Abstract
Tardive dyskinesia (TD) is a delayed and potentially irreversible motor complication arising in patients chronically exposed to antipsychotic drugs. As several modern (so-called atypical) antipsychotic drugs are common offenders, the widening clinical indications for prescription as well as exposure of vulnerable individuals, TD will remain a significant drug-induced unwanted side effect. In addition, the pathophysiology of TD remains elusive and therapeutics difficult. Based on rodent experiments, we have previously shown that the transcriptional factor Nur77 (also known as NGFI-B or Nr4a1) is induced in the striatum following antipsychotic drug exposure as part of a long-term neuroadaptive process. To confirm this, we exposed adult capuchin (Cebus apella) monkeys to prolonged treatments with haloperidol (median 18.5 months, N=11) or clozapine (median 6 months, N=6). Six untreated animals were used as controls. Six haloperidol-treated animals developed mild TD movements similar to those found in humans. No TD was observed in the clozapine group. Postmortem analysis of Nur77 expression measured by in situ hybridization revealed a stark contrast between the two drugs, as Nur77 mRNA levels in the caudate-putamen were strongly upregulated in animals exposed to haloperidol while spared following clozapine treatment. Interestingly, within the haloperidol-treated group, TD-free animals showed higher Nur77 expression in putamen subterritories compared to dyskinetic animals. This suggests that Nur77 expression might be associated with a reduced risk to TD in this experimental model and could provide a novel target for drug intervention.
Keywords: NGFI-B, Nr4a1, transcription factor, typical antipsychotic drug, clozapine, caudate nucleus, putamen, abnormal involuntary movements, monkey, in situ hybridization
Introduction
Tardive dyskinesia (TD) is a troublesome and potentially irreversible motor complication encompassing all persistent, abnormal, involuntary movements occurring in the setting of chronic therapy with dopamine receptor-blocking agents, such as antipsychotic drugs and metoclopramide (Kenney et al., 2008; Blanchet et al., 2012). The resulting movement disorder is most often stereotyped in nature and typically involves the orofacial musculature. As TD remains an elusive drug complication over 50 years since its initial description, it is not surprising that the treatment options available are non-specific and produce mixed results (van Harten & Tenback, 2011).
New generations of antipsychotic drugs such as clozapine and olanzapine are defined as drugs active in the treatment of schizophrenia but with a lesser propensity to induce motor symptoms (Miyamoto et al., 2005). Unfortunately, the early hope that second-generation (so-called atypical) antipsychotic drugs would afford a disappearance of TD has been challenged by a recent literature review, which reports that a proportion of one-third of patients chronically exposed to commonly used antipsychotic drugs such as risperidone and olanzapine still displays TD (Woods et al., 2010). In fact, the only atypical antipsychotic drug associated with a non significant induction of TD is clozapine (Tarsy & Baldessarini, 2006). The annual risk remains greater in older adults, particularly in those living with a dementing illness (Lee et al., 2005), and severe forms of TD still develop with the new antipsychotic drugs (de Leon, 2007). As a consequence of the persistence of TD in the community, combined with the aging of the population, and the enlarging spectrum of conditions for which antipsychotic drugs are prescribed (e.g., bipolar disorder, depression), TD will remain a significant problem in human pharmacotherapy. In addition, the results of recent large trials and meta-analyses have shown that there is no effectiveness or tolerability advantage when comparing the first and second generations of antipsychotic drugs (Rosenheck et al., 2003; Jones et al., 2006; Leucht et al., 2009; Peluso et al., 2012). Therefore, a better understanding of the molecular mechanisms leading to tardive motor complications may help to design antipsychotic drugs devoid of these untoward effects or develop more effective adjunct anti-dyskinetic agents.
It is well documented that typical antipsychotic drugs rapidly induce genes like c-fos, Zif268 and Nur77 (Nerve-growth factor Inducible gene B [NGFI-B], Nr4a1) in the rodent striatum, a key structure in the regulation of motor control (Herrera & Robertson, 1996; Herdegen & Leah, 1998; Lévesque & Rouillard, 2007). Nur77 is a transcription factor of the nuclear receptor family that is rapidly induced after treatment with typical antipsychotic drugs (D2 antagonists) (Beaudry et al., 2000; Maheux et al., 2005). Previous reports from our laboratory implicated Nur77 in a neuroadaptive response mounted against abnormal motor behaviors following typical antipsychotic drug exposure in rodents (reviewed in (Lévesque & Rouillard, 2007)). For example, Nur77 knockout mice not only showed spontaneous vacuous chewing movements (VCMs), a behavior that displays some similarities to human TD (Turrone et al., 2002; Blanchet et al., 2012), but also worsened haloperidol-induced VCMs compared to wild type mice (Ethier et al., 2004b). This suggests that neurochemical changes induced by genetic deletion of Nur77 might have recapitulated some susceptibility processes observed in TD. Nur77 can display a functional transcriptional activity through heterodimerization with Retinoid X Receptor (RXR) (Perlmann & Jansson, 1995). Interestingly, we have shown that retinoid drugs (called rexinoids) can modulate haloperidol-induced VCMs in wild-type mice, whereas rexinoids remained without effect in Nur77 knockout mice (Ethier et al., 2004b). This suggests that Nur77/RXR transcriptional complex might represent an interesting pharmacological target to reduce abnormal involuntary movements induced by antipsychotic drugs (Lévesque & Rouillard, 2007). In addition, Nur77 mRNA up-regulation is sustained during subchronic typical antipsychotic drug administration in rodents without apparent desensitization, suggesting that Nur77 not only participate in the initiation of a neuroadaptive signaling cascade, but also to more prolonged effects (Beaudry et al., 2000; Langlois et al., 2001).
We also recently showed that a single nucleotide polymorphism (SNP, rs2603751) located in the 3′-UTR (untranslated regulatory region) of the Nur77 mRNA displayed a nominal association with the risk of developing TD, as well as with TD intensity based on Abnormal Involuntary Movement Scale (AIMS) scores, in a group of schizophrenia patients (Novak et al., 2010).
In the present study, we chronically exposed Cebus apella monkeys to typical and atypical antipsychotic drugs in an attempt to associate TD induction and intensity of Nur77 mRNA levels in various parts of the monkey basal ganglia. The results indicate that Nur77 mRNA levels are upregulated within the haloperidol-treated group and TD-free animals showed higher Nur77 expression compared to dyskinetic animals.
Material and methods
Animals and treatments
Handling of primates proceeded in accordance to the National Institute of Health Guide for the Care and Use of Laboratory Animals. All procedures, including means to minimize discomfort, were approved by the Institutional Animal Care Committee of University of Montreal. Animals were housed separately in observation cages in a temperature-controlled room and exposed to a 12-hour light/dark cycle. They were fed once daily in the afternoon, and water was provided ad libitum. The number of animals was kept to a minimum, and all efforts were made to avoid animal stress and suffering.
Twenty-four adult female capuchin (Cebus apella) monkeys were used. All monkeys first underwent bilateral ovariectomy in order to reproduce the hormonal status and TD susceptibility of postmenopausal women (Yassa & Jeste, 1992). Twelve animals were injected on a weekly basis with a depot preparation of haloperidol decanoate (0.1–0.9 mg/kg, i.m.) for up to 36 months. A low dose was given initially and titrated upward, and the maintenance dose individually adjusted to prevent overt sedation, bradykinesia, or acute dystonic reaction. Benztropine i.m. was occasionally needed during the initial titration phase to stop prolonged dystonic reactions. The drug protocol was briefly suspended a few times to ensure that TD manifestations were not masked by parkinsonian features. During the last 3 weeks of exposure, the haloperidol group (N=11) was switched to an oral preparation (0.125–0.3 mg/kg, twice daily) given in a fruit within a dose range proposed previously (Gunne & Barany, 1979), the last dose being administered 3 hours prior to sacrifice, in order to lessen the variability in drug absorption and dopamine receptor blockade between animals prior to brain collecting. In our experience, such a brief oral drug switch has no impact on group allocation and TD intensity. A separate drug-exposed group of 6 animals received the atypical antipsychotic clozapine individually adjusted to tolerance, given twice daily (5–8 mg/kg/dose) in a fruit and treated 5 days a week for 6 months, until 3 hours prior to sacrifice (cumulative doses ranging from 600–960 mg/kg). Clozapine was chosen because it represents the best TD-sparing atypical antipsychotic drug (Woods et al., 2010). Six animals were left untreated as controls. One TD-free animal died unexpectedly 22 months after initiation of haloperidol exposure.
TD measure
The orofacial (forehead, lips, tongue, jaw), neck, trunk, and limb movements were scored along a primate equivalent of the Abnormal Involuntary Movements Scale (AIMS), with each body segment scored between 0–4 points from absent to severe TD, for a maximum score of 40 points. During drug exposure, the presence of TD was deemed unequivocal when it was persistent over time and when a minimum of two separate body segments scored at least 1 point, or a minimum of one body part scored at least 2 points. Motor rating took place over 15 min each hour for 4 consecutive hours in the morning in the fasting state, before administration of the antipsychotic drug dose, behind a one-way mirror, with the animals kept in their home cage. The final score used for each animal is the cumulative score obtained for all 4 observations.
Tissue preparations
Three hours after drug dosing, the animals were anesthetized with ketamine (15 mg/kg, i.m.) followed by pentobarbital (35 mg/kg, i.v.). After clamping the abdominal aorta, they were perfused intracardially with 3 liters of physiologic saline solution. The brains were then rapidly removed, immersed in 2-methylbutane at −50°C for 15 sec, and then kept frozen at −80°C. Hemisected brains were cut into coronal sections of 12 μm on a cryostat (−20°C). The slices were thaw-mounted onto SuperFrostPlus (Fisher Scientific Ltd, Nepean, ON, Canada) 75 × 50 mm slides and stored at −80°C until use.
Complementary RNA probe preparation and synthesis
In order to label Nur77 mRNA in monkey brain tissues, we have produced a complementary RNA (cRNA) probe from total RNA of human caudate-putamen tissues (Mahmoudi et al., 2009). The cRNA probe for Nur77 stems from an 814 bp (nucleotides 19 to 832) fragment of the full-length human cDNA (GeneBank accession no: NM002135) subcloned into pCRII/TOPO and linearized with Bam HI. The antisense probe was synthesized with a T7 RNA polymerase. Synthesis of the specific [35S]UTP-labeled cRNA probe for Nur77 was performed as previously described (Beaudry et al., 2000; Mahmoudi et al., 2009).
In situ hybridization procedure
In situ hybridization with tissue sections was done at 58°C overnight in a standard hybridization buffer containing 50% formamide (Mahmoudi et al., 2009). Tissue sections were then apposed against BiomaxMR (Kodak, New Haven, CT) radioactive sensitive films for 5 to 7 days. Quantification of the autoradiograms was performed using computerized analysis (ImageJ 1.45s software, Wayne Rasband, NIH). Digital brain images were taken using a Grayscale Digital Camera (Model CFW-1612M, Scion Corporation, Maryland, USA). Optical gray densities were transformed into nCi/g of tissue equivalent using standard curves generated with 14C-microscales (ARC 146A-14C standards, American Radiolabelled Chemicals Inc., St-Louis). Brain areas investigated included anterior and posterior parts of the caudate nucleus and putamen corresponding to Bregma 2.70 to 0.45 (anterior caudate-putamen) and Bregma −6.30 to −8.10 (posterior caudate-putamen) in the atlas of Paxinos, respectively (Paxinos, 2009). Anterior and posterior caudate-putamens have been subdivided into medial and lateral caudate (CM, CL), and dorsolateral (PDL), dorsomedial (PDM), ventrolateral (PVL) and ventromedial putamen (PVM). Average levels of labeling for each area were calculated from three adjacent brain sections of the same animals. Background intensities were taken in white matter tracts for each section and were subtracted from every measurement.
Statistical analysis
Statistical analysis was performed with Prism version 5.0 program (Graph Pad Software Inc. San Diego, CA, USA). All data were expressed as group means ± S.E.M. We performed a Shapiro-Wilk normality test to estimate if the data display a Gaussian distribution (normally distributed population). All data sets passed the normally test (with an α level of 0.05) indicating that no significant departure from normally can be assumed. Then, we proceeded to parametric statistical comparison of mRNA levels in controls, haloperidol- and clozapine-treated groups using a one-way analysis of variance (ANOVA). We first performed a test of homogeneity using Bartlett’s test, followed by a logarithmic transformation (when Bartlett’s test was significant) and finally applied a one-way ANOVA on transformed data. When the ANOVA revealed significant differences, a Tukey’s test was performed as post hoc analysis. Comparison between dyskinetic and non-dyskinetic haloperidol-treated animals was performed using an unpaired t-test with a two-tailed p value. Statistical significance was set at p < 0.05.
Results
Behavioral observations
The chronic haloperidol regimen proposed was well tolerated. Motor slowing, action tremor, and sedation were generally mild if present. Occasional acute dystonic reactions prior to TD induction occurred in 6 out of 12 animals, rapidly reversed with benztropine, and minimized by a reduction in antipsychotic drug dose. We feel this is advantageous to avoid interference with food intake, optimize general well-being, and facilitate TD rating. A total of 6 (4 with early dystonic reactions on record) capuchins treated with haloperidol developed lasting TD. The latency of onset of TD was variable, with a mean (±SD) of 19 (±12) months (median, 18.5 months; range 7–35 months), while the mean duration of drug exposure in the TD-free animals was 19 (±4.5) months (median, 17.5 months; range 16–27 months). The cumulative i.m. drug exposure (mg/kg) up to the onset of TD or the time of the last observation for the TD-free group was 34.3 (±37.9) and 41.5 (±16.4), respectively. The abnormal purposeless movements were similar to those found in humans and typically stereotyped in nature, at times admixed with mild dystonic features. Variable orofacial dyskinetic movements were seen in all but one animal, including forehead contractions, chewing movements, tongue protrusions, and lip retraction (Fig. 1). Neck rotations, brief back extension, and flexion/extension movements of the toes, were also seen. Upper limb involvement was rarely observed. The mean cumulative motor score of haloperidol-treated animals showing TD was 16.5 (±8.5) points. The orofacial scores accounted for 39% of the mean TD score for the whole group. In contrast, the chronic clozapine treatment was well tolerated and caused only mild behavioral changes such as a decrease in general activity, sedation, and hypersalivation. No acute dystonic reaction or TD was documented.
Figure 1.
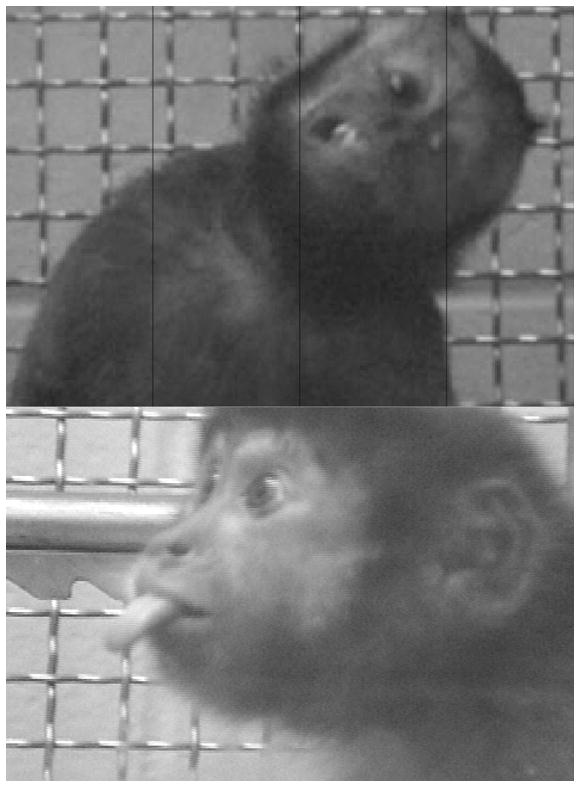
Representative photographs of tardive dyskinesia manifestations in two female capuchins displaying forehead muscle retraction, neck twisting and lip retraction (top panel), and tongue protrusion (lower panel). The figure was adapted with permission from (Blanchet et al., 2012).
Nur77 mRNA levels were selectively induced by haloperidol
Nur77 mRNA levels were evaluated using a specific complementary RNA probe from the human Nur77 DNA sequence. The hybridization signal was consistent with previous Nur77 mRNA reports in primates (Mahmoudi et al., 2009). The non-specific signal was very low (not shown). A relatively high basal Nur77 expression was observed in caudate-putamen nuclei (Fig. 2, Table 1), whereas very low basal levels of Nur77 were observed in nucleus accumbens (Acc), and external and internal segments of the globus pallidus (GPe and GPi, respectively) (Fig. 2). Haloperidol treatment strongly increased Nur77 mRNA levels in all caudate and putamen subterritorries in the anterior level (Fig. 3), while the typical antipsychotic drug significantly increase Nur77 mRNA levels in posterior lateral caudate, and posterior ventromedial and ventrolateral putamen (Fig. 4). Clozapine treatment remained without effect in all caudate-putamen areas (Figs. 3 and 4). Haloperidol also induced Nur77 expression in various cortical areas including frontal, insular, temporal and secondary somatosensory cortices (Fig. 2). In the nucleus accumbens, both haloperidol and clozapine tended to increase Nur77 (CTL = 0.4 ± 0.2; HAL = 9.6 ± 3.6 and CLZ = 11.2 ± 5.4 nCi/g of tissue), but significance was not reached because of the important variability inherent to such low signals.
Figure 2.
Representative autoradiograms showing the in situ hybridization signals obtained with the monkey radiolabeled Nur77 mRNA probe. Representative examples of monkey brain coronal sections taken at anterior A) and posterior B) levels of the caudate-putamen in control (CTL), haloperidol (HAL)- and clozapine (CLZ)-treated groups. The left panels illustrate schematic representations of caudate nucleus and putamen subdivision areas used for quantification. Abbreviations are: Acc, nucleus accumbens, lateral (CL) and medial (CM) portions of the caudate nucleus, dorsolateral (PDL), dorsomedial (PDM), ventrolateral (PVL) and ventromedial (PVM) portions of the putamen, GPe, external globus pallidus and GPi, internal globus pallidus.
Table 1.
Basal Nur77 mRNA levels in monkey caudate nucleus and putamen in control animals
|
Nur77 mRNA levels (nCi/g tissue)
|
||
|---|---|---|
| Anterior level | Posterior level | |
| Caudate nucleus | ||
| CM | 366 ± 38 | 149 ± 10 |
| CL | 325 ± 27 | 197 ± 10 |
| Putamen | ||
| PDM | 317 ± 47 | 174 ± 4 |
| PDL | 344 ± 37 | 149 ± 11 |
| PVM | 204 ± 21 | 111 ± 8 |
| PVL | 256 ± 13 | 110 ± 15 |
Data represent means ± SEM. Abbreviations: lateral (CL) and medial (CM) portions of the caudate nucleus as well as in dorsolateral (PDL), dorsomedial (PDM), ventrolateral (PVL) and ventromedial (PVM) portions of the putamen. These values were used to establish 100 % control values of Nur77 mRNA levels presented in Figures 3 and 4.
Figure 3.
Modulation of Nur77 mRNA levels in antipsychotic drug-treated monkeys in the anterior caudate-putamen. Nur77 mRNA levels were measured in control (CTL), haloperidol-(HAL) and clozapine (CLZ)-treated monkeys in the anterior caudate nucleus and putamen. Nur77 mRNA levels were evaluated in lateral (CL) and medial (CM) portions of the caudate nucleus as well as in dorsolateral (PDL), dorsomedial (PDM), ventrolateral (PVL) and ventromedial (PVM) portions of the putamen. Values are expressed in percent (%) of control values. Absolute values in nCi/g tissue of controls are presented in Table 1. Histogram bars represent means ± SEM (N=5–11 per group) (* p < 0.05, ** p < 0.01 and *** p < 0.001 vs CTL group). Inset graphs represent Nur77 mRNA levels in haloperidol-treated animals that have been subdivided into dyskinetic (Dysk) and non-dyskinetic (No-dysk) groups.
Figure 4.
Modulation of Nur77 mRNA levels in antipsychotic drug-treated monkeys in the posterior caudate-putamen. Nur77 mRNA levels were measured in control (CTL), haloperidol-(HAL) and clozapine (CLZ)-treated monkeys in the posterior caudate nucleus and putamen. Nur77 mRNA levels were evaluated in lateral (CL) and medial (CM) portions of the caudate nucleus as well as in dorsolateral (PDL), dorsomedial (PDM), ventrolateral (PVL) and ventromedial (PVM) portions of the putamen. Values are expressed in percent (%) of control values. Absolute values in nCi/g tissue of controls are presented in Table 1. Histogram bars represent means ± SEM (N=5–11 per group) (* p < 0.05 and ** p < 0.01 vs CTL group). Inset graphs represent Nur77 mRNA levels in haloperidol-treated animals that have been subdivided into dyskinetic (Dysk) and non-dyskinetic (No-dysk) groups (## p < 0.01 vs Dysk group).
Nur77 mRNA levels were selectively elevated in some putamen areas in animals not showing TD
We then performed a further analysis in which we separated TD from TD-free haloperidol-treated animals. No significant Nur77 mRNA levels difference between dyskinetic and non-dyskinetic haloperidol-treated animals was observed in the anterior caudate and putamen (Fig. 3, insets). However, animals not showing TD tended to have higher Nur77 mRNA levels compared to dyskinetic animals in anterior lateral putamen subterritories, but these statistical comparisons did not reach significance (Fig. 3, insets). Interestingly, the statistical analysis indicated that animals not showing TD had significant higher Nur77 mRNA levels compared to dyskinetic animals in posterior PDM, PVM and PVL putamen subterritories (Fig. 4, insets). According to the present results, it seems that the relationship between Nur77 expression and TD scores is all or none in nature instead of a linear relationship. However, the limited TD score range obtained in our sample and the relatively small number of animals in the TD group (5) might be responsible for the lack of linearity between TD scores and Nur77 expression in the present experiment.
Discussion
The present results confirm the sensitivity of Cebus apella monkeys to display TD during long-term antipsychotic drug exposure, half of our animals under chronic depot haloperidol developing TD after a median period of 18 months. The abnormal movements observed were similar to those found in humans and typically stereotyped in nature, without concomitant acute dystonic reaction. Clozapine caused no acute dystonic reaction or TD during the 6-month exposure, reflecting clinical experience (Woods et al., 2010). But, since clozapine exposure was shorter than haloperidol in the present experiment, the two drugs cannot be directly compared in terms of their liability to trigger TD. For the purpose of drug impregnation, we feel the oral clozapine dose selected (between 5–8 mg/kg/dose, twice daily) was sufficient and compared favorably to the chronic oral daily dosing protocol (5.2 mg/kg/day) previously administered to rhesus monkeys (Lidow & Goldman-Rakic, 1994). Single s.c. dosing at 2 mg/kg is not well tolerated in capuchins with TD and triggers an atypical acute dystonic reaction (Peacock & Gerlach, 1999). Further, single oral doses of 10 mg/kg have produced a marked decrease in locomotion in rhesus (Kumar et al., 2003).
Chronic treatments with typical antipsychotic drugs induced immediate-early genes such as stable forms of Fos (FosB/ΔFosB) or Nur77 in the striatum of rodents, whereas atypical antipsychotic drugs do not, suggesting that induction of immediate-early genes in the striatum is associated with the sustain extrapyramidal side effects of typical antipsychotic drugs (Beaudry et al., 2000; Rodriguez et al., 2001; Grande et al., 2004). Acute haloperidol as well as antagonist commonly used to treat nausea and associated with a metoclopramide, a 5-HT3/D2 high incidence of TD (Pasricha et al., 2006), can induce Fos immunoreactivity in monkey caudate-putamen (Deutch et al., 1996). However, no data is available on the modulation of immediate-early genes after prolonged antipsychotic drug exposure in primates. The possibility of functionally significant species differences is particularly important to consider since differences between rodents and primates in certain anatomical, pharmacological, and molecular features of forebrain dopamine system have been observed (Berger et al., 1991; Joel & Weiner, 2000). The present results show that caudate-putamen upregulation of Nur77 expression is selectively associated with the chronic administration of a typical antipsychotic drug (haloperidol), whereas the atypical antipsychotic drug clozapine administration spared Nur77 expression in the caudate-putamen. This nicely supports previous experiments in rodents that have shown a differential regulation of striatal Nur77 expression between typical and atypical antipsychotic drugs (Beaudry et al., 2000; Werme et al., 2000; Maheux et al., 2005), and indicates that the long-term modulation of Nur77 expression induced by antipsychotic drugs in rodents can be extended to primates. Although both haloperidol and clozapine tended to increase Nur77 mRNA levels in the nucleus accumbens, in accordance with rodent data (Beaudry et al., 2000; Werme et al., 2000; Maheux et al., 2005), basal Nur77 expression in the nucleus accumbens is much lower than in caudate-putamen in primates, whereas it has similar expression in both brain areas in rodents (Beaudry et al., 2000; Werme et al., 2000; Maheux et al., 2005).
In mice, we have shown that gene ablation of Nur77 (knockout) generated spontaneous vacuous chewing movements (VCMs) reminiscent of TD, and exacerbated haloperidol-induced VCMs (Ethier et al., 2004b). This suggests that Nur77 upregulation induced by this typical antipsychotic drug is associated with cellular neuroadaptative events that tend to protect against the development of involuntary abnormal movements. The upregulation of Nur77 in posterior putamen subterritories specifically observed in our TD-free monkeys is supportive of this view. Conceivably, this system is eventually overwhelmed during chronic drug exposure, leading to the delayed expression of motor complications associated with antipsychotic drugs. Alternatively, the regulation of Nur77 in central dopaminoceptive circuits under conditions of dopamine D2 receptor blockade could be genetically determined. We recently identified a single nucleotide polymorphism (SNP, rs2603751) located in the 3′-untranslated region (3′-UTR) of the Nur77 mRNA that displayed a nominal association with the risk of TD, as well as with the severity of TD based on AIMS scores in a group of schizophrenia patients (Novak et al., 2010). The non coding 3′-UTR of transcripts has been recognized to be important for the control of gene expression (Shim & Karin, 2002), raising the possibility that the SNP rs2603751 might alter Nur77 expression. Indeed, using reporter plasmids in HEK293 cells containing the Nur77 3′-UTR along with the native allele (T allele), or the mutated allele (C allele) associated with a higher risk of TD, we observed that the expression of the reporter gene is significantly reduced in the presence of the Nur77 3′-UTR containing the mutated allele (unpublished observation), suggesting that this SNP might be associated with a reduction of Nur77 expression. Thus, it is tempting to speculate that the induction of TD by a typical antipsychotic drug is linked with lower Nur77 expression and that individuals bearing this SNP have a higher susceptibility to develop TD, compared to those bearing the native allele. In order to support this claim, the presence of this Nur77 SNP correlated with high TD scores and low brain Nur77 expression levels must be sought in a large number of patients treated with antipsychotic drugs.
The absence of modulation of Nur77 expression in non-dyskinetic clozapine-treated monkeys may seem contradictory to haloperidol data, where non-dyskinetic animals showed higher Nur77 mRNA levels. However, the pharmacological profile of clozapine is much more complex than haloperidol. We have previously shown that the differential effect of typical and atypical antipsychotic drugs on Nur77 expression is at least in part explained by interactions of atypical drugs with serotonin 5-HT1A and 5-HT2A/C receptor subtypes, which prevent the induction of striatal Nur77 expression (Maheux et al., 2012). In other words, the resulting intracellular signaling pathways induced by certain atypical antipsychotic drugs, such as clozapine, which combines complex effects on dopamine, 5-HT, and many other receptor activities, do not trigger TD, thereby avoiding the need to switch on nuclear Nur77 transcription.
Interestingly, the relationship between Nur77 mRNA expression and TD was observed in medio-dorsal portions of the caudal putamen (Fig. 4), which display sensorimotor functionality relative to their cortical inputs in primates (Parent & Hazrati, 1995). In other areas sharing associative functionality, such as the caudate nucleus and anterior putamen (Parent & Hazrati, 1995), Nur77 mRNA levels were upregulated, but no relationship between Nur77 expression and TD was apparent. The animals exposed for several months to haloperidol developed TD mainly in the orofacial region, but other body segments, including neck and forelimbs, were also affected. Thus, although somatotopic organization of the primate basal ganglia associates ventral portions of the putamen with orofacial movements (Nambu, 2011), neuroanatomical alterations in brain dopamine circuits in TD could well vary from one animal to another.
In conclusion, the latency of onset, individual susceptibility, phenomenologic expression of the purposeless movements, and persistence of TD signs, make the non-human primate experimental TD model convincingly similar to the human condition. In this unique model, we confirmed the inverse relationship between striatal Nur77 expression and TD-like movements previously documented in rodents, supporting the validity of these observations to the human condition. We have previously shown that haloperidol-induced expression of neuromodulatory neuropeptides enkephalin and neurotensin is blunted in Nur77 knockout mice (Ethier et al., 2004a), suggesting that this transcription factor might contribute to the modulation of gene expression involved in the control of dopamine neurotransmission homeostasis. By promoting adaptive gene expression patterns, activation of transcriptional factors of the nuclear receptor family may provide an interesting novel approach for drug intervention in the prevention and palliation of TD.
Acknowledgments
The authors wish to thank Mrs. Marie-T. Parent, as well as the staff of the animal care facilities at Université de Montréal and Institut National de Recherche Scientifique (Armand-Frappier Institute, Laval, Canada), for their assistance and expertise during the animal experiments. This work was supported by a grant from the Canadian Institutes for Health Research (CIHR, MOP-81321). S.M. holds a doctoral fellowship from the “Fonds de Recherche du Québec en Santé (FRQS)”.
Abbreviations
- 3′-UTR
3′-untranslated regulatory region
- Acc
nucleus accumbens
- AIMS
abnormal involuntary movement scale
- CL
caudate lateral
- CM
caudate medial
- cRNA
complementary RNA
- GPe
external globus pallidus
- GPi
internal globus pallidus
- NGFI-B
Nerve-Growth Factor Inducible gene B
- PDL
putamen dorsolateral
- PDM
putamen dorsomedial
- PVL
putamen ventrolateral
- PVM
putamen ventromedial
- SNP
single nucleotide polymorphism
- TD
tardive dyskinesia
- VCM
vacuous chewing movement
Footnotes
Conflict of interest
The authors have no actual or potential conflict of interest including any financial, personal or other relationship with other people or organizations that could inappropriately influence, or be perceptive to influence the present work.
References
- Beaudry G, Langlois MC, Weppe I, Rouillard C, Lévesque D. Contrasting patterns and cellular specificity of transcriptional regulation of the nuclear receptor Nerve Growth Factor-Inducible B by haloperidol and clozapine in the rat forebrain. J Neurochem. 2000;75:1694–1702. doi: 10.1046/j.1471-4159.2000.0751694.x. [DOI] [PubMed] [Google Scholar]
- Berger B, Gaspar P, Verney C. Dopaminergic innervation of the cerebral cortex: unexpected differences between rodents and primates [published erratum appears in Trends Neurosci 1991 Mar;14(3):119] Trends Neurosci. 1991;14:21–27. doi: 10.1016/0166-2236(91)90179-x. [DOI] [PubMed] [Google Scholar]
- Blanchet PJ, Parent MT, Rompré PH, Lévesque D. Relevance of animal models to human tardive dyskinesia. Behav Brain Funct. 2012;8:12. doi: 10.1186/1744-9081-8-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Leon J. The effect of atypical versus typical antipsychotics on tardive dyskinesia: a naturalistic study. Eur Arch Psychiatry Clin Neurosci. 2007;257:169–172. doi: 10.1007/s00406-006-0705-z. [DOI] [PubMed] [Google Scholar]
- Deutch AY, Lewis DA, Whitehead RE, Elsworth JD, Iadarola MJ, Redmond JDE, Roth RH. Effects of D2 dopamine receptor antagonists on Fos protein expression in the striatal complex and entorhinal cortex of the nonhuman primate. Synapse. 1996;23:182–191. doi: 10.1002/(SICI)1098-2396(199607)23:3<182::AID-SYN7>3.0.CO;2-4. [DOI] [PubMed] [Google Scholar]
- Ethier I, Beaudry G, St-Hilaire M, Milbrandt J, Rouillard C, Lévesque D. The transcription factor NGFI-B (Nur77) and retinoids play a critical role in acute neuroleptic-induced extrapyramidal effect and striatal neuropeptide gene expression. Neuropsychopharmacology. 2004a;29:335–346. doi: 10.1038/sj.npp.1300318. [DOI] [PubMed] [Google Scholar]
- Ethier I, Kagechika H, Shudo K, Rouillard C, Lévesque D. Docosahexaenoic acid reduces haloperidol-induced dyskinesias in mice: Involvement of Nur77 and retinoid receptors. Biol Psychiatry. 2004b;56:522–526. doi: 10.1016/j.biopsych.2004.06.036. [DOI] [PubMed] [Google Scholar]
- Grande C, Zhu HW, Martin AB, Lee M, Ortiz O, Hiroi N, Moratalla R. Chronic treatment with atypical neuroleptics induces striosomal FosB/DeltaFosB expression in rats. Biol Psychiatry. 2004;55:457–463. doi: 10.1016/j.biopsych.2003.08.008. [DOI] [PubMed] [Google Scholar]
- Gunne LM, Barany S. A monitoring test for the liability of neuroleptic drugs to induce tardive dyskinesia. Psychopharmacology (Berl) 1979;63:195–198. doi: 10.1007/BF00433548. [DOI] [PubMed] [Google Scholar]
- Herdegen T, Leah JD. Inducible and constitutive transcription factors in the mammalian nervous system: control of gene expression by Jun, Fos and Krox, and CREB/ATF proteins. Brain Res Brain Res Rev. 1998;28:370–490. doi: 10.1016/s0165-0173(98)00018-6. [DOI] [PubMed] [Google Scholar]
- Herrera DG, Robertson HA. Activation of c-fos in the brain. Prog Neurobiol. 1996;50:83–107. doi: 10.1016/s0301-0082(96)00021-4. [DOI] [PubMed] [Google Scholar]
- Joel D, Weiner I. The connections of the dopaminergic system with the striatum in rats and primates: an analysis with respect to the functional and compartmental organization of the striatum. Neuroscience. 2000;96:451–474. doi: 10.1016/s0306-4522(99)00575-8. [DOI] [PubMed] [Google Scholar]
- Jones PB, Barnes TR, Davies L, Dunn G, Lloyd H, Hayhurst KP, Murray RM, Markwick A, Lewis SW. Randomized controlled trial of the effect on Quality of Life of second- vs first-generation antipsychotic drugs in schizophrenia: Cost Utility of the Latest Antipsychotic Drugs in Schizophrenia Study (CUtLASS 1) Arch Gen Psychiatry. 2006;63:1079–1087. doi: 10.1001/archpsyc.63.10.1079. [DOI] [PubMed] [Google Scholar]
- Kenney C, Hunter C, Davidson A, Jankovic J. Metoclopramide, an increasingly recognized cause of tardive dyskinesia. J Clin Pharmacol. 2008;48:379–384. doi: 10.1177/0091270007312258. [DOI] [PubMed] [Google Scholar]
- Kumar R, Palit G, Dhawan BN. Comparative behavioural effects of typical and atypical antipsychotic drugs in rhesus monkey. Eur J Pharmacol. 2003;462:133–138. doi: 10.1016/s0014-2999(02)02957-6. [DOI] [PubMed] [Google Scholar]
- Langlois MC, Beaudry G, Zekki H, Rouillard C, Lévesque D. Impact of antipsychotic drug administration on the expression of nuclear receptors in the neocortex and striatum of the rat brain. Neuroscience. 2001;106:117–128. doi: 10.1016/s0306-4522(01)00248-2. [DOI] [PubMed] [Google Scholar]
- Lee PE, Sykora K, Gill SS, Mamdani M, Marras C, Anderson G, Shulman KI, Stukel T, Normand SL, Rochon PA. Antipsychotic medications and drug-induced movement disorders other than parkinsonism: a population-based cohort study in older adults. J Am Geriatr Soc. 2005;53:1374–1379. doi: 10.1111/j.1532-5415.2005.53418.x. [DOI] [PubMed] [Google Scholar]
- Leucht S, Corves C, Arbter D, Engel RR, Li C, Davis JM. Second-generation versus first-generation antipsychotic drugs for schizophrenia: a meta-analysis. Lancet. 2009;373:31–41. doi: 10.1016/S0140-6736(08)61764-X. [DOI] [PubMed] [Google Scholar]
- Lévesque D, Rouillard C. Nur77 and retinoid X receptors: crucial factors in dopamine-related neuroadaptation. Trends Neurosci. 2007;30:22–30. doi: 10.1016/j.tins.2006.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lidow MS, Goldman-Rakic PS. A common action of clozapine, haloperidol, and remoxipride on D1- and D2-dopaminergic receptors in the primate cerebral cortex. Proc Natl Acad Sci USA. 1994;91:4353–4356. doi: 10.1073/pnas.91.10.4353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maheux J, Ethier I, Rouillard C, Lévesque D. Induction patterns of transcription factors of the Nur family (Nurr1, Nur77 and Nor-1) by typical and atypical antipsychotics in the mouse brain: implication for their mechanism of action. J Pharmacol Exp Ther. 2005;313:460–473. doi: 10.1124/jpet.104.080184. [DOI] [PubMed] [Google Scholar]
- Maheux J, Vuillier L, Mahfouz M, Rouillard C, Lévesque D. Modulation of haloperidol-induced patterns of the transcription factor Nur77 and Nor-1 expression by serotonergic and adrenergic drugs in the mouse brain. Int J Neuropsychopharmacol. 2012;15:509–521. doi: 10.1017/S1461145711000630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahmoudi S, Samadi P, Gilbert F, Ouattara B, Morissette M, Grégoire L, Rouillard C, Di Paolo T, Lévesque D. Nur77 mRNA levels and L-Dopa-induced dyskinesias in MPTP monkeys treated with docosahexaenoic acid. Neurobiol Dis. 2009;36:213–222. doi: 10.1016/j.nbd.2009.07.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miyamoto S, Duncan GE, Marx CE, Lieberman JA. Treatments for schizophrenia: a critical review of pharmacology and mechanisms of action of antipsychotic drugs. Mol Psychiatry. 2005;10:79–104. doi: 10.1038/sj.mp.4001556. [DOI] [PubMed] [Google Scholar]
- Nambu A. Somatotopic organization of the primate Basal Ganglia. Front Neuroanat. 2011;5:26. doi: 10.3389/fnana.2011.00026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Novak G, Gallo A, Zai CC, Meltzer HY, Lieberman JA, Potkin SG, Voineskos AN, Remington G, Kennedy JL, Lévesque D, Le Foll B. Association of the orphan nuclear receptor NR4A1 with tardive dyskinesia. Psychiatr Genet. 2010;20:39–43. doi: 10.1097/YPG.0b013e3283351221. [DOI] [PubMed] [Google Scholar]
- Parent A, Hazrati LN. Functional anatomy of the basal ganglia. I The cortico-basal ganglia-thalamo-cortical loop. Brain Res Brain Res Rev. 1995;20:91–127. doi: 10.1016/0165-0173(94)00007-c. [DOI] [PubMed] [Google Scholar]
- Pasricha PJ, Pehlivanov N, Sugumar A, Jankovic J. Drug Insight: from disturbed motility to disordered movement - a review of the clinical benefits and medicolegal risks of metoclopramide. Nat Clin Pract Gastroenterol Hepatol. 2006;3:138–148. doi: 10.1038/ncpgasthep0442. [DOI] [PubMed] [Google Scholar]
- Paxinos G. The rherus monkey brain in stereotaxic coordinates. Academic Press; Boston: 2009. [Google Scholar]
- Peacock L, Gerlach J. New and old antipsychotics versus clozapine in a monkey model: adverse effects and antiamphetamine effects. Psychopharmacology (Berl) 1999;144:189–197. doi: 10.1007/s002130050993. [DOI] [PubMed] [Google Scholar]
- Peluso MJ, Lewis SW, Barnes TR, Jones PB. Extrapyramidal motor side-effects of first- and second-generation antipsychotic drugs. Br J Psychiatry. 2012;200:387–392. doi: 10.1192/bjp.bp.111.101485. [DOI] [PubMed] [Google Scholar]
- Perlmann T, Jansson L. A novel pathway for vitamin A signaling mediated by RXR heterodimerization with NGFI-B and NURR1. Genes Dev. 1995;9:769–782. doi: 10.1101/gad.9.7.769. [DOI] [PubMed] [Google Scholar]
- Rodriguez JJ, Garcia DR, Nakabeppu Y, Pickel VM. FosB in rat striatum: normal regional distribution and enhanced expression after 6-month haloperidol administration. Synapse. 2001;39:122–132. doi: 10.1002/1098-2396(200102)39:2<122::AID-SYN3>3.0.CO;2-R. [DOI] [PubMed] [Google Scholar]
- Rosenheck R, Perlick D, Bingham S, Liu-Mares W, Collins J, Warren S, Leslie D, Allan E, Campbell EC, Caroff S, Corwin J, Davis L, Douyon R, Dunn L, Evans D, Frecska E, Grabowski J, Graeber D, Herz L, Kwon K, Lawson W, Mena F, Sheikh J, Smelson D, Smith-Gamble V. Effectiveness and cost of olanzapine and haloperidol in the treatment of schizophrenia: a randomized controlled trial. JAMA. 2003;290:2693–2702. doi: 10.1001/jama.290.20.2693. [DOI] [PubMed] [Google Scholar]
- Shim J, Karin M. The control of mRNA stability in response to extracellular stimuli. Mol Cells. 2002;14:323–331. [PubMed] [Google Scholar]
- Tarsy D, Baldessarini RJ. Epidemiology of tardive dyskinesia: is risk declining with modern antipsychotics? Mov Dis. 2006;21:589–598. doi: 10.1002/mds.20823. [DOI] [PubMed] [Google Scholar]
- Turrone P, Remington G, Nobrega JN. The vacuous chewing movement (VCM) model of tardive dyskinesia revisited: is there a relationship to dopamine D2 receptor occupancy? Neurosci Biobehav Rev. 2002;26:361–380. doi: 10.1016/s0149-7634(02)00008-8. [DOI] [PubMed] [Google Scholar]
- van Harten PN, Tenback DE. Tardive dyskinesia: clinical presentation and treatment. Int Rev Neurobiol. 2011;98:187–210. doi: 10.1016/B978-0-12-381328-2.00008-0. [DOI] [PubMed] [Google Scholar]
- Werme M, Ringholm A, Olson L, Brené S. Differential patterns of induction of NGFI-B, Nor1 and c-fos mRNAs in striatal subregions by haloperidol and clozapine. Brain Res. 2000;863:112–119. doi: 10.1016/s0006-8993(00)02109-0. [DOI] [PubMed] [Google Scholar]
- Woods SW, Morgenstern H, Saksa JR, Walsh BC, Sullivan MC, Money R, Hawkins KA, Gueorguieva RV, Glazer WM. Incidence of tardive dyskinesia with atypical versus conventional antipsychotic medications: a prospective cohort study. J Clin Psychiatry. 2010;71:463–474. doi: 10.4088/JCP.07m03890yel. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yassa R, Jeste DV. Gender differences in tardive dyskinesia: a critical review of the literature. Schizophr Bull. 1992;18:701–715. doi: 10.1093/schbul/18.4.701. [DOI] [PubMed] [Google Scholar]





