Abstract
Objective
We aimed to determine whether there is a seasonal variation of out-of-hospital cardiac arrests (OHCA) in an equatorial climate, which does not experience seasonal environmental change.
Methods
We conducted an observational prospective study looking at the occurrence of OHCA in Singapore. Included were all patients with OHCA presented to Emergency Departments across the country. We examined the monthly, daily, and hourly number of cases over a three-year period. Data was analyzed using analysis of variance (ANOVA).
Results
From October, 1st 2001 to October, 14th 2004, 2428 patients were enrolled in the study. Mean age for cardiac arrests was 60.6 years with 68.0% male. Ethnic distribution was 69.5% Chinese, 15.0% Malay, 11.0% Indian, and 4.4% Others. There was no significant seasonal variation (spring/summer/fall/winter) of events (ANOVA P = 0.71), monthly variation (P = 0.88) or yearly variation (P = 0.26). We did find weekly peaks on Mondays and a circadian pattern with daily peaks from 9–10 am.
Conclusions
We did not find any discernable seasonal pattern of cardiac arrests. This contrasts with findings from temperate countries and suggests a climatic influence on cardiac arrest occurrence. We also found that sudden cardiac arrests follow a circadian pattern.
Keywords: cardiopulmonary resuscitation, cardiac arrest, seasonal pattern, circadian pattern
Introduction
A number of acute cardiovascular events including acute myocardial infarction, cardiac arrest, and stroke have definite time distribution patterns rather than occurring as random events.1 For example, it has been observed that sudden cardiac arrests follow a circadian pattern,2–5 with increasing incidence in the mornings until noon.1,6 Weekly patterns have also been noticed, with increased frequency of cardiac events on Mondays.7–10
Seasonal patterns have been observed for acute myocardial infarction11,12 and sudden death8 in temperate climates. A higher volume of myocardial infarction cases have been reported in winter than in summer.13,14 Similarly, a higher incidence of cardiac arrests during winter has been observed.8 However, it is currently unclear if this is a climatic effect or due to other factors. Describing the seasonal pattern of cardiac arrests in an equatorial location might shed light on whether this observation is due to a climatic effect.
We aimed to determine whether there is a seasonal variation of out-of-hospital cardiac arrests (OHCA) in an equatorial climate, which does not experience seasonal environmental change, using data from the Cardiac Arrest and Resuscitation Epidemiology (CARE) project,15–17 an OHCA registry based in equatorial Singapore.
Methods
Study design and setting
The CARE study is a large prospective registry of OHCA in Singapore. The study period was October 1st, 2001 to October 14th, 2004. Institutional Review Board approval was obtained from all participating institutions.
Singapore is a city-state with a land area of 682.3 square kilometers and a population of 4.1 million. The island’s emergency medical services (EMS) system is run by the Singapore Civil Defence Force (SCDF) which currently operates 36 ambulances based in 15 fire stations and 16 satellite stations. It is primarily a single-tier system, able to provide basic life support and defibrillation with automated external defibrillators (AEDs). Private ambulances do not attend to emergencies like cardiac arrest. It is also unusual for paramedics in our system to pronounce death in the field except for obvious decapitation, decomposition or rigor mortis. Thus, almost all out-of-hospital cardiac arrests in Singapore would have been transported to hospital.
The CARE study group includes representatives from the six major public hospitals in Singapore, the Singapore Civil Defence Force, Health Sciences Authority, and the Clinical Trials and Epidemiology Research Unit, Singapore. CARE Phase I found survival from OHCA in Singapore to be 2.0%.15 EMS response time was 10.2 ± 4.3 minutes. Time from call to defibrillation was 16.7 ± 7.2 minutes.
Patient characteristics, cardiac arrest circumstances, ECG rhythms, EMS response times, and outcomes were recorded in a standard report according to the Utstein style.
EMS timings were recorded automatically by the computerized central dispatch system and ambulance AEDs. All watches and AEDs were synchronized with the central dispatch clock at the beginning of each shift. Survival to hospital discharge was defined as the patient leaving the hospital alive or survival to 30 days post-cardiac arrest, whichever came first.
For purposes of this analysis, we defined the climatic seasons based on the northern hemisphere calendar definitions: winter (December 21 to March 19 [89 days]); spring (March 20 to June 20 [93 days]); summer (June 21 to September 22 [94 days]); fall (September 23 to December 20 [89 days]).13
Participants
All patients with prehospital cardiac arrest as confirmed by the absence of a pulse, unresponsiveness, and apnea were included. Exclusion criteria were those ‘obviously dead’ as defined by the presence of decomposition, rigor mortis or dependent lividity. We also excluded all cardiac arrests due to trauma (including drowning, choking, and poisoning) from this analysis.
Statistical analysis
Data management was carried out using the Clintrial application software version 4.4. All data analyses were performed using SPSS version 15.0 (SPSS Inc., Chicago, IL), presenting descriptive statistics and frequencies. Statistical analysis was conducted using analysis of variance (ANOVA) to analyze the mean number of cardiac arrest cases in different seasons, months, and years. The F-test from ANOVA (Type III) determined the overall main effect of season. Significance was set at P < 0.05.
Results
From October, 1st 2001 to October, 14th 2004, 2428 patients were enrolled in the study. Table 1 shows the characteristics of patients in the study. Mean age was 60.6 years with 68.0% male. 67.8% of cardiac arrests occurred in residences, with 54.5% bystander-witnessed, and another 10.5% EMS-witnessed. Mean EMS response time was 9.6 minutes with 21.7% receiving prehospital defibrillation.
Table 1.
Characteristics of all cardiac arrest patients in the study
| Characteristics | All patients N = 2428 (%) |
|---|---|
| Mean age (SD) | 60.6 (19.3) |
| Male | 1652 (68.0) |
| Race | |
| Chinese | 1687 (69.5) |
| Malay | 365 (15.0) |
| Indian | 267 (11.0) |
| Others | 108 (4.4) |
| Arrest location | |
| Residential homes | 1629 (67.8) |
| Other | 772 (32.2) |
| Collapse witness | |
| Bystander-witnessed | 1318 (54.5) |
| EMS-witnessed | 255 (10.5) |
| Not witnessed | 845 (34.9) |
| Bystander CPR | 477 (22.1) |
| Initial rhythm | |
| Ventricular Fibrillation | 424 (18.9) |
| Ventricular Tachycardia | 12 (0.5) |
| Asystole | 1162 (51.8) |
| Pulseless Electrical Activity | 599 (26.7) |
| Defibrillated | 525 (21.7) |
| Call receipt to vehicle stops, min (SD) | 9.59 (4.4) |
| Past medical history | |
| Heart disease | 786 (37.0) |
| Diabetes | 569 (26.8) |
| Hypertension | 751 (35.3) |
| Stroke | 164 (7.7) |
| Cancer | 173 (8.1) |
| Others | 449 (21.1) |
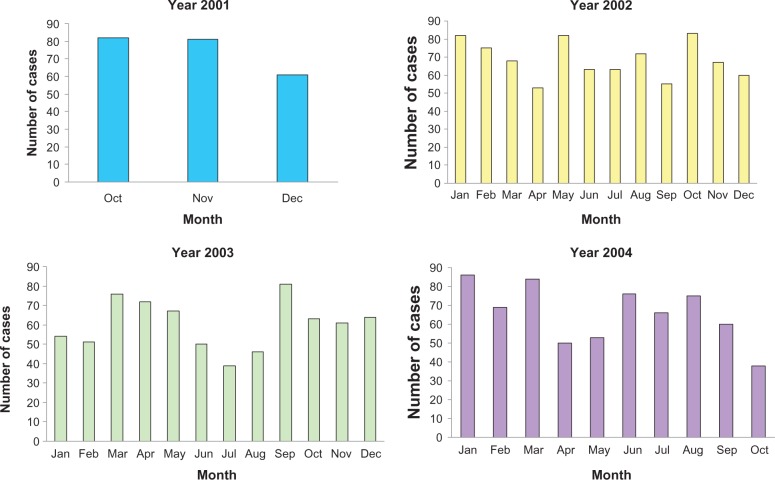
Figure 1 shows the number of cardiac arrests occurring per month over the study period.
Figure 1.
Number of cardiac arrests per year by month.
Table 2a shows the number of cardiac arrests per month by ‘season’. There was no significant seasonal variation (spring/summer/fall/winter) of events (ANOVA P = 0.71, F = 0.46). Table 2b shows the number of cardiac arrests per month, by year. There was no significant yearly variation (ANOVA P = 0.26, F = 1.40).
Table 2a.
Number of cardiac arrests per month (by ‘season’)
| N = 2428 | Mean (SD) | 95% confidence interval for mean | P-value |
|---|---|---|---|
| Winter | 66. 9 (12.1) | 57.6–76.2 | |
| (n = 602) | |||
| Spring | 67.2 (12.8) | 57.4–77.0 | |
| (n = 605) | 0.71 | ||
| Summer | 61.1 (13.3) | 50.9–71.3 | |
| (n = 550) | |||
| Fall | 67.1 (14.8) | 56.6–77.7 | |
| (n = 671) |
Table 2b.
Number of cardiac arrests per month (by year)
| N = 2428 | Mean (SD) | 95% confidenceinterval for mean | P-value |
|---|---|---|---|
| 2001 (n = 224) | 74.7 (11.9) | 45.2–104.1 | |
| 2002 (n = 823) | 68.6 (10.4) | 62.0–75.2 | 0.26 |
| 2003 (n = 724) | 60.3 (12.7) | 52.3–68.4 | |
| 2004 (n = 657) | 65.7 (15.5) | 54.6–76.8 |
Table 3 shows the number of cardiac arrests per month, by month. There was no significant monthly variation (ANOVA P = 0.88, F = 0.51).
Table 3.
Number of cardiac arrests per month (by month)
| N = 2428 | Mean (SD) | 95% confidence interval for mean | P-value |
|---|---|---|---|
| January | 74.0 (17.4) | 30.7–117.3 | |
| February | 65.0 (12.5) | 34.0–96.0 | |
| March | 76.0 (8.0) | 56.1–95.9 | |
| April | 58.3 (11.9) | 28.7–88.0 | |
| May | 67.3 (14.5) | 31.3–103.4 | |
| June | 63.0 (13.0) | 30.7–95.3 | 0.88 |
| July | 56.0 (14.8) | 19.2–92.8 | |
| August | 64.3 (15.9) | 24.7–104.0 | |
| September | 65.3 (13.8) | 31.1–99.6 | |
| October | 66.5 (21.1) | 32.9–100.1 | |
| November | 69.7 (10.3) | 44.2–95.2 | |
| December | 61.7 (2.1) | 56.5–66.8 |
There were also no significant differences in the comparison of cardiac arrest cases by gender and age, as shown in Table 4.
Table 4.
Comparison of cardiac arrest events by gender and age
| Winter (n = 602) | Spring (n = 605) | Summer (n = 550) | Fall (n = 671) | P-value | |
|---|---|---|---|---|---|
| Gender, mean (SD) | |||||
| Male | 44.3 (10.0) | 45.9 (10.6) | 43.1 (10.0) | 45.2 (13.8) | 0.96 |
| Female | 22.6 (3.0) | 21.3 (3.0) | 18 (4.9) | 21.9 (6.9) | 0.21 |
| Age, mean (SD) | |||||
| <60 years | 28 (6.1) | 28.2 (5.4) | 27.2 (7.4) | 29.4 (7.5) | 0.91 |
| ≥60 years | 38.4 (7.6) | 38.4 (8.4) | 33.3 (7.2) | 37.6 (9.4) | 0.50 |
Figure 2 shows the distribution of cardiac arrest cases by day of the week. The highest number of cardiac arrests occurred on Mondays and the lowest on Thursdays.
Figure 2.
Number of cardiac arrest cases by day.
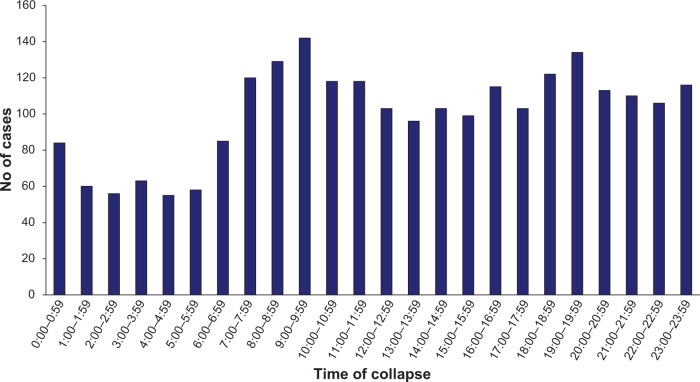
Figure 3 shows the distribution of cardiac arrest cases by time of day. There was a peak in the occurrence of cardiac arrest cases in the mornings from 9–10 am and a secondary peak from 7–8 pm. There was a trough in cardiac arrest occurrence from 1–5 am.
Figure 3.
Number of cardiac arrest cases by hour.
Discussion
In this study we did not find any discernable seasonal pattern of cardiac arrests. This contrasts with findings from temperate countries and suggests a climatic influence on cardiac arrest occurrence. However, we did notice a four to five monthly pattern of cardiac arrest occurrence locally, although the reason for this is not entirely clear.
In contrast, similar to other studies, we did find weekly peaks on Mondays and a circadian pattern with daily peaks from 9–10 am.8 These patterns were consistent year-on-year over the period of the study.
The equatorial climate of Singapore has constant temperature and weather throughout the year, without the seasonal variations of temperate countries. This makes it an ideal ‘laboratory’ for the observations made in our study. Although we did find some month-to-month variation, there was no discernable seasonal pattern, nor were there any obvious trends or factors that we could relate to the variation seen.
Identification of specific patterns in the timing of OHCA is of scientific importance because such patterns imply that there are external triggers to such events. A large number of studies have confirmed that there is a seasonal pattern to cardiac deaths in the United States,13,14,18 Australia,19 Sweden,3 England,18 and Germany.8
Theories that have been proposed to explain an increased prevalence of cardiac deaths in winter include cold weather affecting arterial blood pressure,20 arterial spasm, platelet and red blood cell counts, blood viscosity,21 plasma fibrinogen, factor VII,22 and serum cholesterol levels.23,24 Low environmental temperature has an important hemodynamic effect, including an increase in systemic vascular resistance and myocardial oxygen consumption.25
Our study also confirms that sudden cardiac arrests follow a circadian pattern,2,3 with increasing incidence in the mornings until noon.6,26 Weekly patterns have also been noticed in other studies, with increased frequency of cardiac events on Mondays.7–10 These weekly patterns might be more related to human behavior, activity, work patterns, and possibly stress levels. In Singapore, the work week begins on Mondays, and Sundays are usually rest days.
Similar patterns have been observed in acute myocardial infarction,27–32 stroke,33,34 and pulmonary embolism.35 Various explanations for this effect that have been proposed include circadian variations in the autonomic nervous system,36 variations in electrical activity,37–39 vascular changes,40,41 and hormonal/metabolic fluctuations.42
Human autonomic/hormonal/metabolic responses to the seasonal cycle have been previously documented,43 but not much is currently known about seasonal modulation of such variables in an equatorial climate. This would be an interesting area for further study. We postulate that the length of light in the day, which is more constant on the equator, might have a different effect on brain peptides or the autonomic nervous system. This contrasts with more temperate or arctic regions where the length of light in the day changes dramatically.
Study limitations
One limitation of this study is that data is based on cardiac arrest cases reported to the national ambulance service or presented to the Emergency Departments in the country. There may have been a number of cardiac arrests that were not reported and might not have been brought to a healthcare facility. However, our subjective experience is that this number is likely to be small.
Another limitation of our study is that it assumes that there were no sudden changes in the population demographics, disease patterns, and health-seeking behavior over the period.
Other areas for future study would include a death certificate-based study of cardiac deaths in Singapore, or an analysis of acute myocardial infarction registry data. This would confirm the seasonal, weekly, and daily patterns observed in this study.
Conclusion
We did not find any discernable seasonal pattern of cardiac arrests. This contrasts with findings from temperate countries and suggests a climatic influence on cardiac arrest occurrence. We did find weekly peaks on Mondays and a circadian pattern with daily peaks from 9–10 am. These patterns confirm that sudden cardiac arrests follow a circadian pattern.
Footnotes
Disclosures
This paper was presented at the Society for Emergency Medicine in Singapore 10th Annual Scientific Meeting, Singapore in February 2009, the Singapore General Hospital 18th Annual Scientific Meeting, Singapore in April 2009, and the 5th Mediterranean Emergency Meeting Congress (MEMC V), Valencia, Spain in September 2009.
All the authors have neither commercial nor personal associations or any sources of support that might pose a conflict of interest in the subject matter or materials discussed in this manuscript.
References
- 1.Gerber Y, Jacobsen SJ, Killian JM, Weston SA, Roger VL. Seasonality and daily weather conditions in relation to myocardial infarction and sudden cardiac death in Olmsted County, Minnesota, 1979 to 2002. J Am Coll Cardiol. 2006;48(2):287–292. doi: 10.1016/j.jacc.2006.02.065. [DOI] [PubMed] [Google Scholar]
- 2.Hayashi S, Toyoshima H, Tanabe N, Miyanishi K. Daily peaks in the incidence of sudden cardiac death and fatal stroke in Niigata Prefecture. Jpn Circ J. 1996;60(4):193–200. doi: 10.1253/jcj.60.193. [DOI] [PubMed] [Google Scholar]
- 3.Herlitz J, Eek M, Holmberg M, Holmberg S. Diurnal, weekly, and seasonal rhythm of out-of-hospital cardiac arrest in Sweden. Resuscitation. 2002;54(2):133–138. doi: 10.1016/s0300-9572(02)00097-7. [DOI] [PubMed] [Google Scholar]
- 4.Jones-Crawford JL, Parish DC, Smith BE, Dane FC. Resuscitation in the hospital: circadian variation of cardiopulmonary arrest. Am J Med. 2007;120(2):158–164. doi: 10.1016/j.amjmed.2006.06.032. [DOI] [PubMed] [Google Scholar]
- 5.Savopoulos C, Ziakas A, Hatzitolios A, et al. Circadian rhythm in sudden cardiac death: a retrospective study of 2,665 cases. Angiology. 2006;57(2):197–204. doi: 10.1177/000331970605700210. [DOI] [PubMed] [Google Scholar]
- 6.Cho JG, Park HW, Rhew JY, et al. Clinical characteristics of unexplained sudden cardiac death in Korea. Jpn Circ J. 2001;65(1):18–22. doi: 10.1253/jcj.65.18. [DOI] [PubMed] [Google Scholar]
- 7.Arntz HR, Muller-Nordhorn J, Willich SN. Cold Monday mornings prove dangerous: epidemiology of sudden cardiac death. Curr Opin Crit Care. 2001;7(3):139–144. doi: 10.1097/00075198-200106000-00001. [DOI] [PubMed] [Google Scholar]
- 8.Arntz HR, Willich SN, Schreiber C, Bruggemann T, Stern R, Schultheiss HP. Diurnal, weekly, and seasonal variation of sudden death. Population-based analysis of 24,061 consecutive cases. Eur Heart J. 2000;21(4):315–320. doi: 10.1053/euhj.1999.1739. [DOI] [PubMed] [Google Scholar]
- 9.Gruska M, Gaul GB, Winkler M, et al. Increased occurrence of out-of-hospital cardiac arrest on Mondays in a community-based study. Chronobiol Int. 2005;22(1):107–120. doi: 10.1081/cbi-200041046. [DOI] [PubMed] [Google Scholar]
- 10.Peckova M, Fahrenbruch CE, Cobb LA, Hallstrom AP. Weekly and seasonal variation in the incidence of cardiac arrests. Am Heart J. 1999;137(3):512–515. doi: 10.1016/s0002-8703(99)70507-7. [DOI] [PubMed] [Google Scholar]
- 11.Lee JH, Chae SC, Yang DH, et al. Influence of weather on daily hospital admissions for acute myocardial infarction (from the Korea Acute Myocardial Infarction Registry) Int J Cardiol. 2009 doi: 10.1016/j.ijcard.2009.03.122. [DOI] [PubMed] [Google Scholar]
- 12.Manfredini R, Boari B, Smolensky MH, et al. Seasonal variation in onset of myocardial infarction – a 7-year single-center study in Italy. Chronobiol Int. 2005;22(6):1121–1135. doi: 10.1080/07420520500398106. [DOI] [PubMed] [Google Scholar]
- 13.Ornato JP, Peberdy MA, Chandra NC, Bush DE. Seasonal pattern of acute myocardial infarction in the National Registry of Myocardial Infarction. J Am Coll Cardiol. 1996;28(7):1684–1688. doi: 10.1016/s0735-1097(96)00411-1. [DOI] [PubMed] [Google Scholar]
- 14.Spencer FA, Goldberg RJ, Becker RC, Gore JM. Seasonal distribution of acute myocardial infarction in the second National Registry of Myocardial Infarction. J Am Coll Cardiol. 1998;31(6):1226–1233. doi: 10.1016/s0735-1097(98)00098-9. [DOI] [PubMed] [Google Scholar]
- 15.Ong ME, Chan YH, Anantharaman V, Lau ST, Lim SH, Seldrup J. Cardiac arrest and resuscitation epidemiology in Singapore (CARE I study) Prehosp Emerg Care. 2003;7(4):427–433. doi: 10.1080/312703002120. [DOI] [PubMed] [Google Scholar]
- 16.Ong ME, Tan EH, Ng FS, et al. Survival outcomes with the introduction of intravenous epinephrine in the management of out-of-hospital cardiac arrest. Ann Emerg Med. 2007;50(6):635–642. doi: 10.1016/j.annemergmed.2007.03.028. [DOI] [PubMed] [Google Scholar]
- 17.Ong ME, Tan EH, Yan X, et al. An observational study describing the geographic-time distribution of cardiac arrests in Singapore: what is the utility of geographic information systems for planning public access defibrillation? (PADS Phase I) Resuscitation. 2008;76(3):388–396. doi: 10.1016/j.resuscitation.2007.09.006. [DOI] [PubMed] [Google Scholar]
- 18.Brooks SC, Schmicker RH, Rea TD, et al. Out-of-hospital cardiac arrest frequency and survival: Evidence for temporal variability. Resuscitation. 2010;81(2):175–181. doi: 10.1016/j.resuscitation.2009.10.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Loughnan ME, Nicholls N, Tapper NJ. Demographic, seasonal, and spatial differences in acute myocardial infarction admissions to hospital in Melbourne, Australia. Int J Health Geogr. 2008;7:42. doi: 10.1186/1476-072X-7-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Alperovitch A, Lacombe JM, Hanon O, et al. Relationship between blood pressure and outdoor temperature in a large sample of elderly individuals: the Three-City study. Arch Intern Med. 2009;169(1):75–80. doi: 10.1001/archinternmed.2008.512. [DOI] [PubMed] [Google Scholar]
- 21.Frohlich M, Sund M, Russ S, et al. Seasonal variations of rheological and hemostatic parameters and acute-phase reactants in young, healthy subjects. Arterioscler Thromb Vasc Biol. 1997;17(11):2692–2697. doi: 10.1161/01.atv.17.11.2692. [DOI] [PubMed] [Google Scholar]
- 22.Woodhouse PR, Khaw KT, Plummer M, Foley A, Meade TW. Seasonal variations of plasma fibrinogen and factor VII activity in the elderly: winter infections and death from cardiovascular disease. Lancet. 1994;343(8895):435–439. doi: 10.1016/s0140-6736(94)92689-1. [DOI] [PubMed] [Google Scholar]
- 23.Ockene IS, Chiriboga DE, Stanek EJ, III, et al. Seasonal variation in serum cholesterol levels: treatment implications and possible mechanisms. Arch Inter Med. 2004;164(8):863–870. doi: 10.1001/archinte.164.8.863. [DOI] [PubMed] [Google Scholar]
- 24.Shephard RJ, Aoyagi Y. Seasonal variations in physical activity and implications for human health. Eur J Appl Physiol. 2009;107(3):251–271. doi: 10.1007/s00421-009-1127-1. [DOI] [PubMed] [Google Scholar]
- 25.Wilmshurst P. Temperature and cardiovascular mortality. BMJ. 1994;309(6961):1029–1030. doi: 10.1136/bmj.309.6961.1029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Thakur RK, Hoffmann RG, Olson DW, et al. Circadian variation in sudden cardiac death: effects of age, sex, and initial cardiac rhythm. Ann Emerg Med. 1996;27(1):29–34. doi: 10.1016/s0196-0644(96)70292-5. [DOI] [PubMed] [Google Scholar]
- 27.Cannon CP, McCabe CH, Stone PH, et al. Circadian variation in the onset of unstable angina and non-Q-wave acute myocardial infarction (the TIMI III Registry and TIMI IIIB) Am J Cardiol. 1997;79(3):253–258. doi: 10.1016/s0002-9149(97)00743-1. [DOI] [PubMed] [Google Scholar]
- 28.Manfredini R, Manfredini F, Boari B, et al. Seasonal and weekly patterns of hospital admissions for nonfatal and fatal myocardial infarction. Am J Emerg Med. 2009;27(9):1097–1103. doi: 10.1016/j.ajem.2008.08.009. [DOI] [PubMed] [Google Scholar]
- 29.Shaw E, Tofler GH. Circadian rhythm and cardiovascular disease. Curr Atheroscler Rep. 2009;11(4):289–295. doi: 10.1007/s11883-009-0044-4. [DOI] [PubMed] [Google Scholar]
- 30.Turin TC, Kita Y, Rumana N, et al. Incidence, admission, and case-fatality of acute myocardial infarction: weekend versus weekday in a Japanese population: 16-year results from Takashima AMI Registry (1988–2003) Eur J Epidemiol. 2009;24(2):93–100. doi: 10.1007/s10654-008-9308-5. [DOI] [PubMed] [Google Scholar]
- 31.Van der Palen J, Doggen CJ, Beaglehole R. Variation in the time and day of onset of myocardial infarction and sudden death. N Z Med J. 1995;108(1006):332–334. [PubMed] [Google Scholar]
- 32.Witte DR, Grobbee DE, Bots ML, Hoes AW. A meta-analysis of excess cardiac mortality on Monday. Eur J Epidemiol. 2005;20(5):401–406. doi: 10.1007/s10654-004-8783-6. [DOI] [PubMed] [Google Scholar]
- 33.Manfredini R, Boari B, Smolensky MH, et al. Circadian variation in stroke onset: identical temporal pattern in ischemic and hemorrhagic events. Chronobiol Int. 2005;22(3):417–453. doi: 10.1081/CBI-200062927. [DOI] [PubMed] [Google Scholar]
- 34.Turin TC, Kita Y, Rumana N, et al. Stroke case fatality shows seasonal variation regardless of risk factor status in a Japanese population: 15-year results from the Takashima Stroke Registry. Neuroepidemiology. 2009;32(1):53–60. doi: 10.1159/000170907. [DOI] [PubMed] [Google Scholar]
- 35.Gallerani M, Boari B, Smolensky MH, et al. Seasonal variation in occurrence of pulmonary embolism: analysis of the database of the Emilia-Romagna region, Italy. Chronobiol Int. 2007;24(1):143–160. doi: 10.1080/07420520601139755. [DOI] [PubMed] [Google Scholar]
- 36.Piepoli MF, Capucci A. Autonomic nervous system in the genesis of arrhythmias in chronic heart failure: implication for risk stratification. Minerva Cardioangiol. 2007;55(3):325–333. [PubMed] [Google Scholar]
- 37.Beyerbach DM, Kovacs RJ, Dmitrienko AA, Rebhun DM, Zipes DP. Heart rate-corrected QT interval in men increases during winter months. Heart Rhythm. 2007;4(3):277–281. doi: 10.1016/j.hrthm.2006.11.008. [DOI] [PubMed] [Google Scholar]
- 38.Oren H, Cosgun A. Weekly variation of the QT dispersion in healthy subjects and in patients with coronary heart disease. Cardiology. 2007;108(1):55–61. doi: 10.1159/000095882. [DOI] [PubMed] [Google Scholar]
- 39.Wennerblom B, Lurje L, Karlsson T, Tygesen H, Vahisalo R, Hjalmarson A. Circadian variation of heart rate variability and the rate of autonomic change in the morning hours in healthy subjects and angina patients. Int J Cardiol. 2001;79(1):61–69. doi: 10.1016/s0167-5273(01)00405-3. [DOI] [PubMed] [Google Scholar]
- 40.Otto ME, Svatikova A, Barretto RB, et al. Early morning attenuation of endothelial function in healthy humans. Circulation. 2004;109(21):2507–2510. doi: 10.1161/01.CIR.0000128207.26863.C4. [DOI] [PubMed] [Google Scholar]
- 41.Pringle E, Phillips C, Thijs L, et al. Systolic blood pressure variability as a risk factor for stroke and cardiovascular mortality in the elderly hypertensive population. J Hypertens. 2003;21(12):2251–2257. doi: 10.1097/00004872-200312000-00012. [DOI] [PubMed] [Google Scholar]
- 42.Li JJ. Circadian variation in myocardial ischemia: the possible mechanisms involving in this phenomenon. Med Hypotheses. 2003;61(2):240–243. doi: 10.1016/s0306-9877(03)00154-3. [DOI] [PubMed] [Google Scholar]
- 43.Foster RG, Roenneberg T. Human responses to the geophysical daily, annual, and lunar cycles. Curr Biol. 2008;18(17):R784–R794. doi: 10.1016/j.cub.2008.07.003. [DOI] [PubMed] [Google Scholar]