Abstract
Objectives
There are significant geographical differences in the prevalence and incidence of celiac disease that cannot be explained by HLA alone. More than 40 loci outside of the HLA region have been associated with celiac disease. We investigated the roles of these non-HLA genes in the development of tissue transglutaminase autoantibodies (tTGA) and celiac disease in a large international prospective cohort study.
Methods
A total of 424,788 newborns from the US and European general populations and first-degree relatives with type 1 diabetes were screened for specific HLA genotypes. Of these, 21,589 carried 1 of the 9 HLA genotypes associated with increased risk for type 1 diabetes and celiac disease; we followed 8676 of the children in a 15 y prospective follow-up study. Genotype analyses were performed on 6010 children using the Illumina ImmunoChip. Levels of tTGA were measured in serum samples using radio-ligand binding assays; diagnoses of celiac disease were made based on persistent detection of tTGA and biopsy analysis. Data were analyzed using Cox proportional hazards analyses.
Results
We found 54 single-nucleotide polymorphisms (SNPs) in 5 genes associated with celiac disease (TAGAP, IL18R1, RGS21, PLEK, and CCR9) in time to celiac disease analyses (10−4>P>5.8x10−6). The hazard ratios (HR) for the SNPs with the smallest P values in each region were 1.59, 1.45, 2.23, 2.64, and 1.40, respectively. Outside of regions previously associated with celiac disease, we identified 10 SNPs in 8 regions that could also be associated with the disease (P<10−4). A SNP near PKIA (rs117128341, P = 6.5x10−8, HR = 2.8) and a SNP near PFKFB3 (rs117139146, P<2.8x10−7, HR = 4.9) reached the genome-wide association threshold in subjects from Sweden. Analyses of time to detection of tTGA identified 29 SNPs in 2 regions previously associated with celiac disease (CTLA4, P = 1.3x10−6, HR = 0.76 and LPP, P = 2.8x10−5, HR = .80) and 6 SNPs in 5 regions not previously associated with celiac disease (P<10−4); non-HLA genes are therefore involved in development of tTGA.
Conclusions
In conclusion, using a genetic analysis of a large international cohort of children, we associated celiac disease development with 5 non-HLA regions previously associated with the disease and 8 regions not previously associated with celiac disease. We identified 5 regions associated with development of tTGA. Two loci associated with celiac disease progression reached a genome-wide association threshold in subjects from Sweden.
Introduction
Celiac disease is strongly associated with the human leukocyte antigen (HLA) DR3–DQ2.5 (i.e., DRB1*03-DQA1*05:01-DQB1*02:01) or DR4-DQ8 (DRB1*04-DQA1*03-DQB1*03:02) haplotypes on chromosome 6 [1]. Moreover, there is an HLA gene-dose effect on the disease risk as individuals carrying two copies of DR3-DQ2.5 are at a higher susceptibility for celiac disease than those with only one copy [2,3]. Although carrying either DR3–DQ2.5 or DR4–DQ8 is almost a necessity to develop celiac disease, these haplotypes are common in the general population and not all carriers develop clinical disease [4]. Since the first genome-wide case/control association study (GWAS) on celiac disease was published in 2007, a total of 40 non-HLA loci have been suggested as being associated with celiac disease[5–9]. A significant proportion of the genetic predisposition comes from the HLA region (odds ratio of >5) while non-HLA genes have modest effect sizes with an odds ratio between 1.12 and 1.36 for celiac disease [10]. The role of these non-HLA genes have not been assessed in those with early onset celiac disease, particularly using a prospective cohort.
Celiac disease is increasing in frequency, with significant intra- and inter-country differences in the prevalence and incidence of the disease[11]. Despite recent advances in celiac disease genetics, it remains elusive why some, but not all, individuals with the HLA risk genotypes develop celiac disease. Although the ingestion of gluten is required to trigger and maintain celiac disease, gluten exposure is nearly universal. Therefore, exposures to other environmental factors may also be important in the pathogenesis. Celiac disease is likely a multifactorial disorder where multiple genes and multiple environmental factors interact in a complex manner. Disease risk genes may act at various stages of autoimmunity progression, with some genes playing a role early in autoantibody development, and others playing a critical role in the later stages of celiac disease development. This stage-specific contribution of different genes to the celiac disease risk is an important concept, which cannot be investigated using the cross-sectional case/control study design employed in all previous studies. Furthermore, genetic factors responsible for the development of tissue transglutaminase autoantibodies (tTGA) and ethnic- or country-specific differences in a genetically predisposed population have not been reported previously.
The Environmental Determinants of Diabetes in the Young (TEDDY) is an international multicenter study that screened over 420,000 newborns from the general population in four different countries to identify children with high risk HLA genes for the development of type 1 diabetes (T1D) [12]. Recently, TEDDY demonstrated the impact of different HLA genotypes on the risk of celiac disease as well as tTGA development, and furthermore confirmed that the HLA-DR3-DQ2/DR3-DQ2 genotype confers the single highest genetic risk for the disease during early childhood[13]. We also found differences in risk of disease between the participating countries that could not be explained by HLA-DR-DQ, suggesting that the risk may be influenced by variations in the environment and/or involvement of genes outside the HLA-DR-DQ region. One such recent finding from the TEDDY study was the protective association of HLA-DRB1*0401 with celiac disease autoimmunity[14].
The present study genotyped 195,806 SNPs on ImmunoChip in 6,010 TEDDY children to identify potential genetic factors responsible for the development of early autoimmunity (tTGA development) and celiac disease as well as country-specific differences in genetic predisposition.
Results
A total of 703 subjects developed persistent tTGA and were considered “events” in the Cox proportional hazards models for persistent tTGA. Only 317 of these 703 persistently tTGA positive children received an intestinal biopsy and 262 of the 317 subjects were confirmed to have celiac disease at the time the procedure was performed. Eleven children with positive tTGA tests at the initial time point were biopsied before they could be confirmed as having persistent tTGA and eight of them also had biopsy-proven celiac disease. Eighteen other children who had persistent tTGA levels >100 units but did not have a biopsy were also considered to have celiac disease for purposes of the study. Therefore, 288 subjects were considered as “events” in the analysis of the time-to-celiac disease. There are known differences based upon the family history of celiac disease, HLA-DR-DQ genotype, gender, HLA-DPB1 and country of residence. These factors were adjusted in the Cox proportional hazard models.
Analysis of reported celiac disease SNPs
A total of 69 SNPs were previously reported to be associated with celiac disease based on the NHGRI GWAS Catalog[5,7,15–17], of which 48 were represented on the ImmunoChip (S4 Table). Risk Variants that have been reported but are not on the ImmunoChip are listed in S6 Table. In the time-to-celiac disease analysis, only one SNP (rs13015714/IL18R on 2q12.1, HR = 1.42, p = 1.38x10-4) attained significance after Bonferroni correction (p = 0.05/48 = 0.001). Several other SNPs were close to the significance threshold of 0.001 or had p-value <0.05: rs653178/SH2B3 (HR = 1.30; p = 0.002); rs1464510/LPP (HR = 1.28; p = 0.002); rs17035378/PLEK (HR = 0.75; p = 0.004); rs6806528/FRMD4B (HR = 1.44; p = 0.004); rs11221332/ETS1 (HR = 1.29; p = 0.006); rs2298428/YDJC (HR = 1.27; p = 0.012); rs2327832/TNFAIP3 (HR = 1.24; p = 0.025); rs802734/PTPRK (HR = 1.21; p = 0.034); rs13098911/CCR9 (HR = 1.29; p = 0.041); and rs10876993/CDK4 (HR = 0.84; p = 0.042).
For time-to-persistent tTGA analysis, we observed 10 SNPs with p<0.05: rs1464510/LPP (HR = 1.16; p = 0.004); rs2298428/YDJC (HR = 1.17; p = 0.011); rs864537/CD247 (HR = 0.87; p = 0.013); rs13015714/IL18R1 (HR = 1.15; p = 0.02); rs10936599/MYNN (HR = 1.15; p = 0.022); rs11203203/UBASH3A (HR = 1.13; p = 0.027); rs11712165/CD80 (HR = 1.12; p = 0.035); rs7574865/STAT4 (HR = 1.14; p = 0.036); rs2816316/RGS1 (HR = 0.859; p = 0.038); and rs802734/PTPRK (HR = 1.12; p = 0.046).
Analysis of previously reported celiac disease regions
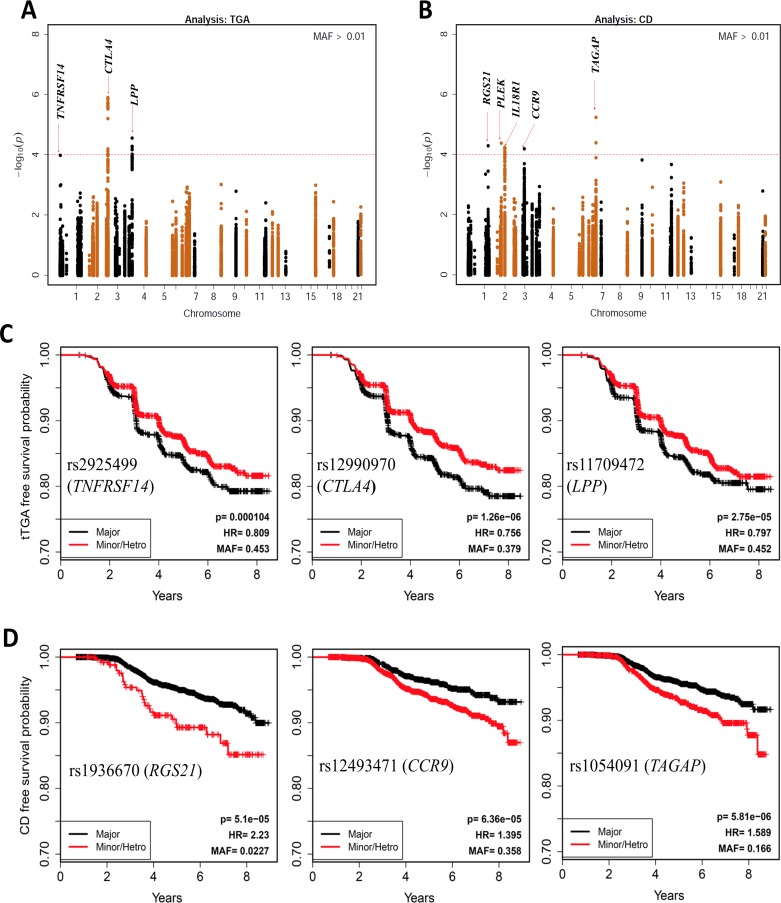
Next, we extended our analysis to all SNPs within 400 kb up- and downstream of the 48 reported SNPs. The–log10 p-values for all SNPs in these regions are plotted in Fig 1A for tTGA and Fig 1B for celiac disease. Since these are analyses for candidate regions, we considered p<10−4 as suggestive evidence for confirmation because multiple SNPs are tested in each region and the SNPs are in high linkage disequilibrium.
Fig 1. SNPs in the previously reported celiac disease associated regions.
Manhattan plot of P-values on the −log10 scale for SNPs (±400kb) previously associated with celiac disease (A) and persistent tissue transglutaminase autoantibody (tTGA) positivity (B). HRs and p-values are calculated using three possible genotypes and adjusted for family history of celiac disease, HLA-DR-DQ genotype, gender, HLA-DPB1, population stratification (ancestral heterogeneity) and country of residence (as strata). The red dashed line represents p = 1x10−4. Kaplan-Meier plots of the three most significant SNPs associated with celiac disease (C) and tTGA (D) are plotted by dividing the subjects in two groups: (i) Major homozygous (black curves) and (ii) Heterozygous combined with minor homozygous (red curves).
In the tTGA plots, the two regions with strongest evidence were CTLA4 and LPP (S1 Fig). The SNPs with smallest p-value in these two regions are: rs12990970/CTLA4 (HR = 0.76; p = 1.3x10-6) and rs11709472/LPP (HR = 0.80; P = 2.8x10-5) (Table 1). It is important to note that in our study, the presence of the minor allele of rs12990970/CTLA4 is protective (HR<1). In contrast, earlier studies have shown that CTLA4 (rs4675374-A) is a risk factor for celiac disease (OR = 1.14)[5,18]. The Kaplan-Meier plots for the three SNPs with smallest p-values in time-to-tTGA analysis (rs12990970/CTLA4; rs11709472/LPP; rs2925499/TNFRSF14) are shown in Fig 1C.
Table 1. Associations with celiac disease or tissue transglutaminase autoantibody (tTGA) positivity (p<10−4), mapped to previously known regions.
| SNPa | CHR | BP | MAF | HR CD | P-valueb CD | HR tTGA | P-valueb tTGA | # SNPS (P<10−4) | Nearby Gene |
|---|---|---|---|---|---|---|---|---|---|
| rs1936670 | 1 | 190598185 | 0.02 | 2.23 | 5.10x10-5 | 1.36 | 0.038 | 1 | RGS21 |
| rs4851575 | 2 | 102391635 | 0.24 | 1.45 | 5.69x10-5 | 1.16 | 0.014 | 49 | IL18R1, IL18RAP |
| rs114569351 | 2 | 68520426 | 0.02 | 2.64 | 4.19x10-5 | 1.73 | 0.002 | 1 | PLEK,FBXO48 |
| rs12493471 | 3 | 45926682 | 0.36 | 1.40 | 6.36x10-5 | 1.09 | 0.098 | 1 | CCR9,LZTFL1,CXCR6 |
| rs1054091 | 6 | 159389500 | 0.17 | 1.59 | 5.81x10-6 | 1.22 | 0.004 | 2 | RSPH3,TAGAP |
| rs12990970 | 2 | 204408934 | 0.38 | 0.82 | 0.027 | 0.76 | 1.26x10-6 | 21 | NPM1P33,CTLA4 |
| rs11709472 | 3 | 189560280 | 0.45 | 0.82 | 0.019 | 0.80 | 2.75x10-5 | 8 | LPP |
CHR: Chromosome; BP: Base Pair Position (NCBI 36.3); MAF: Minor Allele Frequency; HRCD: Hazard Ratio in celiac disease analysis; HRtTGA: Hazard Ratio in tTGA analysis. P-values < 10−4 are highlighted in bold
aThe data for the SNP with smallest p-value is presented from each region.
bHRs and p-value adjusted for family history of celiac disease, HLA-DR-DQ genotype, gender, HLA-DPB1, population stratification (ancestral heterogeneity) and country of residence (as strata).
In the celiac disease analysis, we found 5 regions (TAGAP, IL18R1, RGS21, PLEK, and CCR9) with SNPs that had p-values <10−4: rs1054091/TAGAP (HR = 1.59; p = 5.8x10-6); rs4851575/IL18R1 (HR = 1.45; p = 5.7x10-5); rs1936670/RGS21 (HR = 2.23; p = 5.1x10-5); rs114569351/PLEK (HR = 2.64; p = 4.2x10-5); and rs12493471/CCR9 (HR = 1.40; p = 6.4x10-5) (Table 1, S2 Fig). The Kaplan-Meier plots of three SNPs with smallest p-values in the time-to-celiac disease analysis (rs1936670/RGS21, rs12493471/CCR9, rs1054091/TAGAP) are shown in Fig 1D.
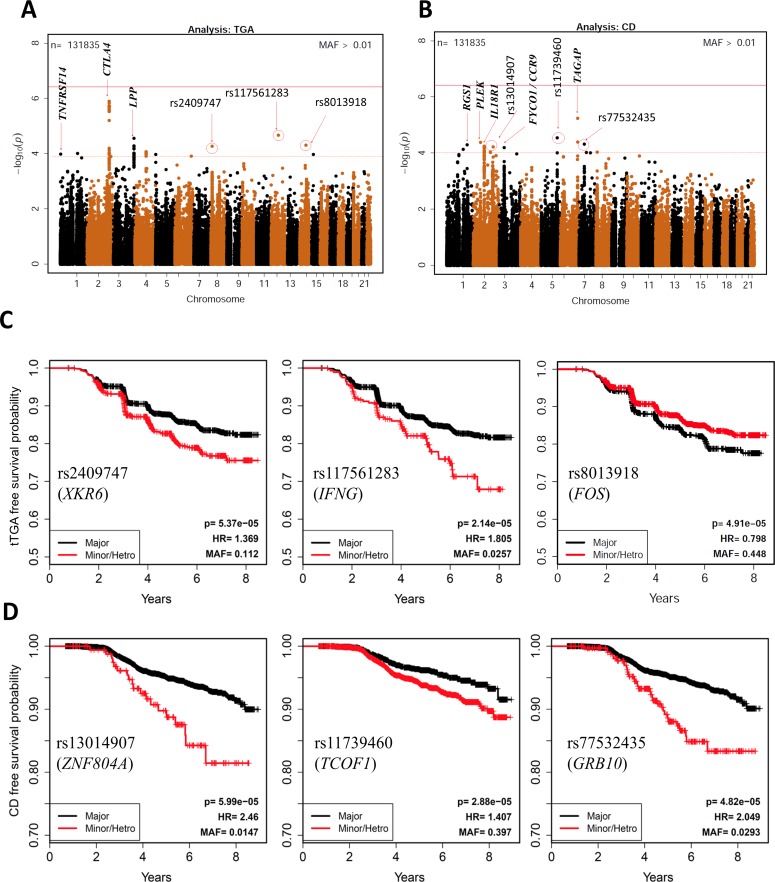
SNPs associated with progression to persistent tTGA outside of the known celiac disease regions
We then extended the analysis to include all SNPs genotyped on the ImmunoChip in search of novel SNP associations. For these analyses, 133,620 with minor allele frequencies of at least 0.01 were tested and therefore the statistical significance for any single SNP requires a Bonferroni-corrected p<3.7x10-7. In the time-to-persistent tTGA analyses, none of the SNPs reached this significance threshold, but 7 SNPs were identified in 5 novel celiac disease regions with p<10−4: rs117561283/IFNG (HR = 1.81; p = 2.1x10-5); rs8013918/FOS (HR = 0.80; p = 4.9x10-5); rs2409747/XKR6 (HR = 1.37; p = 5.4x10-5); rs114157400/BANK1 (HR = 1.62; p = 8.4x10-5); and rs72717025/FCGR2A (HR = 1.84; p = 9.6x10-5) (Fig 2A; Table 2). These SNPs are novel candidate SNPs with suggestive evidence and require further confirmation studies to rule out false positive discoveries. The Kaplan-Meier plots of three SNPs (rs2409747/XKR6, rs117561283/IFNG, and rs8013918/FOS discovered in time-to-tTGA analysis are shown in Fig 2C.
Fig 2. Associations with risk of celiac disease and risk of persistent tissue transglutaminase autoantibody (tTGA) positivity.
Manhattan plot of 133,620 SNPs with MAF>0.01, displaying the P-values on the −log10 scale for SNP associations with celiac disease (A) and persistent tTGA positivity (B). HRs and p-values are calculated using three possible genotypes and adjusted for family history of celiac disease, HLA-DR-DQ genotype, gender, HLA-DPB1, population stratification (ancestral heterogeneity) and country of residence (as strata). The red dashed line represents p = 1x10−4, the red solid line represents Bonferroni correction threshold. Kaplan-Meier plots of selected SNPs associated with celiac disease (C) and persistent tTGA (D) are plotted by dividing the subjects in two groups: (i) Major homozygous (black curves) and (ii) Heterozygous combined with minor homozygous (red curves).
Table 2. Novel associations with celiac disease or tissue transglutaminase autoantibody (tTGA) positivity (p<10−4).
| SNPa | CHR | BP | MAF | HR CD | P-valueb CD | HR tTGA | P-valueb tTGA | # SNPS (P<10−4) | Nearby Gene |
|---|---|---|---|---|---|---|---|---|---|
| rs72704176 | 1 | 153692482 | 0.02 | 2.26 | 7.42x10-5 | 1.31 | 0.085 | 1 | ASH1L |
| rs3771689 | 2 | 159930048 | 0.14 | 0.56 | 9.27x10-5 | 0.85 | 0.037 | 2 | BAZ2B |
| rs13014907 | 2 | 185781851 | 0.01 | 2.46 | 5.99x10-5 | 1.45 | 0.050 | 1 | ZNF804A |
| rs11739460 | 5 | 149685099 | 0.40 | 1.41 | 2.88x10-5 | 1.05 | 0.319 | 2 | TCOF1 |
| rs77532435 | 7 | 50641412 | 0.03 | 2.05 | 4.82x10-5 | 1.38 | 0.015 | 1 | GRB10 |
| rs6967298 | 7 | 69652445 | 0.19 | 0.61 | 9.42x10-5 | 0.90 | 0.137 | 1 | AUTS2 |
| rs61751041 | 7 | 107381421 | 0.02 | 2.23 | 9.76x10-5 | 1.61 | 0.002 | 1 | LAMB1 |
| rs72717025 | 1 | 159736883 | 0.02 | 1.41 | 0.207 | 1.84 | 9.61x10-5 | 1 | FCGR2A |
| rs114157400 | 4 | 103154484 | 0.04 | 1.71 | 0.003 | 1.62 | 8.43x10-5 | 2 | BANK1 |
| rs2409747 | 8 | 11115872 | 0.11 | 1.58 | 9.28x10-5 | 1.37 | 5.37x10-5 | 1 | XKR6 |
| rs117561283 | 12 | 66732860 | 0.03 | 1.96 | 0.002 | 1.81 | 2.14x10-5 | 1 | IFNG |
| rs8013918 | 14 | 74779319 | 0.45 | 0.85 | 0.066 | 0.80 | 4.91x10-5 | 1 | FOS |
CHR: Chromosome; BP: Base Pair Position (NCBI 36.3); MAF: Minor Allele Frequency; HRCD: Hazard Ratio in celiac disease analysis; HRtTGA: Hazard Ratio in tTGA analysis. P-values < 10−4 are highlighted in bold
aThe data for the SNP with smallest p-value is presented from each region.
bHRs and p-value adjusted for family history of celiac disease, HLA-DR-DQ genotype, gender, HLA-DPB1, population stratification (ancestral heterogeneity) and country of residence (as strata).
SNPs associated with progression to celiac disease outside of the known celiac disease regions
In a similar analysis using time-to-celiac disease with all SNPs, no SNP reached the Bonferroni-corrected p<3.7x10-7 significance threshold but 10 SNPs outside of the known celiac disease regions reached the suggestive threshold (p<10−4) (Fig 2B). These SNPs mapped to 8 different regions: rs11739460/TCOF1 (HR = 1.41; p = 2.9x10-5); rs77532435/GRB10 (HR = 2.05; p = 4.8x10-5); rs13014907/ZNF804A (HR = 2.46; p = 6.0x10-5); rs72704176/ASH1L (HR = 2.26; p = 7.4x10-5); rs3771689/BAZ2B (HR = 0.56; p = 9.3x10-5); rs2409747/XKR6 (HR = 1.58; p = 9.3x10-5); rs6967298/AUTS2 (HR = 0.61; p = 9.4x10-5); and rs61751041/LAMB1 (HR = 2.23; p = 9.8 x10-5) (Table 2). The Kaplan-Meier plots of three novel SNPs (rs13014907/ZNF804A, rs11739460/TCOF1, and rs77532435/GRB10 discovered in time-to-celiac disease analysis are shown in Fig 2D.
Country-specific genetic factors associated with progression to celiac disease
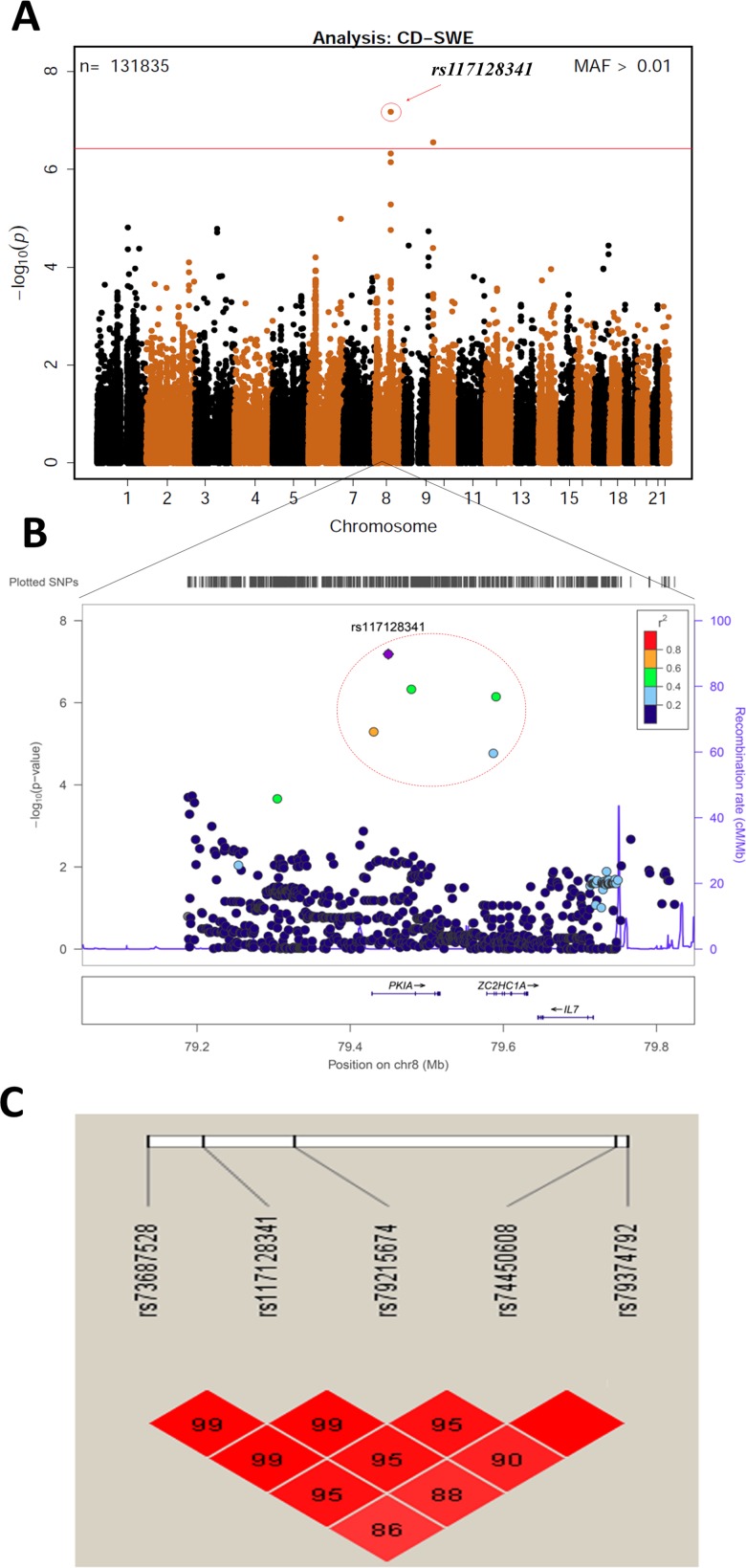
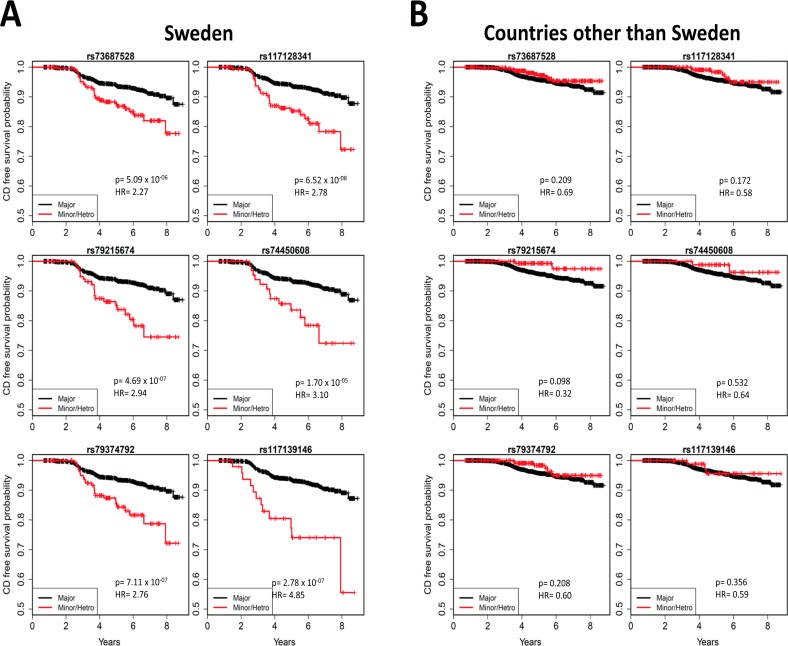
To explore country-specific genetic factors, the data with all 133,620 SNPs were analysed for each country. In the analysis of celiac disease risk among the Swedish participants, SNPs reached the Bonferroni-corrected p<3.7x10-7 significance threshold in two regions: 8q21.1 and 10p15 (Fig 3). The SNP with the smallest p-value in the 8q21.1 region was rs117128341 (p = 6.52x10-8, HR = 2.78, MAF = 0.04), a SNP in the intragenic region of the protein kinase inhibitor alpha (PKIA) gene. The other two nearby genes in this region are ZC2HC1A and IL7. The SNP with the smallest p-value in the chromosome 10p15 region was rs117139146 (p = 2.78x10-7, HR = 4.85, MAF = 0.014). A nearby gene in this region is PFKFB3, which was previously shown to be associated with celiac disease. Five SNPs with p<10−4 map to the PKIA region, and one SNP maps to the PFKFB3 region (Table 3). In the separate analyses of two other countries, the US and Finland, none of the six SNPs reached the significance threshold. The analysis in Germany was not conducted due to small sample size. Kaplan-Meier plots of these six SNPs for different countries (Fig 4) clearly indicated country-specific differences. The associations of these six SNPs with celiac disease in Sweden and the other three countries are listed in Table 3. There was no evidence of difference between US and Finland, therefore we combined US, Finland and Germany together to compare with Sweden in the analysis of interaction. A Cox proportional hazards model with an interaction term of the SNP with country was used to compare the effects of these six SNPs between Sweden and other countries, adjusting for country (Sweden vs other), gender, HLA-DPB1 genotype, HLA-DR-DQ genotype, family history of celiac disease, and population stratification. The analysis shows that the effect of any of these SNPs in Sweden is statistically different (p<0.05) from the effect in the other countries (rs73687528: p<0.001; rs117128341: p<0.001; rs79215674: p = 0.002; rs74450608: p = 0.029; rs79374792: p<0.001; rs117139146: p = 0.001).
Fig 3. Associations with risk of celiac disease in the Swedish population.
A: Manhattan plot of 133620 SNPs with MAF>0.01, displaying the P-values on the −log10 scale for the SNPs associated with celiac disease in the Swedish TEDDY population. B: Regional association plots at the PKIA locus generated by LocusZoom, showing the significance of association and the recombination rate. Colors represent HapMap CEU linkage disequilibrium r2 values with the most significantly associated SNP (rs117128341; shown in purple). C: Pairwise LD plot for five SNPs in the region of PKIA. The five most significant SNPs from this region are in high LD with each other.
Table 3. Six SNPs from two genomic regions significantly associated with celiac disease in Sweden.
Five SNPs mapped to PKIA region and one SNP mapped PFKFB3 region.
| Sweden | Other TEDDY countries than Swedenc | Sweden vs other TEDDY countriesc | ||||||
|---|---|---|---|---|---|---|---|---|
| SNP | CHR | BP | MAF | HRa | pa | HRa | pa | pb |
| rs73687528 | 8 | 79593304 | 0.064 | 2.27 | 5.09x10-6 | 0.69 | 0.209 | <0.001 |
| rs117128341 | 8 | 79612329 | 0.040 | 2.78 | 6.52x10-8 | 0.58 | 0.172 | <0.001 |
| rs79215674 | 8 | 79642439 | 0.027 | 2.94 | 4.69x10-7 | 0.32 | 0.098 | 0.002 |
| rs74450608 | 8 | 79749568 | 0.016 | 3.10 | 1.70x10-5 | 0.64 | 0.532 | 0.029 |
| rs79374792 | 8 | 79753034 | 0.040 | 2.76 | 7.11x10-7 | 0.60 | 0.208 | <0.001 |
| rs117139146 | 10 | 6240562 | 0.014 | 4.85 | 2.78x10-7 | 0.59 | 0.356 | 0.001 |
CHR: Chromosome; BP: Base Pair Position (NCBI 36.3); MAF: Minor Allele Frequency; HR: Hazard Ratio.
aHRs and p-value adjusted for family history of celiac disease, HLA-DR-DQ genotype, gender, HLA-DPB1 and population stratification (ancestral heterogeneity).
bP-value of testing the hypothesis that the effects of the SNP are the same between Sweden and other countries from a Cox model with adjustment for family history of celiac disease, HLA-DR-DQ genotype, gender, HLA-DPB1, population stratification (ancestral heterogeneity) and country of residence (Sweden vs. other).
cOther participating countries of TEDDY are Germany, Finland and the US.
Fig 4. Country-specific associations with risk of celiac disease.
Kaplan-Meier plots of five SNPs mapped to the PKIA region and one SNP mapped to the PFKFB3 region, in the Swedish TEDDY population (A) and in the other TEDDY countries (B). Kaplan-Meier plots clearly indicate country-specific differences. HRs and p-values are calculated using three possible genotypes and adjusted for family history of celiac disease, HLA-DR-DQ genotype, gender, HLA-DPB1 and population stratification (ancestral heterogeneity).
Country-specific associations with progression to tTGA
In time-to-persistent tTGA analysis among subjects from Sweden, none of the SNPs reached the Bonferroni-corrected p<3.7x10-7 significance threshold, however, 9 SNPs in 9 different genomic regions had p<10−4 (S5 Table). One such SNP was rs117139146 in the region of PFKFB3 (p = 7.34x10-5, HR = 2.79, MAF = 0.014).
Discussion
HLA-DR3-DQ2.5 and DR4-DQ8 are known as the most important genetic risk factors for celiac disease; however, these two haplotypes only account for part of the genetic risk. Recently, we demonstrated that HLA can be used to assess the risk of celiac disease using the large prospective TEDDY cohort [13]. This previous study clearly demonstrated an HLA gene dose effect of HLA-DR3-DQ2.5 on the risk of celiac disease autoimmunity was doubled among heterozygotes (HR = 2.09) but was a near 6-fold increased among homozygotes (HR = 5.70) as compared to children carrying the lowest-risk genotype DR4-DQ8 [13]. However, another finding of importance from this study was the difference in incidence of celiac disease between the participating countries which could not be attributed to HLA suggesting that environmental factors or other genes could contribute to the disease risk. In the current study, we used the same cohort to assess the association of non-HLA genes to the progression to tTGA in addition to progression to celiac disease in early childhood. A strength of this study includes the prospective nature of the study cohort that time-to-events analyses can be conducted, looking specifically in this case for genetic factors that could be related to the early development of celiac disease. Genetic studies have been traditionally done using cross-sectional case/control study design, with populations of individuals with celiac disease who have an unknown age of actual onset of autoimmunity. We know that the rate of seroconversion and subsequent development of celiac disease is high in childhood, and suspect that the yearly incidence slows down some time in adulthood. It is therefore possible that the genes involved in early onset celiac disease may be different from those involved in adult (or late) onset celiac disease. However, it may not be feasible to perform a prospective cohort study in at-risk adults due to the presumed decline in incidence.
In the first stage of analyses, we only considered the 48 SNPs previously reported to be associated with celiac disease and only one SNP was significant after Bonferroni correction. However, confirmatory evidence (p<10−4) was found for SNPs in five regions previously reported to be associated with celiac disease (TAGAP, IL18R1, RGS21, PLEK, and CCR9). The HRs estimated in this prospective cohort (HR = 1.40–2.64) are generally much higher than the odds ratios (OR) estimated in the case control studies (OR = 1.12–1.36). The TAGAP gene encodes a member of the Rho GTPase-activator protein superfamily involved in T cell activation and co-regulation with IL-2, which has been previously associated with several autoimmune diseases, including rheumatoid arthritis [19], celiac disease [20], and multiple sclerosis[21]. IL18R1 is part of the cytokine receptor cluster on chromosome 2q12 which encodes for the receptors of IL18; a cytokine involved in IFN-gamma synthesis and its mRNA expression is upregulated in active patients with celiac disease [22]. Both genes play roles in the immune response and are therefore rational candidates for conferring risk in an autoimmune disease such as celiac disease.
The development of tTGA usually appears before the clinical onset of celiac disease and often represents the earliest stage of autoimmunity, signifying a breakdown in tolerance. The specificity of tTGA is high such that negative testing will almost certainly rule out celiac disease. However the positive predictive value of the antibody especially in screened cohorts is lower, between 70–83%[23], and some may even be transient[24]. Nevertheless, individuals with only positive tTGA (even without evidence of villous atrophy) should not be disregarded. Positive tTGA is an independent predictor of reduced bone mineral density[25], growth[26] and mortality[27] and has been demonstrated to progress to celiac disease. In addition, many individuals with positive celiac disease serology but normal villous morphology have been shown to subsequently develop celiac disease in subsequent follow-up[28].
Although HLA genes are known to contribute to the development of tTGA, the contribution of non-HLA genes to the development tTGA and its role in early childhood celiac autoimmunity is still not well characterized. This study suggests that there are a number of non-HLA genes potentially implicated in the development of tTGA, and that there is overlap between genes involved in both tTGA and celiac disease development. For example, CTLA4 and LPP are implicated in both celiac disease and tTGA development, although the association with tTGA appears to be stronger than with celiac disease. On the other hand, association evidence for RGS21, IL18R1, PLEK, CCR9, TAGAP was only found for celiac disease (Table 1).
Our recent studies on HLA class II genes in the TEDDY cohort also demonstrated that the Swedish participants were at an increased risk for early celiac disease as compared to other participating countries in TEDDY when adjusted for previously known risk factors[13]. We hypothesized that this increased risk was due to variations in exposures to environmental factors. However, an alternative explanation is that there could be genetic differences outside of the HLA-DR-DQ genes between Sweden and other countries which, in part, may account for differences in disease incidences. The current study tested this hypothesis and found two regions (chromosomes 8q21.1 and 10p15) with Bonferroni-corrected significance evidence in the Swedish dataset, but not in the other three countries.
The chromosome 8q21.1 region is a novel genomic interval associated with celiac disease in Sweden and contains five SNPs with strong evidence (1.7x10-5>p>6.5x10-8). It is near the PKIA gene which encodes an extremely potent competitive inhibitor of cAMP-dependent protein kinase. It has been previously reported that intestinal PKIA gene expression was increased among patients with untreated celiac disease [29]. Another study suggests a potential role of cAMP-dependent protein kinase-A activation in the TNF-alpha production by gliadin-derived peptides in intestinal epithelial cells [30].
One SNP (rs117139146) located in the intragenic region of chromosome 10p15 encoding for PFKFB3 (6-phosphofructo-2-kinase/fructose-2,6-biphosphatase 3) was initially identified as being associated with celiac disease through the 1000 Genomes Project using the ImmunoChip in 2012 [8]. The 440kB region between PFKFB3 and Protein Kinase C Theta (PRKCQ) has been reported in a meta-analysis to identify rheumatoid arthritis (RA) risk loci in European populations [31], and also has been shown to be associated with T1D [32]. In a meta-analysis of Dutch and UK data sets, shared association with this PFKFB3/PRKCQ region was observed in both RA and celiac disease [33]. In a study of North Americans, this region was suggestive of an association with celiac disease, but did not reach significance[9].
Recently, two other studies have also shown region-specific associations observed in celiac disease. The prevalence of tTGA and celiac disease is lower in Russian Karelia than in Finland, which may be associated with a lower economic status and inferior hygienic environment.[34] Also, discrepancy of celiac disease autoimmunity between Swedish and Danish T1D cohorts suggests that regional variations in comorbidity of celiac disease in T1D is caused by difference in exposure to environmental factors. [35]. Country-specific associations have also been observed in other autoimmune diseases. For example, PADI4 was the first non-HLA genetic risk factor known to be associated with RA, in a Japanese population[36]. However, in Spanish, Swedish and UK populations, PADI4 polymorphisms were not associated with RA [37,38]. Gene-environment interactions probably are more important in diseases where the ingestion of a particular type of food is required to maintain or trigger the disease. Recently, it has been shown in Australia that infants of Asian-born parents are at increased risk of peanut allergy compared to infants with parents migrating from other countries, suggesting gene-environment interactions are important in food allergy [39].
It is worth noting that our inference is based on a subset of SNPs included in the Illumina ImmunoChip genotyping platform. Also, this analysis lacks power to confirm or discover genetic factors with small effect size due to the limited number of events and short follow-up time. None of the SNPs reached the Bonferroni-corrected significance threshold in the entire dataset, although two regions reached the significance level in the Sweden population that has a higher incidence rate of celiac disease. Analyses of the TEDDY cohort with longer follow-up and more events will likely provide more robust evidence for the newly suggested and previously identified genetic factors. However, current age of our cohort allows the analysis of factors involved in the earliest development of celiac autoimmunity and celiac disease, which may vary from celiac disease that develops in an older population. Our study also highlights the necessity of having another large prospective cohort like TEDDY to fully elucidate the genetic mechanism of celiac disease. It is also worth noting that the HRs presented in this analysis are based on a population of children enriched for the high-risk celiac HLAs, and the findings may not be generalizable to the general population. TEDDY is the largest and most intensive study focusing on the genetic and environmental factors as well as gene-environment interactions for diabetes and celiac disease [12]. The current study has not explored genetic factors in the context of environmental exposure data and we believe that future integrated analyses of gene-environment interactions will allow us to reveal the underlying molecular mechanism of the disease.
Material and Methods
Material
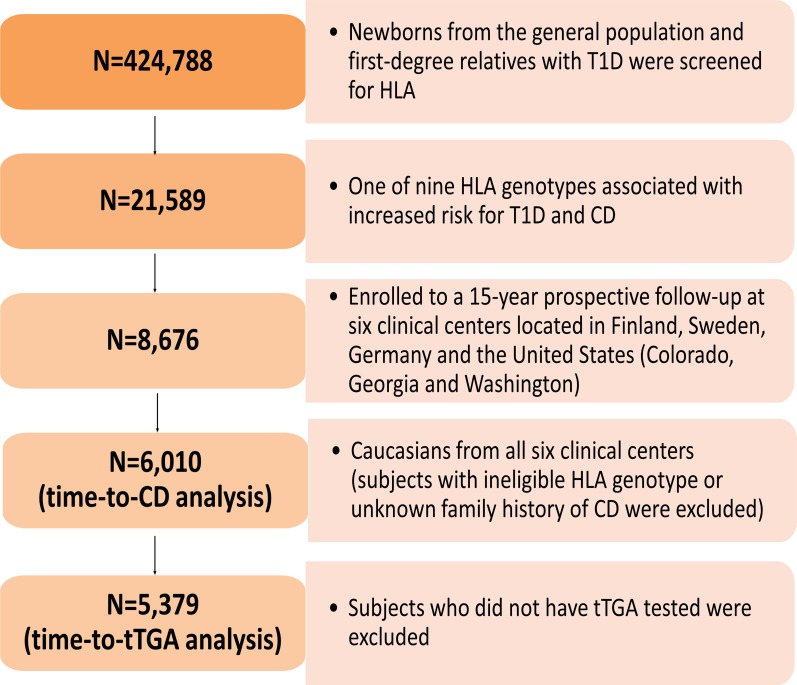
A total of 424,788 newborns from both the general population and first-degree relatives with T1D were screened for specific HLA genotypes. Of these, 21,589 had one of the nine HLA genotypes associated with increased risk for T1D and celiac disease (S1 Table) and 8,676 eligible children were enrolled to a 15-year prospective follow-up[40] (Fig 5).
Fig 5. Flow chart of study participants.
The Environmental Determinants of Diabetes in the Young (TEDDY) is an international multicenter study that screened over 420,000 newborns from the general population in four different countries. The present study genotyped 195,806 SNPs on ImmunoChip in 6,010 TEDDY children to identify potential genetic factors responsible for the development of CD and country-specific differences in genetic predisposition. As shown in flow chart, a total of 6,010 subjects were included in the analysis of time-to-CD, and 5379 subjects were included in the analysis of time-to-tTGA.
The Environmental Determinants of Diabetes in the Young (TEDDY) is a prospective cohort study with the primary goal to identify environmental causes of T1D. This study was performed according to the principles of the Declaration of Helsinki. Written informed consent was obtained for all study participants from a parent or legal guardian. The TEDDY study was approved by local Institutional Review Boards at 6 clinical research centers (3 in the United States and 3 in Europe): University of Colorado Health Science Center, Georgia Regents University, Pacific Northwest Diabetes Research Institute, Turku University Hospital (Finland), Institute of Diabetes Research (Germany), and Lund University (Sweden). The study is also monitored by an external evaluation committee formed by the National Institutes of Health.
Assessment of tissue transglutaminase autoantibodies (tTGA)
Sera were measured for tTGA using radioligand binding assays in two laboratories, IgA-tTGA assay at the Barbara Davis Center for Childhood Diabetes for the US samples and IgA-tTGA and IgG-tTGA assay at the University of Bristol for European samples. All positive US samples were also assayed by the Bristol lab. Levels of tTGA were expressed in arbitrary units derived from a standard curve and were considered to be positive if the value was ≥1.3 units. The inter-assay coefficient of variation was 22% at both 6 units and 20 units.
Study outcomes
Persistent tTGA was defined as having two consecutive positive tTGA tests (as measured by the Bristol laboratory) taken at least three months apart. Children meeting this criterion were referred to a pediatric gastroenterologist for a clinical evaluation for celiac disease. Celiac disease was defined as having an intestinal biopsy showing a Marsh score of 2 or greater by original Marsh criteria [41]. Children who had persistent tTGA with a mean level of >100 units in two consecutive samples but had no intestinal biopsy data, were also considered as having celiac disease for the purpose of this study [13].
Single-nucleotide polymorphism (SNP) analysis by ImmunoChip
SNPs were genotyped by the Center for Public Health Genomics at University of Virginia, using the Illumina ImmunoChip Infinium array. The ImmunoChip is a custom genotyping array of 195,806 SNPs selected from 186 regions associated with 12 autoimmune diseases. Genotype calling and quality control steps were applied to the dataset: (1) individuals with low call rate (<95%), or discordance with reported gender and prior genotyping were not considered in the analysis, (2) SNP markers with low call rates (<95%) were excluded, and (3) markers with allele distributions strongly deviating from Hardy-Weinberg equilibrium (HWE) in controls (p<10−6) were discarded (except for chromosome 6 due to HLA eligibility requirements). This resulted in a total of 7,023 subjects with genotype data on 176,586 SNPs.
Statistical analysis
The time-to-persistent tTGA and the time-to-celiac disease were the two primary outcomes analysed in this study. The time-to-persistent tTGA was defined as the age when the sample for the first tTGA positive test was collected, and the right-censored time was the age when the participant’s last blood sample was collected for testing of tTGA. The time-to-celiac disease was the child’s age at the time of biopsy for the diagnosis of celiac disease, or the age of the first high-level tTGA result (defined as ≥100 units). The right-censored time was the age of the last TEDDY clinic visit that was confirmed to be celiac disease-free. Cox proportional hazards modelling was used to analyse the effect of each individual SNP (by genotype 0,1,2) on the outcome, after adjusting for country (as strata), gender, HLA-DPB1 genotype, HLA-DR-DQ genotype (e.g., DR3-DQ2/DR3-DQ2, DR3-DQ2/X, DR4-DQ8/DR4-DQ8 and Other), family history (first-degree relative) of celiac disease, and principal components to account for population stratification (ancestral heterogeneity). The Cox models were fitted using the “survival” package in R [42]. The first four principal components were used in these analyses, calculated from the SNP data using the SNPRelate software [43]. As the majority of the subjects were Caucasians, and to reduce population stratification further, subjects from other races were excluded and analyses were restricted to the 6,258 Caucasians from all six clinical centers.
Subject exclusion included those who had either an ineligible HLA genotype or unknown family history (among first-degree relatives) of celiac disease. Further, subjects who did not have tTGA tested were also excluded in the analysis of time-to-persistent tTGA. As a result, 6,010 subjects were included in the analysis of time-to- celiac disease, and 5,379 subjects were included in the analysis of time-to- persistent tTGA (Fig 5). Among the 6,010 subjects included in the analysis of celiac disease, the median follow-up time was 5 years (interquartile range: 3.75–6.44 years). Whereas, among the 5,379 subjects included in the analysis of persistent tTGA, the median follow-up time was 5.18 years with an interquartile range of 4.04–6.54 years. During the follow-up, a total of 703 subjects developed persistent tTGA (US: 191 out of 1785; Finland: 167 out of 1414; Germany: 37 out of 328; Sweden: 308 out of 1852) and a total of 288 subjects were considered as having celiac disease (US: 83 out of 2028; Finland: 53 out of 1551; Germany: 9 out of 399; Sweden: 143 out of 2032). The characteristics of TEDDY participants in the analyses of persistent tTGA (S2 Table) and celiac disease (S3 Table) are provided in the Supplementary material.
From the 176,586 SNPs that passed quality control filters, the analysis focused on those 133,620 with minor allele frequencies of at least 0.01; thus, statistical significance for any single SNP required a Bonferoni-corrected p<3.7x10-7. This is a highly stringent threshold as a large number of SNPs are in linkage disequilibrium which should reduce the total number of independent tests. For the analyses of the 48 candidate SNPs that have been identified in previous studies, we considered p<10−3 as suggestive evidence for confirmation (p = 0.05/48 = 10−3). For the analyses of the 48 candidate regions, we considered p<10−4 as suggestive evidence for confirmation as multiple SNPs are tested in each region and the SNPs are in high linkage disequilibrium.
All analyses were performed using R 2.15.1. A web-based plotting tool locuszoom [44] was used to plot HapMap CEU linkage disequilibrium r2 values for additional SNPs in the candidate SNP regions.
Supporting Information
(PDF)
(PDF)
(PDF)
(PDF)
(PDF)
(PDF)
(PDF)
(PDF)
(PDF)
Acknowledgments
The Teddy Study Group
Lead author: Dr. Jin-Xiong She, Email: jshe@gru.edu, Phone: 706-721-3410, Fax: 706-721-3688
Colorado Clinical Center: Marian Rewers, M.D., Ph.D., PI1,4,5,6,10,11, Kimberly Bautista12, Judith Baxter9,10,12,15, Ruth Bedoy2, Daniel Felipe-Morales, Brigitte Frohnert, M.D., Patricia Gesualdo2,6,12,14,15, Michelle Hoffman12,13,14, Rachel Karban12, Edwin Liu, M.D.13, Jill Norris, Ph.D.2,3,12, Adela Samper-Imaz, Andrea Steck, M.D.3,14, Kathleen Waugh6,7,12,15, Hali Wright12. University of Colorado, Anschutz Medical Campus, Barbara Davis Center for Childhood Diabetes.
Georgia/Florida Clinical Center: Jin-Xiong She, Ph.D., PI1,3,4,11,†, Desmond Schatz, M.D.*4,5,7,8, Diane Hopkins12, Leigh Steed12,13,14,15, Jamie Thomas*6,12, Katherine Silvis2, Michael Haller, M.D.*14, Meena Shankar*2, Eleni Sheehan*, Melissa Gardiner, Richard McIndoe, Ph.D., Haitao Liu, M.D.†, John Nechtman†, Ashok Sharma, Joshua Williams, Gabriela Foghis, Stephen W. Anderson, M.D.^. Medical College of Georgia, Georgia Regents University. *University of Florida, †Jinfiniti Biosciences LLC, Augusta, GA, ^Pediatric Endocrine Associates, Atlanta, GA.
Germany Clinical Center: Anette G. Ziegler, M.D., PI1,3,4,11, Andreas Beyerlein Ph.D.2, Ezio Bonifacio Ph.D.* 5, Michael Hummel, M.D.13, Sandra Hummel, Ph.D.2, Kristina Foterek¥2, Mathilde Kersting, Ph.D.¥2, Annette Knopff7, Sibylle Koletzko, M.D.¶13, Claudia Peplow12, Roswith Roth, Ph.D.9, Joanna Stock9,12, Elisabeth Strauss12, Katharina Warncke, M.D.14, Christiane Winkler, Ph.D.2,12,15. Forschergruppe Diabetes e.V. and Institute of Diabetes Research, Helmholtz Zentrum München, and Klinikum rechts der Isar, Technische Universität München. *Center for Regenerative Therapies, TU Dresden, ¶Dr. von Hauner Children´s Hospital, Department of Gastroenterology, Ludwig Maximillians University Munich, ¥Research Institute for Child Nutrition, Dortmund.
Finland Clinical Center: Jorma Toppari, M.D., Ph.D., PI¥^1,4,11,14, Olli G. Simell, M.D., Ph.D., PI¥^1,4,11,13, Annika Adamsson, Ph.D.^12, Heikki Hyöty, M.D., Ph.D.*±6, Jorma Ilonen, M.D., Ph.D.¥ ¶3, Miia Kähönenμ¤, Mikael Knip, M.D., Ph.D.*±5, Annika Koivu¥^, Mirva Koreasalo*±§2, Kalle Kurppa, M.D., Ph.D.* ±13, Maria Lönnrot, M.D., Ph.D.* ±6, Elina Mäntymäki¥^, Katja Multasuoμ¤, Juha Mykkänen, Ph.D.^¥ 3, Tiina Niininen±* 12, Mia Nyblom*±, Petra Rajala^, Jenna Rautanen±§, Anne Riikonen* ±, Minna Romo¥^, Satu Simell, M.D., Ph.D.^±13, Tuula Simell, Ph.D., Ville Simell^¥13, Maija Sjöberg¥^12,14, Aino Steniusμ¤12, Eeva Varjonen¥^12, Riitta Veijola, M.D., Ph.D.μ¤14, Suvi M. Virtanen, M.D., Ph.D.*±§2, Mari Åkerlund*±§. ¥University of Turku, *University of Tampere, μUniversity of Oulu, ^Turku University Hospital, Hospital District of Southwest Finland, ±Tampere University Hospital, ¤Oulu University Hospital, §National Institute for Health and Welfare, Finland, ¶University of Kuopio.
Sweden Clinical Center: Åke Lernmark, Ph.D., PI1,3,4,5,6,8,10,11,15, Daniel Agardh, M.D., Ph.D.13, Carin Andrén Aronsson2,13, Maria Ask, Jenny Bremer, Ulla-Marie Carlsson, Corrado Cilio, Ph.D., M.D.5, Camilla Ekstrand, Emelie Ericson-Hallström2, Lina Fransson, Thomas Gard, Joanna Gerardsson, Rasmus Håkansson, Monica Hansen, Gertie Hansson12, Susanne Hyberg, Fredrik Johansen, Berglind Jonasdottir M.D., Linda Jonsson, Helena Elding Larsson M.D., Ph.D. 6,14, Barbro Lernmark, Ph.D., Maria Månsson-Martinez, Maria Markan, Theodosia Massadakis, Jessica Melin12, Zeliha Mestan, Kobra Rahmati, Anita Ramelius, Falastin Salami, Monica Sedig Järvirova, Sara Sibthorpe, Birgitta Sjöberg, Ulrica Swartling, Ph.D.9,12, Erika Trulsson, Carina Törn, Ph.D. 3,15, Anne Wallin, Åsa Wimar12,14, Sofie Åberg. Lund University.
Washington Clinical Center: William A. Hagopian, M.D., Ph.D., PI1,3,4, 5, 6,7,11,13, 14, Xiang Yan, M.D., Michael Killian6,7,12,13, Claire Cowen Crouch12,14,15, Jennifer Skidmore2, Stephen Ayres, Kayleen Dunson, Diana Heaney, Rachel Hervey, Corbin Johnson, Rachel Lyons, Arlene Meyer, Denise Mulenga, Emma Schulte, Elizabeth Scott, Joshua Stabbert, John Willis. Pacific Northwest Diabetes Research Institute.
Pennsylvania Satellite Center: Dorothy Becker, M.D., Margaret Franciscus, MaryEllen Dalmagro-Elias Smith2, Ashi Daftary, M.D., Mary Beth Klein, Chrystal Yates. Children’s Hospital of Pittsburgh of UPMC.
Data Coordinating Center: Jeffrey P. Krischer, Ph.D.,PI1,4,5,10,11, Michael Abbondondolo, Sarah Austin-Gonzalez, Rasheedah Brown12,15, Brant Burkhardt, Ph.D.5,6, Martha Butterworth2, David Cuthbertson, Christopher Eberhard, Steven Fiske9, Dena Garcia, Veena Gowda, David Hadley, Ph.D.3,13, Hye-Seung Lee, Ph.D.1,2,13,15, Shu Liu, Xiang Liu, Ph.D.2,9,12, Kristian Lynch, Ph.D. 5,6,9,15, Jamie Malloy, Cristina McCarthy12,15, Wendy McLeod2,5,6,13,15, Chris Shaffer, Laura Smith, Ph.D.9,12, Susan Smith12,15, Roy Tamura, Ph.D.1,2,13, Ulla Uusitalo, Ph.D.2,15, Kendra Vehik, Ph.D.4,5,6,14,15, Ponni Vijayakandipan, Keith Wood, Jimin Yang, Ph.D., R.D.2,15. University of South Florida.
Project scientist: Beena Akolkar, Ph.D.1,3,4,5,6,7,10,11. National Institutes of Diabetes and Digestive and Kidney Diseases.
Other contributors: Kasia Bourcier, Ph.D.5, National Institutes of Allergy and Infectious Diseases. Thomas Briese, Ph.D.6,15, Columbia University. Suzanne Bennett Johnson, Ph.D.9,12, Florida State University. Steve Oberste, Ph.D.6, Centers for Disease Control and Prevention. Eric Triplett, Ph.D.6, University of Florida.
Autoantibody Reference Laboratories: Liping Yu, M.D.^5, Dongmei Miao, M.D.^, Polly Bingley, M.D., FRCP* 5, Alistair Williams*, Kyla Chandler*, Saba Rokni*, Joanna Boldison*, Jacob Butterly*, Gabriella Carreno*, Claire Caygill*, Ivey Geoghan*, Anna Long*, Molly Payne*, James Pearson*, Sophie Ridewood*, Rebecca Wyatt*. ^Barbara Davis Center for Childhood Diabetes, University of Colorado Denver, *School of Clinical Sciences, University of Bristol UK.
Cortisol Laboratory: Elisabeth Aardal Eriksson, M.D., Ph.D., Ing-Marie Lundgren, Ewa Lönn Karlsson, Dzeneta Nezirevic Dernroth, Ph.D. Department of Clinical Chemistry, Linköping University Hospital, Linköping, Sweden
Dietary Biomarkers Laboratory: Iris Erlund, Ph.D.2, Irma Salminen, Jouko Sundvall, Jaana Leiviskä, Mari Lehtonen, Ph.D. National Institute for Health and Welfare, Helsinki, Finland.
HbA1c Laboratory: Randie R. Little, Ph.D., Alethea L. Tennill. Diabetes Diagnostic Laboratory, Dept. of Pathology, University of Missouri School of Medicine.
HLA Reference Laboratory: Henry Erlich, Ph.D.3, Steven J. Mack, Ph.D., Anna Lisa Fear. Center for Genetics, Children’s Hospital Oakland Research Institute.
Metabolomics Laboratory: Oliver Fiehn, Ph.D., Bill Wikoff, Ph.D., Brian Defelice, Dmitry Grapov, Ph.D., Tobias Kind, Ph.D., Mine Palazoglu, Luis Valdiviez, Benjamin Wancewicz, Gert Wohlgemuth, Joyce Wong. UC Davis Metabolomics Center.
Microbiome and Viral Metagenomics Laboratory: Joseph F. Petrosino, Ph.D.6. Alkek Center for Metagenomics and Microbiome Research, Department of Molecular Virology and Microbiology, Baylor College of Medicine.
OGTT Laboratory: Santica M. Marcovina, Ph.D., Sc.D., Vinod P. Gaur, Ph.D., Northwest Lipid Metabolism and Diabetes Research Laboratories, University of Washington.
Proteomics Laboratory: Richard D. Smith, Ph.D., Thomas O. Metz, Ph.D., Charles Ansong, Ph.D., Bobbie-Jo Webb-Robertson, Ph.D., and Hugh D. Mitchell, Ph.D. Pacific Northwest National Laboratory.
Repository: Heather Higgins, Sandra Ke. NIDDK Biosample Repository at Fisher BioServices.
RNA Laboratory and Gene Expression Laboratory: Jin-Xiong She, Ph.D., PI1,3,4,11, Richard McIndoe, Ph.D., Haitao Liu, M.D., John Nechtman, Yansheng Zhao, Na Jiang, M.D. Jinfiniti Biosciences, LLC.
SNP Laboratory: Stephen S. Rich, Ph.D.3, Wei-Min Chen, Ph.D.3, Suna OnengutGumuscu, Ph.D.3, Emily Farber, Rebecca Roche Pickin, Ph.D., Jordan Davis, Dan Gallo, Jessica Bonnie, Paul Campolieto. Center for Public Health Genomics, University of Virginia.
Committees: 1Ancillary Studies, 2Diet, 3Genetics, 4Human Subjects/Publicity/Publications, 5 Immune Markers, 6infectious Agents, 7Laboratory Implementation, 8Maternal Studies, 9Psychosocial, 10Quality Assurance, 11Steering, 12Study Coordinators, 13Celiac Disease, 14Clinical Implementation, 15Quality Assurance Subcommittee on Data Quality.
Abbreviations
- RA
rheumatoid arthritis
- SNP
Single-nucleotide polymorphism
- TEDDY
The Environmental Determinants of Diabetes in the Young
- tTGA
tissue transglutaminase autoantibodies
- T1D
type 1 diabetes
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
None of the authors listed has any financial or other conflicts to disclose relevant to this article. This study was funded by DK 63829, 63861, 63821, 63865, 63863, 63836, 63790 and UC4DK095300 and contract no. HHSN267200700014C from the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), National Institute of Allergy and Infectious Diseases (NIAID), National Institute of Child Health and Human Development (NICHD), National Institute of Environmental Health Sciences (NIEHS), Juvenile Diabetes Research Foundation (JDRF), and Centers for Disease Control and Prevention (CDC). The complete TEDDY Study Group is listed in the Supplementary material.
References
- 1.DeMarchi M, Borelli I, Olivetti E, Richiardi P, Wright P, Ansaldi N, et al. (1979) Two HLA-D and DR alleles are associated with coeliac disease. Tissue Antigens 14: 309–316. [DOI] [PubMed] [Google Scholar]
- 2.Ploski R, Ek J, Thorsby E, Sollid LM (1993) On the HLA-DQ(alpha 1*0501, beta 1*0201)-associated susceptibility in celiac disease: a possible gene dosage effect of DQB1*0201. Tissue Antigens 41: 173–177. [DOI] [PubMed] [Google Scholar]
- 3.Margaritte-Jeannin P, Babron MC, Bourgey M, Louka AS, Clot F, Percopo S, et al. (2004) HLA-DQ relative risks for coeliac disease in European populations: a study of the European Genetics Cluster on Coeliac Disease. Tissue Antigens 63: 562–567. [DOI] [PubMed] [Google Scholar]
- 4.Kaukinen K, Partanen J, Maki M, Collin P (2002) HLA-DQ typing in the diagnosis of celiac disease. Am J Gastroenterol 97: 695–699. [DOI] [PubMed] [Google Scholar]
- 5.Dubois PC, Trynka G, Franke L, Hunt KA, Romanos J, Curtotti A, et al. (2010) Multiple common variants for celiac disease influencing immune gene expression. Nat Genet 42: 295–302. 10.1038/ng.543 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.van Heel DA, Hunt K, Greco L, Wijmenga C (2005) Genetics in coeliac disease. Best Pract Res Clin Gastroenterol 19: 323–339. [DOI] [PubMed] [Google Scholar]
- 7.van Heel DA, Franke L, Hunt KA, Gwilliam R, Zhernakova A, Inouye M, et al. (2007) A genome-wide association study for celiac disease identifies risk variants in the region harboring IL2 and IL21. Nat Genet 39: 827–829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Trynka G, Hunt KA, Bockett NA, Romanos J, Mistry V, Szperl A, et al. (2011) Dense genotyping identifies and localizes multiple common and rare variant association signals in celiac disease. Nat Genet 43: 1193–1201. 10.1038/ng.998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Garner C, Ahn R, Ding YC, Steele L, Stoven S, Green PH, et al. (2014) Genome-Wide Association Study of Celiac Disease in North America Confirms FRMD4B as New Celiac Locus. PLoS One 9: e101428 10.1371/journal.pone.0101428 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kumar V, Wijmenga C, Withoff S (2012) From genome-wide association studies to disease mechanisms: celiac disease as a model for autoimmune diseases. Semin Immunopathol 34: 567–580. 10.1007/s00281-012-0312-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kang JY, Kang AH, Green A, Gwee KA, Ho KY (2013) Systematic review: worldwide variation in the frequency of coeliac disease and changes over time. Aliment Pharmacol Ther 38: 226–245. 10.1111/apt.12373 [DOI] [PubMed] [Google Scholar]
- 12.(2007) The Environmental Determinants of Diabetes in the Young (TEDDY) study: study design. Pediatr Diabetes 8: 286–298. [DOI] [PubMed] [Google Scholar]
- 13.Liu E, Lee HS, Aronsson CA, Hagopian WA, Koletzko S, Rewers MJ, et al. (2014) Risk of pediatric celiac disease according to HLA haplotype and country. N Engl J Med 371: 42–49. 10.1056/NEJMoa1313977 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hadley D, Hagopian W, Liu E, She JX, Simell O, Beena Akolkar A-GZ, Marian Rewers, Krischer Jeffrey P., Wei-Min Chen, Suna Onengut-Gumuscu, Teodorica L., et al. (2015) HLA-DPB1*04:01 protects genetically susceptible children from celiac disease autoimmunity in the TEDDY study. American Journal of Gastroenterology. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Welter D, MacArthur J, Morales J, Burdett T, Hall P, Junkins H, et al. (2014) The NHGRI GWAS Catalog, a curated resource of SNP-trait associations. Nucleic Acids Res 42: D1001–1006. 10.1093/nar/gkt1229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ostensson M, Monten C, Bacelis J, Gudjonsdottir AH, Adamovic S, Ek J, et al. (2013) A possible mechanism behind autoimmune disorders discovered by genome-wide linkage and association analysis in celiac disease. PLoS One 8: e70174 10.1371/journal.pone.0070174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hunt KA, Zhernakova A, Turner G, Heap GA, Franke L, Bruinenberg M, et al. (2008) Newly identified genetic risk variants for celiac disease related to the immune response. Nat Genet 40: 395–402. 10.1038/ng.102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Holopainen P, Arvas M, Sistonen P, Mustalahti K, Collin P, Maki M, et al. (1999) CD28/CTLA4 gene region on chromosome 2q33 confers genetic susceptibility to celiac disease. A linkage and family-based association study. Tissue Antigens 53: 470–475. [DOI] [PubMed] [Google Scholar]
- 19.Chen R, Stahl EA, Kurreeman FA, Gregersen PK, Siminovitch KA, Worthington J, et al. (2011) Fine mapping the TAGAP risk locus in rheumatoid arthritis. Genes Immun 12: 314–318. 10.1038/gene.2011.8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Smyth DJ, Plagnol V, Walker NM, Cooper JD, Downes K, Yang JH, et al. (2008) Shared and distinct genetic variants in type 1 diabetes and celiac disease. N Engl J Med 359: 2767–2777. 10.1056/NEJMoa0807917 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Patsopoulos NA, Esposito F, Reischl J, Lehr S, Bauer D, Heubach J, et al. (2011) Genome-wide meta-analysis identifies novel multiple sclerosis susceptibility loci. Ann Neurol 70: 897–912. 10.1002/ana.22609 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Salvati VM, MacDonald TT, Bajaj-Elliott M, Borrelli M, Staiano A, Auricchio S, et al. (2002) Interleukin 18 and associated markers of T helper cell type 1 activity in coeliac disease. Gut 50: 186–190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hoffenberg EJ, Bao F, Eisenbarth GS, Uhlhorn C, Haas JE, Sokol RJ, et al. (2000) Transglutaminase antibodies in children with a genetic risk for celiac disease. J Pediatr 137: 356–360. [DOI] [PubMed] [Google Scholar]
- 24.Auricchio R, Tosco A, Piccolo E, Galatola M, Izzo V, Maglio M, et al. (2014) Potential celiac children: 9-year follow-up on a gluten-containing diet. Am J Gastroenterol 109: 913–921. 10.1038/ajg.2014.77 [DOI] [PubMed] [Google Scholar]
- 25.Simmons JH, Klingensmith GJ, McFann K, Rewers M, Ide LM, Taki I, et al. (2011) Celiac autoimmunity in children with type 1 diabetes: a two-year follow-up. J Pediatr 158: 276–281 e271. 10.1016/j.jpeds.2010.07.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jansen MA, Kiefte-de Jong JC, Gaillard R, Escher JC, Hofman A, Jaddoe VW, et al. (2015) Growth trajectories and bone mineral density in anti-tissue transglutaminase antibody-positive children: the Generation R Study. Clin Gastroenterol Hepatol 13: 913–920 e915. 10.1016/j.cgh.2014.09.032 [DOI] [PubMed] [Google Scholar]
- 27.Metzger MH, Heier M, Maki M, Bravi E, Schneider A, Lowel H, et al. (2006) Mortality excess in individuals with elevated IgA anti-transglutaminase antibodies: the KORA/MONICA Augsburg cohort study 1989–1998. Eur J Epidemiol 21: 359–365. [DOI] [PubMed] [Google Scholar]
- 28.Kurppa K, Ashorn M, Iltanen S, Koskinen LL, Saavalainen P, Koskinen O, et al. (2010) Celiac disease without villous atrophy in children: a prospective study. J Pediatr 157: 373–380, 380 e371. 10.1016/j.jpeds.2010.02.070 [DOI] [PubMed] [Google Scholar]
- 29.Juuti-Uusitalo K, Maki M, Kainulainen H, Isola J, Kaukinen K (2007) Gluten affects epithelial differentiation-associated genes in small intestinal mucosa of coeliac patients. Clin Exp Immunol 150: 294–305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Laparra Llopis JM, Sanz Herranz Y (2010) Gliadins induce TNFalpha production through cAMP-dependent protein kinase A activation in intestinal cells (Caco-2). J Physiol Biochem 66: 153–159. 10.1007/s13105-010-0020-z [DOI] [PubMed] [Google Scholar]
- 31.Raychaudhuri S, Remmers EF, Lee AT, Hackett R, Guiducci C, Burtt NP, et al. (2008) Common variants at CD40 and other loci confer risk of rheumatoid arthritis. Nat Genet 40: 1216–1223. 10.1038/ng.233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cooper JD, Smyth DJ, Smiles AM, Plagnol V, Walker NM, Allen JE, et al. (2008) Meta-analysis of genome-wide association study data identifies additional type 1 diabetes risk loci. Nat Genet 40: 1399–1401. 10.1038/ng.249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Coenen MJ, Trynka G, Heskamp S, Franke B, van Diemen CC, Smolonska J, et al. (2009) Common and different genetic background for rheumatoid arthritis and coeliac disease. Hum Mol Genet 18: 4195–4203. 10.1093/hmg/ddp365 [DOI] [PubMed] [Google Scholar]
- 34.Kondrashova A, Mustalahti K, Kaukinen K, Viskari H, Volodicheva V, Haapala AM, et al. (2008) Lower economic status and inferior hygienic environment may protect against celiac disease. Ann Med 40: 223–231. 10.1080/07853890701678689 [DOI] [PubMed] [Google Scholar]
- 35.Adlercreutz EH, Svensson J, Hansen D, Buschard K, Lernmark A, Mortensen HB, et al. (2015) Prevalence of celiac disease autoimmunity in children with type 1 diabetes: regional variations across the Oresund strait between Denmark and southernmost Sweden. Pediatr Diabetes 16: 504–509. 10.1111/pedi.12200 [DOI] [PubMed] [Google Scholar]
- 36.Suzuki A, Yamada R, Chang X, Tokuhiro S, Sawada T, Suzuki M, et al. (2003) Functional haplotypes of PADI4, encoding citrullinating enzyme peptidylarginine deiminase 4, are associated with rheumatoid arthritis. Nat Genet 34: 395–402. [DOI] [PubMed] [Google Scholar]
- 37.Caponi L, Petit-Teixeira E, Sebbag M, Bongiorni F, Moscato S, Pratesi F, et al. (2005) A family based study shows no association between rheumatoid arthritis and the PADI4 gene in a white French population. Ann Rheum Dis 64: 587–593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Martinez A, Valdivia A, Pascual-Salcedo D, Lamas JR, Fernandez-Arquero M, Balsa A, et al. (2005) PADI4 polymorphisms are not associated with rheumatoid arthritis in the Spanish population. Rheumatology (Oxford) 44: 1263–1266. [DOI] [PubMed] [Google Scholar]
- 39.Koplin JJ, Peters RL, Ponsonby AL, Gurrin LC, Hill D, Tang ML, et al. (2014) Increased risk of peanut allergy in infants of Asian-born parents compared to those of Australian-born parents. Allergy. [DOI] [PubMed] [Google Scholar]
- 40.Hagopian WA, Erlich H, Lernmark A, Rewers M, Ziegler AG, Simell O, et al. (2011) The Environmental Determinants of Diabetes in the Young (TEDDY): genetic criteria and international diabetes risk screening of 421 000 infants. Pediatr Diabetes 12: 733–743. 10.1111/j.1399-5448.2011.00774.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Oberhuber G (2000) Histopathology of celiac disease. Biomed Pharmacother 54: 368–372. [DOI] [PubMed] [Google Scholar]
- 42.Therneau T, (2015) A Package for Survival Analysis in S.
- 43.Zheng X, Levine D, Shen J, Gogarten SM, Laurie C, Weir BS (2012) A high-performance computing toolset for relatedness and principal component analysis of SNP data. Bioinformatics 28: 3326–3328. 10.1093/bioinformatics/bts606 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Pruim RJ, Welch RP, Sanna S, Teslovich TM, Chines PS, Gliedt TP, et al. (2010) LocusZoom: regional visualization of genome-wide association scan results. Bioinformatics 26: 2336–2337. 10.1093/bioinformatics/btq419 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF)
(PDF)
(PDF)
(PDF)
(PDF)
(PDF)
(PDF)
(PDF)
(PDF)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.