Abstract
Objective
The purposes of this study were to measure the orthodontic forces generated by thermoplastic aligners and investigate the possible influences of different activations for lingual bodily movements on orthodontic forces, and their attenuation.
Methods
Thermoplastic material of 1.0-mm in thickness was used to manufacture aligners for 0.2, 0.3, 0.4, 0.5, and 0.6 mm activations for lingual bodily movements of the maxillary central incisor. The orthodontic force in the lingual direction delivered by the thermoplastic aligners was measured using a micro-stress sensor system for the invisible orthodontic technique, and was monitored for 2 weeks.
Results
Orthodontic force increased with the amount of activation of the aligner in the initial measurements. The attenuation speed in the 0.6 mm group was faster than that of the other groups (p < 0.05). All aligners demonstrated rapid relaxation in the first 8 hours, which then decreased slowly and plateaued on day 4 or 5.
Conclusions
The amount of activation had a substantial influence on the orthodontic force imparted by the aligners. The results suggest that the activation of lingual bodily movement of the maxillary central incisor should not exceed 0.5 mm. The initial 4 or 5 days is important with respect to orthodontic treatment incorporating an aligner.
Keywords: Aligners, Orthodontic treatment, Orthodontic force, Activation amount
INTRODUCTION
The invisible orthodontic technique is considered one of the greatest developments in orthodontic clinical treatment technology in the 21st century, and since its inception there have been great improvements in new technologies such as three-dimensional (3D) reconstruction, modern engineering, and computer-aided design and computer-aided manufacturing (CAD/CAM). With advantages such as improved esthetics, comfort, and maintenance of oral hygiene,1,2,3 Invisalign (Align Technology, Inc., San Jose, CA, USA) has been used to treat over 2,000,000 orthodontic patients worldwide. Recent technical progress and clinical experiences have greatly extended the potential applications of invisible orthodontic techniques, to include conditions such as severe crowding, rotation, and open bite.4,5,6 However, the orthodontic performance of the invisible orthodontic technique remains inferior to that of the fixed appliance technique. Kassas et al.7 evaluated treatment outcomes of 31 Invisalign cases with mild to moderate malocclusions using the Model Grading System of the American Board of Orthodontics,8 and found that the occlusal contacts and occlusal relationships showed numerically negative changes. Rossini et al.9 evaluated the efficacy of tooth movement with removable aligners reported in 11 relevant articles, and concluded that the most accurate movement was upper molar distalization (88% accuracy), and the least accurate was extrusion (30%), followed by rotation (36%). It has been reported that 70–80% of Invisalign patients require case refinement, midcourse correction, or combined auxiliaries or fixed appliances.10
The invisible orthodontic technique uses a set of overlay aligners, which is different from the fixed appliance technique; thus, it has been a challenge to study the exact biomechanical mechanisms involved in each technique. The current study focused on material mechanics performance analysis. Kohda et al.11 used nanoindentation testing to obtain elastic modulus and hardness values, and reported a strong correlation between the mechanical properties of thermoplastic materials and the associated forces produced by aligners. Fang et al.12 reported that the residual stresses within five thermoplastic materials decreased over time, and that this process was significantly accelerated by immersion in a 37℃ water bath. Accurate measurement of the orthodontic forces generated by thermoplastic aligners is particularly important for the characterization of the biomechanical mechanisms involved in the invisible orthodontic technique.
Recently, with the development of micro-sensor technology, it has become possible to determine orthodontic force in real time. Rues et al.13 developed a true-scale orthodontic bracket with an integrated microelectronic stress sensor system for 3D force and moment measurements on individual teeth, and evaluated the measurement accuracy of the smart bracket on the basis of finite element simulations. To date, relatively few studies have investigated the force delivery system of this technology. A German research group14,15,16 has quantitatively investigated the rotation and tipping forces associated with a maxillary central incisor delivered by different thermoplastic appliances, and reported the effects from different materials and thicknesses. Kohda et al.11 measured the forces delivered by aligners for 0.5-mm and 1.0-mm activation for bodily tooth movement made from three thermoplastic materials with two different thicknesses, and compared the effects of mechanical properties, material thickness, and amount of activation on orthodontic forces. The possible influence of the amount of activation on orthodontic force, and its attenuation, is important to know when planning orthodontic treatment with an aligner system. However, no conclusive investigations of this have been reported to date.
In the current study we manufactured five sets of removable thermoplastic aligners designed for different amounts of lingual movement, and measured the corresponding orthodontic forces they exhibited in the lingual direction with a micro-stress sensor measurement system.17 The goal was to investigate the relationships between various amounts of activation of the aligner, the corresponding orthodontic forces, and the attenuation of those forces.
MATERIALS AND METHODS
Manufacturing the aligner
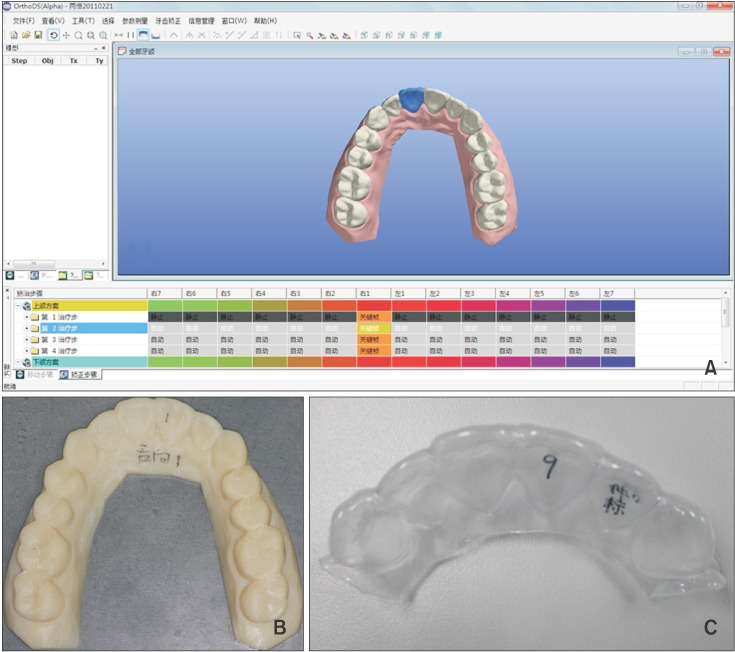
OrthoDS_D software ver. 4.4 (Wuxi Angel Align Biotechnology Co., Ltd., Wuxi, China) was used to design aligners with 0.2, 0.3, 0.4, 0.5, and 0.6 mm activations for lingual bodily movement of the maxillary right central incisor on a model twice the size of the digitized maxillary standard model. A 3D printer (Objet30 Pro; Objet Ltd., Rehovot, Israel) was used to transform the digital models into five corresponding photosensitive resin models. Five corresponding thermoplastic aligners were manufactured using the thermoforming technology with 1.0-mm thick thermoplastic materials (Erkodent Erich Kopp GmbH, Pfalzgrafenweiler, Germany). The production process is shown in Figure 1.
Figure 1. Production process for the thermoplastic aligners. A, OrthoDS_D software ver. 4.4 (Wuxi Angel Align Biotech nology Co., Ltd., Wuxi, China) was used to design different activation ranges for the lingual bodily movement of the maxillary right central incisor on a model twice the size of the digitized maxillary standard model. B, The resin models. C, The aligners.
Measurement and analysis of invisible orthodontic force in the lingual direction
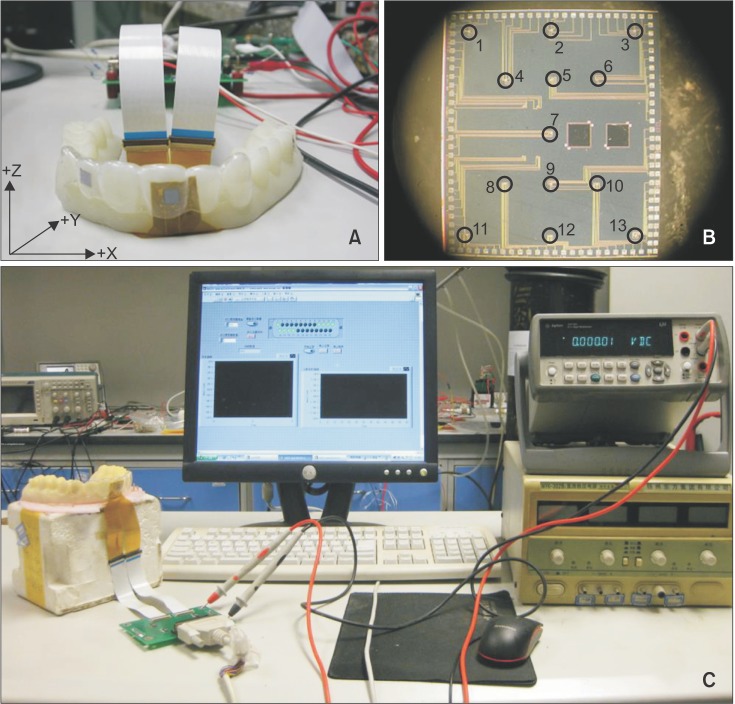
Our research group cooperated with the Institute of Microelectrics, Tsinghua University, China, to develop ultrasensitive piezoresistive stress sensors17,18,19 for orthodontic force measurement (Figure 2A). The stress sensor was a 0.05-mm thin 7 × 6 mm silicon chip consisting of 11 rosettes (cells) of metal-oxide-semiconductor field-effect-transistors (MOSFET) fabricated using integrated circuit technology (Figure 2B). When the sensor chip is subjected to external force or moment, the resulting deformation of the sensor chip changes the electrical parameters of the MOSFET.20,21 By measuring the electrical parameters of each MOSFET, the stresses they are subjected to can be obtained. Each MOSFET rosette consists of 4 MOSFETs, and can measure all the in-plane stress components at a given location. From all 11 MOSFET rosettes, the resulting three forces and three moments acting on the sensor chip can be calculated using reverse engineering.17 When the sensor chip is firmly bonded to a tooth, the sensor chip experiences the same deformation as the tooth surfaces as a result of the force and the moment applied to the tooth by the invisible aligner. Through the electrical signal of the MOSFETs, the stress and thus the deformation of the sensor chip can be measured. Prior to loading the aligner, known forces are applied to the tooth and the fitting coefficients correlating the measured stresses and the known forces are obtained. This establishes an inverse algorithm to express the external force as a function of the measured stresses. Finally, by using the fitting coefficients, the orthodontic forces induced by the invisible aligner are reconstructed from the measured stresses. Before loading the invisible aligner and measuring the orthodontic forces, we conducted 3D mechanical calibration on the chip. The results revealed that the mean calibration errors of the X, Y, and Z axes were within the range of engineering error.17
Figure 2. The orthodontic force generated by the thermoplastic aligners was measured using a micro-stress sensor measurement system for invisible orthodontic techniques. A, The micro-stress sensor measurement system. B, The standard resin model with invisible aligner and the sensor chip bonded on the tooth surface and connected with flexible cables. C, A photograph of the stress sensor.
The micro-stress sensor measurement system (Figure 2C) was connected and the five sets of aligners were successively placed on the model of the force measuring system. The orthodontic forces in the lingual direction generated by different aligners were measured and recorded. To compare the differences between the five activation amounts, residual orthodontic force percentiles were analyzed with the statistical software PASW Statistics ver. 17.0 (IBM Co., Armonk, NY, USA). Repeated-measures analysis of variance (ANOVA), the independent t-test, one-way ANOVA, and Bonferroni's test were performed to detect statistically significant differences. The significance level was set at p < 0.05.
Monitoring the attenuation of orthodontic force
We measured the orthodontic force generated by the aligners using a micro-stress sensor measurement system at 0, 1, 2, 3, 4, 5, 6, 7, and 8 hours, and at 1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, and 14 days. For each group, the percentage of residual orthodontic force was calculated as (Nn/N0) × 100, where Nn is the residual orthodontic force value at time Tn, and N0 is the initial orthodontic force value.
RESULTS
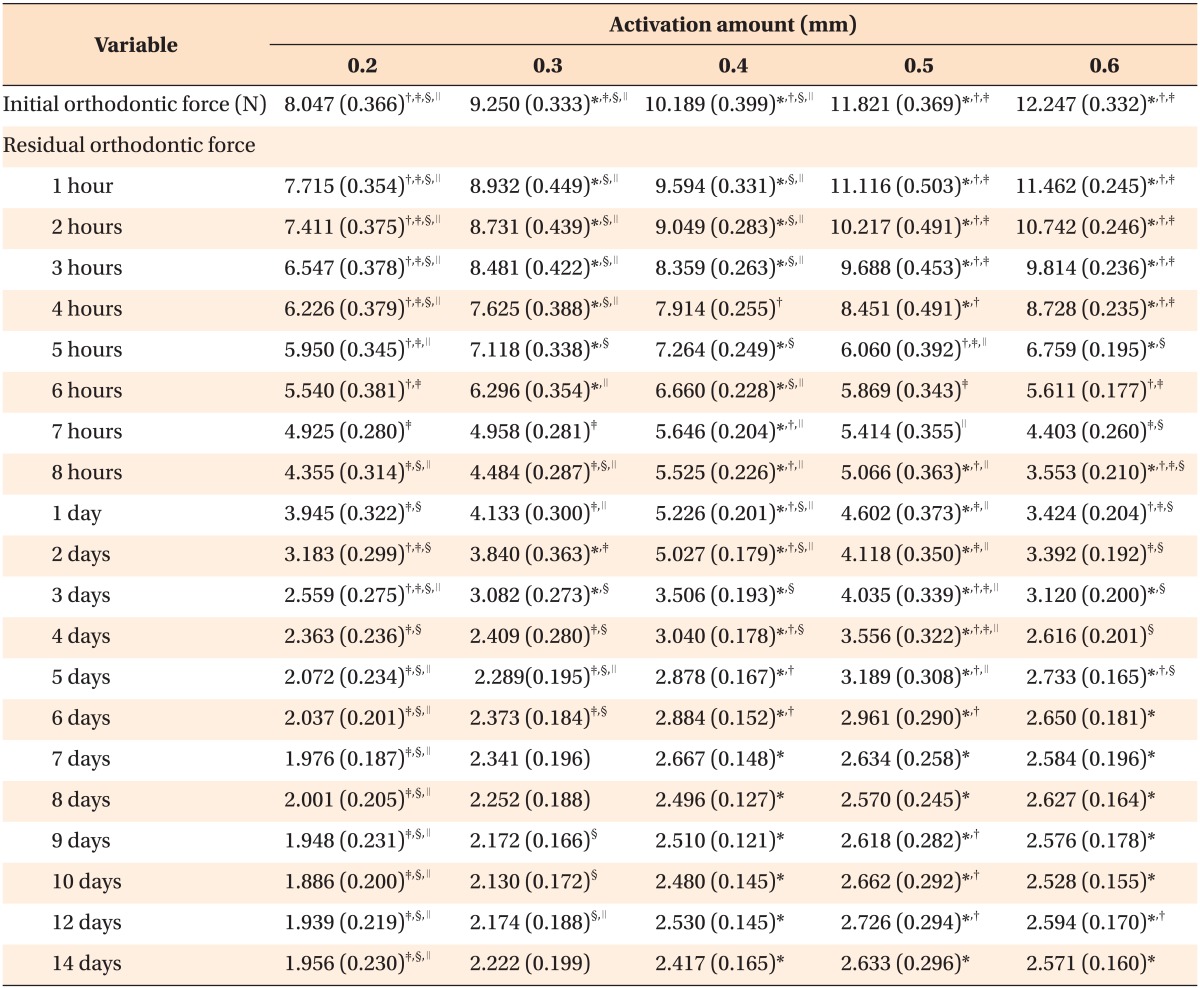
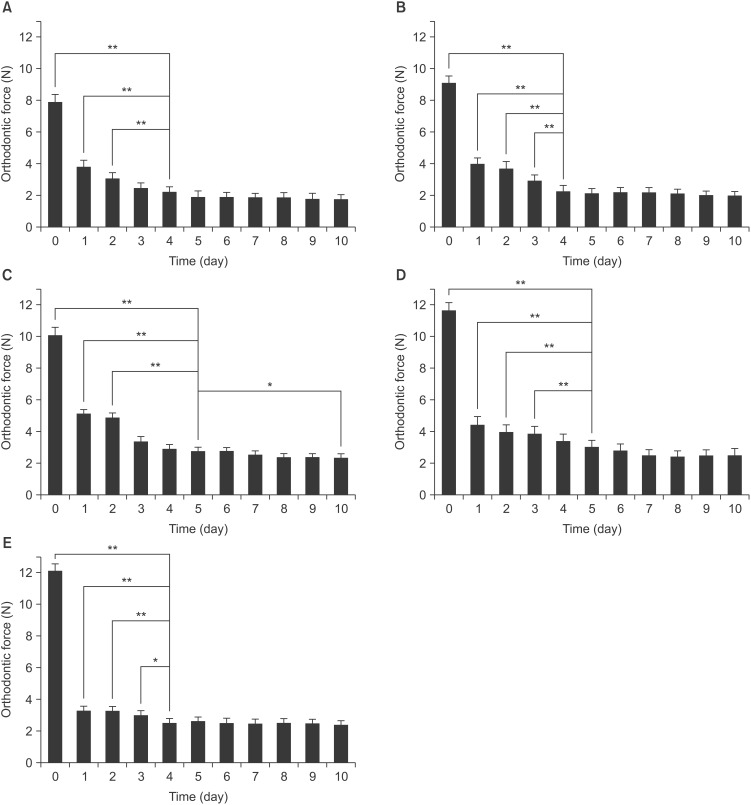
The orthodontic forces in the lingual direction generated by the five sets of lingual movement aligners and the statistical analysis results are shown in Table 1. The orthodontic force increased with the amount of activation of the aligner in the initial measurement. However, there was no statistically significant difference (p > 0.05) between the orthodontic force of the 0.5 mm group and the 0.6 mm group. All aligners exhibited time-dependent force attenuation behavior. The orthodontic force of the 0.6 mm group was significantly lower than that of the 0.5 mm group from 7 hours—5 days, the 0.4 mm group from 7 hours—5 days, the 0.3 mm group from 6 hours—1 day except for at 7 hours, and the 0.2 mm group at 8 hours (p < 0.05). Figure 3 shows orthodontic force relaxation curves. In the first 8 hours, the attenuation speeds of the 0.2, 0.3, and 0.4 mm groups were slower than those of the 0.5 and 0.6 mm groups (p < 0.01). From 1–14 days the attenuation speed of the 0.6 mm group was faster than those of the other groups (p < 0.05). There were no statistically significant differences between the 0.2, 0.3, 0.4, and 0.5 mm groups. As shown in Figure 4, all aligners demonstrated rapid relaxation during the first day, which decreased slowly and plateaued on day 4 or 5. There was no statistically significant difference between days 4 and 5, or any of the subsequent days (p > 0.05).
Table 1. Comparisons of the initial and residual orthodontic forces of the five sets of lingual movement aligners.
Significantly different from the 0.2 mm group*, from the 0.3 mm group†, from the 0.4 mm group‡, from the 0.5 mm group§, and from the 0.6 mm group∥ at the same time-point (Bonferroni's test; p < 0.05).
Figure 3. Orthodontic force relaxation curves for the five sets of lingual movement aligners.
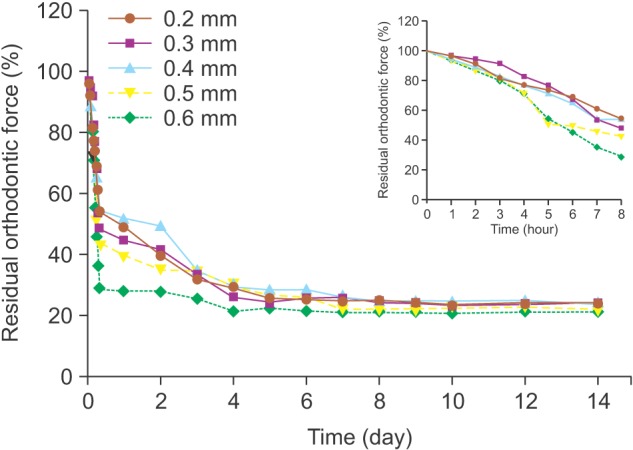
Figure 4. Mean forces of the thermoplastic aligners, with standard deviations. A, There were no statistically significant differences between day 4 and any of the subsequent days as determined by Bonferroni's test (p > 0.05) in the 0.2 mm group. B, There were no statistically significant differences between day 4 and any of the subsequent days as determined by Bonferroni's test (p > 0.05) in the 0.3 mm group. C, There were no statistically significant differences between day 5 and any of the subsequent days except days 10 and 14, as determined by Bonferroni's test (p > 0.05) in the 0.4 mm group. D, There were no statistically significant differences between day 5 and any of the subsequent days as determined by Bonferroni's test (p > 0.05) in the 0.5 mm group. E, There were no statistically significant differences between day 4 and the subsequent days as determined by Bonferroni's test (p > 0.05) in the 0.6 mm group.
*p < 0.05, **p < 0.01; Bonferroni's test.
DISCUSSION
Align Technology (San Jose, CA, USA) recommends an activation of 0.25–0.33 mm for each tooth,22 while DENTSPLY Raintree Essix (York, PA, USA) suggests 0.50–1.00 mm.23 In the present study, aligners with 0.2, 0.3, 0.4, 0.5, and 0.6-mm activations for lingual bodily movement of the maxillary central incisor were manufactured. We found that the orthodontic force in the lingual direction generated by the aligners increased as the amount of activation of the aligner increased. When the results were compared in pairs, there were significant differences (p < 0.01) between the orthodontic forces generated by most pairs of aligners, demonstrating that the amount of activation of the aligner was an important factor affecting invisible orthodontic force. However, the difference in orthodontic force between the 0.5 mm and 0.6 mm groups was not statistically significant (p > 0.05), probably because the design of the 0.6 mm aligner was excessive and caused plastic deformation of the aligner material; thus, it does not accurately reflect the influence of the different amount of activation on orthodontic force.
When loaded with appropriate orthodontic forces, teeth would move fast with only the slightest harm to the periodontal support. Barbagallo et al.24 measured the orthodontic force of 0.8-mm thick thermoplastic aligners with 0.5 mm activation of tooth movement, and reported that the initial orthodontic force was 5.12 N. Hahn et al.14 reported that the orthodontic force of 0.8-mm thick aligners with 0.151 mm activation was 2.38–3.14 N. In the current study, the periodontal ligament could not be simulated in the resin model. The periodontal ligament is composed of a kind of viscoelastic material with a thickness of 0.15–0.38 mm. The orthodontic force compresses the periodontal ligament, leading to a series of biological effects. In the current study, the invisible orthodontic forces were greater than the optimal force (0.75–1.25 N) for bodily movement of teeth, as suggested by Proffit and Fields.25 This may be because the resin model used could not simulate the periodontal ligament and tissues.
There are some reports that thermoplastic material can be modified by prolonged exposure to heat, moisture, enzymes of the oral cavity, and abrasion of the aligner.26 Eliades and Bourauel27 discovered that there was an aging phenomenon associated with the thermoplastic aligner. They reported that over time the chewing load changes the crystalline state of the high polymer, and consequently the Vickers hardness of the aligner increases. In addition, due to preset activation the aligners produce elastic deformation when placed on the denture, and generate a resilience force against the teeth which could change the width of the periodontal ligament, slightly change tooth positions, and reduce orthodontic force.
The intra-oral environment could not be simulated in this study; particularly, the viscoelastic periodontal ligament. Therefore, we aimed to investigate the changes in the aligners' mechanical properties caused by internal stress. The results indicated that the aligners went through rapid relaxation in this laboratory study, and achieved a plateau of orthodontic force on day 4 or 5. Thus, the initial 4 or 5 days is important in orthodontic treatment involving an aligner.
The attenuations of aligners activated 0.6 mm movements were more obvious than the other aligners. At certain time-points, the orthodontic force of the 0.6 mm group was even lower than aligners with smaller amounts of activation. This might be because the greater activation exceeds the stress yield of the aligner material, causing plastic deformation of the aligner and a more rapid attenuation speed. Ralph28 examined the relationships between the amount of deformation of the periodontal ligament and load, in vitro. When the load reached 0.3 N the amount of deformation of the periodontal ligament was 31 µm, and when the load was increased to 0.6 N the amount of deformation was 41 µm. Yet, when the load was increased to 5 N, the amount of deformation was only 66 µm. The current study suggested, without considering the periodontal ligament, that the amount of activation should not exceed 0.5 mm for the lingual bodily movement of the maxillary central incisors, so that the thermoplastic aligners can release light and continuous orthodontic force, and maintain the greatest efficiency.
Our experimental results provide a reference for clinical treatment design. However, the experiments did not emulate the clinical situation, as the intra-oral environment and periodontal ligaments could not be simulated in this study. Further, the teeth could not change position with the orthodontic force delivered by the aligners. In addition, because our study was limited by the size and number of the stress sensors, the aligners only covered anterior teeth and the force could only be measured on one target tooth at a time. Further studies with smaller sensor sizes, and with each tooth connected to a sensor simultaneously are needed to obtain realtime measurements of the forces of related teeth. Accordingly, we will now focus on the development of a wireless and waterproof micro-stress sensor system, with a view to applying it in an in vivo study.
CONCLUSION
In this study, the influence of different activations for lingual bodily movements on orthodontic force and its attenuation was analyzed. The following conclusions can be drawn from the data. Firstly, the amount of activation had a substantial effect on the orthodontic forces generated by the thermoplastic aligners. Secondly, the aligners relaxed quickly in this laboratory study, especially those with an activation of 0.6 mm. The activation should not exceed 0.5 mm for the lingual bodily movement of maxillary central incisors. Lastly, the initial 4 or 5 days plays an important role in orthodontic treatments involving an aligner.
ACKNOWLEDGMENTS
We thank Mr. Zheyao Wang and Mr. Pai Zhao for their assistance with experiments.
Footnotes
This work was supported by the Beijing Municipal Science and Technology Commission, China (Grant No. 2011084) and the National Natural Science Foundation of China (NSFC grant No. 81100773 and 81271184).
The authors report no commercial, proprietary, or financial interest in the products or companies described in this article.
References
- 1.Rosvall MD, Fields HW, Ziuchkovski J, Rosenstiel SF, Johnston WM. Attractiveness, acceptability, and value of orthodontic appliances. Am J Orthod Dentofacial Orthop. 2009;135:276.e1–276.e12. doi: 10.1016/j.ajodo.2008.09.020. [DOI] [PubMed] [Google Scholar]
- 2.Fujiyama K, Honjo T, Suzuki M, Matsuoka S, Deguchi T. Analysis of pain level in cases treated with Invisalign aligner: comparison with fixed edgewise appliance therapy. Prog Orthod. 2014;15:64. doi: 10.1186/s40510-014-0064-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schaefer I, Braumann B. Halitosis, oral health and quality of life during treatment with Invisalign(®) and the effect of a low-dose chlorhexidine solution. J Orofac Orthop. 2010;71:430–441. doi: 10.1007/s00056-010-1040-6. [DOI] [PubMed] [Google Scholar]
- 4.Harnick DJ. Using clear aligner therapy to correct malocclusion with crowding and an open bite. Gen Dent. 2012;60:218–223. [PubMed] [Google Scholar]
- 5.Frongia G, Castroflorio T. Correction of severe tooth rotations using clear aligners: a case report. Aust Orthod J. 2012;28:245–249. [PubMed] [Google Scholar]
- 6.Giancotti A, Germano F, Muzzi F, Greco M. A miniscrew-supported intrusion auxiliary for openbite treatment with Invisalign. J Clin Orthod. 2014;48:348–358. [PubMed] [Google Scholar]
- 7.Kassas W, Al-Jewair T, Preston CB, Tabbaa S. Assessment of invisalign treatment outcomes using the ABO model grading system. J World Fed Orthod. 2013;2:e61–e64. [Google Scholar]
- 8.Casko JS, Vaden JL, Kokich VG, Damone J, James RD, Cangialosi TJ, et al. Objective grading system for dental casts and panoramic radiographs. American Board of Orthodontics. Am J Orthod Dentofacial Orthop. 1998;114:589–599. doi: 10.1016/s0889-5406(98)70179-9. [DOI] [PubMed] [Google Scholar]
- 9.Rossini G, Parrini S, Castroflorio T, Deregibus A, Debernardi CL. Efficacy of clear aligners in controlling orthodontic tooth movement: a systematic review. Angle Orthod. 2015;85:881–889. doi: 10.2319/061614-436.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sheridan JJ. The readers' corner. 2. What percentage of your patients are being treated with Invisalign appliances? J Clin Orthod. 2004;38:544–545. [PubMed] [Google Scholar]
- 11.Kohda N, Iijima M, Muguruma T, Brantley WA, Ahluwalia KS, Mizoguchi I. Effects of mechanical properties of thermoplastic materials on the initial force of thermoplastic appliances. Angle Orthod. 2013;83:476–483. doi: 10.2319/052512-432.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fang D, Zhang N, Chen H, Bai Y. Dynamic stress relaxation of orthodontic thermoplastic materials in a simulated oral environment. Dent Mater J. 2013;32:946–951. doi: 10.4012/dmj.2013-131. [DOI] [PubMed] [Google Scholar]
- 13.Rues S, Panchaphongsaphak B, Gieschke P, Paul O, Lapatki BG. An analysis of the measurement principle of smart brackets for 3D force and moment monitoring in orthodontics. J Biomech. 2011;44:1892–1900. doi: 10.1016/j.jbiomech.2011.04.029. [DOI] [PubMed] [Google Scholar]
- 14.Hahn W, Dathe H, Fialka-Fricke J, Fricke-Zech S, Zapf A, Kubein-Meesenburg D, et al. Influence of thermoplastic appliance thickness on the magnitude of force delivered to a maxillary central incisor during tipping. Am J Orthod Dentofacial Orthop. 2009;136:12.e1–12.e7. doi: 10.1016/j.ajodo.2008.12.015. [DOI] [PubMed] [Google Scholar]
- 15.Hahn W, Engelke B, Jung K, Dathe H, Fialka-Fricke J, Kubein-Meesenburg D, et al. Initial forces and moments delivered by removable thermoplastic appliances during rotation of an upper central incisor. Angle Orthod. 2010;80:239–246. doi: 10.2319/033009-181.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hahn W, Fialka-Fricke J, Dathe H, Fricke-Zech S, Zapf A, Gruber R, et al. Initial forces generated by three types of thermoplastic appliances on an upper central incisor during tipping. Eur J Orthod. 2009;31:625–631. doi: 10.1093/ejo/cjp047. [DOI] [PubMed] [Google Scholar]
- 17.Ren CC, Bai YX, Wang ZY, Zhang M. [Establishment of the micro-stress sensor measurement system for invisible aligner technique] Zhonghua Kou Qiang Yi Xue Za Zhi. 2011;46:600–603. Chinese. [PubMed] [Google Scholar]
- 18.Tian K, Wang ZY, Zhang M, Liu LT. Design, fabrication, and calibration of a piezoresistive stress sensor on SOI wafers for electronic packaging applications. IEEE Trans Comp Packag Tech. 2009;32:513–520. [Google Scholar]
- 19.Shi Y, Ren CC, Hao W, Zhang M, Bai YX, Wang ZY, et al. An ultra-thin piezoresistive stress sensor for measurement of tooth orthodontic force in Invisible aligners. IEEE Sens J. 2012;12:1090–1097. [Google Scholar]
- 20.Lapatki BG, Bartholomeyczik J, Ruther P, Jonas IE, Paul O. Smart bracket for multi-dimensional force and moment measurement. J Dent Res. 2007;86:73–78. doi: 10.1177/154405910708600112. [DOI] [PubMed] [Google Scholar]
- 21.Lapatki BG, Paul O. Smart brackets for 3D-force-moment measurements in orthodontic research and therapy - developmental status and prospects. J Orofac Orthop. 2007;68:377–396. doi: 10.1007/s00056-007-0728-8. [DOI] [PubMed] [Google Scholar]
- 22.Boyd RL, Miller RJ, Vlaskalic V. The Invisalign system in adult orthodontics: mild crowding and space closure case. J Clin Orthod. 2000;34:203–212. [Google Scholar]
- 23.Sheridan JJ, Ledoux W, McMinn R. Essix appliance: minor tooth movement with divots and windows. J Clin Orthod. 1994;28:659–663. [Google Scholar]
- 24.Barbagallo LJ, Shen G, Jones AS, Swain MV, Petocz P, Darendeliler MA. A novel pressure film approach for determining the force imparted by clear removable thermoplastic appliances. Ann Biomed Eng. 2008;36:335–341. doi: 10.1007/s10439-007-9424-5. [DOI] [PubMed] [Google Scholar]
- 25.Proffit WR, Fields HW. Contemporary orthodontics. 3rd ed. St. Louis: Mosby; 2000. pp. 341–358. [Google Scholar]
- 26.Kusy RP. Orthodontic biomaterials: from the past to the present. Angle Orthod. 2002;72:501–512. doi: 10.1043/0003-3219(2002)072<0501:OBFTPT>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 27.Eliades T, Bourauel C. Intraoral aging of orthodontic materials: the picture we miss and its clinical relevance. Am J Orthod Dentofacial Orthop. 2005;127:403–412. doi: 10.1016/j.ajodo.2004.09.015. [DOI] [PubMed] [Google Scholar]
- 28.Ralph WJ. Tensile behaviour of the periodontal ligament. J Periodontal Res. 1982;17:423–426. doi: 10.1111/j.1600-0765.1982.tb01172.x. [DOI] [PubMed] [Google Scholar]