Abstract
Osteoarthritis (OA) of the hip is a common cause of hip pain. The arthroscopic management of patients with femoro-acetabular impingement (FAI) has been reported to yield good outcomes. The purpose of this study was to report on outcome following the arthroscopic treatment of patients with FAI in the presence of mild to moderate OA. Seventy-five patients undergoing arthroscopic surgery for FAI, all with preoperative radiological signs of mild to moderate OA were prospectively included in this study. A 2-year follow-up, using web-based patient-reported outcome measures, including the International Hip Outcome Tool (iHOT-12), Copenhagen Hip and Groin Outcome (HAGOS), EQ-5D, Hip Sports Activity Scale (HSAS) for physical activity level and a visual analogue scale (VAS) for overall hip function, was performed, complemented by a radiographic evaluation. At follow-up (mean 26 months, SD 5), five patients (7%) had undergone total hip arthroplasty, leaving 70 patients for the analysis. Preoperative scores compared with those obtained at the 2-year follow-up revealed significant improvements (P < 0.0001) for all measured outcomes; the iHOT-12 (42 versus 65), VAS for global hip function (48 versus 68), HSAS (2.5 versus 3), EQ5D index (0.62 versus 0.76), EQ VAS (69 versus 75) and different HAGOS subscales (54 versus 72, 47 versus 67, 56 versus 75, 40 versus 61, 33 versus 56, 31 versus 55). At follow-up, 56 (82%) patients reported that they was satisfied with the outcome of surgery. Arthroscopic treatment for patients with FAI in the presence of mild to moderate OA resulted in statistically significant and clinically relevant improvements in outcome measures related to pain, symptoms, function, physical activity level and quality of life in the majority of patients.
INTRODUCTION
Femoro-acetabular impingement (FAI) has been regarded as a causal factor in the development of hip osteoarthritis (OA) [1–4]. FAI has also been reported to be an isolated cause of pain and reduced range of motion (ROM) in the hip and groin area [5, 6]. High-level physical activity in adolescents has, furthermore, been regarded as a causal factor in the development of cam deformity, leading to FAI [7, 8]. Athletes have also been reported to have an increased risk of developing hip OA [9].
Moreover, sports including repetitive hip flexion, such as soccer or ice-hockey, may cause chondrolabral damage to the hip joint and thereby pain in the hip and groin area [10, 11].
The arthroscopic management of patients with FAI has been reported to produce good outcome [12–14]. Only a few studies have specifically evaluated patients with FAI and OA. These studies report generally positive results in terms of patient-reported outcome measures (PROMs) [15–19]. However, higher conversion rates to total hip arthroplasty (THA) in patients who have a joint space of 2 mm or less have been reported, suggesting inferior results in this patient category [20–22].
The results of the arthroscopic treatment of FAI in patients with varying degrees of OA are still largely unknown.
The purpose of this study was to evaluate the arthroscopic treatment of FAI in the presence of OA in terms of pain, symptoms, function, physical activity level and quality of life using outcome measures validated for young, active patients with hip symptoms.
MATERIALS AND METHODS
Preoperative radiographs of all primary hip arthroscopies performed by three surgeons due to FAI from November 2011 through December 2012 (n = 569) at two centres were assessed prospectively by a single observer. The inclusion criterion was signs of OA, defined as Tönnis grade 1 or 2. The exclusion criteria were re-operation (n = 10), non-FAI cases (n = 2) and diabetes (n = 1). A total of 80 hips in 75 patients (males n = 59, females n = 16) were included (Table I) and followed prospectively with regard to PROMs for 2 years. The number of re-operations was recorded.
Table I.
Patient demographics and preoperative data
| Demographics | Total |
|---|---|
| Total number of patients | 75 |
| Total number of hips | 80 |
| Operated side R/L/bilateral (%) | 40/53/7 |
| Male/female (%) | 77/23 |
| Symptom duration | 48/6–252/78 |
| Median/range/IQR (months) | |
| Percentage day surgery (%) | 100 |
| Age–mean (SD) (years) | 47 (10) |
| Operation time–mean (SD) (min) | 77 (18) |
| Traction time–mean (SD) (min) | 11 (8) |
| Joint could not be distracted (%) | 13 |
Indications for surgery were a clinical and radiological diagnosis of FAI and failed non-surgical treatment consisting of structured physical therapy of minimum 3 months sometimes adding cortisone injection. No PRP injections or viscosupplementation were used. The diagnosis of FAI was made from patient history, physical examination and radiological findings consistent with FAI of cam type, pincer type or mixed. Preoperative data were registered at the time of surgery. All patients could be discharged the same day as the surgical procedure was performed.
Patient-reported outcomes, physical activity and follow-up
All patients completed self-administered web-based health-related PROMs, including the International Hip Outcome Tool (iHOT-12), the Copenhagen Hip and Groin Outcome Score (HAGOS, six subscales), the Hip Sports Activity Scale (HSAS), a visual analogue scale (VAS) for overall hip function and a standardized instrument (EQ-5D, two subscales) as a quality of life measure [23–26]. All these outcome measures have previously been validated and culturally adapted to Swedish [23, 25, 27]. Moreover, the patients reported whether or not they were satisfied with the surgery with a single, non-validated question. The questionnaires were administered preoperatively, 12 and 24 months post-operatively.
Radiology
Radiographs were taken at baseline and 1-year post-operatively and classified according to Tönnis [28] by an independent radiologist, an expert in musculoskeletal radiology. Moreover, the joint space was measured at three locations preoperatively and at the 1-year follow-up on an anteroposterior pelvic radiograph (lateral sourcil, middle sourcil and above the level of the fovea) [20]. If a THA had been performed, this was registered.
Surgical technique
The preferred arthroscopic procedure, previously described by Sansone et al. [29], utilizes an anterolateral portal and a mid-anterior portal with the patient in a supine position. Axial traction was used to view the central compartment for diagnostic evaluation, free-body removal or microfracture.
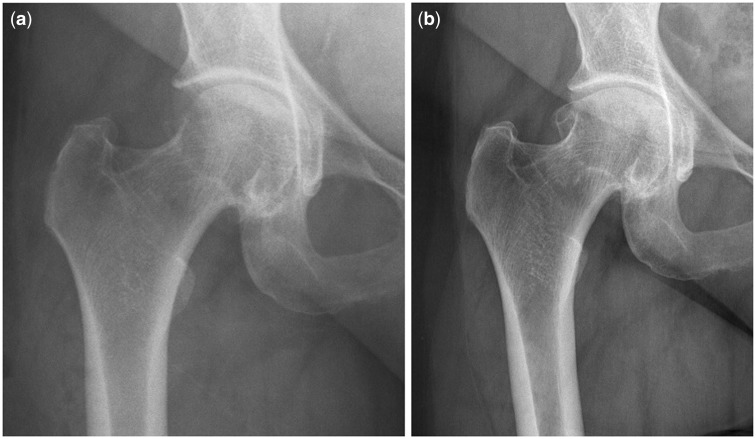
Access to the peripheral compartment was achieved through a ligament-sparing capsulotomy, which was parallel to the fibres of the ileo-femoral ligament and had a minimal component of transverse cut. By minimizing the damage to the ligaments and capsule, the risk of an iatrogenic increase in the laxity of the hip can be reduced. Acetabular over-coverage (pincer) was removed using an ‘over-the-top’ technique, where the burr was placed in the peri-labral sulcus and the resection of the pincer was made with the labrum in situ. In patients in whom small rim resections were performed the labrum was left in situ. With larger rim resections, the labrum was re-attached using suture anchors. A meticulous cam resection, spanning between far lateral, far medial/caudal and posterior, as well as an intra-operative dynamic assessment of impingement, was performed in order to avoid residual impingement (Fig.1a and b). In patients with a pistol-grip deformity or posterior/lateral osteophytes, a resection was also performed posterior and cranial to the lateral retinacular fold to correct posterolateral impingement. However, care was taken to preserve the lateral retinacular vessels. Microfracture was performed in cases with localized bare bone lesions, but not in cases with more general OA and complete cartilage loss.
Fig. 1.
(a) Preoperative images of cam deformity. (b) Post-operative image after cam resection in (a).
Post-operatively, all patients were allowed free ROM and full weight-bearing during the early rehabilitation phase. Crutches were recommended for one month for outdoor and longer ambulation. Physiotherapy was started immediately post-operatively, with a protocol of rehabilitation exercises for ROM, strength, endurance, balance and co-ordination. The intensity of the protocol was gradually increased, as tolerated by the patient, and carefully monitored by the physiotherapist. Patients were prescribed non-steroidal anti-inflammatory medication, such as 50 mg × 3 of diclofenac daily for 1-month post-operatively, in order to minimize the risk of heterotopic ossification. Antibiotic prophylaxis was not routinely used.
The surgical procedure was individualized, depending on the intra-operative findings. This calls for high diagnostic accuracy. The identification of the cause of pain is demanding and necessitates a careful evaluation of patient history, clinical findings, radiology and intra-operative findings.
For further information on the performed procedures, see Table II.
Table II.
Arthroscopic procedures performed on 75 patients and a total of 85 hips
| Surgical procedure | Number of hips |
|---|---|
| Isolated CAM | 25 |
| CAM + pincer (combined) | 55 |
| Labral suture | 6 |
| Microfracture | 4 |
| Labral resection | 9 |
| Labral debridement | 19 |
| Os acetabuli | 3 |
| Ossified labrum | 2 |
| Labral calcarea | 1 |
Ethics
Ethical approval for the study was granted by the regional ethical review board in Gothenburg, Sweden (registration number 071‐12).
Statistical analysis
The sample size calculations with an α-value of 0.05, 75 subjects, 10 points as a clinically relevant difference on iHOT12 score (based on data from a previous study) and a SD of difference in the response of matched pairs of 21 points gives a power of >90% [24]. Statistical analysis was performed using the Statistical Package for the Social Sciences (SPSS) (version 20, 2010 SPSS Inc., Chicago, Illinois, USA). Descriptive statistics were used for patient demographics. The data were not normally distributed and non-parametric statistical testing was therefore employed. Wilcoxon’s signed rank test was used to evaluate differences between PROM values used preoperatively with those obtained at follow-up. Differences between patients with a progression of Tönnis grade and those without a progression were evaluated with the Mann-Whitney U-test. Differences between patients with 1–2 mm of any joint space and those with 3 mm or more were evaluated with the Mann-Whitney U-test. Differences in terms of medial, central and lateral joint space from pre- to post-operative radiographs were evaluated with the Mann-Whitney U-test. The level of statistical significance was set at P < 0.05.
RESULTS
The patients’ mean age was 47 years (SD 10). First follow-up was first made at an average of 12.8 months (SD 1.7), including radiographs, where all 71 available patients responded (four had underwent THA and did not report PROM). Second follow-up was made at an average of 26 months (SD 5), where 68 patients responded (97%) and at this time point, a total of five patients had undergone THA and did not report PROM. The average time to follow-up was 12.8 months (SD 1.7). The reported average time of symptom duration prior to surgery was 5.8 years (SD 5.7).
Of the included procedures (Table II), 28 were isolated cam resections and 57 were combined cam and pincer resections. The labrum was sutured in six hips and a microfracture was performed in four hips.
A comparison of preoperative scores compared with those obtained at the 24-month follow-up revealed improvements (P < 0.0001) for all measured outcomes; the iHOT-12 (42 versus 65), VAS for global hip function (48 versus 68), HSAS (2.5 versus 3), EQ5D index (0.62 versus 0.76), EQ VAS (69 versus 75) and different HAGOS subscales (54 versus 72, 47 versus 67, 56 versus 75, 40 versus 61, 33 versus 56, 31 versus 55) (Table III).
Table III.
Mean and SD for the outcome scores for the entire group preoperatively and at the 12/24-month follow-up
| Outcome | Preoperative (n = 75) | 12 months (n = 71) | Change (Δ) | 24 months (n = 68) | Change (Δ) | P-value |
|---|---|---|---|---|---|---|
| iHOT-12 | 42 (18) | 61 (25) | 19 | 65 (27) | 23 | <0.0001 |
| Mean (SD) | ||||||
| EQ-5D | 0.62 (25) | 77 (15) | 0.13 | 0.76 (23) | 0.14 | <0.0001 |
| Mean (SD) | ||||||
| EQ-VASMean (SD) | 69 (15) | 76 (17) | 7 | 75 (20) | 6 | <0.001 |
| HAGOS–pain | 54 (19) | 72 (18) | 18 | 72 (22) | 18 | <0.0001 |
| Mean (SD) | ||||||
| HAGOS–symptoms | 47 (19) | 66 (17) | 19 | 67 (23) | 20 | <0.0001 |
| Mean (SD) | ||||||
| HAGOS–daily activity | 56 (23) | 75 (19) | 19 | 75 (23) | 19 | <0.0001 |
| Mean (SD) | ||||||
| HAGOS–sports | 40 (21) | 58 (26) | 18 | 61 (30) | 21 | <0.0001 |
| Mean (SD) | ||||||
| HAGOS–physical activity | 33 (26) | 52 (34) | 19 | 56 (33) | 23 | <0.0001 |
| Mean (SD) | ||||||
| HAGOS–quality of life | 31 (16) | 54 (25) | 23 | 55 (28) | 24 | <0.0001 |
| Mean (SD) | ||||||
| VAS–overall hip function | 48 (21) | 67 (22) | 19 | 68 (25) | 20 | <0.0001 |
| Mean (SD) | ||||||
| HSAS | 2.5 (2.2) | 3.1 (1.8) | 0.6 | 3 (1.6) | 0.5 | <0.005 |
| Mean (SD) | ||||||
| Satisfied with surgery | NA | 83 (%) | NA | 82% | NA | NA |
| n (%) | ||||||
| Undergone THA | NA | 4 (5%) | NA | 5 (7%) | NA | NA |
In total, 56 of 68 (82%) patients reported that they were satisfied with the outcome of the surgery. Ten patients (14%) reported dissatisfaction.
Ten re-operations (13%) were performed during follow-up, of which one was a fascia lata release. In total 5 of 75 (7%) patients had undergone or were planned for a THA at the 2-year follow-up.
The mean alpha angle preoperatively was 74 degrees (SD 12), as compared with 46 (SD 9) degrees post-operatively (P < 0.05). See Table IV for all radiographic measurements.
Table IV.
Radiographic evaluation
| Measurement | Preoperative | 12-month Post-operative |
|---|---|---|
| Alpha angle (degrees) | 74 (SD 12) | 46 (SD 9) |
| CE angle (SD) degrees | 32 (7) | NA |
| Tönnis grade 1 (no) | 48 | 41 |
| Tönnis grade 2 (no) | 31 | 34 |
| Tönnis grade 3 (no) | 0 | 1 |
| Tönnis progression grade 1 to 2 | NA | 7 |
| Tönnis progression grade 2 to 3 | NA | 2 |
| Tönnis progression grade 1 to 3 | NA | 1 |
| Any joint space of 1 (mm) | 3 | 10 |
| Any joint space of 2 (mm) | 17 | 14 |
| Any joint space of 3+ (mm) | 57 | 52 |
At follow-up, when comparing medial, central and lateral joint space, only the lateral space decreased to a statistically significant degree (P < 0.05) from a mean of 3.6 mm (SD 1.2, median 4, range 1–6) to 3.2 mm (SD 1.3, median 4, range 0–6).
At follow-up, the PROMs did not differ significantly in patients with any joint space of 1–2 mm compared with those with any joint space of 3+ mm. However, all four patients who received or were planned to receive a THA had a joint space of 2 mm or less in at least one of the three measurement sites. The intraclass correlation coefficient, (two-way mixed-effects model absolute agreement) was calculated in terms of the Tönnis score pre- and post-operatively and was found to be 0.9.
At follow-up, there were no significant differences in PROM results in terms of Tönnis grade progression versus no progression (n = 10, 13% versus n = 75, 87%).
DISCUSSION
The most important finding in this study was that the arthroscopic treatment of patients with FAI with mild to moderate OA showed significant improvements in all outcome measurements at the 2-year follow-up. No significant differences were found in terms of PROMs between 1- and 2-year follow-up.
In two studies, Philippon et al. report on the outcome of the arthroscopic treatment of FAI and reveal that patients improve in terms of PROMs, but that they had an increased rate of conversion to THA with any joint space of 2 mm or less. They reported a THA conversion rate of 9 and 20%, respectively [20, 21].
In 2014, Gicquel et al. [22] reported on 53 hips treated arthroscopically for FAI. Patients with Tönnis grade 1 hips had lower satisfaction rates and a higher conversion rate to THA than patients with Tönnis grade 0.
In a systematic review by Kemp et al., it is concluded that patients with hip OA report positive outcomes from hip arthroscopy. Patients with hip OA had inferior outcomes compared with those with no hip OA. The severity of chondropathy and higher patient age were associated with a higher risk and more rapid progression to THA.
The multitude and type of outcome measures in this study is a major strength. Previous studies have mainly used older scores that are not validated for this young, active patient category [14]. The iHOT-12, HAGOS and HSAS are modern, validated scores, developed to study patients with hip symptoms [26, 30, 31]. The EQ-5D is a valid and reliable quality-of-life score, which is commonly used. It would be valuable if future studies used the same validated outcome measures in similar study populations in order to be able to compare results.
In this study, significant (P < 0.005) improvements were found for all PROMs that were used. Most preoperative values, such as the iHOT-12, HAGOS sports and HAGOS physical activity, are low, reflecting that patients in the studied cohort had major pre-operative symptoms and disability. Coupled with long symptom duration in many patients, this could affect the result negatively.
In this study, patients with mild to moderate OA (Tönnis grades 1 or 2) benefited from the arthroscopic treatment of FAI. No statistically significant difference in outcomes was seen when the group with 1–2 mm of joint space width was compared with patients with 3+ mm joint space widths. However, the group size (n = 16) may be too small to enable any definitive conclusions.
In this study, lateral joint space was reduced, when comparing pre- and post-operative radiographs, from 3.6 to 3.2 mm (P < 0.05). Given the findings of reduction of lateral joint space between the pre- and post-operative time points, it is important to understand whether the surgery itself contributed to this finding, or if it is related to the natural history of the disease or possibly measurent error. Future studies comparing matched groups who undergo surgery to those who don’t are needed to answer this question. Osteophytes can theoretically be seen as the body’s own attempt to fuse the joint in order to reduce symptoms. With increased joint motion, cartilage stress and wear could increase. Likewise, patients with fewer symptoms can perform at a higher level of physical activity, which may increase cartilage wear. On the other hand, cartilage benefits from joint motion and loading [32, 33]. In this study, no statistically significant changes in PROMs were seen in the group with reduced lateral joint space post-operatively. It is important to monitor the patients in this study with a longer follow-up.
Five patients (7%) underwent THA during follow-up. This is a low rate compared with other similar studies, especially since many of the patients were at an age where THA could be considered a primary treatment option considering the amount of symptoms the patients reported preoperatively [34].
It can be discussed whether the end PROM level, 65 points in terms of iHOT-12 and 55–75 in terms of HAGOS subscales, is a good result, even if significant improvement were reported. Unfortunately, there is little data describing the normal values for this population. We conclude that further studies with longer follow-up on this population can further enhance our knowledge.
The limitations of this study are the non-randomized study design, the somewhat limited sample size, patients lost to follow-up and the lack of a control group. Longer follow-up would be of interest in this cohort as OA can progress and affect the long-term result.
In the registry that this study is based on, we routinely record cartilage status using the classification by Konan et al. [35]. Because this classification is not validated for OA, we did not present data on intraoperative findings in this study.
On the other hand, prospective register studies, like this study, describe the actual outcome without selection bias, which increases the external validity of the results. Strength of this study is the multitude of outcome measures that have been validated for a young, active population.
Taken together, arthroscopic treatment appears to be favourable in this group of patients and, with further development of diagnostic, surgical and rehabilitation procedures, the results could possibly improve even more. Moreover, the PROMs used in this study could be further investigated in order to improve validity.
CONCLUSION
Arthroscopic treatment for FAI in patients with concomitant mild to moderate OA resulted in statistically significant and clinically relevant improvements in all outcomes for pain, symptoms, function, physical activity level and quality of life.
FUNDING
This work was financially supported by the Swedish National Centre for Research in Sports.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- 1.Ganz R, Parvizi J, Beck M, et al. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res 2003; 417: 112–20. [DOI] [PubMed] [Google Scholar]
- 2.Beck M, Kalhor M, Leunig M, et al. Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br 2005; 87: 1012–8. [DOI] [PubMed] [Google Scholar]
- 3.Kohl S, Hosalkar HS, Mainil-Varlet P, et al. Histology of damaged acetabular cartilage in symptomatic femoroacetabular impingement: an observational analysis. Hip Int 2011; 21: 154–62. [DOI] [PubMed] [Google Scholar]
- 4.Stulberg SD, Cooperman DR, Wallensten R. The natural history of Legg-Calve-Perthes disease. J Bone Joint Surg Am 1981; 63: 1095–108. [PubMed] [Google Scholar]
- 5.Ganz R, Leunig M, Leunig-Ganz K, et al. The etiology of osteoarthritis of the hip: an integrated mechanical concept. Clin Orthop Relat Res 2008; 466: 264–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Notzli HP, Wyss TF, Stoecklin CH, et al. The contour of the femoral head-neck junction as a predictor for the risk of anterior impingement. J Bone Joint Surg Br 2002; 84: 556–60. [DOI] [PubMed] [Google Scholar]
- 7.Agricola R, Bessems JH, Ginai AZ, et al. The development of Cam-type deformity in adolescent and young male soccer players. Am J Sports Med 2012; 40: 1099–106. [DOI] [PubMed] [Google Scholar]
- 8.Tak I, Weir A, Langhout R, et al. The relationship between the frequency of football practice during skeletal growth and the presence of a cam deformity in adult elite football players. Br J Sports Med 2015; 49: 630–4. [DOI] [PubMed] [Google Scholar]
- 9.Tveit M, Rosengren BE, Nilsson JA, et al. Former male elite athletes have a higher prevalence of osteoarthritis and arthroplasty in the hip and knee than expected. Am J Sports Med 2012; 40: 527–33. [DOI] [PubMed] [Google Scholar]
- 10.Siebenrock KA, Ferner F, Noble PC, et al. The cam-type deformity of the proximal femur arises in childhood in response to vigorous sporting activity. Clin Orthop Relat Res 2011; 469: 3229–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Domb BG, Jackson TJ, Carter CC, et al. Magnetic resonance imaging findings in the symptomatic hips of younger retired national football league players. Am J Sports Med 2014; 42: 1704–9. [DOI] [PubMed] [Google Scholar]
- 12.Ng VY, Arora N, Best TM, et al. Efficacy of surgery for femoroacetabular impingement: a systematic review. Am J Sports Med 2010; 38: 2337–45. [DOI] [PubMed] [Google Scholar]
- 13.Alradwan H, Philippon MJ, Farrokhyar F, et al. Return to preinjury activity levels after surgical management of femoroacetabular impingement in athletes. Arthroscopy 2012; 28: 1567–76. [DOI] [PubMed] [Google Scholar]
- 14.Harris JD, Erickson BJ, Bush-Joseph CA, et al. Treatment of femoroacetabular impingement: a systematic review. Curr Rev Musculoskelet Med 2013; 6: 207–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Egerton T, Hinman RS, Takla A, et al. Intraoperative cartilage degeneration predicts outcome 12 months after hip arthroscopy. Clin Orthop Relat Res 2013; 471: 593–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Haviv B, O’Donnell J. The incidence of total hip arthroplasty after hip arthroscopy in osteoarthritic patients. Sports Med Arthrosc Rehab Ther Technol 2010; 2: 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kemp JL, MacDonald D, Collins NJ, et al. Hip arthroscopy in the setting of hip osteoarthritis: systematic review of outcomes and progression to hip arthroplasty. Clin Orthop Relat Res 2015; 473: 1055–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Daivajna S, Bajwa A, Villar R. Outcome of arthroscopy in patients with advanced osteoarthritis of the hip. PLoS One 2015; 10: e0113970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McCormick F, Nwachukwu BU, Alpaugh K, et al. Predictors of hip arthroscopy outcomes for labral tears at minimum 2-year follow-up: the influence of age and arthritis. Arthroscopy 2012; 28: 1359–64. [DOI] [PubMed] [Google Scholar]
- 20.Philippon MJ, Briggs KK, Yen YM, et al. Outcomes following hip arthroscopy for femoroacetabular impingement with associated chondrolabral dysfunction: minimum two-year follow-up. J Bone Joint Surg Br 2009; 91: 16–23. [DOI] [PubMed] [Google Scholar]
- 21.Philippon MJ, Schroder ESBG, Briggs KK. Hip arthroscopy for femoroacetabular impingement in patients aged 50 years or older. Arthroscopy 2012; 28: 59–65. [DOI] [PubMed] [Google Scholar]
- 22.Gicquel T, Gedouin JE, Krantz N, et al. Function and osteoarthritis progression after arthroscopic treatment of femoro-acetabular impingement: a prospective study after a mean follow-up of 4.6 (4.2–5.5) years. Orthop Traumatol Surg Res 2014; 100: 651–6. [DOI] [PubMed] [Google Scholar]
- 23.Thomee R, Jonasson P, Thorborg K, et al. Cross-cultural adaptation to Swedish and validation of the Copenhagen Hip and Groin Outcome Score (HAGOS) for pain, symptoms and physical function in patients with hip and groin disability due to femoro-acetabular impingement. Knee Surg Sports Traumatol Arthrosc 2013; 22: 835–42. [DOI] [PubMed] [Google Scholar]
- 24.Jonasson P, Baranto A, Karlsson J, et al. A standardised outcome measure of pain, symptoms and physical function in patients with hip and groin disability due to femoro-acetabular impingement: cross-cultural adaptation and validation of the international Hip Outcome Tool (iHOT12) in Swedish. Knee Surg Sports Traumatol Arthrosc 2014; 22: 826–34. [DOI] [PubMed] [Google Scholar]
- 25.Burstrom K, Johannesson M, Diderichsen F. Swedish population health-related quality of life results using the EQ-5D. Qual Life Res 2001; 10: 621–35. [DOI] [PubMed] [Google Scholar]
- 26.Naal FD, Miozzari HH, Kelly BT, et al. The Hip Sports Activity Scale (HSAS) for patients with femoroacetabular impingement. Hip Int 2013; 23: 204–11. [DOI] [PubMed] [Google Scholar]
- 27.Jonasson P, Baranto A, Karlsson J, et al. A standardised outcome measure of pain, symptoms and physical function in patients with hip and groin disability due to femoro-acetabular impingement: cross-cultural adaptation and validation of the international Hip Outcome Tool (iHOT12) in Swedish. Knee Surg Sports Traumatol Arthrosc 2013; 22: 826–34. [DOI] [PubMed] [Google Scholar]
- 28.Tonnis D, Heinecke A. Acetabular and femoral anteversion: relationship with osteoarthritis of the hip. J Bone Joint Surg Am 1999; 81: 1747–70. [DOI] [PubMed] [Google Scholar]
- 29.Sansone M, Ahldén M, Jonasson P, et al. A Swedish hip arthroscopy registry: demographics and development. Knee Surg Sports Traumatol Arthrosc 2014; 22: 774–80. [DOI] [PubMed] [Google Scholar]
- 30.Griffin DR, Parsons N, Mohtadi NG, et al. A short version of the International Hip Outcome Tool (iHOT-12) for use in routine clinical practice. Arthroscopy 2012; 28: 611–6 quiz 16–8. [DOI] [PubMed] [Google Scholar]
- 31.Thorborg K, Holmich P, Christensen R, et al. The Copenhagen Hip and Groin Outcome Score (HAGOS): development and validation according to the COSMIN checklist. Br J Sports Med 2011; 45: 478–91. [DOI] [PubMed] [Google Scholar]
- 32.Wang Y, Wei L, Zeng L, et al. Nutrition and degeneration of articular cartilage. Knee Surg Sports Traumatol Arthrosc 2013; 21: 1751–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Buckwalter JA, Mankin HJ. Articular cartilage: tissue design and chondrocyte-matrix interactions. Instr Course Lect 1998; 47: 477–86. [PubMed] [Google Scholar]
- 34.Sing DC, Feeley BT, Tay B, et al. Age-related trends in hip arthroscopy: a large cross-sectional analysis. Arthroscopy 2015; pii: S0749–8063. [DOI] [PubMed] [Google Scholar]
- 35.Konan S, Rayan F, Meermans G, et al. Validation of the classification system for acetabular chondral lesions identified at arthroscopy in patients with femoroacetabular impingement. J Bone Joint Surg Br 2011; 93: 332–6. [DOI] [PubMed] [Google Scholar]