Abstract
Several studies provide evidence supporting a beneficial effect from the traditional Mediterranean diet (MedDiet) on the risk of type 2 diabetes mellitus (T2DM) and metabolic syndrome (MetS). This review summarizes the current scientific evidence from epidemiologic studies and clinical trials on the relation between the MedDiet and T2DM and MetS and the possible mechanisms underlying the reported associations. A recent meta-analysis of prospective cohort studies showed that greater adherence to the MedDiet was associated with a significant reduction in the risk of diabetes. The MedDiet has also been found to be beneficial in the prevention of gestational diabetes. Four large prospective studies have observed inverse associations between the MedDiet and MetS or its components. Few randomized controlled trials (RCTs) have evaluated the effect of the MedDiet on T2DM and MetS. Results from the landmark PREvención con DIeta MEDiterránea (PREDIMED) nutrition intervention trial showed that participants assigned to the MedDiet had a significant 30% reduction in the risk of T2DM and that it also promoted the reversion of MetS and its components, hyperglycemia and central obesity. In addition, 5 RCTs showed the beneficial effects of the MedDiet compared with other dietary patterns on glycemic control in patients with T2DM. A recent meta-analysis of RCTs revealed that, compared with a variety of control diets, the MedDiet was associated with beneficial effects on all MetS components. Bioactive components of the MedDiet synergize to affect various metabolic pathways, leading to a reduced cardiometabolic disease risk. The abundance of healthy, nutrient-dense foods that make up the plant-based MedDiet predicts its bioactivity and potential to beneficially influence metabolic pathways that lead to MetS and T2DM, as well as other chronic conditions. Abundant epidemiologic and clinical trial evidence supports the role of the MedDiet on the prevention and management of T2DM and MetS.
Keywords: Mediterranean diet, diabetes, metabolic syndrome, metabolic syndrome components, cardiovascular disease, review
Introduction
Type 2 diabetes mellitus (T2DM)10 is a global epidemic, and it is estimated that ∼592 million individuals worldwide will harbor the disease by the year 2035 (1). T2DM is a main component of metabolic syndrome (MetS), a cluster of metabolic alterations that leads to an increased risk of cardiovascular disease (CVD), mortality, and some types of cancer (2). In developed countries, it is estimated that MetS affects around 25% of the population (3, 4). Importantly, there is consistent evidence that lifestyle changes promoting a healthy diet, physical exercise, and weight loss are effective in delaying the onset of or preventing T2DM in subjects with impaired glucose tolerance (5–8). Lifestyle modification is also a critical component of treatment strategies for MetS (9).
The study of whole dietary patterns such as the Mediterranean diet (MedDiet) has become instrumental in nutritional epidemiology. The reputedly healthy MedDiet is characterized by a high intake of fruits, vegetables, legumes, fish, whole grains, nuts, and olive oil; moderate consumption of dairy products and wine; and low intake of red and processed meats and foods that contain high amounts of added sugars (9). The relatively high intake of olive oil and nuts, together with a moderate intake of wine—particularly red wine—during meals, and frequent use of sauces with tomato, onions, garlic, and spices simmered in olive oil for meal preparation, makes the MedDiet unique and different from other healthy dietary patterns. Several a priori–defined scores measuring adherence to the MedDiet have been used in epidemiologic studies (10) and a few randomized controlled trials (RCTs) (11–14). Unfortunately these scores are not homogeneous and differ between studies and populations assessed, making international comparisons difficult. Even considering this limitation, adherence to the traditional MedDiet frequently has been associated with a reduced risk of several chronic prevalent diseases, including T2DM and MetS.
Findings from observational studies (15–17) and RCTs (15, 18) provide strong evidence to support the beneficial effects of the MedDiet on the risk of T2DM. The results from epidemiologic observations, including prospective cohort studies and less-powerful cross-sectional studies, suggest associations, but they are subject to bias and do not provide causal links, unlike RCTs. Nevertheless, the mechanisms of cardiometabolic protection by the nutrient and food components of the MedDiet add to the plausibility of the results from both epidemiologic studies and RCTs (19).
Recent results from the PREDIMED (PREvención con DIeta MEDiterránea) randomized nutrition intervention trial for the primary prevention of CVD showed a 40% reduction in the incidence of T2DM in participants assigned to a MedDiet supplemented with extra-virgin olive oil compared with those assigned to a low-fat control diet (18). Higher adherence to the MedDiet has also shown benefit in the prevention and treatment of MetS and its components (15, 16). Indeed, a meta-analysis of 50 prospective studies and RCTs suggested that adherence to the MedDiet was associated with a 50% reduction of MetS (17).
The present narrative review summarizes the current scientific evidence from epidemiologic studies and clinical trials on the relation between the MedDiet change and with T2DM and MetS. In order to understand the associations between the MedDiet and cardiometabolic outcomes, we also discuss the possible mechanisms underlying the reported associations. Because it was not conducted as a systematic review of the literature, we cannot rule out that some relevant publications might have been missed.
Epidemiologic Studies
Epidemiologic studies relating to the MedDiet and impaired glucose metabolism and diabetes.
A considerable body of evidence from prospective studies supports the importance of individual nutrients, foods, and dietary patterns in the prevention and management of T2DM (20–27). The quality of dietary fats and carbohydrates consumed is more important than the quantity of these macronutrients (28, 29). Several “healthy” dietary patterns have been inversely associated with the risk of T2DM (29, 30). These protective diets include both a priori–defined patterns (20), such as the Dietary Approaches to Stop Hypertension (DASH) diet, or dietary patterns assessed by the Alternative Healthy Eating Index and various prudent/healthy dietary patterns derived by a posteriori factor or cluster analysis. Despite variation among studies, most of these protective dietary patterns present many similarities with the traditional MedDiet, because they are mostly plant-based. Diets rich in whole grains, fruits, vegetables, legumes, and nuts; moderate in alcohol consumption; and lower in refined grains, red or processed meats, and sugar-sweetened beverages have been shown to be associated with lower risk of diabetes (28, 29).
Epidemiologic evidence regarding the association between adherence to the MedDiet and T2DM stems from cross-sectional (31, 32) and prospective studies (20–27). Cross-sectional studies have provided some degree of equivocal evidence. For example, in the Attica study, conducted in 1514 men and 1528 women living in the province of Attica, Greece, adherence to the MedDiet was inversely associated with the prevalence of T2DM (31), whereas the Di@bet.es study, a national survey aimed at examining the prevalence of impaired glucose regulation in 5076 individuals from Spain, did not find an association between adherence to the MedDiet and prevalence of known diabetes; however, a modest inverse association with the presence of prediabetes or unknown diabetes was reported (32). The lack of association to the prevalence of diabetes reported in this study compared with the Attica study might be explained by differences in the questionnaires used to assess adherence to the MedDiet, as well as dissimilar criteria used for the diagnosis of diabetes. Nevertheless, reverse causation bias cannot be ruled out in cross-sectional studies.
The results of prospective studies providing estimates of T2DM risk according to different levels of adherence to the MedDiet (20–23, 26, 27, 33, 34) have provided more consistent evidence of benefit. All prospective studies (20–23, 26, 27, 33, 34) support the protective role of the MedDiet against T2DM, with overall risk reductions ranging from 12% to 83% for subjects closely adhering to the MedDiet compared with those reporting the lowest adherence, after adjusting for several confounders. In a recent meta-analysis of prospective cohort studies published between 2007 and 2014 and including 122,810 subjects, greater adherence to the MedDiet was associated with a significant 19% lower risk of diabetes (35), with a moderate quality of evidence rated according to the Grades of Recommendation, Assessment, Development, and Evaluation (GRADE) guidelines for the main outcome (36). In the case of the Gruppo Italiano per lo Studio della Sopravvivenza nell'Infarto Miocardico (GISSI)-Prevenzione study, a secondary analysis of this trial of ω-3 FA supplementation in survivors of a myocardial infarction showed that increased adherence to a MedDiet (score assigned according to consumption of cooked and raw vegetables, fruit, fish, and olive oil) was associated not only with a lower risk of T2DM, but also with a 35% lower risk of impaired fasting glucose (21). In the Multi-Ethnic Study of Atherosclerosis (MESA) cohort, which included 5390 men and women aged 45–87 y free of T2DM and CVD at baseline that had 416 cases of incident T2DM after a 6 y follow-up, a higher MedDiet score was associated with lower insulin concentrations in nondiabetic subjects but not with a lower incidence of T2DM (26). A recent 10 y prospective analysis conducted in the cohort of the ATTICA study showed that medium and high adherence to the MedDiet was associated with lower T2DM risk by 49% (95% CI: 0.30, 0.88) and 62% (95% CI: 0.16, 0.88), respectively, compared with low adherence (33). A recent meta-analysis of prospective studies evaluating the effect of the MedDiet on the risk of T2DM concluded that higher adherence was associated with a 23% lower risk (combined RR for upper compared with lower available centile: 0.77; 95% CI: 0.66, 0.89) (34).
Gestational diabetes, defined as glucose intolerance with onset during pregnancy, is one of the most common complications of pregnancy and is linked with a subsequent higher risk of T2DM (37, 38). Two prospective studies have been conducted relating exposure to the MedDiet to the risk of gestational diabetes or its consequences. In the Nurses’ Health Study, 4430 women aged 22–44 y with prior gestational diabetes were analyzed. After 14 y of follow-up, 419 incident cases of T2DM were observed, and participants at the highest quartile of MedDiet adherence showed a 40% lower risk than did those in the lowest quartile (25). Recently, in a study conducted in 1076 pregnant women from 10 countries, adherence to a MedDiet pattern was associated with a lower incidence of gestational diabetes and better glucose tolerance, even in women without gestational diabetes (39).
Epidemiologic studies relating to the MedDiet and MetS.
Several cross-sectional and prospective studies have suggested that the MedDiet has protective effects on different components of MetS (17). A meta-analysis of epidemiologic studies and RCTs analyzing the association between MedDiet adherence and MetS was published by Kastorini et al. in 2011 (17). The combined effect of both clinical trials and prospective studies showed a protective effect of the MedDiet on MetS. However, no association between MedDiet and MetS or T2DM prevalence was demonstrated for the combined effect of cross-sectional studies (17). This can be explained by low statistical power and limitations inherent to the type of study design. Four cross-sectional studies conducted in Greece, Italy, and Poland and published after this meta-analysis also found a beneficial association between MedDiet adherence and risk of MetS prevalence (40–43).
The association between MedDiet adherence and MetS development has been explored in 4 large prospective studies (44–47). In the Seguimiento Universidad de Navarra (SUN) study, conducted in 2563 Spanish university graduates at low CVD risk who were followed for 6 y, adherence to the MedDiet measured by a modified MedDiet scale was associated with an 80% lower risk of MetS (44). Similarly, in the Framingham Offspring Cohort, which included 1918 participants without T2DM at baseline and followed for 7 y, participants in the highest quintile of adherence to a Mediterranean-style dietary pattern score had a 30% lower risk of incident MetS than did those in the lowest quintile, together with better values for the majority of MetS components (45). In the context of the Supplementation en Vitamines et Mineraux Antioxydants study, which was conducted in French adults who were followed for 6 y, adherence to the MedDiet assessed with a 9-point score was also inversely associated with incidence of MetS and its components (46). Finally, a recent report from the Coronary Artery Risk Development in Young Adults study (47) showed that an increased MedDiet score (represented by a dietary pattern rich in fruit, vegetables, whole grains, nuts, and fish, but poor in red and processed meats and snack foods) was significantly associated with a lower risk of MetS development. The consistency of results in these 4 large prospective studies supports the association between the MedDiet and a lower risk of MetS.
In conclusion, even though results from prospective studies provide less scientific evidence than those of RCTs, available epidemiologic data strongly suggest a potential protective role for the MedDiet on T2DM and MetS.
Clinical Trials
Clinical trials examining the effect of the MedDiet on T2DM.
Although there is accruing evidence from observational studies on the association between the MedDiet and T2DM, few RCTs have evaluated the effect of the MedDiet on incident T2DM.
Preliminary data from one center of the PREDIMED Study showed that, compared with a control diet consisting of advice to reduce all dietary fat sources, a traditional MedDiet supplemented with extra-virgin olive oil or nuts reduced the risk of incident T2DM by 52% in individuals at high CVD risk (48). The PREDIMED results on the whole cohort showed that after 4.1 y of follow-up, participants assigned to the MedDiet had a significant 30% reduction in the risk of T2DM (18). Increased adherence to the MedDiet also reduced the risk of T2DM by 35% in patients who had suffered a myocardial infarction participating in the GISSI-Prevenzione trial (21).
The MedDiet has also proven to be effective in the management of T2DM. Five RCTs evaluated the effects of the MedDiet compared with other dietary patterns on glycemic control in patients with T2DM (11, 49–52). The reduction of glycated hemoglobin associated with the MedDiet ranged from 0.1% to 0.6% in the different studies. In accordance with these results, a recent meta-analysis that included 20 RCTs with interventions that lasted ≥6 mo found a greater improvement in glycemic control and insulin sensitivity for the MedDiet arms compared with control diets such as low-carbohydrate or vegetarian diets (53).
There is also RCT evidence supporting a beneficial effect from the MedDiet on CVD risk factors, including BMI, systolic blood pressure, TGs, the total-to-HDL cholesterol ratio, and inflammatory markers in diabetic patients (50, 51), including those at high CVD risk (11). In the context of a clinical setting, 11,323 myocardial infarction survivors, 1700 of whom had T2DM, had a 15% reduced risk of mortality per 1 unit increase in MedDiet score after a 6.5 y follow-up (54). The PREDIMED trial, in which 3614 of the total 7447 recruited participants had a diagnosis of T2DM, showed a similar reduction in the risk of cardiovascular events (myocardial infarction, stroke, or death from CVD causes) for diabetic and nondiabetic participants (55).
Clinical trials on the MedDiet and MetS.
Findings from RCTs also support a benefit from the MedDiet on MetS and its individual components. In the context of MetS prevention, a preliminary report from the PREDIMED trial, in which 1224 participants at high CVD risk were followed for 1 y, showed that an unrestricted-calorie MedDiet was associated with reversion of MetS. The ORs for reversion of MetS were 1.3 (95% CI: 0.8, 2.1) for the group consuming the MedDiet supplemented with extra-virgin olive oil and 1.7 (95% CI 1.1, 2.6) for the group consuming the MedDiet supplemented with nuts compared with the group consuming the control diet (56). The recent findings from the total PREDIMED cohort after 4.8 y of follow-up also showed that the MedDiet was associated with reversion of MetS, but not with prevention of its incidence, and the beneficial effect was driven by a reduction in the hyperglycemia and waist circumference components of the syndrome in spite of little weight loss (57). A subanalysis of the PREDIMED trial involving 110 women with MetS also reported that, compared with the control diet, the MedDiet reduced oxidative damage to lipids and DNA (58).
The results from an RCT conducted in Italy in 180 patients with MetS showed that a restricted-calorie MedDiet was effective in reducing the prevalence of MetS and associated cardiovascular factors compared with a low-fat diet (59). Additional RCTs have evaluated the relation between the MedDiet and the individual components of MetS, as shown in a systematic review and meta-analysis of epidemiologic studies and RCTs (17). This meta-analysis included 36 RCTs conducted in healthy, hypercholesterolemic, overweight, or obese individuals, or patients at high CVD risk, with T2DM, or with a prior myocardial infarction and concluded that, compared with a variety of control diets, the MedDiet was associated with a beneficial effect on all MetS components, including waist circumference, HDL cholesterol, TGs, systolic and diastolic blood pressure, and fasting glucose and HOMA-IR (17).
In summary, there is consistent evidence from RCTs supporting the MedDiet as a useful tool in the prevention and treatment of T2DM and MetS.
Mechanisms
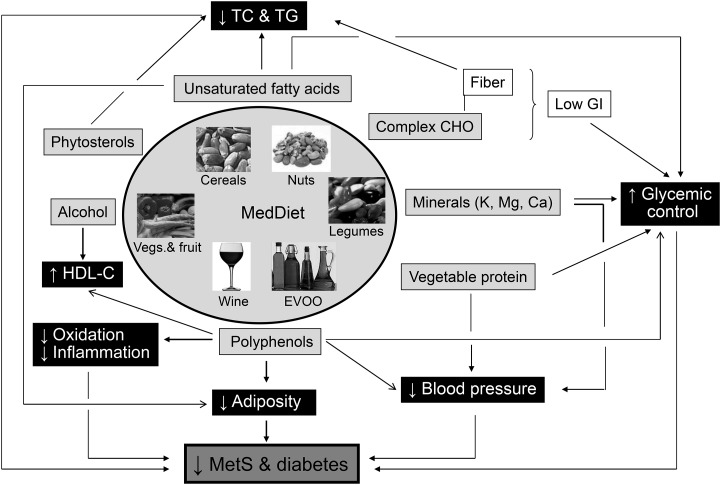
As stated, the traditional MedDiet is a plant-based dietary pattern that is fat-rich due to customary use of olive oil in the kitchen and at the table. Characteristically, there is abundant consumption of fresh vegetables, fruit, wholegrain cereal, legumes, and nuts; moderate consumption of seafood and wine; and reduced consumption of meat and meat products and sweet solid foods and beverages. The nutrient density in the complex matrices of plant foods, together with a low glycemic load, probably explain the lower risk of MetS and T2DM observed with higher adherence to the MedDiet. The main known bioactive food constituents of the MedDiet, namely unsaturated FAs, complex carbohydrate and fiber, vegetable protein, nonsodium minerals, phytosterols, and polyphenols appear to synergistically interact to beneficially affect various metabolic pathways in the risk of MetS, T2DM, and CVD in general (Figure 1). The scientific evidence on the bioactivity of these MedDiet components will be summarized to provide a mechanistic framework for their cardiometabolic benefit.
FIGURE 1.
Consumption of Mediterranean foods improves cardiometabolic health because of their rich composition in bioactive nutrients and phytochemicals and their synergizing effects on metabolic pathways. The main nutrients of the MedDiet are shown along with their principal biological targets (arrow connections). The net effects on intermediate markers of cardiometabolic disease risk shown for these nutrients and their parent foods in clinical trials include the lowering of cholesterol and TGs, increased HDL cholesterol, improved glycemic control, decreased blood pressure, reduced adiposity, and antioxidant and anti-inflammatory actions. The overall result is reduced MetS and type 2 diabetes mellitus risk, as suggested for most of the MedDiet in observational cohort studies and the PREvención con DIeta MEDiterránea trial. See text for details. CHO, carbohydrate; EVOO, extra-virgin olive oil; GI, glycemic index; HDL-C, HDL cholesterol; MedDiet, Mediterranean diet; MetS, metabolic syndrome; TC, total cholesterol; Vegs., vegetables. Adapted from reference 60 with permission.
FAs.
The MedDiet is rich in vegetable fat, which almost by definition is predominantly unsaturated, with a high proportion of MUFAs derived from olive oil and nuts and smaller amounts of essential PUFAs, such as linoleic (18:2n–6) and α-linolenic (18:3n–3) acids, derived from vegetables and nuts. It has been known for decades that SFA intake raises blood cholesterol and TGs, and that replacing SFAs with MUFAs or n–6 PUFAs decreases the concentrations of these lipids (61), with parallel effects on CVD risk (62). Also, substituting SFAs with unsaturated FAs, either MUFA or n–6 PUFA, improves insulin sensitivity and likely reduces the risk of T2DM (63). Dietary MUFA intake is also associated with the maintenance of body weight and a reduction in central body fat adiposity (64). n–3 PUFAs from seafood additionally contribute to the lowering of blood pressure and TGs, in addition to having a beneficial effect on adiposity (65). Thus, by way of salutary effects on lipid and glucose metabolism, the fat fraction of the MedDiet could help reduce cardiometabolic disease risk.
Carbohydrate and fiber.
Plant foods, particularly seeds (cereals, legumes, and nuts), are important sources of slow-release carbohydrate and dietary fiber. There are 2 main types of dietary fiber: metabolically inert insoluble fiber and bioactive soluble or viscous (gel-forming) fiber, which has cholesterol-lowering properties and reduces postprandial glucose responses after carbohydrate-rich meals (66). The main sources of insoluble fiber are cereal grains, whereas those of soluble fiber are fruit and vegetables. Observational studies have consistently shown that an increased intake of dietary fiber, usually from cereals rather than fruit and vegetables, is associated with a reduced incidence of T2DM (29). The reason for this apparent contradiction is that, in epidemiologic studies, insoluble fiber cannot easily be dissociated from whole-grain foods, which provide many other bioactive phytochemicals associated with beneficial health effects. Dietary fiber may also reduce MetS and T2DM risk through a reduction in blood pressure, improved insulin sensitivity, changes in secretion of gut hormones that act as satiety factors, and anti-inflammatory effects (67). Finally, the low glycemic index of the MedDiet is an additional factor that reduces insulin resistance and lowers the risk of T2DM (29).
Protein.
The consumption of vegetable protein, abundant in the MedDiet, relates inversely to blood pressure (68). The Optimal Macronutrient Intake Trial to Prevent Heart Disease (OmniHeart) trial showed that partial substitution of carbohydrate with protein (about one-half from plant sources) lowered blood pressure and improved the lipid profile in prehypertensive and hypertensive subjects (69). However, it is difficult to dissociate the benefit of the vegetable protein per se from the synergizing effects of other bioactive constituents in the protein-containing foods.
Minerals.
Plant foods, particularly seeds such as cereals, legumes, and nuts, contain little sodium but are rich in K+, Mg2+, and Ca2+. All 3 are critical in cellular metabolism and many physiologic processes, of which blood pressure regulation has been most studied. For instance, increased dietary mineral intake is thought to underlie the blood pressure–lowering effect of the DASH diet (70). There is also evidence from observational studies that suggests a protective effect from nonsodium minerals on T2DM, particularly for Mg2+ (71). This beneficial effect of minerals can be ascribed to their participation in intracellular processes related to glucose homeostasis leading to increased insulin sensitivity (72). Besides blood pressure reduction, an increased intake of K+, Mg2+, and Ca2+ in the DASH dietary pattern is also believed to be instrumental in its effect of improving insulin sensitivity (73), a clear example of nutrient synergy having a salutary effect on different metabolic pathways.
Sterols.
All plant foods are cholesterol-free, but their fatty fraction in nuts and oils contains sizeable amounts of chemically related noncholesterol sterols known as phytosterols, non-nutritive components that play important structural roles in membranes. Thus a MedDiet rich in olive oil and nuts is relatively rich in these compounds. Phytosterols interfere with cholesterol absorption in the intestinal lumen and thus have cholesterol-lowering properties, even at the low doses found in natural, nonsupplemented foods (74), and there is evidence that they also have a modest TG-lowering effect (75).
Polyphenols.
Phenolic compounds are strong antioxidants that are ubiquitous in plants. Because they need extra protection for the DNA of the future plant, seeds (cereal grains, legumes, nuts, cocoa, and coffee), fruits (particularly olives and grapes and derived products, unrefined or virgin olive oil, and red wine), and spices such as pepper or clove are rich in polyphenols (76). Besides their antioxidant power, these molecules appear to have pleiotropic effects, and there is mounting evidence that they may have an impact on human physiology in many ways, including in reduced adiposity and blood pressure, improved lipid profiles, and anti-inflammatory effects, in addition to protecting from CVD (77). Growing evidence also shows that polyphenol-rich foods and beverages reduce postprandial glycemic responses and fasting hyperglycemia and enhance insulin secretion and insulin sensitivity, with a suggested benefit on MetS and T2DM risk (78).
Alcohol.
Although red wine is the most common alcoholic drink consumed in the MedDiet, most scientific evidence on health effects stems from epidemiologic studies assessing exposure to alcoholic beverages in general. Besides a cardioprotective effect, moderate alcohol consumption also protects from diabetes, as shown in a meta-analysis of 20 cohort studies (79). There is inconclusive evidence regarding the effect of alcohol consumption on body weight (80). A meta-analysis of RCTs examining the effects of moderate alcohol consumption on cardiometabolic disease risk markers confirmed that the most consistent effect is increased HDL cholesterol, which is dose-dependent and occurs with any type of alcoholic beverage; thus, it may be ascribed to ethanol itself (81). Because HDL cholesterol, a component of MetS, relates inversely to CVD risk in epidemiologic studies (82), this has traditionally been considered the main mechanism for the cardiovascular protection of alcoholic beverages. However, the cardiovascular benefit of increasing HDL cholesterol is unclear, given the inconsistent evidence from HDL-raising pharmacologic trials (83). A meta-analysis that included studies with different alcoholic beverages suggests that moderate daily intake of wine and beer may confer higher protection against CVD than moderate intake of liquors and spirits, mainly because of the higher polyphenolic content of fermented alcoholic beverages (84). Polyphenols in red wine, not alcohol, also appear to have a blood pressure–lowering effect through increased nitrous oxide bioavailability, as shown by an RCT testing moderate doses of dealcoholized red wine (85). Finally, postprandial reduction of oxidative stress has also been observed after red wine consumption, an interesting effect that supports the Mediterranean way of drinking wine with meals (86).
As summarized in Figure 1, bioactive components of the MedDiet may synergize to affect various metabolic pathways, leading to a reduced risk of cardiometabolic disease. Such pleiotropic effects illustrate the importance of the MedDiet for protection from MetS and T2DM.
Conclusions and Perspectives for the Future
The abundance of healthy nutrient-dense foods that make up the plant-based MedDiet, characterized by high consumption of whole grains, vegetables, fruits, legumes, nuts, fish, and olive oil, predicts its bioactivity and potential to beneficially influence metabolic pathways leading to MetS and T2DM, as well as CVD and other chronic prevalent conditions. Abundant epidemiologic and clinical trial evidence supports the role of the MedDiet in preventing T2DM and MetS by way of a beneficial impact on cardiometabolic disease risk factors, including all components of MetS. Importantly, this benefit is achieved even though the MedDiet is a high-fat dietary pattern. The fat, however, is of vegetable origin and mostly unsaturated and comes to the MedDiet in the form of complex matrices, such as olive oil and tree nuts, which also contain highly bioactive micronutrients and phytochemicals. In this sense, the high-fat MedDiet is clearly superior to the long-recommended low-fat dietary pattern in terms of both cardiometabolic benefit and palatability, as demonstrated by the landmark PREDIMED trial.
The future looks bright for the MedDiet and its main components, as scientific societies worldwide recognize its many beneficial aspects and recommend its inclusion in public health policy, in good part thanks to the impact of the PREDIMED study. Nevertheless, MetS and T2DM were secondary outcomes of the PREDIMED study, and nutritional science would be well served if more RCTs of the MedDiet targeting cardiometabolic disease risk markers, MetS, and T2DM were undertaken.
Acknowledgments
JS-S, MG-F, and ER provided the scope of the research, oversaw the writing of the manuscript, and wrote the manuscript; and C-HL, RE, and CBC revised the manuscript for important intellectual content. All authors read and approved the final manuscript.
Footnotes
Abbreviations used: CVD, cardiovascular disease; DASH, Dietary Approaches to Stop Hypertension; MedDiet, Mediterranean diet; MetS, metabolic syndrome; PREDIMED, PREvención con DIeta MEDiterránea; RCT, randomized controlled trial; T2DM, type 2 diabetes mellitus.
References
- 1.International Diabetes Federation. IDF diabetes atlas. 6th ed 2014. [Google Scholar]
- 2.Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, Fruchart JC, James WP, Loria CM, Smith SC Jr, et al. Harmonizing the metabolic syndrome: A joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International. Circulation 2009;120:1640–5. [DOI] [PubMed] [Google Scholar]
- 3.Athyros VG, Ganotakis ES, Elisaf M, Mikhailidis DP. The prevalence of the metabolic syndrome using the National Cholesterol Educational Program and International Diabetes Federation definitions. Curr Med Res Opin 2005;21:1157–9. [DOI] [PubMed] [Google Scholar]
- 4.Ford ES, Li C, Zhao G. Prevalence and correlates of metabolic syndrome based on a harmonious definition among adults in the US. J Diabetes 2010;2:180–93. [DOI] [PubMed] [Google Scholar]
- 5.Narayan KM, Gregg EW, Fagot-Campagna A, Engelgau MM, Vinicor F. Diabetes-A common, growing, serious, costly, and potentially preventable public health problem. Diabetes Res Clin Pract 2000;50 Suppl 2:S77–84. [DOI] [PubMed] [Google Scholar]
- 6.Tuomilehto J, Lindstrom J, Eriksson JG, Valle TT, Hamalainen H, Ilanne-Parikka P, Keinanen-Kiukaanniemi S, Laakso M, Louheranta A, Rastas M, et al. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med 2001;344:1343–50. [DOI] [PubMed] [Google Scholar]
- 7.Knowler WC, Fowler SE, Hamman RF, Christophi CA, Hoffman HJ, Brenneman AT, Brown-Friday JO, Goldberg R, Venditti E, Nathan DM. 10-year follow-up of diabetes incidence and weight loss in the Diabetes Prevention Program Outcomes Study. Lancet 2009;374:1677–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Li G, Zhang P, Wang J, An Y, Gong Q, Gregg EW, Yang W, Zhang B, Shuai Y, Hong J, et al. Cardiovascular mortality, all-cause mortality, and diabetes incidence after lifestyle intervention for people with impaired glucose tolerance in the Da Qing Diabetes Prevention Study: a 23-year follow-up study. Lancet Diabetes Endocrinol 2014;2:474–80. [DOI] [PubMed] [Google Scholar]
- 9.Trichopoulou A, Costacou T, Bamia C, Trichopoulos D. Adherence to a Mediterranean diet and survival in a Greek population. N Engl J Med 2003;348:2599–608. [DOI] [PubMed] [Google Scholar]
- 10.Bach A, Serra-Majem L, Carrasco JL, Roman B, Ngo J, Bertomeu I, Obrador B. The use of indexes evaluating the adherence to the Mediterranean diet in epidemiological studies: a review. Public Health Nutr 2006;9:132–46. [DOI] [PubMed] [Google Scholar]
- 11.Estruch R, Martínez-González MA, Corella D, Salas-Salvadó J, Ruiz-Gutiérrez V, Covas MI, Fiol M, Gómez-Gracia E, López-Sabater MC, Vinyoles E, et al. Effects of a Mediterranean-style diet on cardiovascular risk factors: a randomized trial. Ann Intern Med 2006;145:1–11. [DOI] [PubMed] [Google Scholar]
- 12.Goulet J, Lapointe A, Lamarche B, Lemieux S. Effect of a nutritional intervention promoting the Mediterranean food pattern on anthropometric profile in healthy women from the Québec city metropolitan area. Eur J Clin Nutr 2007;61:1293–300. [DOI] [PubMed] [Google Scholar]
- 13.Leighton F, Polic G, Strobel P, Pérez D, Martínez C, Vásquez L, Castillo O, Villarroel L, Echeverría G, Urguiaga I, et al. Health impact of Mediterranean diets in food at work. Public Health Nutr 2009;12:1635–43. [DOI] [PubMed] [Google Scholar]
- 14.Gomez-Huelgas R, Jansen-Chaparro S, Baca-Osorio AJ, Mancera-Romero J, Tinahones FJ, Bernal-López MR. Effects of a long-term lifestyle intervention program with Mediterranean diet and exercise for the management of patients with metabolic syndrome in a primary care setting. Eur J Intern Med 2015;26:317–23. [DOI] [PubMed] [Google Scholar]
- 15.Huo R, Du T, Xu Y, Xu W, Chen X, Sun K, Yu X. Effects of Mediterranean-style diet on glycemic control, weight loss and cardiovascular risk factors among type 2 diabetes individuals: a meta-analysis. Eur J Clin Nutr 2014; Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 16.Babio N, Bulló M, Salas-Salvadó J. Mediterranean diet and metabolic syndrome: the evidence. Public Health Nutr 2009;12:1607–17. [DOI] [PubMed] [Google Scholar]
- 17.Kastorini C-M, Milionis HJ, Esposito K, Giugliano D, Goudevenos JA, Panagiotakos DB. The effect of Mediterranean diet on metabolic syndrome and its components: a meta-analysis of 50 studies and 534,906 individuals. J Am Coll Cardiol 2011;57:1299–313. [DOI] [PubMed] [Google Scholar]
- 18.Salas-Salvadó J, Bulló M, Estruch R, Ros E, Covas M-I, Ibarrola-Jurado N, Corella D, Arós F, Gómez-Gracia E, Ruiz-Gutiérrez V, et al. Prevention of diabetes with Mediterranean diets: a subgroup analysis of a randomized trial. Ann Intern Med 2014;160:1–10. [DOI] [PubMed] [Google Scholar]
- 19.Sala-Vila A, Estruch R, Ros E. New insights into the role of nutrition in CVD prevention. Curr Cardiol Rep 2015;17:26. [DOI] [PubMed] [Google Scholar]
- 20.de Koning L, Chiuve SE, Fung TT, Willett WC, Rimm EB, Hu FB. Diet-quality scores and the risk of type 2 diabetes in men. Diabetes Care 2011;34:1150–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mozaffarian D, Marfisi R, Levantesi G, Silletta MG, Tavazzi L, Tognoni G, Valagussa F, Marchioli R. Incidence of new-onset diabetes and impaired fasting glucose in patients with recent myocardial infarction and the effect of clinical and lifestyle risk factors. Lancet 2007;370:667–75. [DOI] [PubMed] [Google Scholar]
- 22.Martínez-González MA, de la Fuente-Arrillaga C, Nunez-Cordoba JM, Basterra-Gortari FJ, Beunza JJ, Vazquez Z, Benito S, Tortosa A, Bes-Rastrollo M. Adherence to Mediterranean diet and risk of developing diabetes: prospective cohort study. BMJ 2008;336:1348–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Romaguera D, Guevara M, Norat T, Langenberg C, Forouhi NG, Sharp S, Slimani N, Schulze MB, Buijsse B, et al. Mediterranean diet and type 2 diabetes risk in the European Prospective Investigation into Cancer and Nutrition (EPIC) study: The InterAct project. Diabetes Care 2011;34:1913–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tobias DK, Zhang C, Chavarro J, Bowers K, Rich-Edwards J, Rosner B, Mozaffarian D, Hu FB. Prepregnancy adherence to dietary patterns and lower risk of gestational diabetes mellitus. Am J Clin Nutr 2012;96:289–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tobias DK, Hu FB, Chavarro J, Rosner B, Mozaffarian D, Zhang C. Healthful dietary patterns and type 2 diabetes mellitus risk among women with a history of gestational diabetes mellitus. Arch Intern Med 2012;172:1566–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Abiemo EE, Alonso A, Nettleton JA, Steffen LM, Bertoni AG, Jain A, Lutsey PL. Relationships of the Mediterranean dietary pattern with insulin resistance and diabetes incidence in the Multi-Ethnic Study of Atherosclerosis (MESA). Br J Nutr 2013;109:1490–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rossi M, Turati F, Lagiou P, Trichopoulos D, Augustin LS, La Vecchia C, Trichopoulou A. Mediterranean diet and glycaemic load in relation to incidence of type 2 diabetes: results from the Greek cohort of the population-based European Prospective Investigation into Cancer and Nutrition (EPIC). Diabetologia 2013;56:2405–13. [DOI] [PubMed] [Google Scholar]
- 28.Salas-Salvadó J, Martinez-Gonzalez MA, Bullo M, Ros E. The role of diet in the prevention of type 2 diabetes. Nutr Metab Cardiovasc Dis 2011;21 Suppl 2:B32–48. [DOI] [PubMed] [Google Scholar]
- 29.Ley SH, Hamdy O, Mohan V, Hu FB. Prevention and management of type 2 diabetes: Dietary components and nutritional strategies. Lancet 2014;383:1999–2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Alhazmi A, Stojanovski E, McEvoy M, Garg ML. The association between dietary patterns and type 2 diabetes: a systematic review and meta-analysis of cohort studies. J Hum Nutr Diet 2014;27:251–60. [DOI] [PubMed] [Google Scholar]
- 31.Panagiotakos DB, Pitsavos C, Chrysohoou C, Stefanadis C. The epidemiology of type 2 diabetes mellitus in Greek adults: the ATTICA study. Diabet Med 2005;22:1581–8. [DOI] [PubMed] [Google Scholar]
- 32.Ortega E, Franch J, Castell C, Goday A, Ribas-Barba L, Soriguer F, Vendrell J, Casamitjana R, Bosch-Comas A, Bordiú E, et al. Mediterranean diet adherence in individuals with prediabetes and unknown diabetes: The Di@bet.es Study. Ann Nutr Metab 2013;62:339–46. [DOI] [PubMed] [Google Scholar]
- 33.Koloverou E, Panagiotakos DB, Pitsavos C, Chrysohoou C, Georgousopoulou EN, Grekas A, Christou A, Chatzigeorgiou M, Skoumas I, Tousoulis D, et al. Adherence to Mediterranean diet and 10-year incidence (2002–2012) of diabetes: Correlations with inflammatory and oxidative stress biomarkers in the ATTICA cohort study. Diabetes Metab Res Rev 2015; Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 34.Koloverou E, Esposito K, Giugliano D, Panagiotakos D. The effect of Mediterranean diet on the development of type 2 diabetes mellitus: A meta-analysis of 10 prospective studies and 136,846 participants. Metabolism 2014;63:903–11. [DOI] [PubMed] [Google Scholar]
- 35.Schwingshackl L, Missbach B, König J, Hoffmann G. Adherence to a Mediterranean diet and risk of diabetes: a systematic review and meta-analysis. Public Health Nutr 2015;18:1292–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Guyatt G, Oxman AD, Akl EA, Kunz R, Vist G, Brozek J, Norris S, Falck-Ytter Y, Glasziou P, DeBeer H, et al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol 2011;64:383–94. [DOI] [PubMed] [Google Scholar]
- 37.American Diabetes Association. Gestational diabetes mellitus. Diabetes Care 2004;27 Suppl 1:S88–90. [DOI] [PubMed] [Google Scholar]
- 38.Bellamy L, Casas J-P, Hingorani AD, Williams D. Type 2 diabetes mellitus after gestational diabetes: A systematic review and meta-analysis. Lancet 2009;373:1773–9. [DOI] [PubMed] [Google Scholar]
- 39.Karamanos B, Thanopoulou A, Anastasiou E, Assaad-Khalil S, Albache N, Bachaoui M, Slama CB, El Ghomari H, Jotic A, Lalic N, et al. Relation of the Mediterranean diet with the incidence of gestational diabetes. Eur J Clin Nutr 2014;68:8–13. [DOI] [PubMed] [Google Scholar]
- 40.Paletas K, Athanasiadou E, Sarigianni M, Paschos P, Kalogirou A, Hassapidou M, Tsapas A. The protective role of the Mediterranean diet on the prevalence of metabolic syndrome in a population of Greek obese subjects. J Am Coll Nutr 2010;29:41–5. [DOI] [PubMed] [Google Scholar]
- 41.Gouveri ET, Tzavara C, Drakopanagiotakis F, Tsaoussoglou M, Marakomichelakis GE, Tountas Y, Diamantopoulos EJ. Mediterranean diet and metabolic syndrome in an urban population: the Athens Study. Nutr Clin Pract 2011;26:598–606. [DOI] [PubMed] [Google Scholar]
- 42.Viscogliosi G, Cipriani E, Liguori ML, Marigliano B, Saliola M, Ettorre E, Andreozzi P. Mediterranean dietary pattern adherence: Associations with prediabetes, metabolic syndrome, and related microinflammation. Metab Syndr Relat Disord 2013;11:210–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Grosso G, Stepaniak U, Micek A, Topor-Mądry R, Stefler D, Szafraniec K, Bobak M, Pająk A. A Mediterranean-type diet is associated with better metabolic profile in urban Polish adults: Results from the HAPIEE study. Metabolism 2015;64:738–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tortosa A, Bes-Rastrollo M, Sanchez-Villegas A, Basterra-Gortari FJ, Nuñez-Cordoba JM, Martinez-Gonzalez MA. Mediterranean diet inversely associated with the incidence of metabolic syndrome: The SUN prospective cohort. Diabetes Care 2007;30:2957–9. [DOI] [PubMed] [Google Scholar]
- 45.Rumawas ME, Dwyer JT, McKeown NM, Meigs JB, Rogers G, Jacques PF. The development of the Mediterranean-style dietary pattern score and its application to the American diet in the Framingham Offspring Cohort. J Nutr 2009;139:1150–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kesse-Guyot E, Ahluwalia N, Lassale C, Hercberg S, Fezeu L, Lairon D. Adherence to Mediterranean diet reduces the risk of metabolic syndrome: A 6-year prospective study. Nutr Metab Cardiovasc Dis 2013;23:677–83. [DOI] [PubMed] [Google Scholar]
- 47.Steffen LM, Van Horn L, Daviglus ML, Zhou X, Reis JP, Loria CM, Jacobs DR, Duffey KJ. A modified Mediterranean diet score is associated with a lower risk of incident metabolic syndrome over 25 years among young adults: The CARDIA (Coronary Artery Risk Development in Young Adults) study. Br J Nutr 2014;112:1654–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Salas-Salvadó J, Bulló M, Babio N, Martínez-González MÁ, Ibarrola-Jurado N, Basora J, Estruch R, Covas MI, Corella D, Arós F, et al. Reduction in the incidence of type 2 diabetes with the Mediterranean diet: results of the PREDIMED-Reus nutrition intervention randomized trial. Diabetes Care 2011;34:14–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Toobert DJ, Glasgow RE, Strycker LA, Barrera M, Radcliffe JL, Wander RC, Bagdade JD. Biologic and quality-of-life outcomes from the Mediterranean Lifestyle Program: A randomized clinical trial. Diabetes Care 2003;26:2288–93. [DOI] [PubMed] [Google Scholar]
- 50.Shai I, Schwarzfuchs D, Henkin Y, Shahar DR, Witkow S, Greenberg I, Golan R, Fraser D, Bolotin A, Vardi H, et al. Weight loss with a low-carbohydrate, Mediterranean, or low-fat diet. N Engl J Med 2008;359:229–41. [DOI] [PubMed] [Google Scholar]
- 51.Esposito K, Maiorino MI, Ciotola M, Di Palo C, Scognamiglio P, Gicchino M, Petrizzo M, Saccomanno F, Beneduce F, Ceriello A, et al. Effects of a Mediterranean-style diet on the need for antihyperglycemic drug therapy in patients with newly diagnosed type 2 diabetes: A randomized trial. Ann Intern Med 2009;151:306–14. [DOI] [PubMed] [Google Scholar]
- 52.Elhayany A, Lustman A, Abel R, Attal-Singer J, Vinker S. A low carbohydrate Mediterranean diet improves cardiovascular risk factors and diabetes control among overweight patients with type 2 diabetes mellitus: A 1-year prospective randomized intervention study. Diabetes Obes Metab 2010;12:204–9. [DOI] [PubMed] [Google Scholar]
- 53.Ajala O, English P, Pinkney J. Systematic review and meta-analysis of different dietary approaches to the management of type 2 diabetes. Am J Clin Nutr 2013;97:505–16. [DOI] [PubMed] [Google Scholar]
- 54.Barzi F, Woodward M, Marfisi RM, Tavazzi L, Valagussa F, Marchioli R. Mediterranean diet and all-causes mortality after myocardial infarction: results from the GISSI-Prevenzione trial. Eur J Clin Nutr 2003;57:604–11. [DOI] [PubMed] [Google Scholar]
- 55.Estruch R, Ros E, Salas-Salvado J, Covas MI, Corella D, Aros F, Gomez-Gracia E, Ruiz-Gutierrez V, Fiol M, Lapetra J, et al. Primary prevention of cardiovascular disease with a Mediterranean diet. N Engl J Med 2013;368:1279–90. [DOI] [PubMed] [Google Scholar]
- 56.Salas-Salvadó J, Fernandez-Ballart J, Ros E, Martinez-Gonzalez MA, Fito M, Estruch R, Corella D, Fiol M, Gomez-Gracia E, Arós F, et al. Effect of a Mediterranean diet supplemented with nuts on metabolic syndrome status: One-year results of the PREDIMED randomized trial. Arch Intern Med 2008;168:2449–58. [DOI] [PubMed] [Google Scholar]
- 57.Babio N, Toledo E, Estruch R, Ros E, Martínez-González MA, Castañer O, Bulló M, Corella D, Arós F, Gómez-Gracia E, et al. Mediterranean diets and metabolic syndrome status in the PREDIMED randomized trial. CMAJ 2014;186:E649–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Mitjavila MT, Fandos M, Salas-Salvadó J, Covas M-I, Borrego S, Estruch R, Lamuela-Raventós R, Corella D, Martínez-Gonzalez MÁ, Sánchez JM, et al. The Mediterranean diet improves the systemic lipid and DNA oxidative damage in metabolic syndrome individuals. A randomized, controlled, trial. Clin Nutr 2013;32:172–8. [DOI] [PubMed] [Google Scholar]
- 59.Esposito K, Marfella R, Ciotola M, Di Palo C, Giugliano F, Giugliano G, D’Armiento M, D’Andrea F, Giugliano D. Effect of a Mediterranean-style diet on endothelial dysfunction and markers of vascular inflammation in the metabolic syndrome: A randomized trial. JAMA 2004;292:1440–6. [DOI] [PubMed] [Google Scholar]
- 60.Ros E and Hu FB. Consumption of plant seeds and cardiovascular health: Epidemiologic and clinical trial evidence. Circulation 2013;128:553–65. [DOI] [PMC free article] [PubMed]
- 61.Mensink RP, Zock PL, Kester ADM, Katan MB. Effects of dietary fatty acids and carbohydrates on the ratio of serum total to HDL cholesterol and on serum lipids and apolipoproteins: a meta-analysis of 60 controlled trials. Am J Clin Nutr 2003;77:1146–55. [DOI] [PubMed] [Google Scholar]
- 62.Mente A, de Koning L, Shannon HS, Anand SS. A systematic review of the evidence supporting a causal link between dietary factors and coronary heart disease. Arch Intern Med 2009;169:659–69. [DOI] [PubMed] [Google Scholar]
- 63.Risérus U, Willett WC, Hu FB. Dietary fats and prevention of type 2 diabetes. Prog Lipid Res 2009;48:44–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Gillingham LG, Harris-Janz S, Jones PJH. Dietary monounsaturated fatty acids are protective against metabolic syndrome and cardiovascular disease risk factors. Lipids 2011;46:209–28. [DOI] [PubMed] [Google Scholar]
- 65.Poudyal H, Panchal SK, Diwan V, Brown L. Omega-3 fatty acids and metabolic syndrome: effects and emerging mechanisms of action. Prog Lipid Res 2011;50:372–87. [DOI] [PubMed] [Google Scholar]
- 66.Jenkins DJ, Kendall CW, Axelsen M, Augustin LS, Vuksan V. Viscous and nonviscous fibres, nonabsorbable and low glycaemic index carbohydrates, blood lipids and coronary heart disease. Curr Opin Lipidol 2000;11:49–56. [DOI] [PubMed] [Google Scholar]
- 67.Weickert MO, Pfeiffer AFH. Metabolic effects of dietary fiber consumption and prevention of diabetes. J Nutr 2008;138:439–42. [DOI] [PubMed] [Google Scholar]
- 68.Altorf-van der Kuil W, Engberink MF, Brink EJ, van Baak MA, Bakker SJL, Navis G, van ’t Veer P, Geleijnse JM. Dietary protein and blood pressure: A systematic review. PLoS One 2010;5:e12102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Appel LJ, Sacks FM, Carey VJ, Obarzanek E, Swain JF, Miller ER, Conlin PR, Erlinger TP, Rosner BA, Laranjo NM, et al. Effects of protein, monounsaturated fat, and carbohydrate intake on blood pressure and serum lipids: Results of the OmniHeart randomized trial. JAMA 2005;294:2455–64. [DOI] [PubMed] [Google Scholar]
- 70.Akita S, Sacks FM, Svetkey LP, Conlin PR, Kimura G. Effects of the Dietary Approaches to Stop Hypertension (DASH) diet on the pressure-natriuresis relationship. Hypertension 2003;42:8–13. [DOI] [PubMed] [Google Scholar]
- 71.Dong J-Y, Zhang Y-H, Wang P, Qin L-Q. Meta-analysis of dietary glycemic load and glycemic index in relation to risk of coronary heart disease. Am J Cardiol 2012;109:1608–13. [DOI] [PubMed] [Google Scholar]
- 72.Martini LA, Catania AS, Ferreira SRG. Role of vitamins and minerals in prevention and management of type 2 diabetes mellitus. Nutr Rev 2010;68:341–54. [DOI] [PubMed] [Google Scholar]
- 73.Ard JD, Grambow SC, Liu D, Slentz CA, Kraus WE, Svetkey LP. The effect of the PREMIER interventions on insulin sensitivity. Diabetes Care 2004;27:340–7. [DOI] [PubMed] [Google Scholar]
- 74.Escurriol V, Cofán M, Serra M, Bulló M, Basora J, Salas-Salvadó J, Corella D, Zazpe I, Martínez-González MA, Ruiz-Gutiérrez V, et al. Serum sterol responses to increasing plant sterol intake from natural foods in the Mediterranean diet. Eur J Nutr 2009;48:373–82. [DOI] [PubMed] [Google Scholar]
- 75.Demonty I, Ras RT, van der Knaap HCM, Meijer L, Zock PL, Geleijnse JM, Trautwein EA. The effect of plant sterols on serum triglyceride concentrations is dependent on baseline concentrations: A pooled analysis of 12 randomised controlled trials. Eur J Nutr 2013;52:153–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Pérez-Jiménez J, Neveu V, Vos F, Scalbert A. Identification of the 100 richest dietary sources of polyphenols: An application of the Phenol-Explorer database. Eur J Clin Nutr 2010;64 Suppl 3:S112–20. [DOI] [PubMed] [Google Scholar]
- 77.Del Rio D, Rodriguez-Mateos A, Spencer JPE, Tognolini M, Borges G, Crozier A. Dietary (poly)phenolics in human health: Structures, bioavailability, and evidence of protective effects against chronic diseases. Antioxid Redox Signal 2013;18:1818–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Hanhineva K, Törrönen R, Bondia-Pons I, Pekkinen J, Kolehmainen M, Mykkänen H, Poutanen K. Impact of dietary polyphenols on carbohydrate metabolism. Int J Mol Sci 2010;11:1365–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Baliunas DO, Taylor BJ, Irving H, Roerecke M, Patra J, Mohapatra S, Rehm J. Alcohol as a risk factor for type 2 diabetes: A systematic review and meta-analysis. Diabetes Care 2009;32:2123–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Sayon-Orea C, Martinez-Gonzalez MA, Bes-Rastrollo M. Alcohol consumption and body weight: a systematic review. Nutr Rev 2011;69:419–31. [DOI] [PubMed] [Google Scholar]
- 81.Brien SE, Ronksley PE, Turner BJ, Mukamal KJ, Ghali WA. Effect of alcohol consumption on biological markers associated with risk of coronary heart disease: systematic review and meta-analysis of interventional studies. BMJ 2011;342:d636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Di Angelantonio E, Sarwar N, Perry P, Kaptoge S, Ray KK, Thompson A, Wood AM, Lewington S, Sattar N, et al. Major lipids, apolipoproteins, and risk of vascular disease. JAMA 2009;302:1993–2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Keene D, Price C, Shun-Shin MJ, Francis DP. Effect on cardiovascular risk of high density lipoprotein targeted drug treatments niacin, fibrates, and CETP inhibitors: Meta-analysis of randomised controlled trials including 117,411 patients. BMJ 2014;349:g4379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Costanzo S, Di Castelnuovo A, Donati MB, Iacoviello L, de Gaetano G. Wine, beer or spirit drinking in relation to fatal and non-fatal cardiovascular events: A meta-analysis. Eur J Epidemiol 2011;26:833–50. [DOI] [PubMed] [Google Scholar]
- 85.Chiva-Blanch G, Urpi-Sarda M, Ros E, Arranz S, Valderas-Martínez P, Casas R, Sacanella E, Llorach R, Lamuela-Raventos RM, Andres-Lacueva C, et al. Dealcoholized red wine decreases systolic and diastolic blood pressure and increases plasma nitric oxide: Short communication. Circ Res 2012;111:1065–8. [DOI] [PubMed] [Google Scholar]
- 86.Covas MI, Gambert P, Fitó M, de la Torre R. Wine and oxidative stress: Up-to-date evidence of the effects of moderate wine consumption on oxidative damage in humans. Atherosclerosis 2010;208:297–304. [DOI] [PubMed] [Google Scholar]