Abstract
Doravirine (DOR), which is currently in a phase 3 clinical trial, is a novel human immunodeficiency type 1 virus (HIV-1) nonnucleoside reverse transcriptase inhibitor (NNRTI). DOR exhibits potent antiviral activity against wild-type virus and K103N, Y181C, and K103N/Y181C mutant viruses, with 50% inhibitory concentrations (IC50s) of 12, 21, 31, and 33 nM, respectively, when measured in 100% normal human serum (NHS). To assess the potential for DOR to suppress NNRTI-associated and rilpivirine (RPV)-specific mutants at concentrations achieved in the clinic setting, inhibitory quotients (IQs) were calculated by determining the ratio of the clinical trough concentration over the antiviral IC50 for each virus with DOR and RPV and efavirenz (EFV). DOR displayed IQs of 39, 27, and 25 against the K103N, Y181C, and K103N/Y181C mutants, respectively. In contrast, RPV exhibited IQs of 4.6, 1.4, and 0.8, and EFV showed IQs of 2.5, 60, and 1.9 against these viruses, respectively. DOR also displayed higher IQs than those of RPV and EFV against other prevalent NNRTI-associated mutants, with the exception of Y188L. Both DOR and EFV exhibited higher IQs than RPV when analyzed with RPV-associated mutants. Resistance selections were conducted with K103N, Y181C, G190A, and K103N/Y181C mutants at clinically relevant concentrations of DOR, RPV, and EFV. No viral breakthrough was observed with DOR, whereas breakthrough viruses were readily detected with RPV and EFV against Y181C and K103N viruses, respectively. These data suggest that DOR should impose a higher barrier to the development of resistance than RPV and EFV at the concentrations achieved in the clinic setting.
INTRODUCTION
The introduction of highly active antiretroviral therapy (HAART) in 1996 has significantly reduced the morbidity and mortality associated with HIV-1 infection (1, 2). However, the clinical and immunologic benefits of antiretroviral therapy can be compromised by the emergence of drug-resistant viruses due to suboptimal treatment or adherence.
Drug-resistant mutants can be transmitted to an uninfected individual. Transmitted drug-resistant (TDR) mutants limit the choice of first-line combination antiretroviral therapy, decrease the efficacy of subsequent antiretroviral regimens, and increase the risk of treatment failure (3–5). TDR mutants have been documented among treatment-naive patients, with prevalences ranging from 3% to 24%, depending on the cohort and geographic characteristics (6). Importantly, transmitted nonnucleoside reverse transcriptase inhibitor (NNRTI)-resistant mutants are of particular concern, as they have the ability to persist for years after initial infection, suggesting the low impact of NNRTI-resistant mutations on viral fitness (7–9). The persistence of NNRTI-associated mutants after the discontinuation of an NNRTI-containing regimen may contribute to the prevalence of NNRTI-associated TDR mutants.
Three mutants, K103N, Y181C, and G190A, account for >90% of the NNRTI-associated TDR mutants in the United States (10). K103N, Y181C, and K103N/Y181C are the top 3 most prevalent NNRTI-associated mutants representing >60% of NNRTI-associated mutants in experienced patients, based on the Stanford HIV database (11). A new NNRTI capable of suppressing the most prevalent NNRTI-associated and TDR mutants would therefore be a significant addition to current HIV-1 therapeutic options. Doravirine (DOR, formerly MK-1439) is a novel NNRTI that displays excellent antiviral activity against these most prevalent NNRTI-associated mutants in vitro (12).
The inhibitory quotient (IQ), defined as the ratio of the clinical trough concentration to the 50% inhibitory concentration (IC50), has been shown to be a good predictor of clinical efficacy (13). To assess the potential clinical efficacy of DOR against common NNRTI-resistant mutants, we determined the IQs for DOR, RPV, and efavirenz (EFV) and conducted in vitro resistance selections with K103N, Y181C, G190A, and K103N/Y181C mutants using clinically relevant concentrations. Compared to RPV and EFV, DOR exhibited the best potency and the highest IQ against prevalent NNRTI-associated and TDR mutants, except Y188L. Consistent with the high calculated IQ for DOR, no viral breakthrough was detected in the resistance selection with the K103N, Y181C, G190A, and K103N/Y181C mutant viruses at clinically relevant concentrations. In contrast, viral breakthrough was detected when the K103N and K103N/Y181C NNRTI-resistant variants were in the selection with EFV or when the Y181C and K103N/Y181C mutant viruses were in the selection with RPV. The high IQ and resistance barrier of DOR compared to those of other NNRTIs suggests it will be a valuable addition to current antiretroviral therapies.
MATERIALS AND METHODS
Generation of mutant viruses.
Each mutant was created by site-directed mutagenesis methods via gene synthesis and subcloning in plasmid RT112, which contained full-length R8 provirus DNA. The 293T cells were seeded at 2.5 × 106 cells in a 10-cm-diameter dish. After incubation for 24 h, cells were transfected with 18 μg of provirus plasmid DNA using FuGENE HD transfection reagent. The supernatant was harvested at 48 h posttransfection. Each mutant virus was validated and evaluated for viral infectivity using MT4-green fluorescent protein (GFP) reporter cells.
Antiviral assay in the presence of 100% NHS.
HIV-1 replication was monitored using MT4-gag-GFP cells (here designated MT4-GFP), which are MT4 cells modified to harbor a GFP reporter gene, the expression of which is dependent on the HIV-1-expressed proteins encoded by tat and rev. The productive infection of an MT4-GFP cell with HIV-1 results in GFP expression at approximately 24 h postinfection. MT4-GFP cells were maintained at 37°C, 5% CO2, and 90% relative humidity in RPMI 1640 supplemented with 10% fetal bovine serum, 100 U/ml penicillin-streptomycin, and 400 μg/ml G418 to maintain the reporter gene. For infections, MT4-GFP cells were placed in the same medium lacking G418 and were typically infected overnight with an HIV-1 virus stock at an approximate multiplicity of infection of 0.01, under the same incubation conditions. The experiments were conducted using wild-type strain R8 and variants containing mutations in reverse transcriptase known to confer resistance to NNRTIs. Cells were then washed and resuspended in RPMI 1640 containing 10% normal human serum (NHS) at 1.6 × 105 cells/ml (10% NHS conditions). Compound plates were prepared by dispensing compounds dissolved in dimethyl sulfoxide (DMSO) into wells of 384-well poly-d-lysine-coated plates (0.2 μl/well) using an acoustic dispenser. Each compound was tested in a 10-point serial 3-fold dilution (typical final concentrations, 4.2 μM to 0.21 nM). The controls included no inhibitor (DMSO only) and a combination of three antiviral agents (efavirenz, indinavir, and an in-house integrase strand transfer inhibitor, at final concentrations of 4 μM each). The infected cells were added (50 μl/well) to the compound plates, and the resulting plates were maintained at 37°C, 5% CO2, and 90% relative humidity.
The infected cells were quantified at two time points, ∼48 h and ∼72 h postinfection, by counting the number of green cells in each well using an Acumen eX3 scanner. The ratio of the number of green cells at 48 h to that at 72 h was employed to determine the IC50s.
In vitro resistance selection with HIV-1 mutant viruses at clinically relevant concentrations.
In vitro resistance selection was performed in a 96-well format with prevalent NNRTI-associated mutants and MT4-GFP cells (75,000 cells/per well) at 0.5×, 1×, and 2× of the calculated clinically relevant concentrations of NNRTIs in the presence of 10% NHS. After 3 to 4 days of culturing, a new selection cycle was initiated. Culture medium or fresh MT4-GFP cells were added to a preprepared compound plate. The culture mixture (30 μl) from each well was transferred from the previous selection plate to the new drug plate. This procedure was repeated every 3 to 4 days using a liquid handling station. For every passage, the plates were scanned with an Acumen eX3 fluorescence detector to monitor signs of viral breakthrough by the emission of green fluorescence via GFP upon viral infection. Once viral breakthrough was detected, the supernatant was removed from the wells and subjected to genotyping analysis.
Analysis of RT mutation(s) in the breakthrough viruses from resistance selection studies.
Viral RNA was extracted from culture supernatant of breakthrough virus stock from the resistance studies described above using the MagMAX-96 viral RNA isolation kit. The encoding reverse transcriptase (RT) region was amplified by one-step RT-PCR. PCR products were genotyped using an automated population-based full-length sequencing method. The primers used for PCR amplification were the same as those described previously (12).
RESULTS
In vitro inhibitory potency of DOR, RPV, and EFV against the most prevalent NNRTI-associated mutants in the presence of 100% NHS.
For highly protein-bound inhibitors, in vitro antiviral potencies shift significantly when the assays are conducted in the presence of 50% serum compared with 10% serum (14–17). Although it is highly desirable to assess activity in the presence of 100% serum, the potency at 100% serum is often extrapolated from the potency determined at a lower percentage of serum, assuming a linear relationship between inhibitory potency and serum concentration. Depending on the degree of hydrophobicity, however, the correlation is often not in a linear relationship, especially for highly protein-bound compounds, such as NNRTIs (17). Therefore, the potency obtained from the extrapolation does not accurately reflect the potency in 100% serum. To avoid these discrepancies, we determined the inhibitory potencies of DOR and other NNRTIs using K103N, Y181C, and K103N/Y181C mutant viruses in the presence of 100% NHS.
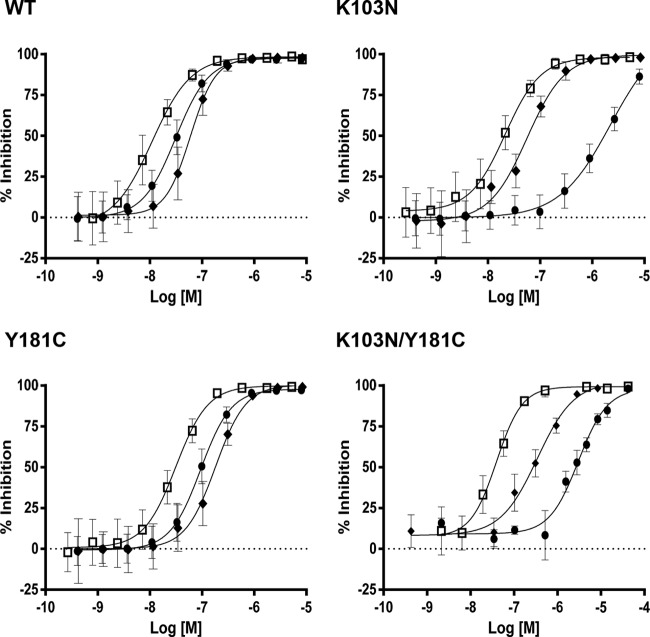
DOR displayed similar potency against wild-type (WT) virus and the K103N, Y181C, and K103N/Y181C mutants. Although DOR was less potent than RPV and EFV when the assays were performed in the presence of 10% NHS, DOR is 4.7-, 2.7-, 5.5-, and 9.6-fold more potent than RPV and 2.5-, 56-, 2.9-, and 94.5-fold more potent than EFV against these viruses in the presence of 100% NHS, as shown in Fig. 1 (15). The better potency of DOR in 100% NHS can be attributed to the lower level of protein binding compared to that with RPV and EFV, at 76% versus 99.6% and 99.6%, respectively.
FIG 1.
Titration curves for the antiviral activities of DOR, RPV, and EFV against WT virus, K103N, Y181C, and K103N/Y181C mutants in the presence of 100% NHS (open square, DOR; filled diamond, RPV; filled circle, EFV). The potencies (IC50s) is as follows: WT virus: DOR, 12 ± 4.2 nM; RPV, 58 ± 15 nM; EFV, 30 ± 8.7 nM); for the K103N mutant: DOR, 21 ± 6.8 nM; RPV, 56 ± 15 nM; EFV, 1,173 ± 448 nM); Y181C mutant: DOR, 31 ± 10 nM; RPV, 169 ± 45 nM; EFV, 90 ± 21 nM). K103N/Y181C mutant: DOR, 33 ± 5.4 nM; RPV, 318 ± 62 nM; EFV, 3,119 ± 920 nM). [M], concentration of NNRTIs. The data are represented as the means ± standard deviations from the results of >3 replicates.
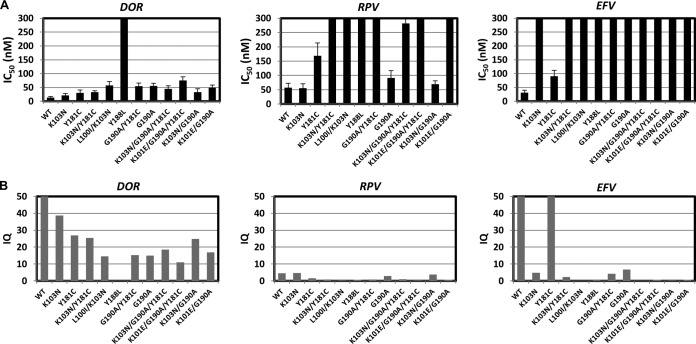
To further characterize the mutant profile of DOR versus that of RPV and EFV, we also evaluated their activities against an additional 8 prevalent NNRTI-associated mutant viruses, according to the Stanford HIV database. The antiviral potency of DOR, RPV, and EFV against prevalent NNRTI-associated mutants in 100% NHS is summarized in Fig. 2A. With the exception of Y188L, DOR also exhibited the best potency against this panel of mutants.
FIG 2.
Antiviral activities (IC50s) (A) and inhibitory quotients (IQs) (B) of DOR, RPV, and EFV against prevalent NNRTI-associated mutants in the presence of 100% NHS. The data are represented as the means ± standard deviations from the results of >3 replicates.
For antiretroviral agents in general, and specifically NNRTIs, the trough concentration plays an essential role with respect to sustained efficacy, and the calculated IQ using drug concentrations observed at trough has been used to predict clinical efficacy. For DOR, at a daily dose of 100 mg (the dose employed in the phase 3 clinical trials), the plasma trough concentration at 24 h is 830 nM. The trough concentrations of EFV and RPV are 5,600 nM and 260 nM at 24 h at clinical doses of 600 mg and 25 mg, respectively (18, 19). These values and the respective IC50s determined in the presence of 100% serum were used to calculate IQs for each of these drugs versus the panel of NNRTI mutants, as shown in Fig. 2B. In addition, we also evaluated the IQ values against WT virus for NNRTIs that were licensed or under clinical development. EFV exhibited the highest IQ, 178, and RPV displayed the lowest IQ, 4.5, followed by IDX899, with an IQ of 5.5 (20). Those NNRTIs all achieved efficacy in the clinic setting at these trough concentrations. Therefore, we can assume that the IQs of ≥4.5 are required for efficacy.
With the exception of Y188L, DOR displayed an IQ of >10 against all mutants evaluated. For DOR, the IQs were 39, 27, and 25 against the K103N, Y181C, and K103N/Y181C mutants. In contrast, only 2 mutants (Y181C and G190A) showed an IQ of >5 with EFV, and all IQs were <5 with RPV. Furthermore, 5 and 7 mutants displayed IQs of <1 with EFV and RPV, respectively. These results suggest DOR may have a significant advantage over EFV and RPV against these prevalent NNRTI-associated mutants in clinical settings.
IQs were also determined for several other TDR mutants, such as the P225H, K101E, and L100I mutants. DOR again showed significant higher IQs than those of RPV and was comparable to that with EFV (except P225H, for which the IQs were 94 for EFV and 14 for DOR).
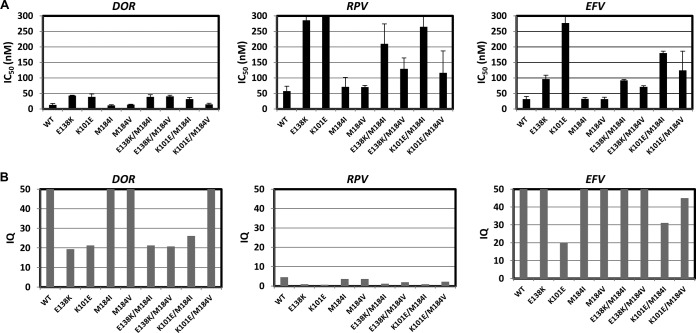
In vitro inhibitory potency of DOR, RPV, and EFV against RPV-associated mutants in the presence of 100% NHS.
In the ECHO and THRIVE phase 3 trials of RPV, the most common NNRTI-resistant mutants that emerged upon virologic failure in the RPV-treated group were those with E138K (45%), followed by K101E (13%) (21). In these studies, most of the E138K substitutions occurred along with NRTI-resistant mutants, particularly M184I/V. We evaluated the susceptibility of these RPV-associated mutants to DOR, RPV, and EFV in the presence of 100% NHS (Fig. 3A). The IQs were calculated and are summarized in Fig. 3B. Against this panel of RPV-associated mutants, DOR was more potent than either RPV or EFV. DOR again displayed high IQs (>15) with this panel of mutant viruses, as was observed for the common NNRTI mutants. In contrast to the results with prevalent NNRTI-associated mutants, EFV also exhibited high IQs against the RPV-associated mutant viruses. Surprisingly, RPV not only had low IQs (<1) against E138K and K101E, but it also had low IQs versus M184V and M184I mutants (<5), the most prevalent NRTI mutants observed with lamivudine (3TC) or emtricitabine (FTC). The low clinical trough concentration of RPV resulting in low IQ may explain the prevalence of the E138 variants along with M184I/V identified in patients who have failed an RPV-containing regimen. Although the uncertainty has been raised regarding the usefulness of IQs of NNRTIs in predicting clinical efficacy (22), these results suggest that IQ may be a good predictor of clinical efficacy for NNRTIs.
FIG 3.
Antiviral activities (IC50s) (A) and inhibitory quotients (IQs) (B) of DOR, RPV, and EFV against RPV-associated mutants in the presence of 100% NHS. The data are represented as the means ± standard deviations from the results of >3 replicates.
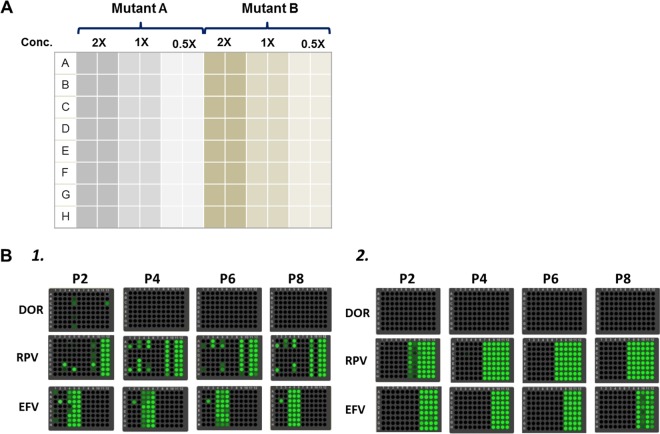
Resistance selection of DOR, RPV, and EFV with prevalent NNRTI-associated mutant viruses.
As mentioned above, the K103N and Y181C mutants are the 2 most prevalent NNRTI-associated and TDR mutants. K103N/Y181C and G190A account for the third most prevalent NNRTI-associated and TDR mutants, respectively. To evaluate the capability of DOR, EFV, and RPV in suppressing these mutants, in vitro resistance selection studies were conducted with the NNRTIs against these mutants using the clinical trough concentration of each NNRTI. Although resistance selection would ideally be performed in the presence of 100% NHS, the viability of MT4-GFP reporter cells was significantly compromised after long-term incubation in the presence of 100% serum. As a result, these studies could be performed only in the presence of 10% serum. To determine the clinically relevant concentrations to be employed for selection studies, we used the IQ, calculated with the IC50 determined with 100% serum to multiply the IC50 determined in the presence of 10% serum, as shown in Table 1. The calculated concentrations used for the resistance selection study were 200 nM, 20 nM, and 500 nM for DOR, RPV, and EFV, respectively. To take into account potential pharmacokinetic (PK) variability in the clinic setting, we also included 2× and 0.5× the calculated concentrations in the study. Resistance selections were performed in a 96-well format, as shown in Fig. 4A. Two mutants were included on each plate (one mutant in columns 1 to 6 and the other in columns 7 to 12), and each concentration was distributed into 2 columns with 8 rows in each column, accounting for a total of 16 repeats. The plates were monitored for viral breakthrough by the appearance of green fluorescence. As shown in Fig. 4B1, in the selection with K103N and Y181C mutants, there was no viral breakthrough observed with DOR at any concentrations. In contrast, fluorescence was detected in many wells in the selection of both Y181C and K103N mutants with RPV. Not surprisingly, viral breakthrough was observed in the selection with K103N at 0.5× and 1× concentrations of EFV. However, no viral breakthrough was detected in the selection with the Y181C mutant at any concentrations of EFV.
TABLE 1.
Calculation of clinically relevant concentrations of drug for in vitro resistance selection studies
| Parametera | DOR | RPV | EFV |
|---|---|---|---|
| Clinical dose (mg) | 100 | 25 | 600 |
| C24 (nM) | 610b | 260 | 5,600 |
| IC50 in 100% NHS (nM) | 12.3 | 56 | 30 |
| IQ | 49.6 | 4.6 | 187 |
| IC50 in 10% NHS (nM) | 3.7 | 4.5 | 2.6 |
| Concn calculated for resistance selection in 10% NHS (nM) (IQ × IC50 in 100% NHS) | 184 | 21 | 486 |
| Selected concn for resistance selection in 10% NHS (nM) | 200 | 20 | 500 |
C24, clinical trough concentration. IQ was calculated as the ratio of C24/IC50 in 100% NHS.
The trough concentration of DOR used in this calculation was based on the preliminary phase 1a trial. However, the trough concentration was projected to be 830 nM, based on both phase 1 and 2 trials, which was used to calculate the IQs described above.
FIG 4.
In vitro resistance selection with prevalent NNRTI-associated mutants. (A) Plate layout. 1× represents the concentration (conc.) selected for resistance selection based on the calculation from Table 1. Each concentration was included in two columns (16 replicates). (B1) K103N mutant (columns 1 to 6) and Y181C mutant (columns 7 to 12). (B2) G190A mutant (columns 1 to 6) and K103N/Y181C mutant (columns 7 to 12). P, passage number.
In the resistance selection with K103N/Y181C and G190A mutants, shown in Fig. 4B2, no viral breakthrough was identified with the G190A mutant for all 3 drugs at any concentration. DOR also successfully prevented the K103N/Y181C double mutant from breaking through. On the other hand, viral breakthrough was detected with the double mutant at all 3 concentrations of RPV and 0.5× and 1× concentrations of EFV.
DNA sequencing was performed with the RNA samples prepared from breakthrough viruses. The results are summarized in Table 2. In the resistance selection study with the K103N mutant in the presence of RPV, additional mutations were identified, including L100I, V179I/T/A, and Y181C substitutions, with a minor portion of breakthrough viruses containing an additional E138Q substitution. In the selection with the K103N mutant in the presence of EFV, additional mutations, such as L100I, L234I, and V108I, were detected. Several other mutations were also identified at smaller fractions of the breakthrough viruses. In the selection using the Y181C mutant, RPV selected additional M230I, V106I, and H221Y substitutions. In the selection with the K103N/Y181C double mutant with RPV, significant numbers of additional mutations were identified, including V179L, V90I, H221Y, K101E, and L100I. Similarly, mutants with the L100I, V108I, V179E, H221Y, and P225H substitutions were selected by EFV with the double mutant at the 0.5× and 1× concentrations.
TABLE 2.
Mutations identified in the resistance selection studies of NNRTIs with prevalent NNRTI-associated mutants
| Mutant | Additional mutation(s) selecteda |
||
|---|---|---|---|
| DOR | RPV | EFV | |
| K103N | None | L100I, V179I/T/A, Y181C, E138Q | L100I, V108I, L234I, V179A, M230I, P225H/S, Y188C, V90I, H221Y, F227L, K101Q |
| Y181C | None | V106I, H221Y, M230I, K101E, V179 M, V90I, V189I, F227C | None |
| K103N/Y181C | None | V90I, L100I , K101E V179L, H221Y | L100I, V108I, V179E, H221Y, P225H |
| G190A | None | None | None |
Mutants in bold represent the most frequent mutations identified in breakthrough viruses.
DISCUSSION
The fold change in potency compared to that of the WT should be similar regardless of whether the assay was done in the presence of 10% or 100% serum. For high-protein-binding compounds, such as RPV and EFV, however, the potency determined in 100% NHS shifts significantly compared to the potency determined in the presence of 10% NHS and is not accurately extrapolated from the assessment made at a lower percentage of NHS. For example, the IC50 was 14 nM when the assay was conducted with RPV against the Y181C mutant in the presence of 10% NHS, whereas the IC50 was 169 nM when it was determined in the presence of 100% NHS, representing a >10-fold shift in potency compared to an only 3-fold shift with the lower-protein-binding DOR (9.7 nM in 10% NHS versus 31 nM in 100% NHS, respectively). Here, we determined the inhibitory potency of NNRTIs with various mutants in the presence of 100% NHS. The determination of these exact values is critical to the use of IQ as a tool to predict clinical efficacy (23). Given the high level of protein binding of EFV and RPV compared to that with DOR (99.6% versus 76.0%), if the free fraction of each respective NNRTI is factored into the IQ calculation, the advantage of DOR over RPV and EFV is more prominent because of the high trough concentration and low protein binding.
The IQ of EFV against WT virus is 178 versus 4.6 for the K103N mutant. As a result, when patient adherence is not optimal, the lower threshold may allow K103N breakthrough, as supported by the results of our in vitro resistance selection study with the mutant. In contrast, the IQ for Y181C is 62, which may explain why the Y181C mutant is rarely associated with EFV, and it supports the observation that no breakthrough virus observed in our selection studies with this mutant using clinically relevant concentrations of EFV. The K103N/Y181C and K103N/L100I double mutants, which represent the number the third- and fourth most prevalent NNRTI-associated mutants, displayed IQs of 2.3 and 0.3 with EFV, respectively, which is also consistent with the clinical findings in patients who fail an EFV-containing regimen. With RPV, the relatively low trough concentration of 260 nM resulted in IQs of <5 for all 11 common NNRTI-associated mutants that we evaluated, and the most frequent mutations associated with RPV failure of E138K, K101E, and Y181C mutants displayed IQs that were even lower, at 0.9, 0.7, and 1.5, respectively. These data are therefore consistent with the clinical findings for these drugs and suggest that the lower protein binding and resultant higher IQ of DOR may offer an advantage over both EFV and RPV with respect to the suppression of both WT and NNRTI mutants. In resistance selection studies in which DOR was compared to EFV and RPV at clinically relevant concentrations, DOR but not EFV or RPV was able to suppress prevalent NNRTI-associated mutants, including K103N, Y181C, and G190A mutants and the K103N/Y181C double mutant. However, resistance mutants to DOR might emerge if study was performed for longer period of time.
The DOR trough concentration employed in the calculation of the target concentration to be used for the resistance selection study with mutant viruses was 610 nM (Table 1) based on limited phase 1 data. As mentioned above, the projected trough concentration was 830 nM, based on data from phase 1 and 2 trials. Therefore, the DOR concentration that was used in the resistance study should have been 1/3 times higher, which is 270 nM instead of 200 nM. Despite this, DOR was still able to successfully suppress the 4 mutants from breakthrough when 200 nM was employed for resistance selection (Table 2). The results from these studies suggest that DOR displayed better antiviral activity than the other two drugs. The higher IQ of DOR against the prevalent NNRTI-associated mutants, which also includes prevalent TDR mutants, such as K103N, Y181C, and G190A, was confirmed in resistance selection studies at clinically relevant concentrations. Taken together, these data suggest DOR may possess a higher barrier for the development of resistance compared to the other drugs tested, representing a valuable addition to the antiretroviral (ARV) armamentarium.
REFERENCES
- 1.Palella FJ Jr, Delaney KM, Moorman AC, Loveless MO, Fuhrer J, Satten GA, Aschman DJ, Holmberg SD. 1998. Declining morbidity and mortality among patients with advanced human immunodeficiency virus infection. HIV Outpatient Study Investigators. N Engl J Med 338:853–860. [DOI] [PubMed] [Google Scholar]
- 2.Schneider MF, Gange SJ, Williams CM, Anastos K, Greenblatt RM, Kingsley L, Detels R, Muñoz A. 2005. Patterns of the hazard of death after AIDS through the evolution of antiretroviral therapy: 1984–2004. AIDS 19:2009–2018. doi: 10.1097/01.aids.0000189864.90053.22. [DOI] [PubMed] [Google Scholar]
- 3.Johnson JA, Li JF, Wei X, Lipscomb J, Irlbeck D, Craig C, Smith A, Bennett DE, Monsour M, Sandstrom P, Lanier ER, Heneine W. 2008. Minority HIV-1 drug resistance mutations are present in antiretroviral treatment-naive populations and associate with reduced treatment efficacy. PLoS Med 5:e158. doi: 10.1371/journal.pmed.0050158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pillay D, Bhaskaran K, Jurriaans S, Prins M, Masquelier B, Dabis F, Gifford R, Nielsen C, Pedersen C, Balotta C, Rezza G, Ortiz M, de Mendoza C, Kücherer C, Poggensee G, Gill J, Porter K, CASCADE Virology Collaboration . 2006. The impact of transmitted drug resistance on the natural history of HIV infection and response to first-line therapy. AIDS 20:21–28. doi: 10.1097/01.aids.0000196172.35056.b7. [DOI] [PubMed] [Google Scholar]
- 5.Metzner KJ, Giulieri SG, Knoepfel SA, Rauch P, Burgisser P, Yerly S, Günthard HF, Cavassini M. 2009. Minority quasispecies of drug-resistant HIV-1 that lead to early therapy failure in treatment-naive and -adherent patients. Clin Infect Dis 48:239–247. doi: 10.1086/595703. [DOI] [PubMed] [Google Scholar]
- 6.Taniguchi T, Nurutdinova D, Grubb JR, Önen NF, Shacham E, Donovan M, Overton ET. 2012. Transmitted drug-resistant HIV type 1 remains prevalent and impacts virologic outcomes despite genotype-guided antiretroviral therapy. AIDS Res Hum Retroviruses 28:259–264. doi: 10.1089/aid.2011.0022. [DOI] [PubMed] [Google Scholar]
- 7.Little SJ, Frost SD, Wong JK, Smith DM, Pond SL, Ignacio CC, Parkin NT, Petropoulos CJ, Richman DD. 2008. Persistence of transmitted drug resistance among subjects with primary human immunodeficiency virus infection. J Virol 82:5510–5518. doi: 10.1128/JVI.02579-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Joly V, Descamps D, Peytavin G, Touati F, Mentre F, Duval X, Delarue S, Yeni P, Brun-Vezinet F. 2004. Evolution of human immunodeficiency virus type 1 (HIV-1) resistance mutations in nonnucleoside reverse transcriptase inhibitors (NNRTIs) in HIV-1-infected patients switched to antiretroviral therapy without NNRTIs. Antimicrob Agents Chemother 48:172–175. doi: 10.1128/AAC.48.1.172-175.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pineda-Peña AC, Bello DC, Sussmann O, Vandamme AM, Vercauteren J, van Laethem K, Gomez-Lopez A. 2012. HIV-1 transmitted drug resistance in Latin America and the Caribbean: what do we know? AIDS Rev 14:256–267. [PubMed] [Google Scholar]
- 10.Ocfemia MC, Kim D, Ziebell R, Prejean J, Saduvala N, Pieniazek D. Prevalence and trends of transmitted drug resistance-associated mutations by duration of infection among persons newly diagnosed with HIV-1 infection: 5 states and 3 municipalities, US, 20062009, by duration of infection among persons newly diagnosed with HIV-1 infection: 5 states and 3 municipalities, US, 2006--2009, abstr 730 19th Conf Retroviruses Opportun Infect (CROI), 8 May 2012. Seattle, WA. [Google Scholar]
- 11.Rhee SY, Blanco JL, Jordan MR, Taylor J, Lemey P, Varghese V, Hamers RL, Bertagnolio S, Rinke de Wit TF, Aghokeng AF, Albert J, Avi R, Avila-Rios S, Bessong PO, Brooks JI, Boucher CA, Brumme ZL, Busch MP, Bussmann H, Chaix ML, Chin BS D'Aquin TT, De Gascun CF, Derache A, Descamps D, Deshpande AK, Djoko CF, Eshleman SH, Fleury H, Frange P, Fujisaki S, Harrigan PR, Hattori J, Holguin A, Hunt GM, Ichimura H, Kaleebu P, Katzenstein D, Kiertiburanakul S, Kim JH, Kim SS, Li Y, Lutsar I, Morris L, Ndembi N, Ng KP, Paranjape RS, Peeters M, Poljak M, Price MA, et al. 2015. Geographic and temporal trends in the molecular epidemiology and genetic mechanisms of transmitted HIV-1 drug resistance: an individual-patient- and sequence-level meta-analysis. PLoS Med 12:e1001810. doi: 10.1371/journal.pmed.1001810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Feng M, Wang D, Grobler JA, Hazuda DJ, Miller MD, Lai MT. 2015. In vitro resistance selection with doravirine (MK-1439), a novel nonnucleoside reverse transcriptase inhibitor with distinct mutation development pathways. Antimicrob Agents Chemother 59:590–598. doi: 10.1128/AAC.04201-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hsu A, Isaacson J, Brun S, Bernstein B, Lam W, Bertz R, Foit C, Rynkiewicz K, Richards B, King M, Rode R, Kempf DJ, Granneman GR, Sun E. 2003. Pharmacokinetic-pharmacodynamic analysis of lopinavir-ritonavir in combination with efavirenz and two nucleoside reverse transcriptase inhibitors in extensively pretreated human immunodeficiency virus-infected patients. Antimicrob Agents Chemother 47:350–359. doi: 10.1128/AAC.47.1.350-359.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lai MT, Munshi V, Touch S, Tynebor RM, Tucker TJ, McKenna PM, Williams TM, DiStefano DJ, Hazuda DJ, Miller MD. 2009. Antiviral activity of MK-4965, a novel nonnucleoside reverse transcriptase inhibitor. Antimicrob Agents Chemother 53:2424–2431. doi: 10.1128/AAC.01559-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lai MT, Feng M, Falgueyret JP, Tawa P, Witmer M, DiStefano D, Li Y, Burch J, Sachs N, Lu M, Cauchon E, Campeau LC, Grobler J, Yan Y, Ducharme Y, Cote B, Asante-Appiah E, Hazuda DJ, Miller MD. 2014. In vitro characterization of MK-1439, a novel HIV-1 nonnucleoside reverse transcriptase inhibitor. Antimicrob Agents Chemother 58:1652–1663. doi: 10.1128/AAC.02403-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lu M, Felock PJ, Munshi V, Hrin RC, Wang YJ, Yan Y, Munshi S, McGaughey GB, Gomez R, Anthony NJ, Williams TM, Grobler JA, Hazuda DJ, McKenna PM, Miller MD, Lai MT. 2012. Antiviral activity and in vitro mutation development pathways of MK-6186, a novel nonnucleoside reverse transcriptase inhibitor. Antimicrob Agents Chemother 56:3324–3335. doi: 10.1128/AAC.00102-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Acosta EP, Limoli KL, Trinh L, Parkin NT, King JR, Weidler JM, Ofotokun I, Petropoulos CJ. 2012. Novel method to assess antiretroviral target trough concentrations using in vitro susceptibility data. Antimicrob Agents Chemother 56:5938–5945. doi: 10.1128/AAC.00691-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mills AM, Cohen C, Dejesus E, Brinson C, Williams S, Yale KL, Ramanathan S, Wang MH, White K, Chuck SK, Cheng AK. 2013. Efficacy and safety 48 weeks after switching from efavirenz to rilpivirine using emtricitabine/tenofovir disoproxil fumarate-based single-tablet regimens. HIV Clin Trials 14:216–223. doi: 10.1310/hct1405-216. [DOI] [PubMed] [Google Scholar]
- 19.Dickinson L, Amin J, Else L, Boffito M, Egan D, Owen A, Khoo S, Back D, Orrell C, Clarke A, Losso M, Phanuphak P, Carey D, Cooper DA, Emery S, Puls R, ENCORE1 Study Group . 2015. Pharmacokinetic and pharmacodynamic comparison of once-daily efavirenz (400 mg vs. 600 mg) in treatment-naive HIV-infected patients: results of the ENCORE1 study. Clin Pharmacol Ther 98:406–416. doi: 10.1002/cpt.156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zala C, St Clair M, Dudas K, Kim J, Lou Y, White S, Piscitelli S, Dumont E, Pietropaolo K, Zhou XJ, Mayers D. 2012. Safety and efficacy of GSK2248761, a next-generation nonnucleoside reverse transcriptase inhibitor, in treatment-naive HIV-1-infected subjects. Antimicrob Agents Chemother 56:2570–2575. doi: 10.1128/AAC.05597-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rimsky L, Vingerhoets J, Van Eygen Eron J, Clotet B, Hoogstoel A, Boven K, Picchio G. 2012. Genotypic and phenotypic characterization of HIV-1 isolates obtained from patients on rilpivirine therapy experiencing virologic failure in the phase 3 ECHO and THRIVE studies: 48-week analysis. J Acquir Immune Defic Syndr 59:39–46. [DOI] [PubMed] [Google Scholar]
- 22.la Porte C. 2008. Inhibitory quotient in HIV pharmacology. Curr Opin HIV AIDS 3:283–287. [DOI] [PubMed] [Google Scholar]
- 23.Sadler BM, Gillotin C, Lou Y, Stein DS. 2001. Pharmacokinetic and pharmacodynamic study of the human immunodeficiency virus protease inhibitor amprenavir after multiple oral dosing. Antimicrob Agents Chemother 45:30–37. doi: 10.1128/AAC.45.1.30-37.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]