Abstract
AIM: To compare the results after revision of primary vertical banded gastroplasty (Re-VBG) and conversion to sleeve gastrectomy (cSG) or gastric bypass (cRYGB).
METHODS: In this retrospective single-center study, all patients with a failed VBG who underwent revisional surgery were included. Medical charts were reviewed and additional postal questionnaires were sent to update follow-up. Weight loss, postoperative complications and long-term outcome were assessed.
RESULTS: A total 152 patients were included in this study, of which 21 underwent Re-VBG, 16 underwent cSG and 115 patients underwent cRYGB. Sixteen patients necessitated a second revisional procedure. No patients were lost-to-follow-up. Two patients deceased during the follow-up period, 23 patients did not return the questionnaire. Main reasons for revision were dysphagia/vomiting, weight regain and insufficient weight loss. Excess weight loss (%EWL) after Re-VBG, cSG and cRYGB was, respectively, 45%, 57% and 72%. Eighteen patients (11.8%) reported postoperative complications and 27% reported long-term complaints.
CONCLUSION: In terms of additional weight loss, postoperative complaints and reintervention rate, Roux-en-Y gastric bypass seems feasible as a revision for a failed VBG.
Keywords: Vertical banded gastroplasty, Conversion, Revision, Gastric bypass, Sleeve gastrectomy, Additional weight loss
Core tip: This study assesses the long-term outcome after revision of a failed vertical banded gastroplasty (VBG). This manuscript compares three types of revision: revision of the primary VBG, conversion to sleeve gastrectomy and conversion to Roux-en-Y gastric bypass. The main finding in this study is that in terms of additional weight loss, postoperative complaints and reintervention rate, Roux-en-Y gastric bypass seems feasible as a revision for a failed VBG.
INTRODUCTION
Obesity is a growing global problem, associated with morbidity, health care costs and even an increased mortality rate[1]. For the treatment of obesity, bariatric surgery is very effective in achieving significantly more long-term weight loss and an improved lifestyle compared with conventional therapy[2,3]. In 2011, over 340000 bariatric procedures were performed worldwide. Among those procedures, around 2300 procedures were a vertical banded gastroplasty (VBG), first described by Mason et al[4] and later altered by MacLean et al[5] and Buchwald et al[6]. Aim of this procedure was to establish a restriction on food intake with a small stomach pouch, without compromising passage of food through the entire gastro-intestinal tract and thereby avoiding malabsorption of nutrients and medication[7]. This procedure has shown in earlier reports to have good short-term results in terms of weight loss and reduction in comorbidities[8-11]. However, there are many studies reporting on the poor long-term results after VBG, showing a tendency for weight regain and other complications resulting in a high revision rate[12-14]. Various options are available for revisional surgery after VBG, such as revision of the VBG (Re-VBG), conversion to sleeve gastrectomy (cSG) and conversion to Roux-en-Y gastric bypass (cRYGB), in which Re-VBG appears to have the poorest outcome and cRYGB has the best short- and long-term results[15-19]. However, data on the comparison between the revisional options remains scarce.
Although VBG had been abandoned some years ago in the Netherlands, still a number of patients can be expected to return with complaints after VBG. In the current series, all three mentioned options for revision have been performed. The aim of this study is to compare the outcome after these revisional procedures.
MATERIALS AND METHODS
Methods
This is a single-center retrospective study. A total of 392 patients underwent primary VBG, between January 1998 and December 2008. Since 2009, VBG was not performed anymore. Only patients undergoing primary VBG at the current center were included to reduce heterogeneity. Medical charts as well as additional postal questionnaires were reviewed. Included parameters were patient’s characteristics, operative details of primary and secondary procedures, evolution of weight and comorbidities following both operations, findings at additional imaging, reason for revision, short-term complications and long-term complaints after revisional surgery. The postal questionnaire contained questions on weight and comorbidities, on complaints dysphagia, vitamin deficiencies and incisional hernia. In case of insufficient weight loss, weight regain or complaints and without participation the follow-up program, the patient was invited to the outpatients department. In case of non-response, patients received a phone call and when there was no response at all, the data of the latest visit at the outpatient clinic were used as final outcome.
Excess weight was defined as the difference between the weight before surgery and the highest healthy weight, which is at a body mass index (BMI) of 25 kg/m2. Total excess weight loss (%EWL) was defined as a percentage of the amount of excess weight lost after surgery, as described by Deitel et al[20] The weight before the primary VBG was used as baseline value to calculate %EWL.
Weight loss was categorized according to the criteria described by Reinhold et al[21] These criteria consider a bariatric procedure successful when an %EWL of at least 50% is achieved. Furthermore, change in BMI and % total body weight loss (TBWL) was calculated. The evolution of any present comorbidities was categorized in stable, improved (reduced amount of medication used and/or a lower setting of a Continuous Positive Airway Pressure-device), resolved (no treatment), worse and de novo.
Treatment
Before primary VBG, all patients underwent assessment at our outpatient clinic by a surgeon, a psychologist and a dietitian to consider whether or not they were qualified for a bariatric procedure according to the standard IFSO guidelines for bariatric surgery. There was no specific algorithm for choosing the operative technique if they were approved for a bariatric procedure. There was a tendency for the option of a gastric bypass in case of more comorbidities, otherwise a VBG was chosen at the time. All patients underwent Mason-MacLean VBG, a standard VBG first described by Mason et al[4] with transection of the vertical staple line as described by MacLean et al[5].
Follow-up for these patients consisted of one year guidance by a psychologist, dietician and surgeon. Thereafter, a GP continued care unless weight loss problems or complaints were an issue. In such case patients underwent an analysis by all three disciplines and/or by means of a stomach X-ray and/or a gastroscopy. If considered eligible for revision the options were a re-VBG, cSG or cRYGB.
The Re-VBG technique meant in essence one of the 2 following adjustments. If the pouch was too large, a reshaping of the pouch was performed. The other option was an adjustment of the primarily placed band at the end of the gastric pouch.
A cSG meant a division of the lower part of the stomach 6cm from the pylorus up to the transgastric window to remove the gastric fundus and part of the corpus and antrum[22]. All sleeve gastrectomies were performed using a 34-Fr intraluminal boogie and stapled by use of the Endo GIATM (Covidien, New Haven, CT, United States).
A cRYGB started with identification of the polytetrafluoroethylene (PTFE) band. Then the stomach was transected horizontally at the proximal side of the band. The band was removed in most cases. The pouch was resized with use of the endoscopic stapler up to the angle of His. Then, an end-to-side gastro-jejunostomy was constructed by a linear stapler and closed using PolysorbTM sutures before 2009 and V-LocTM sutures after 2009 (Covidien, Mansfield, MA, United States). The alimentary limb, measuring 150-180 cm, was pulled up in an antecolic position. Finally, a side-to-side jejuno-jejunostomy was constructed, also using a linear stapler and closing the defect again with either PolysorbTM or V-locTM sutures. Mostly, the procedure was finished by closing the mesenteric defects.
Statistical analysis
All data were collected retrospectively. Management and analysis as performed by using SPSS version 22, for Windows (SPSS Inc, Chicago, IL). Quantitative data are denoted as mean ± SD, whereas rates of complications and evolution on comorbidities are presented as a percentage. The student t test, linear regression analysis and logistic regression analysis were used to determine any significance of the observed differences among subgroups. Statistical significance was identified when the P value was less than 0.05. An odds ratio (OR) was provided when applicable and considered significant when OR (95%CI) ≠ 1. Summative figures and tables were used when necessary.
No ethical approval was required for this study.
RESULTS
Three hundred and ninety-two patients who underwent primary VBG were identified. According to the medical charts and questionnaires a total of 152 revisional procedures (38.7%) were performed between April 1999 and June 2014, of which six patients underwent revision in another hospital. Necessary data of these patients was retrieved. Furthermore, these six patients did complete the postal questionnaire, so they were included in the analysis, together with the rest of the study population. Baseline characteristics are shown in Table 1.
Table 1.
Baseline characteristics (n = 152)
| Re-VBG n = 21 (13.8%) Mean ± SD | cSG n = 16 (10.5%) Mean ± SD | cRYGB n = 115 (75.7%) Mean ± SD | P value | |
| Age (yr) | 42.3 ± 8.6 | 41.6 ± 11.4 | 43.0 ± 8.9 | 0.828 |
| Male:female | 5:16 | 3:13 | 19:96 | 0.674 |
| Body mass index before VBG (kg/m2) | 42.6 ± 5.4 | 43.6 ± 5.0 | 44.1 ± 4.9 | 0.445 |
| Preoperative comorbidities | ||||
| Type 2 diabetes mellitus (n) | 4 | 2 | 13 | 0.538 |
| Hypertension (n) | 4 | 2 | 25 | 0.79 |
| Dyslipidemia (n) | 0 | 3 | 11 | 0.111 |
| Sleep apnea (n) | 1 | 1 | 2 | 0.249 |
| Osteo-articular disease (n) | 5 | 0 | 9 | 0.038 |
| Patients with 1 or more comorbidity | 10 | 5 | 41 | 0.512 |
| Operative time (min) | 77.0 ± 39.2 | 100.6 ± 19.6 | 130.7 ± 47.3 | < 0.001 |
| Length of hospital stay (d) | 3.1 ± 2.9 | 3.8 ± 2.2 | 4.1 ± 5.8 | 0.761 |
| Interval between VBG and revision (mo) | 12.3 ± 10.7 | 30.7 ± 26.5 | 47.8 ± 34.8 | < 0.001 |
| Average %EWL after VBG (%) | 61.7 ± 27.0 | 38.7 ± 22.9 | 43.5 ± 25.0 | 0.007 |
Re-VBG: Revision of the vertical banded gastroplasty; cSG: Conversion to sleeve gastrectomy; cRYGB: Conversion to Roux-en-Y gastric bypass; VBG: Vertical banded gastroplasty; %EWL: Percentage of excess weight loss.
The initial 392 patients showed an average %EWL of 51.2% ± 27.4% and 54% of all known comorbidities were either improved or resolved. The resolved comorbidities were not taken into account in the current study. The patients necessitating revision showed a lower %EWL of 45.4% ± 25.8%, compared to those not necessitating revision (54.9% ± 27.7%, P = 0.001). At last follow-up, 58.4% (n = 229) of the total of 392 patients reported long-term complaints, which in 152 patients led to a revisional procedure.
Eighty-two point two percent of the current study population was female. Follow-up of patients necessitating second revision was taken into account until second revision. A total of 127 patients (83.6%) successfully completed last follow-up by either returning the postal questionnaire or answering the questions on the phone. This resulted in a mean follow-up after revisional surgery of 56.5 ± 37.9 mo. In total, 25 patients did not return the postal questionnaire and could not be reached despite repeated attempts. Of these 25 patients, two patients deceased during follow-up due to a cause unrelated to bariatric surgery. Of these patients, the unreturned questionnaires were considered as missing data and the data of last known follow-up was used as final outcome so patients could be included in the analysis.
Reasons for revision
Complaints leading to revisional surgery are shown in Table 2. Six patients have had their revisional procedure in another center and therefore the complaints remained unknown. A possible surgically technical cause for failure of the VBG was found in 54.2% of all patients in this study.
Table 2.
Complaints before revision (n = 152)
| Re-VBG n = 21 (n) | cSG n = 16 (n) | cRYGB n = 115 (n) | Total (%) | P value | |
| Vomiting/ dysphagia/food intolerance | 17 | 8 | 36 | 40.2 | < 0.001 |
| Weight regain | 1 | 4 | 42 | 30.8 | 0.007 |
| Insufficient weight loss | 3 | 4 | 25 | 21.1 | 0.665 |
| Unknown | 0 | 0 | 6 | 3.9 | 0.792 |
| Severe GERD | 0 | 0 | 4 | 2.6 | 1.000 |
| Decline comorbidities | 0 | 0 | 1 | 0.7 | 1.000 |
| Excessive weight loss | 0 | 0 | 1 | 0.7 | 1.000 |
Re-VBG: Revision of the vertical banded gastroplasty; cSG: Conversion to sleeve gastrectomy; cRYGB: Conversion to Roux-en-Y gastric bypass; GERD: Gastro esophageal reflux disease.
Additional tests, in this study a stomach X-ray and/or a gastroscopy, were performed for additional analysis when necessary. The three main technical problems in this study population were a wide outlet, allowing faster passage of food through the pouch (17.1%), pouch dilatation (15.8%) and outlet stenosis (9.9%). Other technical reasons for failure were band erosion (5.3%), band luxation (displacement of the PTFE-band from its original position) (2.0%), staple line dehiscence resulting in a fistula (2.7%), pouch rotation (0.7%) and band dehiscence (0.7%).
Intra- and post-operative complications
126 procedures (82.9%) were performed laparoscopically, 15 procedures (9.9%) had a primary open approach and 11 (7.2%) procedures were converted from a laparoscopic to an open approach. One conversion was due to an intra-operative gastro-intestinal perforation which could not be managed laparoscopically, the other procedures were converted because of an unacceptable laparoscopic overview due to extensive intra-abdominal adhesions. Only 2 intra-operative complications (1.4%) occurred during surgery, both being an iatrogenic gastro-intestinal perforation.
Complications in the 30-d postoperative period were seen in a combined total of 18 patients (11.8%). No complications were seen after revision of the primary VBG (0/21). After cSG, three complications were objectified (3/16 = 18.8%): One pneumonia, one patient suffering from persistent vomiting after surgery causing dehydration. No evident cause was found for the persistent vomiting. The third patient had an ileus. In the group of patients who underwent cRYGB, 15 complications were registered (15/115 = 13.0%). Reoperation was necessary in two out of three patients with bleeding and in all patients with anastomotic leakage (n = 3). All leakages were found at the gastro-jejunostomy. Other complications included intra-abdominal abscesses (n = 3), wound infection (n = 2), pneumonia (n = 1), urinary tract infection (n = 1), ileus (n = 1) and deep venous thrombosis (n = 1). The intra-abdominal abscesses all necessitated re-admission to the hospital for intravenous antibiotic treatment combined with either CT- or ultrasound-guided drainage. In total, eight patients were admitted for appropriate treatment of the complication, three patients did not necessitate readmission and seven complications occurred during primary admission. No significant difference was found in the total number of complications between the groups.
Weight loss and evolution of comorbidities
When not including the follow-up after any secondary revisional procedure, the mean total %EWL at last follow-up after primary revisional surgery was 66.4% ± 25.8%. In terms of change in BMI, this meant an average reduction of 12.5 ± 5.6 kg/m2. Mean TBWL was 28.1% ± 11.2%. When including the 16 patients that underwent a second revisional procedure, %EWL was 68.2% ± 26.4%. Change in BMI was 12.7 ± 5.4 kg/m2 and TBWL was 28.7% ± 11.1%.
At baseline, a total of 82 comorbidities were found amongst 56 patients. The separate improvement/resolution percentages for the three different procedures were 71.4%, 77.8% and 67.8% for respectively Re-VBG, cSG and cRYGB when considering each comorbidity as a separate entity. Figure 1 shows the improvement/resolution rates divided between the three groups. Table 3 shows the results after primary revisional surgery, stratified for each procedure.
Figure 1.
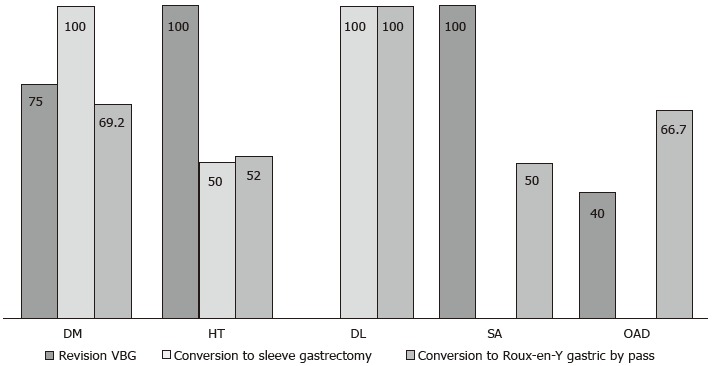
Improvement/resolution rates comorbidities. DM: Type 2 diabetes mellitus; HT: Hypertension; DL: Dyslipidemia; SA: Sleep apnea; OAD: Osteo-articular disease; VBG: Vertical banded gastroplasty.
Table 3.
Results after primary revision at last follow-up (n = 152)
| Re-VBG n = 21 Mean ± SD | cSG n = 16 Mean ± SD | cRYGB n = 115 Mean ± SD |
Corrected P value |
|||
| Re-VBG vs cSG | cRYGB vs Re-VBG | cRYGB vs cSG | ||||
| Follow-up (mo) | 39.1 ± 48.7 | 49.3 ± 17.6 | 50.0 ± 33.3 | |||
| Average %EWL after VBG (%) | 61.7 ± 27.0 | 38.7 ± 22.9 | 43.5 ± 25.0 | |||
| Additional %EWL | -14.6 ± 19.9 | 17.9 ± 32.7 | ||||
| Total %EWL (%) | 45.4 ± 25.5 | 56.6 ± 24.4 | 71.7 ± 23.8 | 0.614 | 0.006 | 0.025 |
| Total body weight loss (%) | 18.4 ± 11.1 | 24.1 ± 11.6 | 30.4 ± 10.1 | 0.049 | < 0.001 | 0.016 |
| Change body mass index (kg/m2) | 8.1 ± 5.8 | 10.8 ± 5.8 | 13.5 ± 5.1 | 0.119 | < 0.001 | 0.042 |
| Reinhold (%EWL > 50%) (%) | 47.6 | 56.3 | 82.6 | 0.7911 (0.211; 2.972) | 0.3421 (0.125; 0.934) | 0.2711 (0.090; 0.812) |
| Long-term complications (%) | 61.9 | 62.5 | 15.7 | 0.8331 (0.214; 3.244) | 10.1051 (3.600; 28.367) | 8.4211 (2.733; 25.950) |
| 2nd revisional procedure (n, %) | 10 (47.6%) | 5 (31.3%) | 1 (0.9%) | NA | NA | NA |
| Improvement/ resolution in patients with 1 or more comorbidities (%) | 80 (8/10) | 60 (3/5) | 92.7 (38/41) | 0.3751 (0.081; 1.738) | 1.2471 (0.476; 3.265) | 0.4681 (0.126; 1.740) |
Odds ratio (95%CI). Re-VBG: Revision of the vertical banded gastroplasty; cSG: Conversion to sleeve gastrectomy; cRYGB: Conversion to Roux-en-Y gastric bypass; %EWL: Excess weight loss; NA: Not available. P value is corrected for operative time, time between VBG and revision, osteo-articular disease and mean %EWL after VBG. No correction possible in logistic regression analysis due to limited events and group sizes. In case of a second revisional procedure, follow-up until second was taken into account.
Long-term complaints
At last follow-up after revisional surgery, 41 patients (27.0%) reported complaints, which in 16 cases necessitated a second revisional procedure. All long-term complaints are displayed in Table 4. In one patient after Re-VBG, complaints were caused by band erosion.
Table 4.
Long-term complaints after revision (n = 152)
| Re-VBG n = 21 (n) | cSG n = 16 (n) | cRYGB n = 115 (n) | Total (%) | |
| Vomiting/dysphagia/ food intolerance | 4 | 4 | 6 | 9.2 |
| Weight regain | 6 | 4 | 4 | 9.2 |
| Insufficient weight loss | 2 | 1 | 0 | 2.0 |
| Petersen’s hernia | NA | NA | 4 | 2.6 |
| Incisional hernia | 0 | 0 | 3 | 2.0 |
| Recurrent abdominal pain | 1 | 1 | 1 | 2.0 |
| None | 8 | 6 | 97 | 73.0 |
Re-VBG: Revision of the vertical banded gastroplasty; cSG: Conversion to sleeve gastrectomy; cRYGB: Conversion to Roux-en-Y gastric bypass; NA: Not available.
Subgroups based on reason for revision
Since the reason for revision may affect the outcome of the total weight loss, the evolution of comorbidities and potentially also the early postoperative course, additional analysis was performed. Patients undergoing revision for either weight regain or insufficient weight loss (WR/IWL) were compared to the other reasons given earlier in this manuscript. Results are shown in Table 5.
Table 5.
Subgroup analysis (n = 152) (weight regain/insufficient weight loss vs other complaints)
| WR/IWL n = 79 Mean ± SD | Other n = 73 Mean ± SD | P value | |
| Age (yr) | 41.6 ± 7.4 | 43.9 ± 10.7 | 0.121 |
| Male:female (n) | 13:66 | 14:59 | 0.661 |
| Body mass index before VBG (kg/m2) | 44.7 ± 5.0 | 42.8 ± 4.8 | 0.016 |
| Operative time (min) | 128.2 ± 46.3 | 109.7 ± 48.6 | 0.02 |
| Length of hospital stay (d) | 4.3 ± 6.8 | 3.4 ± 2.0 | 0.858 |
| Type of revision | |||
| Re-VBG | 4 | 17 | 0.004 |
| cSG | 8 | 8 | |
| cRYGB | 67 | 48 | |
| Average %EWL after VBG (%) | 31.3 ± 19.0 | 61.2 ± 23.1 | < 0.001 |
| Postoperative complications < 30 d (n, %) | 12 (15.2%) | 6 (8.2%) | 0.184 |
| Total %EWL (%) | 67.5 ± 23.7 | 65.2 ± 28.1 | 0.583 |
| Reinhold (%EWL > 50%) (%) | 79.7 | 74 | 0.398 |
| Long-term complications (%) | 22.8 | 28.8 | 0.399 |
| 2nd revisional procedure (n) | 5 | 11 | 0.079 |
| Improvement/resolution rate (%, n) | |||
| Type 2 diabetes mellitus | 90 (9/10) | 55.6 (5/9) | NA |
| Hypertension | 76.9 (10/13) | 44.4 (8/18) | NA |
| Dyslipidemia | 100 (9/9) | 100 (5/5) | NA |
| Sleep apnea | 0 (0/1) | 66.7 (2/3) | NA |
| Osteo-articular disease | 57.1 (4/7) | 57.1 (4/7) | NA |
WR: Weight regain; IWL: Insufficient weight loss; Re-VBG: Revision of the vertical banded gastroplasty; cSG: Conversion to sleeve gastrectomy; cRYGB: Conversion to Roux-en-Y gastric bypass; %EWL: Excess weight loss; NA: Not available.
Second revisional procedures
A total number of 16 patients underwent a second revisional procedure. 10 patients underwent conversion from a revised VBG to RYGB, five patients had their sleeve converted to RYGB. One patient necessitated revision due to persistent vomiting after RYGB. Additional analysis showed a stenosis of the gastrojejunostomy. The most common reasons for second revision were weight regain (43.7%) and DVFI (31.3%). Other reasons were insufficient weight loss (18.7%) and band erosion (6.3%).
DISCUSSION
The absolute number of performed bariatric procedures is still increasing and therefore the number of revisional procedures can be expected to rise as well. Combined with the known poor long-term outcome after VBG, this fact strengthens the belief that more revisional procedures of failed VBG can be expected in the future. This study is the first to report on the comparison between Re-VBG, cSG and cRYGB after failed primary VBG.
The revision rate of VBG was almost 39% (152 patients out of a total of 392 primary VBGs). The average %EWL after failed VBG was 45.4% ± 25.8% at last follow-up before revision. Patients who underwent Re-VBG had a noticeable better %EWL after VBG at baseline. This can be explained by the much shorter average interval of only 12 mo between the VBG and the revision, making follow-up too short to start noticing weight regain, a common reason for revision[17].
The main reasons for revision overall were similar to many other studies assessing either the long-term follow-up after VBG or the results after revision of the failed VBG[12,15,17,19,23]. However, there is a difference in the type of complaints leading to the different revisional procedures in this study. Furthermore, the number of procedures differed between the groups in this study. These facts can be explained by various reasons. First of all, the indication for Re-VBG was limited (mainly band-related problems). In the early years, when a patient had complaints of DVFI, a Re-VBG was performed, especially when the DVFI was caused by band erosion. As more reports became available over the years, showing that cRYGB is a better revisional option than Re-VBG, that latter procedure was abandoned at an early stage and cRYGB has proven to be a better option and has been for quite some years, explaining the low number of VBGs[15,16,18]. The last Re-VBG was performed in 2006. The second group, representing the cSGs, appears to have a more similar pattern of reasons for revision as seen in the cRYGB group, compared to the Re-VBG group. The size of the cSG group however is small, mainly due to early abandonment of this procedure, because there are very limited reports on the outcome of cSG over the last years and the larger experience with cRYGB, which had already proven to be a reliable procedure[16,17,22]. The last cSG after VBG was performed in January 2010. Since then, all revisional procedures after failed VBG were cRYGB.
The results in this study show that, although no early postoperative complications were seen in this group and the improvement/resolution rate of comorbidities is comparable with the other groups, Re-VBG is not the preferred revisional procedure after failed primary VBG. The reasons are a low total %EWL, high long-term complication rate and a high revision rate at long-term follow-up. Considering %EWL, this study actually showed an average decrease after Re-VBG, resulting in patients regaining nearly 15% of their initial excess weight. This result may be biased by the already available experience that cRYGB appeared superior to Re-VBG and the limited indication for Re-VBG[18].
The second group in this study was the cSGs. The long-term results after cSG are acceptable, with a significant better additional excess weight loss compared to Re-VBG and an improvement/resolution rate of comorbidities comparable with cRYGB. Although cSG appears to give a lower chance on postoperative complications compared to cRYGB, a significant higher long-term complication rate compared to cRYGB and a high second revision rate are showing the limits of this revisional procedure after failed primary VBG.
Although cSG appears to be superior compared to Re-VBG, this study confirms that cRYGB seems to be the best option of these three procedures. At last follow-up, patients showed an average %EWL of almost 72%, improvement or even resolution of comorbidities in 92.8% patients familiar with one or more obesity-related comorbidities. Furthermore, the chance of developing long-term complications after cRYGB is lower compared to the other two revisional procedures. In contrast of these good results, we noticed a high postoperative complication rate of 13.0% after cRYGB. However, this rate is comparable with many previously published results showing postoperative complication rates of 6.5%-25%[15,23-25]. In terms of %EWL, these results are comparable with previously reported data after both revisional RYGB for failed VBG as well as after primary RYGB[24-27]. The current good results may be affected by the used alimentary limb length of 150-180 cm, on the other hand, this seems unlikely, since previous studies have shown that a limb length of 150 cm did not produce a better %EWL compared to a limb length of 75-100 cm[28,29].
Considering the subgroup analysis performed to differentiate between weight loss related complaints and other complaints, an expected significant difference was found in terms of %EWL. Furthermore, a difference was found in the number of different revisional procedures between the two groups, which can be explained by the earlier reported difference in reason for revision between procedures. This may also explain the difference in operative time, since a Re-VBG takes a significant shorter time than a cRYGB. After revisional surgery, no significant differences were found in terms of %EWL, postoperative complications and number of long-term complications and number of performed 2nd revisional procedures.
The reported high revision rate and previously published unfavorable results underline the limits of this old restrictive procedure[12,13]. These rates also strengthen the expectation that a number of patients will necessitate revision in the future, since VBG is currently still performed as a primary procedure[6]. Although revisional surgery seems feasible, the high number of complications after revision should be taken into account.
These results should be interpreted with caution due to a number of limitations in this study. First of all, the unequal distribution of groups, mainly due to a bias caused by the center’s greater experience with cRYGB, thereby explaining the small number of Re-VBGs and cSGs. Furthermore, the retrospective design limits the reliability of the reported outcome. Since not all patients responded to our question to update the last known follow-up, a number of long-term complaints might have been missed, as well as potential revisional procedures performed in other hospitals. Not only the distribution between groups is unequal, also total time of follow-up is unequal, since Re-VBGs were performed only in the early and cRYGBs are still performed nowadays. The mean follow-up appears to be similar, but it should be kept in mind that Re-VBG showed a higher second revision rate as opposed to cSG and cRYGB and follow-up of the primary revision was taken into account until second revision. Keeping these limitations in mind, this study still suggests that Roux-en-Y gastric bypass is the superior choice for revisional surgery after failed primary VBG due to a good long-term %EWL, a high improvement rate of comorbidities, a low long-term complication rate and a low percentage of necessitated second revisional procedures.
In conclusion, in terms of additional weight loss, number of postoperative complaints and necessitation of a second revision, the Roux-en-Y gastric bypass seems feasible as a revision for a failed. Furthermore, the high number of complications after VBG and complications due to revisional procedures underline that VBG should be excluded as a primary option in bariatric surgery and other restrictive should be considered instead.
COMMENTS
Background
Vertical banded gastroplasty (VBG) was a popular restrictive bariatric procedure however, has been abandoned due to a high long-term complications rate in many cases leading to the necessitation of revisional surgery. As a number of these revisions can be expected, this study reports and compares the results after revision of the primary VBG (Re-VBG), conversion to sleeve gastrectomy (cSG) and conversion to Roux-en-Y gastric bypass (cRYGB). As the number of patients with a bariatric procedure rises annually, the number of failed procedures will rise as well, some necessitating surgical treatment (by either revision or conversion). It is good to know what can be expected in both the short term and the long term when it comes to complications, weight loss and other complaints.
Research frontiers
Research on the conversion or revision of failed VBG is limited to mainly results after conversion to Roux-en-Y gastric bypass. These articles show decent results, suggesting that Roux-en-Y gastric is a feasible option as revision of a failed VBG. Results on the comparison of different conversions after failed VBG are limited.
Innovations and breakthroughs
The current article is, by the authors’ knowledge, the first to compare different surgical options as treatment of failed VBG.
Applications
When confronted with failed VBG, either due to insufficient weight loss, weight regain or (other) physical complaints, conversion to Roux-en-Y gastric bypass appears to be more feasible compared to revision of the VBG or cSG.
Terminology
Re-VBG: Revision of a primary VBG; cSG: Conversion to sleeve gastrectomy; cRYGB: Conversion to Roux-en-Y gastric bypass.
Peer-review
The paper is acceptable and very interesting.
Footnotes
Institutional review board statement: This manuscript was approved by the Catharina Hospital Institutional Review Board, Eindhoven, the Netherlands.
Informed consent statement: All involved patients gave their informed consent (written or verbal, as appropriate) to have their data used anonymously for retrospective review prior to their primary bariatric surgery.
Conflict-of-interest statement: None of the authors have anything to disclose that might be a conflict of interest to this article.
Data sharing statement: Technical appendix, statistical code, and dataset available from the corresponding author at (email address or URL). Participants gave informed consent for data sharing and data was anonymized.
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Peer-review started: July 8, 2015
First decision: September 17, 2015
Article in press: January 11, 2016
P- Reviewer: Vilallonga R, Zhang ZM S- Editor: Ji FF L- Editor: A E- Editor: Wu HL
References
- 1.Selassie M, Sinha AC. The epidemiology and aetiology of obesity: a global challenge. Best Pract Res Clin Anaesthesiol. 2011;25:1–9. doi: 10.1016/j.bpa.2011.01.002. [DOI] [PubMed] [Google Scholar]
- 2.Sjöström L. Bariatric surgery and reduction in morbidity and mortality: experiences from the SOS study. Int J Obes (Lond) 2008;32 Suppl 7:S93–S97. doi: 10.1038/ijo.2008.244. [DOI] [PubMed] [Google Scholar]
- 3.Sjöström L, Lindroos AK, Peltonen M, Torgerson J, Bouchard C, Carlsson B, Dahlgren S, Larsson B, Narbro K, Sjöström CD, et al. Lifestyle, diabetes, and cardiovascular risk factors 10 years after bariatric surgery. N Engl J Med. 2004;351:2683–2693. doi: 10.1056/NEJMoa035622. [DOI] [PubMed] [Google Scholar]
- 4.Mason EE. Vertical banded gastroplasty for obesity. Arch Surg. 1982;117:701–706. doi: 10.1001/archsurg.1982.01380290147026. [DOI] [PubMed] [Google Scholar]
- 5.MacLean LD, Rhode BM, Forse RA. A gastroplasty that avoids stapling in continuity. Surgery. 1993;113:380–388. [PubMed] [Google Scholar]
- 6.Buchwald H, Oien DM. Metabolic/bariatric surgery worldwide 2011. Obes Surg. 2013;23:427–436. doi: 10.1007/s11695-012-0864-0. [DOI] [PubMed] [Google Scholar]
- 7.Mason EE, Doherty C, Cullen JJ, Scott D, Rodriguez EM, Maher JW. Vertical gastroplasty: evolution of vertical banded gastroplasty. World J Surg. 1998;22:919–924. doi: 10.1007/s002689900495. [DOI] [PubMed] [Google Scholar]
- 8.Lin YC, Chou FF, Chen SM, Wu CH. Vertical banded gastroplasty: a simple, effective and safe surgery for morbid obesity. Chang Gung Med J. 2003;26:754–760. [PubMed] [Google Scholar]
- 9.Morino M, Toppino M, Bonnet G, Rosa R, Garrone C. Laparoscopic vertical banded gastroplasty for morbid obesity. Assessment of efficacy. Surg Endosc. 2002;16:1566–1572. doi: 10.1007/s00464-001-9196-1. [DOI] [PubMed] [Google Scholar]
- 10.Wang W, Yu PJ, Lee YC, Wei PL, Lee WJ. Laparoscopic vertical banded gastroplasty: 5-year results. Obes Surg. 2005;15:1299–1303. doi: 10.1381/096089205774512519. [DOI] [PubMed] [Google Scholar]
- 11.Bekheit M, Katri K, Salam WN, Ezzat T, El Kayal el S. Rejecting the demise of vertical-banded gastroplasty: a long-term single-institute experience. Obes Surg. 2013;23:1604–1610. doi: 10.1007/s11695-013-0969-0. [DOI] [PubMed] [Google Scholar]
- 12.Marsk R, Jonas E, Gartzios H, Stockeld D, Granström L, Freedman J. High revision rates after laparoscopic vertical banded gastroplasty. Surg Obes Relat Dis. 2009;5:94–98. doi: 10.1016/j.soard.2008.05.011. [DOI] [PubMed] [Google Scholar]
- 13.Miller K, Pump A, Hell E. Vertical banded gastroplasty versus adjustable gastric banding: prospective long-term follow-up study. Surg Obes Relat Dis. 2007;3:84–90. doi: 10.1016/j.soard.2006.08.013. [DOI] [PubMed] [Google Scholar]
- 14.Schouten R, Wiryasaputra DC, van Dielen FM, van Gemert WG, Greve JW. Long-term results of bariatric restrictive procedures: a prospective study. Obes Surg. 2010;20:1617–1626. doi: 10.1007/s11695-010-0211-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cariani S, Agostinelli L, Leuratti L, Giorgini E, Biondi P, Amenta E. Bariatric Revisionary Surgery for Failed or Complicated Vertical Banded Gastroplasty (VBG): Comparison of VBG Reoperation (re-VBG) versus Roux-en-Y Gastric Bypass-on-VBG (RYGB-on-VBG) J Obes. 2010;2010:pii: 206249. doi: 10.1155/2010/206249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Iannelli A, Schneck AS, Ragot E, Liagre A, Anduze Y, Msika S, Gugenheim J. Laparoscopic sleeve gastrectomy as revisional procedure for failed gastric banding and vertical banded gastroplasty. Obes Surg. 2009;19:1216–1220. doi: 10.1007/s11695-009-9903-x. [DOI] [PubMed] [Google Scholar]
- 17.Suter M, Ralea S, Millo P, Allé JL. Laparoscopic Roux-en-Y Gastric bypass after failed vertical banded gastroplasty: a multicenter experience with 203 patients. Obes Surg. 2012;22:1554–1561. doi: 10.1007/s11695-012-0692-2. [DOI] [PubMed] [Google Scholar]
- 18.van Gemert WG, van Wersch MM, Greve JW, Soeters PB. Revisional surgery after failed vertical banded gastroplasty: restoration of vertical banded gastroplasty or conversion to gastric bypass. Obes Surg. 1998;8:21–28. doi: 10.1381/096089298765555006. [DOI] [PubMed] [Google Scholar]
- 19.Vasas P, Dillemans B, Van Cauwenberge S, De Visschere M, Vercauteren C. Short- and long-term outcomes of vertical banded gastroplasty converted to Roux-en-Y gastric bypass. Obes Surg. 2013;23:241–248. doi: 10.1007/s11695-012-0796-8. [DOI] [PubMed] [Google Scholar]
- 20.Deitel M, Greenstein RJ. Recommendations for reporting weight loss. Obes Surg. 2003;13:159–160. doi: 10.1381/096089203764467117. [DOI] [PubMed] [Google Scholar]
- 21.Reinhold RB. Critical analysis of long term weight loss following gastric bypass. Surg Gynecol Obstet. 1982;155:385–394. [PubMed] [Google Scholar]
- 22.Berende CA, de Zoete JP, Smulders JF, Nienhuijs SW. Laparoscopic sleeve gastrectomy feasible for bariatric revision surgery. Obes Surg. 2012;22:330–334. doi: 10.1007/s11695-011-0501-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schouten R, van Dielen FM, van Gemert WG, Greve JW. Conversion of vertical banded gastroplasty to Roux-en-Y gastric bypass results in restoration of the positive effect on weight loss and co-morbidities: evaluation of 101 patients. Obes Surg. 2007;17:622–630. doi: 10.1007/s11695-007-9106-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cordera F, Mai JL, Thompson GB, Sarr MG. Unsatisfactory weight loss after vertical banded gastroplasty: is conversion to Roux-en-Y gastric bypass successful? Surgery. 2004;136:731–737. doi: 10.1016/j.surg.2004.05.055. [DOI] [PubMed] [Google Scholar]
- 25.Iannelli A, Amato D, Addeo P, Buratti MS, Damhan M, Ben Amor I, Sejor E, Facchiano E, Gugenheim J. Laparoscopic conversion of vertical banded gastroplasty (Mason MacLean) into Roux-en-Y gastric bypass. Obes Surg. 2008;18:43–46. doi: 10.1007/s11695-007-9255-3. [DOI] [PubMed] [Google Scholar]
- 26.Edholm D, Näslund I, Anders Karlsson F, Rask E, Sundbom M. Twelve-year results for revisional gastric bypass after failed restrictive surgery in 131 patients. Surg Obes Relat Dis. 2014;10:44–48. doi: 10.1016/j.soard.2013.05.011. [DOI] [PubMed] [Google Scholar]
- 27.Mognol P, Chosidow D, Marmuse JP. Roux-en-Y gastric bypass after failed vertical banded gastroplasty. Obes Surg. 2007;17:1431–1434. doi: 10.1007/s11695-008-9419-9. [DOI] [PubMed] [Google Scholar]
- 28.Choban PS, Flancbaum L. The effect of Roux limb lengths on outcome after Roux-en-Y gastric bypass: a prospective, randomized clinical trial. Obes Surg. 2002;12:540–545. doi: 10.1381/096089202762252316. [DOI] [PubMed] [Google Scholar]
- 29.Stefanidis D, Kuwada TS, Gersin KS. The importance of the length of the limbs for gastric bypass patients--an evidence-based review. Obes Surg. 2011;21:119–124. doi: 10.1007/s11695-010-0239-3. [DOI] [PubMed] [Google Scholar]


