Abstract
Elderly patients frequently present with surgical emergencies to health care providers, and outcomes in this group of patients remain poor. Contributing factors include frailty, preexisting comorbidity, polypharmacy, delayed diagnosis, and lack of timely and consultant-led treatment. In this review, we address common emergency surgical presentations in the elderly and highlight the specific challenges in caring for these patients. We summarize 20 years of reports by various medical bodies that have aimed to improve the care of these patients. To improve morbidity and mortality, several aspects of care need to be addressed. These include accurate and timely preoperative assessment to identify treatable pathology and, where possible, to consider and correct age-specific disease processes. Identification of patients in whom treatment would be futile or associated with high risk is needed to avoid unnecessary interventions and to give patients and carers realistic expectations. The use of multidisciplinary teams to identify common postoperative complications and age-specific syndromes is paramount. Prevention of complications is preferable to rescue treatment due to the high proportion of patients who fail to recover from adverse events. Even with successful surgical treatment, long-term functional decline and increased dependency are common. More research into emergency surgery in the elderly is needed to improve care for this growing group of vulnerable patients.
Keywords: emergency surgery, elderly care, risk assessment, frailty
Introduction
This review aims to address the issues facing clinicians looking after elderly patients presenting as a surgical emergency. Common presentations and potential pitfalls are highlighted. Evidence-based solutions to improve care are discussed.
Defining old age
The World Health Organization defines old age as 60 years and over, although in poorer countries with lower life expectancy than in developed countries, ages as low as 50–55 years can be used.1 In the UK, the government’s National Service Framework for Older People further classifies old age into stages (shown in Table 1), reflecting how disease states and physiological deterioration can affect different individuals in different ways.2 This continuum of old age progresses from fit and healthy through to frailty. Frail older people are at greater risk of complication and death when they present with acute surgical emergencies.
Table 1.
Definitions of old age
| Group | Age | Goals |
|---|---|---|
| Entering old age | ||
| Completed their career in paid employment and/or child rearing Are active and independent and many remain so into late old age | Includes people as young as 50 years old, or from the official retirement ages of 60 for women and 65 for men | Promote and extend healthy active life Compress morbidity (the period of life before death spent in frailty and dependency) |
| Transitional phase | ||
| In transition between healthy, active life and frailty | This transition often occurs in the seventh or eighth decades of life but can occur at any stage of older age | Identify emerging problems ahead of crisis Ensure effective responses that will prevent crisis and reduce long-term dependency |
| Frail older people | ||
| These people are vulnerable as a result of health problems such as stroke or dementia, social care needs, or a combination of both | Frailty is often experienced only in late old age, so services for older people should be designed with their needs in mind | Anticipate and respond to problems, recognizing the complex interaction of physical, mental, and social care factors, which can compromise independence and quality of life |
Note: Data from Department of Health UK.2
Epidemiology
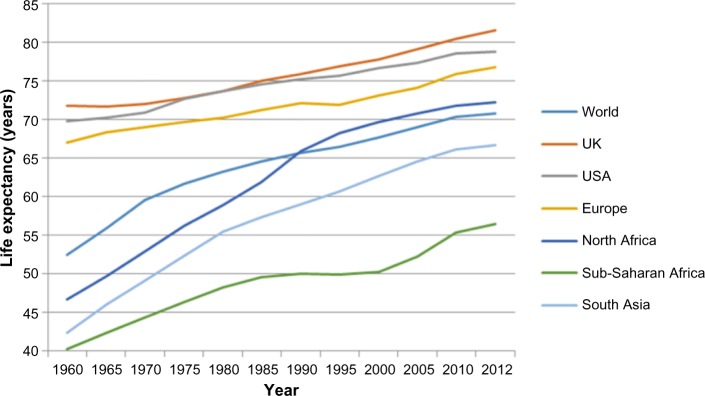
Across the globe, populations are getting older. Currently, 17% of the UK population is aged 65 years and older. Average life expectancy for this group of patients currently stands at a further 20–30 years. Surgical emergency presentations are increasingly common in this age category, so this represents a significant workload for the emergency clinician.3 The challenge of caring for an aging population is only set to increase. It is estimated that the number of people in the UK aged 65 years and older will increase by nearly two-thirds to reach 15.8 million by 2031. By this time, those aged 65 years and older will account for 22% of the UK population, with 5% being older than 90 years.4 This trend is replicated globally (Figure 1).5
Figure 1.
Life expectancy spanning the years between 1960 and 2012.
Note: Data were downloaded from the World Bank Web site (http://www.worldbank.org).64
Emergency admissions to hospital have increased considerably over the past 15 years around the world.6 Recent data from the Centre for Health Service Economics and Organisation have shown that 40% of hospital admissions occur in people aged older than 65 years and this age group accounts for the largest increase in admissions since 2000 when compared to patients aged 18–64 years (increase of 45.6% vs 36%, respectively).6 In addition, increases in rates of emergency admission in patients aged older than 90 years (50%) are being observed compared to patients aged 65–69 years (10%).
Older patients can present emergency health care providers with specific challenges owing to an increase in comorbidity and increased risk of perioperative morbidity and mortality relative to their younger counterparts.7,8 Mortality in elderly patients after emergency surgical presentations can approach 50% in some studies. It is not only poor survival that has been a driver to improve outcome in this vulnerable elderly group; surviving patients also have increased dependency following emergency presentation. This can manifest as patients needing additional care and support in their own homes or needing to move into 24-hour care.9 This constitutes a considerable burden on acute and social care services, with subsequent resource and financial implications.10
There is an acknowledgment that at times, older people still may not be offered or may not accept elective surgical procedures as frequently as their younger counterparts. This was an issue addressed in the joint Royal College of Surgeons of England document “Access all ages”, which looked at elective surgery rates.11 This document quoted figures showing that elective inguinal hernia repairs peak in the age group of 75–79 years, as opposed to emergency repairs, which are commonest in the 85–89 age group. The authors suggested that earlier elective surgery may have avoided later higher-risk emergency surgery.
It must be recognized, however, that the elderly population is very heterogeneous in many ways and that chronological age can be fairly meaningless and a better marker of outcome after surgery is usually biological age.
Emergency surgery in the elderly – a publication timeline
It has long been acknowledged that elderly patients having surgery can have worse outcomes. Depending on the specific scenario, these poor outcomes can manifest in different ways, eg, as increased risk of peri- or postoperative death, development of postoperative complications, prolonged length of hospital stay, or discharge destination being other than the patient’s own home (ie, the need for rehabilitation, care, or nursing home placement). This inequality has been the focus of several high-profile reports by medical bodies in the UK. These reports span two decades, during which there has been growing understanding of the scale of the problems facing elderly patients and increasing pressure to minimize this inequality and reduce age discrimination. However, improvements in holistic surgical care have been slow to develop and more remains to be done to see a significant improvement in the emergency care of elderly patients. Data from these audits and reports are being used to drive quality improvement. A summary of all significant reports and guidance relating to emergency surgery in the elderly is provided in Table 2. Much more high-quality research data are required on this group of vulnerable patients to improve care.
Table 2.
Summary of reports and guidance on elderly emergency surgery
| Year | Title, reference | Publishing body | Key recommendations or findings |
|---|---|---|---|
| 1999 | Extremes of age10 | NCEPOD | Failings in perioperative management of elderly patients Poor intravenous fluid management Lack of multidisciplinary teams and senior clinician involvement |
| 2001 | National Service Framework for Older People2 | Department of Health, UK | Outlines the quality standards for organizations delivering care to older people in the UK Equality of access to and provision of care for older people |
| 2009 | Ageism and age discrimination in secondary health care in the UK60 | Department of Health and Centre for Policy on Ageing | Highlighted inequality for older people in both perceived and actual access to health care and treatment within the NHS |
| 2010 | An age old problem1 | NCEPOD | 44% of elderly patients admitted to surgical specialties; there was room for improvement in care 6% received care that was less than satisfactory |
| 2010 | Falling standards, broken promises. National audit of falls and bone health in older people61 |
Royal College of Physicians, UK | One-third of hip fracture patients did not receive adequate pain relief within an hour of arriving in hospital Inadequate attention to pressure area care in the first 4 hours and early prescription of intravenous fluids was lacking in many cases |
| 2011 | The management of hip fractures in adults16 | NICE | Recommended the use of integrated multidisciplinary geriatric care and to focus on osteoporosis management, polypharmacy, frailty management, and prevention and assessment of falls |
| 2011 | High-risk surgical patient17 | ASGBI | Elderly patients at particular risk of complications, including death Improved care would come by improving the identification of patients at risk and ensuring early access to definitive treatment by a trained specialist Rapid and appropriate escalation of care to higher dependency wards (ie, intensive care unit) was also recommended as a means of improving outcome |
| 2012 | Silver Book: quality care for older people with urgent and emergency care needs62 | British Geriatric Society | Focuses on the first 24 hours of care Specifically highlights multidisciplinary working |
| 2012 | Access all ages: assessing the impact of age on access to surgical treatment11 | RCSEng, Age UK, and MHP Health Mandate | 25 Recommendations focusing on six key areas: 1. Informing and communicating with patients to encourage them to seek help and take part in decisions about their treatment and care 2. Improving the evidence base to further our understanding of the impact of age on surgical decision making. 3. Developing guidance to promote age equality in surgical care 4. Delivering the most appropriate care by improving models of working and developing guidance for clinicians 5. Measuring progress and tackling underperformance 6. Delivering high-quality commissioning for older people |
| 2014 | National Hip Fracture Database Annual Report63 | Falls and Fragility Fractures Audit Programme | One of the key elements is “best practice tariff” for surgery within 48 hours Target was achieved for 70.6% in the 2012–2013 report and slightly increased to 71.7% for 2013 Range in hospital performance is dramatic, with some sites reporting just 13% of patients having surgery within 36 hours and yet some hospitals reporting rates of 91% |
| 2014 | Perioperative care of the elderly guidelines48 | AAGBI | Highlights the ageing population and the challenges elderly patients place on the NHS Outlines specific considerations regarding perioperative management; recommends a multidisciplinary approach with the role of geriatricians in the assessment and ongoing care of the elderly emergency patients |
Abbreviations: AAGBI, Association of Anaesthetists of Great Britain and Ireland; ASGBI, Association of Surgeons of Great Britain and Ireland; NCEPOD, National Confidential Enquiry into Patient Outcome and Death; NICE, National Institute for Health and Care Excellence; NHS, National Health Service; RCSEng: Royal College of Surgeons of England.
Specific challenges of emergency surgery in the elderly
By no means exhaustive, the areas discussed herein demonstrate the breadth and depth of the problems faced by surgeons and emergency physicians in caring for elderly patients presenting as an emergency. Conditions affecting communication such as stroke, dementia, and hearing loss can affect the timely diagnosis of conditions. In addition, premorbid function can affect both choice of treatment and the level of perioperative support that may reasonably be offered to elderly patients.
Frailty
Campbell and Buchner12 defined frailty as “a condition or syndrome which results from a multisystem reduction in reserve capacity to the extent that a number of physiological systems are close to, or past, the threshold of symptomatic clinical failure”. This definition fits with a phenotypic model of frailty.13 Another model can be easier to quantify using a “frailty index” taking a holistic approach to accumulated issues, including social support and mood. Key elements of frailty include the following: unintentional weight loss, self-reported exhaustion, weakness (reduced grip strength and other factors), slow walking speed, and low physical activity. Patients with frailty presenting as an emergency have little physiological reserve and undergoing major operative intervention results in high mortality and increased dependence.6,14 Correctly identifying frailty can help emergency clinicians in decision making about the care of patients and aid in the informed consent process involving patients, families, and carers. It is important to remember that frailty is not an inevitability of aging and may be the only long-term condition an individual has.
Functional decline
Following a period of inactivity or bed rest, elderly patients can experience deconditioning.15 This is a multifactorial process of physiological changes, which results in loss of f unctional ability in areas such as mental capacity, continence, mobility, and daily activities. Deconditioning is common after emergency admission to hospital.
The effects are wide ranging and include loss of muscle mass, causing reduced mobility and contributing to falls and pressure sores. In addition, patients can develop anorexia and malnutrition (with constipation or incontinence) and, psychologically, patients can become disoriented, feel socially isolated, and suffer anxiety and depression. Functional decline can be debilitating and impede recovery to normal activities of daily living.
Functional decline following surgery can be reversed in most instances, with a return of function by 6 months. Some elderly patients are at particular risk of functional disability, including those having frailty, dementia, or chronic renal impairment. Targeting patients who show early signs of functional decline with physiotherapy can help maintain function.
Hip fracture
Hip fractures are common in the elderly, with around one million hip fractures occurring per year in the UK. These types of fractures are often labeled “fragility fractures”, a phrase that also reflects the typical patient who suffers them. Most hip fracture patients are in their mid-80s with osteoporosis or osteopenia and multiple comorbidities.16 Up to a third of patients will die in the 12 months following a hip fracture and up to 20% of patients become more dependent, requiring ongoing institutional care.16
It is prudent to remember that falls in the elderly can be attributed to causes other than simply slips and trips: hypotension or dizziness from medications, as well as syncope from cardiac events or underlying diseases, such as infections, should all be considered during assessment of any patient who has fallen.
Following several critical reports on the care received by elderly patients following hip fracture, there is now a change in clinical practice.1,17 The National Institute for Health and Care Excellence (NICE) published guidance strongly recommending multidisciplinary management of this predominantly frail cohort of elderly patients to include review by a specialist geriatric team.18 This novel, structured approach to care of the high-risk elderly population represents a dramatic change in the approach to care for these patients. In hip fracture, the focus of postoperative care has moved from surgical outcomes, such as mortality and complication rate, to encompass other outcome measures, such as timeliness of surgery, dependency, and quality of life. There is now compelling evidence that delays in surgery increase mortality, and therefore surgery within 48 hours of admission is viewed as a quality standard. The funding of hip fracture programs and orthogeriatricians is still a significant barrier to implementation of this guidance.19
Major trauma in the elderly
Major trauma is a significant cause of morbidity and mortality in younger patients, but it also affects the elderly.20 Mortality in this group is high, and although ~10% of trauma patients are older than 65 years of age, this group accounts for more than a quarter of fatalities.20 Identification of injury and rapid intervention are the keys to successful trauma outcomes, although this can leave little time for optimization of existing comorbidity and postoperative physiological support from critical care is often required.
Trauma pathways based on risk prediction scoring systems are commonly used to triage severely injured patients. However, severely injured elderly patients can be missed by standard scoring systems due to abnormal response to trauma, eg, due to artificially elevated blood pressure (BP) from preexisting disease and delirium. Therefore, pulse rate and systolic BP as predictors of injury severity are unreliable in geriatric trauma patients.21 In a study by Heffernan et al,22 it was demonstrated that in elderly patients with a “normal” BP (>110 mmHg) and heart rate (<90 beats per minute), many were actually shocked, resulting in a significant increase in mortality compared to their younger counterparts. Owing to age-related physiological deconditioning, elderly patients are at increased risk of poor outcome, and trauma pathway activation using age (>70 years) alone as a criterion has been advocated by some.23
Temporary or permanent increased physical dependency following trauma is not uncommon in the elderly. This puts increased emotional and financial burden on family and friends, as well as demands on social services to provide increased care for patients. Early inpatient rehabilitation can help reduce the risk of long-term dependency, shorten in-patient stay, and reduce mortality.20
Acute abdomen
Diagnosis in elderly patients presenting with an acute abdomen is challenging. Comorbidity such as stroke and dementia can result in communication difficulties. In addition, elderly patients may not present with the typical features one would expect in certain intra-abdominal conditions. Elderly patients may have reduced or atypical pain or show absence of signs in intra-abdominal sepsis. Emergency laparotomy carries a significant mortality and this has been shown to increase with age.8,24 Below are listed some important emergency presenting complaints in elderly patients and points to consider in their assessment and management.
Mesenteric ischemia
Acute mesenteric ischemia, whether secondary to embolus, thrombosis, or low flow states, typically presents in later life and is an increasingly common diagnosis.25 Comorbidities such as atrial fibrillation, ischemic heart disease, and atherosclerosis are diseases common in old age. These risk factors contribute to the development of mesenteric ischemia and their existence should prompt the clinician to consider the diagnosis in patients presenting unwell with abdominal pain, especially when the pain is out of proportion to clinical signs and a high white cell count is present. Preceding mesenteric angina symptoms may be described by the patient or family and weight loss with fear of eating may also precede an acute presentation if the cause is arterial thrombosis. Features of intestinal necrosis (acidosis, hypotension, and high lactate) appear late and may not be salvageable. Early arterial and venous phase computed tomography (CT) is required for accurate diagnosis.25
Treatment with major abdominal surgery, bowel resection, and/or vascular reconstruction is often required for successful outcome. However, interventional radiology with or without anticoagulation can also be considered a less-invasive option in patients in whom surgery would involve high risk, but this is only successful when the condition is identified early prior to intestinal infarction.
Diverticulitis
The incidence of diverticular disease increases with age. It is relatively uncommon before the age of 40 and is seen in up to 60% of patients in their 80s. The Royal College of Surgeons of England has suggested that all patients presenting with symptoms of acute diverticulitis should undergo CT assessment of the abdomen. Mortality remains high in patients presenting acutely, and a high index of suspicion and early diagnosis are paramount in reducing mortality. Morbidity is also high, with older patients experiencing more adverse events and complications postsurgery.
Appendicitis
Appendicitis is common at all ages, with patients older than 60 years of age accounting for 10% of cases but 50% of mortality. Delay in presentation and diagnosis can be due to atypical clinical features such as pain not localizing to the right lower quadrant, lack of tenderness, and lack of fever or leukocytosis. The outcome of elderly patients undergoing appendectomy is worse, mainly due to delayed diagnosis and time to surgery and the higher rates of complex appendicitis.26 Obstruction of the appendiceal lumen by a cecal tumor should be considered in all elderly patients presenting with suspected appendicitis and where diagnostic uncertainty exists, CT scanning can be a useful tool.27
Bowel obstruction
Elderly patients presenting with symptoms of bowel obstruction may be misdiagnosed with other conditions causing vomiting, particularly in the absence of a reliable history. A detailed history to include previous surgical operations and red flag symptoms (anemia, change in bowel habit, etc) for colorectal cancer, as well as deliberate and thorough examination for groin and abdominal hernia, should be performed in all cases. Small bowel obstruction due to a missed femoral hernia can be overlooked in the elderly female if not specifically looked for clinically. Attributing a first presentation of bowel obstruction to adhesions alone in the elderly without adequate cross-sectional imaging with CT is not advised, as other pathologies (such as cancers) are more likely in the elderly.
Sigmoid volvulus is common in elderly, immobile patients and should be considered in painless, gross abdominal distension. There may or may not be a previous history of volvulus. Risk factors include chronic constipation, institutionalization, and antipsychotic and other constipating medication. It should be noted that previous episodes of obstruction may have been attributed to sigmoid volvulus but up to date investigation may be necessary to exclude an underlying malignancy. Immediate treatment with colonic decompression (rigid sigmoidoscopy and flatus tube or flexible endoscopic decompression) is necessary to prevent gangrenous infarction of the colon.
Biliary disease
Cholelithiasis is common in elderly patients, with gallstones present in up to 50% of patients older than 65 years of age. In the acute presentation of cholecystitis, eg, up to 25% of elderly patients may have no significant pain, and less than one half have fever, vomiting, or leukocytosis. In terms of investigation, cholecystitis is acalculous in approximately 10% of elderly patients. The mortality rate of elderly patients diagnosed with cholecystitis is approximately 10%. The diagnosis therefore can be difficult in this age group, requiring a high index of suspicion and early resort to abdominal ultrasound examination.
Delayed diagnosis can lead to complications including gallbladder perforation, empyema, and severe sepsis. While cholecystectomy within 48 hours of admission is the ideal treatment, many very elderly patients are not fit for this. The role of interventional radiology should not be underestimated here; percutaneous radiologically guided drainage of the gallbladder in the cases of empyema or advanced cholecystitis can often negate the need for difficult surgery.28 Where definitive treatment with cholecystectomy may be inappropriate, treatment with endoscopic retrograde cholangiopancreatography and sphincterotomy has been shown to be a safe and effective alternative in elderly patients with gallstone pancreatitis or common bile duct stones.29
Emergency presentation of colorectal cancer
The risk of developing some cancers increases with age; the reasons for this are multifactorial but can be due to environmental exposure to risk factors and tumor biology. Emergency presentation can result in increased stress and anxiety for patients and families, the need for emergency surgical management, and poorer outcomes in terms of survival.30
Approximately 20% of colorectal cancer cases present as an emergency often necessitating emergency treatment.31 A systematic review of literature from the year 2000 of the management of colorectal cancer in elderly patients found increased emergency presentation, more advanced disease stage at presentation, and increased morbidity and mortality with increasing age.31 The recent National Bowel Cancer Audit Project’s national audit from 2013 has demonstrated that things are not much better with elderly patients still presenting late, with advanced disease or in a state deemed too frail to undergo major surgery.32 Of note, comorbidity was a weak discriminator of the patients who were offered surgery, suggesting age alone may be the driver in surgical decision-making processes. In addition, those elderly patients who do undergo major colorectal surgery are at higher risk of permanent stoma at 18 months’ follow-up compared to their younger counterparts.32 The patient may not have the cognitive or visual ability or manual dexterity to cope with a stoma, which may be the factor precipitating loss of independence and the move to a care home.
Other cancers presenting as emergencies
The increasing trend for emergency presentation is not confined to colorectal cancers. Abel et al30 recently published data from the National Cancer Data Repository in England. They showed that for many cancers, emergency presentation was more common with increasing age. The authors suggest lack of awareness by patients and clinicians as well as comorbidity as the possible contributing factors in this variation. Cancer outcomes are also poorer in the elderly population, with more advanced cancers requiring more aggressive treatment, which elderly patients may be unable to tolerate.
Vascular emergencies
Ruptured abdominal aortic aneurysm
Abdominal aortic aneurysm (AAA) rupture occurs predominantly in patients in their seventh and eighth decades of life. Overall mortality is 75%, with age being a strong independent risk factor for mortality. Approximately 10%–25% of patients presenting with a ruptured AAA are managed expectantly, with 75% of this cohort being >80 years old. In appropriately equipped centers, a large proportion of AAAs can now be managed without recourse to major open abdominal surgery. Increasingly, elderly patients are being treated by endovascular aortic aneurysm repair (EVAR). Although this avoids major open surgery, specific complications from the EVAR technique exist. For example, the use of large volumes of nephrotoxic contrast mediums required to perform the procedure can affect preexisting renal disease. The IMPROVE trial33 was a prospective cohort study that assessed patients who were thought to have ruptured AAA and treated with either open repair or EVAR. Interesting findings of the study were that 1) 10% of patients thought to have a ruptured AAA were found to have another diagnosis on emergency CT imaging; 2) a systolic BP of <70 mmHg was an independent predictor of mortality; and 3) local anesthetic-aided EVAR was protective against mortality, compared with that done under general anesthesia.
A recent single-center retrospective review of the management of ruptured AAA in the Netherlands has demonstrated in selected patients similar postoperative mortality rates following both open and endovascular repair.34 Older patients (defined here as aged >70 years) had more postoperative complications than their younger counterparts. The authors highlight the importance of careful preoperative assessment of patients and realistic expectation. They list their thought process with old age and comorbidity being the main factors contributing to nonoperative approach although stressing that age alone should not influence selection for intervention. In addition, they also make use of risk prediction scoring systems and medical expertise to aid this decision-making process.
Stroke
Stroke pathways have developed following the publication of the Department of Health’s National Stroke Strategy in 2007.35 The NICE guidelines recommend early access to multidisciplinary specialist stroke teams to improve outcome. In the 20% of patients in whom stroke is a result of carotid artery stenosis, it is recommended that patients receive surgical intervention (carotid endarterectomy) within 1 week.36 Carotid endarterectomy in elderly patients is not without risk and a recent study has demonstrated up to a 2.5-fold increase in mortality and adverse events such as stroke and myocardial infarction in frail patients undergoing carotid revascularization.37 Frailty in this study was assessed using a frailty screening tool and highlights the increased risk associated with this subgroup of patients.
Ischemic limbs
Atherosclerosis and atrial fibrillation are common in the elderly. These common predisposing factors should help the clinician identify the likely cause of acute limb ischemia and prompt appropriate treatment. As with the acute abdomen, communication difficulties and atypical presentations can conspire to prevent the timely presentation and diagnosis of limb ischemia in elderly patients. Missed diagnosis in acute limb ischemia often results in an unsalvageable limb, amputation, and death.
In a study conducted in 1998,38 the in-hospital mortality of elderly patients from acute limb ischemia approached 40%, with an amputation rate of 5%. More recent evidence has shown that outcomes have not improved for elderly patients, with mortality still ~25% and amputation rates of up to 12%.39,40 In a recent study by Saarinen et al41 of revascularization of acute and chronic limb ischemia in patients aged >90 years, the authors demonstrated similar rates of mortality and limb salvage. In addition, the authors included patient-centered outcomes alongside standard surgical outcomes. They report functional outcomes such as independent living and ambulation and demonstrate good results in patients at discharge, although this was tempered by poor 1-year survival in this extremely elderly group. Lower limb revascularization by interventional radiology/endovascular means has been shown to be as effective as surgery and provides a less-invasive option for patients.
Possible solutions to reduce morbidity and mortality associated with emergency surgical care of the elderly
The following is a framework to help clinicians treat elderly patients presenting as an emergency who by definition are at high risk (predicted mortality: >10%). The suggested order of the framework is to guide the inexperienced emergency room physician in assessing and treating elderly patients with acute surgical pathology.
Appropriate and timely resuscitation
Prompt diagnosis
Realistic risk prediction and identification of frailty
Taking account of the patients’ wishes and the avoidance of futile surgery
Consideration of nonsurgical treatments
Timely surgical intervention that is consultant delivered
Fully supported, expert perioperative and operative care
Careful postoperative management and avoiding “failure to rescue”
Comprehensive geriatric assessment (CGA)
Management of comorbidities and polypharmacy
Trainee and surgeon education
Future research and audit.
Appropriate and timely resuscitation
Supportive care with timely intravenous (IV) fluids, correction of electrolyte disturbances, IV antibiotics if sepsis is diagnosed, and appropriate analgesia and monitoring should begin on admission to hospital. Guidelines suggest that patients with high early warning scores should be seen immediately by senior surgical and anesthetic/critical care staff.17
Prompt diagnosis (eg, liberal CT imaging)
Table 3 lists some commonly missed diagnoses in elderly patients and tips for avoiding these. A high index of suspicion is important when assessing elderly patients and will help reduce missed diagnoses and delays in treatment. As identified in the National Confidential Inquiry into Patient Outcome and Death report of 2010, delay in diagnosis and subsequent treatment was found to significantly contribute to poor outcome in elderly patients. Being aware that elderly patients present with atypical features compared with younger patients can help focus radiological investigation appropriately.42,43 Early CT imaging significantly improves management of elderly patients with acute abdomen, and its liberal use is recommended.44
Table 3.
Common pitfalls and missed diagnoses in the elderly
| Condition | Index of suspicion | Tips |
|---|---|---|
| Ruptured AAA | May be confused for cardiac event (collapse, hypotension), renal colic (first presentation with renal calculi is uncommon in patients >60 years of age); pulsatile mass may be difficult to feel in the hypotensive or obese patient | Back pain ± collapse + hypotension should prompt FAST or CT scan to assess abdominal aorta |
| Acute groin hernia | 70% Patients >70 years old, increasing age means increasing risk of obstruction and strangulation | Careful and thorough examination of femoral and inguinal canals must be performed |
| Ischemic bowel | Nonspecific features, sudden onset abdominal pain out of proportion to clinical signs; patients have a soft abdomen in the early stages of the disease | Raised lactate and acidosis levels are late features Low threshold for CT imaging White cell count is typically high Peritonism and rigidity usually indicate infarcted intestine |
| Appendicitis | Still common in elderly patients but not as common as in young patients | Consider cecal malignancy or diverticulitis as cause and consider CT to exclude |
| Gastric volvulus | Nonbilious vomiting; more common in the elderly; associated with chest pain and retching; patient may have a history of a hiatus hernia or signs of a hiatus hernia on plain chest X-ray; often misdiagnosed as a upper GI bleed with “coffee ground” type vomiting | Chest X-ray reveals a hiatus hernia with a distended stomach, typically visible in the chest and the upper abdomen |
| Ischemic lower limb | Common cause for “off-legs”, consider in AF/cancer patients | Always examine unwell patients’ feet |
| Hip fracture | Easily missed, particularly if bedbound; the severity of the fall can be fairly minor; contractures may make external rotation difficult to assess | Maintain a high index of suspicion and consider routine hip X-ray after fall in high-risk patients |
Abbreviations: AAA, abdominal aortic aneurysm; AF, atrial fibrillation; CT, computed tomography; FAST, Focused Assessment with Sonography in Trauma; GI, gastrointestinal.
Realistic risk prediction and identification of frailty
The report of the Royal College of Surgeons of England on the “Higher Risk General Surgical Patient” includes discussion on the use of risk assessment in emergency surgery.17 There are many risk prediction models available to the emergency clinician, eg, ASA, P-POSSUM, and APACHE-2 (http://riskprediction.org.uk/). None of these risk scores make any adjustment for frailty. Some are more complicated and time-consuming than others and whilst more accurate, a balance is required between accuracy of prediction and real-world applicability. Although age-specific risk prediction models do exist, they are often cumbersome requiring multiple inputs, making them of limited practical utility in the emergency situation. However, it is encouraging to see that attempts to accurately assess the risks in the elderly are being made. The American College of Surgeons has developed a comprehensive online morbidity and mortality calculator for use in emergency and elective surgery (http://riskcalculator.facs.org). This was developed using data from >1.4 million operations in American hospitals between 2009 and 2012 and is a very powerful tool to help with informed consent and individual surgical risk.
Accurate preoperative risk assessment is not only crucial in informed consent for operative surgery but also provides valuable information for clinicians (eg, clinical audit and morbidity and mortality meetings), patients, and relatives. It can be used to predict likelihood of adverse events and allows steps to be taken to reduce the effects of these on a patient (eg, to guide level of care postoperatively). Realistic and frank discussion of the risk of dying during or after an intervention may also allow sensible, respectful, and dignified decisions about end-of-life care.
Underpinning this strategy, it is important to acknowledge that there is a need for a real shift in thinking when a team is assessing and managing older persons, specifically if they have frailty. The recent document “Safe compassionate care for frail older people using an integrated care pathway” states “frail people should not be perceived as a problem to the system, but rather, clinicians should support people living with frailty”.45
Teams, such as the Proactive care of Older People undergoing Surgery (“POPS” team) at Guys and St Thomas’ Hospital, use an emergency surgical admission proforma that specifically questions if a patient has frailty.46 This may be identified by “phenotype” or may be indicated by the presentation itself with a frailty syndrome (previously known as the geriatric giants), eg, a patient presenting with falls. Alternatively, there are screening tools for frailty, but many are designed for use in the community or elective setting (eg, Edmonton Frailty Scale) rather than the emergency setting.47
Taking account of the patients’ wishes and the avoidance of futile surgery
Not all patients with conditions amenable to operative management should be taken to theater. Futile surgery must be avoided and this requires robust risk assessment and discussion with the patient, family, carers, and patient advocates. Some older patients admitted with life-threatening pathology will be aware that they are approaching death and would rather have the focus shifted to palliative measures rather than heroic and unrealistic surgery.
Deciding not to operate can be a difficult task and is certainly not the easy option. With patient and family emotions running high, deciding against surgery can often be viewed as “giving up”. Pressure from patients, family, and other health care professionals can influence decision making wherein chances of treatment success is low. In our litigious age, ensuring that patients, families, and carers are fully involved in decision-making processes is essential. Multidisciplinary discussion with or without a formal second opinion may be required in particularly difficult cases.
It is important to remember, as specifically highlighted in the recent Association of Anaesthetists of Great Britain and Ireland (AAGBI) guidelines for the perioperative care of the elderly,48 that all elderly patients should be assumed to have capacity to make decisions regarding their health and treatment. Respecting patient wishes when expressed at the time of presentation or in the form of an advanced decision to refuse treatment must be at the forefront of the emergency clinician’s mind when deciding on a course of treatment. In addition, prior advanced care planning should avoid unnecessary, psychologically distressing, and costly emergency admission and investigations when the wishes of the patient are already known. However, this requires coordination of care with the family, general practitioner, and social service team and access to high-quality and accessible community teams to provide family support and palliative services.
Consideration of nonsurgical treatments
Table 4 outlines a number of new technologies that are available to treat conditions that have previously been treated surgically. While a full discussion of the pros and cons of each treatment method is beyond the scope of this article, they are included to highlight that they are available and their use can be considered in patients who are deemed unfit for emergency open surgery.49,50 It may be necessary to transfer patients to larger better-equipped hospitals to take advantage of these new techniques, and local referral pathways should be developed to allow this to occur.
Table 4.
Potential nonsurgical treatments for various acute abdominal conditions
| Diagnosis | Nonsurgical treatment option |
|---|---|
| Diverticular or appendix abscess | Radiological drainage for abscess or collection formation |
| Nongangrenous mesenteric ischemia | Anticoagulation Interventional radiology (clot thrombolysis or retrieval, arterial dilatation, and stenting) |
| Obstructing colorectal cancer | Endoluminal stenting |
| Severe cholecystitis or gallbladder empyema | Radiological drainage, “cholecystostomy”, gallbladder drainage |
| Ruptured abdominal aortic aneurysm | Endovascular aortic aneurysm repair |
| Major upper gastrointestinal hemorrhage, eg, bleeding duodenal ulcer | Endoscopic hemostasis (adrenaline, clips, spray etc) Selective interventional radiological embolization of the bleeding vessel |
| Gastric volvulus/incarcerated hiatus hernia | Endoscopic decompression and guided nasogastric decompression Percutaneous endoscopic gastrostomy as fixation to prevent recurrence |
| Sigmoid volvulus | Rigid or flexible endoscopic decompression Percutaneous endoscopic colostomy as fixation to prevent recurrence |
Timely surgical intervention that is consultant delivered
One of the key recommendations from the several guidelines and reports is early access to theater when required. If definitive intervention is not undertaken in a timely manner, then this can result in deterioration, development of adverse events, and poor outcome.1,17 In the most severe cases, delays in delivering definitive treatment have contributed to death in many cases.1
Studies have demonstrated that elderly patients are more likely to experience a delay in access to theater than younger patients, with most waiting >24 hours for surgery in some studies.51 Although the time before theater can be used for investigation and optimization, there is clearly a limit to the amount of time elderly patients can wait before their risk of adverse events outweighs the benefit of optimization.48 Although there are limited data available on the reason for delay to theater, unnecessary delays due to organizational reasons or error must be limited.
Fully supported, expert perioperative and operative care
Several reports highlight the lack of consultant involvement in emergency care in elderly patients resulting in increased complication rates and mortality.1,8,10,16,17 Operative inter vention in high-risk elderly patients should be delivered by the consultant surgeon, with anesthesia being provided at a similar consultant grade.
Careful postoperative management and avoiding “failure to rescue”
The AAGBI describes in detail what is expected of postoperative care in the elderly.48 Ongoing postoperative monitoring and support in a high-dependency or critical care environment is ideal for high-risk elderly patients.
The concept of “failure to rescue” arises when a potentially treatable or avoidable postoperative complication results in a patient’s death and may be due to a variety of factors.52 It appears to be more common in elderly patients and can be due to either lack of recognition of the complication or a failure to treat a known complication in a timely and appropriate manner. It is also important to appreciate that postoperative complications can manifest differently in elderly patients; eg, delirium or confusion can be the presenting features of an anastomotic leak.
Delirium or acute confusional state is common in the elderly (as high as 50% in patients undergoing emergency surgery53). It is associated with increased adverse events, including falls and in-hospital death. NICE has recently published guidelines on identifying and preventing in-hospital delirium, which the reader is referred to.53
In a population-based review of survival following adverse events in elderly patients, it was noted that cardiac events were more often adequately rescued than respiratory or infective events.52 The authors postulate that this may be due to increased awareness of risks and better diagnostic pathways in managing cardiac conditions compared to others. While “failure to rescue” is a useful concept and an important quality improvement tool, it is important to realize that not all patients who die postoperatively succumb to potentially remediable complications.
Comprehensive geriatric assessment
The early multidisciplinary management of elderly patients can influence outcome. In 2011, Ellis et al54 published a Cochrane review of the use of CGA in elderly patients admitted to hospital. The review compared 22 randomized trials comparing CGA to usual care and identified significant reduction in dependence and mortality at 1 year in patients receiving CGA.54
Despite good evidence in acute medical patients, the surgical community has been slow to adopt this collaborative model of care in elderly patients. In the elective surgery setting, Harari et al46 have pioneered work examining the role and effectiveness of multidisciplinary geriatric involvement in the care of elderly patients undergoing elective surgery. They advocate the use of a proactive multidisciplinary review of surgical patients and have shown impressive improvements in morbidity and mortality. A recent systematic review examining the use of preoperative CGA in surgical patients identified five studies showing encouraging results on postoperative outcomes in elderly patients.19
The role of CGA in postoperative care of surgical patients still needs further evidence. The most compelling current evidence comes from the orthopedic community, which has embraced the idea of multidisciplinary team (MDT) care and orthogeriatricians. There is evidence that involvement of an orthogeriatrician can lead to reduced length of stays, reduced mortality, better teamwork, and improved discharge planning.16,18
In a recent survey of geriatric centers across the UK, it was identified that <30% of centers provided geriatric medicine input to the care of older surgical patients.55 In emergency surgery, the majority of centers provided care postoperatively, with half of centers responding to referral and half actively seeking cases. Despite mounting evidence to show that multidisciplinary CGA and subsequent optimization improves outcomes in elderly patients, the authors found that funding was the main barrier to delivery of this service.19
Return to function should be regarded as a key outcome for elderly patients. With life expectancy of an additional 20–30 years for an average 65-year-old person, the cost of increased dependency can be massive. Efforts can be made to reduce functional decline at all points in a patient pathway, especially by the use of a MDT of physiotherapists, dieticians, and occupational therapists. Early rehabilitation starting in hospitals with dedicated rehabilitation centers has been shown to improve independent living. This requires engagement by the emergency surgical community and can be facilitated by geriatricians, many of whom are already working within these MDTs and have a working knowledge of rehabilitation pathways and methods.
Management of comorbidities and polypharmacy
An extensive discussion on specific comorbidity management is beyond the scope of this review. However, timely and efficient management of patient comorbidities is essential to improve outcome. The Royal College of Anaesthetists report includes recommendations on the management of several key comorbidities and highlights ways of reducing risk or anticipating it.48
Comorbidity and frailty often coexist with polypharmacy. Polypharmacy is defined as the use of multiple medicines by one individual and has been defined in patients taking as few as four or more medications. Polypharmacy is estimated to cost the USA $50 billion per annum and has been implicated in poor outcome and adverse events.56–58 Polypharmacy itself has been used as a surrogate for frailty, with the prescription of more than five medications being shown to correlate to frailty in elderly patients and result in poorer outcomes.47
An in-depth discussion of polypharmacy management is beyond the scope of this review. However, the reader is directed to publications by NICE and the King’s Fund,56,58 which have reviewed this topic and outline several strategies to improve practice with specific reference to elderly patients.
Trainee and surgeon education
The majority of surgeons lack any formal training in geriatric medicine. One study has shown that a formal teaching program in geriatrics for general surgical trainees is effective in developing skills at recognizing geriatric issues, such as delirium and acute renal impairment in the elderly.59 Equally, increasing the knowledge and skills of geriatric medicine trainees in understanding more about surgical and nonsurgical management of patients and working with surgeons through the pathway is vital and this has been acknowledged with the addition of “perioperative medicine for older people” to the UK’s Geriatric Specialty training curriculum.
Future research and audit
The compulsory Healthcare Quality Improvement Partnership (HQIP) National Emergency Laparotomy Audit (NELA; http://www.nela.org.uk) is under way in the UK and will publish risk-adjusted outcomes for patients across National Health Service (NHS) hospitals in England and Wales. It aims to help with quality improvement, identifying hospitals with the lowest mortality and using them as exemplars of best practice. Auditable standards in risk assessment, preoperative care, intraoperative management, end-of-surgery care bundles, and MDT care have been defined. The first full NELA report is eagerly awaited and will be a practice-changing step. Early presented results suggest that only 10% of laparotomy patients >70 years of age are assessed by geriatricians. There is an overall 11.3% mortality in the first 30 days, and patients with the highest risk are being operated on at night with the least consultant input.
Randomized clinical trials focusing on elderly surgical patients are rare. Trials and research into the very elderly are even rarer. Important research questions to be answered in the future include the following:
Assess different models of preoperative optimization prior to emergency surgery in the elderly
Define the most accurate risk prediction tool to use in elderly patients requiring emergency surgery
Define the optimum model of care for geriatric surgical patients undergoing emergency surgery
Develop cost-effectiveness models of different approaches (surgical vs nonsurgical, for instance) in elderly patients with emergency surgical pathology.
Conclusion
Emergency surgical presentations in the elderly are increasing rapidly and present many significant challenges. Although, for many years, evidence has shown that elderly patients have poorer outcomes, there are specific strategies that hospitals and teams can develop to improve the care received by this vulnerable group. Clinicians need awareness of factors contributing to poor outcome in elderly patients and tools to aid accurate and timely identification and correction of some of these factors to drive up standards. Surgeons cannot achieve this change alone and this paradigm shift should be driven by expert MDTs. which should include emergency physicians, geriatricians, anesthetists, critical care specialists, specialist nurses, therapists, and dieticians. New research and audit evidence will allow this change in practice to be truly evidence based.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Wilkinson K, Martin I, Gough M, et al. An age old problem: A review of the care received by elderly patients undergoing surgery. London: NCE-POD; 2010. [Accessed August 13, 2015]. Available from: http://www.ncepod.org.uk/2010report3/downloads/EESE_fullReport.pdf. [Google Scholar]
- 2.Department of Health UK . The National Service Framework for Older People. London: Department of Health UK; 2001. [Google Scholar]
- 3.Søreide K, Desserud KF. Emergency surgery in the elderly: the balance between function, frailty, fatality and futility. Scand J Trauma Resusc Emerg Med. 2015;23(1):10. doi: 10.1186/s13049-015-0099-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bayliss J, Sly F. Ageing across the UK. London: Office for National Statistics; 2010. [Google Scholar]
- 5.Ageing well: a global priority. Lancet. 2012;379(9823):1274. doi: 10.1016/S0140-6736(12)60518-2. [DOI] [PubMed] [Google Scholar]
- 6.Wittenberg R, Sharpin L, McCormick B, Hurst J. Understanding Emergency Hospital Admissions of Older People. Oxford: CHSEO; 2014. [Google Scholar]
- 7.McVeigh TP, Al-Azawi D, O’Donoghue GT, Kerin MJ. Assessing the impact of an ageing population on complication rates and in-patient length of stay. Int J Surg. 2013;11(9):872–875. doi: 10.1016/j.ijsu.2013.07.016. [DOI] [PubMed] [Google Scholar]
- 8.Saunders DI, Murray D, Pichel AC, Varley S, Peden CJ. Variations in mortality after emergency laparotomy: the first report of the UK Emergency Laparotomy Network. Br J Anaesth. 2012;109(3):368–375. doi: 10.1093/bja/aes165. [DOI] [PubMed] [Google Scholar]
- 9.Lawrence VA, Hazuda HP, Cornell JE, et al. Functional independence after major abdominal surgery in the elderly. J Am Coll Surg. 2004;199(5):762–772. doi: 10.1016/j.jamcollsurg.2004.05.280. [DOI] [PubMed] [Google Scholar]
- 10.Callum K, Gray A, Hoile R, et al. Extremes of age. The 1999 report of the National Confidential Enquiry into Perioperative Deaths. London: NCEPOD; 1999. [Accessed August 13, 2015]. Available from: http://www.ncepod.org.uk/pdf/1999/99full.pdf. [Google Scholar]
- 11.RCSEng, Age UK, MHP Health Mandate Access All Ages: Assessing the Impact of Age on Access to Surgical Treatment. 2012. Available from: https://www.rcseng.ac.uk/publications/docs/access-all-ages.
- 12.Campbell AJ, Buchner DM. Unstable disability and the fluctuations of frailty. Age Ageing. 1997;26(4):315–318. doi: 10.1093/ageing/26.4.315. [DOI] [PubMed] [Google Scholar]
- 13.Fried LP, Tangen CM, Walston J, et al. Cardiovascular Health Study Collaborative Research Group Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56(3):M146–M156. doi: 10.1093/gerona/56.3.m146. [DOI] [PubMed] [Google Scholar]
- 14.Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K. Frailty in elderly people. Lancet. 2013;381(9868):752–762. doi: 10.1016/S0140-6736(12)62167-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rosentha R, Zenilman M, Katlic M. Principles and Practice of Geriatric Surgery. Berlin: Springer Science and Business Media; 2011. [Google Scholar]
- 16.NICE Hip Fracture: The Management of Hip Fracture in Adults. 2011. Available from: https://www.nice.org.uk/guidance/cg124.
- 17.Anderson I, Eddleston J, Grocott M, et al. The Higher Risk General Surgical Patient Towards Improved Care for a Forgotten Group. London: RCS; 2011. [Google Scholar]
- 18.Grigoryan KV, Javedan H, Rudolph JL. Orthogeriatric care models and outcomes in hip fracture patients: a systematic review and meta-analysis. J Orthop Trauma. 2014;28(3):e49–e55. doi: 10.1097/BOT.0b013e3182a5a045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Partridge JSL, Harari D, Martin FC, Dhesi JK. The impact of preoperative comprehensive geriatric assessment on postoperative outcomes in older patients undergoing scheduled surgery: a systematic review. Anaesthesia. 2014;69(Suppl 1):8–16. doi: 10.1111/anae.12494. [DOI] [PubMed] [Google Scholar]
- 20.Yelon J, Luchette F. Geriatric Trauma and Critical Care. Berlin: Springer Science and Business Media; 2013. [Google Scholar]
- 21.Pandit V, Rhee P, Hashmi A, et al. Shock index predicts mortality in geriatric trauma patients: an analysis of the National Trauma Data Bank. J Trauma Acute Care Surg. 2014;76(4):1111–1115. doi: 10.1097/TA.0000000000000160. [DOI] [PubMed] [Google Scholar]
- 22.Heffernan DS, Thakkar RK, Monaghan SF, et al. Normal presenting vital signs are unreliable in geriatric blunt trauma victims. J Trauma. 2010;69(4):813–820. doi: 10.1097/TA.0b013e3181f41af8. [DOI] [PubMed] [Google Scholar]
- 23.Demetriades D, Sava J, Alo K, et al. Old age as a criterion for trauma team activation. J Trauma. 2001;51(4):754–756. doi: 10.1097/00005373-200110000-00022. [DOI] [PubMed] [Google Scholar]
- 24.Symons NR, Moorthy K, Almoudaris AM, et al. Mortality in high-risk emergency general surgical admissions. Br J Surg. 2013;100(10):1318–1325. doi: 10.1002/bjs.9208. [DOI] [PubMed] [Google Scholar]
- 25.Kärkkäinen JM, Lehtimäki TT, Manninen H, Paajanen H. Acute mesenteric ischemia is a more common cause than expected of acute abdomen in the Elderly. J Gastrointest Surg. 2015;19(8):1407–1414. doi: 10.1007/s11605-015-2830-3. [DOI] [PubMed] [Google Scholar]
- 26.Segev L, Keidar A, Schrier I, Rayman S, Wasserberg N, Sadot E. Acute appendicitis in the elderly in the twenty-first century. J Gastrointest Surg. 2015;19(4):730–735. doi: 10.1007/s11605-014-2716-9. [DOI] [PubMed] [Google Scholar]
- 27.Lee JF, Leow CK, Lau WY. Appendicitis in the elderly. Aust N Z J Surg. 2000;70(8):593–596. doi: 10.1046/j.1440-1622.2000.01905.x. [DOI] [PubMed] [Google Scholar]
- 28.Flexer SM, Peter MB, Durham-Hall AC, Ausobsky JR. Patient outcomes after treatment with percutaneous cholecystostomy for biliary sepsis. Ann R Coll Surg Engl. 2014;96(3):229–233. doi: 10.1308/003588414X13814021679799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lukens FJ, Howell DA, Upender S, Sheth SG, Jafri S-MR. ERCP in the very elderly: outcomes among patients older than eighty. Dig Dis Sci. 2010;55(3):847–851. doi: 10.1007/s10620-009-0784-6. [DOI] [PubMed] [Google Scholar]
- 30.Abel GA, Shelton J, Johnson S, Elliss-Brookes L, Lyratzopoulos G. Cancer-specific variation in emergency presentation by sex, age and deprivation across 27 common and rarer cancers. Br J Cancer. 2015;112(Suppl):S129–S136. doi: 10.1038/bjc.2015.52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Surgery for colorectal cancer in elderly patients: a systematic review. Colorectal Cancer Collaborative Group. Lancet. 2000;356(9234):968–974. [PubMed] [Google Scholar]
- 32.Health and Social Care Information Centre . National Bowel Cancer Audit Annual Report 2013. Leeds: hscic; 2013. [Accessed August 13, 2015]. Available from: http://www.hscic.gov.uk/catalogue/PUB11105/nati-clin-audi-supp-prog-bowe-canc-2013-rep1.pdf. [Google Scholar]
- 33.IMPROVE Trial Investigators. Powell JT, Hinchliffe RJ, et al. Observations from the IMPROVE trial concerning the clinical care of patients with ruptured abdominal aortic aneurysm. Br J Surg. 2014;101(3):216–224. doi: 10.1002/bjs.9410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Raats JW, Flu HC, Ho GH, et al. Long-term outcome of ruptured abdominal aortic aneurysm: impact of treatment and age. Clin Interv Aging. 2014;9:1721–1732. doi: 10.2147/CIA.S64718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Department of Health UK . National Stroke Strategy. London: Department of Health UK; 2007. [Google Scholar]
- 36.Royal College of Physicians . National Clinical Guideline for Stroke. London: Royal College of Physicians; 2012. [Google Scholar]
- 37.Melin AA, Schmid KK, Lynch TG, et al. Preoperative frailty Risk Analysis Index to stratify patients undergoing carotid endarterectomy. J Vasc Surg. 2015;61(3):683–689. doi: 10.1016/j.jvs.2014.10.009. [DOI] [PubMed] [Google Scholar]
- 38.Braithwaite BD, Davies B, Birch PA, Heather BP, Earnshaw JJ. Management of acute leg ischaemia in the elderly. Br J Surg. 1998;85(2):217–220. doi: 10.1046/j.1365-2168.1998.00577.x. [DOI] [PubMed] [Google Scholar]
- 39.De Leur K, van Zeeland MLP, Ho GH, de Groot HGW, Veen EJ, van der Laan L. Treatment for critical lower limb ischemia in elderly patients. World J Surg. 2012;36(12):2937–2943. doi: 10.1007/s00268-012-1758-y. [DOI] [PubMed] [Google Scholar]
- 40.Martini R, Andreozzi GM, Deri A, et al. Amputation rate and mortality in elderly patients with critical limb ischemia not suitable for revascularization. Aging Clin Exp Res. 2012;24(3 suppl):24–27. [PubMed] [Google Scholar]
- 41.Saarinen E, Vuorisalo S, Kauhanen P, Albäck A, Venermo M. The benefit of revascularization in nonagenarians with lower limb ischemia is limited by high mortality. Eur J Vasc Endovasc Surg. 2015;49(4):420–425. doi: 10.1016/j.ejvs.2014.12.027. [DOI] [PubMed] [Google Scholar]
- 42.Laurell H, Hansson L-E, Gunnarsson U. Acute abdominal pain among elderly patients. Gerontology. 2006;52(6):339–344. doi: 10.1159/000094982. [DOI] [PubMed] [Google Scholar]
- 43.Lewis LM, Banet GA, Blanda M, Hustey FM, Meldon SW, Gerson LW. Etiology and clinical course of abdominal pain in senior patients: a prospective, multicenter study. J Gerontol A Biol Sci Med Sci. 2005;60(8):1071–1076. doi: 10.1093/gerona/60.8.1071. [DOI] [PubMed] [Google Scholar]
- 44.Esses D, Birnbaum A, Bijur P, Shah S, Gleyzer A, Gallagher EJ. Ability of CT to alter decision making in elderly patients with acute abdominal pain. Am J Emerg Med. 2004;22(4):270–272. doi: 10.1016/j.ajem.2004.04.004. [DOI] [PubMed] [Google Scholar]
- 45.NHS England. Safe, Compassionate Care for Frail Older People Using an Integrated Care Pathway. Redditch: NHS England; 2014. [Google Scholar]
- 46.Harari D, Hopper A, Dhesi J, Babic-Illman G, Lockwood L, Martin F. Proactive care of older people undergoing surgery (’POPS’): designing, embedding, evaluating and funding a comprehensive geriatric assessment service for older elective surgical patients. Age Ageing. 2007;36(2):190–196. doi: 10.1093/ageing/afl163. [DOI] [PubMed] [Google Scholar]
- 47.British Geriatrics Society Fit for Frailty: Consensus Best Practice Guidance for the Care of Older People Living with Frailty in Community and Outpatient Settings. 2014. Available from: http://www.bgs.org.uk/campaigns/fff/fff_full.pdf.
- 48.Griffiths R, Beech F, Brown A, et al. Association of Anesthetists of Great Britain and Ireland Peri-operative care of the elderly. Anaesthesia. 2014;69(Suppl 1):81–98. doi: 10.1111/anae.12524. [DOI] [PubMed] [Google Scholar]
- 49.Beggs AD, Dilworth MP, Powell SL, Atherton H, Griffiths EA. A systematic review of transarterial embolization versus emergency surgery in treatment of major nonvariceal upper gastrointestinal bleeding. Clin Exp Gastroenterol. 2014;7:93–104. doi: 10.2147/CEG.S56725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Griffiths EA, McDonald CR, Bryant RV, et al. Retrospective analysis of surgery and trans-arterial embolization for major non-variceal upper gastrointestinal bleeding. ANZ J Surg. 2014 Apr 3; doi: 10.1111/ans.12588. Epub. [DOI] [PubMed] [Google Scholar]
- 51.O’Leary DP, Beecher S, McLaughlin R. Emergency surgery preoperative delays – realities and economic impacts. Int J Surg. 2014;12(12):1333–1336. doi: 10.1016/j.ijsu.2014.10.002. [DOI] [PubMed] [Google Scholar]
- 52.Sheetz KH, Krell RW, Englesbe MJ, Birkmeyer JD, Campbell DA, Ghaferi AA. The importance of the first complication: understanding failure to rescue after emergent surgery in the elderly. J Am Coll Surg. 2014;219(3):365–370. doi: 10.1016/j.jamcollsurg.2014.02.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.NICE Delirium: Diagnosis, Prevention and Management. 2010. Available from: https://www.nice.org.uk/guidance/cg103. [PubMed]
- 54.Ellis G, Whitehead MA, O’Neill D, Langhorne P, Robinson D. Comprehensive geriatric assessment for older adults admitted to hospital. Cochrane database. Syst Rev. 2011;7:CD006211. doi: 10.1002/14651858.CD006211.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Partridge JSL, Collingridge G, Gordon AL, Martin FC, Harari D, Dhesi JK. Where are we in perioperative medicine for older surgical patients? A UK survey of geriatric medicine delivered services in surgery. Age Ageing. 2014;43(5):721–724. doi: 10.1093/ageing/afu084. [DOI] [PubMed] [Google Scholar]
- 56.NICE Medicines Optimisation: The Safe and Effective Use of Medicines to Enable the Best Possible Outcomes. 2015. Available from: https://www.nice.org.uk/guidance/ng5. [PubMed]
- 57.Bushardt RL, Massey EB, Simpson TW, Ariail JC, Simpson KN. Polypharmacy: misleading, but manageable. Clin Interv Aging. 2008;3(2):383–389. doi: 10.2147/cia.s2468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.The Kings Fund . Polypharmacy and Medicines Optimisation: Making It Safe and Sound. London: 2013. Available from: http://www.kingsfund.org.uk/publications/polypharmacy-and-medicines-optimisation. [Google Scholar]
- 59.Barbas AS, Haney JC, Henry BV, Heflin MT, Lagoo SA. Development and implementation of a formalized geriatric surgery curriculum for general surgery residents. Gerontol Geriatr Educ. 2014;35(4):380–394. doi: 10.1080/02701960.2013.879444. [DOI] [PubMed] [Google Scholar]
- 60.Hayes R, Jones K, Clark A. Ageism and Age Discrimination in Secondary Health Care in the United Kingdom. London: CPA; 2009. [Google Scholar]
- 61.Treml J, Husk J, Lowe D, Vasilakis N. Falling Standards, Broken Promises. Report of the National Audit of Falls and Bone Health in Older People. London: HQIP; 2010. [Google Scholar]
- 62.British Geriatrics Society . Quality care for older people with urgent and emergency care needs. London: British Geriatrics Society; 2012. [Accessed August 13, 2015]. Available from: http://www.bgs.org.uk/campaigns/silverb/silver_book_complete.pdf. [Google Scholar]
- 63.Royal College of Physicians . National Hip Fracture Database annual report 2014. London: RCP; 2014. [Accessed August 13, 2015]. Avaialble from: http://www.nhfd.co.uk/20/hipfractureR.nsf/vwcontent/2014reportPDFs/$file/NHFD2014ExtendedReport.pdf?OpenElement. [Google Scholar]
- 64.worldbankorg [homepage on the Internet] The World Bank; [Accessed August 19, 2015]. Available from: http://www.worldbank.org/ [Google Scholar]