Abstract
Groin pain is common in athletes. Yet, there is disagreement on aetiology, pathomechanics and terminology. A plethora of terms have been employed to explain inguinal-related groin pain in athletes. Recently, at the British Hernia Society in Manchester 2012, a consensus was reached to use the term inguinal disruption based on the pathophysiology while lately the Doha agreement in 2014 defined it as inguinal-related groin pain, a clinically based taxonomy.
This review article emphasizes the anatomy, pathogenesis, standard clinical assessment and imaging, and highlights the treatment options for inguinal disruption.
Keywords: Groin pain, sportsman’s hernia, sports hernia, inguinal hernia, sports groin, athletic pubalgia, inguinal disruption
INTRODUCTION
Groin injuries are commonly seen in athletes and account for up to 6% of all athletic injuries [1–3]. Most commonly seen in sports that require repetitive twisting, cutting, rapid acceleration and deceleration movements such as soccer, rugby, ice hockey and Australian Rules football [1, 4, 5]. Significant pain and disability in inguinal region during and after athletic activities have been reported and many terms have been employed for this condition, such as sportsman’s hernia, sports hernia, inguinal hernia, incipient hernia, cryptic hernia, Gilmore’s groin, hockey player’s syndrome, groin pull, sports groin, chronic symphysis syndrome, athletic pubalgia. Recently, a consensus has been achieved to rename this entity as inguinal disruption [6] while lately a clinically based taxonomy defines it as inguinal-related groin pain [7].
The aim of this article is to review the anatomy, pathogenesis, standard clinical assessment, imaging and to highlight the treatment options for inguinal disruption.
ANATOMY
The inguinal region is located on the lower part of the abdominal wall. Its anterior portion (anterior wall) is formed of the internal oblique muscle and the aponeurosis of the external oblique muscle while its posterior wall is made up of the fascia transversalis and the conjoint tendon (common insertion of the internal oblique and transverse abdominus muscles) [8].
Between these two portions runs the inguinal canal, formed by these two walls respectively, with its roof (superior wall) is made up of the internal oblique and transverse abdominus muscles and with its floor (inferior wall) is composed of the inguinal ligament (or Poupart ligament) which is formed from the external oblique aponeurosis as it folds over and inserts from the anterior superior iliac spine to the pubic tubercle [8].
The inguinal canal contains the spermatic cord alongside with the genital branch of the genitofemoral nerve (motor function to the cremaster muscle and sensory to the scrotum) and the ilioinguinal nerve (cutaneous nerve, sensory to the groin) in males and the round ligament, the genital branch of the genitofemoral nerve (sensory to the labia) and the ilioinguinal nerve (cutaneous nerve, sensory to the groin) in females. It is an oblique canal, about 4 cm long and has two openings: the internal (deep) and the external (superficial) inguinal ring [8].
Both rings are larger in men than in females because of the large size of the spermatic cord. The posterior abdominal wall at the inguinal canal is considered weaker in males due to testicular descent from the abdominal cavity to the scrotal cavity during the embryological formation.
THE FUNCTION AND ROLE OF THE ABDOMINAL MUSCLES
Abdominal muscles play a crucial role in core stability and help create a rigid cylinder, enhancing stiffness of the lumbar spine, increase the intra-abdominal pressure and contribute in rotational movements of the trunk and lateral flexion of the spine (external and internal oblique muscles) [9]. The oblique abdominals are activated in direction-specific patterns with respect to limb movements, thus providing postural support before limb movements. The hip and pelvis muscles also support the core stability and due to their large muscular cross-sectional area can generate great forces and power for athletic activities [9, 10].
INGUINAL DISRUPTION
Consensus on definition and pathophysiology
A consensus was reached by experts during the British Hernia Society’s conference in Manchester, UK 2012 [6]. The agreed term, to accurately describe the pain in the inguinal region close to pubic tubercle is inguinal disruption. It is referred as the abnormal tension in the inguinal canal and it is recognised as posterior wall weakness, disruption of the external oblique aponeurosis, external inguinal ring (EIR), conjoint tendon tears and inguinal ligament dehiscence but with no obvious hernia. It is seen in very active sports persons and may have an acute or insidious onset. The diagnosis can be made if at least three out of the five clinical signs are present (Table I).
Table I.
Clinical signs for detecting inguinal disruption; at least three out of five symptoms must be present
| Inguinal disruption based on the Manchester Consensus statement | |
|---|---|
| 1 | Pinpoint tenderness over the pubic tubercle at the point of insertion of the conjoint tendon |
| 2 | Palpable tenderness over the deep inguinal ring |
| 3 | Pain and/or dilation of the external ring with no obvious hernia evident |
| 4 | Pain at the origin of the adductor longus tendon |
| 5 | Dull, diffuse pain in the groin, often radiating to the perineum and inner thigh or across the midline |
Consensus on definition based on the anatomical area of the condition
International experts on groin and hip problems in athletes gathered in one-day meeting in Doha, Qatar 2014 in an attempt to agree on definitions in groin pain in athletes [7]. Consensus was accomplished to refer to as inguinal-related groin pain and it was a taxonomy based only on history and physical examination findings. However, the experts recognized that currently there is no gold standard for history, examination and imaging and moreover little is known on the reliability of examination of the inguinal region.
Epidemiology
Groin injuries have been reported to account for approximately 6.2% of sports injuries [1–3] but the actual incidence has been underestimated due to the difficult diagnosis and confusing injury definitions. Meyers et al. [11] reported 5460 operations in groin area, of which 82.8% of patients were considered athletes. Athletic activities that involve kicking, twisting, cutting and rapid acceleration and deceleration movements often lead to groin pain. Most commonly seen in soccer, rugby, ice and field hockey, Australian Rules football, middle distance running and may represent 5–7% of all injuries [5, 12, 13], whereas in male soccer ranges from 10 to 18% annually [14]. Inguinal-related injuries can be present in a variety of age groups and although there are several reports in women, it is almost exclusively present in men [15].
Aetiology
The aetiology varies widely in the literature. It is defined as a bulge or weakness of the posterior wall of the inguinal canal without the presence of a true hernia [2, 15, 16], which widens the inguinal canal, compresses the genital branch of the genitofemoral nerve and forces the rectus abdominus muscle to retract cranially and medially [17].
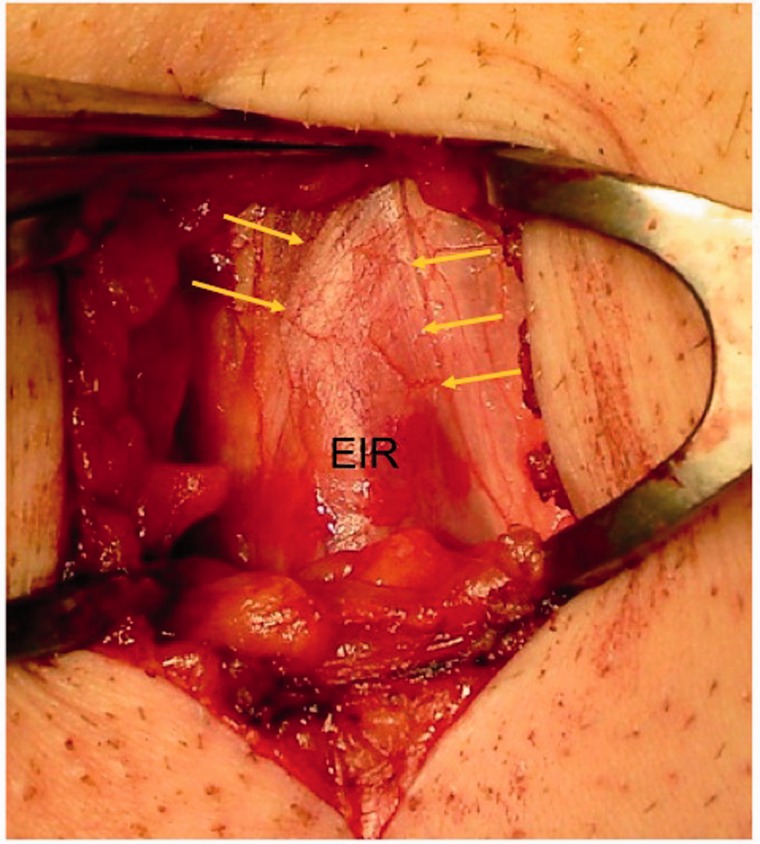
Other causes that can dilate or weaken the inguinal wall or ring include pelvic instability [18], generalized weakness of the pelvic floor including dehiscence between the conjoint tendon-inguinal ligament, attenuation of external oblique aponeurosis (Fig. 1), tearing of conjoined tendon, thin or torn rectus abdominus insertion and a thin or torn internal oblique [11, 19–21]. Anterior inguinal wall defects have also been identified in athletes with chronic groin pain [19, 22].
Fig 1.
The arrows show the disruption of the external oblique aponeurosis with dilation of EIR.
Mechanism of injury
Inguinal disruption may develop from overuse, increased shear forces across the pelvis, trunk and leg, coordination imbalances, loss of dynamic abdominal wall rotational stability or congenital inguinal wall weakness [4, 23]. Excessive shear forces across the pubic symphysis from the stronger hip adductor muscles—pulling down—against a weaker lower abdominal musculature (the conjoined tendon)—pulling up and rotating the trunk—may cause a disruption of the fascia transversalis and or conjoined tendon [1, 24]. Restricted hip range of movements (abduction, external and internal rotations) [25–27], reduced muscle strength endurance [28], extensibility and coordination imbalances may increase the stress in inguinal region leading to attenuation or tearing of the fascia transversalis, conjoined tendon [29] and dilation of the inguinal rings [29, 30]. It has been suggested that when the hip is in 90 degrees of flexion, adduction and internal rotation (anterior impingement test for femoroacetabular impingement [FAI]) there is increased rotation at the symphysis pubis initiating the inguinal disruption [31].
Less frequently, a sudden forceful movement may cause a tear of the abdominal fascia [32]. External oblique aponeurosis defects have also been reported to lead to a painful ilioinguinal nerve entrapment [33].
Balduini et al. [34] explained that the inguinal pain radiates to the scrotum because the cremaster and spermatic fascia are formed by the internal and external oblique muscles.
DIAGNOSIS OF INJURY
Clinical presentation
The diagnosis is based on patient’s history and clinical examination. The onset may be sudden but most often is insidious, present for several months with the athletes complain of a dull, diffuse ache in their groin. The pain is usually unilateral, sharp or burning in nature and radiates to lower abdomen, proximal thigh, low back, perineum or scrotum [17, 18, 21]. It is exacerbated by athletic activities like sprinting/running, kicking/striking a ball, cutting/twisting, sit-ups, side-stepping [17]. Coughing, sneezing or other Valsava-type manoeuvres may worsen the pain. Getting out of bed can be painful but rarely wake up patients from sleep as it is activity-related pain and relieved by rest [17].
In early stages, the pain occurs after sports but later can become so intense that athletes are impaired or disabled from training or performing their sport.
Physical examination
Thorough examination of the groin and hip should be performed. Inspection of an obvious bulge in the inguinal area may expose a true inguinal or femoral hernia. Palpation over the pubic tubercle, conjoined tendon, medial inguinal canal, insertion of rectus abdominus or adductor origin may reveal pain or tenderness [17, 30, 35]. A dilated external inguinal ring or weak inguinal floor can be diagnosed through scrotal invagination but no hernia is palpated during coughing or sneezing (Valsava manoeuvre) [17, 35–37].
Discomfort can be elicited with resisted sit-ups and resisted hip adduction (adductor squeeze test). Examination of the hip can reveal a decreased range of movements (internal and external rotation) and anterior impingement test may be positive [26]. Reduced strength of adductor/abductor has also been noticed.
Differential diagnosis
Because of the close proximity of numerous anatomical structures there is a strong likelihood of co-existing pathologies including muscle injuries, hip pathologies, low back problems, nerve entrapments, intestinal, genitourinary and gynaecological pathologies (Table II) [17, 35].
Table II.
Differential diagnosis of inguinal disruption
| Other pathologies | |
|---|---|
| Orthopaedic | Muscle injuries (adductors strain/avulsion, distal rectus abdominus strain/avulsion, iliopsoas strain) |
| Hip problems (FAI, intra-articular injuries, degenerative changes) | |
| Osteitis pubis/athletic pubalgia | |
| Stress fracture (pubic ramus, femoral neck) | |
| Nerve entrapment, irritation, low back pain | |
| Genitourinary | Prostatitis, epididymitis |
| Hydrocele, varicocele | |
| Urinary tract infections | |
| Gynecological | Endometriosis |
| Menstrual pain | |
| Urinary tract infections | |
| Intestinal | Diverticulitis, irritable bowel syndrome, adhesions, appendicitis |
Imaging assessment
Imaging studies are necessary to rule out other diagnoses. Plain radiographs may reveal FAI, degenerative changes and fractures or avulsions of the hip, spine and sacroiliac joints [38, 39]. Osteitis pubis can be diagnosed from the irregular periosteal changes, sclerosis and symphyseal widening [38, 39]. Abnormal isotope uptake in bone scans can be evident in infection, stress fractures or osteitis pubis [38].
Magnetic resonance imaging (MRI) with or without contrast can show osteitis pubis (fluid in symphysis), bone marrow oedema, stress fractures, avascular necrosis and transient osteoporosis of the femoral head, intra-articular hip pathologies and tendon injuries [39–41]. In an MRI study [42], subtle abnormalities in the musculofascial layers of the abdominal wall similar to inguinal disruption have been reported.
Dynamic ultrasound can be valuable in detecting the defect of posterior inguinal wall during Valsava manoeuvres [43, 44] and the size of the defect can be measured (∼2 cm) [45]. Herniography, an invasive technique injecting a contrast medium into the peritoneal cavity and taking fluoroscopic views after the patient performs Valsava-type manoeuvres, is positive when abnormal contrast flows outside of the peritoneum [46, 47]. Its use is still debatable as the complications rate from 3 to 6% [48, 49].
TREATMENT
The initial treatment consists of activity modification with 6–8 weeks of rest, anti-inflammatory medication and physical therapy with core strengthening and stretching exercises. Ultrasound treatment, electrical stimulation, ice, deep massage with soft-tissues mobilization may be helpful [29, 50, 51]. An active programme to improve muscular strength, endurance, balance and coordination of trunk and hip stabilizing muscles has been proved to be more effective [52]. Gradually the patient is allowed to perform sport-specific exercises and at ∼10–12 weeks when patient is pain-free may return to sports [30].
Occasionally therapeutic injections of corticosteroids can be considered in-season in competitive athletes particularly when adductor longus pathology co-exists [53, 54]. Radiofrequency denervation of the ilioinguinal nerve and inguinal ligament has also provided some short-term benefit [55]. Regenerative injections with platelet rich plasma, prolotherapy, Traumeel, stem cells that aim to stimulate the body to repair itself from damage have been engaged but there is minimal-to-no scientific literature supporting these injections [46, 56].
Surgical exploration and repair should be considered when non-operative treatment failed to improve patient’s symptoms or an athlete fails to make progress. An open or laparoscopic approach has been employed and can be effective with similar results: 62.5–100% (mean 92.8%) and 93–100% (mean 96%), respectively [21]. On a systematic literature review [21] was reported that on average 35% of open and 100% of laparoscopic procedures used mesh. Most patients return to their previous athletic activities but the only decisive factor for surgical success is the return to sport, which cannot determine the efficacy of the treatment.
A wide variety of open repair techniques are described to reinforce the posterior wall of the inguinal canal with [32, 51, 57, 58] or without a mesh [2, 11, 19, 45, 59, 60]. Inguinal ligament tenolysis (release of the abnormal tension in the inguinal canal) open or laparoscopically [61], simultaneous percutaneous adductor tenotomy [11, 26, 27, 59, 62], excision of the ilioinguinal nerve [63, 64], resection of the compressed genital branch of the genitofemoral nerve [45] have also been undertaken. When symptomatic FAI is present surgery undertaken of both entities, inguinal disruption and FAI resulted in return to play athletes from 85 to 93% but isolated management of either inguinal disruption or FAI led a return to sports 25 and 50%, respectively [26].
Laparoscopic approaches involve a totally extraperitoneal [16, 65–67] or transabdominal pre-peritoneal technique [22, 65, 68] and also attempt to support the posterior wall. A quicker return to sporting activity (1–3 months) has been reported with this surgical approach than with the open approach (3-6 months). However, a higher recurrence rate (10.1%) compared with an open repaired with mesh (4.9%) has been reported and this may be explained due to incomplete repair of the disruption caused by restricted visualization during operation [69].
Therefore, it is still debatable which operative approach is more effective. A functional rehabilitation programme should be designed to suit the specific demands of the sport/occupation allowing athletes to return to sports in 4–8 weeks post-operatively.
FUTURE RESEARCH
An attempt to communicate effectively by using the proper terms has already been started. Emphasis should be given to the different pathologies of the groin with similar symptoms that may co-exist, to their close relationship and with future studies on epidemiology of these entities separately.
Further research is needed with prospective randomized-controlled studies to compare both open and laparoscopic techniques, the effectiveness of mesh and therefore to establish the true efficacy of the operations in order to better define the optimal treatment. More studies to assess the role and value of regenerative injections.
A well-structured exercise programme specific for inguinal disruption should be developed followed by randomized-controlled studies to compare it with operative treatment as would have led fewer athletes requiring surgery. Protocols for prevention and for treatment should be recommended and specific outcome scoring tools should be established.
CONCLUSION
The anatomy and physiology of the groin is complex. Understanding the pathophysiology is a key to success. The focus should be based on basic anatomy and biomechanical inter-relationships between the different structures. A multi-disciplinary approach for the pathologies of the groin area may optimize the outcomes.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- 1.Anderson K, Strickland SM, Warren R. Hip and groin injuries in athletes. Am J Sports Med 2001; 29: 521–33. [DOI] [PubMed] [Google Scholar]
- 2.Malycha P, Lovell G. Inguinal surgery in athletes with chronic groin pain: sportsmans’ hernia. Aust NZ J Surg 1992; 62: 123–5. [DOI] [PubMed] [Google Scholar]
- 3.Lovell G. The diagnosis of chronic groin pain in athletes: a review of 189 cases. Aust J Sci Med Sport 1995; 27: 76–9. [PubMed] [Google Scholar]
- 4.Morelli V, Weaver V. Groin injuries and groin pain in athletes. Part 1. Prim Care 2005; 32: 163–83. [DOI] [PubMed] [Google Scholar]
- 5.Verrall GM, Slavotinek JP, Fon GT. et al. Outcome of conservative management of athletic chronic groin injury diagnosed as pubic bone stress injury. Am J Sports Med 2007; 35: 467–74. [DOI] [PubMed] [Google Scholar]
- 6.Sheen AJ, Stephenson BM, Lloyd DM. et al. Treatment of the sportsman’s groin: British Hernia Society’s 2014 position statement based on the Manchester Consensus Conference. Br J Sports Med 2014; 48: 1079–87. [DOI] [PubMed] [Google Scholar]
- 7.Weir A, Brukner P, Delahunt E. et al. Doha agreement meeting on terminology and definitions in groin pain in athletes. Br J Sports Med 2015; 49: 768–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Drake RL, Vogl AW, Mitchell AWM. Gray’s Anatomy for Students. 2nd edn. Philadelphia, PA: Churchill-Livingstone, 2009, 282–6. [Google Scholar]
- 9.Kibler WB, Press J, Sciascia A. The role of core stability in athletic function. Sports Med 2006; 36: 189–98. [DOI] [PubMed] [Google Scholar]
- 10.Ng JK, Parnianpour M, Richardson CA. et al. Functional roles of abdominal and back muscles during isometric axial rotation of the trunk. J Orthop Res 2001; 19: 463–71. [DOI] [PubMed] [Google Scholar]
- 11.Meyers WC, McKechnie A, Philippon MJ. et al. Experience with “sports hernia” spanning two decades. Ann Surg 2008; 248: 656–65. [DOI] [PubMed] [Google Scholar]
- 12.Holmich P, Thorborg K, Dehlendorff C. et al. Incidence and clinical presentation of groin injuries in sub-elite male soccer. Br J Sports Med 2014; 48: 1245–50. [DOI] [PubMed] [Google Scholar]
- 13.Emery CA, Meeuwisse WH, Powell GW. Groin and abdominal strain injuries in the national hockey league. Clin J Sort Med 1999; 9: 151–6. [DOI] [PubMed] [Google Scholar]
- 14.Ekstrand J, Hilding J. The incidence and differential diagnosis of acute groin injuries in male soccer players. Scand J Med Sci Sports 1999; 9: 98–103. [DOI] [PubMed] [Google Scholar]
- 15.Moeller JL. Sportsman’s hernia. Curr Sports Med Rep 2007; 6: 111–4. [DOI] [PubMed] [Google Scholar]
- 16.Genitsaris M, Goulimaris I, Sikas N. Laparoscopic repair of groin pain in athletes. Am J Sports Med 2004; 32: 1238–42. [DOI] [PubMed] [Google Scholar]
- 17.Minnich JM, Hanks JB, Muschaweck U. et al. Sports hernia. Diagnosis and treatment highlighting a minimal repair surgical technique. Am J Sports Med 2011; 399: 1341–9. [DOI] [PubMed] [Google Scholar]
- 18.Garvey JF, Read JW, Turner A. Sportsman hernia: what can we do? Hernia 2010; 14: 17–25. [DOI] [PubMed] [Google Scholar]
- 19.Gilmore OJ. Gilmore’s groin: ten years experience of groin disruption-a previously unsolved problem in sportsmen. Sports Med Soft Tissue Trauma 1991; 3: 12–4. [Google Scholar]
- 20.Farber AJ, Wilckens JH. Sports hernia: diagnosis and therapeutic approach. J Am Acad Orthop Surg 2007; 15: 507–14. [DOI] [PubMed] [Google Scholar]
- 21.Caudill PH, Nyland JA, Smith CE. et al. Sports hernias: a systematic literature review. Br J Sports Med 2008; 42: 954–64. [DOI] [PubMed] [Google Scholar]
- 22.Azurin DJ, Go LS, Schuricht A. et al. Endoscopic pre peritoneal herniorraphy in professional athletes with groin pain. J Laparoendosc Adv Surg Tech A 1997; 7: 7–12. [DOI] [PubMed] [Google Scholar]
- 23.Macintyre J, Johson C, Schroeder EL. Groin pain in athletes. Curr Sports Med Rep 2006; 5: 293–9. [DOI] [PubMed] [Google Scholar]
- 24.Cowan SM, Schache AG, Brukner P. et al. Delayed onset of transverses abdominus in long-standing groin pain. Med Sci Sports Exerc 2004; 36: 2040–5. [DOI] [PubMed] [Google Scholar]
- 25.Schilders E, Dimitrakopoulou A, Cooke M. et al. Effectiveness of a selective partial adductor release for chronic adductor-related groin pain in professional athletes. Am J Sports Med 2013; 41: 603–7. [DOI] [PubMed] [Google Scholar]
- 26.Larson CM, Pierce BR, Giveans MR. Treatment of athletes with symptomatic intra-articular hip pathology and athletic pubalgia/ sports hernia:a case series. Arthroscopy 2011; 27: 768–75. [DOI] [PubMed] [Google Scholar]
- 27.Hammoud S, Bedi A, Magennis E. et al. High incidence of athletic pubalgia symptoms in professional athletes with symptomatic femoroacetabular impingement. Arthroscopy 2012; 28: 1388–95. [DOI] [PubMed] [Google Scholar]
- 28.Verrall GM, Hamilton IA, Slavotinek JP. et al. Hip joint range of motion reduction in sports-related chronic groin injury diagnoses as pubic bone stress injury. J Sci Med Sport 2005; 8: 77–84. [DOI] [PubMed] [Google Scholar]
- 29.Verrall GM, Slavotinek JP, Barnes PG. et al. Hip joint range of motion restriction precedes athletic chronic groin injury. J Sci Med Sport 2007; 10: 463–6. [DOI] [PubMed] [Google Scholar]
- 30.Biedert RM, Warnke K, Meyer SPR. Symphysis syndrome in athletes:surgical treatment for chronic lower abdominal, groin and adductor pain in athletes. Clin J Sport Med 2003; 13: 278–84. [DOI] [PubMed] [Google Scholar]
- 31.Birmingham PM, Kelly BT, Jacobs R. et al. The effect of dynamic femoroacetabular impingement on pubic symphysis motion: a cadaveric study. Am J Sports Med 2012; 40: 1113–8. [DOI] [PubMed] [Google Scholar]
- 32.Irshad K, Feldman LS, Lavoie C. et al. Operative management of “hockey groin syndrome”: 12 years of experience in National Hockey League players. Surg 2001; 130: 759–66. [DOI] [PubMed] [Google Scholar]
- 33.Ziprin P, Williams P, Foster E. External oblique aponeurosis nerve entrapment as a cause of groin pain in the athlete. Br J Surg 1999; 86: 566–8. [DOI] [PubMed] [Google Scholar]
- 34.Balduini FC. Abdominal and groin injuries in tennis. Clin Sports Med 1988; 7: 349–57. [PubMed] [Google Scholar]
- 35.Meyers WC, Yoo E, Devon O. et al. Understanding “sports hernia” (athletic pubalgia) - The anatomic and pathophysiologic basis for abdominal and groin pain in athletes. Oper Tech Sports Med. 2007; 15: 165–77. [Google Scholar]
- 36.Hackney RG. The sports hernia: a cause of chronic groin pain. Br J Sports Med 1993; 27: 58–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Garvey JF1, Hazard H. Sports hernia or groin disruption injury? Chronic athletic groin pain: a retrospective study of 100 patients with long-term follow-up. Hernia 2014; 18: 815–23. [DOI] [PubMed] [Google Scholar]
- 38.Koulouris G. Imaging review of groin pain in elite athletes: an anatomic approach to imaging findings. AJR Am J Roentgenol. 2008; 191: 962–72. [DOI] [PubMed] [Google Scholar]
- 39.Zoga AC, Kavanagh EC, Omar IM. et al. Athletic pubalgia and the “sports hernia”: MR imaging findings. Radiology 2008; 247: 797–807. [DOI] [PubMed] [Google Scholar]
- 40.Paajanen H, Hermunen H, Karonen J. et al. Pubic magnetic resonance imaging findings in surgically and conservatively treated athletes with osteitits pubis compared to asymptomatic athletes during heavy training. Am J Sports Med 2008; 36: 117–21. [DOI] [PubMed] [Google Scholar]
- 41.Khan W, Zoga AC, Meyers WC. Magnetic resonance imaging of athletic pubalgia and the sports hernia: current understanding and practice. Magn Reson Imaging Clin N Am 2013; 21: 97–110. [DOI] [PubMed] [Google Scholar]
- 42.Albers SL, Spritzer CE, Garrett WE. et al. MR findings in athletes with pubalgia. Skeletal Radiol 2001; 30: 270–7. [DOI] [PubMed] [Google Scholar]
- 43.Orchard JW, Read JW, Neophyton J. et al. Groin pain associated with ultrasound finding of inguinal canal posterior wall deficiency in Australian Rules footballers. Br J Sports Med 1998; 32: 134–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Robinson P, Grainger AJ, Hensor EM. et al. Do MRI and ultrasound of the anterior pelvis correlate with, or predict, young football players’ clinical findings? A 4-year prospective study of elite academy soccer players. Br J Sports Med 2015; 49: 176–82. [DOI] [PubMed] [Google Scholar]
- 45.Muschaweck U, Berger LM. Sportsmen’s groin- diagnostic approach and treatment with the minimal repair technique: a single-center uncontrolled clinical review. Sports Health 2010; 2: 216–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Swan KG, Jr, Wolcott M. The athletic hernia. A systematic review. Clin Orthop Relat Res 2007; 455: 78–87. [DOI] [PubMed] [Google Scholar]
- 47.Sutcliffe JR, Taylor OM, Ambrose NS. et al. The use, value and safety of herniography. Clin Radiol 1999; 54: 468–72. [DOI] [PubMed] [Google Scholar]
- 48.Ekberg O. Complications after herniography in adults. AJR Am J Roentgenol 1983; 140: 491–5. [DOI] [PubMed] [Google Scholar]
- 49.Hamlin JA, Kahn AM. Herniography: a review of 333 herniograms. Am Surg 1998; 64: 965–9. [PubMed] [Google Scholar]
- 50.Taylor DC, Meyers WC, Moylan JA. et al. Abdominal musculature abnormalities as a cause of groin pain in athletes: inguinal hernias and pubalgia. Am J Sports Med 1991; 19: 239–42. [DOI] [PubMed] [Google Scholar]
- 51.Steele P, Annear P, Grove JR. Surgery for posterior inguinal wall deficiency in athletes. J Sci Med Sport 2004; 7: 415–21. [DOI] [PubMed] [Google Scholar]
- 52.Hemingway AE, Herrington L, Blower AL. Changes in muscle strength and pain in response to surgical repair of posterior abdominal wall disruption followed by rehabilitation. Br J Sports Med 2003; 37: 54–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Schilders E, Talbot JC, Robinson P, Dimitrakopoulou A. et al. Adductor-related groin pain in recreational athletes: role of adductor enthesis, magnetic resonance imaging, and entheseal pubic cleft injections. J Bone Joint Surg Am 2009; 91: 2455–60. [DOI] [PubMed] [Google Scholar]
- 54.Schilders E, Bismil Q, Robinson P. et al. Adductor-related groin pain in competitive athletes: role of adductor enthesis, magnetic resonance imaging, and entheseal pubic cleft injections. J Bone Joint Surg Am 2007; 89: 2173–8. [DOI] [PubMed] [Google Scholar]
- 55.Comin J, Obaid H, Lammers G. et al. Radiofrequency denervation of the inguinal ligament for the treatment of “sportsman’s hernia”: a pilot study. Br J Sports Med 2013; 47: 380–6. [DOI] [PubMed] [Google Scholar]
- 56.Topol GA, Reeves KD, Hassanein KM. Efficacy of dextrose prolotherapy in elite male kicking-sport athletes with chronic groin pain. Arch Phys Med Rehabil 2005; 86: 697–02. [DOI] [PubMed] [Google Scholar]
- 57.Diaco JF, Diaco DS, Lockhart L. Sports Hernia. Op Tech Sports Med 2005; 13: 68–70. [Google Scholar]
- 58.Edelman DS, Selesnick H. “Sports” hernia: treatment with biologic mesh (Surgisis). Surg Endosc 2006; 20: 971–3. [DOI] [PubMed] [Google Scholar]
- 59.Van Der Donckt K, Steenbrugge F, Van Den Abbeele K. et al. Bassini’s hernial repair and adductor longus tenotomy in the treatment of chronic groin pain in athletes. Acta Orthop Belg 2003; 69: 35–41. [PubMed] [Google Scholar]
- 60.Economopoulos KJ, Milewski MD, Hanks JB, et al. Sports hernia treatment: modified bassini versus minimal repair. Sports Health 2013; 5: 463–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Mann CD, Sutton CD, Garcea G, Lloyd DM. The inguinal release procedure for groin pain: initial experience in 73 sportsmen/women. Br J Sports Med 2009; 43: 579–83. [DOI] [PubMed] [Google Scholar]
- 62.Jans C, Messaoudi N, Pauli S. et al. Results of surgical treatment of athletes with sportsman’s hernia. Acta Orthop Belg 2012; 78: 35–40. [PubMed] [Google Scholar]
- 63.Johner A, Faulds J, Wiseman SM. Planned ilioinguinal nerve excision for prevention of chronic pain after inguinal hernia repair: a meta-analysis. Surgery 2011; 150: 534–41. [DOI] [PubMed] [Google Scholar]
- 64.Malekpour F, Mirhashemi SH, Hajinasrolah E. et al. Ilioinguinal nerve excision in open mesh repair of inguinal hernia-results of a randomized clinical trial: simple solution for difficult problem? Am J Surg 2008; 195: 735–40. [DOI] [PubMed] [Google Scholar]
- 65.Paajanen H, Syvahuoko I, Airo I. Totally extraperitoneal endoscopic (TEP) treatment of sportsman’s hernia. Surg Laparosc Endosc Percutan Tech 2004; 14: 215–8. [DOI] [PubMed] [Google Scholar]
- 66.VanVeen RN, De Baat P, Heijboer MP. et al. Successful endoscopic treatment of chronic groin pain in athletes. Surg Endosc 2007; 21: 189–93. [DOI] [PubMed] [Google Scholar]
- 67.Kluin J, Den Hoed PT, Van Linschoten R. et al. Endoscopic evaluation and treatment of groin pain in the athlete. Am J Sports Med 2004; 32: 944–9. [DOI] [PubMed] [Google Scholar]
- 68.Moldovanu R, Pavy G. Laparoscopic transabdominal pre-peritoneal (TAPP) procedure –step-by-step tips and tricks. Chirurgia 2014; 109: 407–15. [PubMed] [Google Scholar]
- 69.Neumayer L, Giobbie-Hurder A, Jonasson O. et al. Open mesh versus laparoscopic mesh of inguinal hernia. N Eng J Med 2004; 350: 1819–27. [DOI] [PubMed] [Google Scholar]