Abstract
Introduction:
Among pelvic landmarks routinely palpated by manual therapists, the posterior superior iliac spines (PSISs) are particularly important. In addition to serving as landmarks for identifying possible pelvic torsion, contacting the PSISs is integral to many other static and dynamic pelvic palpatory procedures. The primary study goal was to systematically review the literature on the intra- and interexaminer reliability of PSIS palpation.
Methods:
Electronic databases and secondary searches led to the retrieval of articles that satisfied inclusion criteria. Two investigators rated the quality of included articles using the QAREL instrument.
Results:
The search identified 13 articles, one judged high quality, satisfying the inclusion criteria. Intraexaminer exceeded interexaminer reliability. Among 8 studies that reported interexaminer agreement using kappa, mean ϰ=0.27 (adjusted for sample size).
Discussion and Conclusion:
Current methods of palpating for PSIS asymmetry do not result in levels of interexaminer reliability supporting clinical utility. Improved methods should be sought.
Keywords: chiropractic, palpation, posterior superior iliac spine, systematic review
Abstract
Introduction :
En ce qui concerne la région pelvienne régulièrement palpée par des thérapeutes manuels, les épines iliaques postéro-supérieures (EIPS) sont particulièrement importantes. En plus de servir de points de repère pour l’identification d’une possible torsion pelvienne, la palpation de l’EIPS fait partie intégrante de nombreuses autres procédures palpatoires pelviennes statiques et dynamiques. L’objectif principal de l’étude était d’examiner systématiquement les documents scientifiques concernant la fiabilité intra- et inter-examinateurs de la palpation de l’EIPS.
Méthodologie :
Les bases de données électroniques et les recherches secondaires ont abouti à la découverte d’articles qui répondaient aux critères d’inclusion. À l’aide de l’instrument QAREL, deux enquêteurs ont évalué la qualité des articles inclus.
Résultats :
La recherche a révélé 13 articles, dont un de haute qualité, répondant aux critères d’inclusion. Le nombre d’articles traitant de la fiabilité intraexaminateurs était supérieur à ceux traitant de la fiabilité interexaminateurs. Pour les 8 études qui ont mentionné un accord d’interexaminateurs utilisant l’indice kappa, la moyenne ϰ = 0,27 (ajusté à la taille de l’échantillon).
Discussion et conclusion :
Les méthodes actuelles de palpation pour l’asymétrie de l’EIPS ne mènent pas à des niveaux de fiabilité interexaminateurs pour soutenir l’utilité clinique. Il faut rechercher des méthodes améliorées.
Keywords: chiropratique, palpation, épine iliaque postéro-supérieure, examen systématique
Introduction
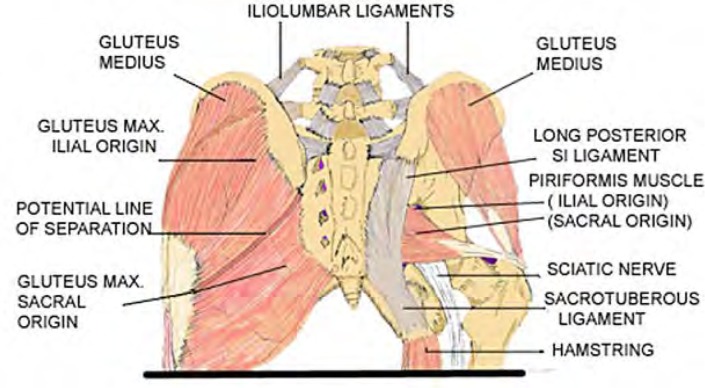
Manual therapists draw upon a number of physical examination procedures to establish indications for sacroiliac interventions.1 Broadly speaking these procedures fall into four categories: palpation for positional asymmetry of bony landmarks, tests for joint hypomobility or hypermobility, assessment of changes in tissue texture, and tests for pain provocation and/or amelioration. The anatomical landmarks that are commonly located and contacted to perform these tests include the anterior superior iliac spine (ASIS), the posterior superior iliac spine (PSIS), the iliac crest, the sacral sulcus, the sacral apex, and the inferior lateral angle of the sacrum (SILA). Among the pelvic landmarks routinely palpated, the posterior superior iliac spines (PSISs) may be singled out as particularly important, in that identifying them is the starting point for a variety of patient assessment procedures (see Table 1). As the most posterior projection of the iliac crest, it serves for the attachment of the long posterior sacroiliac ligament, which blends with the sacrotuberous ligament, as well as the multifidus and gluteus maximus muscles. Figure 1 depicts the muscular and ligamentous attachments to the PSIS.
Table 1.
Some orthopedic tests requiring PSIS identification
| Procedure | How performed | Interpretation |
|---|---|---|
| Seated bilateral PSIS palpation | Examiner places thumbs on PSISs, assessing for vertical displacement. | Inferior PSIS –> posterior innominate rotation; Superior PSIS–>anterior rotation2,3 |
| Prone PSIS identification as anatomical landmark | Examiner identifies PSIS in relation to sacrum. | Using a PSIS landmark may increase accuracy of numerating lumbar segments4,5 |
| Palpation of PSIS Y-axis unleveling, seated vs. standing, as indicator of anatomic LLI | Vertical PSIS displacement seated compared with standing displacement. | Any difference in vertical PSIS displacement seated compared with standing displacement suggests anatomical LLI6,7 |
| Sacroiliac motion palpation | Seated or standing, examiner observes or palpates for sacroiliac excursion during movement (sitting flexion test8, step test9, etc.) or endfeel with digital pressure. | Lack of excursion during active or passive sacroiliac movement indicates restriction; hard end-feel with digital pressure indicates fixation10,11 |
| Pain provocation | Digital pressure applied to PSISs. | Tenderness of PSIS on palpation indicates sacroiliac dysfunction12 |
| PSIS identification to allow sulcus depth determination | Thumbs probe relative depth of the sacroiliac joints. | Asymmetry indicates inter-innominate sacral base rotation13 |
Figure 1.
Muscular and ligamentous attachments to the PSIS (Permission to reprint from http://www.thelowback.com/granted by Richard DonTigny)
Given the importance of PSIS palpation, the authors elected to conduct a systematic review of the literature pertaining to the intra and interexaminer reliability of identifying the location of a single PSIS, or the bilateral positional asymmetry of the left and right PSISs. The primary goals of this study were to both identify such articles and summarize their data; and to assess their methodological quality.
Methods
Inclusion criterion for an article to be included in this review was that it concerned the intraexaminer or interexaminer reliability of static palpation of the PSIS(s) and was published in an English language peer reviewed journal. Reliability could pertain to assessing the location of a single PSIS, or to assessing the bilateral symmetry of the PSISs on the superior-inferior axis (i.e., assessing whether one PSIS was caudal to the other). Review articles and validity studies related to PSIS palpation were excluded, as were articles concerned with pelvic landmarks other than the PSIS. Theses written in connection with obtaining a degree in an academic program were also excluded. Databases consulted included PubMed, ICL, CINAHL, AMED, Osteopathic Research Web, OstMed, and MANTIS. After searching these biomedical databases, we supplemented our search using the global Google search engine. Searches were conducted using the following terms and combinations of them: reliability, agreement, PSIS, palpation, physical examination, posterior superior iliac spine, pelvis, pelvic, sacroiliac, and landmark. It was not necessary to construct complicated Boolean phrases to limit the number of returned citations, because even very inclusive search terms returned relatively few citations; e.g., “posterior superior iliac spine + reliability” returned only 11 citations in the PubMed database, and sacroiliac + palpation only 70 citations. The “related citations” function was deployed when articles were retrieved which fit the inclusion criteria. In one case, an email was sent to an author to clarify the methodology used. The bibliographies for included articles were also inspected for additional candidates for inclusion. Each of the included articles was rated for quality using the The Quality Appraisal of Reliability Studies (QAREL) instrument.14 These articles were rated for quality by two reviewers using the QAREL instrument14; disagreements between reviewers were resolved by coming to consensus following discussion. QAREL index quality scores ranged from 2 to 10, average 5.1. Table 2 summarizes the search strategy used in this study.
Table 2.
STARLITE Mnemonic summarizing search strategy
| Sampling Strategy | Electronic databases searched for articles satisfying inclusion criteria. Google searching supplemented database searching. |
| Type of Studies | Studies investigating intra or interexaminer reliability of PSIS palpation. |
| Approaches | “Related articles” function used following successful retrieval. Secondary search used to reach a point of data saturation (i.e., no new references could be identified). |
| Range of Years | No restrictions. |
| Limits: | Only English-language articles were included. |
| Inclusions/Exclusions | Included only English language primary reliability studies. Excluded theses, validity studies, and review articles. |
| Terms Used | PSIS reliability, posterior superior iliac spine reliability, PSIS agreement, posterior superior iliac spine agreement; PSIS palpation; posterior superior iliac spine palpation. This strategy was repeated substituting the words “sacroiliac” and “pelvic” and “landmark” for the acronym PSIS. |
| Electronic Sources | PubMed, ICL, CINAHL, AMED, Osteopathic Research Web, OstMed, MANTIS |
Results
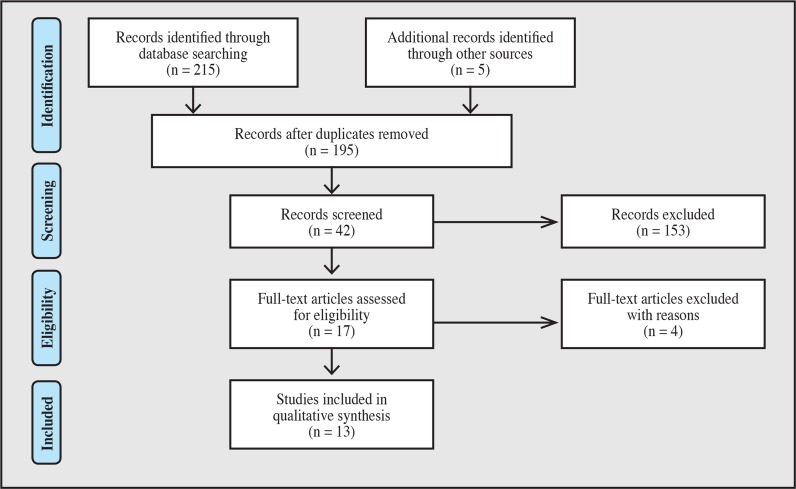
The original search retrieved 215 citations. Another 5 articles were included based on a secondary search of the included articles, or because the first author was personally familiar with them. After removing duplicates, there were 195 citations remaining. After inspecting their titles, 153 were excluded from further consideration, leaving 42 abstracts to be read for consideration of possible inclusion. This resulted in the retrieval of 17 full text articles. Three of the retrieved full text articles were excluded because they did not involve PSIS palpation13,15,16 and one because it involved radiological rather than manual assessment17. This resulted in a total of 13 articles published between 1985 and 2008 that met the inclusion/exclusion criteria. The literature retrieval flow process is depicted in Figure 2.
Figure 2.
Literature retrieval flow diagram
Three studies utilized seated PSIS palpation only10,18,19; 6 utilized prone palpation only4,20–24; 3 used standing palpation only25–27; and one include seated and standing palpation8. Ten of the included studies8,10,18,19,21–25,27 asked assessors to examine the PSISs bilaterally to determine if they were symmetric or displaced on the superior-inferior axis; 2 studies20,28 asked examiners to locate one of the PSISs, reporting their agreement in terms of the distance between the sites identified by the assessors, making no attempt to analyze their continuous data by calculating their Intraclass Correlation Coefficient (ICC); and 1 study4 assessed agreement as the midline distance between lines examiners drew between the bilateral PSISs. Of the 10 studies that involved bilateral palpation, all but one used inferential statistics to report their data, the exception being Potter et al.8 who reported percent agreement only. Only 1 study reported data using an inferential statistic other than kappa: Kim4 used the Wilcoxon signed rank test statistic as a surrogate measure of reliability4, basing calculations on the distance between lines that 2 examiners drew between the PSISs, as measured where these lines intersected a midline ruler. (The Wilcoxon test may be used to assess reliability when paired data are not normally distributed, in order to test the hypothesis that the median difference between the pairs is significantly different from zero.) None of the studies included in this review attained kappa levels for interexaminer reliability that would be considered to reflect “substantial” agreement according to the widely accepted Landis and Koch scale.29 The 5 studies10,20,22–24 that included intraexaminer reliability modules found intraexaminer reliability to exceed interexaminer reliability. In the 8 studies that reported interexaminer agreement using the kappa statistic, the mean value, weighted by sample size, was ϰ=0.27. One study25 did not provide exact kappa results, reporting only that ϰ<0.40, and thus could not be included in this mean calculation. The data are abstracted in Table 3, and the QAREL ratings in Table 4. There was a non-significant trend for moderate correlation between the reported kappa values and study quality (Pearson’s product moment correlation r = 0.43, p = 0.28), suggesting that the higher quality studies demonstrated higher interexaminer reliability.
Table 3.
Reliability studies, PSIS palpation
| Author, date | Palpatory method (bilateral unless unilateral noted) | Examiners/participants (E/P) | Reliability (ϰ, % agreement, or other statistic) | Quality. score (n/11) | Study conclusions |
|---|---|---|---|---|---|
| Potter, 19858 | Seated and standing, cadual aspect | E: 8 PTs P: 17 buttock pain |
%=35.29 seated %=35.29 standing (interexaminer only) |
4 | Need for improved methods for SI palpation; PSIS palpation under the conditions of this study was unreliable. |
| Byfield, 199228 | Standing position, aspect of PSIS not specified | E: 10 DCs & 10 students P: 2 patients, clinical status unspecified |
“Horizontal spread” for DCs 1.1 (0.7) cm, for students 2.0 (0.1) cm “Vertical spread” for DCs 1.4 (0.7) cm, for students 4.5 (2.2) cm students |
4 | The DC’s skin marks for PSIS location were more “concentrated” than students’ marks; DCs were “reasonably” reliable. |
| Simmonds, 199220 | Prone, not further specified | E: 20 PTs P: 20 asymp. |
Intraexaminer: mean distance between UV skin marks= 8 ±5 mm Interexaminer: mean distance between UV skin marks= 20 ±13 mm |
5 | PSIS palpation was associated with a statistically significant low within-rater but high between-rater error. |
| Paydar, 199410 | Seated, caudal aspect | E: 2 DC students P: 32 asymp. |
ϰ=.25 (intraexaminer) %=51.6 ϰ=.15 (interexaminer) %=46.8 |
2 | The clinical decision on which sacroiliac joint to treat should not be based on palpatory findings alone. |
| Lindsay, 199521 | Prone, not further specified | E: 2 experienced manual therapists P: 8 skiers (unknown symptom status) Apparently dichotomous protocol |
ϰ= −.10 %=50 (interexaminer only) |
3 | PSIS palpation failed to meet a predetermined agreement criterion of 70%; sacroiliac very unreliable. |
| O’Haire, 200023 | Prone, caudal aspect | E: 10 DO students P: 10 asymp. |
ϰ=.07 to .58, mean .33 %=43–94 (intraexaminer) ϰ=.04, %=51 (interexaminer only) |
6 | Only slight inter-examiner reliability; efforts should be made to improve levels of agreement. |
| Riddle, 200218 | Seated | E: 34, pairwise P: 65 pain |
ϰ:=.37 %=55.6 (interexaminer only) |
5 | Pain provocation tests appear to have more support for identifying sacroiliac problems than sacroiliac alignment or movement tests. |
| Fryer, 200522 | Prone, caudal aspect | E: 10 final year osteopathic students (5 trained) P: 10 asymp. female volunteers |
ϰ=0.49 untrained, .54 trained (intraexaminer) ϰ=0.15 untrained; .08 trained %=53 trained, %=34 untrained (interexaminer) |
7 | Training did not improve reliability |
| Kim, 20074 | Prone, caudal aspect | E: 4, experienced P: 60 patients |
Wilcoxon statistic: mean PSIS delta = .60(.60) mm (interexaminer only) | 6 | Palpating the PSIS with accuracy might be difficult. |
| Kimita, 200824 | Prone, caudal aspect | E: 2 students, 2 experienced DOs P: 5 symptomatic, 4 asymp. |
ϰ= −.29 to 0.39 (intraexaminer) %=11–67 ϰ= .38 to 0.35 (interexaminer) %=11–56 |
10 | Inter-examiner reliability was low, irrespective of examiners’ years of experience. |
| van Kessel-Cobelens, 200819 | Seated, caudal aspect | E: 2 PTs P: Total 60 20 Control 22 w/pelvic pain, 20 wks pregnant 20 no pelvic pain, 20 weeks pregnant (interexaminer only) |
Total group: ϰ=0.26, %=63 Control: ϰ=0.47, %=75 Pain: ϰ=.20, %=60 Non-pain: ϰ=0.10, %=55 |
7 | Poor interexaminer reliability for palpation, should not be used for diagnostic purposes. |
| Sutton, 201227 | Standing, caudal aspect, unilateral | E: 15 final year osteopathy students, 15 3rd year, 10 exp. osteopaths P: 1 asymp. model; 5mm wedge inserted 2/3 trials (interexaminer only) |
3rd year students ϰ=.025; 4th year ϰ=.065; DOs ϰ=.058; all combined ϰ=.063 | 6 | Inter-reliability of palpation to locate PSISs and assess levels is poor in both students and experienced osteopaths. |
| Suwanasri, 201425 | Standing, aspect unspecified | E: PTs, number unclear P: 10 PT students |
ϰ<.40 | 2 | Inter-reliability of palpation to locate PSISs is poor. |
Abbreviations: DO=Osteopath, DC=Chiropractor, PT=Physiotherapist, E=Examiner, P=Patient, ϰ=Kappa, mm=millimeter, asymp.= asymptomatic patient
Table 4.
QAREL ratings14
| Item # | Criterion |
|---|---|
| 1 | Was the test evaluated in a sample of subjects who were representative of those to whom the authors intended the results to be applied? |
| 2 | Was the test performed by raters who were representative of those to whom the authors intended the results to be applied? |
| 3 | Were raters blinded to the findings of other raters during the study? |
| 4 | Were raters blinded to their own prior findings of the test under evaluation? |
| 5 | Were raters blinded to the subjects’ disease status or the results of the accepted reference standard for the target disorder (or variable) being evaluated? |
| 6 | Were raters blinded to clinical information that was not intended to form part of the study design or testing procedure? |
| 7 | Were raters blinded to additional cues that were not part of the test? |
| 8 | Was the order of examination varied? |
| 9 | Was the stability (or theoretical stability) of the variable being measured taken into account when determining the suitability of the time interval between repeated measures? |
| 10 | Was the test applied correctly and interpreted appropriately? |
| 11 | Were appropriate statistical measures of agreement used? |
| QAREL assessments for articles in review | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Item # | Byfield | Fryer | Kim | Kmita | Lindsay | O’Haire | Paydar | Potter | Riddle | Simmonds | Sutton | Van Kessel | Suwanasri |
| 1 | Y | Y | Y | Y | Y | Y | Y | ||||||
| 2 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | |||
| 3 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | |||
| 4 | Y | Y | |||||||||||
| 5 | Y | Y | Y | ||||||||||
| 6 | Y | Y | Y | Y | |||||||||
| 7 | Y | Y | Y | ||||||||||
| 8 | Y | Y | Y | Y | Y | ||||||||
| 9 | |||||||||||||
| 10 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | |
| 11 | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | ||
| Total Y | 4 | 7 | 6 | 10 | 3 | 6 | 2 | 4 | 5 | 5 | 6 | 7 | 2 |
An established categorical hierarchy of scores has not been established for the QAREL instrument. That stated, the authors established the following arbitrary categorical hierarchy of scores to interpret the QAREL quality assessments (1–4: low; 5–8: moderate; 9–11: high) also supports this trend. The results were: ϰ=0.03 for the 2 low quality studies, ϰ=0.33 for the 5 moderate quality studies, and ϰ=0.37 for the 1 high quality study.
An intra-examiner reliability study was conducted in which 3 final year osteopathic students served as examiners attempting to reliably identify the location of a single PSIS on repeated examinations.30 Although the full text of the thesis was not available to us, precluding including it in our review, we may point out that the investigators reported “low to moderate intra-rater reliability” and recommended “cautious presentation of palpation in osteopathic curricula.”
Discussion
Most manual therapists perform tests for both joint fixation and misalignment. The term “joint fixation” may refer either to an examiner’s sense of a hard endfeel on palpatory digital pressure, or restriction in or a specific direction during palpation for joint excursion.31 The authors are not aware of evidence supporting the view that either type of finding is more important than the other, nor definitive evidence that the information supplied by either test has an important impact upon the outcome of care. Beyond the interexaminer reliability being demonstrably wanting, the validity has hardly been studied. Kmita24 calls attention to the fact that “the field of diagnostic accuracy has been labelled in the British Medical Journal as the ‘new frontier’”32. Despite the lack of evidentiary support, a typical manual therapy examination involves finding asymmetry (e.g., pelvic torsion), then determining the clinically relevant side through motion palpation and other examination procedures.33 The sequence could be reversed, so the clinician would identify a fixated or restricted joint, then determine via static palpation if there is positional asymmetry that might inform the vector of correction. Asymmetric PSIS locations may imply opposed rotations of the innominate bones, wherein the bone on the side of the inferior PSIS has rotated posteriorly in relation to the other side, which in turn is judged to have rotated anteriorly.34
There are basic science threats to the feasibility of using PSIS palpation to derive clinically useful information, beyond the demonstrable low reliability of the procedure. Congenital and/or acquired asymmetry of the pelvis may confound the interpretation of palpable or visible misalignment. That stated, there is evidence that although there may be substantial left-right asymmetry of the innominate bones in any one individual, on average such differences are usually small and average only 2mm.35–37 Roentgen Stereophotogrammetric Analysis (RSA) poses another challenge to the clinical utility of PSIS palpation. RSA technology, which involves 3-D digitizing of metallic markers implanted in the skeleton, is generally considered the most accurate method for measuring 3-D motions of the sacroiliac joints.38 Motions of the sacroiliac joint in stressed positions, such as one-legged stance and straddle position, have been found to be much smaller than those reported by most other measuring technologies; Goode38 concludes that “the limited movements may not support a clinician’s ability to palpate selected movements.” Small sacroiliac movements notwithstanding, it must be emphasized that RSA measures movement, not position. Therefore this technology does not refute the possibility of asymmetric positions, if not movements, of the innominate bones, in principle detectable by means of manual palpation. Likewise, RSA technology does not rule out that findings of asymmetry could suggest vectors for manual therapy that are more optimal than contrary vectors, even were it found that such vectors had not resulted in measurable repositioning of the innominate bones.
Although the interexaminer reliability of most palpatory pelvic positional tests (PSIS levels, ASIS levels, sacral sulcus depth) has been poor39, instrumented measurements of innominate positions suggest these do in fact occur2. Since many studies of clinical interventions that attempt to improve symmetry confirm clinical improvement in both pain reduction and functional measures, it may be hypothesized that these interventions normalize neuromusculoskeletal function, if not bone positions. It remains to be seen whether interventions using vectors contrary to those intended to improve symmetry would get equivalent results, but there is some evidence that they may not. Long et al.40 showed that the direction of prescribed McKenzie exercises did make a clinical difference, while another author showed that patients preferred being blocked in positions that reversed their palpable pelvic torsion pattern41.
Manipulative strategies for pelvic structures should involve reliable and valid assessment procedures. However, none of the studies included in this review that reported their data using kappa calculations obtained the ϰ ≥. 60 level that is considered to reflect “substantial” agreement and identify a clinically useful procedure.42 In fact, none achieved the ϰ ≥ .40 level that defines “moderate” agreement. Fryer et al found that training did not improve reliability22, similar to findings reported in other studies43. In a review, Seffinger et al.44 found that neither examiners’ discipline, experience level, agreement on procedure used, nor use of symptomatic participants increased reliability. Since palpation of the PSISs is the starting point for other pelvic examination procedures, examiner inability to agree on the location of the PSIS may negatively impact their ability to perform, interpret, and agree upon the results of other manual pelvic examination procedures.23
The articles in this review that specified the aspect of the PSIS with which the examiners made contact specified either the inferior aspect or the most posterior point. Since the PSIS in some individuals has a rather blade-like (rather than protuberant) anatomy, it is unlikely that attempting to locate the most posterior aspect would result in consistent findings – in effect, there would be no “most posterior” aspect. Palpating the inferior aspect of the PSIS, on the other hand, is not likely to yield consistent results because this method precludes easily using the index fingers to serve as stabilizing anchors on an adjacent anatomical structure. The first author of this study routinely anchors his index fingers on the lateral iliac crests while using his thumbs to probe an area somewhat superolateral to the superior aspect of the PSISs, in order to make better use of tactile sense. Figure 3 illustrates seated PSIS palpation using this method.45 The authors are unaware of any published evidence regarding the reproducibility of this method, contacting the superior aspect of the PSISs.
Figure 3.
PSIS palpation at superior aspect
The fact that examiners may not agree with each other on the location of landmarks, but may manifest internal consistency in their individual palpatory efforts, may explain why intraexaminer generally exceeds interexaminer reliability in the included studies, as in many other manual therapy studies. One of the authors included in this review wrote: “No attempt was made to rigidly standardize each test as this would have interfered with each therapist’s normal assessments”.21 Although we recognize this author’s effort to increase the external validity of the study, the resulting lack of methodological standardization may have contributed to poor examiner agreement. The present authors think it more appropriate that examiners develop reproducible patient examination methods, refining and standardizing methods as required. Demonstrating reliability alone does not establish an examination method as clinically useful; but without reliability, there would be no point in proceeding to validity studies, nor reason to think the method may remain clinically useful.
Limitations of the study
By excluding studies not in the English language, and also studies written to fulfill a thesis requirement, relevant information may not have been included. None of the authors who reported kappa values for interexaminer reliability provided the standard deviation, thus precluding meta-analysis using the method described by Goldman.46 Among the included studies, the data were reported using dissimilar methods, although most did use the kappa statistic. Given there were some differences in the aspect of the PSIS that was palpated among the included studies, it should not be assumed that the palpatory methods gathered entirely equivalent data, which warrants caution in interpreting the mean kappa levels reported. Combining data from studies with very different quality scores also warrants cautious interpretation, especially given the statistical tendency for the higher quality studies to show more reliability. None of the included studies reported a palpatory method involving the superior aspect of the PSIS, the first author’s preferred method. The authors are unaware of any published evidence regarding the reproducibility of this method. Unless and until this method undergoes reliability assessment, it would be premature to entirely reject the possible clinical utility of PSIS palpation.
Conclusion
Although claims have been made that palpatory procedures can detect subtle misalignments, fixations, and soft tissue changes in patients with neuromusculoskeletal disorders, and that the requisite skills take a considerable amount of time to acquire, there is little evidence at this time in support of these contentions with regard to PSIS palpation. Although the evidence available at the present time does not support clinical utility of manual PSIS palpation as a self-contained assessment nor as a component of other pelvic examination methods, it remains to be seen whether an alternative method or improvements in standardizing the methods can increase examiner reliability and thus clinical utility.
Footnotes
Disclosures:
None of the authors has any commercial interest in the results of this study or belongs to any organizations that may benefit from the publication.
Support:
This study was conducted with no funding beyond the internal support provided by the two chiropractic colleges that employ the authors.
Support:
This study was conducted with no funding beyond the internal support provided by Palmer West and Life West Chiropractic Colleges, which employ the first and second authors, respectively.
References:
- 1.Bergmann T, Peterson DH. Chiropractic Technique. St. Louis: Elsevier; 2011. pp. 35–83. [Google Scholar]
- 2.Levangie PK. The association between static pelvic asymmetry and low back pain. Spine. 1999;24(12):1234–1242. doi: 10.1097/00007632-199906150-00011. [DOI] [PubMed] [Google Scholar]
- 3.Levangie PK. Four clinical tests of sacroiliac joint dysfunction: the association of test results with innominate torsion among patients with and without low back pain. Phys Ther. 1999;79(11):1043–1057. [PubMed] [Google Scholar]
- 4.Kim HW, Ko YJ, Rhee WI, Lee JS, Lim JE, Lee SJ, et al. Interexaminer reliability and accuracy of posterior superior iliac spine and iliac crest palpation for spinal level estimations. J Manipulative Physiol Ther. 2007;30(5):386–389. doi: 10.1016/j.jmpt.2007.04.005. [DOI] [PubMed] [Google Scholar]
- 5.Chakraverty R, Pynsent P, Isaacs K. Which spinal levels are identified by palpation of the iliac crests and the posterior superior iliac spines? J Anat. 2007;210(2):232–236. doi: 10.1111/j.1469-7580.2006.00686.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bourdillon J, Day E. Spinal Manipulation. 4th ed. Over Wallop, New Hamphsire, England: BAS Printers, Limited; 1987. p. 250. [Google Scholar]
- 7.Cooperstein R. Assessment of sitting-standing pelvic landmarks for anatomical LLI: Or Darwin’s finches and leg checking. J Am Chiropr Assoc. 2006;43(2):12–14. [Google Scholar]
- 8.Potter NA, Rothstein JM. Intertester reliability for selected clinical tests of the sacroiliac joint. Phys Ther. 1985;65(11):1671–1675. doi: 10.1093/ptj/65.11.1671. [DOI] [PubMed] [Google Scholar]
- 9.Peterson DH, Bergmann T. Chiropractic Technique. 2 ed. Saint Louis, MI: Churchill Livingstone Inc; 2002. p. 532. [Google Scholar]
- 10.Paydar D, Thiel H, Gemmell H. Intra- and Interexaminer reliability of certain pelvic palpatory procedures and the sitting flexion test for sacroiliac joint mobility and dysfunction. J Neuromusculoskel Sys. 1994;2(2):65–69. [Google Scholar]
- 11.Meijne W, van Neerbos K, Aufdemkampe G, van der Wurff P. Intraexaminer and interexaminer reliability of the Gillet test. J Manipulative Physiol Ther. 1999;22(1):4–9. doi: 10.1016/s0161-4754(99)70098-9. [DOI] [PubMed] [Google Scholar]
- 12.Forst SL, Wheeler MT, Fortin JD, Vilensky JA. The sacroiliac joint: anatomy, physiology and clinical significance. Pain Physician. 2006;9(1):61–67. [PubMed] [Google Scholar]
- 13.Holmgren U, Waling K. Inter-examiner reliability of four static palpation tests used for assessing pelvic dysfunction. Man Ther. 2008;13(1):50–56. doi: 10.1016/j.math.2006.09.009. [DOI] [PubMed] [Google Scholar]
- 14.Lucas NP, Macaskill P, Irwig L, Bogduk N. The development of a quality appraisal tool for studies of diagnostic reliability (QAREL) J Clin Epidemiol. 2010;63(8) doi: 10.1016/j.jclinepi.2009.10.002. [DOI] [PubMed] [Google Scholar]
- 15.Tong HC, Heyman OG, Lado DA, Isser MM. Interexaminer reliability of three methods of combining test results to determine side of sacral restriction, sacral base position, and innominate bone position. J Am Osteopath Assoc. 2006;106(8):464–468. [PubMed] [Google Scholar]
- 16.Moriguchi CS, Carnaz L, Silva LC, Salasar LE, Carregaro RL, Sato Tde O, et al. Reliability of intra- and inter-rater palpation discrepancy and estimation of its effects on joint angle measurements. Man Ther. 2009;14(3):299–305. doi: 10.1016/j.math.2008.04.002. [DOI] [PubMed] [Google Scholar]
- 17.McGaugh JM, Brismee JM, Dedrick GS, Jones EA, Sizer PS. Comparing the anatomical consistency of the posterior superior iliac spine to the iliac crest as reference landmarks for the lumbopelvic spine: a retrospective radiological study. Clin Anat. 2007;20(7):819–825. doi: 10.1002/ca.20531. [DOI] [PubMed] [Google Scholar]
- 18.Riddle DL, Freburger JK. Evaluation of the presence of sacroiliac joint region dysfunction using a combination of tests: a multicenter intertester reliability study. Phys Ther. 2002;82(8):772–781. [PubMed] [Google Scholar]
- 19.van Kessel-Cobelens AM, Verhagen AP, Mens JM, Snijders CJ, Koes BW. Pregnancy-related pelvic girdle pain: intertester reliability of 3 tests to determine asymmetric mobility of the sacroiliac joints. J Manipulative Physiol Ther. 2008;31(2):130–136. doi: 10.1016/j.jmpt.2007.12.003. [DOI] [PubMed] [Google Scholar]
- 20.Simmonds MJ, Kumar S. Health care ergonomics Part II: Location of body structures by palpation - A reliability study. In J Indust Ergon. 1993;11:145–151. [Google Scholar]
- 21.Lindsay D, Meeuwisse W, Mooney M, Summersides J. Interrater reliability of manual therapy assessment techniques. Physiother Canada. 1995;47(3):173–180. [Google Scholar]
- 22.Fryer G, McPherson HC, O’Keefe P. The effect of training on the inter-examiner and intra-examiner reliability of the seated flexion test and assessment of pelvic anatomical landmarks with palpation. Int J Osteopath Med. 2005;8(4):131. [Google Scholar]
- 23.O’Haire C, Gibbons P. Inter-examiner and intra-examiner agreement for assessing sacroiliac anatomical landmarks using palpation and observation: pilot study. Man Ther. 2000;5(1):13–20. doi: 10.1054/math.1999.0203. [DOI] [PubMed] [Google Scholar]
- 24.Kmita A, Lucas N. Reliability of physical examination to assess asymmetry of anatomical landmarks indicative of pelvic somatic dysfunction in subjects with and without low back pain. Int J Osteopath Med. 2008;11:16–25. [Google Scholar]
- 25.Suwanasri C, Sakullertphasuk W, Tosiriphattana M, Sangounsak T, Ekabutr W. Inter- and intra-rater reliability of postural assessment for scoliosis. J Med Assoc Thai. 2014;97(Suppl 7):S1–5. [PubMed] [Google Scholar]
- 26.Byfield DC, Kinsigner S. A manual therapists guide to surface anatomy & palpation skills. Oxford: Butterworth Heinemann; 2002. p. 173. [Google Scholar]
- 27.Sutton C, Nono L, Johnston RG, Thomson OP. The effects of experience on the inter-reliability of osteopaths to detect changes in posterior superior iliac spine levels using a hidden heel wedge. J Bodywork Movement Ther. 2013;17(2):143–150. doi: 10.1016/j.jbmt.2012.07.005. [DOI] [PubMed] [Google Scholar]
- 28.Byfield DC, Mathiasen J, Sangren C. The reliability of osseous landmark palpation in the lumbar spine and pelvis. Eur J Chiro. 1992;40:83–88. [Google Scholar]
- 29.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159–174. [PubMed] [Google Scholar]
- 30.Cossart E. Statistic palpation of posterior superior iliac spines: An intra-examiner reliability study of final-year undergraduate osteopathic students. United Kingdom: European School of Osteopathy; 2013. [Google Scholar]
- 31.Cooperstein R. Two types of motion palpation: The excursion and tne end-feel methods. JACA Online. 2008;45(5) Online access only p 25–26. [Google Scholar]
- 32.Delamothe T. Diagnosis - The next frontier. Br Med J. 2006;333 [Google Scholar]
- 33.Cooperstein R. A shortish treatise on determining the optimum place to adjust. J Amer Chiropr Assoc. 2010;47(9):12–17. [Google Scholar]
- 34.Cooperstein R, Lisi A. Pelvic torsion: anatomical considerations, construct validity, and chiropractic examination procedures. Topics Clin Chiro. 2000;7(3):38–49. [Google Scholar]
- 35.Thompson DM, Vrugtman R. Biometric comparison of the heights and widths of paired innominates. J Chirop Educ. 2003;17(1):39–40. [Google Scholar]
- 36.Badii M, Shin S, Torreggiani WC, Jankovic B, Gustafson P, Munk PL, et al. Pelvic Bone Asymmetry in 323 Study Participants Receiving Abdominal CT Scans. Spine. 2003;28(12):1335–1339. doi: 10.1097/01.BRS.0000065480.44620.C5. [DOI] [PubMed] [Google Scholar]
- 37.Preece SJ, Willan P, Nester CJ, Graham-Smith P, Herrington L, Bowker P. Variation in pelvic morphology may prevent the identification of anterior pelvic tilt. J Man Manip Ther. 2008;16(2):113–117. doi: 10.1179/106698108790818459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Goode A, Hegedus EJ, Sizer P, Brismee JM, Linberg A, Cook CE. Three-dimensional movements of the sacroiliac joint: a systematic review of the literature and assessment of clinical utility. J Man Manip Ther. 2008;16(1):25–38. doi: 10.1179/106698108790818639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Stovall BA, Kumar S. Reliability of bony anatomic landmark asymmetry assessment in the lumbopelvic region: application to osteopathic medical education. J Am Osteopath Assoc. 2010;110(11):667–674. [PMC free article] [PubMed] [Google Scholar]
- 40.Long A, Donelson R, Fung T. Does it matter which exercise? A randomized control trial of exercise for low back pain. Spine. 2004;29(23):2593–602. doi: 10.1097/01.brs.0000146464.23007.2a. [DOI] [PubMed] [Google Scholar]
- 41.Lisi AJ, Cooperstein R, Morschhauser E. A pilot study of provocation testing with pelvic wedges: Can prone blocking demonstrate a directional preference? J Chirop Educ. 2002;16(1):30–31. doi: 10.1016/j.jmpt.2003.12.005. [DOI] [PubMed] [Google Scholar]
- 42.Landis JR, Koch GG. An application of hierarchical kappa-type statistics in the assessment of majority agreement among multiple observers. Biometrics. 1977;33(2):363–374. [PubMed] [Google Scholar]
- 43.Mior SA, Kopansky-Giles DR, Crowther ER, Wright JG. A comparison of radiographic and electrogoniometric angles in adolescent idiopathic scoliosis. Spine. 1996;21(13):1549–1555. doi: 10.1097/00007632-199607010-00013. [DOI] [PubMed] [Google Scholar]
- 44.Seffinger MA, Najm WI, Mishra SI, Adams A, Dickerson VM, Murphy LS, et al. Reliability of spinal palpation for diagnosis of back and neck pain: a systematic review of the literature. Spine. 2004;29(19):E413–425. doi: 10.1097/01.brs.0000141178.98157.8e. [DOI] [PubMed] [Google Scholar]
- 45.Cooperstein R. Palpating the pelvis for torsion. J Am Chiropractic Assoc. 2004;41(9):48–50. [Google Scholar]
- 46.Goldman RL. The reliability of peer assessments. A meta-analysis. Eval Health Prof. 1994;17(1):3–21. doi: 10.1177/016327879401700101. [DOI] [PubMed] [Google Scholar]