Abstract
BACKGROUND
Preventable readmission has become a national focus. It is clear that surgical patients present specific challenges to those interested in preventing readmission. Little is known about this outcome in the emergent population. We are interested in determining if there are readily available data variables to predict risk of readmission. The surgical Apgar score (SAS) is calculated from objective intraoperative variables and has been shown to be predictive of postoperative mortality in the nonemergent setting. The objectives of this study were to characterize 30-day readmissions in emergent general surgery and to determine whether certain variables were associated with readmissions. We hypothesized that the SAS correlates with the risk for readmission in emergency general surgery patients.
PATIENTS AND METHODS
Variables of interest were obtained from a retrospective analysis of the American College of Surgeons’ National Surgical Quality Improvement Program database at an academic institution, paired with the electronic medical record. We identified adult general surgery patients who underwent an emergency procedure from 2006 to 2012. Univariate analysis identified factors associated with 30-day readmission. Factors with p < 0.1 were included in the multivariate analysis to reveal potential risk factors. SPSS version 20 was used for the statistical analysis, with p < 0.05 considered to be significant on multivariate analysis.
RESULTS
As compared with nonemergency surgery patients, emergency surgery patients had a higher readmission rate (11.1% vs. 15.2%, p = 0.004). The SAS (odds ratio, 3.297; 95% confidence interval, 1.074–10.121; p = 0.037) and the combined variable of the American Society of Anesthesiologists Physical Status Classification and length of stay (odds ratio, 4.370; 95% confidence interval, 2.251–8.486; p < 0.001) were associated with elevated risk for readmission in emergency general surgery patients.
CONCLUSION
We have identified readily available measures that allow for the stratification of patients into low- and high-risk groups for 30-day readmission. The stratification of patients will enable the study of prospective interventions designed to decrease unplanned readmissions in emergency surgery patients.
LEVEL OF EVIDENCE
Prognostic study, level II.
Keywords: Emergency surgery, readmissions, risk factors
Preventable readmission has become a topic of interest in discussing health care reform.1,2 It is not only a concern for clinicians regarding patient health but also a contributor to the rising cost of health care. It is estimated that unplanned readmissions cost $17.4 billion in 2004.1 Readmissions and postoperative complications have been examined for nonemergency surgeries, including the identification of potential predictors of such outcomes.3–6 Despite an assumed high risk of readmission after emergency surgery, little is known about readmissions in this patient population. Associations have been described between postoperative outcomes and perioperative variables in the older adult emergency surgery population, including complications and disease scoring systems (e.g., POSSUM).7–10 However, risk factors in the entire adult emergency surgery population are less clear particularly for readmissions. Elucidating such risk factors may allow for earlier a modification of patient care or an enhancement of the discharge process to prevent unplanned readmissions.
The surgical Apgar score (SAS) has been developed by Gawande et al.11 to evaluate outcomes in surgical patients. It is a score calculated from intraoperative variables for which poorer outcomes correspond with lower surgical scores.11 The SAS has been studied in the nonemergency setting and has been shown to be associated with mortality and other major postoperative complications, particularly regarding general and vascular surgery patients.4,5,11,12 The SAS is easily calculated and derived from objective intraoperative data, making it an ideal measure to include in a predictive model for readmissions after emergency surgery.
The purpose of this study was to characterize 30-day readmissions in patients undergoing emergency general surgery, in comparison with nonemergency general surgery patients. Furthermore, we hoped to identify objective factors that predict readmission following emergency surgery. Our goal was to determine whether certain readily available variables or measures, including the SAS, were associated with readmissions in emergency surgery patients. We hypothesized that the SAS correlates with a risk for readmission in the emergency general surgery patient population.
PATIENTS AND METHODS
Study patients were identified from the American College of Surgeons’ National Surgical Quality Improvement Program (NSQIP) database at the University of Wisconsin. The database is maintained by postoperative collection of perioperative data on patients included through a systematic selection process.13 Any variable not collected by the NSQIP Surgical Clinical Reviewer (SCR) was retrospectively collected via thorough examination of the electronic medical record. This study was approved by our institutional review board and human subjects committee. We included patients 18 years or older who underwent general surgery procedures after inpatient admission between August 2006 and June 2012 at the University of Wisconsin. Procedures defined as emergency, according to the standard NSQIP definition, were surgeries performed during the index hospitalization, which were deemed emergent by the attending surgeon and/or anesthesiologist. Urgent cases were not included. Trained nursing staff extracted the data, and in instances of inconsistency between the surgical and anesthesia reports, the attending surgeon’s assessment was given priority. Patients who died before discharge or within 30 days of discharge were excluded from the study because the primary outcome was 30-day readmission after discharge following emergency general surgery.
Variables examined as potential predictors of readmission included preoperative comorbidities and measures of health (diabetes mellitus, dyspnea, smoker, steroid use, weight loss, systemic inflammatory response syndrome, body mass index (BMI),wound class, ventilator dependence, chronic obstructive pulmonary disease, ascites, congestive heart failure, hypertension, acute renal failure, dialysis, disseminated cancer, open wound, bleeding disorder, transfusion, and sepsis), in addition to hospital length of stay (LOS) and demographics (sex, race, and older age on operation day). The American Society of Anesthesiologists Physical Status Classification (ASA class) was another included health measure. All variables were dichotomized as described in Table 1, as per standard NSQIP definitions.
TABLE 1.
Dichotomized Perioperative Variables
| Positive Criteria | |
|---|---|
| Diabetes | Non–insulin-dependent or insulin-dependent diabetes |
| Smoker | Cigarette smoking within the year before admission |
| Steroid | Intake of steroids and/or immunosuppressive medications for a chronic condition within 30 d before surgery |
| Weight loss | Weight loss greater than 10% of body weight within 6 mo before surgery |
| SIRS | SIRS within 48 hours before surgery |
| Sepsis | Septic shock within 48 h before surgery |
| BMI | Obese (>30 kg/m2) |
| Wound class | Contaminated or dirty/infected wound |
| Ventilator dependence | Need for ventilator assisted respiration in the 48 h before surgery |
| Ascites, congestive heart failure, COPD, dyspnea, hypertension | Conditions present within 30 d before the operation |
| Open wound | Open wound in the skin with or without infection |
| Disseminated cancer | Dissemination or metastasis of primary cancer within 1 y before surgery |
| Bleeding disorder | Documented chronic hematologic disorder or medication use that interferes with clotting |
| Acute renal failure | Present within 24 h before surgery |
| Dialysis | Dialysis at any point within the 2 wk before surgery |
| Transfusion | Documented events requiring at least 5 U of blood within the 72 h before surgery |
| ASA class | ASA class ≥3 |
| LOS | Prolonged LOS defined by the fourth quartile (>12 d) |
| Age | Older (≥65 y) |
COPD, chronic obstructive pulmonary disease; SIRS, systemic inflammatory response syndrome.
Components of the SAS were obtained from the electronic medical record. Intraoperative lowest heart rate (HR), lowest mean arterial blood pressure (MAP), and estimated blood loss (EBL) were obtained from anesthesia records in all instances. The SAS was calculated as shown previously to give a 0 to 10 score.4,11 The individual points from EBL (0–3 points), MAP (0–3 points), and HR (0–4 points) were summed as described by Gawande et al., with smaller point values assigned for larger EBL, lower MAP, and higher HR.4,11 Approximate SAS quartiles were established by dividing the patient population into four groups as evenly as allowed by integer SAS values. To create a dichotomized score, a cutoff was established for the SAS using the first quartile (<6), given that lower scores have previously correlated with poorer outcomes.11 Note that for patients with missing data, an “unknown” category was created for which readmission rates were determined, given that such data may not be missing at random.14
Readmission rates were compared between the emergency and nonemergency cohorts via Χ2 analysis. Descriptive statistics were performed for the emergency patient population. Univariate Χ2 analysis was performed to determine the relationship between potential predictive variables (including the SAS) and 30-day readmissions after emergency general surgery. A binary logistic regression was used to identify predictors of readmissions. Only variables with p < 0.1 by Χ2 testing were included in the multivariate analysis. Variables with less than 10 patients in the high-risk group in univariate analysis were excluded from our multivariate model. Given the presence of multicollinearity, single variables were established (either via exclusion or combination of variables) for intercorrelated variables (Pearson coefficient > 0.3) whose presence significantly impacted the influence of the other factor(s). ASA class was chosen over hypertension because these two variables were highly correlated. Because of the strong intercorrelation, SAS, ASA class, and LOS were combined into one variable where patients were split into groups of patients with one or more of the following: SAS less than 6, ASA class of 3 or higher, or LOS greater than 12. LOS and ASA class were the highest correlated variables and thus considered the same factor. Multivariate analysis was performed via a binary logistic regression. Variables with p < 0.05 were considered significant, allowing for the assessment of risk of readmission. All statistical analyses were performed in SPSS version 20.
RESULTS
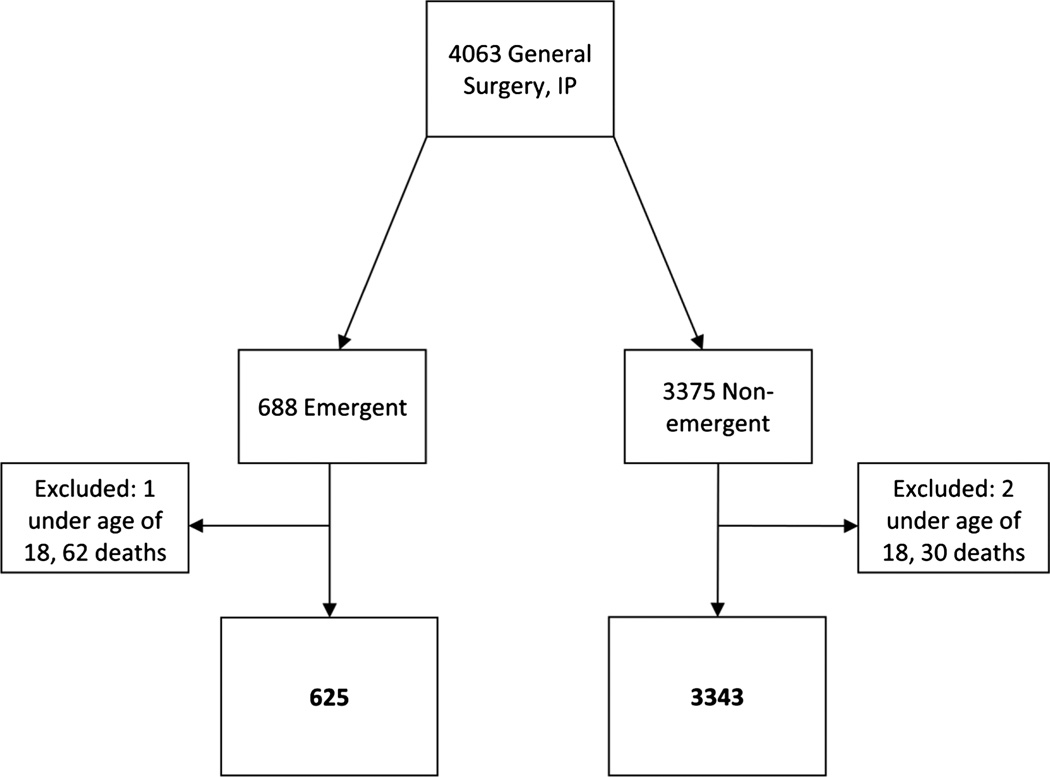
After exclusions, 625 patients were identified in the emergency surgery cohort and 3343 patients were identified in the nonemergency surgery cohort (Fig. 1). The readmission rate was 15.2% for patients undergoing emergency procedures, as compared with 11.1% for patients undergoing nonemergency surgery (p = 0.004).
Figure 1.
General surgery study population. IP, in-patient.
Table 2 demonstrates patient characteristics for patients who underwent emergency surgery. Note that of the patient characteristics evaluated, only BMI, ASA class, and number of complications were significantly different between patients readmitted and those who were not readmitted. Not surprisingly, we found that patients with a BMI greater than 30 kg/m2, ASA class of 3 or higher, and those with one or more postoperative complications had higher risk for readmission.
TABLE 2.
Emergency General Surgery Patient Population Characteristics
| Overall (N = 625), n (%) | No Readmission (n = 530), n (%) | Readmission (n = 95), n (%) | p | |
|---|---|---|---|---|
| Sex | 0.757 | |||
| Female | 292 (46.7) | 249 (47.0) | 43 (45.3) | |
| Age, y | 0.477 | |||
| ≥65 | 170 (27.2) | 147 (27.7) | 23 (24.2) | |
| Median, 53.4 y | ||||
| Range, 18.0–101.6 y | ||||
| Race | 0.390 | |||
| White | 536 (85.8) | 453 (85.5) | 83 (87.4) | |
| Non-white | 72 (11.5) | 64 (12.1) | 8 (8.4) | |
| Unavailable | 17 (2.7) | 13 (2.5) | 4 (4.2) | |
| BMI, kg/m2 | 0.027 | |||
| >30 | 202 (32.3) | 160 (30.2) | 42 (44.2) | |
| ≤30 | 414 (66.2) | 362 (68.3) | 52 (54.7) | |
| Unknown | 9 (1.4) | 8 (1.5) | 1 (1.1) | |
| ASA class | <0.001 | |||
| ≥3 | 291 (46.6) | 223 (42.1) | 68 (71.6) | |
| No. complications | <0.001 | |||
| ≥1 | 268 (42.9) | 185 (34.9) | 83 (87.4) | |
| Mean, 1 | ||||
| Range, 0–8 |
The American College of Surgeons’ NSQIP variables significantly associated with 30-day readmissions (p < 0.1) upon univariate analysis are included in Table 3. After exclusions for small sample size, none of the variables were found to be protective for readmission. The relationship between approximate SAS quartiles and readmissions is included in Table 4. Patients within the first quartile had the highest readmission rate. Note that the intraoperative data were missing for seven patients, who consequently were excluded from further analysis. Patients with SAS less than 6 had a readmission rate of 25.4%, as opposed to 12.4% in patients with higher surgical scores.
TABLE 3.
Perioperative Variables Associated With 30-Day Readmissions in Emergency General Surgery Patients
| Readmission Rate, % | ||||
|---|---|---|---|---|
| n | Factor Absent | Factor Present | p | |
| Ventilator dependence | 43 | 14.4 | 25.6 | 0.049 |
| Congestive heart failure* | 15 | 15.6 | 0.0 | 0.097 |
| Hypertension | 261 | 12.4 | 19.2 | 0.020 |
| Open wound | 58 | 14.1 | 25.9 | 0.018 |
| Steroid | 52 | 14.0 | 28.8 | 0.004 |
| Weight loss* | 25 | 14.5 | 32.0 | 0.017 |
| Bleeding disorder | 81 | 13.8 | 24.7 | 0.011 |
| Sepsis | 344 | 12.5 | 17.4 | 0.084 |
| BMI > 30 | 202 | 12.6 | 20.8 | 0.027 |
| ASA class ≥ 3 | 291 | 8.1 | 23.4 | <0.001 |
| LOS > 12 | 156 | 11.5 | 26.3 | <0.001 |
Note that congestive heart failure and weight loss had less than 10 patients in the high-risk group.
Insignificant independent variables were diabetes, smoker, dyspnea, COPD, ascites, acute renal failure, dialysis, disseminated cancer, transfusion, SIRS, age of 65 years or older at operation, sex, wound class, race.
COPD, chronic obstructive pulmonary disease.
TABLE 4.
The SAS and 30-Day Readmission Rates
| n | Readmission Rate, % | ||
|---|---|---|---|
| SAS* | 1–5 | 142 | 25.4 |
| 6–7 | 225 | 12.9 | |
| 8 | 138 | 14.5 | |
| 9–10 | 113 | 8.8 |
Intraoperative data were missing for seven patients, for whom the SAS could not be calculated.
p = 0.001.
Table 5 contains results of the univariate analysis of the combined SAS, ASA class, and LOS variables, and rate of readmission. In comparison with patients with high SAS, low ASA class, and LOS of 12 days or less, patients with low SAS had an elevated readmission rate. An even higher rate of readmission was observed in patients with high ASA class and/or LOS. Note that adding low SAS to the latter group of patients resulted in the highest readmission rate.
TABLE 5.
Thirty-Day Readmissions for the Collinear SAS, ASA Class, and Hospital LOS
| n | % Readmitted |
|
|---|---|---|
| Low-risk reference, SAS ≥ 6,* LOS ≤ 12, ASA class < 3 | 273 | 5.1 |
| SAS < 6* | 33 | 15.2 |
| LOS > 12 and/or ASA class ≥ 3 | 203 | 22.2 |
| SAS < 6,* and LOS > 12, and/or ASA class ≥ 3 | 109 | 28.4 |
Intraoperative data were missing for seven patients, for whom the SAS could not be calculated.
p < 0.001.
In the multivariate model, only the combined variables SAS, ASA class, and LOS were significant (Table 6). Patients with low SASs had greater odds of being readmitted, as did patients with increased LOS and/or high ASA class. Having all three risk factors corresponded with the greatest odds of 30-day readmission after emergency general surgery.
TABLE 6.
Multivariate Analysis for 30-Day Readmissions in Emergency General Surgery Patients
| Odds Ratio |
95% Confidence Interval |
p | |
|---|---|---|---|
| Combined SAS, LOS, ASA class* | |||
| SAS < 6 | 3.297 | 1.074–10.121 | 0.037 |
| LOS > 12 and/or ASA class ≥ 3 | 4.370 | 2.251–8.486 | <0.001 |
| SAS < 6, and LOS > 12 and/or ASA class ≥ 3 | 6.086 | 2.867–12.919 | <0.001 |
| Ventilator dependence | 0.920 | 0.403–2.099 | 0.843 |
| Open wound | 1.234 | 0.622–2.450 | 0.548 |
| Steroid | 1.804 | 0.915–3.557 | 0.088 |
| Bleeding disorder | 1.224 | 0.668–2.244 | 0.512 |
| Sepsis | 0.957 | 0.577–1.587 | 0.864 |
| BMI | |||
| >30 | 1.436 | 0.886–2.326 | 0.142 |
| Unknown | 1.013 | 0.109–9.449 | 0.991 |
DISCUSSION
The purpose of this study was to characterize 30-day readmissions after emergency general surgery in comparison with nonemergency general surgery. Furthermore, we sought to establish risk factors for readmissions in the emergency general surgery patient population. We have demonstrated a higher rate of readmission in the emergency setting of general surgery versus nonemergency general surgery. We found the readily available variables of SAS, LOS, and ASA class were strong predictors of risk for readmission after emergency general surgery.
Our finding that readmissions are more common in the emergency population is in agreement with studies that have characterized poor postoperative outcomes as more prevalent in emergency patients versus nonemergency patients.8,15–17 What distinguishes our study is the observation of easy-to-measure risk factors for 30-day readmissions, including the SAS. Reynolds et al.5 did look at the extension of the SAS as a mortality predictor across more surgical specialties, including emergency surgery. They were able to show that lower scores correlated with greater risk for mortality in certain specialties but the risk was diminished for emergency surgery after adjustment for ASA class. Our study suggests that this is not the case for readmissions after emergency surgery, given that patients who did not have a high ASA class but had a low surgical score were still at increased risk. Furthermore, the addition of low SAS to high ASA class increased risk for readmission in our patient population. This is similar to what was shown for mortality regarding general and vascular surgery, among others, where the SAS was found to be a predictor of the outcome independent of ASA class.5 This is really the crux in including the SAS, ASA class, and LOS in one model because it identifies a greater proportion of patients at higher risk of readmission and allows one to better assess different magnitudes of increased risk.
The literature on postoperative readmissions suggests that postoperative complications play a large role in readmissions.2,8,18 Similar to Primatesta and Goldacre,15 we also observed a high correlation between 30-day readmissions and postoperative complications in emergency surgery patients. It is not surprising that patients who were readmitted with poor health often had at least one complication postoperatively. It is clear that complications and readmissions go hand in hand in surgical patients, and perhaps, readmission should be considered a major type of complication as done by Manilich et al.19 However, we sought to identify other predictors of readmission that would be easy to measure and would identify at-risk patients before discharge.
The basis for identifying risk factors for readmission after emergency general surgery is the overriding vision of modifying postoperative care or the discharge plan for these patients to prevent unplanned readmissions. We have described factors that may serve a role in a predictive model. If one can anticipate readmissions by establishing risk before discharge, there is opportunity to modify discharge plans to decrease the likelihood of readmission. This may involve targeted patient education, improved care transition, closer follow-up, and/or discharge to a destination with a higher level of care than otherwise planned. There are studies that suggest that certain modifications lead to decreased unplanned readmissions in other patient populations,20–22 but the literature also suggests that proposed interventions may not work, as demonstrated by a lack of readmission prevention with more stringent discharge planning and follow-up in general internal medicine and congestive heart failure patients, among others.23–25 Future studies are necessary to examine what interventions are truly effective, specifically within the emergency surgery population. We believe that the results of this study set the stage for future prospective studies targeted toward reducing unplanned readmissions in high-risk emergency surgery patients.
Given that our study was performed at a single academic institution, the results may not be generalized to other experiences. Expansion across a greater number of institutions would increase patient numbers across more specific surgical scores and perhaps allow for better separation between LOS and ASA class. Further limitation stems from the retrospective nature of this study, which involved review of anesthesia records with varying amounts of data (fewer data points in scanned paper charts before electronic anesthesia charts). However, the prospective use of the SAS would not encounter this problem. We believe that together the easily attained variables adequately factor patient health, operative performance, and level of hospital care to overcome limitations in the application to other settings.
In conclusion, this study has shown a significant level of readmission in emergency general surgery patients. We identified the following risk factors for readmission: the SAS, LOS, and ASA class. This study demonstrates the predictive power of the SAS, in conjunction with LOS and ASA class, in identifying patients at risk for readmission. Together, these three model components can distinguish high-risk patients, such that future studies may implement prospective interventions with the goal of reducing unplanned readmissions in high-risk emergency surgery patients.
Acknowledgments
We are also thankful for the statistical support provided by Glen Leverson, PhD.
DISCLOSURE
Support for this study was provided by the NIH T35 training grant (DK062709).
Footnotes
AUTHORSHIP
G.M., S.E.T, and G.D.K. performed the literature search. G.D.K. was responsible for the study design. G.M. performed the data collection and analysis. G.M., S.E.T, S.K.A, and G.D.K. contributed to the data interpretation. G.M., S.E.T, A.E.L, S.K.A., and G.D.K. were responsible for drafting and revising the manuscript, in addition to the final approval.
This study has been accepted for poster presentation at the 2013 Wisconsin Surgical Society Meeting, Kohler, Wisconsin (November 2013), and for oral presentation at the 9th Annual Academic Surgical Congress, San Diego, California (February 2014).
REFERENCES
- 1.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360:1418–1428. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 2.Lawson EH, Hall BL, Louie R, Ettner SL, Zingmond DS, Han L, Rapp M, Ko CY. Association Between Occurrence of a Postoperative Complication and Readmission: Implications for Quality Improvement and Cost Savings. Annals of Surgery. 2013;258:10–18. doi: 10.1097/SLA.0b013e31828e3ac3. [DOI] [PubMed] [Google Scholar]
- 3.Kassin MT, Owen RM, Perez SD, Leeds I, Cox JC, Schnier K, Sadiraj V, Sweeney JF. Risk factors for 30-day hospital readmission among general surgery patients. Journal of the American College of Surgeons. 2012;215:322–330. doi: 10.1016/j.jamcollsurg.2012.05.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Regenbogen SE, Lancaster RT, Lipsitz SR, Greenberg CC, Hutter MM, Gawande AA. Does the Surgical Apgar Score measure intraoperative performance? Annals of surgery. 2008;248:320–328. doi: 10.1097/SLA.0b013e318181c6b1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Reynolds PQ, Sanders NW, Schildcrout JS, Mercaldo ND, St Jacques PJ. Expansion of the surgical Apgar score across all surgical subspecialties as a means to predict postoperative mortality. Anesthesiology. 2011;114:1305–1312. doi: 10.1097/ALN.0b013e318219d734. [DOI] [PubMed] [Google Scholar]
- 6.Barbas AS, Turley RS, Mallipeddi MK, Lidsky ME, Reddy SK, White RR, Clary BM. Examining reoperation and readmission after hepatic surgery. Journal of the American College of Surgeons. 2013;216:915–923. doi: 10.1016/j.jamcollsurg.2013.01.008. [DOI] [PubMed] [Google Scholar]
- 7.Kurian A, Suryadevara S, Ramaraju D, Gallagher S, Hofmann M, Kim S, Zebley M, Fassler S. In-hospital and 6-month mortality rates after open elective vs open emergent colectomy in patients older than 80 years. Diseases of the colon and rectum. 2011;54:467–471. doi: 10.1007/DCR.0b013e3182060904. [DOI] [PubMed] [Google Scholar]
- 8.Racz J, Dubois L, Katchky A, Wall W. Elective and emergency abdominal surgery in patients 90 years of age or older. Canadian journal of surgery Journal canadien de chirurgie. 2012;55:322–328. doi: 10.1503/cjs.007611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lidsky ME, Thacker JK, Lagoo-Deenadayalan SA, Scarborough JE. Advanced age is an independent predictor for increased morbidity and mortality after emergent surgery for diverticulitis. Surgery. 2012;152:465–472. doi: 10.1016/j.surg.2012.06.038. [DOI] [PubMed] [Google Scholar]
- 10.Fukuda N, Wada J, Niki M, Sugiyama Y, Mushiake H. Factors predicting mortality in emergency abdominal surgery in the elderly. World journal of emergency surgery : WJES. 2012;7:12. doi: 10.1186/1749-7922-7-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gawande AA, Kwaan MR, Regenbogen SE, Lipsitz SA, Zinner MJ. An Apgar score for surgery. Journal of the American College of Surgeons. 2007;204:201–208. doi: 10.1016/j.jamcollsurg.2006.11.011. [DOI] [PubMed] [Google Scholar]
- 12.Regenbogen SE, Ehrenfeld JM, Lipsitz SR, Greenberg CC, Hutter MM, Gawande AA. Utility of the surgical apgar score: validation in 4119 patients. Archives of Surgery (Chicago, Ill: 1960) 2009;144:30–36. doi: 10.1001/archsurg.2008.504. discussion 37. [DOI] [PubMed] [Google Scholar]
- 13. [ http://site.acsnsqip.org/] [Google Scholar]
- 14.Hamilton BH, Ko CY, Richards K, Hall BL. Missing data in the American College of Surgeons National Surgical Quality Improvement Program are not missing at random: implications and potential impact on quality assessments. Journal of the American College of Surgeons. 2010;210:125–139. e122. doi: 10.1016/j.jamcollsurg.2009.10.021. [DOI] [PubMed] [Google Scholar]
- 15.Primatesta P, Goldacre MJ. Inguinal hernia repair: incidence of elective and emergency surgery, readmission and mortality. Int J Epidemiol. 1996;25:835–839. doi: 10.1093/ije/25.4.835. [DOI] [PubMed] [Google Scholar]
- 16.Sobol JB, Gershengorn HB, Wunsch H, Li G. The surgical Apgar score is strongly associated with intensive care unit admission after high-risk intraabdominal surgery. Anesthesia and analgesia. 2013;117:438–446. doi: 10.1213/ANE.0b013e31829180b7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yoo PS, Mulkeen AL, Frattini JC, Longo WE, Cha CH. Assessing risk factors for adverse outcomes in emergent colorectal surgery. Surg Oncol. 2006;15:85–89. doi: 10.1016/j.suronc.2006.08.002. [DOI] [PubMed] [Google Scholar]
- 18.Kwaan MR, Vogler SA, Sun MY, Sirany AM, Melton GB, Madoff RD, Rothenberger DA. Readmission after colorectal surgery is related to preoperative clinical conditions and major complications. Diseases of the colon and rectum. 2013;56:1087–1092. doi: 10.1097/DCR.0b013e31829aa758. [DOI] [PubMed] [Google Scholar]
- 19.Manilich E, Vogel JD, Kiran RP, Church JM, Seyidova-Khoshknabi D, Remzi FH. Key factors associated with postoperative complications in patients undergoing colorectal surgery. Diseases of the colon and rectum. 2013;56:64–71. doi: 10.1097/DCR.0b013e31827175f6. [DOI] [PubMed] [Google Scholar]
- 20.Coleman EA, Parry C, Chalmers S, Min SJ. The care transitions intervention: results of a randomized controlled trial. Arch Intern Med. 2006;166:1822–1828. doi: 10.1001/archinte.166.17.1822. [DOI] [PubMed] [Google Scholar]
- 21.Jack BW, Chetty VK, Anthony D, Greenwald JL, Sanchez GM, Johnson AE, Forsythe SR, O’Donnell JK, Paasche-Orlow MK, Manasseh C, et al. A reengineered hospital discharge program to decrease rehospitalization: a randomized trial. Ann Intern Med. 2009;150:178–187. doi: 10.7326/0003-4819-150-3-200902030-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hernandez AF, Greiner MA, Fonarow GC, Hammill BG, Heidenreich PA, Yancy CW, Peterson ED, Curtis LH. Relationship between early physician follow-up and 30-day readmission among Medicare beneficiaries hospitalized for heart failure. JAMA : the journal of the American Medical Association. 2010;303:1716–1722. doi: 10.1001/jama.2010.533. [DOI] [PubMed] [Google Scholar]
- 23.Showalter JW, Rafferty CM, Swallow NA, Dasilva KO, Chuang CH. Effect of standardized electronic discharge instructions on post-discharge hospital utilization. Journal of general internal medicine. 2011;26:718–723. doi: 10.1007/s11606-011-1712-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Grafft CA, McDonald FS, Ruud KL, Liesinger JT, Johnson MG, Naessens JM. Effect of hospital follow-up appointment on clinical event outcomes and mortality. Arch Intern Med. 2010;170:955–960. doi: 10.1001/archinternmed.2010.105. [DOI] [PubMed] [Google Scholar]
- 25.Jha AK, Orav EJ, Epstein AM. Public reporting of discharge planning and rates of readmissions. N Engl JMed. 2009;361:2637–2645. doi: 10.1056/NEJMsa0904859. [DOI] [PubMed] [Google Scholar]