Abstract
Background
Incarceration is common among people who inject drugs. Prior research has shown that incarceration is a marker of elevated risk for opioid overdose, suggesting that the criminal justice system may be an important, under-utilized venue for implementing overdose prevention strategies. To better understand the feasibility and acceptability of such strategies, we evaluated the utilization of naloxone-based overdose prevention training among people who inject drugs with and without a history of incarceration.
Methods
We surveyed clients who utilize a multi-site syringe exchange program (SEP) in 2 cities in the Midwestern United States. Participants completed an 88-item, computerized survey assessing history of incarceration, consequences associated with injection, injecting practices, and uptake of harm reduction strategies.
Results
Among 543 respondents who injected drugs in the prior 30 days, 243 (43%) reported prior incarceration. Comparing those with and without a history of incarceration, there were no significant differences with respect to age, gender, or race. Those who observed an overdose, experienced overdose, and received training to administer or have administered naloxone were more likely to report incarceration. Overall, 69% of previously incarcerated clients had been trained to administer naloxone.
Conclusion
People who inject drugs with a history of incarceration appear to have a higher risk of opioid overdose than those never incarcerated, and are more willing to utilize naloxone as an overdose prevention strategy. Naloxone training and distribution is an important component of comprehensive prevention services for persons with opioid use disorders. Expansion of services for persons leaving correctional facilities should be considered.
Keywords: People who inject drugs, overdose, risky health behaviors, take-home naloxone, correctional facilities
1. INTRODUCTION
Opioid overdose is a major source of morbidity and mortality among people who inject drugs. In the United States, drug overdose has become the leading cause of death among people who inject drugs (Centers for Disease Control and Prevention, 2014; Evans et al., 2012). Nationally, death rates from heroin overdoses doubled from 1.0 to 2.1 per 100,000 from 2010 to 2012 (Rudd et al., 2014), suggesting that overdose prevention is an increasingly important public health issue.
Several studies have demonstrated that the period following release from jail or prison is associated with high risk for fatal overdose among injecting drug users (Binswanger et al., 2007; Bird and Hutchinson, 2003; Merrall et al., 2010; World Health Organization, 2010). An estimated 1 in 200 heroin users who are released from prison will die of a heroin overdose within the first 4 weeks of release (Strang et al., 2013). Binswanger et al (2007) found that within the first two weeks after release, the risk of death was 12.7 times greater than the general population, which was largely due to drug overdose. This increased risk may be due to loss of tolerance following a period of abstinence (Leach and Oliver, 2011; Strang et al., 2003).
Community-based naloxone training and distribution programs are effective and increasing in popularity as a strategy to reduce deaths to opioid overdose (Seal et al., 2005; Tobin et al., 2009). There is evidence that people who inject drugs with a history of incarceration desire naloxone administration training (Wakeman et al., 2009). In this study, we aimed to improve our understanding of the acceptability and current uptake of naloxone-based overdose prevention training among people who inject drugs who interact with the criminal justice system. We compared receipt of naloxone training and prior naloxone administration among people who inject drugs with and without a history of incarceration.
2. METHODS
2.1. Study participants
We surveyed people who inject drugs utilizing a free, multi-site syringe exchange program (SEP) operating in Southern Wisconsin between June and August, 2012. The Lifepoint Needle Exchange operates through office-based locations in the cities of Madison and Milwaukee, and via mobile van units that serve the Milwaukee suburbs and rural communities surrounding Madison. All individuals who speak and read English, were 18 years or older, and reported a history of injecting drugs were invited to participate. Participants provided verbal informed consent and were paid $10 in cash as compensation for completing the survey.
2.2. Ethics statement
The study protocol was approved by the Minimal Risk Institutional Review Board at the University of Wisconsin School of Medicine and Public Health, which approved a waiver of signed consent due to the anonymous nature of the data collected.
2.3. Survey administration
We developed and pilot-tested an 88-item questionnaire assessing demographic characteristics, types and frequency of drug use, and personal history of medical and social consequences of injecting drugs. The main overdose-related variables were (1) personal history of overdose (2) witnessing a peer overdose, (3) receiving training to administer naloxone, and (4) administering naloxone to someone in the past. Incarceration was assessed using two questions, which asked whether respondents had ever (1) “Been arrested/put in jail” and (2) “Served more than one month in prison.” The second of these was intended to capture longer periods of incarceration that would typically result from a criminal conviction. We did not collect data on prison sentences less than 30 days. The multiple-choice surveys were self-administered by the respondent, who read the survey and recorded responses using a tablet computer. This allowed respondents to provide information dealing with sensitive subjects such as illicit drug use in a private manner, decreasing the likelihood of socially desirable responding.
2.4. Statistical analysis
All variables were entered into an anonymous database for analysis. Descriptive statistics were used to characterize the study population and examine any differences with respect to demographic and behavioral characteristics between those who did and did not report a history of incarceration. The former group included those who reported ever having been arrested or put in jail for any period of time and those who had served more than 30 days in prison. The two groups were analyzed by Wald chi-squared tests for categorical variables with significance defined as p<0.05. Simple logistic regression was utilized to generate odds ratios and 95% confidence intervals representing bivariate association between overdose characteristics and personal history of incarceration. An alpha level of 0.05 was assumed to indicate statistical significance. Separate analysis was performed based on incarceration type. Statistical analyses were conducted using STATA Version 11 (Cary, NC).
3. RESULTS
3.1. Study participants
Over the 8-week study period, 862 consecutive SEP participants were invited to participate in the study and 543 eligible participants (63%) agreed to complete the survey. Characteristics of the study participants are shown in Table 1, stratified by incarceration history. The mean age was 31.6 years; most respondents were white (79%) and male (69%). Overall, 43% of participants indicated they had ever been arrested, been put in jail, or spent more than 30 days in prison. Of those who reported incarceration, 31% had spent more than 30 days in prison. Ninety percent of previously incarcerated respondents used heroin as their “main drug.” In this sub-population, opioids (i.e., heroin, oxycodone) accounted for 93% of the most frequently used drug, whereas only 7% primarily used drugs other than opioids (i.e., crack, cocaine, methamphetamines).
Table 1.
Characteristics of PWID sample, by history of incarceration (N=543)
| Characteristics | No history of incarceration | History of incarceration |
|---|---|---|
| Overall number of participants | 309 | 234 |
| Age (mean years ± SD) | 31.4 ± 0.6 | 31.2 ± 0.6 |
| Gender (%) | ||
| Male | 208 (67) | 166 (71) |
| Female | 101 (33) | 68 (29) |
| Hispanic ethnicity (%) | ||
| No | 289 (94) | 218 (93) |
| Yes | 20 (6) | 16 (7) |
| Currently employed (part- or full-time) (%) | ||
| No | 196 (63) | 138 (59) |
| Yes | 113 (37) | 96 (41) |
| Area of Residence (%) | ||
| Urban | 126 (41) | 96 (41) |
| Suburban/Rural | 176 (59) | 134 (59) |
| Race (%) | ||
| Caucasian | 257 (83) | 196 (84) |
| Black | 39 (13) | 23 (10) |
| Asian/Pacific Islander | 1 (4) | 2 (6) |
| Education (%) | ||
| Completed some college or technical school | 119 (39) | 57 (24) |
| Completed no college or technical school | 190 (61) | 177 (76) |
| Observed an overdose (%) | ||
| No | 135 (44) | 36 (15) |
| Yes | 174 (56) | 198 (85) |
| Overdosed from injecting drugs (%) | ||
| No | 239 (77) | 138 (59) |
| Yes | 70 (23) | 96 (41) |
| Trained to administer naloxone (%) | ||
| No | 134 (43) | 72 (31) |
| Yes | 175 (57) | 162 (69) |
| Gave naloxone to another person (%) | ||
| No | 196 (63) | 127 (54) |
| Yes | 85 (37) | 98 (46) |
All values are n (%) unless otherwise noted
3.2. Incarceration and overdose characteristics
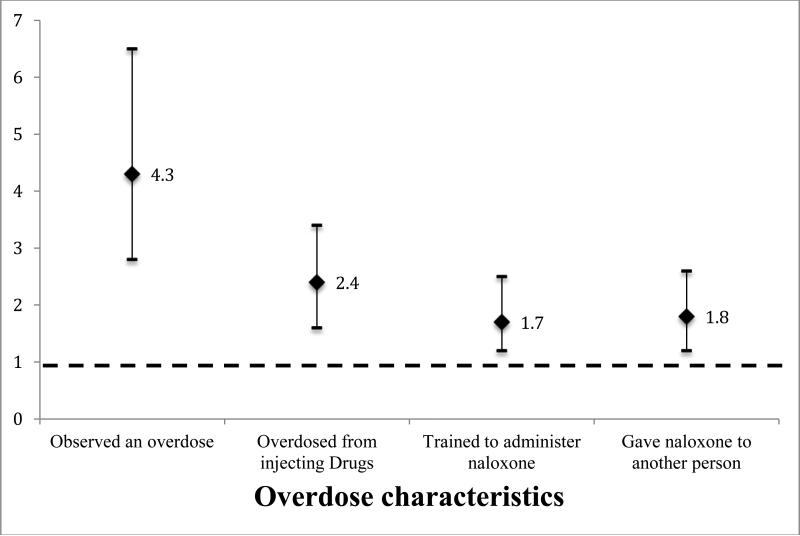
Figure 1 shows relative odds of incarceration history with overdose characteristics. After adjusting for age, sex, and race, univariate regression showed that those respondents who observed an overdose (odds ratio (OR) 4.3, 95% confidence interval (C.I.) 2.8-6.5) or experienced an overdose (OR 2.4, 95% C.I. 1.7-3.5) were more likely to have a history of incarceration. Similarly, the respondents who were trained to administer naloxone (OR 1.7, 95% C.I. 1.2-2.5) or who had administered naloxone to another person (OR 1.8, 95% C.I. 1.2-2.6) were more likely to have a history of incarceration. The majority (88%) of previously incarcerated individuals with naloxone administration training were trained by Lifepoint Needle Exchange staff. No participants specifically reported receiving naloxone training in a prison or jail.
Figure 1.
Relative Odds of Incarceration in Prison or Jail, by Selected Overdose Variables
Separate univariate regression that also adjusted for age, sex, and race showed that those respondents who had experienced an overdose (OR 2.4, 95% C.I. 1.6-3.5), observed an overdose (OR 4.2, 95% C.I. 2.7-6.4), administered naloxone to another person (OR 1.8, 95% C.I. 1.3-2.7), or were trained to administer naloxone (OR 1.7, 95% C.I. 1.2-2.5) were more like to have been arrested or spent time in jail than those without prior arrest/jail. Prison stays were similarly associated with the two overdose variables, but not naloxone training or administration. Respondents who had experienced an overdose (OR 3.5, 95% C.I. 2.1-5.9) or witnessed an overdose (OR 10.0, 95% C.I. 3.5-28.1) were more likely than not to have spent at least one month in prison. As mentioned, neither naloxone training (OR 1.2, 95% C.I. 0.7-2.1) nor previous naloxone administration (OR 1.0, 95% C.I. 0.6-1.7) were associated with spending at least one month in prison.
4. DISCUSSION
In this cross-sectional survey of people who inject drugs in Wisconsin, we found that nearly half of the respondents had a history of incarceration. Those who had been incarcerated were more likely to have witnessed or experienced an overdose from injection drug use, and reported higher utilization of naloxone training in community settings. We found that nearly half (44%) of our study population had administered naloxone and 69% had been trained to properly administer it. Both naloxone training and administration were associated with arrest or jail, but were not associated with spending more than one month in prison.
Multiple studies have shown that people who inject drugs are eager to learn and capable of administering naloxone in the event of a witnessed overdose. The first study to demonstrate willingness to carry naloxone conducted by Strang et al (1999), demonstrated that 70% of previous or current drug misusers considered naloxone distribution a good proposal. Eighty-nine percent of those who had witnessed a fatal overdose stated that they would have administered naloxone had it been available (Strang et al., 1999). Tobin et al. (2009) observed more than half of the participants who received training to administer naloxone later used it to rescue someone experiencing overdose. In a study of 137 long-term opioid users with previous involvement in the criminal justice system, 72% reported interest in having naloxone prescribed to them in case of emergency and 90% reported willingness to participate in a two-hour training session to learn about overdose prevention and recognition, rescue breathing, and naloxone administration (Wakeman et al., 2009). Our data add to this literature by demonstrating that when naloxone training is made available through community-based SEPs, criminal justice-involved clients will utilize the service and administer naloxone in practice.
There are relatively few US-based in-prison prevention programs (Rich, 2005). The US currently has overdose recognition and response training and naloxone administration training in a small number of correctional facilities, notably in San Francisco, New York City, Pittsburgh, and Rhode Island (DOPE Project, 2015). To date, only one randomized trial is underway based in the United Kingdom that aims to investigate the “extent to which deaths from heroin overdose [in the UK] in the first 12 weeks post-release from prison can be prevented by prior provision of a take-home emergency naloxone supply” (Strang et al., 2013). This take-home naloxone program is implemented at the point of prison release as opposed. Given the significantly higher rates of overdose and witnessed overdose in our study participants with an incarceration history, continued efforts to increase naloxone training may decrease mortality from overdose. While community efforts for naloxone training are ongoing through the SEPs, there may be opportunities during incarceration or upon release to distribute naloxone and train people to administer it.
There are several limitations to our study. First, since all participants were clients at a SEP, our study sample may exclude a subset of people who do not use prevention services and may engage in higher risk behaviors making it possible that our data may not be fully representative of higher risk people who inject drugs. Second, our study may not be generalizable outside of the Midwestern United States since it was performed in a single Midwestern state with a mix of urban, rural, and suburban participants; there was a predominance of Caucasian participants in our sample is not representative of other communities in the US; and due to the modest response rate (63%). Next, whether incarceration is causally related to increased willingness to utilize naloxone cannot be determined from this cross-sectional study. It is plausible that SEP staff may more aggressively encourage recently-incarcerated clients to complete naloxone training because these individuals are perceived as having a particularly high risk of experiencing or witnessing an overdose. Finally, we were unable to determine number or length of incarcerations, incarceration not related to injecting drugs, the time elapsed from release to survey completion, frequency of SEP or other prevention services utilization, or the time elapsed from release to naloxone training. This cross-sectional study does show, however, that higher rates of overdose and higher-risk behaviors are associated with previous incarceration at any point in time. This may be beneficial as interventions can be implemented at various pre- and post-release time points.
There is a critical need for harm reduction strategies among people who inject drugs, particularly those with a history of incarceration. Our data support the fact that compared with those without history of incarceration, previously-incarcerated people who inject drugs who utilize SEPs are at higher risk of overdose, but may be more willing to participate in naloxone training. Future studies are needed to determine the utility and feasibility of naloxone training in correctional settings in the United States.
Highlights.
Forty-three percent of 543 respondents who reported injecting drugs in the prior 30 days also reported prior incarceration
Those who experienced an overdose or witnessed an overdose were more likely to report incarceration
Those who had been trained to administer naloxone were more likely to report overdose
Acknowledgements
None
Role of Funding
This manuscript was supported by the Clinical and Translational Science Award (CTSA) program, through the NIH National Center for Advancing Translational Sciences (NCATS), grant UL1TR000427. RPW is supported by NIH grant K23DA032306. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributors Page:
Joshua Barocas: Participated in the design and conception of the initial project including proposal and IRB submission; participated in data collection; performed data analysis; and drafted the manuscript. This author has approved the final article.
Lisa Baker: Participated in edits of the manuscript. This author has approved the final article.
Shawnika Hull: Participated in the initial design of the study including question formulation and participated in edits of the manuscript. This author has approved the final article.
Scott Stokes: Participated in organization of data collectors. This author has approved the final article.
Ryan Westergaard: Conceived of the study, participated in its design and coordination and helped to draft the manuscript. This author has approved the final article.
Conflicts of Interest
None of the authors have financial or non-financial conflicts of interests.
REFERENCES
- Binswanger IA, Stern MF, Deyo RA, Heagerty PJ, Cheadle A, Elmore JG, Koepsell TD. Release from prison--a high risk of death for former inmates. N. Engl. J. Med. 2007;356:157–165. doi: 10.1056/NEJMsa064115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bird SM, Hutchinson SJ. Male drugs-related deaths in the fortnight after release from prison: Scotland, 1996-99. Addiction. 2003;98:185–190. doi: 10.1046/j.1360-0443.2003.00264.x. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention Web-based Injury Statistics Query and Reporting System (WISQARS) 2014 Retrieved from http://www.cdc.gov/injury/wisqars/fatal.html.
- DOPE Project DOPE Project: Naloxone Program Case Studies. Harm Reduction Coalition. 2015 Retrieved from http://harmreduction.org/issues/overdose-prevention/tools-best-practices/naloxone-program-case-studies/dope-project/
- Evans JL, Tsui JI, Hahn JA, Davidson PJ, Lum PJ, Page K. Mortality among young injection drug users in San Francisco: a 10-year follow-up of the UFO study. Am. J. Epidemiol. 2012;175:302–308. doi: 10.1093/aje/kwr318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- International Drug Policy Consortium. 1st Prison Naloxone Peer Educator Group Launched In Scotland. 2013 Retrieved from http://idpc.net/alerts/2013/12/1st-prison-naloxone-peer-educator-group-launched-in-scotland.
- Leach D, Oliver P. Drug-related death following release from prison: a brief review of the literature with recommendations for practice. Curr. Drug Abuse Rev. 2011;4:292–297. doi: 10.2174/1874473711104040292. [DOI] [PubMed] [Google Scholar]
- Merrall ELC, Kariminia A, Binswanger IA, Hobbs MS, Farrell M, Marsden J, Hutchinson SJ, Bird SM. Meta-analysis of drug-related deaths soon after release from prison: drug-related deaths after release from prison. Addiction. 2010;105:1545–1554. doi: 10.1111/j.1360-0443.2010.02990.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Services Scotland . National Naloxone Programme Scotland-naloxone kits Issued In 2013/14 And Trends In Opioid-Related Deaths. National Services; Scotland: 2014. Retrieved from http://www.isdscotland.org/Health-Topics/Drugs-and-Alcohol-Misuse/Publications/2014-10-28/2014-10-28-Naloxone-Report.pdf. [Google Scholar]
- Rich JD. Attitudes and practices regarding the use of methadone in US state and federal prisons. J. Urban Health. 2005;82:411–419. doi: 10.1093/jurban/jti072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rudd RA, Paulozzi LJ, Bauer MJ, Burleson RW, Carlson RE, Dao D, Davis JW, Dudek J, Eichler BA, Fernandes JC, Fondario A, Gabella B, et al. Increases in heroin overdose deaths - 28 States, 2010 to 2012. MMWR. 2014;63:849–854. [PMC free article] [PubMed] [Google Scholar]
- Seal KH, Thawley R, Gee L, Barnberger J, Kral AH, Ciccarone D, Downing M, Edlin BR. Naloxone distribution and cardiopulmonary resuscitation training for injection drug users to prevent heroin overdose death: a pilot intervention study. J. Urban Health. 2005;82:303–311. doi: 10.1093/jurban/jti053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strang J, Powis B, Best D, Vingoe L, Griffiths P, Taylor C, Welch S, Gossop M. Preventing opiate overdose fatalities with take-home naloxone: pre-launch study of possible impact and acceptability. Addiction. 1999;94:199–204. doi: 10.1046/j.1360-0443.1999.9421993.x. [DOI] [PubMed] [Google Scholar]
- Strang J, Bird SM, Parmar MKB. Take-home emergency naloxone to prevent heroin overdose deaths after prison release: rationale and practicalities for the n-alive randomized trial. J. Urban Health. 2013;90:983–996. doi: 10.1007/s11524-013-9803-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strang J, McCambridge J, Best D, Beswick T, Bearn J, Rees S, Gossop M. Loss of tolerance and overdose mortality after inpatient opiate detoxification: follow up study. BMJ. 2003;326:959–960. doi: 10.1136/bmj.326.7396.959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tobin KE, Sherman SG, Beilenson P, Welsh C, Latkin CA. Evaluation of the Staying Alive programme: training injection drug users to properly administer naloxone and save lives. Int. J. Drug Policy. 2009;20:131–136. doi: 10.1016/j.drugpo.2008.03.002. [DOI] [PubMed] [Google Scholar]
- Wakeman SE, Bowman SE, McKenzie M, Jeronimo A, Rich JD. Preventing death among the recently incarcerated: an argument for naloxone prescription before release. J. Addict. Dis. 2009;28:124–129. doi: 10.1080/10550880902772423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . Prevention Of Acute Drug-Related Mortality In Prison Populations During The Immediate Post-Release Period. WHO Regional Office for Europe; Copenhagen: 2010. [Google Scholar]