Abstract
Purpose of Review
The optimal strategy for assessing and preventing ventilator induced lung injury in the acute respiratory distress syndrome (ARDS) is controversial. Recent investigative efforts have focused on personalizing ventilator settings to individual respiratory mechanics. This review examines the strengths and weaknesses of using transpulmonary pressure measurements to guide ventilator management in ARDS.
Recent findings
Recent clinical studies suggest that adjusting ventilator settings based on transpulmonary pressure measurements is feasible, may improve oxygenation, and reduce ventilator induced lung injury
Summary
The measurement of transpulmonary pressure relies upon esophageal manometry, which requires the acceptance of several assumptions and potential errors. Notably, this includes the ability of localized esophageal pressures to represent global pleural pressure. Recent investigations demonstrated improved oxygenation in ARDS patients when PEEP was adjusted to target a specific end-inspiratory or end-expiratory transpulmonary pressures. However, there are different methods for estimating transpulmonary pressure and different goals for PEEP titration among recent studies. More research is needed to refine techniques for the estimation and utilization of transpulmonary pressure to guide ventilator settings in ARDS patients.
Keywords: acute respiratory distress syndrome, transpulmonary pressure, positive end-expiratory pressure, esophageal pressure
Introduction
Mechanical ventilation of patients with acute respiratory distress syndrome (ARDS) may contribute to morbidity and mortality by causing ventilator-induced lung injury (VILI). VILI may develop from excessive pressure and volume during inspiration causing injurious stretching (overdistention) in the lung parenchyma.(1, 2) Other mechanisms of VILI occur when there is too little airway pressure and volume during exhalation. This may cause cyclic alveolar recruitment and derecruitment with each tidal breath or excessive tension in alveolar septae at margins between aerated and non-aerated lung.(3, 4)
As mechanical ventilation is critical for survival for many ARDS patients, numerous efforts over the past 25 years have been directed towards minimizing VILI. Many lung protective strategies utilize the pressure at the airway opening (Pao) to monitor the potential for VILI. For example, the NIH ARDS Network lower tidal volume protocol utilizes inspiratory plateau pressure to guide adjustments to tidal volume.(5) As the limitations of airway pressure alone to assess VILI have become more evident, some have suggested that estimating transpulmonary pressure (PTP) would be a better approach to guide ventilator management. This review examines the considerations for and against the use of PTP measurements in ARDS.
Airway Pressure Can Be Misleading
The transmural pressure of the lung (Ptm,L), which represents stress in the lung parenchyma, is alveolar pressure minus pleural pressure, (Ptm,L = Palv – Ppl). During most static conditions, the alveolar transmural and transpulmonary pressure (PTP = Pao – Ppl) are the same, since alveolar and airway pressures should be in equilibrium in the absence of airflow. However, airway pressure alone can misrepresent the stress on lung parenchyma because several variables affect it independent of injurious mechanical forces in the lung. During mechanical ventilation, airway pressure distends the lung and the chest wall in series. Increases in chest wall elastance, as with chest wall edema, kyphoscoliosis, and intra-abdominal hypertension, are usually associated with increases in pleural pressure, as more force is necessary to distend the chest wall. Thus, depending on the pleural pressure, the same measured Pao can be associated with considerably different PTP and consequently have considerably different implications for injury to the lung. (FIGURE 1)
Figure 1.
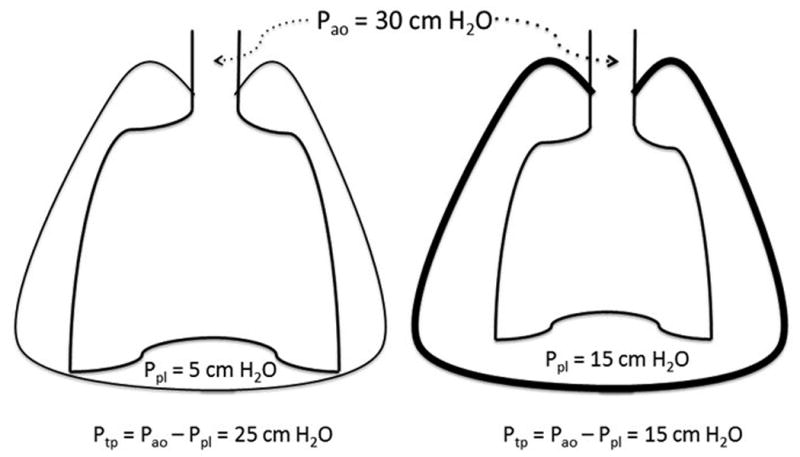
Airway pressure alone can be misleading. The same measured airway pressure can be associated with different transpulmonary pressures depending on the individual pleural pressures. These different transpulmonary pressures represent different levels of stress in the lung parenchyma which would be misinterpreted if only airway pressure is evaluated.
PTP to Monitor Potential for VILI
The use of PTP is a physiologically appealing approach to reduce VILI from high volumes and pressures during inspiration and low volumes and pressures during expiration. The injurious forces that cause alveolar overdistention are correlated directly with the peak inspiratory PTP, and the trauma from recurrent alveolar collapse and re-opening is related to the minimum end-expiratory PTP. Thus, knowledge of the PTP at end-inspiration and end-expiration, rather than airway pressure alone, could allow mechanical ventilator settings to be customized for each patient to minimize both causes of VILI.
Many intensive care physicians have adopted a strategy for mechanical ventilation in ARDS that utilizes tidal volumes of approximately 6ml/kg of predicted body weight and plateau pressures less than 30 cm H2O.(5) However, these measures may be insufficient to minimize VILI from overdistention in some patients because PTP and lung stress may exceed safe limits on these settings during inspiration.(6-8)
Moreover, there is still no consensus for how to select optimal PEEP levels. Although studies in animal models suggest that higher PEEP levels are beneficial (2, 3, 9), this was not been corroborated in three recent randomized clinical trials.(10-12) However, these three trials applied uniform strategies for higher PEEP in all patients randomized to receive higher PEEP, rather than tailoring PEEP levels to their specific lung and chest wall mechanics. If PTP was known, then tidal volumes and PEEP could be titrated to individuals' respiratory system mechanics to prevent alveolar overdistention or to promote lung recruitment and limit cyclic collapse. In this fashion, at the same measured Pao, patients with high chest wall elastance, high pleural pressures and low PTP could receive higher levels of PEEP; and patients with normal chest wall elastance, low pleural pressures and high PTP could receive lower tidal volumes or PEEP.(13) Thus, the use of PTP to guide ventilator management in ARDS is intellectually attractive. However, the limitations of utilizing PTP for this purpose must be understood before conclusions regarding its clinical value can be determined.
How to Measure Pleural Pressure
The major obstacle to measuring PTP is finding a practical and accurate method for estimating pleural pressure. Theoretically, pleural pressure can be measured by inserting a pressure monitoring device directly into the pleural space.(14) However, this technique is invasive and fraught with potential complications. Moreover, a device introduced into the pleural space alters the pressure in that space. The most commonly used method for estimating pleural pressure is esophageal manometry. Esophageal pressures (Pes) were frequently employed in studies of respiratory mechanics in the 1950-1960s.(14-17) An air-filled catheter with a long thin-walled balloon near its distal end is inserted through the nose and positioned into the lower third of the esophagus. Pes has been considered representative of average pleural pressure surrounding the lung in upright, healthy individuals.(15, 16, 18) There is skepticism, however, in extrapolating the validity of Pes as a surrogate for pleural pressure to mechanically ventilated supine patients with ARDS.(19, 20)
Sources of error in measuring pleural pressure
There are several sources of error in the estimation of pleural pressure from esophageal manometry. The pressure measured in the esophageal balloon may be affected by elastic recoil of the balloon, elastic recoil of the esophagus, esophageal muscle tone, and pressure transmitted from surrounding structures. (FIGURE 2) Because of gravitational forces, there is a vertical gradient of pleural pressure in both the upright and supine positions. Esophageal pressure correlates best with pleural pressure in the middle of this gravitational plane in either position, but the relationship between the esophageal and pleural pressure is inconsistent between different subjects.(14) Early studies also demonstrated significant variability in the relationship between esophageal and pleural pressures when subjects changed from the upright to supine position, probably because of cephalad movement of the diaphragm and the weight of the mediastinal contents.(14, 15, 18)
Figure 2.
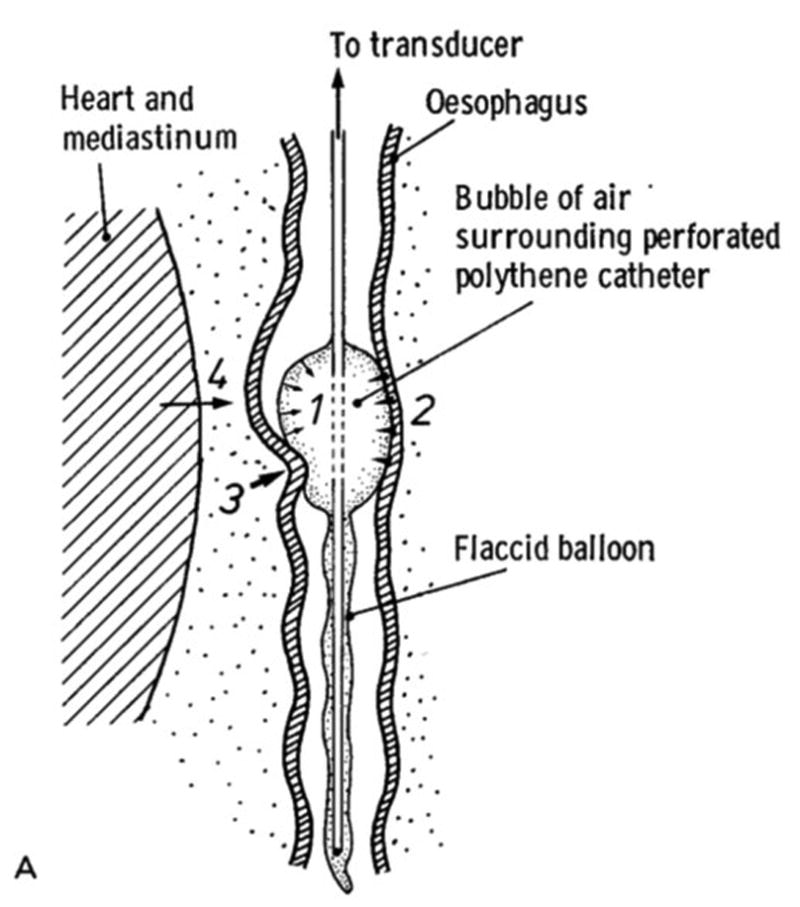
Sources of error in pleural pressure estimation by esophageal manometry. Esophageal Pressure may be affected by a) elastic recoil of the balloon; b) elastic recoil of the esophagus; c) active esophageal contractions; or d) transmitted pressure from surrounding structures. Reprinted with permission from Elsevier. (17)
Washko and colleagues assessed effects of body position change (erect to supine) in 10 healthy individuals and found that Pes consistently increased in the supine position.(21) They suggested that a constant correction factor of 3 cm H2O could be added to PTP, calculated from Pao – Pes, to account for the weight of the mediastinum and movement of the diaphragm in the supine position. However, there was substantial inter-individual variability of this correction factor (95% confidence interval -1 - +7 cm H2O), and it was obtained in normal individuals.(21) Variability may be considerably greater in patients with consolidated lungs, pleural effusions, cardiomegaly, and abdominal distention, introducing even more error into the estimation of PTP based on Pes.
Rather than using the direct measurement of Pes with an assumed correction factor, Gattinoni and colleagues proposed an elastance-derived calculation of pleural pressure. This allows the absolute value of esophageal pressure to be ignored, as the chest wall elastance is calculated from only the change in esophageal pressure from end-inspiration to end-expiration ( ). (22) Elastance of the respiratory system (Ers) is calculated from the change in plateau pressure minus PEEP divided by the tidal volume ( ). Finally, the pleural pressure is then estimated by calculating the fraction of airway pressure that distends the chest wall and thus is transmitted to the pleural space, . Assuming the influence of the mediastinum is constant throughout the respiratory cycle, no correction factor would be necessary.(23) However, an important assumption with the elastance-derived method is that Ppl is 0 when airway pressure is 0, which is seldom true. If true pleural pressure is higher or lower than 0 when airway pressure equals 0, the calculated pleural pressures with this technique will be under- or over-estimated, respectively. It should also be noted that the elastance-derived calculation measures expiratory Pes at PEEP rather than atmospheric pressure and assumes that changes in esophageal and airway pressure are linear during tidal ventilation or with changes in PEEP.(6) A recent study addressed this by measuring Pes with esophageal manometry when airway pressure was zero by disconnecting patients from ventilators and allowing them to exhale to atmospheric pressure.(24) The elastance-derived PTP had excellent correlation with that technique and does not require the patient to be disconnected from the ventilator. The investigators concluded that the elastance derived PTP could be used as a proxy for end-inspiratory stress with mechanical ventilation.(24)
Further assumptions must also be made with either calculation technique regarding the generalizability of the measured Pes to the surface pleural pressures surrounding the entire lung. Pelosi et al demonstrated that Pes accurately estimated pleural pressure in the middle lung zone in a canine model of ARDS.(25) However, Pes also overestimated pleural pressure in the nondependent regions of lung and underestimated it in the dependent regions of the lung.(25) In addition to the gravitational pleural pressure gradient, there may also be local variations of pleural pressure related to the resistance to parenchymal shape deformation in consolidated lung.(26, 27) Left lower lobe atelectasis is common in supine patients, presumably from localized increases in pleural pressure, and the esophageal catheter is typically in position closest to the left lower lobe. For these reasons, Pes may be an accurate surrogate for pleural pressure in a localized area of the lung but may not be a good representation for much of the aerated lung in other regions. In this fashion, using PTP to set PEEP or tidal volume may prevent lung collapse or promote recruitment in the area of the esophageal catheter, but it may actually promote derecruitment or overdistention injury in other areas of lung. The location of VILI may be shifted but not necessarily reduced.
PTP-guided Mechanical Ventilation
Despite these caveats, several studies have used PTP to adjust mechanical ventilation in patients with lung injury. In a small cohort of patients with severe H1N1-associated ARDS referred for ECMO, clinicians increased PEEP until the end-inspiratory PTP was 25 cm H2O, using the elastance method.(13) Approximately half of the patients substantially improved their arterial oxygenation and could then be managed with conventional ventilation without ECMO. Similar to the “open lung approach”(28), this strategy focuses on promoting lung recruitment while limiting overdistention injury by monitoring end-inspiratory lung stress. It is unclear, however, if it addresses the potential for VILI during expiration, as end-expiratory PTP is not evaluated.
Talmor and colleagues noted that the directly calculated PTP at end-expiration was often negative in patients with ARDS, suggesting that airway closure or flooding had prevented alveolar pressure from equilibrating with airway pressure.(29-31) Therefore, they suggested that PEEP should be adjusted to maintain a positive end-expiratory PTP to keep airways open at end-expiration, prevent derecruitment, and thus lower the risk of VILI.(31) They utilized the direct calculation method (PTP = Pao – Pes) to guide PEEP levels in 61 ARDS patients. (29-31) Patients were randomized to either a control group in which PEEP was set using the NIH ARDS Network PEEP/FiO2 table(5) or an experimental group in which PEEP was titrated to an end-expiratory PTP of 0-10 cm H2O while maintaining end-inspiratory PTP less than 25 cm H2O.(30) The study was terminated early after interim analyses demonstrated substantial improvements in the primary outcome of arterial oxygenation. It is not surprising that the higher PEEP levels used in the intervention group (18 vs 12 cm H2O) would lead to improved oxygenation, but there were also significant gains in respiratory system compliance, suggesting that there was greater lung recruitment in the group managed by PTP. The trial was not powered to compare mortality between the two groups, but there was a trend towards lower 28-day mortality in the PTP-guided group.(30) The same research group is now conducting a larger randomized trial in moderate-to-severe ARDS patients, comparing PTP-guided PEEP titration to a uniform higher PEEP strategy, with primary outcomes of ventilator free days and mortality.(32) Until results from further clinical trials demonstrate significant improvements in survival using PTP guided mechanical ventilation, there will continue to be reservations regarding its general applicability to this heterogeneous population.
Even when esophageal catheters are used to estimate Ppl, there remains substantial heterogeneity regarding the best method for calculating PTP and setting PEEP. As described, one approach utilizes directly calculated PTP to adjust PEEP to maintain end-expiratory PTP > 0 cm H2O.(30) The other utilizes elastance-derived PTP to target an end-inspiratory PTP equal to 25 cm H2O.(13) It is not surprising that when both strategies were applied to the same patients, they yielded very different PEEP values.(33) Moreover, in a third of the patients the two approaches recommended PEEP changes in opposite directions.
The PEEP settings recommended by these methods have not always had face validity. Most clinicians would expect that the optimal approach to setting PEEP would bear some relationship to ARDS severity or lung recruitability. For example, it would provide higher levels of PEEP to patients with more potential for lung recruitment, often those patients with more severe ARDS. It would also provide lower levels of PEEP in patients with less severe ARDS who might only suffer overdistention injury with higher pressures. However, in a recent study of 51 ARDS patients, the PEEP levels that resulted from targeting positive end-expiratory PTP were similar for all patients regardless of the severity of their ARDS and were unrelated to lung recruitability as measured by CT scan.(34)
One study suggested that minimizing the changes in PTP during tidal ventilation (transpulmonary driving pressure, PTP,insp – PTP,exp) may be a more appropriate strategy to balance between overdistention and lung recruitment. In an animal model, ventilator strategies designed to maintain low transpulmonary driving pressure also minimized lung inflammatory markers, type I epithelial cell damage, and pulmonary mechanical stress compared to high transpulmonary driving pressure models.(35) Recently, though, Marini and colleagues demonstrated in a large animal model of bilateral lung injury that airway driving pressure (Pplateau,insp – PEEP) parallels transpulmonary driving pressure. This relationship held as intraabdominal pressure was varied, although it was less reliable in normal or unilaterally-injured lungs. (36)
Other Methods for Avoiding Vili
The most intriguing aspect of utilizing PTP in ARDS remains its potential to individualize ventilator settings to each patient's lung mechanics to minimize the risk of VILI. Unfortunately, esophageal manometry is laden with potentially inaccurate assumptions and correction factors. There are alternatives, however, which may allow PEEP to be individually optimized without requiring the measurement of Pes.
For example, one small study of 11 ARDS patients found that the recommended PEEP level to maintain a positive PTP was not significantly different from the PEEP level that achieved maximal respiratory system compliance as measured with a decremental PEEP titration.(37) Another study suggested that calculation of the stress index was better than either plateau pressure or PTP for preventing overdistention injury.(38) Stress index is a characteristic of the airway pressure-time relationship during tidal ventilation that reflects the balance between alveolar overdistention and cyclic recruitment-derecruitment. In a similar fashion, airway driving pressure at a constant tidal volume reflects the tidal compliance of the respiratory system and may represent the potential for VILI from these same mechanisms. Based on a recent analysis by Amato and colleagues, airway driving pressure appears to be a critical mediator of VILI and a strong predictor of mortality.(39) Further prospective trials, however, must be conducted using airway driving pressure to guide ventilator management before it can replace more established methods for adjusting ventilator settings.
Conclusion
There is growing interest in personalizing ventilator interventions to each patient based on physiological principles to ameliorate VILI. The use of PTP to achieve this type of precision medicine is inherently appealing, and esophageal manometry offers a plausible technique for estimating PTP.(40) Some trials utilizing PTP to adjust ventilator settings have shown encouraging results for improving arterial oxygenation and possibly mortality.(13, 30) However, other studies suggest optimal PEEP or tidal volume in ARDS may be achieved through less invasive means than PTP monitoring, fraught with fewer technical errors and assumptions, such as respiratory system compliance, stress index, oxygenation tables, or airway driving pressure. More research is needed to determine the best strategies for PEEP and tidal volume titration in ARDS.
Key Points.
Airway pressure alone may be misleading for the assessment of ventilator induced lung injury in ARDS.
Transpulmonary pressure might provide a more accurate assessment of stress in the lung parenchyma and allow for the customization of ventilator settings to individual lung mechanics.
The measurement of transpulmonary pressure requires the estimation of pleural pressure from esophageal manometry, which may be limited by several assumptions and potential sources of error.
Use of transpulmonary pressure to guide PEEP selection led to improved arterial oxygenation and respiratory system compliance in clinical trials.
Alternative less invasive methods may provide comparable options for optimizing PEEP or tidal volume in patients with ARDS.
Acknowledgments
The authors thank Dr. Henry Fessler for reviewing the manuscript and providing useful comments. Research reported in this publication was supported by the National Heart, Lung, And Blood Institute of the National Institutes of Health under Award Number T32HL007534. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Conflicts of Interest: The authors declare no conflicts of interest
References
- 1.Dreyfuss D, Saumon G. Ventilator-induced Lung Injury. American Journal of Respiratory and Critical Care Medicine. 1998;157(1):294–323. doi: 10.1164/ajrccm.157.1.9604014. [DOI] [PubMed] [Google Scholar]
- 2.Webb H, Tierney D. Experimental Pulmonary Edema due to Intermittent Positive Pressure Ventilation with High Inflation Pressures. Protection by Positive End-Expiratory Pressure. American Review of Respiratory Disease. 1974;110:556–65. doi: 10.1164/arrd.1974.110.5.556. [DOI] [PubMed] [Google Scholar]
- 3.Muscedere JG, Mullen JB, Gan K, Slutsky AS. Tidal ventilation at low airway pressures can augment lung injury. American Journal of Respiratory and Critical Care Medicine. 1994;149(5):1327–34. doi: 10.1164/ajrccm.149.5.8173774. [DOI] [PubMed] [Google Scholar]
- 4.Hubmayr RD. Perspective on Lung Injury and Recruitment. American Journal of Respiratory and Critical Care Medicine. 2002;165(12):1647–53. doi: 10.1164/rccm.2001080-01CP. [DOI] [PubMed] [Google Scholar]
- 5.Ventilation with Lower Tidal Volumes as Compared with Traditional Tidal Volumes for Acute Lung Injury and the Acute Respiratory Distress Syndrome. New England Journal of Medicine. 2000;342(18):1301–8. doi: 10.1056/NEJM200005043421801. [DOI] [PubMed] [Google Scholar]
- 6.Chiumello D, Carlesso E, Cadringher P, Caironi P, Valenza F, Polli F, et al. Lung Stress and Strain during Mechanical Ventilation for Acute Respiratory Distress Syndrome. American Journal of Respiratory and Critical Care Medicine. 2008;178(4):346–55. doi: 10.1164/rccm.200710-1589OC. [DOI] [PubMed] [Google Scholar]
- 7.Hager DN, Brower RG. Customizing lung-protective mechanical ventilation strategies*. Critical Care Medicine. 2006;34(5):1554–5. doi: 10.1097/01.CCM.0000216183.25478.03. [DOI] [PubMed] [Google Scholar]
- 8.Hager DN, Krishnan JA, Hayden DL, Brower RG. Tidal Volume Reduction in Patients with Acute Lung Injury When Plateau Pressures Are Not High. American Journal of Respiratory and Critical Care Medicine. 2005;172(10):1241–5. doi: 10.1164/rccm.200501-048CP. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dreyfuss D, Soler P, Basset G, Saumon G. High Inflation Pressure Pulmonary Edema: Respective Effects of High Airway Pressure, High Tidal Volume, and Positive End-expiratory Pressure. American Review of Respiratory Disease. 1988;137(5):1159–64. doi: 10.1164/ajrccm/137.5.1159. [DOI] [PubMed] [Google Scholar]
- 10.Mercat A, Richard JM, Vielle B, et al. Positive end-expiratory pressure setting in adults with acute lung injury and acute respiratory distress syndrome: A randomized controlled trial. JAMA. 2008;299(6):646–55. doi: 10.1001/jama.299.6.646. [DOI] [PubMed] [Google Scholar]
- 11.Meade MO, Cook DJ, Guyatt GH, et al. Ventilation strategy using low tidal volumes, recruitment maneuvers, and high positive end-expiratory pressure for acute lung injury and acute respiratory distress syndrome: A randomized controlled trial. JAMA. 2008;299(6):637–45. doi: 10.1001/jama.299.6.637. [DOI] [PubMed] [Google Scholar]
- 12.Higher versus Lower Positive End-Expiratory Pressures in Patients with the Acute Respiratory Distress Syndrome. New England Journal of Medicine. 2004;351(4):327–36. doi: 10.1056/NEJMoa032193. [DOI] [PubMed] [Google Scholar]
- 13.Grasso S, Terragni P, Birocco A, Urbino R, Del Sorbo L, Filippini C, et al. ECMO criteria for influenza A (H1N1)-associated ARDS: role of transpulmonary pressure. Intensive Care Med. 2012;38(3):395–403. doi: 10.1007/s00134-012-2490-7. [DOI] [PubMed] [Google Scholar]
- 14.Cherniack RM, Farhi LE, Armstrong BW, Proctor DF. A Comparison of Esophageal and Intrapleural Pressure in Man. Journal of Applied Physiology. 1955;8(2):203–11. doi: 10.1152/jappl.1955.8.2.203. [DOI] [PubMed] [Google Scholar]
- 15.Milic-Emili J, Mead J, Turner JM. Topography of esophageal pressure as a function of posture in man. Journal of Applied Physiology. 1964;19(2):212–6. doi: 10.1152/jappl.1964.19.2.212. [DOI] [PubMed] [Google Scholar]
- 16.Milic-Emili J, Mead J, Turner JM, Glauser EM. Improved technique for estimating pleural pressure from esophageal balloons. Journal of Applied Physiology. 1964;19(2):207–11. doi: 10.1152/jappl.1964.19.2.207. [DOI] [PubMed] [Google Scholar]
- 17.Gibson GJ, Pride NB. Lung Distensibility. The static pressure-volume curve of the lungs and its use in clinical assessment. British Journal of Diseases of the Chest. 1976;70(3):143–84. doi: 10.1016/0007-0971(76)90027-9. [DOI] [PubMed] [Google Scholar]
- 18.Mead J, Gaensler EA. Esophageal and pleural pressures in man, upright and supine. Journal of Applied Physiology. 1959;14(1):81–3. doi: 10.1152/jappl.1959.14.1.81. [DOI] [PubMed] [Google Scholar]
- 19*.Keller SP, Fessler HE. Monitoring of oesophageal pressure. Curr Opin Crit Care. 2014;20(3):340–6. doi: 10.1097/MCC.0000000000000092. Concise review regarding the pros and cons of esophageal pressure monitoring. [DOI] [PubMed] [Google Scholar]
- 20.Talmor DS, Fessler HE. Are Esophageal Pressure Measurements Important in Clinical Decision-Making in Mechanically Ventilated Patients? Respiratory Care. 2010;55(2):162–74. [PubMed] [Google Scholar]
- 21.Washko GR, Donnell CR, Loring SH. Volume-related and volume-independent effects of posture on esophageal and transpulmonary pressures in healthy subjects. Journal of Applied Physiology. 2006;100(3):753–8. doi: 10.1152/japplphysiol.00697.2005. [DOI] [PubMed] [Google Scholar]
- 22.Gattinoni L, Chiumello D, Carlesso E, Valenza F. Bench-to-bedside review: Chest wall elastance in acute lung injury/acute respiratory distress syndrome patients. Critical Care. 2004;8(5):350–5. doi: 10.1186/cc2854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23*.Brochard L. Measurement of esophageal pressure at bedside: pros and cons. Current Opinion in Critical Care. 2014;20(1):39–46. doi: 10.1097/MCC.0000000000000050. This is a review of the arguments for and against esophageal pressure measurements in mechanically ventilated patients. [DOI] [PubMed] [Google Scholar]
- 24*.Chiumello D, Cressoni M, Colombo A, Babini G, Brioni M, Crimella F, et al. The assessment of transpulmonary pressure in mechanically ventilated ARDS patients. Intensive Care Med. 2014;40(11):1670–8. doi: 10.1007/s00134-014-3415-4. This is a clinical study in humans assessing the relationship between different methods of calculating transpulmonary pressures. [DOI] [PubMed] [Google Scholar]
- 25.Pelosi P, Goldner M, McKibben A, Adams A, Eccher G, Caironi P, et al. Recruitment and Derecruitment During Acute Respiratory Failure. American Journal of Respiratory and Critical Care Medicine. 2001;164(1):122–30. doi: 10.1164/ajrccm.164.1.2007010. [DOI] [PubMed] [Google Scholar]
- 26.Wilson TA. Solid Mechanics, Handbook of Physiology Mechanics of Breathing. 3: Am Physiol Soc. 1986:35–40. [Google Scholar]
- 27.Lai-Fook SJ, Rodarte JR. Pleural pressure distribution and its relationship to lung volume and interstitial pressure. Journal of Applied Physiology. 1991;70(3):967–78. doi: 10.1152/jappl.1991.70.3.967. [DOI] [PubMed] [Google Scholar]
- 28.Lachmann B. Open up the lung and keep the lung open. Intensive Care Medicine. 1992;18(6):319–21. doi: 10.1007/BF01694358. [DOI] [PubMed] [Google Scholar]
- 29.Loring SH, O'Donnell CR, Behazin N, Malhotra A, Sarge T, Ritz R, et al. Esophageal pressures in acute lung injury: do they represent artifact or useful information about transpulmonary pressure, chest wall mechanics, and lung stress? Journal of Applied Physiology. 2010;108(3):515–22. doi: 10.1152/japplphysiol.00835.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Talmor D, Sarge T, Malhotra A, O'Donnell CR, Ritz R, Lisbon A, et al. Mechanical Ventilation Guided by Esophageal Pressure in Acute Lung Injury. New England Journal of Medicine. 2008;359(20):2095–104. doi: 10.1056/NEJMoa0708638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Talmor D, Sarge T, O'Donnell CR, Ritz R, Malhotra A, Lisbon A, et al. Esophageal and transpulmonary pressures in acute respiratory failure. Crit Care Med. 2006;34(5):1389–94. doi: 10.1097/01.CCM.0000215515.49001.A2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32*.Fish E, Novack V, Banner-Goodspeed VM, Sarge T, Loring S, Talmor D. The Esophageal Pressure-Guided Ventilation 2 (EPVent2) trial protocol: a multicentre, randomised clinical trial of mechanical ventilation guided by transpulmonary pressure. BMJ Open. 2014;4(10) doi: 10.1136/bmjopen-2014-006356. This is a publication of the methods being used in a trial that will compare PTP-guided PEEP management with an uniform high PEEP strategy for patietns with moderate to severe ARDS. The trial is currently enrolling and primary outcmes will include mortality and ventilator free days. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gulati G, Novero A, Loring SH, Talmor D. Pleural Pressure and Optimal Positive End-Expiratory Pressure Based on Esophageal Pressure Versus Chest Wall Elastance: Incompatible Results*. Critical Care Medicine. 2013;41(8):1951–7. doi: 10.1097/CCM.0b013e31828a3de5. [DOI] [PubMed] [Google Scholar]
- 34**.Chiumello D, Cressoni M, Carlesso E, Caspani ML, Marino A, Gallazzi E, et al. Bedside Selection of Positive End-Expiratory Pressure in Mild, Moderate, and Severe Acute Respiratory Distress Syndrome*. Critical Care Medicine. 2014;42(2):252–64. doi: 10.1097/CCM.0b013e3182a6384f. This study demonstrated that recommended PEEP levels based on targeting a positive end-expiratory PTP did not correlate with severity of lung injury or potential for recruitment by CT scan. [DOI] [PubMed] [Google Scholar]
- 35*.Samary CS, Santos RS, Santos CL, Felix NS, Bentes M, Barboza T, et al. Biological Impact of Transpulmonary Driving Pressure in Experimental Acute Respiratory Distress Syndrome. Anesthesiology. 2015;123(2):423–33. doi: 10.1097/ALN.0000000000000716. This was an animal study demosntrating that ventilator strategies targeting low transpulmonary driving pressure and low tidal volume resulted in the lowest levels of circulating inflammatory markers. [DOI] [PubMed] [Google Scholar]
- 36*.Cortes-Puentes GA, Keenan JC, Adams AB, Parker ED, Dries DJ, Marini JJ. Impact of Chest Wall Modifications and Lung Injury on the Correspondence Between Airway and Transpulmonary Driving Pressures. Critical Care Medicine. 2015;43(8):e287–e95. doi: 10.1097/CCM.0000000000001036. This was a large animal model which compared the relationship between airway driving pressure and transpulmonary driving pressure during different patterns of lung injury and intraabdominal hypertension. Airway driving pressure correlated best with transpulmonary driving pressure with bilateral lung injury. [DOI] [PubMed] [Google Scholar]
- 37.Rodriguez PO, Bonelli I, Setten M, Attie S, Madorno M, Maskin LP, et al. Transpulmonary Pressure and Gas Exchange During Decremental PEEP Titration in Pulmonary ARDS Patients. Respiratory Care. 2013;58(5):754–63. doi: 10.4187/respcare.01977. [DOI] [PubMed] [Google Scholar]
- 38.Terragni PP, Filippini C, Slutsky AS, Birocco A, Tenaglia T, Grasso S, et al. Accuracy of Plateau Pressure and Stress Index to Identify Injurious Ventilation in Patients with Acute Respiratory Distress Syndrome. Anesthesiology. 2013;119(4):880–9. doi: 10.1097/ALN.0b013e3182a05bb8. [DOI] [PubMed] [Google Scholar]
- 39*.Amato MB, Meade MO, Slutsky AS, Brochard L, Costa EL, Schoenfeld DA, et al. Driving pressure and survival in the acute respiratory distress syndrome. N Engl J Med. 2015;372(8):747–55. doi: 10.1056/NEJMsa1410639. This was a retrospective meta-analysis of individual patient data which demonstrated that airway driving pressure is a critical mediator for lung injury and an independent predictor of mortality. [DOI] [PubMed] [Google Scholar]
- 40**.Akoumianaki E, Maggiore SM, Valenza F, Bellani G, Jubran A, Loring SH, et al. The application of esophageal pressure measurement in patients with respiratory failure. Am J Respir Crit Care Med. 2014;189(5):520–31. doi: 10.1164/rccm.201312-2193CI. This is a comprehensive review of esophageal pressure measurements in the ventilated patient. It includes a thorough physiologic review and proposes several ways to utilize esophageal pressures in the care of mechanically ventilated patients. [DOI] [PubMed] [Google Scholar]


