The Global Polio Eradication Initiative is close to achieving its goal. Oral polio vaccines (OPVs) rarely cause vaccine-associated paralytic polio (VAPP) or circulating vaccine-derived poliovirus outbreaks. To diminish these risks, inactivated polio vaccine (IPV) was reintroduced in most industrialized countries in the 1990s. Another vaccine, acellular pertussis (aP), was also incorporated to circumvent the reactogenicity of whole-cell pertussis (wP); the latter is currently used in most developing countries (DCs). However, recent outbreaks of pertussis in countries using aP attributed to waning immunity but seen less with wP mean that most DCs will likely retain wP as the preferred vaccine. How parents regard these changes in DCs is unknown. We investigated parental preferences for polio and pertussis vaccines in Guatemala among different geographical populations.
METHODS
A cross-sectional survey of a nonrandom convenience sample of consenting parents of children two to 18 months of age in June and July 2010 was performed at three well-child clinics: an urban private clinic of high-income strata; a low-income public clinic in Guatemala City; and the rural public clinic in San Juan Sacatepéquez, serving Mayan-Indian communities. The sample size had 80% power to detect a 20% difference between groups. The University Francisco Marroquin Ethics Committee approved the present investigator-funded study. A standardized questionnaire assessing demographics, knowledge, and perceived burden and efficacy of vaccines against polio and pertussis was administered face-to-face in Spanish, the local language. A paragraph containing information about the pros and cons of polio and pertussis vaccines was read to parents as described by Thoms et al (1). The end point was parental preference for each vaccine choice (OPV versus IPV, and DTwP versus DTaP).
Statistical analysis was performed using Stata 11 (Stata Corporation, USA), and included descriptive and inferential statistics using χ2 test and Fischer’s exact test. Multiple logistic regression was performed for factors affecting parental vaccine preferences.
RESULTS
Overall, 270 parents participated in the survey: 90 (33.3%) from each clinic. The majority (89.6%) were women, with a mean age of 30.5 years (range 16 to 46 years). Parents from the rural clinics were younger than those from the urban clinics (28.1 years versus 31.7 years; P<0.001). Most parents (n=175 [64.8%]) reported an income <USD$200 per month, and 69 (76.7%) from the rural clinic compared with eight (4.4%) from the two urban clinics reported not having any education (P<0.001).
Almost all parents (n=266 [98.9%]) believed that vaccines save lives and prevent diseases, and that they are beneficial despite being painful (n=245 [90.7%]). Most (83.3%) parents considered polio to be a deadly disease; however, 110 (40.7%) believed that poliomyelitis remained present in Guatemala. More parents from urban clinics (n=123 [78.3%]) chose IPV compared with those from rural clinics (n=34 [21.7%]) (P<0.001). Parents at the urban clinics (n=168 [93.3%]) preferred IPV because it was safer, while those from rural clinics (n=41 [75.9%]) preferred OPV because it meant fewer injections. More urban parents preferred DTaP compared with rural (n=142 [78.9%] versus n=30 [33.3%], respectively; P<0.001). In the multiple regression model, only the urban clinic location proved determinant of either IPV or DTaP choice (P=0.001). Neither income nor education showed a significant correlation with the parental preference of vaccines.
DISCUSSION
Our results indicate that parents in a low-income country, such as Guatemala, especially from urban areas, would favour the introduction of IPV, even when this implies additional injections. However, those from rural areas, the less educated and the poorer, voiced less acceptance and more concerns about injection pain. One-half of the countries in the world now include IPV, and 74 (38%) plan to introduce it by the end of 2015 after the World Health Assembly recommended the phased withdrawal of OPV starting in 2016. One major obstacle to this could be the additional injections required if IPV is used as a single vaccine. Previous studies conducted in industrialized countries have demonstrated that parents of children were willing to accept additional injections if the vaccines are safer (eg, IPV because it eliminated the low risk for-VAPP) (1,2). While there is strong support for children’s vaccines from parents in DCs, our study showed that added injections may be problematic for some, even if it means a safer vaccine. Hence, parental beliefs and choices need to be considered and addressed when introducing new vaccines. The 2015 WHO strategies for pain mitigation at the time of immunization may help with acceptance of additional injections (3).
Some limitations of our study include not exploring the choice of sequential IPV-OPV schedules and not discriminating responses of parents of children who had received previous doses of vaccines.
Figure 1).
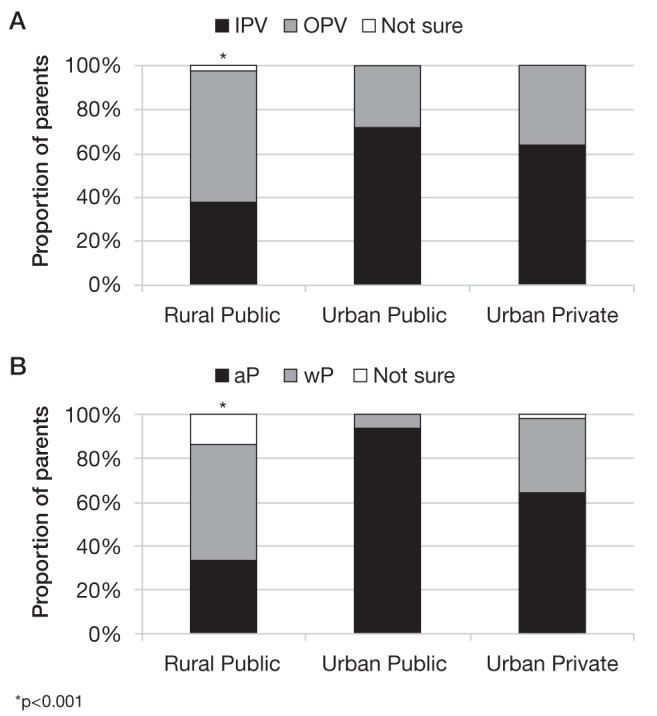
Parent’s preferences for different (A) polio and (B) pertussis vaccines according to clinic location in Guatemala, 2010. aP Acellular pertussis; IPV Inactivated polio vaccine; OPV Oral polio vaccine; wP Whole-cell pertussis
REFERENCES
- 1.Thoms ML, Bodnar PZ, O’Donovan JC, Gouel EG, Walcher JR, Halsey NA. Parental knowledge and choice regarding live and inactivated poliovirus vaccines. Arch Pediatr Adolesc Med. 1997;151:809–12. doi: 10.1001/archpedi.1997.02170450059009. [DOI] [PubMed] [Google Scholar]
- 2.Epee-Bounya A, Gitterman BA, Moon RY. Parental opinions regarding poliomyelitis immunizations. Clin Pediatr (Phila) 2001;40:435–40. doi: 10.1177/000992280104000802. [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization Reducing pain at the time of immunization of vaccination: WHO position paper – September 25, 2015. WER. 2015;90:505–10. [PubMed] [Google Scholar]


