizing excellent nursing environments, is suited to smaller healthcare organizations and long-term care facilities. Regardless of credentials, by adhering to the Magnet criteria (ANCC, 2008), hospitals can foster strong nursing leadership and enable increased nursing autonomy, shared decision-making, and opportunities for professional growth. Additionally, organizations can cultivate successful inter-professional relationships and follow evidence-based guidelines to promote exemplary patient care.
Hospitals with engaged clinical leaders and a culture focused on patient care were more successful in implementing programs to reduce CLABSIs than those with a weak cultural identity and poor relationships (Krein et al., 2010). Conversely, a lack of an impetus to change and insufficient resources have been identified by nurses and other healthcare professionals as organizational barriers to the implementation of HAI reduction initiatives (Flanagan, Welsh, Kiess, Hoke, & Doebbeling, 2011). An overarching organizational perspective that supports nurses’ decision-making and autonomy and fosters positive nurse-physician relationships is necessary to promote nursing excellence. In order for efforts to be successful in reducing CLABSI rates, it is important for hospitals and administrators to create environments that allow for exemplary practice.
Limitations
Due to the cross-sectional nature of this research, we were unable to determine causality. We used propensity score matching and doubly robust logistic regression models in an attempt to reduce selection bias; however, there is the chance that unobserved differences in hospital characteristics influenced our results. We used hospital-level aggregates for CLABSI rates, which limited our ability to draw conclusions about individual hospital units. Additionally, the increasing focus on value-based care and the reliance of hospital Medicare reimbursement payments on optimal CLABSI performance may result in under-reporting of infections in some instances (Lin et al., 2010). Furthermore, we do not know whether Magnet hospitals in our sample were implementing quality improvement initiatives to reduce CLABSIs, which could explain lower CLABSI rates. However, without a positive organizational environment, initiatives to improve preventive clinical practices may have limited effect (Dixon-Woods et al., 2011; Krein et al., 2010; Zingg et al., 2015).
Conclusion
The Affordable Care Act's HAC Reduction Program has levied penalties on hospitals for poor performance regarding CLABSI rates. Thus, hospitals will increasingly engage in efforts to reduce the number of CLABSIs and improve hospital performance. Successful programs and policies that decrease CLABSI rates will not only reduce financial penalties to hospitals, they will improve patient health and outcomes (Kandilov, Coomer, & Dalton, 2014).
Our study is concordant with other literature suggesting a relationship between Magnet status and better patient outcomes. The nature of the relationship between Magnet status and CLABSI rates should be investigated with additional research to determine whether Magnet recognition is the cause, or result, of better CLABSI rates. In either case, our findings add to the literature suggesting that outcomes are better in Magnet hospitals, and that Magnet status may be a useful indicator of quality for patients.
Acknowledgments
This study was funded by the National Institute of Nursing Research/NIH (T32NR007104, Aiken, PI); National Institute on Aging (R01AG041099-01, McHugh, PI); and The Robert Wood Johnson Foundation (Aiken, PI).
Contributor Information
Hilary Barnes, Postdoctoral Research Fellow, Center for Health Outcomes and Policy Research, University of Pennsylvania, School of Nursing, 418 Curie Blvd., Room 388R, Philadelphia, PA 19104.
Jessica Rearden, Postdoctoral Research Fellow, Center for Health Outcomes and Policy Research, University of Pennsylvania, School of Nursing, Philadelphia, PA.
Matthew D. McHugh, Associate Director, Center for Health Outcomes and Policy Research, The Rosemarie Greco Term Endowed, Associate Professorship in Advocacy, University of Pennsylvania, School of Nursing, Philadelphia, PA
References
- Aiken LH, Havens DS, Sloane DM. The Magnet nursing services recognition program: A comparison of two groups of Magnet hospitals. The American Journal of Nursing. 2000;100:26–36. doi: 10.1097/NNA.0b013e3181aeb469. [DOI] [PubMed] [Google Scholar]
- Aiken LH, Smith HL, Lake ET. Lower Medicare mortality among a set of hospitals known for good nursing care. Medical Care. 1994;32:771–787. doi: 10.1097/00005650-199408000-00002. [DOI] [PubMed] [Google Scholar]
- Albert A, Anderson JA. On the existence of maximum likelihood estimates in logistic regression models. Biometrika. 1984;71:1–10. doi: 10.2307/2336390. [DOI] [Google Scholar]
- American Hospital Association. AHA data and directories. n.d Retrieved from http://www.aha.org/research/rc/stat-studies/data-and-directories.shtml.
- American Nurses Credentialing Center. Announcing a new model for ANCC’s Magnet Recognition Program®. 2008 Retrieved from http://www.nursecredentialing.org/MagnetModel.
- American Nurses Credentialing Center. Magnet Recognition Program overview. 2015a Retrieved from http://www.nursecredentialing.org/Magnet/ProgramOverview.
- American Nurses Credentialing Center. ANCC Pathway To Excellence®. 2015b Retrieved from http://www.nursecredentialing.org/Pathway.
- Austin PC. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate Behavioral Research. 2011;46:399–424. doi: 10.1080/00273171.2011.568786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blot K, Bergs J, Vogelaers D, Blot S, Vandijck D. Prevention of central line-associated bloodstream infections through quality improvement interventions: A systematic review and meta-analysis. Clinical Infectious Diseases. 2014;59:96–105. doi: 10.1093/cid/ciu239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cassidy A. Health policy brief: Medicare’s hospital-acquired condition reduction program. 2015 Retrieved from http://www.healthaffairs.org/healthpolicybriefs/brief.php?brief_id=142.
- Centers for Disease Control and Prevention. Healthcare-associated infections (HAIs): Data and statistics. 2015a Retrieved from http://www.cdc.gov/HAI/surveillance/
- Centers for Disease Control and Prevention. Bloodstream infection event (central line-associated bloodstream infection and non-central line associated bloodstream infection) 2015b Retrieved from http://www.cdc.gov/nhsn/PDFs/pscManual/4PSC_CLABScurrent.pdf.
- Centers for Medicare and Medicaid Services. Hospital-Acquired Condition (HAC) Reduction Program. 2014 Retrieved from https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/HAC-Reduction-Program.html.
- Dixon-Woods M, Bosk CL, Aveling EL, Goeschel CA, Pronovost PJ. Explaining Michigan: Developing an ex post theory of a quality improvement program. Milbank Quarterly. 2011;89:167–205. doi: 10.1111/j.1468-0009.2011.00625.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flanagan ME, Welsh CA, Kiess C, Hoke S, Doebbeling BN. A national collaborative for reducing health care-associated infections: Current initiatives, challenges, and opportunities. American Journal of Infection Control. 2011;39:685–689. doi: 10.1016/j.ajic.2010.12.013. [DOI] [PubMed] [Google Scholar]
- Friese CR, Xia R, Ghaferi A, Birkmeyer JD, Banerjee M. Hospitals in ‘Magnet’ program show better patient outcomes on mortality measures compared to non-‘Magnet’ hospitals. Health Affairs (Millwood) 2015;34:986–992. doi: 10.1377/hlthaff.2014.0793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Funk MJ, Westreich D, Wiesen C, Sturmer T, Brookhart MA, Davidian M. Doubly robust estimation of causal effects. American Journal of Epidemiology. 2011;173:761–767. doi: 10.1093/aje/kwq439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goode CJ, Blegen MA, Park SH, Vaughn T, Spetz J. Comparison of patient outcomes in Magnet® and non-Magnet hospitals. Journal of Nursing Administration. 2011;41:517–523. doi: 10.1097/NNA.0b013e3182378b7c. [DOI] [PubMed] [Google Scholar]
- Goudie A, Dynan L, Brady PW, Rettiganti M. Attributable cost and length of stay for central line-associated bloodstream infections. Pediatrics. 2014;133:e1525–e1532. doi: 10.1542/peds.2013-3795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Health Research & Educational Trust. Eliminating CLABSI: A national patient safety imperative. 2011 Retrieved from http://www.ahrq.gov/sites/default/files/publications/files/clabsi-update.pdf.
- Henke RM, Maeda JL, Marder WD, Friedman BS, Wong HS. Medicare and commercial inpatient resource use: Impact of hospital competition. American Journal of Managed Care. 2013;19:e238–e248. [PubMed] [Google Scholar]
- Ho DE, Imai K, King G, Stuart EA. Matching as nonparametric preprocessing for reducing model dependence in parametric causal inference. Political Analysis. 2007;15:199–236. http://j.mp/jPupwz. [Google Scholar]
- Ho D, Imai K, King G, Stuart EA. MatchIt: Nonpara-metric preprocessing for parametric causal inference. Journal of Statistical Software. 2011;42:1–28. doi: 10.18637/jss.v042.i08. [DOI] [Google Scholar]
- The Joint Commission. Preventing central line-associated bloodstream infections: A global challenge, a global perspective. 2012 Retrieved from http://www.jointcommission.org/assets/1/18/CLABSI _Monograph.pdf.
- Kandilov AMG, Coomer NM, Dalton K. The impact of hospital-acquired conditions on Medicare program payments. Medicare & Medicaid Research Review. 2014;4:E1–E23. doi: 10.5600/mmrr.004.04.a01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly LA, McHugh MD, Aiken LH. Nurse outcomes in Magnet® and non-Magnet hospitals. The Journal of Nursing Administration. 2011;41:428–433. doi: 10.1097/NNA.0b013e31822eddbc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krein SL, Damschroder LJ, Kowalski CP, Forman J, Hofer TP, Saint S. The influence of organizational context on quality improvement and patient safety efforts in infection prevention: A multi-center qualitative study. Social Science & Medicine. 2010;71:1692–1701. doi: 10.1016/j.socscimed.2010.07.041. [DOI] [PubMed] [Google Scholar]
- Kutney-Lee A, Stimpfel AW, Sloane DM, Cimiotti JP, Quinn LW, Aiken LH. Changes in patient and nurse outcomes associated with Magnet hospital recognition. Medical Care. 2015;53:550–557. doi: 10.1097/MLR0000000000000355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lake ET, Shang J, Klaus S, Dunton NE. Patient falls: Association with hospital Magnet status and nursing unit staffing. Research in Nursing & Health. 2010;33:413–425. doi: 10.1002/nur.20399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang SY, Marschall J. Vital signs: Central line-associated blood stream infections-United States, 2001, 2008, and 2009. Annals of Emergency Medicine. 2011;58:447–450. doi: 10.1016/j.annemergmed.2011.07.035. [DOI] [PubMed] [Google Scholar]
- Lin MY, Hota B, Khan YM, Woeltje KF, Borlawsky TB, Doherty JA … CDC Prevention Epicenter Program. Quality of traditional surveillance for public reporting of noso-comial bloodstream infection rates. Journal of the American Medical Association. 2010;304:2035–2041. doi: 10.1001/jama.2010.1637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magill SS, Edwards JR, Bamberg W, Beldavs ZG, Dumyati G, Kainer MA, … Fridkin SK. Multistate point-prevalence survey of health care-associated infections. New England Journal of Medicine. 2014;370:1198–1208. doi: 10.1056/NEJMoa1306801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Margolin FS, Robinson W, D’Andrea G, Doyle A. Getting to zero: Reducing rates of CLABSI in community hospitals. 2011 Retrieved from http://www.leapfroggroup.org/media/file/Final_GettingToZero.pdf.
- McHugh MD, Hawkins RE, Mazmanian PE, Romano PS, Smith HL, Spetz J. Challenges and opportunities in nurse credentialing research design. 2014 Retrieved from http://nam.edu/perspectives-2014-challenges-and-opportunities-in-nurse-credentialing-research-design/
- McHugh MD, Kelly LA, Smith HL, Wu ES, Vanak JM, Aiken LH. Lower mortality in Magnet hospitals. Medical Care. 2013;51:382–388. doi: 10.1097/MLR.0b013e3182726cc5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Medicare., gov. About Hospital Compare Data. n.d.a Retrieved from https://www.medicare.gov/hospitalcompare/Data/About.html.
- Medicare., gov. Healthcare-associated infections. n.d.b Retrieved from https://www.medicare.gov/hospitalcompare/Data/Healthcare-Associated-Infections.html.
- Mills AC, Gillespie KN. Effect of Magnet hospital recognition on 2 patient outcomes. Journal of Nursing Care Quality. 2013;28:17–23. doi: 10.1097/NCQ.0b013e318268a710. [DOI] [PubMed] [Google Scholar]
- Quality Net. Overview: Hospital-Acquired Conditions (HAC) Reduction Program. n.d Retrieved from https://www.qualitynet.org/dcs/ContentServer?c=Page&pagename=QnetPublic%2FPage%2FQnetTier2&cid=1228774189166.
- Rau J. Medicare cuts payments to 721 hospitals with highest rates of infections, injuries. 2014 Retrieved from http://khn.org/news/medicare-cuts-payments-to-721-hospitals-with-highest-rates-of-infections-injuries/
- Spetz J, Donaldson N, Aydin C, Brown DS. How many nurses per patient? Measurements of nurse staffing in health services research. Health Services Research. 2008;43:1674–1692. doi: 10.1111/j.1475-6773.2008.00850.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stata, Corp. Stat statistical software: Release 13. College Station, TX: StataCorp LP; 2013. [Google Scholar]
- Stevens V, Geiger K, Concannon C, Nelson RE, Brown J, Dumyati G. Inpatient costs, mortality and 30-day readmission in patients with central line-associated bloodstream infections. Clinical Microbiology and Infection. 2014;20:O318–O324. doi: 10.1111/1469-0691.12407. [DOI] [PubMed] [Google Scholar]
- Stimpfel AW, Rosen JE, McHugh MD. Understanding the role of the professional practice environment on quality of care in Magnet(R) and non-Magnet hospitals. Journal of Nursing Administration. 2014;44:10–16. doi: 10.1097/NNA0000000000000015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stuart EA. Matching methods for causal inference: A review and a look forward. Statistical Science. 2010;25:1–21. doi: 10.1214/09-STS313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weaver SJ, Weeks K, Pham JC, Pronovost PJ. On the CUSP: Stop BSI: Evaluating the relationship between central line-associated bloodstream infection rate and patient safety climate profile. American Journal of Infection Control. 2014;42:S203–S208. doi: 10.1016/j.ajic.2014.05.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zingg W, Holmes A, Dettenkofer M, Goetting T, Secci F, Clack L, … Pittet D. Hospital organisation, management, and structure for prevention of health-care-associated infection: A systematic review and expert consensus. The Lancet Infectious Diseases. 2015;15:212–224. doi: 10.1016/S1473-3099(14)70854-0. [DOI] [PubMed] [Google Scholar]