Abstract
Background
Intensity of therapy is a critical factor influencing outcomes in aphasia. However, there are many barriers to increasing treatment intensity for those with acute/subacute aphasia including the demands of the inpatient medical facilities and the endurance of the participants. Nevertheless, with some modifications to its original procedures, evidence suggests that Constraint Induced Language Therapy (CILT) may yield positive outcomes when given in the early stages of recovery.
Aims
To investigate the feasibility of increasing the amount of therapy provided to individuals with aphasia on an inpatient rehabilitation unit by adding CILT at a modified intensity, and to assess whether those receiving two weeks of the additional CILT show more improvement than control participants who did not receive the additional treatment.
Methods and Procedures
A case-series single-subject design study was conducted. All participants received usual care of approximately an hour of speech and language treatment, five to six days a week. Participants in the experimental condition received an additional hour-long CILT session, five days per week, for two weeks. Trained, untrained, and generalization probes comprising naming of pictured items and oral reading of sentences were taken at baseline, during treatment, and at post-treatment. All participants were probed equally. Probe performance was scored and effect sizes were calculated and compared. Performance gains from pre- to post-treatment on subtests of the Boston Diagnostic Aphasia Examination were also compared.
Outcomes and Results
Thirteen individuals with aphasia onset ranging from 7 to 68 days were recruited, with 6 allocated to the experimental Usual Care + CILT condition and 7 allocated to the control Usual Care condition. Increasing the amount of speech and language therapy by adding an hour of daily CILT was feasible. Individual performance varied within and across conditions with large gains noted in some, but not all participants. As a group, there was a small to medium effect size of the Usual Care + CILT condition over Usual Care alone for trained and untrained oral reading probes and untrained naming probes.
Conclusions
It is feasible to increase the amount of treatment provided to participants with aphasia on an acute inpatient rehabilitation unit. Preliminary results suggest that there may be better outcomes for those who receive more treatment. Further research using larger numbers of homogeneous participants and controlling for content of therapy as well as amount of therapy is warranted.
Keywords: Aphasia, Acute, Rehabilitation, Intensity, Constraint Therapy
A growing body of evidence suggests that intensity of therapy is a critical factor influencing outcomes in aphasia treatment regardless of the treatment approach (Barthel, Meinzer, Djundja, & Rockstroh, 2008; Brady, Kelly, Godwin, & Enderby, 2012; Cherney, 2012; Cherney, Patterson, Raymer, Frymark, & Schooling, 2008). Intensity of treatment has been defined along various dimensions such as the number of repetitions within a task, the length and number of sessions, the period of time across which the intervention is performed, and the workload or effort required by the person (Baker, 2012; Hornby et al., 2011). Presently, no specific intensity recommendations are available for aphasia treatment (Baker, 2012; Cherney, 2012). Indeed, in clinical practice, persons with acute/subacute aphasia receive only a limited amount of therapy. Godecke et al., (2012) noted that the median length of stay across three acute care hospitals in Perth, Australia was 19 days and that the majority of participants in usual care did not receive any therapy during that time. According to a study from Portugal, usual care for individuals with acute/subacute aphasia is two hours per week (Martins et al., 2013). Two hours per week is also reported to be usual care in the UK, but participants in a research study who were enrolled to receive usual care for 12 weeks through the National Health Service in fact only received an average of 0.57 (SD=0.49) hours of therapy per week (Bakheit et al., 2007).
Much of the research regarding treatment intensity has addressed persons with chronic aphasia, with only a few studies targeting those with acute or subacute aphasia. Studies of participants with acute or subacute aphasia have demonstrated inconclusive or equivocal results regarding treatment intensity. For example, Bakheit and colleagues (2007) conducted a prospective randomized controlled trial in a single center, comparing 5 hours of aphasia treatment per week to 2 hours of aphasia treatment per week for 12 consecutive weeks. The average number of days at which treatment was initiated was 28.1 (SD=14.9) for the 46 participants in the 2 hours/week group, and 34.2 (SD=19.1) for the 51 participants in the 5 hours/week group. Treatment typically started in the hospital's rehabilitation unit and continued either in the patient's home or in the outpatient department. In an intent-to-treat analysis, no difference was found between the two groups as measured by the Western Aphasia Battery score. However, by the endpoint of 12 weeks, 16 subjects had withdrawn from the more intensive treatment group whereas 8 subjects had withdrawn from the less intensive group. Furthermore, the authors note that none of the participants randomized to the intensive group received the prescribed amount of therapy, and most of them were not able to tolerate more than 2 hours of therapy per week, especially in the first few weeks after the stroke.
Another study conducted across two centers in Portugal controlled for the number of therapy hours by comparing 100 hours of aphasia therapy provided intensively (2 hours/day, 5 days a week for 10 weeks) versus usual care (2 hours/week for 50 weeks) (Martins et al., 2013). Thirty participants were recruited within 3 months of a left hemisphere ischemic stroke; however, only 17 completed the primary endpoint of the study at 50 weeks. There were several reasons for withdrawal, including transportation difficulties and complications from comorbidities. Although there were no significant differences in outcomes (likely due to the small numbers of participants and insufficient power), the authors note that there was a trend for greater improvement in the intensive group.
These studies illustrate the difficulties of conducting treatment in the acute/subacute period of recovery. Both studies provided treatment over many weeks (ranged from 10 – 50 weeks), and during that time, participants often transitioned across levels of care (e.g. from inpatient to outpatient or home health), making the implementation of the treatment more difficult. In addition, the numbers of participants decreased greatly during the lengthy treatment period. Interpretation of the data is further complicated by difficulties differentiating treatment effects from spontaneous recovery in the more acute phase and the other mechanisms of recovery that may occur as the aphasia becomes more chronic. An intensive treatment that is provided over a shorter period of time while the participant is situated in one location during the acute/subacute recovery period would be easier to implement and to evaluate with regard to outcomes.
Constraint Induced Language Therapy (CILT) is a treatment that incorporates a short period of intensive, massed practice as an integral part of the protocol. In a seminal study on CILT, participants with chronic aphasia received three hours of treatment, five days a week for two weeks (Pulvermuller et al., 2001). Participants, working behind barriers so they were not visible to their communication partner(s), were constrained to use only spoken language to either request or respond to the communication partner's request regarding a pictured object card. The focus of CILT on oral expression is an important feature that differentiates it from usual care where other modalities such as gesture or writing may be targeted. Participants receiving the intensive CILT showed better language outcomes than participants who received the same number of hours of standard therapy distributed over approximately four weeks. Since then, accumulating evidence supports the use of CILT with persons with chronic aphasia (Cherney et al., 2008; Maher et al., 2006; Meinzer, Rodriguez, & Gonzalez Rothi, 2012) with improvements noted on measures of impairment and activity/participation.
The data supporting CILT (also called Constraint Induced Aphasia Therapy or Intensive Language Action Therapy) in persons with acute or subacute aphasia is more limited, in part because of the demands of the inpatient medical facilities and the subsequent practical issues of implementing a research study within their parameters and those of the health care system. In addition, the endurance of the participants is another limiting factor.
Nevertheless, with some modifications to the original procedures of CILT, some investigators have shown positive outcomes from CILT when given in this early stage of recovery. Kirmess and Maher (2010) provided CILT to three individuals with aphasia within 40-60 days post onset (Kirmess & Maher, 2010). Participants were scheduled to receive three hours a day of CILT for ten days (i.e., 30 hours total), with the treatment provided in a small group or one-to-one with a trained speech and language pathologist. The authors note that the intensity of the intervention was one of the challenges in applying the CILT protocol in this setting. Only one of the three participants received the scheduled/planned 30 hours; the others received 20 and 24.5 hours respectively because of issues including participant fatigue and scheduling issues to “accommodate other rehabilitation treatments and medical issues” (p. 728). Although results were positive, there were no control participants who did not receive the CILT and against whom to compare the gains. As noted by the authors, following the end of the CILT protocol, the participants continued with traditional speech therapy, making interpretation of the follow-up results difficult. However, this preliminary study demonstrates the feasibility of applying CILT in a real-world clinical rehabilitation setting.
In a large randomized controlled trial, 100 first-time stroke patients with resultant aphasia were randomized to receive either CILT or standard treatment of the same quantity that targeted several modes of communication (Sickert, Anders, Munte, & Sailer, 2014). Participants were 1-4 months post stroke, with an average duration of 34.8 days. The CILT was provided in a local rehabilitation center and comprised 2 hours of training over 15 days (i.e., 30 hours total). It was administered in a group setting that included 4-6 patients with aphasia, a speech-language pathologist, and two patients without aphasia who served as “co-players with an exemplary function” (p. 52). All participants completed the 30 hours of CILT. The CILT was well tolerated by the participants, demonstrating the feasibility of using a modified CILT in the early subacute phase under real conditions in a rehabilitation center. Both therapies led to significant improvement in language function; although there was no statistical advantage of one type of treatment over the other, those in the CILT group were noted to have a greater increase in the amount of their communication on a communication activity questionnaire. Follow-up assessment on a subgroup of participants was conducted at 8 weeks and one year after the end of treatment. However, since subjects received some outpatient treatment after the end of the CILT protocol, it is difficult to make conclusions about the longer term efficacy of CILT.
Although these studies demonstrate the feasibility of providing a modified intensity of CILT to persons with aphasia, a recent survey of speech-language pathologists practicing in the United States shows that there are many concerns regarding the clinical implementation of CILT (Page & Wallace, 2014). More than 70% of the 167 respondents indicated that their own facilities did not have the appropriate resources to provide CILT, while more than 90% agreed that most facilities likely also lacked such resources. Respondents also indicated their concerns with participant compliance and with reimbursement given the number of hours and the number of consecutive days required for CILT.
In contrast to these concerns, a modified CILT approach in which a single clinician can provide services simultaneously to multiple persons with aphasia may prove feasible for increasing intensity in real-world inpatient settings without placing considerably more demands on therapy resources. The primary purpose of this study sought to investigate the feasibility of implementing CILT at a modified intensity as a way of increasing the amount of therapy provided to individuals with aphasia on an inpatient rehabilitation unit. In addition to feasibility, the following specific questions were addressed for the participants with aphasia in the acute inpatient rehabilitation program:
Do participants receiving a total of ten hours of CILT over two weeks in addition to usual care show improvement on the trained task?
Do participants receiving a total of ten hours of CILT over two weeks in addition to usual care show improvement on a similar untrained task and on a generalization task?
Do participants receiving a total of ten hours of CILT over two weeks in addition to usual care show greater improvement on trained, untrained and generalization tasks than those who receive only usual care?
Do participants receiving a total of ten hours of CILT over two weeks in addition to usual care show greater improvement on standardized measures (i.e. selected subtests of the Boston Diagnostic Aphasia Examination (BDAE) (Goodglass, Kaplan, & Barresi, 2001)) than those who received only usual care?
We anticipated that it would be feasible to provide participants in an inpatient rehabilitation program with an hour of CILT, 5 days a week for two weeks (i.e., for a total of 10 hours), in addition to the usual treatment schedule. We hypothesized that participants receiving an hour of CILT, 5 days a week for two weeks, in addition to their usual speech and language therapy would improve on trained, untrained and generalization tasks, and that these improvements would be greater than the gains made by participants receiving only usual care. We also hypothesized that the participants receiving CILT would show greater gains on standardized measures selected from the BDAE as compared to participants receiving usual care. These hypotheses were based on evidence suggesting that more intensive treatment would benefit participants with acute/subacute aphasia (Godecke et al., 2013; Kirmess & Maher, 2010; Martins et al., 2013).
METHOD
Experimental design
A prospective case-series single-subject experimental design was used to examine the feasibility of adding an additional one-hour session of Constraint Induced Language Therapy (CILT) to the typical daily inpatient therapy schedule. Patients in inpatient rehabilitation routinely receive at least three hours combined of physical, occupational, and/or speech-language treatment (SLT) daily, five to six days per week in accordance with their inpatient plan of care. For this study, participants receiving the experimental condition were provided with an additional ten hours of CILT over a period of two weeks (one hour per day, five days per week for two weeks). The study was approved by the Institutional Review Board (IRB) at Northwestern University and informed consent was obtained from all participants in accordance with the IRB.
Participants
Participants were recruited from consecutive admissions to an urban inpatient rehabilitation hospital. Inclusion criteria included the presence of acute aphasia (i.e. within 3 months of onset) following left hemisphere damage caused by a single stroke or traumatic brain injury. Participants were required to maintain attention for at least 30 minutes with minimal redirection. They also needed to be stimulable for production of novel single words with cueing from the speech-language pathologist. Participants were required to be premorbidly literate in English. Exclusion criteria included: severe aphasia or apraxia of speech precluding production of novel words, even when given maximum cues; the presence of any other neurological condition that could impact cognition or speech (e.g. Parkinson's disease, dementia, multiple sclerosis); or any medical condition that would preclude the participant from sitting for one hour or participating in a session with another participant (e.g. spinal precautions/wounds, active infection requiring isolation, vision/hearing deficits).
Participants who met these criteria were first considered for allocation to the Usual Care + CILT condition. However, if there was no other participant with aphasia on any of the inpatient units meeting criteria and available to serve as a CILT partner during the intervention, the participant was then allocated to receive only usual inpatient speech and language therapy.
Treatment
All participants received usual care. Usual care is typically a one-to-one session that addresses all language modalities including oral expression, auditory comprehension, reading comprehension, and written expression. However, the extent to which treatment emphasizes one or more language modalities depends on the type and severity of each participant's aphasia. The goals, tasks and materials of usual care are individualized to each participant and their functional communication needs. With usual care, participants may have several goals so they may attempt a variety of different tasks within a given 60 minute session. As a result, the number of responses elicited within each task may be limited.
The CILT sessions followed a specific protocol, regardless of the type and severity of the participant's language deficits. CILT sessions were conducted with two participants sitting across from each other with a cardboard barrier placed between them so that neither was visible to the other. The barrier served to preclude participants from using nonverbal strategies (e.g. gesture) to communicate their message during the CILT exchanges. A speech-language pathologist facilitated a language activity in which participants verbally requested and responded to requests for pictured items from a set of 25 household tools, created with Google Images. During each treatment session, the speech-language pathologist randomly drew pictured items from this set to serve as stimuli. Items are listed in the appendix. Verbal targets, as described in Maher (2006), were the following, with a tool item inserted:
Request: John (partner's name), do you have a _____________?
Response: Yes, Mark (partner's name). I have a _________________________.
The speech-language pathologist used various cuing strategies to assist participants in achieving accurate productions including choral reading and written, semantic, and phonemic cues.
Data collection and analysis
Probes
Probes included naming of pictured items and oral reading of sentences. Baseline probes were taken on at least three consecutive days prior to beginning the intervention; treatment probes were taken three times per week during the two-week intervention phase; final probes were taken on three consecutive days following the end of the intervention. Control participants who did not receive the additional CILT sessions were probed the same number of times as the experimental participants. Trained naming probes consisted of five items selected randomly from the set of household tools that were practiced during CILT (n = 25). Untrained naming probes consisted of five items randomly selected from a set of furniture (n = 25) and five items randomly selected from a set of clothing (n = 25); all items were selected from Google Images. Oral reading sentence probes consisted of five sentences each, randomly selected from a set of trained sentences, untrained sentences, and generalization sentences (25 per type). Trained sentences were the same sentences used for requesting during the CILT sessions (i.e. John, do you have a __________?) with an item from the household tool set inserted. Untrained sentences also used the requesting sentence from CILT, but inserted an item from the untrained clothing set. Generalization sentences were unrelated grammatically to the CILT sentences and used an untrained item from the furniture set (e.g., He fell asleep on the couch). All sentences were matched for number of words. Naming and sentence probe stimuli are included in the appendix.
Probe performance was scored by the first author from audio and/or videotapes. Each word produced during the probes was scored using the Naming and Oral Reading for Language in Aphasia (NORLA-6) scale (Gingrich, Hurwitz, Lee, Carpenter, & Cherney, 2013). The scale ranges from 0 (no response) and 1 (unintelligible or unrelated response) to 4 (accurate but delayed or self-corrected response) and 5 (accurate and immediate response). Semantic or phonological paraphasias are scored as 2, while appropriate and intelligible responses with minor errors such as the omission of a grammatical morpheme are scored as 3. The NORLA-6 has previously demonstrated evidence supporting its validity and reliability (Gingrich et al., 2013). Percent accuracy, the dependent variable, was the NORLA-6 score of each item as a percent of the maximum possible score of that named item or sentence. For the naming probes, the maximum score of each item was 5; for the oral sentence reading probes, the maximum score was 30 since each sentence comprised six words. A second, blinded rater rescored 20% of randomly selected probes. Inter-rater reliability was calculated using Interclass Correlation Coefficients (ICCs) 2 way random effects, average measures. For the naming probes, the ICC was .983, .992, and .988 (p < .001) for the tool, clothing, and furniture categories, respectively. For the oral sentence reading probes, the ICC was .999, .998, and .997 (p < .001) for the trained, untrained, and generalization sentences, respectively.
Effect sizes (i.e. a measure of the magnitude of change from baseline for each set of probes for each participant) were calculated by dividing the difference between the baseline and the post-treatment means by the standard deviation of the baseline (Beeson & Robey, 2006). The benchmarks of 2.6, 3.9, and 5.8 for small, medium and large effect sizes were used to aid interpretation. These benchmarks are based on effect sizes derived from 12 studies and reported in a review of single-subject research in aphasia (Robey, Schultz, Crawford, & Sinner, 1999). These values have offered initial benchmarks for the interpretation of data in other single-subject studies (Beeson & Egnor, 2006; Beeson, Magloire, & Robey, 2005).
Effect sizes (ES) were also calculated to compare the magnitude of change across conditions using the group gain scores from baseline to post-treatment. The Cohen's (1988) d statistic was calculated by subtracting the mean gain for the Usual Care group from the mean gain for the Usual Care + CILT group, and then dividing by the pooled standard deviation of their gain scores. This is a conservative approach that controls for practice effects from repeated probes. Effect sizes were interpreted using benchmarks for Cohen's d, whereby 0.2 equates to a small effect, 0.5 equates to a medium effect, and 0.8 equates to large effects (Cohen, 1988, 1992).
Standardized Assessment
Each participant completed the Boston Diagnostic Aphasia Evaluation (BDAE) (including the 15-item Short Form of the Boston Naming Test) prior to the start of the study. Immediately after the intervention phase the repetition and oral reading subtests from the BDAE and the Short Form of the Boston Naming Test were readministered. These subtests were selected because oral reading, repetition and naming were skills that were practiced during the CILT training. The BDAE subtests were administered and scored by the first author. A second trained speech-language pathologist viewed videotapes of the assessments and rescored all the subtests. Scoring discrepancies were minor and were easily resolved. They included occasional response time measurement errors on the oral reading subtest and initial disagreement over whether an isolated phonemic paraphasia or a self-corrected production would count as an error on the repetition subtests. Response time was remeasured and it was determined that any deviation from the target during repetition would be scored as an error.
RESULTS
Participants
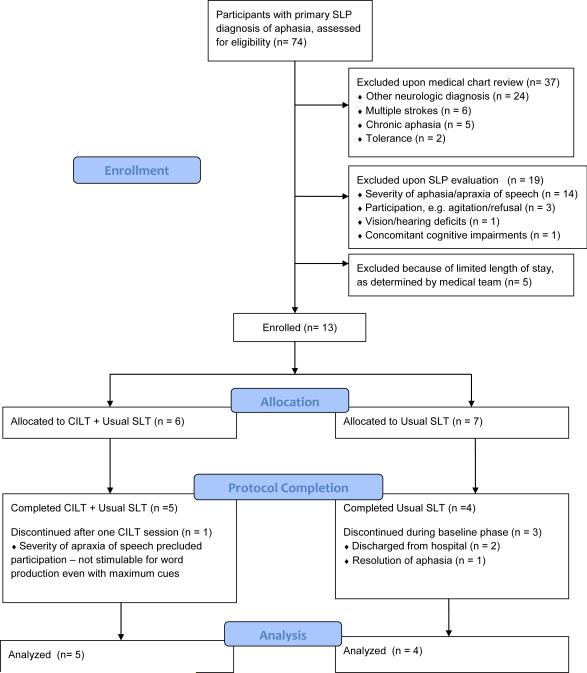
A total of 74 inpatients with a primary diagnosis of aphasia were identified from December 2012-August 2013. Sixty-one inpatients were excluded after chart review, the speech-language pathology evaluation, or the plan of care set by the medical team, as indicated in Table 1 and Figure 1. Thirteen individuals (9M, 4F) were recruited and enrolled in the study, with 6 allocated to the experimental CILT + Usual Care condition and 7 allocated to the Usual Care condition. Three participants in the Usual Care condition discontinued the study during the baseline phase due to resolution of aphasia (one participant) or discharge because of insurance denial for their inpatient stay (two participants). One participant in the CILT + Usual Care condition was removed from the study after one CILT session when the speech-language pathologist determined that he was unable to produce single words with maximum cuing during the treatment session because of continued severe apraxia of speech. He had initially been included in the study because he had produced one novel word during the assessment.
Table 1.
Patients with aphasia excluded from the study
| Reason for Exclusion | Total (n = 61) | Percentage of Sample Excluded |
|---|---|---|
| Other neurological diagnoses | 24 | 39% |
| Aphasia severity | 14 | 23% |
| Multiple strokes | 6 | 10% |
| Chronic aphasia | 5 | 8% |
| Short length of stay | 5 | 8% |
| Participation (e.g., agitation/refusal) | 3 | 5% |
| Tolerance | 2 | 3% |
| Vision/hearing | 1 | 1% |
| Additional cognitive impairments | 1 | 1% |
Figure 1.
Flow chart of participant numbers from potential participants admitted to the inpatient rehabilitation facility to enrollment, allocation, protocol completion and analysis.
Demographic data regarding the 13 enrolled participants are shown in Table 2. Table 2 also indicates with whom each CILT participant was paired. Note that one participant, SAPJO, was originally paired with participant BARWI who later was discontinued secondary to the severity of his apraxia. A trained volunteer served as SAPJO's partner for the remaining CILT sessions.
TABLE 2.
Participant characteristics
| Participant | Age | Gender | Days post onset | Lesion | Aphasia | BDAE Severity Rating (0-5) | |
|---|---|---|---|---|---|---|---|
| Allocated to Usual Care SLT | |||||||
| GRERO | 73 | M | 68 | Traumatic brain injury with left temporal intracranial hemorrhage | Moderate-severe Wernicke's | 2 | |
| LEBPI | 70 | M | 14 | Left middle cerebral artery infarct | Mild-moderate anomic | 2 | |
| FOXSU | 63 | F | 19 | Left middle cerebral artery infarct and intraventricular hemorrhage | Moderate undifferentiated fluent | 2 | |
| TATMI | 45 | M | 41 | Left basal ganglia hemorrhage | Moderate-severe Broca's, moderate apraxia | 2 | |
| MILSU (discontinued) | 47 | F | 10 | Left middle cerebral artery infarct (administered tPA**) | Moderate conduction | 2 | |
| GILRI (discontinued) | 66 | M | 23 | Left parietal infarct | Mild-moderate conduction | 4 | |
| MARRI (discontinued) | 53 | M | 7 | Left middle cerebral artery infarct (administered tPA**) | Mild-moderate anomic→ resolved | 3 | |
| Allocated to Usual Care SLT + CILT | Paired with | ||||||
| KISNO | 45 | M | 21 | Left middle cerebral artery infarct with parietal bleed | Moderate conduction | 3 | SIMLA |
| SIMLA | 60 | M | 49 | Traumatic brain injury with left subdural/subarachnoid hemorrhages | Moderate-severe undifferentiated fluent | 2 | KISNO |
| MCCLA | 37 | F | 11 | Left middle cerebral artery infarct | Moderate-severe Broca's, moderate apraxia | 2 | SALMA |
| SALMA | 76 | F | 17 | Left middle cerebral artery infarct | Severe Broca's, reduced comprehension, apraxia | 1 | MCCLA |
| SAPJO | 53 | M | 25 | Left middle cerebral artery infarct | Severe Broca's, reduced comprehension, apraxia | 1 | BARWI→volunteer* |
| BARWI (Discontinued) | 55 | M | 36 | Left temporoparietal intracranial hemorrhage | Severe Broca's, reduced comprehension, apraxia | 1 | SAPJO |
BDAE = Boston Diagnostic Aphasia Examination. SLT = Speech and Language Therapy. CILT = Constraint Induced Language Therapy
SAPJO was originally paired with BARWI who was discontinued secondary to the severity of his apraxia. A trained volunteer served as SAPJO's partner for remaining CILT sessions.
tPA = Tissue plasminogen activator, administered during acute hospitalization (prior to admission to inpatient rehabilitation)
As previously explained, all participants received usual care. Table 3 displays data that was derived retrospectively from the electronic medical record. It shows how many 15-minute units of treatment were provided routinely by the clinical speech-language pathologists while each participant was involved in the study. The average length of participation in the study was three weeks, including the time of the assessments and baseline probes. Given that usual care provided an hour of speech and language treatment, 5-6 days a week, it was anticipated that participants would receive 60 – 80 units of treatment. It is noted that TATMI, a participant allocated to Usual Care, received only 32 units of speech and language treatment. Further review indicated that he was simultaneously in a specialized clinical high-intensity physical therapy (PT) gait program. As a result, his PT treatment hours were increased while his SLT hours were decreased. In addition, his participation in the Usual Care condition was shortened by two days because of scheduling issues. Table 3 also provides some estimate of the extent to which usual care focused on oral expressive skills. It provides the number of different goals addressed and the percentage of these that targeted oral expression.
TABLE 3.
Usual Care Therapy Distribution
| Units of Therapy* |
Total number of goals | % of Goals Targeting Expression | |||
|---|---|---|---|---|---|
| Participant | Total** | Individual Language Therapy | Group Language Therapy | ||
| Usual SLT | |||||
| GRERO | 78 | 70 | 8 | 94 | 63% |
| LEBPI | 60 | 44 | 2 | 64 | 39% |
| FOXSU | 63 | 46 | 3 | 79 | 27% |
| TATMI | 32 | 26 | 0 | 29 | 34% |
| Usual SLT + CILT | |||||
| KISNO | 59 | 55 | 4 | 59 | 58% |
| SIMLA | 73 | 69 | 0 | 90 | 40% |
| SAPJO | 79 | 63 | 0 | 98 | 49% |
| MCCLA | 64 | 60 | 4 | 61 | 66% |
| SALMA | 73 | 65 | 7 | 57 | 81% |
SLT = Speech and Language Therapy. CILT = Constraint Induced Language Therapy
1 unit = 8-15 minutes
Total includes units charged for dysphagia treatment
The five participants allocated to CILT + Usual Care all received an additional ten hours of CILT (i.e. one-hour long session of CILT daily, five days each week for two weeks). The treatment protocol, treatment materials, and target responses were standard for all participants. However, the amount and type of cues provided to the participants varied to ensure that participants had practice in producing the target responses. Table 4 provides information about the specific cuing strategies that were used with each participant who received the CILT protocol.
TABLE 4.
Type of Cues During CILT
|
Usual SLT + CILT
| |
| KISNO | Written carrier phrase, phonemic or semantic cue for tool item |
| SIMLA | Written carrier phrase, phonemic cue for tool item |
| SAPJO | Choral reading, written carrier phrase, immediate model of tool item |
| MCCLA | Written carrier phrase, phonemic cue for first word of carrier phrase and for tool item |
| SALMA | Choral reading, written carrier phrase, immediate model of tool item |
SLT = Speech and Language Therapy. CILT = Constraint Induced Language Therapy
Questions 1 and 2 asked whether participants receiving the additional CILT sessions show improvement on the trained task, on a similar untrained task, and on a generalization task. Table 5 shows the mean percent accuracy at baseline and post-treatment for both the oral reading of sentences and picture naming probes for the 9 participants who completed the study. Table 6 shows the effect sizes from baseline to post-treatment for both the oral reading of sentences and picture naming probes for these participants. Of the five subjects receiving the additional hour of CILT, 2/5 subjects (KISNO, MCCLA) showed improvements of more than 15% accuracy from baseline to post-treatment on trained oral reading probes, with one subject's probe scores increasing from 37% to 93% (MCCLA), and with an effect size that exceeded 4.0. For the trained picture-naming probes, 4/5 subjects showed gains of greater than 15% accuracy, with effect sizes for these participants ranging from 1.06 to 5.48.
TABLE 5.
Mean % Accuracy of Baseline and Post-treatment Probes
| Oral Reading of Sentences | Naming | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Trained | Untrained | Generalizaton | Trained (Tools) | Untrained (Clothing) | Untrained (Furniture) | |||||||
| Baseline | Final | Baseline | Final | Baseline | Final | Baseline | Final | Baseline | Final | Baseline | Final | |
| Usual SLT | ||||||||||||
| GRERO | 75 | 85 | 80 | 81 | 66 | 68 | 33 | 69 | 40 | 49 | 39 | 52 |
| LEBPI | 99 | 100 | 99 | 100 | 95 | 99 | 61 | 79 | 51 | 84 | 56 | 56 |
| FOXSU | 91 | 98 | 89 | 98 | 64 | 89 | 45 | 43 | 49 | 53 | 36 | 33 |
| TATMI | 58 | 77 | 60 | 72 | 37 | 48 | 61 | 79 | 55 | 71 | 43 | 59 |
| Usual SLT + CILT | ||||||||||||
| KISNO | 77 | 97 | 77 | 98 | 76 | 91 | 72 | 89 | 61 | 84 | 65 | 85 |
| SIMLA | 97 | 99 | 97 | 99 | 93 | 98 | 29 | 56 | 29 | 51 | 21 | 41 |
| SAPJO | 17 | 9 | 15 | 03 | 14 | 11 | 46 | 63 | 27 | 44 | 24 | 20 |
| SALMA | 15 | 20 | 15 | 17 | 15 | 19 | 20 | 23 | 20 | 21 | 19 | 20 |
| MCCLA | 37 | 93 | 35 | 94 | 23 | 50 | 35 | 60 | 20 | 27 | 21 | 31 |
SLT = Speech and Language Therapy. CILT = Constraint Induced Language Therapy
TABLE 6.
Effect Sizes of Probes from Baseline to Post-Treatment
| Oral Reading of Sentences (% Accuracy) | Naming (% Accuracy) | |||||
|---|---|---|---|---|---|---|
| Trained | Untrained | Generalization | Trained (Tools) | Untrained (Clothing) | Untrained (Furniture) | |
| Usual SLT | ||||||
| GRERO | 1.15 | 0.29 | 0.28 | 3.90 | 0.88 | 1.44 |
| LEBPI | 0.65 | 0.29 | 3.18 | 1.88 | 2.37 | 0.00 |
| FOXSU | 1.39 | 1.33 | 0.96 | −0.11 | 0.16 | −0.25 |
| TATMI | 2.48 | 2.16 | 3.42 | 0.92 | 1.59 | 2.62 |
| Usual SLT + CILT | ||||||
| KISNO | 1.40 | 0.93 | 1.53 | 1.06 | 1.18 | 1.13 |
| SIMLA | 4.33 | 1.83 | 2.32 | 2.07 | 2.56 | 8.37 |
| SAPJO | −1.40 | −1.81 | −0.41 | 1.25 | 2.27 | −0.91 |
| SALMA | 0.66 | 0.47 | 0.94 | 0.66 | 0.33 | 0.58 |
| MCCLA | 4.48 | 4.34 | 7.50 | 5.48 | 0.67 | 4.04 |
| Cohen's d | 0.31 | 0.43 | −0.08 | 0.02 | −0.13 | 0.28 |
SLT = Speech and Language Therapy. CILT = Constraint Induced Language Therapy
Effect sizes for individual participants were calculated by dividing the difference between the baseline and the post-treatment probe means by the standard deviation of the baseline (Beeson & Robey, 2006). Benchmarks are 2.6, 3.9, and 5.8 for small, medium and large effect sizes.
Cohen's (1988) d statistic was calculated by subtracting the mean gain for the Usual Care condition from the mean gain for the Usual Care + CILT condition, and dividing by the pooled standard deviation of their gain scores. A positive d statistic indicates greater magnitude of change in the Usual Care + CILT condition. Benchmarks are 0.2, 0.5 and 0.8 for small, medium and large effect sizes.
For untrained probes, oral reading of sentences related to clothing increased by more than 15% accuracy in 2/5 participants. For 3/5 participants, untrained picture naming probes improved by more than 15% accuracy for clothing and/or furniture, with effect sizes ranging from 0.33 to 8.37.
Generalization probes were taken only for oral reading of sentences. For 2/5 participants, there were improvements of greater than 15% accuracy, with effect sizes of 1.53 (KISNO) and 7.50 (MCCLA).
It is interesting to note that one subject, SIMLA, performed at close to the ceiling level for oral reading of sentences, so an increase of 15% accuracy was not possible. However, he showed increases of more than 20% on the trained and untrained picture naming probes, with corresponding effect sizes of 2.07 on the trained items (tools), and 2.56 and 8.37 on the untrained items of clothing and furniture respectively.
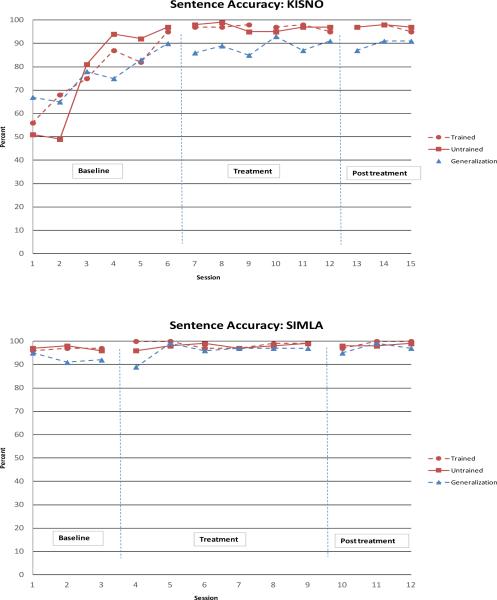
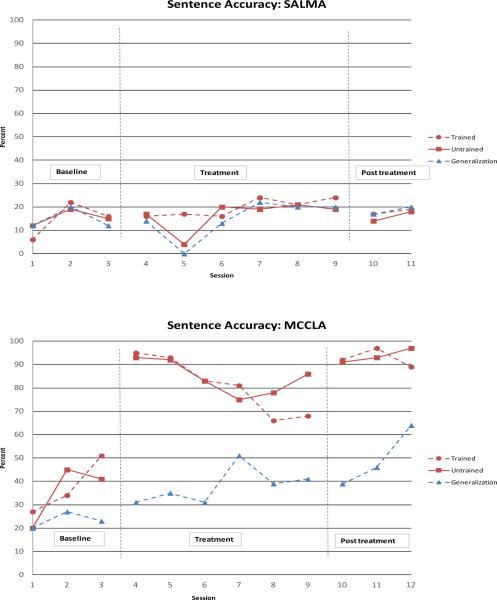
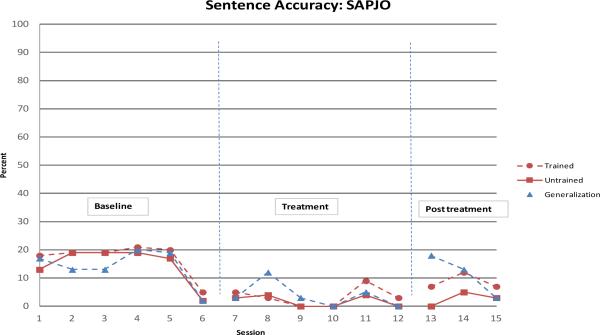
Figures 2, 3 and 4 show the probe performance on oral reading of sentences at baseline, throughout the treatment period, and immediately post treatment for the five participants who received the additional CILT training. Figure 2 displays the performance on trained, untrained and generalization probes for KISNO and SIMLA who were paired together during training; Figure 3 displays the performance on trained, untrained and generalization probes for SALMA and MCCLA who also were paired together during training. Figure 4 displays the performance on trained, untrained and generalization probes for SAPJO who was paired with a trained volunteer during training.
Figure 2.
Trained, untrained, and generalization oral reading sentence probes during pretreatment, treatment, post-treatment for KISNO and SIMLA. Effect sizes for KISNO are 1.40, .93, and 1.53 for trained, untrained, and generalization sentences. For SIMLA they are 4.33, 1.83, 2.32.
Figure 3.
Trained, untrained, and generalization oral reading sentence probes during pretreatment, treatment, post-treatment for SALMA and MCCLA. Effect sizes for MCCLA are 4.48, 4.34, and 7.50 for trained, untrained, and generalization sentences. For SALMA, they are .66, .47, and .94.
Figure 4.
Trained, untrained, and generalization oral reading sentence probes during pretreatment, treatment, post-treatment for SAPJO. Effect sizes are -1.40, -1.81, and -.41 for trained, untrained, and generalization sentences.
The figures illustrate the heterogeneity of response across participants. For example, Figure 3 shows that when treatment was started, MCCLA experienced a large increase in level of performance for both the trained and untrained sentence probes, and this level was maintained at post-treatment. Effect sizes for MCCLA were 4.48, 4.34, and 7.50 for trained, untrained, and generalization sentences. Her CILT partner, SALMA, showed little change from baseline through treatment to post treatment. For SALMA, effect sizes were .66, .47, and .94 respectively. It should also be noted that SALMA did not complete the third post-treatment probe session because of discharge from the hospital.
Figure 2 shows that baseline probes extended for at least 6 days for KISNO until a suitable CILT partner (SIMLA) became available. During this time, baseline performance increased on all oral reading sentence probes (trained, untrained and generalization) almost to ceiling. This increase may have occurred because of spontaneous recovery, because of effects of the usual speech and language therapy that he was receiving, because of repeated practice on the probes, or because of a combination of these factors. Similarly, SAPJO had a lengthy baseline but, in contrast to KISNO, he did not show improvements on probes during this extended baseline period. Therefore, it is difficult to interpret the extent to which the extended baseline with additional CILT probes impacted recovery.
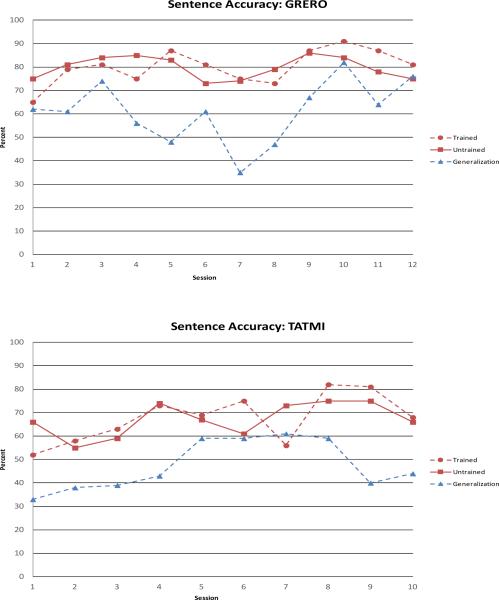
Question 3 asked whether participants receiving the additional daily hour of CILT demonstrated greater improvement on probe tasks than those in the control Usual Care condition without CILT. A comparison of the results in Table 5 indicates that the numbers of subjects showing an increase of more than 15% on the trained, untrained and generalization probes are similar for both groups of participants. For the oral sentence reading probes, 2/4 participants in the control group (GRERO, TATMI) demonstrated this increase on the trained probes, 1/4 participants on the untrained probes (TATMI), and 2/4 (FOXSU, TATMI) on the generalization probes. For the picture naming probes, 3/4 participants showed more than 15 % increase on the trained probes while 2/4 participants showed the 15% increase on the untrained items of clothing and/or furniture.
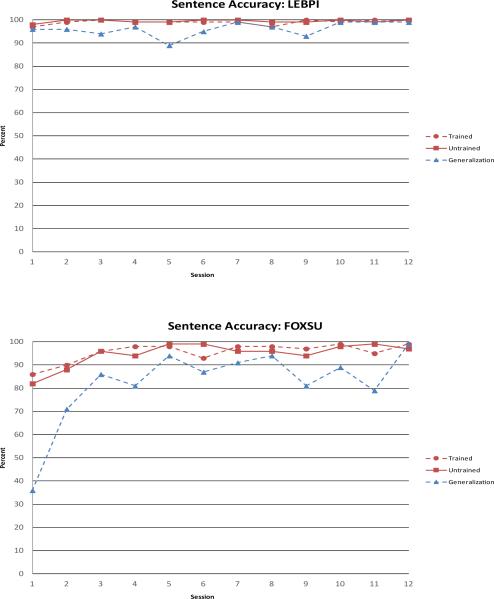
Figures 5 and 6 show the probe performance on oral reading of sentences at baseline, throughout the treatment period, and immediately post treatment for the four control participants who did not receive the additional CILT training. Figure 5 displays the performance on trained, untrained and generalization probes for LEBPI and FOXSU. Like KISNO and SIMLA, probe performance for oral reading of trained and untrained sentences for LEBPI and FOXSU was at or close to ceiling by the end of the baseline period. Figure 6 displays the performance on trained, untrained and generalization probes for GRERO and TATMI. As previously noted, TATMI did not complete two of the probe sessions due to scheduling problems.
Figure 5.
Trained, untrained, and generalization oral reading sentence probes during pretreatment, treatment, post-treatment for LEBPI and FOXSU. These two graphs illustrate the participants reaching the ceiling prior to the implementation of treatment. Effect sizes for LEBPI are .65, .29, and .28 for trained, untrained, generalization sentences. For FOXSU, they are 1.39, 1.33, and .96.
Figure 6.
Trained, untrained, and generalization oral reading sentence probes during pretreatment, treatment, post-treatment for GRERO and TATMI. Effect sizes for GRERO are 1.15, .29, .28 for trained, untrained, and generalization sentences. For TATMI, they are 2.48, 2.16, and 3.42.
Although the numbers of subjects showing change was similar in both groups of participants, the magnitude of change was larger in the participants receiving the additional hours of CILT (see Table 6). Small to medium effect sizes for the Usual Care + CILT condition versus the Usual Care condition were obtained for trained and untrained oral sentence reading (0.31 and 0.43 respectively) and for untrained naming of furniture (0.28). Effect sizes for the other probe tasks were minimal.
Standardized Test Results
With regard to Question 4, Table 7 shows the pretreatment and post treatment BDAE scores for each participant. Examination of individual responses shows large variations across measures. For example, some participants in both groups made large changes on the BNT (LEBPI and TATMI in the Usual Care condition, KISNO in the Usual Care + CILT condition) whereas other participants did not make any change (GRERO, SALMA). Yet, it is interesting to note that the largest changes on the BDAE Repetition and Oral Reading subtests were made by participants in the Usual Care + CILT condition. For Word Repetition, SIMLA and MCCLA, both in the CILT condition, achieved changes of 5 and 6 points respectively. For Sentence Repetition, the largest gains of 4 and 5 points were achieved by KISNO and MCCLA respectively; these same two participants also achieved the largest gains of 8 and 11 points for Oral Word Reading. Only one participant, SIMLA, demonstrated a large gain on Oral Sentence Reading.
TABLE 7.
Pre- and post-treatment scores on Boston Diagnostic Aphasia Evaluation Subtests
| Boston Naming Test (0-15) | Word Repetition (0-10) | Sentence Repetition (0-10) | Oral Word Reading (0-30) | Oral Sentence Reading (0-10) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| pre | post | pre | post | pre | post | pre | post | pre | post | |
| Usual SLT | ||||||||||
| GRERO | 9 | 9 | 6 | 5 | 2 | 4 | 22 | 27 | 1 | 1 |
| LEBPI | 7 | 13 | 9 | 10 | 0 | 0 | 17 | 21 | 1 | 2 |
| FOXSU | 3 | 5 | 9 | 10 | 9 | 9 | 27 | 30 | 1 | 3 |
| TATMI | 4 | 11 | 8 | 9 | 1 | 4 | 17 | 23 | 0 | 1 |
| Usual SLT + CILT | ||||||||||
| KISNO | 7 | 15 | 9 | 8 | 3 | 7 | 14 | 22 | 0 | 1 |
| SIMLA | 1 | 4 | 5 | 10 | 3 | 4 | 27 | 30 | 0 | 5 |
| SAPJO | 2 | 3 | 8 | 8 | 0 | 0 | 0 | 0 | 0 | 0 |
| SALMA | 0 | 0 | 1 | 4 | 0 | 0 | 0 | 1 | 0 | 0 |
| MCCLA | 0 | 3 | 4 | 10 | 1 | 6 | 3 | 14 | 0 | 0 |
SLT = Speech and Language Therapy. CILT = Constraint Induced Language Therapy
DISCUSSION
The primary objective of the current study was to investigate the feasibility of adding an hour of CILT to the usual daily inpatient rehabilitation schedule. A second objective was to assess whether those receiving the additional daily treatment hour, 5 days a week for two weeks, would show greater improvement as compared to those who did not receive the additional daily hour of treatment. Although there were several barriers to implementation, increasing the amount of speech and language therapy by adding an hour of CILT to each day was feasible. Given the small numbers of participants, the heterogeneity of their aphasia, and the difficulty controlling for both spontaneous recovery and the impact of the usual speech and language treatment, results were difficult to interpret. However, there were small to medium effect sizes for trained and untrained probes assessing oral reading of sentences and untrained picture-naming probes (furniture) for the Usual Care + CILT condition compared to Usual Care alone.
Feasibility of Constraint Induced Language Therapy in acute inpatient rehabilitation
This investigation was prompted by research indicating that persons with acute aphasia benefit from speech and language therapy that is more intensive (Brady et al., 2012; Godecke et al., 2013; Martins et al., 2013). Although we found that an additional daily hour of CILT was feasible to implement during the two-week course of the study, there were major barriers with regard to pairing participants and scheduling the sessions. Pairing participants proved difficult because the number of patients with aphasia in the facility at any given time fluctuated. Furthermore, once admitted, patients may have been discharged or readmitted to acute care unexpectedly. Fluctuations in the hospital census were exacerbated by the stringent inclusion/exclusion criteria of the study, which further limited the number of participants for CILT pairing. Figure 1 shows that only nine participants actually completed the study whereas the number of participants screened for the study was 74.
However, many more patients would have been eligible to receive an additional hour of treatment if the CILT sessions were implemented in a clinical context outside of a research project. Table 1 shows reasons for exclusion from the study. Of the 61 participants excluded, it is possible that as many as 40 of them may have been able to participate in and benefit from the extra hour of CILT (24 with other neurological diagnoses, 6 with multiple strokes, 5 with chronic aphasia, 5 with short length of stay). Thus, as speech-language pathologists consider implementing CILT at their sites of care, they may have a sufficient pool of patients to facilitate pairing of participants.
Another barrier, scheduling the CILT sessions, required extensive collaboration with multiple disciplines. This included coordinating inpatient allied health managers across multiple units in order to block patients’ schedules at the same time as well as avoid other therapy sessions; collaboration with case managers to plan around family education, outside appointments, or other procedures; communication with administrative staff who were in charge of inputting schedules into an electronic system; and consideration of physicians’ rounding schedules or nursing staff's typical medication administration times. Participants’ CILT sessions carried an additional label on their daily electronic and paper schedules (“In Chair”) to alert nursing assistants and the rehabilitation technician that the participant needed to be ready for the session in his or her wheelchair. With these additional considerations and modifications, implementation of the CILT sessions on an inpatient unit was accomplished. Participants in the Usual Care + CILT condition received at least the minimum amount of usual care plus the ten hours of CILT, and importantly, none of them discontinued participation in the study due to poor tolerance of the increased intensity of therapy.
Assessing the impact of CILT
As indicated, there were small to medium effect sizes for trained and untrained probes assessing oral reading of sentences and untrained picture-naming probes (furniture) for those receiving the additional daily CILT hour relative to those who did not. However, the varied performance of participants across groups suggests that many inter-related factors may have influenced performance on standardized or probe measures including severity of aphasia, the nature of the probes themselves, and the acuity of the aphasia. In addition, some fundamental differences between CILT and Usual Care may have impacted participant performance.
With regard to aphasia severity, the two most severe subjects were SAPJO and SALMA who had initial BDAE severity scores of 1. Both were allocated to the Usual Care + CILT condition, and probe performance on oral reading of sentences showed relatively little change. However, SAPJO showed improvements in probe naming accuracy for tools (trained) and clothing (untrained) sets while SALMA demonstrated some improvement in Word Repetition on the BDAE. We chose oral reading of sentences as a probe measure because it was similar to the production of the carrier phrases in the CILT task. For the most severe participants, independent oral reading of sentences may have been too difficult for them, and therefore this task was not an appropriate probe task for them. Instead, for these participants, measures such as single word naming or repetition (whereby the model provides some degree of cueing) were better able to measure their improvements.
Alternately, participants such as LEBPI, FOXSU, and SIMLA had relatively less impaired oral reading abilities at the start of the study and quickly reached the ceiling on oral reading of sentences probes. KISNO, although with more impaired oral reading, showed rapid improvement on oral reading probes during the baseline period. For these participants, the probes assessing oral reading of sentences were not able to demonstrate potential improvements during treatment and may not have been appropriate measures to detect change over time.
Furthermore, the interpretation of quantitative data on a single task is not as clear-cut without also considering the qualitative aspects of the participant's performance on the same or other tasks. For example, as shown in Figure 4, SAPJO's performance on oral reading probes decreased with treatment. SAPJO initially responded on the probes by producing perseverative errors without awareness of his inaccuracies. As he became more aware of his communication difficulty, he began to limit his attempts at subsequent words within the sentence probe as soon as he started to produce errors. Therefore, although his oral reading probe performance decreased, SAPJO was demonstrating improvements in awareness and self-monitoring,
Another factor that may have influenced probe performance was the acuity of the aphasia. Participants in both groups showed improvements on at least some measures across the duration of the study, and often showed similar amounts of change. The potential influence of spontaneous recovery cannot be ruled out, and indeed seemed to be a strong factor for a participant like KISNO who improved so rapidly during the baseline period.
A key component of CILT is its focus on spoken language, whereby participants produce a large number of repetitions of a limited number of training items. Usual speech and language therapy, in contrast, may address a variety of modalities and does not provide as much repetitive practice since tasks are changed frequently within a session. The probe tasks were spoken (i.e. oral sentence reading and naming), closely corresponding to the repetitive training that was provided in the CILT sessions. Probe tasks addressing other modalities were not included because of the assumption that all participants would do equally well on them since participants in both conditions received Usual Care. It is interesting to note that we expected the greatest difference between conditions to be on probe performance of the trained items, given the repetitiveness of the CILT training on a limited set of items. Yet, the effect size between conditions was greatest for the untrained probes that assessed oral reading of sentences that were not practiced.
Limitations
This feasibility study demonstrates that some participants with aphasia in an acute inpatient rehabilitation facility benefited from an hour of daily CILT in addition to their usual speech and language therapy. However, it is not clear why some participants (e.g. KISNO, MCCLA) showed large improvements while others did not. Similarly, some participants in the control Usual Care condition also showed large improvements (e.g. FOXSU), while others did not. In addition to the small sample size, participants were heterogeneous in terms of aphasia type, severity, and preserved oral reading abilities. In order to recruit a sufficient number of participants and because CILT has been used successfully with various aphasia diagnoses and severities, we did not limit the potential participant pool to a more homogenous sample that may have shown more clear patterns of improvement.
Usual Care is described as one hour of speech and language treatment per day, 5-6 days a week. Although the minimum amount of treatment was achieved for most participants, it was difficult to ensure that the frequency and duration of usual care was the same for all participants. Also uncontrolled was the content of the participants’ individual speech-language sessions. During these sessions, the participants’ primary speech-language pathologists determined the treatment targets, and those sessions may have targeted language impairments, functional communication, family education, or even dysphagia. Therefore, participants’ individual changes may also be explained by the combination of modalities treated during the usual speech and language sessions.
CILT has typically been investigated with an intensity of 3 hours per day for 2 weeks, while this study only added an additional hour of CILT per day for a total of ten hours over two weeks. CILT delivered at the intensity of 3 hours per day is likely not feasible for patients in acute inpatients rehabilitation given the scheduling demands and potential for fatigue in persons overcoming recent medical events. While an additional hour is feasible, it may not be enough to facilitate more substantial gains for CILT participants as compared to usual speech and language pathology care. Furthermore, CILT represents only one treatment approach that could be used for increasing the amount of treatment for inpatients with acute aphasia. Further investigation is warranted with other treatments that can be added without placing demands on reimbursement or therapy resources.
In this study, performance was assessed at baseline and post-treatment with no short-term or long-term follow-up assessments to determine whether differences between the experimental and control participants were maintained. Although previous studies included follow up assessments as long as one year after the end of treatment (e.g., Sickert et al., 2013), interpretation of these data is difficult. To adequately interpret results from any follow-up assessments, it would be essential that participants in both groups receive the same type and amount of therapy during the interim maintenance periods. Future research is warranted to address whether gains that may result from more intensive treatment are better maintained in the experimental participants as compared to control participants.
This study has focused on measuring only quantitative changes on oral reading and picture-naming probe and standardized measures, without considering the potential for functional communication changes outside of the treatment session. Patients with communication difficulties in inpatient rehabilitation settings may have limited opportunities for spontaneous interactions outside of therapies and may only communicate responses to questions regarding their basic needs (e.g. pain, toileting, medications, etc.) from nursing staff and physicians. We have found that the CILT session provided a context for the person with acute aphasia to meet someone else with a communication impairment and to work with a shared focus on language skills. SALMA, who showed very little spontaneous communication, began waving to her partner, MCCLA, in the hallway between therapies. Although one of the most severe participants, she attempted some degree of banter with MCCLA across their barrier whenever she made a matching pair. KISNO and SIMLA, although residing on different floors of the hospital, continuously inquired about each other during their individual probe sessions and asked when they would see their partner for their next session. Further investigations should include measures of functional communication at baseline, post-treatment and follow-up. It should also assess the extent to which small group treatment such as the pairing of participants during CILT influences outcomes as compared to typical one-to-one sessions provided during Usual Care.
In conclusion, we have demonstrated the feasibility of increasing the amount of therapy provided to persons with aphasia in an acute inpatient rehabilitation facility. Usual care provides an hour of speech and language treatment, five to six days a week. Over a two week period, we were able to schedule and administer an additional hour of CILT, 5 days per week, to five participants with aphasia. Four participants served as control participants and did not receive the additional hour of CILT. We also compared performance on baseline, treatment and post-treatment probes assessing oral reading of sentences and picture-naming, as well as on pre- and post-treatment performance on subtests of the BDAE. While individual results tended to be equivocal, as a group there was a small to medium effect size of the Usual Care + CILT condition over Usual Care alone. Further research with larger numbers of participants is needed to investigate outcomes when amount and intensity of treatment is increased in the acute inpatient rehabilitation setting.
Acknowledgments
This study was supported by the Rehabilitation Institute of Chicago's James Brown IV Fellowship (awarded to JC). Preparation of the manuscript was supported by the National Institute on Deafness and Other Communication Disorders, Award No. 1R01 DC011754 (to LRC) and by the U.S. Department of Education, NIDRR Grant # H133G120123 (to LRC). The content is solely the responsibility of the authors and does not necessarily represent the official views of the funding organizations. Endorsement by the Federal Government should not be assumed. The authors extend their thanks to Rosalind Hurwitz, Mara Nussbaum, and Laura Pitts who assisted with reliability measures.
Appendix
Appendix.
Practice and Probe Items
| Items/Sentences Practiced During CILT | Unpracticed Items/Sentences | ||||
|---|---|---|---|---|---|
| Tools | Trained | Clothing | Untrained | Furniture | Generalization |
| hammer | __________, do you have a hammer? | shirt | __________, do you have a shirt? | chair | My mom's chair is very comfortable. |
| wrench | __________, do you have a wrench? | slipper | __________, do you have a slipper? | desk | He writes papers at the desk. |
| broom | __________, do you have a broom? | sweater | __________, do you have a sweater? | bed | The bed was new and expensive. |
| mop | __________, do you have a mop? | hat | __________, do you have a hat? | table | Leave the book on the table. |
| fork | __________, do you have a fork? | turtleneck | __________, do you have a turtleneck? | nightstand | Put the glasses on the nightstand. |
| knife | __________, do you have a knife? | glove | __________, do you have a glove? | ottoman | That ottoman matches the new chair. |
| spoon | __________, do you have a spoon? | coat | __________, do you have a coat? | dresser | The bedroom needs another small dresser. |
| whisk | __________, do you have a whisk? | boot | __________, do you have a boot? | couch | He fell asleep on the couch. |
| spatula | __________, do you have a spatula? | shoe | __________, do you have a shoe? | cabinet | Open the cabinet under the sink. |
| screwdriver | __________, do you have a screwdriver? | sock | __________, do you have a sock? | chandelier | The chandelier needs a new bulb. |
| saw | __________, do you have a saw? | t-shirt | __________, do you have a t-shirt? | buffet | He stores dishes in the buffet. |
| shovel | __________, do you have a shovel? | belt | __________, do you have a belt? | headboard | The headboard was heavy and sturdy. |
| rake | __________, do you have a rake? | mitten | __________, do you have a mitten? | coffee table | He cleans the coffee table daily. |
| pen | __________, do you have a pen? | scarf | __________, do you have a scarf? | lamp | The lamp lights up the room. |
| pencil | __________, do you have a pencil? | raincoat | __________, do you have a raincoat? | filing cabinet | Put papers in the filing cabinet. |
| vacuum | __________, do you have a vacuum? | dress | __________, do you have a dress? | recliner | The recliner is perfect for napping. |
| ladle | __________, do you have a ladle? | skirt | __________, do you have a skirt? | rug | Do not trip on the rug. |
| paintbrush | __________, do you have a paintbrush? | suit | __________, do you have a suit? | sink | The sink needs to be cleaned. |
| comb | __________, do you have a comb? | tie | __________, do you have a tie? | end table | Put magazines on the end table. |
| toothbrush | __________, do you have a toothbrush? | vest | __________, do you have a vest? | folding chair | We need the extra folding chair. |
| razor | __________, do you have a razor? | sweatshirt | __________, do you have a sweatshirt? | mirror | I hung a mirror above it. |
| hose | __________, do you have a hose? | bowtie | __________, do you have a bowtie? | pillow | His mom bought a new pillow. |
| sponge | __________, do you have a sponge? | sandal | __________, do you have a sandal? | book shelf | Store it in the book shelf. |
| stapler | __________, do you have a stapler? | undershirt | __________, do you have an undershirt? | bench | You can sit on this bench. |
| axe | __________, do you have an axe? | jacket | __________, do you have a jacket? | stool | Please bring the stool for him. |
References
- Baker E. Optimal intervention intensity in speech-language pathology: Discoveries, challenges, and unchartered territories. International Journal of Speech-Language Pathology. 2012;14(5):478–485. doi: 10.3109/17549507.2012.717967. doi: 10.3109/17549507.2012.717967. [DOI] [PubMed] [Google Scholar]
- Bakheit AMO, Shaw S, Barrett L, Wood J, Carrington S, Griffiths S, Koutsi F. A prospective, randomized, parallel group, controlled study of the effect of intensity of speech and language therapy on early recovery from poststroke aphasia. Clinical Rehabilitation. 2007;21(10):885–894. doi: 10.1177/0269215507078486. [DOI] [PubMed] [Google Scholar]
- Barthel G, Meinzer M, Djundja D, Rockstroh B. Intensive language therapy in chronic aphasia: Which aspects contribute most? Aphasiology. 2008;22(4):408–421. [Google Scholar]
- Beeson PM, Egnor H. Combining treatment for written and spoken naming. J Int Neuropsychol Soc. 2006;12(6):816–827. doi: 10.1017/S1355617706061005. doi: 10.1017/s1355617706061005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beeson PM, Magloire JG, Robey RR. Letter-by-letter reading: natural recovery and response to treatment. Behav Neurol. 2005;16(4):191–202. doi: 10.1155/2005/413962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beeson PM, Robey RR. Evaluating single-subject treatment research: lessons learned from the aphasia literature. Neuropsychol Rev. 2006;16(4):161–169. doi: 10.1007/s11065-006-9013-7. doi: 10.1007/s11065-006-9013-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brady MC, Kelly H, Godwin J, Enderby P. Speech and language therapy for aphasia following stroke. Cochrane Database Syst Rev. 2012;5:CD000425. doi: 10.1002/14651858.CD000425.pub3. doi: 10.1002/14651858.CD000425.pub3. [DOI] [PubMed] [Google Scholar]
- Cherney LR. Aphasia treatment: intensity, dose parameters, and script training. Int J Speech Lang Pathol. 2012;14(5):424–431. doi: 10.3109/17549507.2012.686629. doi: 10.3109/17549507.2012.686629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cherney LR, Patterson JP, Raymer A, Frymark T, Schooling T. Evidence- based systematic review: effects of intensity of treatment and constraint-induced language therapy for individuals with stroke-induced aphasia. J Speech Lang Hear Res. 2008;51(5):1282–1299. doi: 10.1044/1092-4388(2008/07-0206). doi: 10.1044/1092-4388(2008/07-0206) [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Erlbaum; Hillsdale, NJ: 1988. [Google Scholar]
- Cohen J. A power primer. Psychological Bulletin. 1992;112:155–159. doi: 10.1037//0033-2909.112.1.155. [DOI] [PubMed] [Google Scholar]
- Gingrich L, Hurwitz R, Lee J, Carpenter J, Cherney LR. Quantifying Naming & Oral Reading Performance in Aphasia: The NORLA-6 Scale.. Presented at the Annual Convention of the American Speech Language Hearing Association; Chicago, IL.. Nov, 2013. [Google Scholar]
- Godecke E, Hird K, Lalor EE, Rai T, Phillips MR. Very early poststroke aphasia therapy: a pilot randomized controlled efficacy trial. Int J Stroke. 2012;7(8):635–644. doi: 10.1111/j.1747-4949.2011.00631.x. [DOI] [PubMed] [Google Scholar]
- Godecke E, Rai T, Ciccone N, Armstrong E, Granger A, Hankey GJ. Amount of therapy matters in very early aphasia rehabilitation after stroke: a clinical prognostic model. Semin Speech Lang. 2013;34(3):129–141. doi: 10.1055/s-0033-1358369. doi: 10.1055/s-0033-1358369. [DOI] [PubMed] [Google Scholar]
- Goodglass H, Kaplan E, Barresi B. The assessment of aphasia and related disorders. Lippincott Williams & Wilkins; 2001. [Google Scholar]
- Hornby TG, Straube DS, Kinnaird CR, Holleran CL, Echauz AJ, Rodriguez KS, Narducci EA. Importance of specificity, amount, and intensity of locomotor training to improve ambulatory function in patients poststroke. Top Stroke Rehabil. 2011;18(4):293–307. doi: 10.1310/tsr1804-293. doi: 10.1310/tsr1804-293. [DOI] [PubMed] [Google Scholar]
- Kirmess M, Maher LM. Constraint induced language therapy in early aphasia rehabilitation. Aphasiology. 2010;24(6-8):725–736. doi: 10.1080/02687030903437682. [Google Scholar]
- Maher LM, Kendall D, Swearengin JA, Rodriguez A, Leon SA, Pingel K, Rothi LJ. A pilot study of use-dependent learning in the context of Constraint Induced Language Therapy. J Int Neuropsychol Soc. 2006;12(6):843–852. doi: 10.1017/S1355617706061029. doi: 10.1017/s1355617706061029. [DOI] [PubMed] [Google Scholar]
- Martins IP, Leal G, Fonseca I, Farrajota L, Aguiar M, Fonseca J, Ferro JM. A randomized, rater-blinded, parallel trial of intensive speech therapy in sub-acute post-stroke aphasia: the SP-I-R-IT study. Int J Lang Commun Disord. 2013;48(4):421–431. doi: 10.1111/1460-6984.12018. doi: 10.1111/1460-6984.12018. [DOI] [PubMed] [Google Scholar]
- Meinzer M, Rodriguez AD, Gonzalez Rothi LJ. First decade of research on constrained-induced treatment approaches for aphasia rehabilitation. Arch Phys Med Rehabil. 2012;93(1 Suppl):S35–45. doi: 10.1016/j.apmr.2011.06.040. doi: 10.1016/j.apmr.2011.06.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Page SJ, Wallace SE. Speech language pathologists' opinions of constraint-induced language therapy. Top Stroke Rehabil. 2014;21(4):332–338. doi: 10.1310/tsr2104-332. doi: 10.1310/tsr2104-332. [DOI] [PubMed] [Google Scholar]
- Pulvermuller F, Neininger B, Elbert T, Mohr B, Rockstroh B, Koebbel P, Taub E. Constraint-induced therapy of chronic aphasia after stroke. Stroke. 2001;32(7):1621–1626. doi: 10.1161/01.str.32.7.1621. [DOI] [PubMed] [Google Scholar]
- Robey RR, Schultz MC, Crawford AB, Sinner CA. Review: Single-subject clinical-outcome research: designs, data, effect sizes, and analyses. Aphasiology. 1999;13(6):445–473. [Google Scholar]
- Sickert A, Anders LC, Munte TF, Sailer M. Constraint-induced aphasia therapy following sub-acute stroke: a single-blind, randomised clinical trial of a modified therapy schedule. J Neurol Neurosurg Psychiatry. 2014;85(1):51–55. doi: 10.1136/jnnp-2012-304297. doi: 10.1136/jnnp-2012-304297. [DOI] [PubMed] [Google Scholar]