Abstract
The transition from pediatric to adult healthcare is often challenging for adolescents and young adults with sickle cell disease (SCD). Our study aimed to identify (1) measures of success for the transition to adult healthcare and (2) barriers and facilitators to this process. We interviewed 13 SCD experts and asked them about their experiences caring for adolescents and young adults with SCD. Our interview guide was developed based on Social-ecological Model of Adolescent and Young Adult Readiness to Transition framework, and interviews were coded using the constant comparative method. Our results showed that transition success was measured by healthcare utilization, quality of life, and continuation on a stable disease trajectory. We also found that barriers to transition include negative experiences in the emergency department, sociodemographic factors, and adolescent skills. Facilitators include a positive relationship with the provider, family support, and developmental maturity. Success in SCD transition is primarily determined by the patients’ quality of relationships with their parents and providers and their developmental maturity and skills. Understanding these concepts will aid in the development of future evidence-based transition care models.
Keywords: Sickle Cell Anemia, Adolescent, Young Adult, Transition to Adult Care
INTRODUCTION
Over the past two decades, survival rates for individuals with Sickle Cell Disease (SCD) have steadily improved. Recent studies show a 93.9–98.4% survival rate to 18 years of age,1 with many individuals with SCD now living into their fifties and sixties.2 However, survival improvements are less evident among young adults aged 20–24.2 This discrepancy coincides with the point in time immediately following transition from pediatric to adult healthcare, with one potential explanation being gaps in care during the sometimes haphazard period of transition.1,2 Additional studies highlight higher hospitalizations, readmissions, and acute care utilization for young adults ages 18–30.3–5 Providers have indicated that there is a high need for more comprehensive transition programming for adolescents and young adults (AYAs) with SCD.6–9 In spite of this identified need, there is still a lack of agreed-upon outcomes of what constitutes a successful transition.8,10 Most transition programs targeted at AYAs with SCD use attendance at the first appointment with an adult provider as an outcome of success, or assess the patients’ transition readiness via questionnaire.6,11–13 However, there is still insufficient knowledge about factors that lead to successful or unsuccessful transitions.8,10
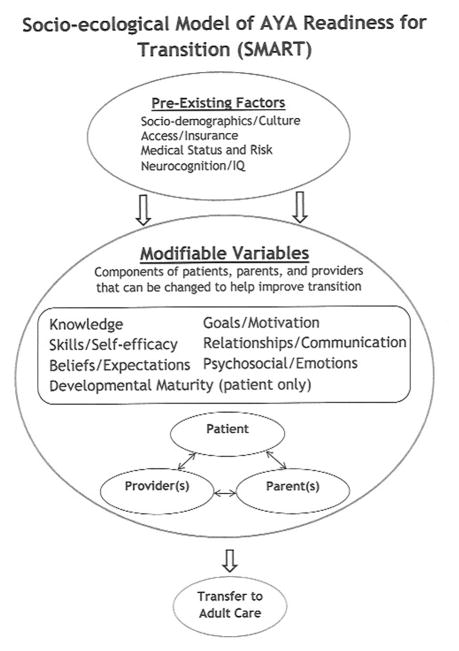
In order to better understand transition readiness and develop evidence-based interventions, Schwartz and colleagues developed the Social-ecological Model of Adolescent and Young Adult Readiness to Transition (SMART). The model outlines 11 domains that contribute to a young adult’s readiness to transition to adult care; seven of these are considered modifiable variables, and the other four are considered less amenable to change (see Figure 1).14,15 All of the variables can act as either threats or facilitators to a successful transition to adult healthcare. Schwartz and colleagues propose that all of the modifiable variables except developmental maturity may relate to the parent, provider and patient. The interactions among these three parties and the improvement of the modifiable domains influence transition readiness.14,15 In this study, we aimed to identify metrics of transition success, and barriers and facilitators to transition from pediatric to adult healthcare for AYAs with SCD, using the SMART model as a framework. We sought diverse perspectives from interviews with SCD providers throughout the United States.
Figure 1.
Socio-Ecological Model of AYA Readiness for Transition (SMART).
Reprinted with permission from JAMA Pediatrics. Original source: Schwartz LA, Brumley LD, Tuchman LK, et al. Stakeholder Validation of a Model of Readiness for Transition to Adult Care. JAMA Pediatr. 2013.
MATERIALS AND METHODS
Setting
We conducted semi-structured qualitative interviews with pediatric and adult providers who specialize in SCD. Two trained research assistants conducted the interviews either over the phone or in person at The Children’s Hospital of Philadelphia. We conducted the interviews between December 2012 and April 2013, and each lasted approximately 60 minutes.
Participant Recruitment
We recruited experts in SCD from the Philadelphia area and other major cities throughout the United States. Initially, we gathered names through discussion with the medical director of the Sickle Cell Program at The Children’s Hospital of Philadelphia and through a review of recent SCD transition literature. We selected first and senior authors from these articles to recruit for the study. We then used a snowball sampling method where we asked each participant to suggest other potential participants.16,17 The snowball sampling method ensured that we recruited participants who were identified and recognized by their colleagues as experts and key stakeholders in the field.16,17 We used a purposive sample in order to be representative of pediatric and adult healthcare perspectives. We continued to recruit participants and conduct interviews until the data reached thematic saturation (interview themes continued to be repeated and new themes were not found). In total we invited 30 clinicians specializing in SCD, and 13 agreed to participate.
Data Collection
We developed the interview guide based on the SMART model, a review of the transition literature, and consultation with experts. We emailed the SMART model to providers before the interview. We first asked them about their level of experience with the transition process and their experience working with AYAs with SCD. We then asked them to recount at least one story of a patient they cared for who had a successful transition and at least one story of a patient who they cared for who had an unsuccessful transition. Using these stories and the SMART model as a basis, we probed for information on outcomes, barriers and facilitators of transition. The complete interview guide is available as supplementary online content.
Data Analysis
All interviews were audiotaped, and transcribed. We used the components of the SMART model to guide the coding process, and derived related themes. At least two of three reviewers (NBS, CWP, MSL) independently coded each transcript. We used the constant comparative method,18 continuously revising our codes as the interviews were ongoing based on emerging themes in the data. When discrepancies occurred, the reviewers discussed the discrepancy and either resolved it through consensus or brought in the third reviewer to assist in resolution.
Human Subjects Research
The Children’s Hospital of Philadelphia Institutional Review Board determined this study to be an exempted study.
RESULTS
Participants
The 13 participants in this study represented the fields of medicine, social work, psychology, and nursing, and had an average of 22.6 years of experience working with AYAs. See Table 1 for additional information about participants. Participants from outside of Philadelphia were from Denver, CO, Greensboro, NC, Baltimore, MD and Cincinnati, OH.
Table 1.
Participant Characteristics
| Pediatrics | Adult | |
|---|---|---|
|
Role
| ||
| Physician | 3 | 4 |
| Psychologist | 2 | 0 |
| Nurse | 1 | 0 |
| Social Worker | 3 | 0 |
|
| ||
|
Location
| ||
| In Philadelphia | 7 | 2 |
| Outside Philadelphia | 2 | 2 |
|
| ||
|
Gender
| ||
| Male | 2 | 1 |
| Female | 7 | 3 |
|
| ||
| # Years working with AYA | ||
|
| ||
| 5–10 | 2 | 0 |
| 11–15 | 0 | 2 |
| 16–20 | 0 | 0 |
| 21–25 | 3 | 1 |
| 26–30 | 2 | 0 |
| <30 | 2 | 1 |
Analysis of the transcripts and coding yielded data on threats and facilitators to transition from pediatric to adult healthcare, as well as metrics of transition success. Below we outline the data results, including the themes of threats and facilitators that are consistent with SMART.
Metrics of transition success
We asked participants how they determined whether a transition was successful. Their answers primarily fell into 3 categories: healthcare utilization, quality of life, and continuing on a stable disease trajectory. Healthcare utilization included making and keeping medical appointments, medication adherence, and avoiding preventable hospitalizations. Quality of life outcomes were often defined as achieving appropriate developmental milestones, such as obtaining post-secondary education or employment, getting married, or having children. Participants described the continuation along a stable disease trajectory as the patient’s disease continuing at the same severity as in pediatric care or improving, and not developing unexpected complications such as stroke. One participant recounted a story about a young man who at 12 was able to independently answer questions about his medical status, and is now successfully pursuing a bachelor’s degree (quality of life), and has not been hospitalized in six years largely due to his excellent medication compliance (stable disease trajectory and appropriate healthcare utilization).
Threats
I. Sociodemographic factors and psychosocial/emotional status
Providers often acknowledged how sociodemographic factors, such as poverty, challenging home life, and parent education level, related to psychological functioning and, ultimately, transition outcomes. Transition planning and healthcare were often in competition with other demands. One participant explained, “They are at risk… socio-demographically, and all of those factors are intertwined with being able to access care appropriately and in a way that will help them manage their disease …[their] coping skills are not good and the social supports are not in place.” Participants were also quick to highlight the positive transition outcomes of patients who were not experiencing these challenges. A provider noted, “She wasn’t dealing with some of the more basic problems of having a stable place to live, having stable income. [That] complicates transition.” These themes are consistent with SMART in that sociodemographic variables impact psychological status and resources such as coping and family functioning, which ultimately compromises the ability to make a smooth transition.
II. Neurocognitive deficits due to stroke
Consistent with SMART’s emphasis on the importance of medical status and cognitive functioning, a number of participants pointed out that stroke and its sequelae can directly impact the patient’s ability to understand their own disease process and navigate the systems that, as discussed, are often difficult for all AYAs. One participant described the impact of stroke limiting patients’ abilities to “1) completely understand their disease; 2) be able to identify appropriate ways to manage their disease; and 3) be able to actually implement them at a time of crisis or when they are not doing well.”
III. Experiences in the emergency department – self-efficacy, beliefs, and expectations
Young adult patient’s negative experiences in adult emergency departments (ED) were reported to impact the SMART components of self-efficacy, beliefs, and expectations. This was particularly detrimental to the transition process when it occurred before the individual had developed a good rapport with his or her adult hematologist. Participants cited three main reasons for negative ED experiences. First, the transfer to adult care was abrupt, and the pediatric or adult provider did not have the opportunity to fully prepare the patient. Participants explained that patients sometimes required ED care because they did not yet feel comfortable with their new adult provider, were not yet receiving proper ambulatory medical care, or had poor disease self-management skills and self-efficacy, which contributed to a sickle cell crisis. Second, participants discussed how patients were sometimes viewed by ED providers as “drug seekers,” and received delayed or inadequate pain medication. Participants perceived that patients generalized this negative experience with the entire adult medical system, subsequently distrusted all providers in an adult institution. Third, patients may have had the unrealistic expectation that the adult ED experience would be similar to that of the pediatric ED, which may have led to what patients’ perceived as a negative experience.
One provider explained the connection between patients’ experiences and their likelihood of seeking appropriate healthcare in the future: “The first experience of the ED can be very negative, and if that experience is a negative experience then I think patients are less likely to present to emergency in the future. They will wait too long before they come into emergency.”
IV. Adolescent skills
In concordance with SMART, many participants noted the complexity of the skills and the level of health literacy expected of AYAs with SCD as a barrier. Comparable skills are typically not demanded of their peers without a chronic illness until much further into adulthood. One participant commented, “I think it takes a fairly above average person to [do] what we ask young people to do… a whole lot more than I ask my healthy young adult [son] to do.” AYAs often have difficulty navigating the healthcare system and following through with scheduling appointments or refilling medication. Participants acknowledged barriers in the healthcare systems that are difficult for some older adults to negotiate, such as knowing what to do about a lapse in insurance or if insurance does not cover a needed medication. Participants also cited the difficult skill of being able to explain sickle cell pain and where it is manifesting, in a believable and articulate manner, while in pain. Participants identified that in addition to requiring adequate health literacy, AYAs need to be proficient in planning and problem solving appropriately. Overall, participants seemed to agree that the majority of AYAs do not acquire these skills before they transition to an adult provider, and having them is the exception and not the rule. As one participant notes, this steep learning curve can have mortal consequences, “I do think they either die or they grow up. There are a few who straggle along with very bad behaviors for a long time, but either, honestly, they die from bad behaviors and no follow-up, or they survive through this process and eventually become more functional.”
Facilitators
I. Developmental Maturity- motivation
Participants identified motivated and bright young people, who often had good social support networks and supportive families, as examples of patients who transitioned successfully. This relates to developmental maturity and motivation in SMART. One provider described one of her successful patients by saying, “I think the fact that she was in college shows that she was meeting all of her developmental milestones and doing well […] the fact that she actually went to college also is a big indicator that she was probably going to be fine regardless.” However, providers also identified a number of successful patients who lacked family support, and were often forced to take on increased responsibility at a young age due to their social and family situation. These participants were often very motivated to take care of themselves and exhibited developmental maturity beyond what might have been expected from someone of that age. One participant explicated this inconsistency quite succinctly with the following statement: “I think they were all very resilient young people, that is the word I would say.”
II. Positive relationships between patient and provider
As SMART emphasizes positive provider-patient relationships and communication, participants who were pediatric providers repeatedly cited trusting relationships between the patient and provider as a facilitator to successful transition. They explained that when patients were comfortable discussing treatment plans and asking questions openly, they were more likely to be successful when they transferred to an adult provider. When asked what factors contributed to a patient’s successful transition, one participant explained, “Talking about transition, setting goals, reinforcement on both sides, I think encouraging him to ask questions and understand his disease in a way that made sense and to think about what it would be like as an adult, what things would he have to do on his own and making sure he had practice to get those done before he transitioned.”
Adult providers discussed the concepts of trust and relationships less often, but did emphasize the importance of assistance from other non-physician staff, such as social workers, in helping AYAs achieve success in the adult system. One of the participants explained his team’s approach to new young adult patients, “When I first started this and I saw my first transition patient I assumed they would be an adult. I was wrong … From my end, anybody who transitions gets a visit with my social worker. My whole team gets to meet them and know them and so that we can help them through the process.”
III. Family support – Positive relationships and parent skills
Participants cited social and family support as facilitators of the transition process, representing the SMART components of relationships and parent skills. In most contexts, participants described family members who were supportive of their children with SCD, but who emphasized independence and self-management as a priority in other areas of the child’s life as well as with regard to healthcare. One participant discussed a patient who he had cared for who came from a family with a low socioeconomic status, a single mother, and many siblings. The participant described the mother’s dedication to helping her children succeed, emphasizing education and disease self-management. According to the participant, the support and high expectations that this mother had for her son’s abilities was a contributing factor to his success. He was able to successfully manage his SCD as a young adult, and went on to graduate from law school.
Participants also emphasized that parents provide support by encouraging the patient to learn independence, but remaining present as a safety net if the patient runs into difficulties. One participant described this situation, “She was comfortable coming to the visits on her own. I am not saying that parents don’t help with the transition, but the absence of her parents and my comfort with her description of her past medical history… were positive indicators.”
DISCUSSION
In summary, participants identified metrics for transition as healthcare utilization, quality of life, and disease trajectory. Additionally according to SCD transition experts, barriers to transition for this population include negative experiences in the ED, limitations in developmental maturity and skills, sociodemographics, and neurocognitive deficits, often due to strokes. Facilitators to transition include positive and supportive relationships with parents and providers, parent skills to facilitate disease self-management, and the patients’ developmental maturity and motivation.
Our study highlights the need for SCD-specific transition planning given the unique issues faced by young adults with SCD, and furthers the field by identifying specific areas to warrant attention. Many studies have identified a need for comprehensive transition planning for SCD patients,1,2,8,10 and some evaluate proposed models of care.8,9,19–21 Few studies have examined facilitators and barriers in the transition process. One study identified the following threats to successful transition: beginning transition education and transition clinic after 21 years of age, having the genotype SC or Sβ+ (considered less severe forms of the disease), and not requiring chronic transfusion therapy.12 Our theoretically informed study builds on this by identifying additional threats to the transition process to be further explored, including developmental maturity, cognitive deficits and negative experiences in the emergency department, and contributes information about facilitators to transition for patients with SCD.
Overall, we found that pediatric and adult providers discussed similar themes related to barriers and facilitators to transition for AYA with SCD. The most notable difference was the way the providers addressed their relationship with the patient. Pediatric providers cited the importance of a trusting relationship with the patient more often than adult providers. Recent studies also show that providers often have negative perceptions of patients with SCD, especially when they present to the emergency department22,23. Challenges in the emergency department also came up as a theme in the current study. Thus, educating adult and emergency room providers about negative experiences and the distrust of medical providers experienced by many AYAs with SCD may help improve the patient-provider relationship, thus improving transition outcomes.
One re-occurring theme in the interviews was that many transition-related expectations are challenging due to limitations in adolescents’ developmental maturity. This idea is consistent with the neuroscience literature demonstrating that brain development and maturation continue into the mid-twenties.24,25 Studies show that one of the last areas to reach maturation is the pre-frontal cortex, which is responsible for executive functioning, specifically complex planning and goal-orientation.25–29 While this challenge is true of all transitioning populations, having SCD confers greater risk for deficits in cognitive skills given that many individuals with SCD experience strokes, further affecting their cognition and executive functioning skills. SCD patients have a high rate of, including silent infarcts, which occur in approximately 27%-37% of this population.21,30 Although patients who experience silent infarcts often do not report any symptoms, neurocognitive testing has shown decreased IQ scores in these patients.
Some literature on transition for populations with intellectual disabilities emphasizes the role of family support31,32. Similarly, because AYA with SCD often have neurocognitive deficits, interventions should focus on incorporating the family system into supporting the AYA with his or her transition. This approach would also address the issue of lack of developmental maturity and difficulty with executive functioning and planning. Another theme of transition challenges that disproportionately impact AYAs with SCD is the impact of poverty, healthcare access and level of education. Other research shows that health disparities exist in transition supports for African American and Hispanic youth33–35. Given that the majority of patients with SCD are African American, the results of our study are consistent with the literature showing health disparities for this population.
However, while these challenges hindered successful transition, many participants recounted stories of successful outcomes for their patients despite these risks. Thus, our results support other research highlighting the importance of resilience factors in at-risk youth36–39. While there is a large body of literature showing interventions that can be used to foster resilience in at-risk youth36–39, this area of research has not been adequately integrated into the transition literature. Utilizing the current body of research on resilience to develop transition interventions could be very useful in improving transition outcomes, specifically because youth with SCD often face both sociodemographic and illness-related challenges.
Finally, our study provides further evidence of validity for and utility of the SMART model.14,15 Almost all of the components of SMART emerged in the coding of the interviews. In addition, the participants described the importance of all stakeholders in the system (patient, providers, and parents) and the reciprocal relationships—an important feature of SMART. As emphasized by SMART, there are variables that confer risk and resilience in the transition process that are amenable to change and should be targets of intervention to improve transition readiness (e.g., skills, relationships, motivation). Clinicians should consider teaching strategies to augment the AYAs still-developing executive functioning skills, paying particular attention to the development of a positive and trusting relationship with AYAs, and, whenever possible, including the family as a support to help enforce the AYAs’ skills. The main element of the SMART model that did not come up frequently in the current study is “knowledge”. This is consistent with the opinion of Schwartz and colleagues that knowledge and skills are not sufficient for a successful transition that leaves the AYA appropriately engaged in the adult healthcare system14. These data suggest that future interventions should target areas other than knowledge, including: motivation, relationships, self-efficacy and developmental maturity.
Limitations
This study has three main limitations. First, our sample size was small. However, we achieved thematic saturation- the closest approximation of a power calculation in qualitative research. Second, we acknowledge that we interviewed few adult providers (n=4) and were also unable to recruit non-physician participants from adult practices. While this may be indicative of the differences between the pediatric and adult healthcare systems,10,40 these perspectives would provide additional insight. Third, we only examined the views of providers. Future studies should ask similar questions to both parents and AYAs.
Conclusions and future directions
The current study characterizes three metrics that may be used to determine transition success, identifies important barriers and facilitators to a successful transition process, validates existing findings in the transition literature, and illustrates the need to look across disciplines to better understand the complexities of transition to adult healthcare. Considering the many common difficulties that adolescents face when they are moving through the transition process, it is important to approach transition planning, education and interventions with an understanding of the neurological maturity of the adolescent brain and the complex systems that young people are expected to navigate to ensure they are receiving appropriate healthcare. With this in mind, additional attention should be paid to teaching problem-solving skills, specifically as they relate to navigating healthcare systems and with an emphasis on explicitly addressing common roadblocks that they will likely face. Another significant consideration is assisting the adolescent in determining who is part of the support system and safety net, and who is available to answer questions and help troubleshoot when issues arise. Also, the use of consistent metrics, such as those defined in this study, could help move clinical and research practice forward, by providing benchmarks for comparison among interventions and practices. For the barriers that are less modifiable on an individual basis, researchers and policy makers should explore systems-level changes that include built in patient-assistance, such as patient navigators to assist with insurance difficulties.
Future research should combine the development of transition practices with neuroscience research, in order to understand the best way to teach adolescents. Further, future research should also seek to identify links between the current findings in the resilience literature and facilitators to successful transition. Finally, providers who are working with AYAs with SCD should be particularly sensitive to their sociodemographic backgrounds and how that impacts their interactions and beliefs about the health care system. Additional research is needed to develop and evaluate culturally competent transition programming for AYAs with SCD.
Supplementary Material
Table 2.
Representative Quotes From Each Theme
| Threats |
|---|
Sociodemographic factors and psychosocial/emotional status
|
Neurocognitive deficits due to stroke
|
Experiences in the emergency department
|
Adolescent skills
|
| Facilitators |
|---|
Developmental maturity
|
Positive relationships between patient and provider
|
Family support
|
Acknowledgments
Funding Source: This study was funded by the Center for Pediatric Clinical Effectiveness, The Children’s Hospital of Philadelphia, Philadelphia, PA.
References
- 1.Quinn CT, Rogers ZR, McCavit TL, Buchanan GR. Improved survival of children and adolescents with sickle cell disease. Blood. 2010;115(17):3447–3452. doi: 10.1182/blood-2009-07-233700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hamideh D, Alvarez O. Sickle cell disease related mortality in the United States (1999–2009) Pediatr Blood Cancer. 2013;60:1482–1486. doi: 10.1002/pbc.24557. [DOI] [PubMed] [Google Scholar]
- 3.Dickerson AK, Klima J, Rhodes MM, O’Brien SH. Young Adults With SCD in US Children’s Hospitals: Are They Different From Adolescents? Pediatr Blood Cancer. 2012;58:741–745. doi: 10.1002/pbc.23262. [DOI] [PubMed] [Google Scholar]
- 4.Brousseau DC, Owens PL, Mosso AL, Panepinto JA, Steiner CA. ACute care utilization and rehospitalizations for sickle cell disease. JAMA. 2010;303(13):1288–1294. doi: 10.1001/jama.2010.378. [DOI] [PubMed] [Google Scholar]
- 5.Hunt SE, Sharma N. TRansition from pediatric to adult care for patients with sickle cell disease. JAMA. 2010;304(4):408–409. doi: 10.1001/jama.2010.1026. [DOI] [PubMed] [Google Scholar]
- 6.McPherson M, Thaniel L, Minniti CP. Transition of Patients With Sickle Cell Disease From Pediatric to Adult Care: Assessing Patient Readiness. Pediatr Blood Cancer. 2009;52:838–841. doi: 10.1002/pbc.21974. [DOI] [PubMed] [Google Scholar]
- 7.Telfair J, Alexander LR, Loosier PS, Alleman-Velez PL, Simmons J. Providers’ Perspectives and Beliefs Regarding Transition to Adult Care for Adolescents with Sickle Cell Disease. J Healthc Underserved. 2004;15(3):443–461. doi: 10.1353/hpu.2004.0049. [DOI] [PubMed] [Google Scholar]
- 8.Treadwell M, Telfair J, Gibson RW, Johnson S, Osunkwo I. Transition from pediatric to adult care in sickle cell disease: Establishing evidence-based practice and directions for research. Am J Hematol. 2011;86(1):116–120. doi: 10.1002/ajh.21880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Doulton D. From cradle to commencement: Transitioning pediatric sickle cell disease patients to adult providers. J Pediatr Oncol Nurs. 2010;27(2):119–123. doi: 10.1177/1043454209350155. [DOI] [PubMed] [Google Scholar]
- 10.DeBaun MR, Telfair J. Transition and Sickle Cell. Pediatrics. 2012;130:926–935. doi: 10.1542/peds.2011-3049. [DOI] [PubMed] [Google Scholar]
- 11.Hankins JS, Osarogiagbon R, Adams-Graves P, et al. A Transition Pilot Program for Adolescents With Sickle Cell Disease. J Pediatr Health Care. 2012;26(6):e45–e49. doi: 10.1016/j.pedhc.2012.06.004. [DOI] [PubMed] [Google Scholar]
- 12.Andemariam B, Owarish-Gross J, Grady J, Boruchov D, Thrall RS, Hagstrom JN. Identification of risk factors for an unsuccessful transition from pediatric to adult sickle cell disease care. Pediatr Blood Cancer. 2014;61:697–701. doi: 10.1002/pbc.24870. [DOI] [PubMed] [Google Scholar]
- 13.Sobota A, Akinlonu A, Champigny M, et al. Self-reported Transition Readiness Among Young Adults With Sickle Cell Disease. J Pediatr Hematol Oncol. 2014;36(3) doi: 10.1097/MPH.0000000000000110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schwartz LA, Tuchman LK, Hobbie WL, Ginsberg JP. A social-ecological model of readiness for transition to adult-oriented care for adolescents and young adults with chronic health conditions. Child Care Health Dev. 2011;37(6):883–895. doi: 10.1111/j.1365-2214.2011.01282.x. [DOI] [PubMed] [Google Scholar]
- 15.Schwartz LA, Brumley LD, Tuchman LK, et al. Stakeholder Validation of a Model of Readiness for Transition to Adult Care. JAMA Pediatr. 2013 doi: 10.1001/jamapediatrics.2013.2223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Crosby R, Salazar L, DiClemente R. Research Methods in Health Promotion. San Francisco, CA: Jossey-Bass; 2006. Principles of sampling; pp. 289–316. [Google Scholar]
- 17.Palinkas LA, Horwitz SM, Green CA, Wisdom JP, Duan N, Hoagwood K. Purposeful Sampling for Qualitative Data Collection and Analysis in Mixed Method Implementation Research. Adm Policy Ment Health Ment Health Serv Res. 2013 doi: 10.1007/s10488-013-0528-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Glaser B, Strauss A. The Discovery of Ground Theory: Strategies for Qualitative Research. New York, NY: Aldine De Gruyter; 1967. [Google Scholar]
- 19.Latzman RD, Majumdar S, Bigelow C, et al. Transitioning to adult care among adolescents with sickle cell disease: A transitioning clinic based on patient and caregiver concerns and needs. Int J Child Adolesc Health. 2011;3(4):537–545. [Google Scholar]
- 20.Smith GM, Lewis VR, Whitworth E, Gold DT, Thornburg CD. Growing up with sickle cell disease: A pilot study of a transition program for adolescents with sickle cell disease. J Pediatr Hematol Oncol. 2011;33:379–382. doi: 10.1097/MPH.0b013e318211bb2e. [DOI] [PubMed] [Google Scholar]
- 21.Wills KE, Nelson SC, Hennessy J, et al. Transition Planning for Youth With Sickle Cell Disease: Embedding Neuropsychological Assessment Into Comprehensive Care. PEDIATRICS. 2010;126(Supplement):S151–S159. doi: 10.1542/peds.2010-1466J. [DOI] [PubMed] [Google Scholar]
- 22.Freiermuth CE, Haywood C, Silva S, et al. Attitudes Toward Patients With Sickle Cell Disease in a Multicenter Sample of Emergency Department Providers. Adv Emerg Nurs J. 2014;36(4):335–347. doi: 10.1097/TME.0000000000000036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Haywood C, Lanzkron S, Hughes MT, et al. A Video-Intervention to Improve Clinician Attitudes Toward Patients with Sickle Cell Disease: The Results of a Randomized Experiment. J Gen Intern Med. 2011;26(5):518–523. doi: 10.1007/s11606-010-1605-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gogtay N, Giedd JN, Lusk L, et al. Dynamic mapping of human cortical development during childhood through early adulthood. Proc Natl Acad Sci U S A. 2004;101(21):8174–8179. doi: 10.1073/pnas.0402680101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yurgelun-Todd D. Emotional and cognitive changes during adolescence. Curr Opin Neurobiol. 2007;17:251–257. doi: 10.1016/j.conb.2007.03.009. [DOI] [PubMed] [Google Scholar]
- 26.Dumontheil I, Houlton R, Christoff K, Blakemore S-J. Development of relational reasoning during adolescence. Dev Sci. 2010;13(6):F15–F24. doi: 10.1111/j.1467-7687.2010.01014.x. [DOI] [PubMed] [Google Scholar]
- 27.Johnson SB, Blum RW, Giedd JN. Adolescent maturity and the brain: The promise and pitfalls of neuroscience research in adolescent health policy. J Adolesc Health. 45:216–221. doi: 10.1016/j.jadohealth.2009.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Luna B, Padmanabhan A, O’Hearn K. What has fMRI told us about the Development of Cognitive Control through Adolescence? Brain Cogn. 72:101–113. doi: 10.1016/j.bandc.2009.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sturman DA, Moghaddam B. The neurobiology of adolescence: Changes in brain architecture, functional dynamics, and behavioral tendencies. Neurosci Biobehav Rev. 2011;35:1704–1712. doi: 10.1016/j.neubiorev.2011.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.DeBaun MR, Armstrong FD, McKinstry RC, Ware RE, Vichinsky E, Kirkham FJ. Silent cerebral infarcts: a review on a prevalent and progressive cause of neurologic injury in sickle cell anemia. Blood. 2012;119(20):4587–4596. doi: 10.1182/blood-2011-02-272682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Henninger NA, Taylor JL. Family Perspectives on a Successful Transition to Adulthood for Individuals With Disabilities. Intellect Dev Disabil. 2014;52(2):98–111. doi: 10.1352/1934-9556-52.2.98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bindels-de Heus KGCB, van Staa A, van Vliet I, Ewals FVPM, Hilberink SR. Transferring Young People With Profound Intellectual and Multiple Disabilities From Pediatric to Adult Medical Care: Parents’ Experiences and Recommendations. Intellect Dev Disabil. 2013;51(3):176–189. doi: 10.1352/1934-9556-51.3.176. [DOI] [PubMed] [Google Scholar]
- 33.Amaral S, Patzer R. Disparities, race/ethnicity and access to pediatric kidney transplantation. Curr Opin Nephrol Hypertens. 2013;22(3):336–343. doi: 10.1097/MNH.0b013e32835fe55b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lotstein DS, Kuo AA, Strickland B, Tait F. The Transition to Adult Health Care for Youth With Special Health Care Needs: Do Racial and Ethnic Disparities Exist? PEDIATRICS. 2010;126(Supplement):S129–S136. doi: 10.1542/peds.2010-1466F. [DOI] [PubMed] [Google Scholar]
- 35.Richmond N, Tran T, Berry S. Receipt of Transition Services Within a Medical Home: Do Racial and Geographic Disparities Exist? Matern Child Health J. 2011;15(6):742–752. doi: 10.1007/s10995-010-0635-2. [DOI] [PubMed] [Google Scholar]
- 36.Rutter M. Annual Research Review: Resilience – clinical implications. J Child Psychol Psychiatry. 2013;54(4):474–487. doi: 10.1111/j.1469-7610.2012.02615.x. [DOI] [PubMed] [Google Scholar]
- 37.Davies SL, Thind HR, Chandler SD, Tucker JA. Enhancing resilience among young people: the role of communities and asset-building approaches to intervention. Adolesc Med State Art Rev. 2011;22(3):402–440. [PubMed] [Google Scholar]
- 38.Earvolino-Ramirez M. Resilience: A Concept Analysis. Nurs Forum (Auckl) 2007;42(2):73–82. doi: 10.1111/j.1744-6198.2007.00070.x. [DOI] [PubMed] [Google Scholar]
- 39.Goldstein AL, Faulkner B, Wekerle C. The relationship among internal resilience, smoking, alcohol use, and depression symptoms in emerging adults transitioning out of child welfare. Child Abuse Negl. 2013;37(1):22–32. doi: 10.1016/j.chiabu.2012.08.007. [DOI] [PubMed] [Google Scholar]
- 40.Grosse SD, Schechter MS, Kulkarni R, Lloyd-Puryear MA, Strickland B, Trevathan E. Models of comprehensive multidisciplinary care for individuals in the United States with genetic disorders. Pediatrics. 2009;123:407–412. doi: 10.1542/peds.2007-2875. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.