Abstract
Background: The dietary sodium-to-potassium ratio (Na:K) is shown to be more strongly associated with an increased risk of cardiovascular disease (CVD) and CVD-related mortality than either sodium or potassium intake alone.
Objective: The aim was to estimate the Na:K in the diet of US adults.
Methods: Among US adults from the 2011–2012 NHANES (≥20 y; 2393 men and 2337 women), the National Cancer Institute method was used to estimate sodium and potassium intakes, Na:K, and the percentage of individuals with Na:K <1.0 utilizing the complex, stratified, multistage probability cluster sampling design.
Results: Overall, women had a significantly lower Na:K than men (mean ± SE: 1.32 ± 0.02 compared with 1.45 ± 0.02). Non-Hispanic whites had a significantly lower Na:K than non-Hispanic blacks and non-Hispanic Asians (1.34 ± 0.02 compared with 1.54 ± 0.03 and 1.49 ± 0.04, respectively). Only 12.2% ± 1.5% of US adults had a Na:K < 1.0. The Na:K decreased linearly as age increased. Most adults (90% ± 0.8%) had sodium intakes >2300 mg/d, whereas <3% had potassium intakes >4700 mg/d. Grains and vegetables were among the highest contributors to sodium intakes for adults with Na:K < 1.0, compared with protein foods and grains for those with Na:K ≥ 1.0. Vegetables and milk and dairy products constituted the primary dietary sources of potassium for individuals with Na:K < 1.0, whereas mixed dishes and protein foods contributed the most potassium for individuals with ratios ≥1.0. Individuals with a Na:K < 1.0 were less likely to consume mixed dishes and condiments and were more likely to consume vegetables, milk and dairy products, and fruit than those with a Na:K ≥ 1.0.
Conclusion: Only about one-tenth of US adults have a Na:K consistent with the WHO guidelines for reduced risk of mortality. Continued efforts to reduce sodium intake in tandem with novel strategies to increase potassium intake are warranted.
Keywords: sodium, potassium, ratio, NHANES, Na:K, diet
Introduction
Sodium and potassium are 2 critical minerals that have consistently been identified as nutrients of concern in the American diet (1). Although health professionals continue to express concerns over high sodium intakes (2), potassium intakes in the US population are also short of the recommendations (3). These 2 cations have an inverse relation in the body, complicating this known intake imbalance. Because of this, it is important to examine not only individual mineral intakes but also the ratio of these 2 minerals in the diet. Recent data suggest that the dietary sodium-to-potassium ratio (Na:K)8 is more strongly associated with an increased risk of hypertension and cardiovascular disease (CVD)-related mortality than the risk associated from either sodium or potassium alone (4–6).
Determining the ideal Na:K has been a matter of debate, mainly because of controversy about what constitutes an ideal sodium intake. The WHO recommends sodium intake <2000 mg/d, whereas US guidance suggests that 1500 mg/d is adequate and <2400 mg/d or <2300 mg/d is recommended (7). The Adequate Intake level for potassium is set at 4700 mg/d for adults in the United States and Canada (8), whereas the WHO guideline is ≥3510 mg/d for adults (9). According to these recommendations, the Na:K would be <0.49 (i.e., 2300 mg Na/d and 4700 mg K/d) for healthy individuals. However, in a historic analysis of the diets of Americans from the 1971–2006 NHANES, Drewnowski et al. (10) showed that the Na:K was never <0.83 in this population; in fact, only <0.015% of the population achieved the recommended Na:K. However, the report by Drewnowski et al. (10) did not use the procedures for estimation of usual intakes of Americans when drawing such conclusions; that is, the data were not adjusted for within-person variability, which is known to substantially influence prevalence estimates at the tails of the distribution (11–14). To monitor the nutrition status of the American population, researchers are often interested in the usual or long-term intake of nutrients (15). The 24-h dietary recall can capture rich details about dietary intake for a given day, but individual diets can vary greatly from day to day. Thus, this measure is not reflective of usual or habitual intake (13, 16, 17). Several statistical methods were previously reported to adjust the 24-h dietary recall to better estimate the long-term intake of a particular nutrient (11, 15, 18–20). With the use of data from NHANES III (1988–1994), Yang et al. (5) found a beneficial protective effect of usual Na:Ks < 1.0 and a reduced risk of CVD and all-cause mortality (5). In light of these findings, this study aimed to 1) characterize the usual intakes of sodium and potassium and the Na:K, 2) evaluate adherence to the target Na:K, and 3) examine dietary patterns by Na:K in the most recently available data on the current diets of American adults.
Methods
NHANES is a nationally representative, cross-sectional survey that samples noninstitutionalized, civilian US residents with the use of a complex, stratified, multistage probability cluster sampling design (21). NHANES is conducted by the US CDC National Center for Health Statistics, who obtained written informed consent for all participants or proxies. The NHANES survey protocol was approved by the National Center for Health Statistics research ethics review board.
In this study, data from the 2011–2012 NHANES were assessed for adults (age ≥20 y; n = 5560). From this sample, fewer adults participated in the examination component (n = 5319); we excluded individuals who did not complete or who had incomplete 24-h dietary recall data (n = 519) or women who were pregnant and/or lactating (n = 70). Thus, this study includes data for 4730 participants.
NHANES participants were asked to complete an in-person household interview, during which time demographic data (including age, sex, and race/ethnicity) were collected through a computer-assisted personal interview. Self-reported racial/ethnic groups, as defined in NHANES and used in this analysis, were as follows: non-Hispanic white, non-Hispanic black, Hispanic, non-Hispanic Asian, and “other” (referred to hereafter as white, black, Hispanic, and Asian). After NHANES participants completed the in-person interview, they underwent a health examination in a Mobile Examination Center, and an in-person 24-h dietary recall was collected as part of the What We Eat in America survey (22). Finally, another 24-h dietary recall was collected via a telephone interview 3–10 d after the visit to ensure that weekday and weekend days were represented. Dietary data were weighted for day of the week of collection to ensure equal distribution across each day of the week. Both 24-h recalls were collected with the use of the USDA’s Automated Multiple-Pass Method (AMPM) (23, 24). The 2011–2012 USDA Food and Nutrient Database for Dietary Studies was used to convert foods and beverages as consumed into gram amounts and to determine their respective nutrient values (25). Foods and beverages were grouped with the use of the 2011–2012 What We Eat in America Food Categories to identify their contributions to sodium and potassium in the diet. Discretionary salt added at the table was not quantified. Because dietary supplements do not contribute substantially to sodium or potassium intakes and are not commonly found in high amounts in US products, supplements were not included in these estimates.
Urinary sodium and potassium are considered the gold standard method of assessment for sodium and potassium intakes but were not available during these survey years for analysis. Validation studies reported accuracy, calculated as the ratio of reported sodium intake to that estimated from the urinary biomarker, as 0.93 (95% CI: 0.89, 0.97) for men and 0.90 (95% CI: 0.87, 0.94) for women on average (26).
All statistical analyses were performed with the use of SAS software (version 9.3; SAS Institute Inc) and SAS-callable Sudaan software (version 11.0; RTI International). Sample weights were used to account for differential nonresponse and/or noncoverage, to adjust for planned oversampling of some groups, and to adjust for uneven representation of days of the week. Means and SEs were estimated for sodium and potassium intakes per 1000 kcal and are presented in mg/d. The Na:K was estimated for each participant.
The means and percentages presented in Tables 1 and 2 reflect an adjustment for within-person variability with the use of the amount-only part of the National Cancer Institute method to estimate usual intake distributions (15). The covariates in the model included the sequence and mode of administration of the 24-h dietary recall and the day of the week on which the 24-h dietary recall was collected, dichotomized as the weekend (Friday to Sunday) or weekday (Monday to Thursday). The National Cancer Institute method was also used to estimate the mean intakes per 1000 kcal, the mean Na:K, and the percentage of individuals with a Na:K < 1.0 over the long term. SEs for the usual intake statistics were approximated by Fay’s Modified Balanced Repeated Replication technique (27, 28). Replicate weights were post-stratified to control totals computed from the initial sample weights. One-day mean intakes were used to compare between individuals by the WHO Na:Ks (i.e., <1.0 compared with ≥1.0) (Figure 1, Table 3, and Supplemental Tables 1 and 2). SEs were approximated by the Taylor Series Expansion. Multiple pairwise t tests were used for all comparisons between population groups, with df dictated by the NHANES sample design. Statistical significance was set at P ≤0.01.
TABLE 1.
Dietary sodium, energy, and potassium intakes adjusted for day-to-day variability in the diets of US adults (≥20 y) by sex, age, and race/ethnicity, NHANES 2011–20121
| Sodium |
Potassium |
|||||||
| n | Energy, kcal/d | mg/d | mg/(d · 1000 kcal) | >2300 mg/d, % | mg/d | mg/(d · 1000 kcal) | <4700 mg/d, % | |
| All adults | 4730 | 2048 ± 16 | 3584 ± 29 | 1741 ± 8 | 90 ± 1 | 2795 ± 34 | 1396 ± 12 | <3 |
| Age, y | ||||||||
| 20–39 | 1647 | 2182 ± 25a | 3910 ± 41a | 1741 ± 17 | 96 ± 1a | 2769 ± 41 | 1268 ± 15c | <3 |
| 40–59 | 1582 | 2081 ± 28b | 3635 ± 58b | 1745 ± 18 | 90 ± 1b | 2859 ± 56 | 1414 ± 20b | <3 |
| ≥60 | 1501 | 1830 ± 24c | 3095 ± 52c | 1738 ± 26 | 82 ± 2c | 2745 ± 42 | 1542 ± 16a | <3 |
| Race/ethnicity | ||||||||
| Non-Hispanic white | 1815 | 2061 ± 25a | 3452 ± 39a,b | 1727 ± 11b | 87 ± 2a,b | 2797 ± 45a | 1429 ± 19a,b | <3 |
| Non-Hispanic black | 1253 | 1998 ± 33a,b | 3310 ± 50b | 1719 ± 17b | 84 ± 2b | 2360 ± 49b | 1241 ± 19c | <3 |
| Hispanic | 920 | 2069 ± 48a | 3489 ± 66a,b | 1727 ± 23b | 88 ± 3a,b | 2670 ± 68a | 1361 ± 24b | <3 |
| Non-Hispanic Asian | 601 | 1878 ± 39b | 3630 ± 94a | 2018 ± 33a | 92 ± 2a | 2666 ± 66a | 1480 ± 23a | <3 |
| Men | 2393 | 2367 ± 19 | 4209 ± 54 | 1753 ± 11 | >97 | 3203 ± 49 | 1335 ± 13 | 7 ± 1 |
| Age, y | ||||||||
| 20–39 | 882 | 2505 ± 46a | 4519 ± 82a | 1747 ± 24 | >97 | 3135 ± 79b | 1221 ± 17c | 6 ± 2 |
| 40–59 | 755 | 2405 ± 66b | 4293 ± 117b | 1768 ± 18 | >97 | 3322 ± 108a | 1360 ± 22b | 4 ± 2 |
| ≥60 | 756 | 2108 ± 37c | 3616 ± 69c | 1748 ± 38 | 93 ± 2 | 3131 ± 48a,b | 1472 ± 17a | 8 ± 2 |
| Race/ethnicity | ||||||||
| Non-Hispanic white | 929 | 2391 ± 31a | 4058 ± 60 | 1750 ± 16b | 97 ± 1 | 3125 ± 59a | 1369 ± 17a | 5 ± 1 |
| Non-Hispanic black | 603 | 2278 ± 56a,b | 3730 ± 70 | 1708 ± 22b | 93 ± 1 | 2619 ± 89b | 1197 ± 15c | <3 |
| Hispanic | 471 | 2378 ± 58a,b | 4060 ± 77 | 1743 ± 27b | 96 ± 3 | 2963 ± 89a | 1292 ± 29b | 3 ± 1 |
| Non-Hispanic Asian | 311 | 2164 ± 62b | 4015 ± 135 | 1915 ± 29a | >97 | 2895 ± 111a | 1391 ± 24a | <3 |
| Women | 2337 | 1734 ± 25 | 2979 ± 23 | 1728 ± 19 | 83 ± 1 | 2403 ± 33 | 1456 ± 18 | <3 |
| Age, y | ||||||||
| 20–39 | 765 | 1812 ± 27a | 3213 ± 58a | 1730 ± 31 | 95 ± 3a | 2350 ± 48 | 1319 ± 21c | <3 |
| 40–59 | 827 | 1772 ± 39a | 3019 ± 61b | 1723 ± 29 | 81 ± 3b | 2431 ± 44 | 1463 ± 27b | <3 |
| ≥60 | 745 | 1596 ± 27b | 2658 ± 54c | 1729 ± 21 | 72 ± 3b | 2422 ± 44 | 1597 ± 20a | <3 |
| Race/ethnicity | ||||||||
| Non-Hispanic white | 886 | 1738 ± 36a,b | 2860 ± 44b | 1705 ± 22b | 80 ± 2 | 2475 ± 51a | 1487 ± 27a | <3 |
| Non-Hispanic black | 650 | 1765 ± 35a | 2956 ± 70b | 1730 ± 23b | 78 ± 2 | 2143 ± 37b | 1280 ± 24b | <3 |
| Hispanic | 449 | 1730 ± 41a,b | 2868 ± 66b | 1707 ± 31b | 81 ± 4 | 2342 ± 58a | 1434 ± 28a | <3 |
| Non-Hispanic Asian | 290 | 1609 ± 44b | 3271 ± 120a | 2111 ± 55a | 87 ± 3 | 2455 ± 25a | 1558 ± 39a | <3 |
Values are means ± SEs unless indicated otherwise. Labeled means in a column within a group without a common superscript letter are significantly different, P ≤ 0.01. Multiple pairwise t tests were used for comparisons between population groups with df dictated by the NHANES sample design. Sex comparisons were not made because of statistically higher energy intakes among men compared with women. Sex differences in nutrient intake per 1000 kcal are presented within the text.
TABLE 2.
The Na:K and prevalence of Na:Ks < 1.0 in the diets of US adults (≥20 y) adjusted for day-to-day variability by sex, age, and race/ethnicity, NHANES 2011–20121
| n | Na:K | Na:K < 1.0, % | |
| All adults | 4730 | 1.38 ± 0.01 | 12 ± 2 |
| Age, y | |||
| 20–39 | 1647 | 1.51 ± 0.02a | 4 ± 1b |
| 40–59 | 1582 | 1.36 ± 0.03b | 13 ± 3a |
| ≥60 | 1501 | 1.23 ± 0.02c | 20 ± 3a |
| Race/ethnicity | |||
| Non-Hispanic white | 1815 | 1.34 ± 0.02c | 16 ± 2a |
| Non-Hispanic black | 1253 | 1.54 ± 0.03a | 2 ± 1b |
| Hispanic | 920 | 1.38 ± 0.03b,c | 6 ± 2b |
| Non-Hispanic Asian | 601 | 1.49 ± 0.04a,b | 8 ± 2b |
| Men | 2393 | 1.45 ± 0.02 | 7 ± 1 |
| Age, y | |||
| 20–39 | 882 | 1.57 ± 0.02a | 2 ± 1b |
| 40–59 | 755 | 1.42 ± 0.03b | 6 ± 2b |
| ≥60 | 756 | 1.30 ± 0.03c | 16 ± 3a |
| Race/ethnicity | |||
| Non-Hispanic white | 929 | 1.42 ± 0.02b | 10 ± 2a |
| Non-Hispanic black | 603 | 1.57 ± 0.03a | 1 ± 1a,b |
| Hispanic | 471 | 1.46 ± 0.04a,b | 3 ± 3a,b |
| Non-Hispanic Asian | 311 | 1.51 ± 0.03b | 7 ± 3b |
| Women | 2337 | 1.32 ± 0.02 | 18 ± 2 |
| Age, y | |||
| 20–39 | 765 | 1.44 ± 0.03a | 7 ± 3b |
| 40–59 | 827 | 1.31 ± 0.03b | 21 ± 4a |
| ≥60 | 745 | 1.17 ± 0.02c | 24 ± 5a |
| Race/ethnicity | |||
| Non-Hispanic white | 886 | 1.27 ± 0.03c | 23 ± 4a |
| Non-Hispanic black | 650 | 1.52 ± 0.03a | 2 ± 2b |
| Hispanic | 449 | 1.30 ± 0.03b,c | 11 ± 2b |
| Non-Hispanic Asian | 290 | 1.47 ± 0.07a,b | 10 ± 4a,b |
Values are means ± SEs unless indicated otherwise. Labeled means in a column within a group without a common superscript letter are significantly different, P ≤ 0.01. Multiple pairwise t tests were used for comparisons between population groups with df dictated by the NHANES sample design. Na:K, dietary sodium-to-potassium ratio.
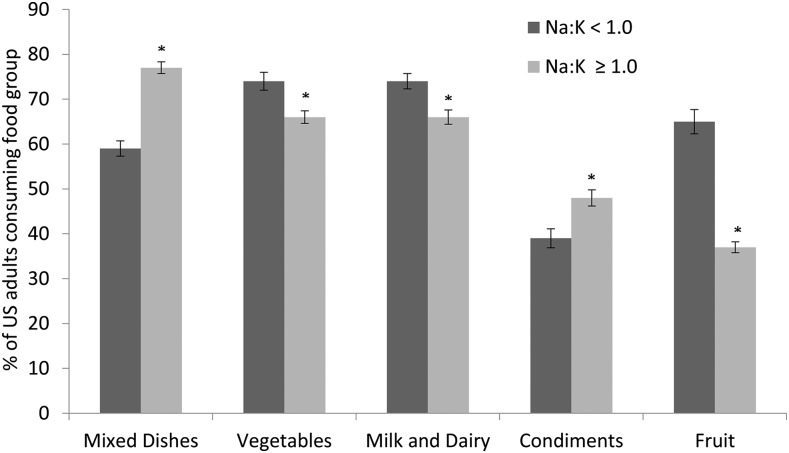
FIGURE 1.
Prevalence (%) of selected food groups in the diets of US adults (≥20 y; Na:K < 1.0: n = 1183; Na:K ≥ 1.0: n = 3547) NHANES by Na:Ks, NHANES 2011–2012. *Different from Na:K < 1.0, P ≤ 0.01. Na:K, dietary sodium-to-potassium ratio.
TABLE 3.
Reported food group contribution to sodium and potassium in the diets of US adults (≥20 y) by Na:K cutoffs, NHANES 2011–20121,2
| Contribution to sodium intakes, % |
Contribution to potassium intakes, % |
|||
| Na:K < 1.0 (n = 1183) | Na:K ≥ 1.0 (n = 3547) | Na:K < 1.0 (n = 1183) | Na:K ≥ 1.0 (n = 3547) | |
| Mixed dishes | 23.3 ± 1.0 | 36.6 ± 1.0* | 10.7 ± 0.7 | 23.4 ± 0.7* |
| Protein foods | 23.6 ± 0.9 | 21.6 ± 0.7 | 14.8 ± 0.7 | 17.8 ± 0.5* |
| Grains | 15.0 ± 0.7 | 12.2 ± 0.3* | 5.9 ± 0.3 | 6.3 ± 0.2 |
| Snacks and sweets | 8.9 ± 0.5 | 7.6 ± 0.3* | 7.4 ± 0.7 | 8.6 ± 0.4 |
| Vegetables | 9.1 ± 0.4 | 5.9 ± 0.3* | 15.5 ± 0.7 | 13.3 ± 0.4* |
| Milk and dairy | 7.8 ± 0.3 | 4.9 ± 0.4* | 11.5 ± 0.71 | 7.6 ± 0.3* |
| Condiments | 3.1 ± 0.3 | 4.8 ± 0.3* | 1.1 ± 0.2 | 2.2 ± 0.1* |
| Fats and oils | 3.4 ± 0.4 | 2.5 ± 0.1* | 0.8 ± 0.1 | 0.8 ± 0.1 |
| Non-alcohol beverages | 3.0 ± 0.4 | 2.2 ± 0.1 | 19.1 ± 1.0 | 12.8 ± 0.4* |
| Water | 1.6 ± 0.1 | 1.1 ± 0.04* | <0.1 | <0.1 |
| Alcohol beverages | <0.5 | <0.5 | 3.0 ± 0.3 | 2.3 ± 0.2* |
| Fruit | <0.1 | <0.1 | 9.3 ± 0.4 | 4.6 ± 0.2* |
Values are means ± SEs unless indicated otherwise. t tests were used to compare the Na:K groups with df dictated by the NHANES sample design. *Difference from Na:K < 1.0, P ≤ 0.01. Na:K, dietary sodium-to-potassium ratio.
Unlike the National Cancer Institute-adjusted statistics that represent long-term, usual dietary intake estimates presented in Tables 1 and 2, the food intake statistics here are estimates of intake on any given day. The above sample sizes reflect a categorization of the NHANES respondents on the basis of their daily Na:Ks and describe the sample, not the population.
Results
On the basis of 2011–2012 NHANES data, US adults consumed ∼2000 kcal/d, 3600 mg sodium/d, and 2800 mg potassium/d on average (Table 1). Among men and women, sodium and energy intakes decreased, and potassium intakes increased with advancing age, although no trends were observed for sodium or potassium intakes when expressed as a function of energy with age. However, the prevalence of intakes >2300 mg sodium/d decreased with age. Asians did not differ from whites or Hispanics for sodium intakes, but Asians had statistically higher intakes than blacks. Non-Hispanic Asian women had higher sodium intakes than all other racial/ethnic groups. No differences were observed for sodium intakes per 1000 kcal when age groups were examined or when men were compared with women for all age and racial/ethnic groups, with the exception of Asian women compared with men, who had values of 2111 mg sodium/(d · 1000 kcal) and 1915 mg sodium/(d · 1000 kcal), respectively (P = 0.0026). However, within both sexes and when both sexes were combined, Asians had the highest intakes compared with all other race/ethnic groups.
Among men, potassium intakes were higher in individuals aged 40–59 y than individuals aged 20–39 y but did not differ from adults aged ≥60 y. By contrast, no differences in mean potassium intakes were observed for women by age group. Overall and among women, potassium intake was significantly lower for blacks than for all other racial/ethnic groups. When potassium was expressed per 1000 kcal, women had higher intakes than men (comparisons not shown in data tables), and intakes increased with age.
The majority of American adults (90%) had sodium intakes >2300 mg/d, whereas a small percentage (<3%) had intakes aligned with the potassium recommendations of 4700 mg/d. Overall, the prevalence of sodium intakes >2300 mg/d decreased with age. Men had higher compliance with potassium recommendations, but the percentage who achieved recommended intakes remained <10% across all age groups.
Women had a significantly lower Na:K than men (1.32 compared with 1.45, respectively), which was consistent across all age groups and for whites and Hispanics but not blacks and Asians (Table 2; statistical comparison not shown). Non-Hispanic whites had significantly lower Na:Ks than did blacks and Asians, but their ratios did not differ from those of Hispanics. Only 12% of adults had a Na:K < 1.0. Among men and women, the Na:K decreased, and the prevalence of meeting the 1.0 cutoff increased linearly as age increased. A significantly higher proportion of women (18%) met the recommended Na:K < 1.0 than did men (7%) (data not shown). Across all categories, a significantly higher proportion of whites had a Na:K < 1.0 than did all other racial/ethnic groups (Table 2).
Mixed dishes (e.g., combinations of foods consumed together not categorized elsewhere, including sandwiches, soups, pizza, and Asian and Mexican dishes) provided the greatest contribution to sodium (34%) and potassium (19%) intakes in the American diet (Supplemental Table 1). When mixed dishes were consumed, pizza alone contributed to 40% of the daily sodium intakes (data not shown). As a group, individuals who had a Na:K < 1.0 were less likely to consume mixed dishes and condiments and were more likely to consume vegetables, milk and dairy, and fruit (Figure 1 and Supplemental Tables 1 and 2). No differences were noted in food group consumption for meeting or exceeding the Na:K for grains, beverages (i.e., alcohol, nonalcohol, water), protein foods, or fats and oils.
Mixed dishes were a large contributor to sodium intakes for both Na:K categories (i.e., <1.0 and ≥1.0); however, mixed dishes and condiments had a higher contribution to sodium intakes of individuals with a Na:K ≥ 1.0. By contrast, grains, snacks/sweets, vegetables, and dairy were among the food groups with higher contributions to sodium for individuals with a Na:K < 1.0 (Table 3). Milk and dairy, beverages, and fruit were more important sources of potassium in the diet for individuals with a Na:K < 1.0, whereas mixed dishes and protein foods contributed the most potassium for individuals with Na:Ks ≥ 1.0 (Table 3).
Discussion
This analysis reveals that 90% of US adults do not meet the recommendations for sodium intake and <3% meet recommendations for potassium intake. These themes were consistent across age and racial/ethnic groups. Asian adults had the highest consumption of both sodium and potassium, adjusted for energy intakes (i.e., per 1000 kcal) compared with all other race/ethnic groups. To our knowledge, this is the first report to characterize sodium, potassium, and the Na:K among Asian adults with the use of NHANES data. However, there is cause for public health concern across all age and racial/ethnic groups, given the literature that documents the role of sodium and potassium in hypertension (8, 29–31). Hypertension is an important contributor to CVD death in the United States (31).
A recent NHANES report documents that individuals with hypertension have higher usual sodium intakes and lower usual intakes of potassium (6). Despite our lack of understanding of the exact mechanisms, both sodium and potassium were shown to have direct roles in blood pressure; therefore, studying the ratio of intakes has been a method to examine dietary intakes relative to hypertension and cardiovascular health. In the 2005–2010 NHANES, adults with hypertension had a significantly higher Na:K than nonhypertensive individuals; however, this NHANES report did not provide overall estimates for all American adults or for Asians. Our analysis extends this previous research and indicates that only about 1 in 4 American adults has a Na:K < 1.0.
Usual Na:Ks < 1.0 reported in NHANES III (1988–1994) were previously associated with a lower risk of increased risk of death from all causes, CVD, and ischemic heart disease. The above-described analysis by Yang et al. (5) dichotomized adults into 2 age groups: <60 y or ≥60 y. Thus, we can make comparisons between the 2 NHANES survey periods from 1988–1994 to 2011–2012 only for older adults (i.e., ≥60 y). Among older adults, the Na:K shifted from 1.16 to 1.30 for men and from 1.03 to 1.32 for women. Both the 1988–1994 NHANES and the 2011–2012 NHANES document the highest Na:K for black adults than for all other race/ethnic groups. Previous NHANES reports have also suggested that blacks had the highest Na:K when stratified by sex (5) and by hypertension status (6) than all other race/ethnic groups; however, neither of these reports assessed the prevalence of Na:Ks < 1.0 or included Asians. Our analysis suggests that Asians have Na:Ks similar to black adults; however, compared with black Americans, Asian adults do not have the high prevalence of hypertension and other cardiovascular disorders. These findings may be explained in part by differences in body weight, genetics, and lifestyle factors, which are beyond the scope of this analysis.
Our examination of US dietary patterns associated with meeting the recommended dietary intake Na:K provides a starting point to evoke dietary changes. The largest contributor to sodium intakes for those with a Na:K ≥ 1.0 were mixed dishes (including chili, stews, pasta dishes, burritos/tacos, pizza, and soups). These same foods are the top contributors to potassium, not because they are a good source of the nutrient but because of their ubiquitous consumption by the American population. Fruits, vegetables, and dairy products are rich sources of potassium but tend to be consumed less frequently by US adults (32). Increasing potassium-rich food intakes while reducing intake of foods high in sodium would improve the Na:K. Overall, our data support previous reports both on sodium and potassium intakes but also on overall dietary patterns consistent with heart health. The Dietary Approaches to Stop Hypertension (DASH) trial and subsequent similar investigations have displayed the importance of the healthy overall combinations and patterns of foods and nutrients for health, rather than simply focusing on sodium reduction in isolation (33).
The strengths of this investigation include the use of a large, nationally representative cohort of adults, inclusion of data from Asians, and examination of both nutrient- and food-level contributions to the diet. Moreover, we estimated usual intakes that account for measurement error and day-to-day variability in dietary assessment. This study has some limitations. Currently, the only available data on Asians are from the 2011–2012 NHANES, and this report does not include sodium and potassium from dietary supplements, although this tends to be low. The analysis did not include discretionary salt added at the table, which accounts for a small amount of daily sodium intake. Mattes and Donnelly (34) previously estimated that 5% of average daily sodium intake came from salt added at the table.
All dietary data are limited by the accuracy and currency of the databases used to estimate nutrient intakes from foods and beverages reported. Sodium validation of the 24-h dietary recall indicates that differential reporting exists by sex: the mean reporting accuracy was 0.93 (95% CI: 0.89, 0.97) for men and 0.90 (95% CI: 0.87, 0.94) for women (26). A pooled analysis of 5 large validation studies of self-reported sodium and potassium intakes from 24-h dietary recall compared with recovery biomarkers indicates under-reporting in the range of 0–4% for potassium and 4–13% for sodium; however, the Na:K was much better assessed than sodium intakes alone (i.e., 5–9%) (35). Furthermore, energy under-reporting is a known limitation with self-reported dietary data (36); however, the AMPM dietary instrument has been validated for energy and sodium. Energy under-reporting by ∼3% in normal adults and 11% in overweight adults was previously documented with the use of the AMPM method (24).
In summary, this report illustrates that about one-tenth of US adults have a Na:K consistent with the WHO guidelines, and these individuals may have a reduced risk of CVD-related mortality. Continued efforts to reduce sodium in tandem with novel strategies to increase potassium intakes are warranted. Dietary modification is a cost-effective public health intervention strategy. Our data suggest that blacks and Asians have the most unfavorable Na:K in the United States
Acknowledgments
RLB and CMW contributed to the concept development and manuscript preparation; EAP, DGR, JDG, JCC, AJM, and SVT contributed to the methodologic and statistical aspects of the work. All authors contributed to manuscript review. All authors read and approved the final manuscript.
Footnotes
Abbreviations used: AMPM, Automated Multiple-Pass Method; CVD, cardiovascular disease; Na:K, dietary sodium-to-potassium ratio.
References
- 1.US Department of Agriculture, US Department of Health and Human Services. Dietary Guidelines for Americans, 2010. 7th ed. Washington (DC): US Government Printing Office, 2010. [Google Scholar]
- 2.Gunn JP, Barron JL, Bowman BA, Merritt RK, Cogswell ME, Angell SY, Bauer UE, Frieden TR. Sodium reduction is a public health priority: reflections on the Institute of Medicine’s report, sodium intake in populations: assessment of evidence. Am J Hypertens 2013;26:1178–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cogswell ME, Zhang Z, Carriquiry AL, Gunn JP, Kuklina EV, Saydah SH, Yang Q, Moshfegh AJ. Sodium and potassium intakes among US adults: NHANES 2003–2008. Am J Clin Nutr 2012;96:647–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Perez V, Chang ET. Sodium-to-potassium ratio and blood pressure, hypertension, and related factors. Adv Nutr 2014;5:712–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yang Q, Liu T, Kuklina EV, Flanders WD, Hong Y, Gillespie C, Chang MH, Gwinn M, Dowling N, Khoury MJ, et al. Sodium and potassium intake and mortality among US adults: prospective data from the Third National Health and Nutrition Examination Survey. Arch Intern Med 2011;171:1183–91. [DOI] [PubMed] [Google Scholar]
- 6.Zhang Z, Cogswell ME, Gillespie C, Fang J, Loustalot F, Dai S, Carriquiry AL, Kuklina EV, Hong Y, Merritt R, et al. Association between usual sodium and potassium intake and blood pressure and hypertension among U.S. adults: NHANES 2005–2010. PLoS One 2013;8:e75289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.World Health Organization. Guideline: sodium intake for adults and children. Geneva: World Heath Organization; 2012. [PubMed] [Google Scholar]
- 8.Food and Nutrition Board. Dietary reference intakes for water, potassium, sodium, chloride, and sulfate. Washington (DC): National Academy Press; 2005. [Google Scholar]
- 9.World Health Organization [Internet]. Geneva: Guideline: potassium intake for adults and children. 2012 [cited 2015 Feb 18]. Available from: http://apps.who.int/iris/bitstream/10665/77986/1/9789241504829_eng.pdf?ua=1&ua=1. [PubMed]
- 10.Drewnowski A, Maillot M, Rehm C. Reducing the sodium-potassium ratio in the US diet: a challenge for public health. Am J Clin Nutr 2012;96:439–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dodd KW, Guenther PM, Freedman LS, Subar AF, Kipnis V, Midthune D, Tooze JA, Krebs-Smith SM. Statistical methods for estimating usual intake of nutrients and foods: a review of the theory. J Am Diet Assoc 2006;106:1640–50. [DOI] [PubMed] [Google Scholar]
- 12.Guenther PM, Kott PS, Carriquiry AL. Development of an approach for estimating usual nutrient intake distributions at the population level. J Nutr 1997;127:1106–12. [DOI] [PubMed] [Google Scholar]
- 13.Kipnis V, Midthune D, Freedman L, Bingham S, Day NE, Riboli E, Ferrari P, Carroll RJ. Bias in dietary-report instruments and its implications for nutritional epidemiology. Public Health Nutr 2002;5:915–23. [DOI] [PubMed] [Google Scholar]
- 14.Carriquiry AL. Estimation of usual intake distributions of nutrients and foods. J Nutr 2003;133:601S–8S. [DOI] [PubMed] [Google Scholar]
- 15.Tooze JA, Midthune D, Dodd KW, Freedman LS, Krebs-Smith SM, Subar AF, Guenther PM, Carroll RJ, Kipnis V. A new statistical method for estimating the usual intake of episodically consumed foods with application to their distribution. J Am Diet Assoc 2006;106:1575–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Beaton GH, Milner J, Corey P, McGuire V, Cousins M, Stewart E, de Ramos M, Hewitt D, Grambsch PV, Kassim N, et al. Sources of variance in 24-hour dietary recall data: implications for nutrition study design and interpretation. Am J Clin Nutr 1979;32:2546–59. [DOI] [PubMed] [Google Scholar]
- 17.Beaton GH, Milner J, McGuire V, Feather TE, Little JA. Source of variance in 24-hour dietary recall data: implications for nutrition study design and interpretation. Carbohydrate sources, vitamins, and minerals. Am J Clin Nutr 1983;37:986–95. [DOI] [PubMed] [Google Scholar]
- 18.National Research Council. Nutrient Adequacy. Washington (DC): National Academy Press; 1986. [Google Scholar]
- 19.Nusser S, Carriquiry AL, Dodd KW, Fuller WA. A semiparametric transformation approach to estimating usual daily intake distributions. J Am Stat Assoc 1996;91:1440–9. [Google Scholar]
- 20.Subar AF, Dodd KW, Guenther PM, Kipnis V, Midthune D, McDowell M, Tooze JA, Freedman LS, Krebs-Smith SM. The food propensity questionnaire: concept, development, and validation for use as a covariate in a model to estimate usual food intake. J Am Diet Assoc 2006;106:1556–63. [DOI] [PubMed] [Google Scholar]
- 21.National Center for Health Statistics [Internet]. Hyattsville (MD): Centers for Disease Control and Prevention; 2009 [cited 2008 Aug 17]. About the National Health and Nutrition Examination Survey. Available from: http://www.cdc.gov/nchs/nhanes/about_nhanes.htm.
- 22.US Department of Agriculture [Internet]. Beltsville (MD): Agricultural Research Service; 2014 [cited 2014 Jul 1]. WWEIA Documentation and Data Sets. Available from: http://www.ars.usda.gov/Services/docs.htm?docid=18354.
- 23.Blanton CA, Moshfegh AJ, Baer DJ, Kretsch MJ. The USDA Automated Multiple-Pass Method accurately estimates group total energy and nutrient intake. J Nutr 2006;136:2594–9. [DOI] [PubMed] [Google Scholar]
- 24.Moshfegh AJ, Rhodes DG, Baer DJ, Murayi T, Clemens JC, Rumpler WV, Paul DR, Sebastian RS, Kuczynski KJ, Ingwersen LA, et al. The US Department of Agriculture Automated Multiple-Pass Method reduces bias in the collection of energy intakes. Am J Clin Nutr 2008;88:324–32. [DOI] [PubMed] [Google Scholar]
- 25.US Department of Agriculture [Internet].Beltsville (MD): Agricultural Research Service. USDA Food and Nutrient Database for Dietary Studies 2011–2012. Food Surveys Research Group Home Page; 2014 [cited 2015 Jun 1]. Available from: http://www.ars.usda.gov/nea/bhnrc/fsrg.
- 26.Rhodes DG, Murayi T, Clemens JC, Baer DJ, Sebastian RS, Moshfegh AJ. The USDA Automated Multiple-Pass Method accurately assesses population sodium intakes. Am J Clin Nutr 2013;97:958–64. [DOI] [PubMed] [Google Scholar]
- 27.Burt VL, Cohen SB. A comparison of methods to approximate standard errors for complex survey data. Rev Public Data Use 1984;12:159–68. [PubMed] [Google Scholar]
- 28.Rao JNK, Shao J. Modified balanced repeated replication for complex survey data. Biometrika 1999;13:403–15. [Google Scholar]
- 29.Intersalt: an international study of electrolyte excretion and blood pressure. Results for 24 hour urinary sodium and potassium excretion. Intersalt Cooperative Research Group. BMJ 1988;297:319–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sica DA, Struthers AD, Cushman WC, Wood M, Banas JS Jr, Epstein M. Importance of potassium in cardiovascular disease. J Clin Hypertens (Greenwich) 2002;4:198–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Blaha MJ, Dai S, Ford ES, Fox CS, Franco S, et al. Heart disease and stroke statistics–2014 update: a report from the American Heart Association. Circulation 2014;129:e28–292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Krebs-Smith SM, Guenther PM, Subar AF, Kirkpatrick SI, Dodd KW. Americans do not meet federal dietary recommendations. J Nutr 2010;140:1832–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Appel LJ, Moore TJ, Obarzanek E, Vollmer WM, Svetkey LP, Sacks FM, Bray GA, Vogt TM, Cutler JA, Windhauser MM, et al. A clinical trial of the effects of dietary patterns on blood pressure. DASH Collaborative Research Group. N Engl J Med 1997;336:1117–24. [DOI] [PubMed] [Google Scholar]
- 34.Mattes RD, Donnelly D. Relative contributions of dietary sodium sources. J Am Coll Nutr 1991;10:383–93. [DOI] [PubMed] [Google Scholar]
- 35.Freedman LS, Commins JM, Moler JE, Willett W, Tinker LF, Subar AF, Spiegelman D, Rhodes D, Potischman N, Neuhouser ML, et al. Pooled results from 5 validation studies of dietary self-report instruments using recovery biomarkers for potassium and sodium intake. Am J Epidemiol 2015;181:473–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Schoeller DA, Bandini LG, Dietz WH. Inaccuracies in self-reported intake identified by comparison with the doubly labelled water method. Can J Physiol Pharmacol 1990;68:941–9. [DOI] [PubMed] [Google Scholar]