Abstract
Background: Studies have reported inconsistent findings on the association between dairy product intake and weight change and obesity. Only a few prospective studies have investigated the role of dairy consumption in both weight change and risk of becoming overweight or obese and whether these associations depend on the initial body weight.
Objective: We prospectively investigated how dairy product intake was associated with weight change and risk of becoming overweight or obese in initially normal-weight women.
Design: We studied 18,438 women aged ≥45 y from the Women’s Health Study who were free of cardiovascular disease, cancer, and diabetes and had initial body mass index (BMI; in kg/m2) from 18.5 to <25 at baseline. Dairy intake was assessed with the use of a 131-item food-frequency questionnaire. Women self-reported body weight along with obesity-related risk factors on baseline and annual follow-up questionnaires. At each follow-up time, women were categorized as normal weight (BMI: 18.5 to <25), overweight (BMI: 25 to <30), or obese (BMI ≥30).
Results: During a mean follow-up of 11.2 y, 8238 women became overweight or obese. Multivariable-adjusted mean ± SD changes in body weight during the follow-up (18 y) were 1.90 ± 0.09, 1.88 ± 0.08, 1.86 ± 0.09, 1.82 ± 0.09, and 1.65 ± 0.09 kg in quintiles 1–5 of total dairy intake, respectively (P-trend = 0.003). Greater intake of high-fat dairy products, but not intake of low-fat dairy products, was associated with less weight gain (P-trend = 0.004). In multivariable-adjusted analyses, lower risk of becoming overweight or obese was observed in the highest quintile of high-fat dairy product intake (HR: 0.92, 95% CI: 0.86, 0.99). Dietary or supplemental calcium or vitamin D was not associated with risk of becoming overweight or obese.
Conclusion: Greater consumption of total dairy products may be of importance in the prevention of weight gain in middle-aged and elderly women who are initially normal weight.
Keywords: cohort, dairy, obesity, overweight, weight
INTRODUCTION
Dairy products are widely consumed in the United States and in other developed countries and have been recommended to meet nutritional requirements for protein, vitamin D, calcium, potassium, and other nutrients (1, 2). In contrast, dairy products may contribute to excessive SFA and caloric intakes. As a result, the current recommendation of the 2010 Dietary Guidelines for Americans is for individuals to consume 2–3 cups low-fat dairy products/d (3). However, the evidence for dairy consumption in chronic disease prevention has been questioned because of the lack of well-powered randomized trials with enough follow-up time to see effects on health outcomes (2).
Obesity remains a major public health concern; in the United States, the NHANES has reported that more than one-third (34.9%) of the US population were obese in 2011–2012 (4). Diet and physical activity have been pointed out as important targets in the prevention of weight gain and obesity development (5). In a meta-analysis of 27 small-scale randomized controlled trials, which included a total of 2101 women and men, higher dairy consumption lowered body weight in the context of energy restriction in short-term (<1 y) but not long-term (≥1 y) trials (6). Prospective cohort studies have reported mixed results, and the heterogeneity in selected study populations on the basis of obesity status has complicate the interpretation of these results (7–13). Moreover, a limited number of prospective studies have investigated dairy consumption with both weight change and risk of becoming overweight or obese and whether these associations depend on initial body weight.
We aimed to prospectively investigate how consumption of dairy products was associated with risk of becoming overweight or obese in a cohort of middle-aged and elderly women and whether the association differed by low-fat and high-fat dairy intakes plus the specific types of dairy products. We also investigated how dietary and supplemental calcium and vitamin D, which are 2 major nutrients in dairy products, were associated with risk of becoming overweight or obese.
METHODS
The Women’s Health Study was a 2 × 2 × 2 factorial trial of low-dose aspirin, vitamin E, and β-carotene in the primary prevention of cardiovascular disease and cancer in female US health professionals. From 1992 to 1995, 39,876 women aged ≥45 y who were postmenopausal or not intending to become pregnant and with no history of myocardial infarction, stroke, transient ischemic attack, or cancer (except nonmelanoma skin cancer) provided information on a wide range of lifestyle, clinical, and dietary factors. A total of 39,310 (98.6%) of the participating women also completed a 131-item validated semiquantitative food-frequency questionnaire (FFQ) (14, 15). At baseline, women further provided self-reported information on weight (lb) and height (in). Because we sought to investigate the incidence of becoming overweight or obese, we restricted our analyses to women with a baseline BMI (in kg/m2; calculated as body weight divided by the square of height) of 18.5–25 (n = 20,106). We also excluded women who reported a history of diabetes (n = 1,143) or, at baseline, had missing information on dairy intake, responded to an insufficient number of food items, or had total energy intake outside the range of 600–3500 kcal/d. Our study population for the analysis consisted of 18,438 women who were followed through 28 February 2012. Written informed consent was obtained from all participants, and the research was approved by the Institutional Review Board of Brigham and Women’s Hospital.
Intakes of dairy products and dietary and supplemental calcium and vitamin D
At baseline, women completed an FFQ that asked about how often they consumed specific food items, on average, during the previous year. Nine response categories ranging from never or less than once per month to ≥6 servings/d were included. For each food group, the average daily intake (servings/d) was calculated by summing the intake frequency of the specific items. Total dairy product intake was calculated by summing intake of low-fat dairy products (skim and low-fat milk, sherbet, yogurt, and cottage and ricotta cheeses) and high-fat dairy products (whole milk, cream, sour cream, ice cream, cream cheese, other cheese, and butter). Dietary calcium and vitamin D intakes were computed by multiplying the intake frequency by the nutrient content of the specified portion size according to food-composition tables from the Harvard T.H. Chang School of Public Health (16). Dietary calcium and vitamin D intakes were energy-adjusted with the use of the residual method (17). Women also self-reported the use of individual or multivitamin supplements including calcium and vitamin D. The validity of self-reported dairy product intake has been investigated in similar cohorts of health professionals, and Pearson correlation coefficients between the FFQ and 24-h dietary records were 0.79 for skim milk, 0.62 for whole milk (18), and 0.68 for dietary calcium (19).
Other covariates
At baseline, women also provided information on age and lifestyle factors such as smoking status, physical activity level, postmenopausal status, and postmenopausal hormone use. Physical activity was based on the following 8 recreational activities: walking and hiking; jogging; running; bicycling; aerobic exercise and dance; lap swimming; tennis, squash, and racquetball; lower-intensity exercise, yoga, stretching, and toning; and the number of flights of stairs climbed daily. The metabolic equivalent task score was calculated to reflect the energy expenditure of ∼1 kcal · kg body weight−1 · h−1 (20). The correlation between self-reported physical activity and four 1-wk activity diaries over 1 y was 0.62 in a similar population of women (21). Women also self-reported information on clinical factors including a history of hypercholesterolemia and hypertension. Dietary factors such as alcohol intake, multivitamin use, and fruit and vegetable intake were estimated from the FFQ.
Development of overweight or obesity during follow-up
At the start of follow-up, we included all women with normal weight (BMI: 18.5 to <25). Body weight was updated on follow-up questionnaires at years 2, 3, 5, 6, 9, and 11 and annually thereafter. Changes in body weight between baseline and the different time points as well as the end of intervention period (10 y) and observational period (17 y) were calculated. At each follow-up time point, women were categorized as normal weight (BMI: 18.5 to <25), overweight (BMI: 25 to <30), or obese (BMI ≥30) (22). In the analysis of risk of becoming overweight or obese, women were followed from baseline to the date of the questionnaire on which they first reported a weight that corresponded to being overweight or obese, their date of death, or the end of follow-up, whichever occurred first. The validity between self-reported and standardized measurements of body weight taken by technicians has been shown to be high in similar cohort of female health professionals with a Pearson correlation coefficient of 0.97 (15).
Statistical analyses
All statistical analyses were performed with SAS version 9.3 software (SAS Institute Inc.) and Stata version 13.1 software (StataCorp LP). We categorized women into quintiles of total, low-fat, or high-fat dairy intake as well as quintiles of dietary calcium and vitamin D intakes. We also categorized women on the basis of calcium and vitamin D supplement dosages. Age-standardized mean values ± SDs for continuous variables and percentages for categorical variables were calculated and compared across categories. Linear trends were calculated with the use of an ANOVA for continuous and categorical variables.
Multivariable-adjusted weight changes (kg) and 95% CIs between baseline and different follow-up time points within quintiles of total dairy intake were estimated with the use of a multilevel mixed-effects linear regression model with the assumption of a Gaussian residual structure with one common variance. Restricted cubic spline analyses modeled the body weight change (lb) within quintiles 1 and 5 of total dairy intake. Cox proportional hazards models were used to calculate HRs (95% CIs) of becoming overweight or obese (23). All HRs were adjusted for baseline age (y; continuous), smoking status (never, past, or currently smoking <15 or ≥15 cigarettes/d), physical activity (energy expenditure in metabolic equivalent task hours per week), postmenopausal status (no, yes, biologically uncertain, or unclear), use of hormone replacement therapy (never, past, or current), history of hypertension (yes or no), history of hypercholesterolemia (yes or no), alcohol consumption (rarely or never, 1–3 drinks/mo, 1–6 drinks/wk, or ≥1 drink/wk), and caloric intake (kcal/d). Baseline BMI (continuous) was finally added to all models. Linear trends across quintiles were tested with the use of the median value of each quintile as an ordinal variable. In a sensitivity analysis, we calculated the person-time by also censoring on the date of diabetes diagnosis during follow-up to avoid possible influence on weight control because of new diabetes diagnosis.
To investigate the effect modification by important lifestyle factors related to dairy consumption and risk of becoming overweight or obese, we performed stratified analyses by age, baseline BMI, smoking status, and physical activity. We tested for interactions with the use of Wald’s chi-square tests. The proportional hazards assumption was tested by entering the product of baseline intakes of total dairy intake and the ln of time in the model. There was evidence of a violation of this assumption (P = 0.0007). Two-sided P values <0.05 were considered statistically significant.
RESULTS
Background characteristics
During an mean of 11.2 y of follow up, 8238 of 18,438 women became overweight or obese. In Table 1, we present baseline characteristics of the women according to quintiles of total dairy intake. Women in the highest quintile of total dairy intake compared with those in the lowest had significantly higher age, physical activity, total calorie intake, and fruit and vegetable intake and were more likely to consume ≥1 alcoholic drink/mo and to use multivitamin supplements. These women were also significantly less likely to be current smokers, be current users of hormone replacement therapy, or have a history of hypercholesterolemia and hypertension.
TABLE 1.
Background characteristics according to quintiles of baseline total dairy product intake1
| Quintiles of total dairy intake |
||||||
| 1 (n = 3649) | 2 (n = 3759) | 3 (n = 3690) | 4 (n = 3705) | 5 (n = 3635) | P-trend | |
| Intake,2 servings/d | 0.6 | 1.3 | 1.8 | 2.6 | 3.9 | |
| Age,3 y | 54.2 ± 7.0 | 54.5 ± 7.0 | 54.4 ± 7.0 | 54.7 ± 7.3 | 54.5 ± 7.3 | 0.03 |
| BMI, kg/m2 | 22.4 ± 1.4 | 22.4 ± 1.6 | 22.4 ± 1.6 | 22.5 ± 1.6 | 22.4 ± 1.6 | 0.65 |
| Total MET-h4/wk | 15.2 ± 19.8 | 16.1 ± 18.7 | 17.2 ± 19.3 | 18.0 ± 20.1 | 18.7 ± 20.9 | <0.0001 |
| Current smokers, % | 18 | 15 | 12 | 11 | 13 | <0.0001 |
| Postmenopausal, % | 55 | 53 | 54 | 53 | 54 | 0.15 |
| Current use of postmenopausal hormones, % | 46 | 45 | 47 | 45 | 42 | <0.0001 |
| Hypercholesterolemia, % | 29 | 27 | 25 | 24 | 21 | <0.0001 |
| Hypertension, % | 18 | 17 | 16 | 15 | 14 | 0.0009 |
| Alcohol use ≥1 drink/mo, % | 58 | 62 | 63 | 63 | 64 | <0.0001 |
| Current users of multivitamins, % | 29 | 31 | 32 | 31 | 32 | 0.02 |
| Total calories, kcal/d | 1368 ± 435 | 1541 ± 433 | 1696 ± 450 | 1845 ± 470 | 2063 ± 497 | <0.0001 |
| Fruit and vegetable intake, servings/d | 5.2 ± 3.3 | 5.6 ± 3.0 | 6.1 ± 2.9 | 6.6 ± 3.2 | 6.9 ± 3.4 | <0.0001 |
| Dairy products, servings/d | ||||||
| Skimmed milk | 0.1 ± 0.2 | 0.5 ± 0.4 | 0.6 ± 0.4 | 1.1 ± 0.8 | 1.8 ± 1.2 | <0.0001 |
| Whole milk | 0.01 ± 0.1 | 0.02 ± 0.1 | 0.03 ± 0.1 | 0.05 ± 0.2 | 0.1 ± 0.5 | <0.0001 |
| Sherbet | 0.05 ± 0.1 | 0.09 ± 0.2 | 0.14 ± 0.2 | 0.18 ± 0.3 | 0.22 ± 0.4 | <0.0001 |
| Cream | 0.01 ± 0.0 | 0.04 ± 0.1 | 0.05 ± 0.2 | 0.1 ± 0.4 | 0.6 ± 1.3 | <0.0001 |
| Yogurt | 0.05 ± 0.1 | 0.1 ± 0.2 | 0.2 ± 0.2 | 0.2 ± 0.3 | 0.3 ± 0.4 | <0.0001 |
| Cheese | 0.1 ± 0.1 | 0.2 ± 0.2 | 0.3 ± 0.3 | 0.4 ± 0.3 | 0.5 ± 0.6 | <0.0001 |
| Cream cheese | 0.03 ± 0.1 | 0.05 ± 0.1 | 0.07 ± 0.1 | 0.08 ± 0.1 | 0.09 ± 0.1 | <0.0001 |
| Cottage cheese | 0.04 ± 0.1 | 0.06 ± 0.1 | 0.09 ± 0.1 | 0.11 ± 0.2 | 0.13 ± 0.2 | <0.0001 |
| Butter | 0.03 ± 0.1 | 0.07 ± 0.2 | 0.1 ± 0.2 | 0.2 ± 0.4 | 0.5 ± 0.9 | <0.0001 |
Unless otherwise specified, all values are means ± SDs for continuous variables and percentages for categorical variables and were standardized to the age distribution of the study population. An ANOVA was used to test for P-trend values.
All values are medians.
Values were not age adjusted.
MET-h, metabolic equivalent task hours.
Dairy intake in association with weight change
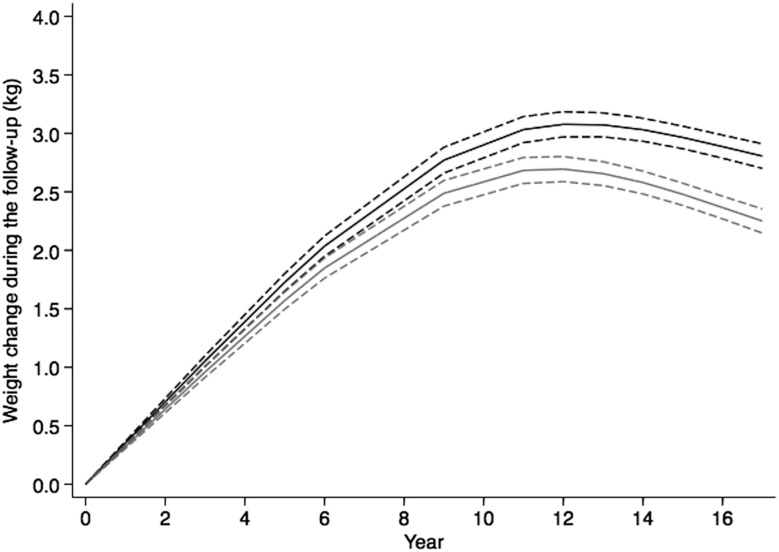
In Table 2, the longitudinal changes in body weight between baseline and the end of observational period (17 y) are presented according to quintiles of consumption of total, high-fat, and low-fat dairy products. The multivariable adjusted mean ± SE changes in body weight during follow-up were 1.90 ± 0.09, 1.88 ± 0.09, 1.86 ± 0.09, 1.82 ± 0.09, and 1.65 ± 0.09 kg in quintiles 1–5 of total dairy intake, respectively (P-trend = 0.003). A similar significant trend was observed for high-fat dairy intake (P-trend = 0.004) but not for low-fat dairy intake (P-trend = 0.36). Additional adjustment for baseline BMI marginally changed the results. Moreover, when dietary fiber was added to the model, similar results were observed (data not shown). In sensitivity analyses, we investigated whether intakes of butter and cream were driving the associations for high-fat dairy intake by excluding these items from this variable. As a result, the association was somewhat attenuated, but a significant trend remained in each model, including the multivariable-adjusted model with the addition of baseline BMI (P-trend = 0.04). We further investigated the association between dairy intake and weight change at the end of the intervention period (10 y) and observed similar trend for intakes of high-fat dairy products (P-trend = 0.002) but a nonsignificant trend for total intake of dairy products (P-trend = 0.14) and intake of low-fat dairy products (P-trend = 0.36) (Supplemental Table 1). In Figure 1, we show the mean change in body weight within quintiles 1 and 5 of total dairy consumption for the different follow-up time points. During follow-up, an increase in body weight was observed regardless of total dairy intake; however, women who consumed greater total dairy products gained less weight than did women who consumed fewer total dairy products. Weight changes within quintile 1 were 1.8, 2.8, and 3.0 kg at years 5, 10, and 15, respectively. The corresponding weight changes for quintile 5 were 1.8, 2.5, and 2.5 kg, respectively. In mixed-modeling analyses, there was a significant interaction between total dairy intake and the follow-up time on the changes in body weight (P < 0.0001).
TABLE 2.
Changes in body weight between baseline and last follow-up time point (year 17) according to quintiles of baseline dairy intake (n = 14,014)1
| n | Age-adjusted weight change, kg | Multivariable-adjusted weight change, kg | Multivariable-adjusted weight change plus baseline BMI, kg | |
| Total dairy intake, servings/d | ||||
| Quintile 1: 0 to <1.0 | 2613 | 1.60 ± 0.062 | 1.90 ± 0.09 | 1.89 ± 0.09 |
| Quintile 2: 1.0 to <1.5 | 2822 | 1.58 ± 0.06 | 1.88 ± 0.09 | 1.87 ± 0.09 |
| Quintile 3: 1.5 to <2.1 | 2927 | 1.54 ± 0.06 | 1.86 ± 0.09 | 1.85 ± 0.09 |
| Quintile 4: 2.1 to <3.1 | 2876 | 1.50 ± 0.06 | 1.82 ± 0.09 | 1.81 ± 0.09 |
| Quintile 5: ≥3.1 | 2776 | 1.33 ± 0.06 | 1.65 ± 0.09 | 1.63 ± 0.09 |
| P-trend | — | 0.0006 | 0.003 | 0.002 |
| Low-fat dairy intake, servings/d | ||||
| Quintile 1: 0 to <0.3 | 2753 | 1.54 ± 0.06 | 1.84 ± 0.08 | 1.83 ± 0.08 |
| Quintile 2: 0.3 to <0.7 | 2631 | 1.56 ± 0.06 | 1.88 ± 0.09 | 1.86 ± 0.09 |
| Quintile 3: 0.7 to <1.1 | 2910 | 1.45 ± 0.06 | 1.77 ± 0.09 | 1.76 ± 0.08 |
| Quintile 4: 1.1 to <2.0 | 2859 | 1.56 ± 0.06 | 1.89 ± 0.09 | 1.87 ± 0.09 |
| Quintile 5: ≥2.0 | 2861 | 1.44 ± 0.06 | 1.77 ± 0.09 | 1.74 ± 0.09 |
| P-trend | — | 0.19 | 0.36 | 0.24 |
| High-fat dairy intake, servings/d | ||||
| Quintile 1: 0 to <0.2 | 3209 | 1.59 ± 0.05 | 1.90 ± 0.09 | 1.89 ± 0.09 |
| Quintile 2: 0.2 to <0.5 | 2300 | 1.62 ± 0.06 | 1.94 ± 0.09 | 1.92 ± 0.09 |
| Quintile 3: 0.5 to <0.8 | 2912 | 1.55 ± 0.06 | 1.88 ± 0.09 | 1.86 ± 0.09 |
| Quintile 4: 1.1 to <1.3 | 2915 | 1.41 ± 0.06 | 1.75 ± 0.09 | 1.74 ± 0.09 |
| Quintile 5: ≥1.3 | 2678 | 1.37 ± 0.06 | 1.71 ± 0.09 | 1.69 ± 0.09 |
| P-trend | — | 0.0006 | 0.004 | 0.005 |
Women who provided information on weight at baseline and year 17 were included in the analysis. Multivariable-adjusted weight changes were adjusted for age, randomization treatment, smoking status, physical activity, postmenopausal status, postmenopausal hormone use, history of hypercholesterolemia, history of hypertension, multivitamin use, alcohol intake, energy intake, and fruit and vegetable intake.
Mean ± SD (all such values).
FIGURE 1.
Multivariable-adjusted weight changes (kg) (solid lines) and 95% CIs (dashed lines) between baseline and different follow-up time points within quintile 1 (black) and quintile 5 (gray) that were estimated with the use of a multilevel mixed-effects linear regression model.
Dairy intake and risk of becoming overweight or obese
In age-adjusted analyses (Table 3), we observed that women in the highest quintile of total dairy intake (≥3.1 servings/d) compared with women in the lowest quintile of total dairy intake (<1.0 servings/d) had lower risk of becoming overweight or obese (HR: 0.91; 95% CI: 0.85, 0.97; P-trend = 0.002). In the highest compared with the lowest quintile of high-fat dairy intake, the age-adjusted HR was 0.90 (95% CI: 0.84, 0.96; P-trend = 0.0003), whereas no association was observed for low-fat dairy intake. Adjustment for other lifestyle, clinical, and dietary factors weakened the associations for total dairy and high-fat dairy intakes, but increased risk of becoming overweight or obese was observed in the highest quintile of low-fat dairy intake (HR: 1.10; 95% CI: 1.02, 1.18). When BMI was added to the model, the results were attenuated. The addition of dietary fiber did not change the results. We further investigated, in a sensitivity analysis, whether risk of becoming overweight or obese was affected by censoring for diabetes during follow-up, and similar associations were observed for total, low-fat, and high-fat dairy intakes (data not shown). In the multivariable-adjusted model, there were no significant associations observed for the highest compared with lowest quintiles of total dairy intake (HR: 1.03; 95% CI: 0.83, 1.29; P-trend = 0.32) or low-fat dairy intake (HR: 1.12; 9%% CI: 0.91, 1.38 P-trend = 0.21), whereas a tendency toward a linear trend was observed for high-fat dairy intake (HR: 0.84; 95% CI: 0.68, 1.04; P-trend = 0.07). Additional adjustment of baseline BMI showed similar results. We also investigated whether intakes of butter and cream were driving the associations for high-fat dairy product intake by excluding these items from the variable. In the multivariable-adjusted model, the HR of becoming overweight or obese in women in the highest compared with lowest quintiles of high-fat dairy product intake was 0.94 (95% CI: 0.88, 1.02; P-trend = 0.10). When BMI was added to the model, the results were further attenuated.
TABLE 3.
HRs (95% CIs) of becoming overweight or obese according to quintiles of baseline dairy intake (n = 18,438)1
| n | Cases, n | Age adjusted | Multivariable adjusted | Multivariable adjusted plus baseline BMI | |
| Total dairy intake, servings/d | |||||
| Quintile 1: 0 to <1.0 | 3649 | 1677 | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) |
| Quintile 2: 1.0 to <1.5 | 3759 | 1710 | 0.99 (0.93, 1.06) | 1.02 (0.95, 1.09) | 1.03 (0.96, 1.10) |
| Quintile 3: 1.5 to <2.1 | 3690 | 1667 | 0.98 (0.92, 1.05) | 1.03 (0.96, 1.10) | 1.05 (0.98, 1.13) |
| Quintile 4: 2.1 to <3.1 | 3705 | 1644 | 0.97 (0.91, 1.04) | 1.02 (0.95, 1.10) | 1.01 (0.94, 1.09) |
| Quintile 5: ≥3.1 | 3635 | 1540 | 0.91 (0.85, 0.97) | 0.97 (0.90, 1.05) | 0.96 (0.89, 1.04) |
| P-trend | — | — | 0.002 | 0.36 | 0.15 |
| Low-fat dairy intake, servings/d | |||||
| Quintile 1: 0 to <0.3 | 3907 | 1732 | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) |
| Quintile 2: 0.3 to <0.7 | 3478 | 1594 | 1.05 (0.98, 1.12) | 1.08 (1.01, 1.16) | 1.08 (1.01, 1.16) |
| Quintile 3: 0.7 to <1.1 | 3768 | 1673 | 1.01 (0.94, 1.08) | 1.05 (0.98, 1.13) | 1.07 (1.00, 1.15) |
| Quintile 4: 1.1 to <2.0 | 3612 | 1629 | 1.04 (0.98, 1.12) | 1.11 (1.04, 1.19) | 1.09 (1.02, 1.17) |
| Quintile 5: ≥2.0 | 3673 | 1610 | 1.02 (0.95, 1.09) | 1.10 (1.02, 1.18) | 1.06 (0.98, 1.13) |
| P-trend | — | — | 0.80 | 0.02 | 0.37 |
| High-fat dairy intake, servings/d | |||||
| Quintile 1: 0 to <0.2 | 4381 | 1979 | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) |
| Quintile 2: 0.2 to <0.5 | 3020 | 1408 | 1.00 (0.93, 1.07) | 1.00 (0.93, 1.07) | 0.98 (0.92, 1.05) |
| Quintile 3: 0.5 to <0.8 | 3740 | 1679 | 0.94 (0.88, 1.00) | 0.95 (0.89, 1.02) | 0.92 (0.86, 0.99) |
| Quintile 4: 1.1 to <1.3 | 3712 | 1624 | 0.90 (0.85, 0.97) | 0.93 (0.87, 0.99) | 0.93 (0.87, 1.00) |
| Quintile 5: ≥1.3 | 3585 | 1548 | 0.90 (0.84, 0.96) | 0.92 (0.85, 0.98) | 0.92 (0.86, 0.99) |
| P-trend | — | — | 0.0003 | 0.007 | 0.04 |
HRs and 95% CIs were calculated with the use of Cox proportional hazards regression models. Multivariable-adjusted HRs were adjusted for age, randomization treatment, smoking status, physical activity, postmenopausal status, postmenopausal hormone use, history of hypercholesterolemia, history of hypertension, multivitamin use, alcohol intake, energy intake, and fruit and vegetable intake.
Because we observed that the association between total dairy product intake and weight change varied by the follow-up time, we performed sensitivity analyses on risk of becoming overweight or obese by ending the follow-up after 8 y, which reflected the time point that was approximately halfway through the follow-up (Supplemental Table 2). In the multivariable-adjusted model that include BMI, no associations were observed for total dairy product intake (HR in the highest quintile: 1.02; 95% CI: 0.93, 1.12; P-trend = 0.83) and high-fat dairy intake (HR in the highest quintile: 0.91; 95% CI: 0.84, 0.995; P-trend = 0.04). However, significant increased risk was observed for low-fat dairy intake (HR in the highest quintile: 1.16; 95% CI: 1.06, 1.26; P-trend = 0.009).
In stratified analyses, we investigated whether the association between total dairy product intake varied by factors such as baseline age, BMI, smoking status, and physical activity (Table 4). We did not find any evidence of an effect modification for any of these factors (all P-interaction ≥ 0.10).
TABLE 4.
HRs (95% CIs) of becoming overweight or obese according to baseline total dairy intake by subgroups of women1
| Total dairy intake, servings/d |
|||||||
| Quintile 1: 0 to <1.0 | Quintile 2: 1.0 to <1.5 | Quintile 3: 1.5 to <2.1 | Quintile 4: 2.1 to <3.1 | Quintile 5: ≥3.1 | P-trend | P-interaction | |
| Age, y | |||||||
| ≤60 | |||||||
| Cases, n | 1453 | 1454 | 1426 | 1380 | 1287 | — | — |
| Multivariable | 1.00 (reference) | 1.05 (0.97, 1.13) | 1.06 (0.98, 1.14) | 1.01 (0.94, 1.09) | 0.96 (0.88, 1.04) | 0.11 | |
| >60 | |||||||
| Cases, n | 224 | 256 | 241 | 264 | 253 | — | — |
| Multivariable | 1.00 (reference) | 0.94 (0.79, 1.13) | 0.97 (0.80, 1.17) | 0.99 (0.82, 1.20) | 0.97 (0.79, 1.19) | 0.99 | 0.80 |
| BMI, kg/m2 | |||||||
| <23 | |||||||
| Cases, n | 544 | 560 | 523 | 516 | 449 | — | — |
| Multivariable | 1.00 (reference) | 1.02 (0.91, 1.15) | 1.00 (0.88, 1.13) | 1.03 (0.90, 1.17) | 0.91 (0.79, 1.05) | 0.18 | — |
| 23 to <24 | |||||||
| Cases, n | 503 | 497 | 489 | 457 | 459 | — | — |
| Multivariable | 1.00 (reference) | 1.03 (0.91, 1.17) | 1.07 (0.94, 1.22) | 0.94 (0.82, 1.08) | 0.95 (0.83, 1.10) | 0.21 | — |
| ≥24 | |||||||
| Cases, n | 630 | 653 | 655 | 671 | 632 | — | — |
| Multivariable | 1.00 (reference) | 1.10 (0.99, 1.23) | 1.15 (1.03, 1.29) | 1.09 (0.97, 1.22) | 1.06 (0.94, 1.20) | 0.77 | 0.10 |
| Smoking | |||||||
| Never | |||||||
| Cases, n | 759 | 815 | 807 | 851 | 773 | — | — |
| Multivariable | 1.00 (reference) | 1.02 (0.92, 1.13) | 1.03 (0.93, 1.14) | 1.03 (0.93, 1.15) | 0.94 (0.84, 1.05) | 0.22 | — |
| Past | |||||||
| Cases, n | 603 | 612 | 629 | 622 | 551 | — | — |
| Multivariable | 1.00 (reference) | 1.07 (0.96, 1.20) | 1.06 (0.95, 1.19) | 1.01 (0.89, 1.13) | 1.02 (0.90, 1.16) | 0.77 | — |
| Current | |||||||
| Cases, n | 315 | 283 | 231 | 171 | 216 | — | — |
| Multivariable | 1.00 (reference) | 0.98 (0.83, 1.16) | 1.09 (0.92, 1.30) | 0.90 (0.74, 1.10) | 0.91 (0.75, 1.11) | 0.25 | 0.36 |
| Physical activity, MET-h2/wk | |||||||
| <7.5 | |||||||
| Cases, n | 822 | 728 | 677 | 620 | 598 | — | — |
| Multivariable | 1.00 (reference) | 1.03 (0.93, 1.14) | 1.06 (0.95, 1.18) | 1.01 (0.91, 1.13) | 0.95 (0.84, 1.07) | 0.28 | — |
| ≥7.5 | |||||||
| Cases, n | 855 | 982 | 990 | 1024 | 942 | — | — |
| Multivariable | 1.00 (reference) | 1.03 (0.94, 1.13) | 1.05 (0.96, 1.15) | 1.01 (0.92, 1.11) | 0.98 (0.87, 1.09) | 0.47 | 0.96 |
HRs and 95% CIs were calculated with the use of Cox proportional hazards regression models. Multivariable adjusted HRs were adjusted for age, randomization treatment, BMI, smoking status, vigorous exercise, postmenopausal status, postmenopausal hormone use, history of hypercholesterolemia, history of hypertension, multivitamin use, alcohol intake, energy intake, and fruit and vegetable intake. Tests for interaction were calculated with the use of Wald’s test.
MET-h, metabolic equivalent task hours.
Types of dairy products and risk of becoming overweight or obese
We investigated specific types of dairy products and risk of becoming overweight and obese (Table 5). Higher risks were observed for ≥1 servings/d compared with 0 servings/d of the following products: skimmed milk (HR: 1.11; 95% CI: 1.04, 1.19; P-trend = 0.03), sherbet (HR: 1.21; 95% CI: 1.04, 1.42; P-trend = 0.003), and yogurt (HR: 1.16; 95% CI: 1.03, 1.31; P-trend = 0.001). Additional adjustment for baseline BMI attenuated the associations for skimmed milk and sherbet but not for yogurt.
TABLE 5.
HRs (95% CIs) of becoming overweight or obese according to categories of baseline intake of types of dairy products (n = 18,438)1
| n | Cases, n | Age adjusted | Multivariable adjusted | Multivariable adjusted plus baseline BMI | |
| Skim milk, servings/d | |||||
| 0 | 3127 | 1326 | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) |
| >0 to <0.5 | 6248 | 2915 | 1.12 (1.04, 1.19) | 1.14 (1.07, 1.22) | 1.07 (1.00, 1.14) |
| 0.5 to <1 | 1545 | 696 | 1.09 (0.99, 1.19) | 1.13 (1.03, 1.24) | 1.03 (0.94, 1.13) |
| ≥1 | 7344 | 3235 | 1.06 (0.99, 1.13) | 1.11 (1.04, 1.19) | 1.05 (0.98, 1.12) |
| P-trend | — | — | 0.45 | 0.03 | 0.44 |
| Whole milk, servings/d | |||||
| 0 | 15,703 | 7068 | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) |
| >0 to <0.5 | 1808 | 788 | 0.97 (0.90, 1.04) | 0.94 (0.88, 1.02) | 0.95 (0.89, 1.03) |
| 0.5 to <1 | 74 | 34 | 1.09 (0.78, 1.52) | 1.03 (0.74, 1.45) | 0.96 (0.68, 1.34) |
| ≥1 | 304 | 123 | 0.94 (0.79, 1.13) | 0.90 (0.76, 1.08) | 0.88 (0.73, 1.05) |
| P-trend | — | — | 0.62 | 0.29 | 0.14 |
| Sherbet, servings/d | |||||
| 0 | 6800 | 2880 | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) |
| >0 to <0.5 | 10,557 | 4873 | 1.12 (1.07, 1.17) | 1.15 (1.10, 1.20) | 1.05 (1.00, 1.10) |
| 0.5 to <1 | 451 | 211 | 1.16 (1.01, 1.34) | 1.22 (1.06, 1.40) | 1.11 (0.96, 1.27) |
| ≥1 | 362 | 167 | 1.16 (1.00, 1.36) | 1.21 (1.04, 1.42) | 1.03 (0.88, 1.21) |
| P-trend | — | — | 0.02 | 0.003 | 0.36 |
| Cream, servings/d | |||||
| 0 | 13,370 | 6015 | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) |
| >0 to <0.5 | 3461 | 1551 | 0.94 (0.89, 1.00) | 0.97 (0.91, 1.02) | 0.99 (0.94, 1.05) |
| 0.5 to <1 | 165 | 65 | 0.79 (0.62, 1.01) | 0.77 (0.60, 0.98) | 0.78 (0.61, 1.00) |
| ≥1 | 925 | 409 | 0.95 (0.86, 1.06) | 0.97 (0.88, 1.07) | 0.96 (0.86, 1.06) |
| P-trend | — | — | 0.33 | 0.45 | 0.27 |
| Yogurt, servings/d | |||||
| 0 | 7442 | 3277 | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) |
| >0 to <0.5 | 9482 | 4272 | 1.00 (0.95, 1.04) | 1.04 (0.99, 1.09) | 1.01 (0.97, 1.06) |
| 0.5 to <1 | 566 | 272 | 1.11 (0.98, 1.26) | 1.20 (1.06, 1.36) | 1.16 (1.03, 1.32) |
| ≥1 | 605 | 281 | 1.08 (0.95, 1.22) | 1.16 (1.02, 1.31) | 1.16 (1.02, 1.31) |
| P-trend | — | — | 0.05 | 0.001 | 0.002 |
| Cheese, servings/d | |||||
| 0 | 1232 | 520 | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) |
| >0 to <0.5 | 14,702 | 6638 | 1.02 (0.93, 1.12) | 1.06 (0.97, 1.16) | 1.04 (0.95, 1.14) |
| 0.5 to <1 | 1332 | 588 | 0.96 (0.85, 1.08) | 1.04 (0.92, 1.17) | 1.05 (0.93, 1.18) |
| ≥1 | 1029 | 429 | 0.90 (0.79, 1.02) | 0.96 (0.85, 1.10) | 1.02 (0.90, 1.17) |
| P-trend | — | — | 0.007 | 0.14 | 0.92 |
| Cream cheese, servings/d | |||||
| 0 | 9611 | 4306 | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) |
| >0 to <0.5 | 8219 | 3674 | 0.97 (0.93, 1.01) | 0.99 (0.95, 1.04) | 0.99 (0.95, 1.03) |
| 0.5 to <1 | 99 | 37 | 0.79 (0.57, 1.08) | 0.78 (0.57, 1.08) | 1.01 (0.73, 1.39) |
| ≥1 | 82 | 32 | 0.79 (0.56, 1.12) | 0.82 (0.58, 1.15) | 1.00 (0.71, 1.42) |
| P-trend | — | — | 0.03 | 0.07 | 0.91 |
| Cottage cheese, servings/d | |||||
| 0 | 7598 | 3435 | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) |
| >0 to <0.5 | 10,337 | 4587 | 1.01 (0.96, 1.05) | 1.03 (0.99, 1.08) | 1.03 (0.98, 1.08) |
| 0.5 to <1 | 159 | 69 | 1.02 (0.81, 1.30) | 1.05 (0.82, 1.33) | 1.19 (0.94, 1.51) |
| ≥1 | 87 | 28 | 0.77 (0.53, 1.12) | 0.80 (0.55, 1.17) | 0.86 (0.59, 1.25) |
| P-trend | — | — | 0.49 | 0.83 | 0.45 |
| Butter, servings/d | |||||
| 0 | 11,382 | 5120 | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) |
| >0 to <0.5 | 4792 | 2161 | 0.98 (0.93, 1.03) | 1.00 (0.95, 1.06) | 0.99 (0.94, 1.04) |
| 0.5 to <1 | 486 | 231 | 1.05 (0.92, 1.20) | 1.07 (0.94, 1.22) | 1.06 (0.93, 1.21) |
| ≥1 | 1273 | 524 | 0.89 (0.81, 0.97) | 0.91 (0.83, 1.00) | 0.88 (0.81, 0.97) |
| P-trend | — | — | 0.04 | 0.16 | 0.04 |
HRs and 95% CIs were calculated with the use of Cox proportional hazards regression models. Multivariable adjusted HRs were adjusted for age, randomization treatment, smoking status, physical activity, postmenopausal status, postmenopausal hormone use, history of hypercholesterolemia, history of hypertension, multivitamin use, alcohol intake, energy intake, and fruit and vegetable intake.
Dietary and supplemental calcium and vitamin D and risk of becoming overweight or obese
Results for how dietary and supplemental calcium and vitamin D, which are nutrients in dairy products, were associated with risk of becoming overweight or obese are presented in Table 6. In age-adjusted analyses, the use of calcium supplements (≥1000 mg/d) compared with no use was associated with an HR of 0.88 (95% CI: 0.81, 0.95; P-trend < 0.0001). A similar association was observed in the multivariable-adjusted analyses. However, the addition of BMI to the model completely attenuated the association. In the multivariable-adjusted model, higher dietary vitamin D intake (≥330 IU/d) tended to be associated with higher risk of becoming overweight or obese (HR: 1.08, 95 CI: 1.00, 1.17; P-trend = 0.09), but the association was, once again, attenuated after additional adjustment for BMI.
TABLE 6.
HRs (95% CIs) of becoming overweight or obese according to baseline dietary and supplemental calcium and vitamin D (n = 18,438)1
| n | Cases, n | Age adjusted | Multivariable adjusted | Multivariable adjusted plus BMI | |
| Dietary calcium, mg/d | |||||
| Quintile 1: <478 | 3688 | 1655 | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) |
| Quintile 2: 478 to <630 | 3688 | 1668 | 1.02 (0.96, 1.10) | 1.06 (0.99, 1.14) | 1.06 (0.99, 1.14) |
| Quintile 3: 630 to <789 | 3689 | 1697 | 1.03 (0.96, 1.10) | 1.09 (1.01, 1.17) | 1.05 (0.98, 1.13) |
| Quintile 4: 789 to <1077 | 3686 | 1613 | 0.98 (0.91, 1.04) | 1.07 (0.99, 1.16) | 1.04 (0.96, 1.13) |
| Quintile 5: ≥1077 | 3687 | 1605 | 0.97 (0.91, 1.04) | 1.08 (0.99, 1.18) | 1.04 (0.95, 1.13) |
| P-trend | — | — | 0.16 | 0.20 | 0.75 |
| Supplemental calcium, mg/d | |||||
| <0.5 | 10,344 | 4816 | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) |
| 0.5 to <200 | 1531 | 712 | 1.01 (0.93, 1.09) | 0.99 (0.91, 1.07) | 1.01 (0.93, 1.10) |
| 200 to <500 | 1824 | 772 | 0.88 (0.82, 0.95) | 0.87 (0.80, 0.94) | 0.92 (0.85, 0.99) |
| 500 to <1000 | 2954 | 1209 | 0.86 (0.80, 0.91) | 0.86 (0.80, 0.91) | 0.94 (0.88, 1.00) |
| ≥1000 | 1785 | 729 | 0.88 (0.81, 0.95) | 0.87 (0.80, 0.94) | 0.97 (0.89, 1.05) |
| P-trend | — | — | <0.0001 | <0.0001 | 0.16 |
| Dietary vitamin D, IU/d | |||||
| Quintile 1: <123 | 3688 | 1643 | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) |
| Quintile 2: 123 to <179 | 3688 | 1674 | 1.04 (0.97, 1.11) | 1.06 (0.99, 1.14) | 1.03 (0.96, 1.10) |
| Quintile 3: 179 to <238 | 3687 | 1695 | 1.06 (0.99, 1.13) | 1.10 (1.03, 1.18) | 1.02 (0.95, 1.10) |
| Quintile 4: 238 to <330 | 3688 | 1652 | 1.03 (0.96, 1.10) | 1.10 (1.02, 1.18) | 1.04 (0.96, 1.12) |
| Quintile 5: ≥330 | 3687 | 1574 | 0.99 (0.92, 1.06) | 1.08 (1.00, 1.17) | 1.00 (0.93, 1.08) |
| P-trend | — | — | 0.49 | 0.09 | 0.94 |
| Supplemental vitamin D, IU/d | |||||
| <2 | 12,236 | 5473 | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) |
| 2 to <250 | 2111 | 953 | 0.98 (0.91, 1.05) | 0.97 (0.90, 1.05) | 0.97 (0.90, 1.05) |
| 250 to ≤400 | 3205 | 1429 | 1.01 (0.95, 1.07) | 0.99 (0.92, 1.07) | 1.03 (0.95, 1.11) |
| >400 | 886 | 383 | 0.98 (0.88, 1.08) | 0.97 (0.86, 1.08) | 0.96 (0.86, 1.08) |
| P-trend | — | — | 0.96 | 0.58 | 0.85 |
HRs and 95% CIs were calculated with the use of Cox proportional hazards regression models. Multivariable-adjusted values were adjusted for age, randomization treatment, smoking status, vigorous exercise, postmenopausal status, postmenopausal hormone use, history of hypercholesterolemia, history of hypertension, multivitamin use, alcohol intake, energy intake, and fruit and vegetable intake.
DISCUSSION
In this prospective cohort of middle-aged and older, initially normal-weight women, increased body weight over time was observed across all categories of total dairy intake; however, women with higher intake of dairy products had less weight gain, which seemed to be driven by high-fat dairy intake. When we investigated risk of becoming overweight or obese, an inverse association was observed for high-fat dairy intake but not for total dairy intake or low-fat dairy intake as well as for specific dairy products or dietary nutrients present in dairy products such as calcium or vitamin D.
Note that our results apply to women who were initially normal weight and not to those who were initially overweight or obese. Thus, different results may have been observed because baseline BMI may be associated with the amount and types of dairy products consumed as well as to baseline risk of becoming more overweight or obese. Initial body weight is an important consideration when examining the role of dietary exposures in weight change. However, in our analyses, there was little evidence for a confounding effect from baseline BMI when we examined total, low-fat, and high-fat dairy product intakes as well as intakes of individual dairy products except for skimmed milk and sherbet intakes. However, it will be important to consider other results in other populations on the basis of sex, initial weight status, and ethnicity (24).
There have been several randomized trials and other prospective cohort studies that have investigated whether dairy intake is associated with weight change or obesity, and they have reported inconsistent results (6–13, 25, 26). The heterogeneity according to baseline obesity status in the different study populations adds to the complexity of making an overall interpretation of the potential role of dairy intake in weight-gain prevention and risk of becoming overweight or obese. Moreover, a limited number of prospective studies have investigated dairy consumption both on weight change and risk of becoming overweight or obese and whether these associations depend on the initial body weight. A meta-analyses of 27 randomized trials with a total of 2101 participants suggested that increasing dairy consumption in the context of energy restriction may reduce body weight according to short-term trial (<1 y) but not to long-term trials (≥1 y) (6).
In our study, we observed modest reductions in weight gain and risk of becoming overweight or obese. However, we believe these results are clinically meaningful because they reflected average estimates in a large population followed for a long time. We observed that higher intakes of high-fat dairy products but not of low-fat dairy products were associated with less weight gain, which seemed to be driven by intakes of whole-fat milk and butter. This result may seem to be a contradictory finding because low-fat dairy products are typically recommended for energy restriction. However, our study population was restricted to women who were normal weight at baseline and may, for the most part, have not been likely to restrict their energy intakes (we did not collect such information). Also in the Coronary Artery Risk Development in Young Adults study, inverse associations with obesity were observed with higher intakes of high-fat dairy products (12), In the Nurse’s Health Study, when women who were obese at baseline were excluded, higher intakes of whole milk but not of low-fat milk were associated with less weight gain over 4-y periods, which is in line with our findings. However, higher butter intake was associated with a 4-y weight gain in the Nurse’s Health Study, the Nurse’s Health Study II, and the Health Professionals Follow-Up Study (7). In the Framingham Heart Study Offspring Cohort, higher total dairy and yogurt intakes were associated with less weight and waist circumference gains over a 9-y period (25). These results are consistent with our findings on total dairy intake but not on yogurt intake, whereby we observed increased risk of becoming overweight or obese with higher intake. Moreover, in a Spanish cohort of women and men who were normal weight at baseline, yogurt intake was associated with lower risk of becoming overweight or obese (26). In a cohort of French adults, intakes of total dairy products, milk, cheese, and yogurt were not associated with a 6-y weight change in women and men who were normal weight at baseline; however, in overweight adults, there was less weight gain in those who had higher intakes of total dairy products, milk, and yogurt (8). In Swedish women with a constant intake of ≥1 serving whole/sour milk, and cheese/d had lower risk of gaining ≥1 kg/y than were women with constant lower intake of these products during a 10-y follow-up (9). When baseline BMI was stratified for, the association for whole milk and sour milk was only apparent in women of normal weight, but because sour milk is not typically available on the US market, it is hard to compare these results with our observed findings.
Dairy products contain several components that may contribute to less weight gain and lower risk of becoming overweight or obese including proteins, vitamin D, calcium, and phosphorus (1, 2). Calcium has been suggested to play a key role in energy metabolism by forming insoluble soaps or binding bile acids (27). Moreover, calcium may play a key role in intracellular pathways both directly and indirectly through 1.25-dihydroxy vitamin D and calcitriols (28). However, dietary or supplemental calcium and vitamin D seemed not to be associated with risk of becoming overweight or obese in our analyses when baseline BMI was controlled for. The role of dietary and supplemental calcium and vitamin D has not been well studied in overweight and obesity prevention. Clinical trials have mostly focused on weight changes in women and men who were overweight or obese at baseline, whereas few studies have investigated long-term longitudinal weight changes (29, 30). Our results of no associations with dietary and supplemental calcium are in agreement with findings from the Health Professionals Follow-Up Study, which observed no associations for the 12-y weight change in 23,504 men (31). There has been some concern that dairy products may contribute to excessive intakes of SFAs and calories, thereby causing people to consume reduced-fat products. However, in our analyses, we observed that high-fat dairy products but not low-fat dairy products were inversely associated with weight gain and risk of becoming overweight or obese.
The current study had several strengths. The study was conducted in a large prospective cohort with a long follow-up. Women in the study provided high-quality, self-reported information for a wide-range of lifestyle, clinical, and dietary factors. Moreover, measures of body weight were updated at several time points during follow-up. However, the current study also had important potential limitations to consider. Self-reported body-weight may be associated with a nondifferential misclassification, which, in turn, could have biased our risk estimates most likely toward the null (32). However, the validity of self-reported weight has been estimated to be very high (15). Moreover, a measurement error may influence self-reported dairy product consumption. We could not exclude a potential effect of survival bias for the weight-change results because these analyses included women who survived the intervention period and agreed to participate in the observational follow-up period. Although we had detailed information on a wide range of potential confounders, residual confounding may have affected our results. We did not have information on whether women were restricting their calorie intakes, which may have influenced our results. Moreover, in this study, we investigated whether high dairy product intake was associated with a weight change and risk of becoming overweight or obese in women who were initially normal weight; thus, our observed findings are not generalizable to women who are overweight or obese. Finally, women in our study were predominantly Caucasian and were health professionals, and thus, these results may not be generalizable to other populations.
In conclusion, in this prospective study of middle-aged and older women with normal BMI at baseline, higher total dairy intake was associated with less weight gain. These findings seemed to be driven by high-fat dairy intake. Future studies, especially well-powered, longer-term randomized trials, are needed to better understand the role of dairy products in the prevention of weight gain and risk of becoming overweight or obese.
Acknowledgments
The authors’ responsibilities were as follows—SR, LW, I-ML, JEB, and HDS: conducted the research; SR and HDS: designed the research and wrote the manuscript; HDS: had primary responsibility for the final content of the manuscript; and all authors: analyzed the data and read and approved the final manuscript. None of the authors reported a conflict of interest related to the study.
REFERENCES
- 1.Rice BH, Quann EE, Miller GD. Meeting and exceeding dairy recommendations: effects of dairy consumption on nutrient intakes and risk of chronic disease. Nutr Rev 2013;71:209–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Weaver CM. How sound is the science behind the dietary recommendations for dairy? Am J Clin Nutr 2014;99(5 Suppl):1217S–22S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.US Department of Agriculture and US Department of Health and Human Services. Dietary Guidelines for Americans, 2010. 7th ed. Washington (DC): US Government Printing Office; 2010. [Google Scholar]
- 4.Ogden CLCM, Kit BK, Flegal KM. Prevalence of obesity in the United States, 2009–2010. NCHS data brief, no 82. Hyattsville (MD): National Center for Health Statistics; 2012. [Google Scholar]
- 5.Kumanyika SK, Obarzanek E, Stettler N, Bell R, Field AE, Fortmann SP, Franklin BA, Gillman MW, Lewis CE, Poston WC 2nd, et al. Population-based prevention of obesity: the need for comprehensive promotion of healthful eating, physical activity, and energy balance: a scientific statement from American Heart Association Council on Epidemiology and Prevention, Interdisciplinary Committee for Prevention (formerly the expert panel on population and prevention science). Circulation 2008;118:428–64. [DOI] [PubMed] [Google Scholar]
- 6.Chen M, Pan A, Malik VS, Hu FB. Effects of dairy intake on body weight and fat: a meta-analysis of randomized controlled trials. Am J Clin Nutr 2012;96:735–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mozaffarian D, Hao T, Rimm EB, Willett WC, Hu FB. Changes in diet and lifestyle and long-term weight gain in women and men. N Engl J Med 2011;364:2392–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vergnaud AC, Peneau S, Chat-Yung S, Kesse E, Czernichow S, Galan P, Hercberg S, Bertrais S. Dairy consumption and 6-y changes in body weight and waist circumference in middle-aged French adults. Am J Clin Nutr 2008;88:1248–55. [DOI] [PubMed] [Google Scholar]
- 9.Rosell M, Hakansson NN, Wolk A. Association between dairy food consumption and weight change over 9 y in 19,352 perimenopausal women. Am J Clin Nutr 2006;84:1481–8. [DOI] [PubMed] [Google Scholar]
- 10.Holmberg S, Thelin A. High dairy fat intake related to less central obesity: a male cohort study with 12 years’ follow-up. Scand J Prim Health Care 2013;31:89–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shahar DR, Schwarzfuchs D, Fraser D, Vardi H, Thiery J, Fiedler GM, Bluher M, Stumvoll M, Stampfer MJ, Shai I, et al. Dairy calcium intake, serum vitamin D, and successful weight loss. Am J Clin Nutr 2010;92:1017–22. [DOI] [PubMed] [Google Scholar]
- 12.Pereira MA, Jacobs DR Jr, Van Horn L, Slattery ML, Kartashov AI, Ludwig DS. Dairy consumption, obesity, and the insulin resistance syndrome in young adults: the CARDIA Study. JAMA 2002;287:2081–9. [DOI] [PubMed] [Google Scholar]
- 13.Drapeau V, Despres JP, Bouchard C, Allard L, Fournier G, Leblanc C, Tremblay A. Modifications in food-group consumption are related to long-term body-weight changes. Am J Clin Nutr 2004;80:29–37. [DOI] [PubMed] [Google Scholar]
- 14.Willett WC, Sampson L, Stampfer MJ, Rosner B, Bain C, Witschi J, Hennekens CH, Speizer FE. Reproducibility and validity of a semiquantitative food frequency questionnaire. Am J Epidemiol 1985;122:51–65. [DOI] [PubMed] [Google Scholar]
- 15.Rimm EB, Stampfer MJ, Colditz GA, Chute CG, Litin LB, Willett WC. Validity of self-reported waist and hip circumferences in men and women. Epidemiology 1990;1:466–73. [DOI] [PubMed] [Google Scholar]
- 16.Watt B, Merrill A. Composition of foods: raw, processed, prepared, 1963–1992: Agriculture Handbook no. 8. Washington (DC): U.S. Department of Agriculture, US government Printing Office; 1993. [Google Scholar]
- 17.Willett W, Stampfer MJ. Total energy intake: implications for epidemiologic analyses. Am J Epidemiol 1986;124:17–27. [DOI] [PubMed] [Google Scholar]
- 18.Salvini S, Hunter DJ, Sampson L, Stampfer MJ, Colditz GA, Rosner B, Willett WC. Food-based validation of a dietary questionnaire: the effects of week-to-week variation in food consumption. Int J Epidemiol 1989;18:858–67. [DOI] [PubMed] [Google Scholar]
- 19.Rimm EB, Giovannucci EL, Stampfer MJ, Colditz GA, Litin LB, Willett WC. Reproducibility and validity of an expanded self-administered semiquantitative food frequency questionnaire among male health professionals. Am J Epidemiol 1992;135:1114–26, discussion 27–36. [DOI] [PubMed] [Google Scholar]
- 20.Lee IM, Rexrode KM, Cook NR, Manson JE, Buring JE. Physical activity and coronary heart disease in women: is “no pain, no gain” passe? JAMA 2001;285:1447–54. [DOI] [PubMed] [Google Scholar]
- 21.Wolf AM, Hunter DJ, Colditz GA, Manson JE, Stampfer MJ, Corsano KA, Rosner B, Kriska A, Willett WC. Reproducibility and validity of a self-administered physical activity questionnaire. Int J Epidemiol 1994;23:991–9. [DOI] [PubMed] [Google Scholar]
- 22.Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: executive summary. Expert Panel on the Identification, Evaluation, and Treatment of Overweight in Adults. Am J Clin Nutr 1998;68:899–917. [DOI] [PubMed] [Google Scholar]
- 23.Cox D. Regression models and life-tables. J R Stat Soc Series B Stat Methodol 1972;34:187–220. [Google Scholar]
- 24.Glymour MM, Weuve J, Berkman LF, Kawachi I, Robins JM. When is baseline adjustment useful in analyses of change? An example with education and cognitive change. Am J Epidemiol 2005;162:267–78. [DOI] [PubMed] [Google Scholar]
- 25.Wang H, Troy LM, Rogers GT, Fox CS, McKeown NM, Meigs JB, Jacques PF. Longitudinal association between dairy consumption and changes of body weight and waist circumference: the Framingham Heart Study. Int J Obes (Lond) 2014;38:299–305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Martinez-Gonzalez MA, Sayon-Orea C, Ruiz-Canela M, de la Fuente C, Gea A, Bes-Rastrollo M. Yogurt consumption, weight change and risk of overweight/obesity: the SUN cohort study. Nutr Metab Cardiovasc Dis 2014;24:1189–96. [DOI] [PubMed] [Google Scholar]
- 27.Kratz M, Baars T, Guyenet S. The relationship between high-fat dairy consumption and obesity, cardiovascular, and metabolic disease. Eur J Nutr 2013;52:1–24. [DOI] [PubMed] [Google Scholar]
- 28.Mundy GR, Guise TA. Hormonal control of calcium homeostasis. Clin Chem 1999;45:1347–52. [PubMed] [Google Scholar]
- 29.Booth AO, Huggins CE, Wattanapenpaiboon N, Nowson CA. Effect of increasing dietary calcium through supplements and dairy food on body weight and body composition: a meta-analysis of randomised controlled trials. Br J Nutr 2015;114:1013–25. [DOI] [PubMed] [Google Scholar]
- 30.Soares MJ, Chan She Ping-Delfos W, Ghanbari MH. Calcium and vitamin D for obesity: a review of randomized controlled trials. Eur J Clin Nutr 2011;65:994–1004. [DOI] [PubMed] [Google Scholar]
- 31.Rajpathak SN, Rimm EB, Rosner B, Willett WC, Hu FB. Calcium and dairy intakes in relation to long-term weight gain in US men. Am J Clin Nutr 2006;83:559–66. [DOI] [PubMed] [Google Scholar]
- 32.Rothman KJ, Greenland S, Lash TL. Modern epidemiology. 3rd ed Philadelphia (PA): Lippincott Williams & Wilkins; 2008. [Google Scholar]