Abstract
Chemoresistant metastatic relapse of minimal residual disease plays a significant role for poor prognosis of cancer. Growing evidence supports a critical role of cancer stem cell (CSC) behind the mechanisms for this deadly disease. This review briefly introduces the basics of the conventional chemotherapies, updates the CSC theories, highlights the molecular and cellular mechanisms by which CSC smartly designs and utilizes multiple lines of self-defense to avoid being killed by chemotherapy, and concisely summarizes recent progress in studies on CSC-targeted therapies in the end, with the hope to help guide future research towards developing more effective therapeutic strategies to eradicate tumor cells in the patients.
Keywords: Cancer stem cell, chemotherapy, chemoresistance, targeted therapy
1. Introduction
1.1. Chemotherapy and chemoresistance
Chemotherapy is one of the current mainstream anticancer therapies. It uses chemicals to kill rapidly dividing cancer cells. These chemicals or chemotherapeutic agents typically induce apoptosis by damaging DNA and/or inhibiting mitotic division (1–3). Despite being an important therapeutic option for most cancer patients and the many agents and strategies available, chemotherapy frequently misses slowly dividing and non-dividing cancer cells. It also leaves behind fast-dividing cancer cells that are less sensitive particularly when reduced doses are given to avoid side effects on rapidly dividing normal cells. The insensitivity of these cancer cells causes resistance to chemotherapy or chemoresistance that is a major cause of treatment failure with treatment strategies involving chemotherapy (4). Some of the tumor cells are already resistant to the “achievable” doses of anticancer drugs. This type of resistance present in therapy-naïve patients is named intrinsic resistance. Other tumor cells are initially sensitive but become resistant to the drug during the course of treatment. This therapy-induced resistance is termed as acquired resistance. Although not pre-existing, adaptive resistance can occur immediately through a rapid rewiring of cancer cell signaling once treatment begins. Regardless of the resistance mechanisms, the chemoresistant cancer cells are the major cause of tumor recurrence or relapse and have garnered the most attention clinically (1, 2, 5).
1.2. Tumor recurrence or relapse
Tumor recurrence or relapse was initially tied to a small number of therapy-resistant leukemic cells that remained in the patient during treatment or post-therapeutic remission without overt symptoms or signs of disease. This phenomenon was termed as minimal residual disease (MRD). It is the major cause of leukemic relapse. This terminology was then extended to non-leukemic cancer types particularly carcinomas and is divided into local residual disease and metastatic residual disease (or micrometastasis) depending upon the location of the residual disease or the recurrent tumor in relation to the primary tumor location. Importantly, minimal residual diseases are highly enriched for cancer stem cells (6).
1.3. Cancer stem cells
The cancer stem cell (CSC) concept was first reported more than a century ago on observing the histological similarities between tumors and embryonic tissues. A tumor contains heterogeneous populations of cells. CSCs are a very small subset of relatively quiescent cells in the tumor that are endowed with the ability to self-renew and differentiate into non-stem daughter cells that make the bulk of tumor, which is the central property of normal stem cells as well (7–10). The concept may explain not only why clonogenic capacity of most malignancies is very low but also why complete initial responses to treatment rarely leads to cures. The initial responses mirror the therapeutic effect on the cells that form the tumor bulk while leaving behind CSCs that are responsible for relapse, the real threat to tumor cell eradication (11, 12).
Growing evidence supports the notion that cancer is a disease driven by CSCs responsible for tumor initiation, growth, metastasis, therapy resistance, relapse and poor prognosis. The isolation of CSCs was first described in 1994 from leukemia and then from solid tumors of many cancer types including breast, lung, prostate, colon, brain, head and neck, skin, and pancreatic cancers (13). Despite extensive studies, there has been a long-lasting debate on the existence of CSCs and their roles in patients. For example, in contrast to the CSC model, a stochastic model describes that all tumor cells in the late stage of melanomas are equipotent and stochastically self-renew or differentiate, resulting in tumor heterogeneity with presumably different CSC types endowed with distinct therapy-resistant phenotypes (12, 14). As a result, more conservative terms instead of CSC have been used such as tumor-initiating cells, tumor-propagating cells, tumor-progenitor cells and tumor stem-like cells.
Direct in vivo evidence of CSC existence in mice came in three back-to-back research articles published in 2012 (15–17). The first group developed a genetically engineered mouse model of glioma. In that model, a nestin-DTK IRES-GFP transgene, alongside the HSV thymidine kinase gene was made that specifically labels quiescent adult neural stem cells. This transgene was also expressed in a subset of spontaneous glioma tumor cells. After the tumor growth was transiently arrested using temozolomid followed by pulse-chase of the tumor growth, the tumor was able to re-grow only from the transgene-expressing cells. If these cells in the tumor were ablated with ganciclovir, the tumor growth and re-growth were inhibited. Thus the study concluded that a subset of quiescent endogenous tumor cells serve as CSCs responsible for sustaining long-term growth of glioma (15). The second group genetically labeled individual tumor cells in vivo and traced them over the progression of papilloma and squamous cell carcinoma. The study demonstrated that only a very small fraction of the labeled cells with CSC characteristics persist long term to grow and form a significant part of the tumor (16). The third group genetically labeled and traced primary intestinal adenoma cells that express the crypt stem cell marker Lgr5. The study revealed that these Lgr5+ cells represent only 5–10% of the tumor cells and could self-renew as well as differentiate into all other adenoma cell types, indicating they are the CSCs (17).
Clinical evidence for CSCs came first from patient studies of MRDs. Post-therapeutic residual tumor cells of breast cancer are found enriched for CSCs (18). The presence of acute myeloid leukemic (AML) CSCs in the minimal residual diseases correlates with poor progression-free survival (19). The myelodysplastic syndrome (MDS) stem cells persist in the patients even with complete clinical and cytogenetic remissions (20). In a latest study the same group reported more direct evidence for CSC presence in patients (21). By establishing molecularly and functionally distinct and hierarchically organized stem and progenitor cell compartments of MDS and back tracking somatic genetic lesions, the group demonstrated that the rare Lin−CD34+CD38−CD90+ CD45RA MDS cell population functions as MDS-propagating cells in the patients. Elimination of this population is essential toward eradication of the entire MDS clone. This discovery strongly supports the CSC theory and could encourages development of CSC-targeted therapies and CSC-based relapse-predicting strategies.
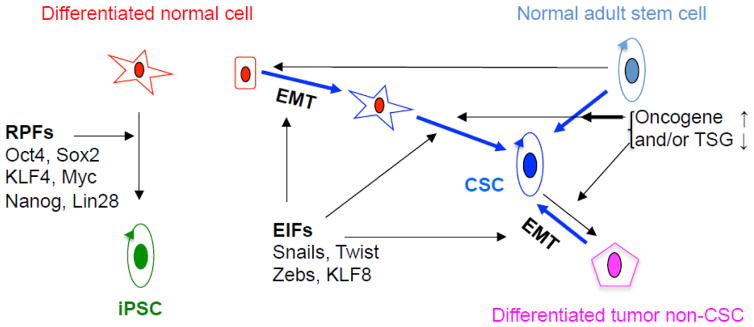
It remains unclear, however, whether CSCs originate from normal stem cells or non-stem cells and what are the driving forces for the transformation process. Regardless, it seems that the physiological balance between the proto-oncogenes and tumor suppressor genes needs to be disrupted and in some cases the epithelial-mesenchymal transition (EMT) process must be involved for CSC formation (22, 23). Hypothesized origins and mechanisms of CSC formation are illustrated in Figure 1.
Figure 1.
Cancer stem cell (CSCs) origins and mechanisms of formation. The three hypotheses are highlighted in bold blue arrows. 1. The epithelial to mesenchymal transition (EMT) induced by EMT-inducing factors (EIFs) turns normal epithelial cell (the red square-shaped) to fibroblast-like cell (the blue star-shaped). The latter subsequently becomes CSC particularly with mutations of oncogenes and/or tumor suppressor genes (TSGs). This process mirrors the formation of induced pluripotent cell (iPSC, green round-shaped) from normal fibroblast (red star-shaped) activated by the reprogramming factors (RPFs) shown on the left. 2. Normal adult stem cell (ASC, light-blue round shaped) is transformed into CSC by mutations of oncogene(s) and/or TSG(s). 3. EMT drives the tumor non-CSC (pink pentagon-shaped) back to be CSC.
2. Mechanisms of CSC chemoresistance - the multiple lines of defense
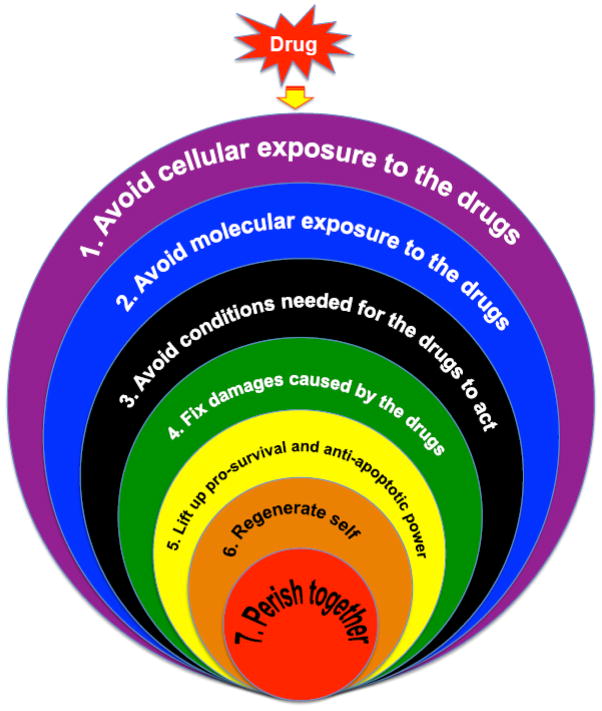
Despite the intensive studies in the past, the mechanisms by which tumors become chemoresistant and the clinical causes of chemoresistance remain only partially understood (24, 25). Recent studies have suggested CSC as a main player for chemoresistance against a variety of drugs including cisplatin and/or paclitaxel (26–32), temozolomide (15, 30), etoposide (29), and doxorubicin or methotrexate (31, 33) in many types of cancer including gliomas and glioblastoma (15), breast (26, 27), colorectal (34–38), AML (39, 40), hepatic (33), lung (41), bone (42), pancreatic (30, 32), ovarian (28) and prostate (31) cancers. Thus, the cellular and molecular mechanisms underlying the CSC’s chemoresistance have drawn accelerating attention for cancer research (37, 43–49). Although still poorly understood, CSCs use a series of self-defense lines against attacks by the chemotherapeutic drugs. These defense lines are outlined in Figure 2 and discussed in details below.
Figure 2.
The multiple lines of defense cancer stem cells use to resist chemotherapy.
2.1. Avoid cellular exposure to the drugs – the 1st line
2.1.1. CSC niches
Normal adult stem cells (ASCs) are usually located at places that are less exposed to potential external attacks. For example, the skin stem cells are housed in the bulge at the side of hair follicle away from the papilla and matrix that are connected with the capillary (50), the mammary stem cells hide under the luminal epithelium away from the acinar lumen (51), the intestinal stem cells are located at the very bottom of the crypt farthest away from the intestinal lumen (52), and the hematopoietic stem cells are shielded in the bone marrow and guarded by the hard bone (53).
CSCs are similarly protected physically albeit in slightly different ways. CSCs take the maximal advantage of the specific tumor microenvironments they are localized in. These particular compartments are called CSC niches. Like normal stem cell niches, CSC niches are thought to maintain a balance between self-renewal and differentiation and therapy resistance of CSCs through either extracellular matrix protein-cell or cell cell communication (54). Although the niche concept is generally accepted (55), the exact types of cells and proteins that constitute these niches remain largely elusive. Still under investigation, if not in debate (56) are the two CSC niche types, the hypoxic niche and the perivascular niche.
The hypoxic niche (12) has been demonstrated for hematopoietic stem cells (HSC) (57, 58), melanoma (59), leukemia (60, 61), brain (62–65), prostate (66, 67), lung (68), pancreatic (69) and breast (70) cancers. Hypoxia is a hallmark of cancer and an important factor for disease progression, therapeutic resistance and poor prognosis. Hypoxia regulates many aspects of cancer including cell survival, proliferation, differentiation, angiogenesis, metabolism, invasion and metastasis. The primary mediator of hypoxia is the hypoxia-inducible factor (HIF) subunits HIF1α and HIF2α, the regulators of tissue oxygen homeostasis (71). Hypoxia plays an important role for stem cell function via HIF (72). Deletion of hif1α leads to inhibition of HSC self-renewal (73) and the clonogenecity of leukemic CSCs (60, 61). In brain, pancreatic and breast cancers, hypoxia has been shown to promote the CSC expansion (62–65, 69, 70). Oxygen plays a crucial role in generating ROSs that mediate the anticancer effects of therapies such as radiotherapy. The low oxygen tensions in the hypoxic area of the tumor thus contain low levels of ROSs, reducing the risk for the cells located in the hypoxic area of being killed (71). Indeed, normal adult epithelial, glial and neuronal stem cells contain lower levels of ROSs than the differentiated progeny (74–77). Upon receiving irradiation, the MCF-7 breast CSCs in mammospheres showed a lower level of ROSs and DNA damage than cells in monolayer culture, suggesting high levels of free radical scavengers in the CSCs (56)
The hypoxic niche concept came at a bit surprising timing in that prior to it many studies had pointed to an essential role of endothelial cells and the perivascular niche for CSCs as was demonstrated for normal stem cells. Tumor vasculatures are required for delivery of nutrients and oxygen, recruitment of stromal cells, endocrine trafficking of growth factors and cytokines and disposal of metabolic wastes (78). In glioblastoma and squamous cell carcinoma, CSCs are localized in close contact with endothelial cells (79–81). Anti-vascular endothelial growth factor (VEGF) receptor (VEGFR2) treatment causes CSC depletion resulting in inhibition of tumor growth or regression of tumor (12). These studies suggest that perivascular niches involving VEGF signaling are crucial for maintaining CSCs or tumorigenic potential. It should be noted, however, that anti-angiogenic therapies have not been as successful as expected in the many years of clinical trials. One of the reasons for the failure could be that the therapies enhance the hypoxic conditions good for maintaining the hypoxic niches of CSCs. As such, the vascular normalization in tumor has emerged as an important therapeutic strategy (82).
At the first thought, the two concepts for CSC niches seem paradoxical. However, they may coexist in distinct compartments of the same tumor and represent distinct requirements of CSCs. Indeed, studies have shown that HSCs reside in a vascular niche (83, 84) and in a hypoxic niche as well (57, 58). ER+ and ER− breast CSCs seem to have distinct preference to hypoxic and perivascular niches, respectively (57, 58, 83, 84). Subsets of CSCs in head and neck squamous cell carcinoma (HNSCC) differ intrinsically in their patterns of oxygen metabolism (68). These studies indicate that both of the niche types are required for CSCs and they may not be independent of each other. Rather, they may be interrelated and HIF-1, the critical regulator for both hypoxia and angiogenesis, may serve as the bridge or switchman between the two niche types. Whether or not the CSCs localized in the hypoxic niches are even the source of the CSCs localized in the perivascular niche (that houses CSCs ready to differentiate yet easier to kill) is worth further investigation. Nevertheless, HIF-1 may be an important molecular target for anti-CSC therapy (85).
2.1.2 CSC-specific stroma
In addition to physically protecting the niches, other components of tumor microenvironment including extracellular matrix (ECM), cancer-associated fibroblasts, immune cells and inflammatory cells (86, 87) also play a role in protecting CSCs against both chemotherapy and other therapies (88). They provide CSCs with resistant signaling stimuli through surface receptors to activate other lines of defense for CSCs. For example, tumor myofibroblasts secrete growth factors such as hepatocyte growth factor (HGF) and periostin to activate Wnt signaling required for tumor stemness in colorectal or breast cancer (89, 90). Stromal cells secrete high levels of HGF which makes co-cultured human cancer cells of many types acquire resistance to various anticancer drugs particularly RAF inhibitors (91). Other growth factors or cytokines including interleukin 6 (IL-6), fibroblast growth factor (FGF) and neuregulin 1 are reported to help form the so-called ‘chemoresistant niche’ of CSCs by activating various survival signaling pathways (92, 93). In addition, the ECM receptors integrins are highly associated with CSC survival and drug resistance (94, 95), suggesting critical roles for the ECM. Lastly, the stem cell surface marker CD44, initially identified as the lymphocyte homing receptor, is commonly expressed in embryonic and adult stem cells as well as CSCs (96). It binds its ligand hyaluronan to regulate many aspects of stem cell function including self-renewal, ECM retention in the niche, proliferation, differentiation and homing or metastasis. CD44 signaling also helps maintain the genomic integrity of stem cells by protecting and repairing DNA from oxidative damage. In addition, CD44 is implicated in regeneration of CSCs responsible for chemoresistance and relapse.
2.2. Avoid molecular exposure to the drugs- the 2nd line
2.2.1. ATP-binding cassette transporters (ABCT) and drug efflux
What if the CSCs have failed to avoid a contact with the drugs? At the organismic level, a toxic chemical accidently taken in is detoxified and filtered out primarily by the liver. The first thing a CSC does once the drug has entered the cytoplasm, however, is to activate the 2nd line of defense, i.e., the drug efflux mechanisms to pump the drug out of the cell. This mechanism has been taken advantage of for isolating CSCs as the side-population (SP) cells by flow cytometry that do not accumulate the drug-mimicking dye. The transmembrane proteins of the ABCT family are the main players of drug efflux (97). Among 49 family members three have been extensively studied and correlated with drug resistance. They are the multidrug resistance protein 1 (MDR1 or ABCB1), multidrug resistance-associated protein 1 (MRP1 or ABCC1) and breast cancer resistance protein (BCRP or ABCG2) (97). They can eliminate various types of chemotherapeutic drugs such as taxanes, topoisomerase inhibitors and antimetabolites. MDR1 are normally expressed on the surface of epithelial cells of intestine and ductules of pancreas, bile and kidney and overexpressed in many tumor types associated with intrinsic resistance (98, 99). Its expression can also be induced by chemotherapy which is associated with acquired resistance (100). MDR1-associated resistance has been seen in kidney, colon, liver, prostate, lung and breast cancers as well as leukemia (101–103). MRP1 has been used as a marker of prediction for chemoresistance (104). BCRP is associated with drug resistance in breast cancer and leukemia (105, 106). Interestingly, MDR1 and BCRP can also perform efflux of small molecule drugs (107). Clinical trials of MDR1 inhibitors such as zosuquidar and tariquidar, however, have been disappointing in breast (108) and squamous cell carcinoma (108, 109) even when used in combination with docetaxel (109). This suggests that a high degree of functional redundancy among the ABCT family members is a critical factor for this particular defense line of CSCs. Indeed, CSCs of several cancer types show high expression of multiple ABCTs (110, 111). The NCI60 panel studies indicated a role in drug resistance for majority of the family members (112). As such, finding the ‘Achilles heel’ of the redundancy is key for ABCT-targeted anti-CSC therapy.
2.3. Avoid conditions needed for the drugs to act- the 3rd line
2.3.1. Intracellular drug inactivation
What if the drug efflux has failed and the drug has invaded the cytoplasm of CSCs? Interestingly, the poison filtering organs like the liver lack ABCTs. However, liver cells are highly drug-resistant because the cells contain enzymes such as the cytochrome-c p450 that can effectively detoxify the drugs in the cytoplasm. On the other hand, some therapeutic drugs are given in a pro-form that needs to be activated after administration. Tumor cells that lack the drug inactivating enzymes or possess the drug activating enzymes are sensitive to the drugs. Conversely, high levels of drug inactivating enzymes or low expression of the drug activating enzymes would make the cells resistant to the drugs as in the case of CSCs. Below are a few examples of such enzymes. The thiol glutathione inactivates platinum drugs (113). Thymidine phosphorylase converts capecitabine into 5-fluorouracil (5-FU) (114). The antimetabolite drugs such as 5-FU and methotrexate need to be converted further into their most active forms to be therapeutically effective, which does not occur when the target cells lack the enzyme activities (115, 116). For example, in CSCs expression of the thymidine phosphorylase can be inhibited via epigenetically silencing mechanisms such as gene promoter methylation catalyzed by the DNA methyltransferases (DNMTs), resulting in capecitabine resistance (117). Using inhibitors of DNMTs can thus sensitize the CSCs to capecitabine. Epigenetic silencing can also activate drugs. For example, UDP glucuronosyltransferase 1 (UGT1A1) is an enzyme that inactivate the topoisomerase I inhibitor irinotecan which is associated with the drug resistance. If UGT1A1 gene promoter is methylated in the cells, irinotecan activity is maintained that sensitizes the cells (118, 119). The aldehyde dehydrogenase (ALDH) is a major marker of CSCs in many cancer types (120) associated with poor prognosis (121–123). ALDH catalyzes the oxidation of aldophosphamide to carboxyphosphamide, the primary mechanism of cyclophosphamide detoxification (124) that occurs in normal stem cells to protect them. This same mechanism, however, is hijacked by CSCs to counteract cyclophosphamide and various relevant chemotherapeutic drugs including temozolomide (125), 4-hydroperoxycyclophosphamide (126), irinotecan (38), paclitaxel, epirubicin and doxorubicin (127, 128).
What if the drug inactivation mechanisms fail in the cytoplasm? Theoretically, the CSC would do something to protect important cytoplasmic components from being damaged and to prevent the drug from further entering the nucleus and subsequently damaging the genomic DNA. Chemotherapy has been shown to activate autophagy. Autophagy is a cellular protective mechanism that promotes cell survival by sacrificing some relatively less important cytoplasmic components in response to catastrophic stresses derived from metabolic, therapeutic or mechanical pressure. Several reports have shown that blocking autophagy pathways using an inhibitor of autophagy such as chloroquine and hydroxychloroquine can sensitize cancer cells to chemotherapies (129, 130). Although extensive studies are needed in order to understand the details regarding role of autophagy for chemoresistance, it would be interesting to test if there are any ABCTs expressed on the membrane of autophagosomes. Do these ABCTs cleanse the drug that has already entered the cytoplasm by pumping the drug from the cytoplasm into autophagosomes? Then does the cell somehow send the drug-loaded autophagosomes out of the cell? Recent studies have shown that in addition to the plasma membrane, nuclear membrane also expresses some of the ABCTs (131–134). Do these ABCTs, like the cell surface ABCTs, pump the drug that has entered the nucleus out of it so that the nuclear DNA can be protected? This would be another interesting possibility to look into.
2.3.2. Quiescence and dormancy
What if the drug has already entered the cytoplasm and even nucleus and is ready to attack the vital intracellular machineries? What does the cell do in this phase to avoid the state susceptible to the potential attack? One of the ‘safe’ states is non-dividing, i.e., quiescence or dormancy. As described above, chemotherapy (as well as radiotherapy) targets fast proliferating cells. It is generally believed that both normal ASCs and CSCs stay in the quiescent phase of the cell cycle most of the times (135–137). Therefore, unlike the rapidly dividing cells, the relatively quiescent CSCs can avoid the attacks from most of the chemotherapeutic drugs. A recent study tracing glioma stem cells in a transgenic mouse model (15) has demonstrated that the slow-cycling tumor cells survived the alkylating drug temozolomide, which eventually led to recurrence. The tumor bearing mice survived for a much longer time if the slow-cycling cells were removed from the tumor. In melanoma, expression of the H3K4 demethylase JAR-ID1B is restricted to a small subset of slow-cycling cells with a doubling time of > 4 weeks. Knockdown of JARID1B from these cells leads to their failure to expand, resulting in reduction in tumor growth and metastases (138). A very small subset of slowly cycling cells specifically retaining the lipophilic labeling dye DiI or the carboxyfluorescein diacetate succinimidyl ester was identified in pancreatic, colon and breast tumors to be responsible for the invasive potential, chemoresistance and relapse (139, 140). Several studies have shown that induction of dormant leukemic CSCs to enter the cell cycle using granulocyte colony-stimulating factor (G-CSF), promyelocytic leukaemia protein (PML) inhibitors or histone deacetylase inhibitors can prime the sensitization of the otherwise slow-cycling CSCs to the subsequent chemotherapies (39, 141, 142).
2.4. Fix damages caused by the drugs - the 4th line
2.4.1. DNA-damage response and repair
The vast majority of chemotherapeutic drugs kill cells by inducing DNA damage (143). Fast dividing cells are sensitive to chemotherapy because they give the drug more chances to interact with and damage their nuclear DNA. DNA damage is inevitable as long as the cell has exposed its DNA to the drug even if to a much slower rate as in the case of slow-cycling CSCs. In normal cells there exist a variety of DNA damage response (DDR) and DNA repair mechanisms that constantly monitor and repair DNA damage to maintain the genomic stability and protect the cell from DNA damage-mediated death. Unfortunately, these mechanisms are inherited by tumor cells and even enhanced in CSCs (144). Unless un-repairable DNA damage occurs, DNA repair is another main reason for chemoresistance of tumor cells particularly CSCs (143, 145).
DNA repair mechanisms are largely categorized into two classes, 1) those that fix single-strand damages including dealkylation (that removes alkyl group from DNA to restore normal DNA structure), base excision repair (BER that removes the wrong base to fix minor, non-structure-distorting damage to DNA), nucleotide excision repair (NER that replaces a fragment of the strand containing a DNA adduct to fix larger, helix-distorting damage), mismatch repair (MMR that corrects miscopied DNA sequences overlooked by DNA polymerases that are responsible for microsatellite instability of the genome) and error-prone repair (EPR that fixes the damaged strand based on a guess of identity of the nucleotide damaged using enzymes lacking proofreading capability), and 2) those that fix double-strand breaks including homology-directed repair (HDR, a sister chromatid based re-synthesis of DNA to fill the gap formed after the double strand break is excised) and non-homologous end joining (NHEJ that re-synthesizes DNA using the resection-generated single strand DNA on the end of the DNA as template to fill the gap formed after the double strand break is excised when sister chromatid is not available particularly on the G1 phase of the cell cycle).
It is an obvious anticancer strategy to combine DNA-damaging agents with DNA repair inhibitors. Inhibiting poly (ADP-ribose) polymerase 1 (PARP1) prevents BER, leading to the double-strand breaks. However, if the cancer cells have a functional double strand break repair mechanism such as the expression of breast cancer associated genes (BRCAs), inhibiting PARP1 alone would not cause un-repairable, death-inducing DNA damage. Cancer cells that do not express functional BRCAs (146) are particularly sensitive to PARP1 inhibitors, suggesting that targeting redundant DNA repair mechanisms simultaneously for induction of so-called synthetic lethality is important to sensitize cancer cells to DNA damaging drugs (147). Notably, aberrant high expression of the excision repair cross-complementing 1 (ERCC1) protein has been associated with chemoresistance to cisplatin in cancer of the lung, stomach and ovary (148, 149) but not testis where there is only marginal expression of ERCC1 (150). MMR deficiency, such as hypermethylation of MLH1 or MLH2, mediates the microsatellite instability that has been linked to resistance of numerous cancer types to a variety of chemotherapeutic agents including the alkylating agents procarbazine, temozolomide, the busulfan, cisplatin and carboplatin, the antimetabolite 6-thioguanine, and the topoisomerase II inhibitors etoposide and doxorubicin (151).
Rapidly growing evidence supports a role of DNA repair for CSC chemoresistance. It has been shown that DNA damage checkpoint and repair proteins such as the ATM, Chk1/2, p53, BRCAs and XRCC5 are aberrantly overexpressed or overactivated in CSCs but not in non-CSCs (152), and is further activated by DNA-damaging therapy such as radiation rendering delayed cell division and prolonged DNA repair time leading to resistance (153–155). Indeed, inhibition of the DNA repair pathways can sensitize CSCs of various cancer types to chemotherapy or radiotherapy. Inhibition of Chk1 or ATM sensitizes the CD24+/CD44+/ESA+ pancreatic or breast CSCs to gemcitabine (156) or radiation (157) treatment. Knockdown of the DNA repair gene O6-methylguanine-DNA methyltransferase (MGMT) or inhibition of the G2 checkpoint kinase Wee1 sensitizes gliomas to temozolomide as well as radiotherapy (158–160). Inhibition of DNA-PKcs sensitizes glioblastoma CSCs to radiation-induced death (161). BMI1, the polycomb group E3-ubiquitin ligase, plays a critical role in assembling DNA repair machinery. Recent studies have shown that BMI1 expression is higher and enhanced by irradiation in CSCs (162–165). Ablation of bmi1 in CSCs promotes double-strand breaks and subsequent radiosensitivity whereas overexpressing BMI1 increases radioresistance (163, 166). These data support DNA repair pathway targeted therapies to overcome CSC resistance.
2.5. Lift up the pro-survival and anti-apoptotic power - the 5th line
2.5.1. Over-activation of pro-survival signaling
If left unrepaired, DNA damage will eventually lead to programmed cell death or apoptosis. Apoptosis is a physiological program controlled by a tightly regulated balance between pro-survival, anti-apoptotic mechanisms and pro-apoptotic mechanisms that eliminate sick, aged or unwanted cells. However, in cancer cells, this balance is frequently and aberrantly tilted to prevent apoptosis even when DNA repair fails. The same is more evident in CSCs. Similar to normal stem cells CSCs rely on specific signaling pathways for maintaining essential proliferation, survival and the balance between self-renewal and differentiation. In response to therapies, CSCs either over-activate pro-survival and anti-apoptotic signaling or down-regulate pro-apoptotic signaling as another mechanism of resistance to therapies.
Several pro-survival signaling pathways have been indicated to play a role in CSCs including the pathways of Notch, Hedgehog (Hh), Wnt, epidermal growth factor receptors (EGFR), bone morphogenetic proteins (BMP), insulin growth factor (IGF), extracellular signal regulated kinases (ERKs), phosphatidylinositol-3-kinase (PI3K)/protein kinase B (PKB or AKT), Janus kinase/signal transducers and activators of transcription (JAK/STAT), and nuclear factor (NF)-κB. Inhibition of these pathways has led to abrogation of CSCs and tumorigenicity (167–173). Notch pathway regulates cell interaction, proliferation, differentiation and apoptosis. Notch signaling can be blocked by impeding its interaction with ligand, inhibiting γ-secretase or interfering with its co-activator MAML1 (167). Inhibition of Notch signaling has been shown to cause a reduction in Akt activity and Mcl-1 expression in glioblastoma CSCs (174) and enhance CSC apoptosis in medulloblastoma (175). Clinical trials of the Notch inhibitors are in progress for treating glioblastoma, leukemia and breast cancer (167). Hh pathway plays a role in maintaining tissue polarity and stemness. Overactivation of Hh pathway was found in CSCs of breast cancer and chronic myeloid leukemia (CML) (167). Inhibition of Hh pathway using cyclopamine reduces glioblastoma stemness (176, 177). Clinical trials of the Hh inhibitors are underway for cancers of the breasts, prostate, lungs, and brain (167). Wnt signaling regulates cell fate determination and tissue self-renewal. This pathway is highly associated with CSC activity (167). Its overactivation has been shown in 5-FU-resistant colorectal CSCs and silencing its downstream main effector TCF4 sensitizes the tumor to radiotherapy (178). EGFR plays a critical role in cancer resistance to various chemotherapies (179–182). EGFR-targeted therapies sensitize various tumor types to agents such as 5-FU, irinotecan, paclitaxel and TRAIL (180–182). Glioblastoma CSCs are resistant to irradiation with aberrantly high Akt activity and double strand break DNA repair capacity. Inhibiting Akt in the CSCs by blocking EGF (168, 183) or Wnt (184) signaling suppresses the cell proliferation and enhances the irradiation-induced DNA damages. Inhibition of Akt has achieved similar sensitizing effect in breast CSCs (185). Forced expression of BMP receptor 1B leads to differentiation and reduced tumorigenecity of patient glioblastoma CSCs (169). Knockdown of IGF-R sensitizes the resistant non-small cell lung cancer (NSCLC) CSCs to radiation (172). Inhibition of STAT3 induces apoptosis in the CSCs in HNSCC (170) and NSCLC (171) tumors resulting in reduced stemness and tumorigenecity. Inhibition of NF-κB hinders the stemness of CSCs in pancreatic cancer (173) and glioblastoma (186). It should be noted that these stem cell signaling pathways often act together and for this reason, simultaneous inhibition of more than one of them is likely needed for effective CSC targeting.
2.5.2. Overactivation of anti-apoptotic and overinhibition of pro-apoptotic signaling
Chemoresistance of cancer cells are typically linked to aberrantly overexpressed or overactivated anti-apoptotic proteins including the BCL-2 family proteins, inhibitors of apoptosis (IAPs) and the caspase 8 inhibitor FLIP (187) and aberrant reduction in expression or activity of the pro-apoptotic proteins such as BIM. These proteins are localized at mitochondria where they play counteracting roles against each other (188–190). Drugs mimicking the IAP antagonist second mitochondria-derived activator of caspases (SMAC) or causing IAP protein degradation have been shown to sensitize various tumor types to chemotherapy and their clinical trials are underway (191). Germline deletion of bim gene has been reported in an Asian population of cancer patients with CML and EGFR-mutated lung cancer intrinsically resistant to tyrosine kinase inhibitor (TKI) therapies (192). Treatment with TKIs induces BIM expression and apoptosis in these cancer cells with inhibition of Akt and Erk (193–195). For this reason, BIM expression has recently been used to predict clinical responsiveness to inhibitors of EGFR, HER2 and PI3K (196). A recent study has shown that treatment with pro-apoptotic BH3 peptide can sensitize chemoresistant cells of several cancer types to chemotherapy (197). This indicates that BCL-2 family proteins play a critical role for cancer cell survival and chemoresistance. It is shown that the glioblastoma CSCs (CD133+) isolated from primary cultures express higher levels of BCL-2, BCLXL, XIAP and FLIP than the non-CSCs (CD133−) (29), and the CSCs are resistant to TRAIL-induced cell death (198). Inhibiting Bcl-2 sensitizes these CSCs to TRAIL death effect both in culture and in tumor-bearing mice (199). Silencing c-FLIP sensitizes CSCs to cisplatin or TRAIL therapy (200, 201). Inhibition of Bcl-2, survivin and XIAP sensitizes prostate CSCs to apoptosis (202, 203). These results hold promise for tilting down anti-apoptotic activity to effectively sensitize cancer to chemotherapy (204).
The role of autophagy in cancer is paradoxical as it functions both to suppress tumor progression and promote cell survival in response to catastrophic stresses (205). CSCs take advantage of the pro-survival side of this double-edged sword feature of autophagy. Many anticancer therapies including chemo-, radio- and targeted therapies have been shown to activate autophagy and subsequent therapy resistance in cancer cells, and inhibiting autophagy sensitizes tumor to chemotherapies resulting in tumor regression (129, 130). In addition, resistance to drug-induced differentiation may also play a role in protecting CSCs from chemotherapeutic death effect.
2.6. Regenerate self - the 6th line
2.6.1. Epithelial-mesenchymal transition (EMT)
EMT is physiologically designed for the epithelial cells to change so that the cells can migrate away during embryonic developmental processes such as gastrulation. During EMT, epithelial cells undergo morphological changes into fibroblast-like mesenchymal phenotype. Typically, the epithelial cells change from a polarized monolayer where they are connected side-by-side and shoulder-by-shoulder via various types of cell-cell junctions into isolated or scattered cells that lose cell-cell interactions and become more motile and invasive. At the molecular level, an expression switch from epithelial marker genes such as E-cadherin and β-catenin to mesenchymal marker genes such as vimentin and fibronectin is turned on by various types of EMT-inducing transcription factors (EIFs) such as Snail, Twist, Zebs and krüppel-like factor 8 (KLF8). These EIFs have recently been found to work closely with microRNAs particularly the miR200 family and miR146a to control EMT, CSC induction and therapy resistance (206–216) (A recent review has more details (217)). In addition to embryonic development, wound healing also requires EMT on the wound edges so that the cells can migrate efficiently towards the center of the wound to eventually heal the wound. Invasive tumor cells hijack this wound healing mechanism to dissociate from the primary tumor mass, migrate away and invade through the stromal matrix including basement membrane that constrains the tumor mass and envelops the vascular vessels to eventually enter the circulation and reach distant metastatic sites (218).
Importantly, EMT has recently been linked to both CSCs and therapy resistance of cancer. Cells undergone EMT gain CSC-like features and CSCs exhibit a mesenchymal phenotype (22, 219, 220). EMT induced by Twist (22), Snail (221) and KLF8 (214) is all accompanied by the induction of CSC properties. Mouse mammary stem cells exhibit a mesenchymal phenotype (22, 222) and transforming growth factor beta (TGF-β) induces both EMT and cell renewal capabilities in human mammary epithelial cells (220). Association of EMT with the CSC properties was also found in metastatic breast (223) and colorectal (224) cancer cells. Many other EMT-regulating signaling pathways such as the Wnt, Notch and Hedgehog pathways were also found to be critical for CSCs (222, 225, 226). Lastly, CSCs express high levels of EMT markers (12). Drug resistance is an intrinsic mechanism of normal stem cells that protects them like seeds for embryonic development or tissue regeneration and repair. Like normal stem cells, CSCs have been found to associate with EMT as well as acquired therapy resistance in various types of cancer (12). Mesenchymal (but not epithelial) phenotype and/or gene expression signature has been linked to therapy resistance in many cancer types including cancers of the lungs (227, 228), head and neck (229, 230), pancreas (44, 231, 232), colon (233), breast (214, 234–238) and ovaries (231, 239) against targeted therapies using erlotinib, gefitinib, lapatinib or tamoxifen as well as chemotherapies using cetuximab, taxol, paclitaxel, vincristine and oxaliplatin, gemcitabine or oxaliplatin. Various studies have provided evidence supporting a role of Notch signaling for cancer chemoresistance (214, 240–243).
2.6.2. CSC plasticity and dynamics
For more than a century, “terminally differentiated cell” has been the terminology used to describe cells that have completed cellular differentiation pathway and believed to no longer be capable of proliferating. The vast majority of this cell category happens to be a component of the epithelia that cover the skin surface or line the lumen of the tubular or ductal organs and are the tumor origin of more than 80% of all cancer types. This terminology, however, has no longer been correct since the induced pluripotent stem cells (iPSCs) were created via dedifferentiation of the “terminally differentiated” cells by re-activation of a few reprogramming transcription factors (RPFs) (244–247) as illustrated above in Figure 1. Similarly to RPFs, EIFs specifically grant the stem capability back to “terminally differentiated” normal or non-tumorigenic epithelial cells. This EMT-associated regeneration of stem or stem-like cells may be critical for refreshing adult epithelial stem cell pool in response to their loss due to any cause. For example, depletion of hair follicle stem cells is followed by repopulation of the stem cells from differentiated skin cells (12). However, the same mechanism could contribute to the initiation of tumorigenic CSCs as is seen in the cells overexpressing the EIFs Twist, Snail or KLF8 (22, 214, 221). This same mechanism could also be utilized in cancer to regenerate CSCs from non-stem cancer cells in the tumor in response to loss of CSCs due to anticancer therapies (248–250). Thus, regeneration of CSCs by EMT is a likely mechanism for chemoresistance of cancer and relapse just as normal ASCs repopulate and redistribute when encountering massive damage by radiation. Indeed, rapid repopulation of CSCs is believed to occur in human tumors during radiotherapy (251), and redistribution of CSCs to the quiescent phase of the cell cycle makes the cells more resistant to radiotherapy (137, 252). The regeneration process could be responsible for the heterogeneous phenotypes of CSCs within a same tumor as recently discovered in melanoma (138). This mechanism of CSC plasticity associated with EMT provides a new challenge for the concept of anti-CSC monotherapy that has been thought to be capable of eradicating the source of tumor. Obviously, elimination and prevention of the regeneration of CSCs are equally important for CSC-targeted therapy.
2.7. Perish together - the last line of defense
The large overlap of the mechanisms of action in CSCs with those in normal stem cells or non-stem cells makes CSC targeting difficult because of likely toxic side effects on the normal cells. This makes CSC-specific targeted therapy particularly important to prevent normal cells and eventually the patient from being harmed alongside the CSCs.
3. An update on CSC-targeted therapy studies
The definition of targeted anticancer therapy is two-fold: 1) To disable the molecules in the tumor cells being targeted and thus the tumor cells. 2) To destroy the tumor cells being targeted by cancer cell-specific molecule-guided delivery of non-targeted drug, mostly chemotherapeutic drugs. Several scores of CSC-targeted small molecule compounds have been reported as outlined in Table 1. These compounds are designed or selected to directly inhibit CSC. Not surprisingly, most of these compounds target the survival/apoptosis and stem signaling pathways in CSCs. Others target the ABCTs and EMT. While this list of compounds is rapidly growing, CSC-specific molecule, such as CD44, directed delivery of non-targeted drugs has drawn increasing attention (253, 254).
Table 1.
CSC-targeted small molecule monotherapy studies
| Mechanisms | Agents | Cancer Types | References |
|---|---|---|---|
| Targeted | |||
| Survival/apoptosis | |||
| NF-κB | Eriocalyxin | Ovarian | (255) |
| NF-κB | MK-5108 | Ovarian | (256) |
| NF-κB | Morusin | Cervical | (257) |
| NF-κB | Parthenolide | Multiple myeloma | (258) |
| NF-κB | Andrographolide | Multiple myeloma | (258) |
| STAT3 | Galiellalactone | Prostate | (259) |
| STAT3 | STX-0119 | Glioblastoma | (260) |
| STAT3 | Tanshinone IIA | Breast | (261) |
| STAT3 | WP1193 | Glioblastoma | (262) |
| Akt, mTOR | Rottlerin | Pancreatic | (263) |
| Akt, MAPK | Sorafenib | Glioblastoma | (264) |
| Akt, MAPK | Strigolactone | Breast | (265) |
| Akt | Harmine | Glioblastoma | (266) |
| Metabolism | Niclosamide | Ovarian | (267) |
| Metabolism | 3-bromopyruvate | Pancreatic | (268) |
| Metabolism | 2-deoxyglucose | Breast | (269) |
| MAPK | Icaritin | Breast | (270) |
| MAPK | Imatinib | Glioblastoma | (271) |
| Survivin | LLP-3 | Glioma | (272) |
| Bcl-2 | ABT-737 | Glioma | (199) |
| FAK, ROCK1 | Atorvastatin | Prostate | (273) |
| AMPK | Metformin | Pancreatic | (274) |
| Telomerase | MST312 | Lung | (275) |
| Mcl-1 | Omacetaxine | CML | (276) |
| Stem signaling | |||
| Wnt | Phosphosulindac | Breast | (277) |
| Wnt | Salinomycin | Endometrial | (278–281) |
| Wnt | Acetaminophen | Breast | (282) |
| Wnt | Celecoxib | Colon | (283) |
| Wnt, IGF-1R | Adamantyl retinoid | Pancreatic | (284) |
| Wnt | Oximatrine | Breast | (285) |
| Wnt, hedgehog | Sulforaphane | Breast, pancreatic | (286–288) |
| Hedgehog | Cyclopamine | Glioblastoma | (176) |
| Hedgehog | Erismodegib | Prostate | (203) |
| Hedgehog | Vismodegib | Pancreatic | (289) |
| Hedgehog | GANT-61 | Pancreatic | (290) |
| Notch | DAPT | Ovarian | (291) |
| Notch | MRK-003 | Breast | (292) |
| Notch | Retinoic acid | Brain | (293, 294) |
| Notch | RO4929097 | Melanoma | (295) |
| Stem factors | SB-T-1214 (taxoid) | Colon | (281) |
| c-Met | Cabozantinib | Pancreatic | (296) |
| ABCTs | |||
| ABCG2 | Curcumin | Colon | (297) |
| ABCG2 | Imatinib, nilotinib | Hematopoietic | (298) |
| ABCG2 | Mithramycin | Lung, esophageal | (299) |
| DNA repair | |||
| ATM, ATR | CCT129202 | Lung | (300) |
| PARP-1 | NSC747854 | Lung | (301) |
| CSC niches/stroma | |||
| HIF1α | 17-AAG | Lymphoma | (302) |
| Glycosaminoglycan | G2.2 | colon | (303) |
| EMT | |||
| EMT/Stem factors | Resveratrol | Pancreatic | (304) |
| EMT/NF-κB | Lupeol | Head and neck | (305) |
| EMT | Cystatin C | Breast | (306) |
| EMT | Dasatinib | Breast | (307) |
| Drug metabolism | |||
| AhR | Tranilast | Breast | (308) |
4. Conclusion
Studies on CSCs have raised tremendous hope for designing tumor cell eliminating anticancer therapy. These same studies have also revealed significant challenges due to the multiple step defense strategy used by CSCs against chemotherapy, leading to the important clinical concerns such as chemoresistance, metastasis and relapse. Since other types of anticancer therapies, particularly radiotherapy, share much in therapeutic mechanisms of action, the mechanisms underlying CSCs chemoresistance might as well be applicable to other types of therapy such as radiotherapy, targeted therapy as well as anti-stromal therapy. The similarity in self-defense between CSCs and normal stem cells and even non-stem cells requires development of smart CSC-specific anticancer therapy. The CSC plasticity and regeneration underscore the importance of combination of CSC-specific therapy with other therapies including the mainstream conventional therapies such as chemotherapy and radiotherapy to prevent regeneration, repopulation and redistribution of CSCs from non-stem tumor cells. Lastly, patient’s individual difference in CSC properties may require patient stratification as well for effective CSC-based anticancer strategies.
Acknowledgments
I am grateful to some of my lab members including Justin Gray, Debarati Mukherjee, Satadru K. Lahiri and Lin Yu for their critical discussions and technical assistance. This work was supported by the NIH-NCI grant (R01CA132977) to J.Z. I apologize to colleagues whose important contributions were not cited due to page limitations. I also wish to dedicate this work to the memory of my father who lost his battle against cancer during my preparation of this manuscript.
Abbreviations
- 5-FU
5-fluorouracil
- ABCT
ATP-binding cassette transporter
- ALDH
aldehyde dehydrogenase
- AML
acute myeloid leukemia
- ASC
adult stem cell
- BCRP or ABCG
breast cancer resistance protein
- BER
base excision repair
- BMP
bone morphogenetic proteins
- BRCA
breast cancer associated gene
- CML
chronic myeloid leukemia
- CSC
cancer stem cell
- DDR
DNA damage response
- DNMT
DNA methyltransferase
- ECM
extracellular matrix
- EGFR
epidermal growth factor receptor
- ERCC1
excision repair cross-complementing 1
- EMT
Epithelial-mesenchymal transition
- EIF
EMT-inducing factor
- EPR
error-prone repair
- ERK
extracellular signal regulated kinase
- FGF
fibroblast growth factor
- G-CSF
granulocyte colony-stimulating factor
- HDR
homology-directed repair
- HGF
hepatocyte growth factor
- Hh
Hedgehog
- HIF
hypoxia-inducible factor
- HSC
hematopoietic stem cells
- IAP
inhibitor of apoptosis
- iPSC
induced pluripotent stem cell
- IGF
insulin growth factor
- IL
interleukin
- JAK
Janus kinase
- KLF8
krüppel-like factor 8
- MDS
myelodysplastic syndrome
- MRD
minimal residual disease
- ROSs
reactive oxygen species
- MDR1 or ABCB1
multidrug resistance protein 1
- MMR
mismatch repair
- MRP1 or ABCC1
multidrug resistance-associated protein 1
- NER
nucleotide excision repair
- NF-κB
nuclear factor-kappa B
- NHEJ
non-homologous end joining
- HNSCC
head and neck squamous cell carcinoma
- NSCLC
non-small cell lung cancer
- PARP-1
poly (ADP-ribose) polymerase 1
- PI3K
phosphatidylinositol-3-kinase
- PKB or AKT
protein kinase B
- PML
promyelocytic leukaemia
- RPF
reprogramming factors
- SMAC
second mitochondria-derived activator of caspase
- SP cell
side-population cell
- STAT
signal transducer and activator of transcription
- TGF-β
transforming growth factor beta
- TKI
tyrosine kinase inhibitor
- TSG
tumor suppressor gene
- UGT1A1
uridine diphosphate (UDP) glucuronosyltransferase 1
- VEGF
vascular endothelial growth factor
Footnotes
Conflict of interest statement
The author declares that there are no conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Lind MJ. Principles of cytotoxic chemotherapy. Medicine. 2011;39:6. [Google Scholar]
- 2.Lind MJ. Principles of cytotoxic chemotherapy. Medicine. 2008;36:5. [Google Scholar]
- 3.Malhotra V, Perry MC. Classical chemotherapy: mechanisms, toxicities and the therapeutic window. Cancer Biol Ther. 2003;2:S2–4. [PubMed] [Google Scholar]
- 4.Szakacs G, Paterson JK, Ludwig JA, Booth-Genthe C, Gottesman MM. Targeting multidrug resistance in cancer. Nat Rev Drug Discov. 2006;5:219–234. doi: 10.1038/nrd1984. [DOI] [PubMed] [Google Scholar]
- 5.Airley R. Cancer Chemotherapy 2009 [Google Scholar]
- 6.Ghiaur G, Gerber J, Jones RJ. Concise review: Cancer stem cells and minimal residual disease. Stem Cells. 2012;30:89–93. doi: 10.1002/stem.769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gupta PB, Chaffer CL, Weinberg RA. Cancer stem cells: mirage or reality? Nat Med. 2009;15:1010–1012. doi: 10.1038/nm0909-1010. [DOI] [PubMed] [Google Scholar]
- 8.Frank NY, Schatton T, Frank MH. The therapeutic promise of the cancer stem cell concept. J Clin Invest. 2010;120:41–50. doi: 10.1172/JCI41004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dirks P. Cancer stem cells: Invitation to a second round. Nature. 2010;466:40–41. doi: 10.1038/466040a. [DOI] [PubMed] [Google Scholar]
- 10.Schatton T, Frank NY, Frank MH. Identification and targeting of cancer stem cells. Bioessays. 2009;31:1038–1049. doi: 10.1002/bies.200900058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nguyen LV, Vanner R, Dirks P, Eaves CJ. Cancer stem cells: an evolving concept. Nat Rev Cancer. 2012;12:133–143. doi: 10.1038/nrc3184. [DOI] [PubMed] [Google Scholar]
- 12.Beck B, Blanpain C. Unravelling cancer stem cell potential. Nat Rev Cancer. 2013;13:727–738. doi: 10.1038/nrc3597. [DOI] [PubMed] [Google Scholar]
- 13.Tang C, Ang BT, Pervaiz S. Cancer stem cell: target for anti-cancer therapy. FASEB J. 2007;21:3777–3785. doi: 10.1096/fj.07-8560rev. [DOI] [PubMed] [Google Scholar]
- 14.Meacham CE, Morrison SJ. Tumour heterogeneity and cancer cell plasticity. Nature. 2013;501:328–337. doi: 10.1038/nature12624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chen J, Li Y, Yu TS, McKay RM, Burns DK, Kernie SG, Parada LF. A restricted cell population propagates glioblastoma growth after chemotherapy. Nature. 2012;488:522–526. doi: 10.1038/nature11287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Driessens G, Beck B, Caauwe A, Simons BD, Blanpain C. Defining the mode of tumour growth by clonal analysis. Nature. 2012;488:527–530. doi: 10.1038/nature11344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schepers AG, Snippert HJ, Stange DE, van den Born M, van Es JH, van de Wetering M, Clevers H. Lineage tracing reveals Lgr5+ stem cell activity in mouse intestinal adenomas. Science. 2012;337:730–735. doi: 10.1126/science.1224676. [DOI] [PubMed] [Google Scholar]
- 18.Creighton CJ, Li X, Landis M, Dixon JM, Neumeister VM, Sjolund A, Rimm DL, Wong H, Rodriguez A, Herschkowitz JI, Fan C, Zhang X, He X, Pavlick A, Gutierrez MC, Renshaw L, Larionov AA, Faratian D, Hilsenbeck SG, Perou CM, Lewis MT, Rosen JM, Chang JC. Residual breast cancers after conventional therapy display mesenchymal as well as tumor-initiating features. Proc Natl Acad Sci U S A. 2009;106:13820–13825. doi: 10.1073/pnas.0905718106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gerber JM, Smith BD, Ngwang B, Zhang H, Vala MS, Morsberger L, Galkin S, Collector MI, Perkins B, Levis MJ, Griffin CA, Sharkis SJ, Borowitz MJ, Karp JE, Jones RJ. A clinically relevant population of leukemic CD34(+)CD38(−) cells in acute myeloid leukemia. Blood. 2012;119:3571–3577. doi: 10.1182/blood-2011-06-364182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tehranchi R, Woll PS, Anderson K, Buza-Vidas N, Mizukami T, Mead AJ, Astrand-Grundstrom I, Strombeck B, Horvat A, Ferry H, Dhanda RS, Hast R, Ryden T, Vyas P, Gohring G, Schlegelberger B, Johansson B, Hellstrom-Lindberg E, List A, Nilsson L, Jacobsen SE. Persistent malignant stem cells in del(5q) myelodysplasia in remission. N Engl J Med. 2010;363:1025–1037. doi: 10.1056/NEJMoa0912228. [DOI] [PubMed] [Google Scholar]
- 21.Woll PS, Kjallquist U, Chowdhury O, Doolittle H, Wedge DC, Thongjuea S, Erlandsson R, Ngara M, Anderson K, Deng Q, Mead AJ, Stenson L, Giustacchini A, Duarte S, Giannoulatou E, Taylor S, Karimi M, Scharenberg C, Mortera-Blanco T, Macaulay IC, Clark SA, Dybedal I, Josefsen D, Fenaux P, Hokland P, Holm MS, Cazzola M, Malcovati L, Tauro S, Bowen D, Boultwood J, Pellagatti A, Pimanda JE, Unnikrishnan A, Vyas P, Gohring G, Schlegelberger B, Tobiasson M, Kvalheim G, Constantinescu SN, Nerlov C, Nilsson L, Campbell PJ, Sandberg R, Papaemmanuil E, Hellstrom-Lindberg E, Linnarsson S, Jacobsen SE. Myelodysplastic syndromes are propagated by rare and distinct human cancer stem cells in vivo. Cancer Cell. 2014;25:794–808. doi: 10.1016/j.ccr.2014.03.036. [DOI] [PubMed] [Google Scholar]
- 22.Mani SA, Guo W, Liao MJ, Eaton EN, Ayyanan A, Zhou AY, Brooks M, Reinhard F, Zhang CC, Shipitsin M, Campbell LL, Polyak K, Brisken C, Yang J, Weinberg RA. The epithelial-mesenchymal transition generates cells with properties of stem cells. Cell. 2008;133:704–715. doi: 10.1016/j.cell.2008.03.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Polyak K, Weinberg RA. Transitions between epithelial and mesenchymal states: acquisition of malignant and stem cell traits. Nat Rev Cancer. 2009;9:265–273. doi: 10.1038/nrc2620. [DOI] [PubMed] [Google Scholar]
- 24.Borst P, Jonkers J, Rottenberg S. What makes tumors multidrug resistant? Cell Cycle. 2007;6:2782–2787. doi: 10.4161/cc.6.22.4936. [DOI] [PubMed] [Google Scholar]
- 25.Broxterman HJ, Gotink KJ, Verheul HM. Understanding the causes of multidrug resistance in cancer: a comparison of doxorubicin and sunitinib. Drug Resist Updat. 2009;12:114–126. doi: 10.1016/j.drup.2009.07.001. [DOI] [PubMed] [Google Scholar]
- 26.Shafee N, Smith CR, Wei S, Kim Y, Mills GB, Hortobagyi GN, Stanbridge EJ, Lee EY. Cancer stem cells contribute to cisplatin resistance in Brca1/p53-mediated mouse mammary tumors. Cancer Res. 2008;68:3243–3250. doi: 10.1158/0008-5472.CAN-07-5480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.To K, Fotovati A, Reipas KM, Law JH, Hu K, Wang J, Astanehe A, Davies AH, Lee L, Stratford AL, Raouf A, Johnson P, Berquin IM, Royer HD, Eaves CJ, Dunn SE. Y-box binding protein-1 induces the expression of CD44 and CD49f leading to enhanced self-renewal, mammosphere growth, and drug resistance. Cancer Res. 2010;70:2840–2851. doi: 10.1158/0008-5472.CAN-09-3155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hu L, McArthur C, Jaffe RB. Ovarian cancer stem-like side-population cells are tumourigenic and chemoresistant. Br J Cancer. 2010;102:1276–1283. doi: 10.1038/sj.bjc.6605626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Liu G, Yuan X, Zeng Z, Tunici P, Ng H, Abdulkadir IR, Lu L, Irvin D, Black KL, Yu JS. Analysis of gene expression and chemoresistance of CD133+ cancer stem cells in glioblastoma. Mol Cancer. 2006;5:67. doi: 10.1186/1476-4598-5-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Liu T, Cheng W, Lai D, Huang Y, Guo L. Characterization of primary ovarian cancer cells in different culture systems. Oncol Rep. 2010;23:1277–1284. doi: 10.3892/or_00000761. [DOI] [PubMed] [Google Scholar]
- 31.Liu T, Xu F, Du X, Lai D, Liu T, Zhao Y, Huang Q, Jiang L, Huang W, Cheng W, Liu Z. Establishment and characterization of multi-drug resistant, prostate carcinoma-initiating stem-like cells from human prostate cancer cell lines 22RV1. Mol Cell Biochem. 2010;340:265–273. doi: 10.1007/s11010-010-0426-5. [DOI] [PubMed] [Google Scholar]
- 32.Shi MF, Jiao J, Lu WG, Ye F, Ma D, Dong QG, Xie X. Identification of cancer stem cell-like cells from human epithelial ovarian carcinoma cell line. Cell Mol Life Sci. 2010;67:3915–3925. doi: 10.1007/s00018-010-0420-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zhang N, Li R, Tao KS, Cao DY, Ti ZY, Ding R, Cai L, Zhang FQ, Dou KF. Characterization of a stem-like population in hepatocellular carcinoma MHCC97 cells. Oncol Rep. 2010;23:827–831. [PubMed] [Google Scholar]
- 34.Cammareri P, Scopelliti A, Todaro M, Eterno V, Francescangeli F, Moyer MP, Agrusa A, Dieli F, Zeuner A, Stassi G. Aurora-a is essential for the tumorigenic capacity and chemoresistance of colorectal cancer stem cells. Cancer Res. 2010;70:4655–4665. doi: 10.1158/0008-5472.CAN-09-3953. [DOI] [PubMed] [Google Scholar]
- 35.Fang DD, Kim YJ, Lee CN, Aggarwal S, McKinnon K, Mesmer D, Norton J, Birse CE, He T, Ruben SM, Moore PA. Expansion of CD133(+) colon cancer cultures retaining stem cell properties to enable cancer stem cell target discovery. Br J Cancer. 2010;102:1265–1275. doi: 10.1038/sj.bjc.6605610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ong CW, Kim LG, Kong HH, Low LY, Iacopetta B, Soong R, Salto-Tellez M. CD133 expression predicts for non-response to chemotherapy in colorectal cancer. Mod Pathol. 2010;23:450–457. doi: 10.1038/modpathol.2009.181. [DOI] [PubMed] [Google Scholar]
- 37.Todaro M, Alea MP, Di Stefano AB, Cammareri P, Vermeulen L, Iovino F, Tripodo C, Russo A, Gulotta G, Medema JP, Stassi G. Colon cancer stem cells dictate tumor growth and resist cell death by production of interleukin-4. Cell Stem Cell. 2007;1:389–402. doi: 10.1016/j.stem.2007.08.001. [DOI] [PubMed] [Google Scholar]
- 38.Dylla SJ, Beviglia L, Park IK, Chartier C, Raval J, Ngan L, Pickell K, Aguilar J, Lazetic S, Smith-Berdan S, Clarke MF, Hoey T, Lewicki J, Gurney AL. Colorectal cancer stem cells are enriched in xenogeneic tumors following chemotherapy. PLoS One. 2008;3:e2428. doi: 10.1371/journal.pone.0002428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Saito Y, Uchida N, Tanaka S, Suzuki N, Tomizawa-Murasawa M, Sone A, Najima Y, Takagi S, Aoki Y, Wake A, Taniguchi S, Shultz LD, Ishikawa F. Induction of cell cycle entry eliminates human leukemia stem cells in a mouse model of AML. Nat Biotechnol. 2010;28:275–280. doi: 10.1038/nbt.1607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ishikawa F, Yoshida S, Saito Y, Hijikata A, Kitamura H, Tanaka S, Nakamura R, Tanaka T, Tomiyama H, Saito N, Fukata M, Miyamoto T, Lyons B, Ohshima K, Uchida N, Taniguchi S, Ohara O, Akashi K, Harada M, Shultz LD. Chemotherapy-resistant human AML stem cells home to and engraft within the bone-marrow endosteal region. Nat Biotechnol. 2007;25:1315–1321. doi: 10.1038/nbt1350. [DOI] [PubMed] [Google Scholar]
- 41.Toole BP, Slomiany MG. Hyaluronan, CD44 and Emmprin: partners in cancer cell chemoresistance. Drug Resist Updat. 2008;11:110–121. doi: 10.1016/j.drup.2008.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hermann PC, Huber SL, Herrler T, Aicher A, Ellwart JW, Guba M, Bruns CJ, Heeschen C. Distinct populations of cancer stem cells determine tumor growth and metastatic activity in human pancreatic cancer. Cell Stem Cell. 2007;1:313–323. doi: 10.1016/j.stem.2007.06.002. [DOI] [PubMed] [Google Scholar]
- 43.Konopleva M, Tabe Y, Zeng Z, Andreeff M. Therapeutic targeting of microenvironmental interactions in leukemia: mechanisms and approaches. Drug Resist Updat. 2009;12:103–113. doi: 10.1016/j.drup.2009.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Voulgari A, Pintzas A. Epithelial-mesenchymal transition in cancer metastasis: mechanisms, markers and strategies to overcome drug resistance in the clinic. Biochim Biophys Acta. 2009;1796:75–90. doi: 10.1016/j.bbcan.2009.03.002. [DOI] [PubMed] [Google Scholar]
- 45.Wang Z, Li Y, Banerjee S, Sarkar FH. Emerging role of Notch in stem cells and cancer. Cancer Lett. 2009;279:8–12. doi: 10.1016/j.canlet.2008.09.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Dean M, Fojo T, Bates S. Tumour stem cells and drug resistance. Nat Rev Cancer. 2005;5:275–284. doi: 10.1038/nrc1590. [DOI] [PubMed] [Google Scholar]
- 47.Patrawala L, Calhoun T, Schneider-Broussard R, Zhou J, Claypool K, Tang DG. Side population is enriched in tumorigenic, stem-like cancer cells, whereas ABCG2+ and ABCG2− cancer cells are similarly tumorigenic. Cancer Res. 2005;65:6207–6219. doi: 10.1158/0008-5472.CAN-05-0592. [DOI] [PubMed] [Google Scholar]
- 48.Styczynski J, Drewa T. Leukemic stem cells: from metabolic pathways and signaling to a new concept of drug resistance targeting. Acta Biochim Pol. 2007;54:717–726. [PubMed] [Google Scholar]
- 49.Zhou S, Schuetz JD, Bunting KD, Colapietro AM, Sampath J, Morris JJ, Lagutina I, Grosveld GC, Osawa M, Nakauchi H, Sorrentino BP. The ABC transporter Bcrp1/ABCG2 is expressed in a wide variety of stem cells and is a molecular determinant of the side-population phenotype. Nat Med. 2001;7:1028–1034. doi: 10.1038/nm0901-1028. [DOI] [PubMed] [Google Scholar]
- 50.Alonso L, Fuchs E. Stem cells of the skin epithelium. Proc Natl Acad Sci U S A. 2003;100(Suppl 1):11830–11835. doi: 10.1073/pnas.1734203100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bai L, Rohrschneider LR. s-SHIP promoter expression marks activated stem cells in developing mouse mammary tissue. Genes Dev. 2010;24:1882–1892. doi: 10.1101/gad.1932810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Medema JP, Vermeulen L. Microenvironmental regulation of stem cells in intestinal homeostasis and cancer. Nature. 2011;474:318–326. doi: 10.1038/nature10212. [DOI] [PubMed] [Google Scholar]
- 53.Shiozawa Y, Havens AM, Pienta KJ, Taichman RS. The bone marrow niche: habitat to hematopoietic and mesenchymal stem cells, and unwitting host to molecular parasites. Leukemia. 2008;22:941–950. doi: 10.1038/leu.2008.48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Fuchs E, Tumbar T, Guasch G. Socializing with the neighbors: stem cells and their niche. Cell. 2004;116:769–778. doi: 10.1016/s0092-8674(04)00255-7. [DOI] [PubMed] [Google Scholar]
- 55.Spradling A, Drummond-Barbosa D, Kai T. Stem cells find their niche. Nature. 2001;414:98–104. doi: 10.1038/35102160. [DOI] [PubMed] [Google Scholar]
- 56.Harrison H, Rogerson L, Gregson HJ, Brennan KR, Clarke RB, Landberg G. Contrasting hypoxic effects on breast cancer stem cell hierarchy is dependent on ER-alpha status. Cancer Res. 2013;73:1420–1433. doi: 10.1158/0008-5472.CAN-12-2505. [DOI] [PubMed] [Google Scholar]
- 57.Chow DC, Wenning LA, Miller WM, Papoutsakis ET. Modeling pO(2) distributions in the bone marrow hematopoietic compartment. I. Krogh’s model. Biophys J. 2001;81:675–684. doi: 10.1016/S0006-3495(01)75732-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Parmar K, Mauch P, Vergilio JA, Sackstein R, Down JD. Distribution of hematopoietic stem cells in the bone marrow according to regional hypoxia. Proc Natl Acad Sci U S A. 2007;104:5431–5436. doi: 10.1073/pnas.0701152104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kumar SM, Liu S, Lu H, Zhang H, Zhang PJ, Gimotty PA, Guerra M, Guo W, Xu X. Acquired cancer stem cell phenotypes through Oct4-mediated dedifferentiation. Oncogene. 2012;31:4898–4911. doi: 10.1038/onc.2011.656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Wang Y, Liu Y, Malek SN, Zheng P, Liu Y. Targeting HIF1alpha eliminates cancer stem cells in hematological malignancies. Cell Stem Cell. 2011;8:399–411. doi: 10.1016/j.stem.2011.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Zhang H, Li H, Xi HS, Li S. HIF1alpha is required for survival maintenance of chronic myeloid leukemia stem cells. Blood. 2012;119:2595–2607. doi: 10.1182/blood-2011-10-387381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Li Z, Bao S, Wu Q, Wang H, Eyler C, Sathornsumetee S, Shi Q, Cao Y, Lathia J, McLendon RE, Hjelmeland AB, Rich JN. Hypoxia-inducible factors regulate tumorigenic capacity of glioma stem cells. Cancer Cell. 2009;15:501–513. doi: 10.1016/j.ccr.2009.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Kim Y, Lin Q, Zelterman D, Yun Z. Hypoxia-regulated delta-like 1 homologue enhances cancer cell stemness and tumorigenicity. Cancer Res. 2009;69:9271–9280. doi: 10.1158/0008-5472.CAN-09-1605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Bar EE, Lin A, Mahairaki V, Matsui W, Eberhart CG. Hypoxia increases the expression of stem-cell markers and promotes clonogenicity in glioblastoma neurospheres. Am J Pathol. 2010;177:1491–1502. doi: 10.2353/ajpath.2010.091021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Soeda A, Park M, Lee D, Mintz A, Androutsellis-Theotokis A, McKay RD, Engh J, Iwama T, Kunisada T, Kassam AB, Pollack IF, Park DM. Hypoxia promotes expansion of the CD133-positive glioma stem cells through activation of HIF-1alpha. Oncogene. 2009;28:3949–3959. doi: 10.1038/onc.2009.252. [DOI] [PubMed] [Google Scholar]
- 66.Bao B, Ali S, Ahmad A, Azmi AS, Li Y, Banerjee S, Kong D, Sethi S, Aboukameel A, Padhye SB, Sarkar FH. Hypoxia-induced aggressiveness of pancreatic cancer cells is due to increased expression of VEGF, IL-6 and miR-21, which can be attenuated by CDF treatment. PLoS One. 2012;7:e50165. doi: 10.1371/journal.pone.0050165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Bao B, Ahmad A, Kong D, Ali S, Azmi AS, Li Y, Banerjee S, Padhye S, Sarkar FH. Hypoxia induced aggressiveness of prostate cancer cells is linked with deregulated expression of VEGF, IL-6 and miRNAs that are attenuated by CDF. PLoS One. 2012;7:e43726. doi: 10.1371/journal.pone.0043726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Gammon L, Biddle A, Heywood HK, Johannessen AC, Mackenzie IC. Subsets of cancer stem cells differ intrinsically in their patterns of oxygen metabolism. PLoS One. 2013;8:e62493. doi: 10.1371/journal.pone.0062493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Hashimoto O, Shimizu K, Semba S, Chiba S, Ku Y, Yokozaki H, Hori Y. Hypoxia induces tumor aggressiveness and the expansion of CD133-positive cells in a hypoxia-inducible factor-1alpha-dependent manner in pancreatic cancer cells. Pathobiology. 2011;78:181–192. doi: 10.1159/000325538. [DOI] [PubMed] [Google Scholar]
- 70.Schwab LP, Peacock DL, Majumdar D, Ingels JF, Jensen LC, Smith KD, Cushing RC, Seagroves TN. Hypoxia-inducible factor 1alpha promotes primary tumor growth and tumor-initiating cell activity in breast cancer. Breast Cancer Res. 2012;14:R6. doi: 10.1186/bcr3087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Brown JM, Wilson WR. Exploiting tumour hypoxia in cancer treatment. Nat Rev Cancer. 2004;4:437–447. doi: 10.1038/nrc1367. [DOI] [PubMed] [Google Scholar]
- 72.Semenza GL. Hypoxia-inducible factors in physiology and medicine. Cell. 2012;148:399–408. doi: 10.1016/j.cell.2012.01.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Takubo K, Goda N, Yamada W, Iriuchishima H, Ikeda E, Kubota Y, Shima H, Johnson RS, Hirao A, Suematsu M, Suda T. Regulation of the HIF-1alpha level is essential for hematopoietic stem cells. Cell Stem Cell. 2010;7:391–402. doi: 10.1016/j.stem.2010.06.020. [DOI] [PubMed] [Google Scholar]
- 74.Diehn M, Cho RW, Lobo NA, Kalisky T, Dorie MJ, Kulp AN, Qian D, Lam JS, Ailles LE, Wong M, Joshua B, Kaplan MJ, Wapnir I, Dirbas FM, Somlo G, Garberoglio C, Paz B, Shen J, Lau SK, Quake SR, Brown JM, Weissman IL, Clarke MF. Association of reactive oxygen species levels and radioresistance in cancer stem cells. Nature. 2009;458:780–783. doi: 10.1038/nature07733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Smith J, Ladi E, Mayer-Proschel M, Noble M. Redox state is a central modulator of the balance between self-renewal and differentiation in a dividing glial precursor cell. Proc Natl Acad Sci U S A. 2000;97:10032–10037. doi: 10.1073/pnas.170209797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Tsatmali M, Walcott EC, Crossin KL. Newborn neurons acquire high levels of reactive oxygen species and increased mitochondrial proteins upon differentiation from progenitors. Brain Res. 2005;1040:137–150. doi: 10.1016/j.brainres.2005.01.087. [DOI] [PubMed] [Google Scholar]
- 77.Riley PA. Free radicals in biology: oxidative stress and the effects of ionizing radiation. Int J Radiat Biol. 1994;65:27–33. doi: 10.1080/09553009414550041. [DOI] [PubMed] [Google Scholar]
- 78.Carmeliet P, Jain RK. Molecular mechanisms and clinical applications of angiogenesis. Nature. 2011;473:298–307. doi: 10.1038/nature10144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Beck B, Driessens G, Goossens S, Youssef KK, Kuchnio A, Caauwe A, Sotiropoulou PA, Loges S, Lapouge G, Candi A, Mascre G, Drogat B, Dekoninck S, Haigh JJ, Carmeliet P, Blanpain C. A vascular niche and a VEGF-Nrp1 loop regulate the initiation and stemness of skin tumours. Nature. 2011;478:399–403. doi: 10.1038/nature10525. [DOI] [PubMed] [Google Scholar]
- 80.Calabrese C, Poppleton H, Kocak M, Hogg TL, Fuller C, Hamner B, Oh EY, Gaber MW, Finklestein D, Allen M, Frank A, Bayazitov IT, Zakharenko SS, Gajjar A, Davidoff A, Gilbertson RJ. A perivascular niche for brain tumor stem cells. Cancer Cell. 2007;11:69–82. doi: 10.1016/j.ccr.2006.11.020. [DOI] [PubMed] [Google Scholar]
- 81.Hamerlik P, Lathia JD, Rasmussen R, Wu Q, Bartkova J, Lee M, Moudry P, Bartek J, Jr, Fischer W, Lukas J, Rich JN, Bartek J. Autocrine VEGF-VEGFR2-Neuropilin-1 signaling promotes glioma stem-like cell viability and tumor growth. J Exp Med. 2012;209:507–520. doi: 10.1084/jem.20111424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Jain RK. Antiangiogenesis strategies revisited: from starving tumors to alleviating hypoxia. Cancer Cell. 2014;26:605–622. doi: 10.1016/j.ccell.2014.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Butler JM, Nolan DJ, Vertes EL, Varnum-Finney B, Kobayashi H, Hooper AT, Seandel M, Shido K, White IA, Kobayashi M, Witte L, May C, Shawber C, Kimura Y, Kitajewski J, Rosenwaks Z, Bernstein ID, Rafii S. Endothelial cells are essential for the self-renewal and repopulation of Notch-dependent hematopoietic stem cells. Cell Stem Cell. 2010;6:251–264. doi: 10.1016/j.stem.2010.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Kiel MJ, Yilmaz OH, Iwashita T, Yilmaz OH, Terhorst C, Morrison SJ. SLAM family receptors distinguish hematopoietic stem and progenitor cells and reveal endothelial niches for stem cells. Cell. 2005;121:1109–1121. doi: 10.1016/j.cell.2005.05.026. [DOI] [PubMed] [Google Scholar]
- 85.Onnis B, Rapisarda A, Melillo G. Development of HIF-1 inhibitors for cancer therapy. J Cell Mol Med. 2009;13:2780–2786. doi: 10.1111/j.1582-4934.2009.00876.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Bhowmick NA, Neilson EG, Moses HL. Stromal fibroblasts in cancer initiation and progression. Nature. 2004;432:332–337. doi: 10.1038/nature03096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Shiao SL, Ganesan AP, Rugo HS, Coussens LM. Immune microenvironments in solid tumors: new targets for therapy. Genes Dev. 2011;25:2559–2572. doi: 10.1101/gad.169029.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.McMillin DW, Negri JM, Mitsiades CS. The role of tumour-stromal interactions in modifying drug response: challenges and opportunities. Nat Rev Drug Discov. 2013;12:217–228. doi: 10.1038/nrd3870. [DOI] [PubMed] [Google Scholar]
- 89.Malanchi I, Santamaria-Martinez A, Susanto E, Peng H, Lehr HA, Delaloye JF, Huelsken J. Interactions between cancer stem cells and their niche govern metastatic colonization. Nature. 2012;481:85–89. doi: 10.1038/nature10694. [DOI] [PubMed] [Google Scholar]
- 90.Vermeulen L, De Sousa EMF, van der Heijden M, Cameron K, de Jong JH, Borovski T, Tuynman JB, Todaro M, Merz C, Rodermond H, Sprick MR, Kemper K, Richel DJ, Stassi G, Medema JP. Wnt activity defines colon cancer stem cells and is regulated by the microenvironment. Nat Cell Biol. 2010;12:468–476. doi: 10.1038/ncb2048. [DOI] [PubMed] [Google Scholar]
- 91.Straussman R, Morikawa T, Shee K, Barzily-Rokni M, Qian ZR, Du J, Davis A, Mongare MM, Gould J, Frederick DT, Cooper ZA, Chapman PB, Solit DB, Ribas A, Lo RS, Flaherty KT, Ogino S, Wargo JA, Golub TR. Tumour micro-environment elicits innate resistance to RAF inhibitors through HGF secretion. Nature. 2012;487:500–504. doi: 10.1038/nature11183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Gilbert LA, Hemann MT. DNA damage-mediated induction of a chemoresistant niche. Cell. 2010;143:355–366. doi: 10.1016/j.cell.2010.09.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Wilson TR, Fridlyand J, Yan Y, Penuel E, Burton L, Chan E, Peng J, Lin E, Wang Y, Sosman J, Ribas A, Li J, Moffat J, Sutherlin DP, Koeppen H, Merchant M, Neve R, Settleman J. Widespread potential for growth-factor-driven resistance to anticancer kinase inhibitors. Nature. 2012;487:505–509. doi: 10.1038/nature11249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Hoyt K, Castaneda B, Zhang M, Nigwekar P, di Sant’agnese PA, Joseph JV, Strang J, Rubens DJ, Parker KJ. Tissue elasticity properties as biomarkers for prostate cancer. Cancer Biomark. 2008;4:213–225. doi: 10.3233/cbm-2008-44-505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Danen EH. Integrins: regulators of tissue function and cancer progression. Curr Pharm Des. 2005;11:881–891. doi: 10.2174/1381612053381756. [DOI] [PubMed] [Google Scholar]
- 96.Williams K, Motiani K, Giridhar PV, Kasper S. CD44 integrates signaling in normal stem cell, cancer stem cell and (pre)metastatic niches. Exp Biol Med (Maywood) 2013;238:324–338. doi: 10.1177/1535370213480714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Gottesman MM, Fojo T, Bates SE. Multidrug resistance in cancer: role of ATP-dependent transporters. Nat Rev Cancer. 2002;2:48–58. doi: 10.1038/nrc706. [DOI] [PubMed] [Google Scholar]
- 98.Ambudkar SV, Dey S, Hrycyna CA, Ramachandra M, Pastan I, Gottesman MM. Biochemical, cellular, and pharmacological aspects of the multidrug transporter. Annu Rev Pharmacol Toxicol. 1999;39:361–398. doi: 10.1146/annurev.pharmtox.39.1.361. [DOI] [PubMed] [Google Scholar]
- 99.Choi CH. ABC transporters as multidrug resistance mechanisms and the development of chemosensitizers for their reversal. Cancer Cell Int. 2005;5:30. doi: 10.1186/1475-2867-5-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Thomas H, Coley HM. Overcoming multidrug resistance in cancer: an update on the clinical strategy of inhibiting p-glycoprotein. Cancer Control. 2003;10:159–165. doi: 10.1177/107327480301000207. [DOI] [PubMed] [Google Scholar]
- 101.Triller N, Korosec P, Kern I, Kosnik M, Debeljak A. Multidrug resistance in small cell lung cancer: expression of P-glycoprotein, multidrug resistance protein 1 and lung resistance protein in chemo-naive patients and in relapsed disease. Lung Cancer. 2006;54:235–240. doi: 10.1016/j.lungcan.2006.06.019. [DOI] [PubMed] [Google Scholar]
- 102.Nooter K, Brutel de la Riviere G, Look MP, van Wingerden KE, Henzen-Logmans SC, Scheper RJ, Flens MJ, Klijn JG, Stoter G, Foekens JA. The prognostic significance of expression of the multidrug resistance-associated protein (MRP) in primary breast cancer. Br J Cancer. 1997;76:486–493. doi: 10.1038/bjc.1997.414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Zalcberg J, Hu XF, Slater A, Parisot J, El-Osta S, Kantharidis P, Chou ST, Parkin JD. MRP1 not MDR1 gene expression is the predominant mechanism of acquired multidrug resistance in two prostate carcinoma cell lines. Prostate Cancer Prostatic Dis. 2000;3:66–75. doi: 10.1038/sj.pcan.4500394. [DOI] [PubMed] [Google Scholar]
- 104.Kunicka T, Soucek P. Importance of ABCC1 for cancer therapy and prognosis. Drug Metab Rev. 2014;46:325–342. doi: 10.3109/03602532.2014.901348. [DOI] [PubMed] [Google Scholar]
- 105.Doyle LA, Yang W, Abruzzo LV, Krogmann T, Gao Y, Rishi AK, Ross DD. A multidrug resistance transporter from human MCF-7 breast cancer cells. Proc Natl Acad Sci U S A. 1998;95:15665–15670. doi: 10.1073/pnas.95.26.15665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Robey RW, Shukla S, Steadman K, Obrzut T, Finley EM, Ambudkar SV, Bates SE. Inhibition of ABCG2-mediated transport by protein kinase inhibitors with a bisindolylmaleimide or indolocarbazole structure. Mol Cancer Ther. 2007;6:1877–1885. doi: 10.1158/1535-7163.MCT-06-0811. [DOI] [PubMed] [Google Scholar]
- 107.Shukla S, Chen ZS, Ambudkar SV. Tyrosine kinase inhibitors as modulators of ABC transporter-mediated drug resistance. Drug Resist Updat. 2012;15:70–80. doi: 10.1016/j.drup.2012.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Pusztai L, Wagner P, Ibrahim N, Rivera E, Theriault R, Booser D, Symmans FW, Wong F, Blumenschein G, Fleming DR, Rouzier R, Boniface G, Hortobagyi GN. Phase II study of tariquidar, a selective P-glycoprotein inhibitor, in patients with chemotherapy-resistant, advanced breast carcinoma. Cancer. 2005;104:682–691. doi: 10.1002/cncr.21227. [DOI] [PubMed] [Google Scholar]
- 109.Ruff P, Vorobiof DA, Jordaan JP, Demetriou GS, Moodley SD, Nosworthy AL, Werner ID, Raats J, Burgess LJ. A randomized, placebo-controlled, double-blind phase 2 study of docetaxel compared to docetaxel plus zosuquidar (LY335979) in women with metastatic or locally recurrent breast cancer who have received one prior chemotherapy regimen. Cancer Chemother Pharmacol. 2009;64:763–768. doi: 10.1007/s00280-009-0925-9. [DOI] [PubMed] [Google Scholar]
- 110.Shervington A, Lu C. Expression of multidrug resistance genes in normal and cancer stem cells. Cancer Invest. 2008;26:535–542. doi: 10.1080/07357900801904140. [DOI] [PubMed] [Google Scholar]
- 111.Golebiewska A, Brons NH, Bjerkvig R, Niclou SP. Critical appraisal of the side population assay in stem cell and cancer stem cell research. Cell Stem Cell. 2011;8:136–147. doi: 10.1016/j.stem.2011.01.007. [DOI] [PubMed] [Google Scholar]
- 112.Szakacs G, Annereau JP, Lababidi S, Shankavaram U, Arciello A, Bussey KJ, Reinhold W, Guo Y, Kruh GD, Reimers M, Weinstein JN, Gottesman MM. Predicting drug sensitivity and resistance: profiling ABC transporter genes in cancer cells. Cancer Cell. 2004;6:129–137. doi: 10.1016/j.ccr.2004.06.026. [DOI] [PubMed] [Google Scholar]
- 113.Meijer C, Mulder NH, Timmer-Bosscha H, Sluiter WJ, Meersma GJ, de Vries EG. Relationship of cellular glutathione to the cytotoxicity and resistance of seven platinum compounds. Cancer Res. 1992;52:6885–6889. [PubMed] [Google Scholar]
- 114.Malet-Martino M, Martino R. Clinical studies of three oral prodrugs of 5-fluorouracil (capecitabine, UFT, S-1): a review. Oncologist. 2002;7:288–323. doi: 10.1634/theoncologist.7-4-288. [DOI] [PubMed] [Google Scholar]
- 115.Schwartz PM, Moir RD, Hyde CM, Turek PJ, Handschumacher RE. Role of uridine phosphorylase in the anabolism of 5-fluorouracil. Biochem Pharmacol. 1985;34:3585–3589. doi: 10.1016/0006-2952(85)90737-3. [DOI] [PubMed] [Google Scholar]
- 116.Houghton JA, Houghton PJ. Elucidation of pathways of 5-fluorouracil metabolism in xenografts of human colorectal adenocarcinoma. Eur J Cancer Clin Oncol. 1983;19:807–815. doi: 10.1016/0277-5379(83)90013-5. [DOI] [PubMed] [Google Scholar]
- 117.Kosuri KV, Wu X, Wang L, Villalona-Calero MA, Otterson GA. An epigenetic mechanism for capecitabine resistance in mesothelioma. Biochem Biophys Res Commun. 2010;391:1465–1470. doi: 10.1016/j.bbrc.2009.12.095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Belanger AS, Tojcic J, Harvey M, Guillemette C. Regulation of UGT1A1 and HNF1 transcription factor gene expression by DNA methylation in colon cancer cells. BMC Mol Biol. 2010;11:9. doi: 10.1186/1471-2199-11-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Toffoli G, Cecchin E, Gasparini G, D’Andrea M, Azzarello G, Basso U, Mini E, Pessa S, De Mattia E, Lo Re G, Buonadonna A, Nobili S, De Paoli P, Innocenti F. Genotype-driven phase I study of irinotecan administered in combination with fluorouracil/leucovorin in patients with metastatic colorectal cancer. J Clin Oncol. 2010;28:866–871. doi: 10.1200/JCO.2009.23.6125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Januchowski R, Wojtowicz K, Zabel M. The role of aldehyde dehydrogenase (ALDH) in cancer drug resistance. Biomed Pharmacother. 2013;67:669–680. doi: 10.1016/j.biopha.2013.04.005. [DOI] [PubMed] [Google Scholar]
- 121.Ginestier C, Hur MH, Charafe-Jauffret E, Monville F, Dutcher J, Brown M, Jacquemier J, Viens P, Kleer CG, Liu S, Schott A, Hayes D, Birnbaum D, Wicha MS, Dontu G. ALDH1 is a marker of normal and malignant human mammary stem cells and a predictor of poor clinical outcome. Cell Stem Cell. 2007;1:555–567. doi: 10.1016/j.stem.2007.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Rasheed ZA, Yang J, Wang Q, Kowalski J, Freed I, Murter C, Hong SM, Koorstra JB, Rajeshkumar NV, He X, Goggins M, Iacobuzio-Donahue C, Berman DM, Laheru D, Jimeno A, Hidalgo M, Maitra A, Matsui W. Prognostic significance of tumorigenic cells with mesenchymal features in pancreatic adenocarcinoma. J Natl Cancer Inst. 2010;102:340–351. doi: 10.1093/jnci/djp535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Li T, Su Y, Mei Y, Leng Q, Leng B, Liu Z, Stass SA, Jiang F. ALDH1A1 is a marker for malignant prostate stem cells and predictor of prostate cancer patients’ outcome. Lab Invest. 2010;90:234–244. doi: 10.1038/labinvest.2009.127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Emadi A, Jones RJ, Brodsky RA. Cyclophosphamide and cancer: golden anniversary. Nat Rev Clin Oncol. 2009;6:638–647. doi: 10.1038/nrclinonc.2009.146. [DOI] [PubMed] [Google Scholar]
- 125.Schafer A, Teufel J, Ringel F, Bettstetter M, Hoepner I, Rasper M, Gempt J, Koeritzer J, Schmidt-Graf F, Meyer B, Beier CP, Schlegel J. Aldehyde dehydrogenase 1A1--a new mediator of resistance to temozolomide in glioblastoma. Neuro Oncol. 2012;14:1452–1464. doi: 10.1093/neuonc/nos270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Koelling TM, Yeager AM, Hilton J, Haynie DT, Wiley JM. Development and characterization of a cyclophosphamide-resistant subline of acute myeloid leukemia in the Lewis x Brown Norway hybrid rat. Blood. 1990;76:1209–1213. [PubMed] [Google Scholar]
- 127.Croker AK, Allan AL. Inhibition of aldehyde dehydrogenase (ALDH) activity reduces chemotherapy and radiation resistance of stem-like ALDHhiCD44(+) human breast cancer cells. Breast Cancer Res Treat. 2012;133:75–87. doi: 10.1007/s10549-011-1692-y. [DOI] [PubMed] [Google Scholar]
- 128.Tanei T, Morimoto K, Shimazu K, Kim SJ, Tanji Y, Taguchi T, Tamaki Y, Noguchi S. Association of breast cancer stem cells identified by aldehyde dehydrogenase 1 expression with resistance to sequential Paclitaxel and epirubicin-based chemotherapy for breast cancers. Clin Cancer Res. 2009;15:4234–4241. doi: 10.1158/1078-0432.CCR-08-1479. [DOI] [PubMed] [Google Scholar]
- 129.Sasaki K, Tsuno NH, Sunami E, Tsurita G, Kawai K, Okaji Y, Nishikawa T, Shuno Y, Hongo K, Hiyoshi M, Kaneko M, Kitayama J, Takahashi K, Nagawa H. Chloroquine potentiates the anti-cancer effect of 5-fluorouracil on colon cancer cells. BMC Cancer. 2010;10:370. doi: 10.1186/1471-2407-10-370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Amaravadi RK, Yu D, Lum JJ, Bui T, Christophorou MA, Evan GI, Thomas-Tikhonenko A, Thompson CB. Autophagy inhibition enhances therapy-induced apoptosis in a Myc-induced model of lymphoma. J Clin Invest. 2007;117:326–336. doi: 10.1172/JCI28833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Maciejczyk A, Jagoda E, Wysocka T, Matkowski R, Gyorffy B, Lage H, Surowiak P. ABCC2 (MRP2, cMOAT) localized in the nuclear envelope of breast carcinoma cells correlates with poor clinical outcome. Pathol Oncol Res. 2012;18:331–342. doi: 10.1007/s12253-011-9449-9. [DOI] [PubMed] [Google Scholar]
- 132.Habicht KL, Singh NS, Khadeer MA, Shimmo R, Wainer IW, Moaddel R. Characterization of a multiple endogenously expressed adenosine triphosphate-binding cassette transporters using nuclear and cellular membrane affinity chromatography columns. J Chromatogr A. 2014;1339:80–85. doi: 10.1016/j.chroma.2014.02.076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Habicht KL, Frazier C, Singh N, Shimmo R, Wainer IW, Moaddel R. The synthesis and characterization of a nuclear membrane affinity chromatography column for the study of human breast cancer resistant protein (BCRP) using nuclear membranes obtained from the LN-229 cells. J Pharm Biomed Anal. 2013;72:159–162. doi: 10.1016/j.jpba.2012.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Bhatia P, Bernier M, Sanghvi M, Moaddel R, Schwarting R, Ramamoorthy A, Wainer IW. Breast cancer resistance protein (BCRP/ABCG2) localises to the nucleus in glioblastoma multiforme cells. Xenobiotica. 2012;42:748–755. doi: 10.3109/00498254.2012.662726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Gao MQ, Choi YP, Kang S, Youn JH, Cho NH. CD24+ cells from hierarchically organized ovarian cancer are enriched in cancer stem cells. Oncogene. 2010;29:2672–2680. doi: 10.1038/onc.2010.35. [DOI] [PubMed] [Google Scholar]
- 136.Pece S, Tosoni D, Confalonieri S, Mazzarol G, Vecchi M, Ronzoni S, Bernard L, Viale G, Pelicci PG, Di Fiore PP. Biological and molecular heterogeneity of breast cancers correlates with their cancer stem cell content. Cell. 2010;140:62–73. doi: 10.1016/j.cell.2009.12.007. [DOI] [PubMed] [Google Scholar]
- 137.Wilson A, Laurenti E, Oser G, van der Wath RC, Blanco-Bose W, Jaworski M, Offner S, Dunant CF, Eshkind L, Bockamp E, Lio P, Macdonald HR, Trumpp A. Hematopoietic stem cells reversibly switch from dormancy to self-renewal during homeostasis and repair. Cell. 2008;135:1118–1129. doi: 10.1016/j.cell.2008.10.048. [DOI] [PubMed] [Google Scholar]
- 138.Roesch A, Fukunaga-Kalabis M, Schmidt EC, Zabierowski SE, Brafford PA, Vultur A, Basu D, Gimotty P, Vogt T, Herlyn M. A temporarily distinct subpopulation of slow-cycling melanoma cells is required for continuous tumor growth. Cell. 2010;141:583–594. doi: 10.1016/j.cell.2010.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Moore N, Houghton J, Lyle S. Slow-cycling therapy-resistant cancer cells. Stem Cells Dev. 2012;21:1822–1830. doi: 10.1089/scd.2011.0477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Dembinski JL, Krauss S. Characterization and functional analysis of a slow cycling stem cell-like subpopulation in pancreas adenocarcinoma. Clin Exp Metastasis. 2009;26:611–623. doi: 10.1007/s10585-009-9260-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Ito K, Bernardi R, Morotti A, Matsuoka S, Saglio G, Ikeda Y, Rosenblatt J, Avigan DE, Teruya-Feldstein J, Pandolfi PP. PML targeting eradicates quiescent leukaemia-initiating cells. Nature. 2008;453:1072–1078. doi: 10.1038/nature07016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Zhang B, Strauss AC, Chu S, Li M, Ho Y, Shiang KD, Snyder DS, Huettner CS, Shultz L, Holyoake T, Bhatia R. Effective targeting of quiescent chronic myelogenous leukemia stem cells by histone deacetylase inhibitors in combination with imatinib mesylate. Cancer Cell. 2010;17:427–442. doi: 10.1016/j.ccr.2010.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Bouwman P, Jonkers J. The effects of deregulated DNA damage signalling on cancer chemotherapy response and resistance. Nat Rev Cancer. 2012;12:587–598. doi: 10.1038/nrc3342. [DOI] [PubMed] [Google Scholar]
- 144.Bao S, Wu Q, McLendon RE, Hao Y, Shi Q, Hjelmeland AB, Dewhirst MW, Bigner DD, Rich JN. Glioma stem cells promote radioresistance by preferential activation of the DNA damage response. Nature. 2006;444:756–760. doi: 10.1038/nature05236. [DOI] [PubMed] [Google Scholar]
- 145.Pajonk F, Vlashi E, McBride WH. Radiation resistance of cancer stem cells: the 4 R’s of radiobiology revisited. Stem Cells. 2010;28:639–648. doi: 10.1002/stem.318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Farmer H, McCabe N, Lord CJ, Tutt AN, Johnson DA, Richardson TB, Santarosa M, Dillon KJ, Hickson I, Knights C, Martin NM, Jackson SP, Smith GC, Ashworth A. Targeting the DNA repair defect in BRCA mutant cells as a therapeutic strategy. Nature. 2005;434:917–921. doi: 10.1038/nature03445. [DOI] [PubMed] [Google Scholar]
- 147.Kaelin WG., Jr The concept of synthetic lethality in the context of anticancer therapy. Nat Rev Cancer. 2005;5:689–698. doi: 10.1038/nrc1691. [DOI] [PubMed] [Google Scholar]
- 148.Lord RV, Brabender J, Gandara D, Alberola V, Camps C, Domine M, Cardenal F, Sanchez JM, Gumerlock PH, Taron M, Sanchez JJ, Danenberg KD, Danenberg PV, Rosell R. Low ERCC1 expression correlates with prolonged survival after cisplatin plus gemcitabine chemotherapy in non-small cell lung cancer. Clin Cancer Res. 2002;8:2286–2291. [PubMed] [Google Scholar]
- 149.Kwon HC, Roh MS, Oh SY, Kim SH, Kim MC, Kim JS, Kim HJ. Prognostic value of expression of ERCC1, thymidylate synthase, and glutathione S-transferase P1 for 5-fluorouracil/oxaliplatin chemotherapy in advanced gastric cancer. Ann Oncol. 2007;18:504–509. doi: 10.1093/annonc/mdl430. [DOI] [PubMed] [Google Scholar]
- 150.Usanova S, Piee-Staffa A, Sied U, Thomale J, Schneider A, Kaina B, Koberle B. Cisplatin sensitivity of testis tumour cells is due to deficiency in interstrand-crosslink repair and low ERCC1–XPF expression. Mol Cancer. 2010;9:248. doi: 10.1186/1476-4598-9-248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Fink D, Aebi S, Howell SB. The role of DNA mismatch repair in drug resistance. Clin Cancer Res. 1998;4:1–6. [PubMed] [Google Scholar]
- 152.Zhang M, Behbod F, Atkinson RL, Landis MD, Kittrell F, Edwards D, Medina D, Tsimelzon A, Hilsenbeck S, Green JE, Michalowska AM, Rosen JM. Identification of tumor-initiating cells in a p53-null mouse model of breast cancer. Cancer Res. 2008;68:4674–4682. doi: 10.1158/0008-5472.CAN-07-6353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Squatrito M, Brennan CW, Helmy K, Huse JT, Petrini JH, Holland EC. Loss of ATM/Chk2/p53 pathway components accelerates tumor development and contributes to radiation resistance in gliomas. Cancer Cell. 2010;18:619–629. doi: 10.1016/j.ccr.2010.10.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Rich JN. Cancer stem cells in radiation resistance. Cancer Res. 2007;67:8980–8984. doi: 10.1158/0008-5472.CAN-07-0895. [DOI] [PubMed] [Google Scholar]
- 155.Ropolo M, Daga A, Griffero F, Foresta M, Casartelli G, Zunino A, Poggi A, Cappelli E, Zona G, Spaziante R, Corte G, Frosina G. Comparative analysis of DNA repair in stem and nonstem glioma cell cultures. Mol Cancer Res. 2009;7:383–392. doi: 10.1158/1541-7786.MCR-08-0409. [DOI] [PubMed] [Google Scholar]
- 156.Venkatesha VA, Parsels LA, Parsels JD, Zhao L, Zabludoff SD, Simeone DM, Maybaum J, Lawrence TS, Morgan MA. Sensitization of pancreatic cancer stem cells to gemcitabine by Chk1 inhibition. Neoplasia. 2012;14:519–525. doi: 10.1593/neo.12538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Yin H, Glass J. The phenotypic radiation resistance of CD44+/CD24(-or low) breast cancer cells is mediated through the enhanced activation of ATM signaling. PLoS One. 2011;6:e24080. doi: 10.1371/journal.pone.0024080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Sciuscio D, Diserens AC, van Dommelen K, Martinet D, Jones G, Janzer RC, Pollo C, Hamou MF, Kaina B, Stupp R, Levivier M, Hegi ME. Extent and patterns of MGMT promoter methylation in glioblastoma- and respective glioblastoma-derived spheres. Clin Cancer Res. 2011;17:255–266. doi: 10.1158/1078-0432.CCR-10-1931. [DOI] [PubMed] [Google Scholar]
- 159.Kato T, Natsume A, Toda H, Iwamizu H, Sugita T, Hachisu R, Watanabe R, Yuki K, Motomura K, Bankiewicz K, Wakabayashi T. Efficient delivery of liposome-mediated MGMT-siRNA reinforces the cytotoxity of temozolomide in GBM-initiating cells. Gene Ther. 2010;17:1363–1371. doi: 10.1038/gt.2010.88. [DOI] [PubMed] [Google Scholar]
- 160.Mir SE, De Witt Hamer PC, Krawczyk PM, Balaj L, Claes A, Niers JM, Van Tilborg AA, Zwinderman AH, Geerts D, Kaspers GJ, Peter Vandertop W, Cloos J, Tannous BA, Wesseling P, Aten JA, Noske DP, Van Noorden CJ, Wurdinger T. In silico analysis of kinase expression identifies WEE1 as a gatekeeper against mitotic catastrophe in glioblastoma. Cancer Cell. 2010;18:244–257. doi: 10.1016/j.ccr.2010.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Zhuang W, Li B, Long L, Chen L, Huang Q, Liang ZQ. Knockdown of the DNA-dependent protein kinase catalytic subunit radiosensitizes glioma-initiating cells by inducing autophagy. Brain Res. 2011;1371:7–15. doi: 10.1016/j.brainres.2010.11.044. [DOI] [PubMed] [Google Scholar]
- 162.Cao R, Tsukada Y, Zhang Y. Role of Bmi-1 and Ring1A in H2A ubiquitylation and Hox gene silencing. Mol Cell. 2005;20:845–854. doi: 10.1016/j.molcel.2005.12.002. [DOI] [PubMed] [Google Scholar]
- 163.Facchino S, Abdouh M, Chatoo W, Bernier G. BMI1 confers radioresistance to normal and cancerous neural stem cells through recruitment of the DNA damage response machinery. J Neurosci. 2010;30:10096–10111. doi: 10.1523/JNEUROSCI.1634-10.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Gieni RS, Ismail IH, Campbell S, Hendzel MJ. Polycomb group proteins in the DNA damage response: a link between radiation resistance and “stemness”. Cell Cycle. 2011;10:883–894. doi: 10.4161/cc.10.6.14907. [DOI] [PubMed] [Google Scholar]
- 165.Wu CY, Hung JJ, Wu KJ. Linkage between Twist1 and Bmi1: molecular mechanism of cancer metastasis/stemness and clinical implications. Clin Exp Pharmacol Physiol. 2012;39:668–673. doi: 10.1111/j.1440-1681.2011.05594.x. [DOI] [PubMed] [Google Scholar]
- 166.Chen YC, Chang CJ, Hsu HS, Chen YW, Tai LK, Tseng LM, Chiou GY, Chang SC, Kao SY, Chiou SH, Lo WL. Inhibition of tumorigenicity and enhancement of radiochemosensitivity in head and neck squamous cell cancer-derived ALDH1-positive cells by knockdown of Bmi-1. Oral Oncol. 2010;46:158–165. doi: 10.1016/j.oraloncology.2009.11.007. [DOI] [PubMed] [Google Scholar]
- 167.Takebe N, Harris PJ, Warren RQ, Ivy SP. Targeting cancer stem cells by inhibiting Wnt, Notch, and Hedgehog pathways. Nat Rev Clin Oncol. 2011;8:97–106. doi: 10.1038/nrclinonc.2010.196. [DOI] [PubMed] [Google Scholar]
- 168.Soeda A, Inagaki A, Oka N, Ikegame Y, Aoki H, Yoshimura S, Nakashima S, Kunisada T, Iwama T. Epidermal growth factor plays a crucial role in mitogenic regulation of human brain tumor stem cells. J Biol Chem. 2008;283:10958–10966. doi: 10.1074/jbc.M704205200. [DOI] [PubMed] [Google Scholar]
- 169.Lee J, Son MJ, Woolard K, Donin NM, Li A, Cheng CH, Kotliarova S, Kotliarov Y, Walling J, Ahn S, Kim M, Totonchy M, Cusack T, Ene C, Ma H, Su Q, Zenklusen JC, Zhang W, Maric D, Fine HA. Epigenetic-mediated dysfunction of the bone morphogenetic protein pathway inhibits differentiation of glioblastoma-initiating cells. Cancer Cell. 2008;13:69–80. doi: 10.1016/j.ccr.2007.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Chen YW, Chen KH, Huang PI, Chen YC, Chiou GY, Lo WL, Tseng LM, Hsu HS, Chang KW, Chiou SH. Cucurbitacin I suppressed stem-like property and enhanced radiation-induced apoptosis in head and neck squamous carcinoma--derived CD44(+)ALDH1(+) cells. Mol Cancer Ther. 2010;9:2879–2892. doi: 10.1158/1535-7163.MCT-10-0504. [DOI] [PubMed] [Google Scholar]
- 171.Hsu HS, Huang PI, Chang YL, Tzao C, Chen YW, Shih HC, Hung SC, Chen YC, Tseng LM, Chiou SH. Cucurbitacin I inhibits tumorigenic ability and enhances radiochemosensitivity in nonsmall cell lung cancer-derived CD133-positive cells. Cancer. 2011;117:2970–2985. doi: 10.1002/cncr.25869. [DOI] [PubMed] [Google Scholar]
- 172.Sun Y, Zheng S, Speirs C, Zhao Z, Lu B. Gene Profiling of Cancer Stem Cells-like Cells Reveals IGF-1R and IGFBP3 Pathway as a Promising Therapeutic Target for Lung Cancer. International Journal of Radiation Oncology. 2010;78 [Google Scholar]
- 173.Sun L, Mathews LA, Cabarcas SM, Zhang X, Yang A, Zhang Y, Young MR, Klarmann KD, Keller JR, Farrar WL. Epigenetic regulation of SOX9 by the NF-kappaB signaling pathway in pancreatic cancer stem cells. Stem Cells. 2013;31:1454–1466. doi: 10.1002/stem.1394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Wang J, Wakeman TP, Lathia JD, Hjelmeland AB, Wang XF, White RR, Rich JN, Sullenger BA. Notch promotes radioresistance of glioma stem cells. Stem Cells. 2010;28:17–28. doi: 10.1002/stem.261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Fan X, Matsui W, Khaki L, Stearns D, Chun J, Li YM, Eberhart CG. Notch pathway inhibition depletes stem-like cells and blocks engraftment in embryonal brain tumors. Cancer Res. 2006;66:7445–7452. doi: 10.1158/0008-5472.CAN-06-0858. [DOI] [PubMed] [Google Scholar]
- 176.Bar EE, Chaudhry A, Lin A, Fan X, Schreck K, Matsui W, Piccirillo S, Vescovi AL, DiMeco F, Olivi A, Eberhart CG. Cyclopamine-mediated hedgehog pathway inhibition depletes stem-like cancer cells in glioblastoma. Stem Cells. 2007;25:2524–2533. doi: 10.1634/stemcells.2007-0166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Clement V, Sanchez P, de Tribolet N, Radovanovic I, Ruiz i Altaba A. HEDGEHOG-GLI1 signaling regulates human glioma growth, cancer stem cell self-renewal, and tumorigenicity. Curr Biol. 2007;17:165–172. doi: 10.1016/j.cub.2006.11.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Kendziorra E, Ahlborn K, Spitzner M, Rave-Frank M, Emons G, Gaedcke J, Kramer F, Wolff HA, Becker H, Beissbarth T, Ebner R, Ghadimi BM, Pukrop T, Ried T, Grade M. Silencing of the Wnt transcription factor TCF4 sensitizes colorectal cancer cells to (chemo-) radiotherapy. Carcinogenesis. 2011;32:1824–1831. doi: 10.1093/carcin/bgr222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Kishida O, Miyazaki Y, Murayama Y, Ogasa M, Miyazaki T, Yamamoto T, Watabe K, Tsutsui S, Kiyohara T, Shimomura I, Shinomura Y. Gefitinib (“Iressa”, ZD1839) inhibits SN38-triggered EGF signals and IL-8 production in gastric cancer cells. Cancer Chemother Pharmacol. 2005;55:393–403. doi: 10.1007/s00280-004-0904-0. [DOI] [PubMed] [Google Scholar]
- 180.Sumitomo M, Asano T, Asakuma J, Asano T, Horiguchi A, Hayakawa M. ZD1839 modulates paclitaxel response in renal cancer by blocking paclitaxel-induced activation of the epidermal growth factor receptor-extracellular signal-regulated kinase pathway. Clin Cancer Res. 2004;10:794–801. doi: 10.1158/1078-0432.ccr-0948-03. [DOI] [PubMed] [Google Scholar]
- 181.Van Schaeybroeck S, Karaiskou-McCaul A, Kelly D, Longley D, Galligan L, Van Cutsem E, Johnston P. Epidermal growth factor receptor activity determines response of colorectal cancer cells to gefitinib alone and in combination with chemotherapy. Clin Cancer Res. 2005;11:7480–7489. doi: 10.1158/1078-0432.CCR-05-0328. [DOI] [PubMed] [Google Scholar]
- 182.Van Schaeybroeck S, Kelly DM, Kyula J, Stokesberry S, Fennell DA, Johnston PG, Longley DB. Src and ADAM-17-mediated shedding of transforming growth factor-alpha is a mechanism of acute resistance to TRAIL. Cancer Res. 2008;68:8312–8321. doi: 10.1158/0008-5472.CAN-07-6736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Kang KB, Zhu C, Wong YL, Gao Q, Ty A, Wong MC. Gefitinib radiosensitizes stem-like glioma cells: inhibition of epidermal growth factor receptor-Akt-DNA-PK signaling, accompanied by inhibition of DNA double-strand break repair. Int J Radiat Oncol Biol Phys. 2012;83:e43–52. doi: 10.1016/j.ijrobp.2011.11.037. [DOI] [PubMed] [Google Scholar]
- 184.Zhang M, Atkinson RL, Rosen JM. Selective targeting of radiation-resistant tumor-initiating cells. Proc Natl Acad Sci U S A. 2010;107:3522–3527. doi: 10.1073/pnas.0910179107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Zhan JF, Wu LP, Chen LH, Yuan YW, Xie GZ, Sun AM, Liu Y, Chen ZX. Pharmacological inhibition of AKT sensitizes MCF-7 human breast cancer-initiating cells to radiation. Cell Oncol (Dordr) 2011;34:451–456. doi: 10.1007/s13402-011-0020-1. [DOI] [PubMed] [Google Scholar]
- 186.Garner JM, Fan M, Yang CH, Du Z, Sims M, Davidoff AM, Pfeffer LM. Constitutive activation of signal transducer and activator of transcription 3 (STAT3) and nuclear factor kappaB signaling in glioblastoma cancer stem cells regulates the Notch pathway. J Biol Chem. 2013;288:26167–26176. doi: 10.1074/jbc.M113.477950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Letai AG. Diagnosing and exploiting cancer’s addiction to blocks in apoptosis. Nat Rev Cancer. 2008;8:121–132. doi: 10.1038/nrc2297. [DOI] [PubMed] [Google Scholar]
- 188.Kitada S, Andersen J, Akar S, Zapata JM, Takayama S, Krajewski S, Wang HG, Zhang X, Bullrich F, Croce CM, Rai K, Hines J, Reed JC. Expression of apoptosis-regulating proteins in chronic lymphocytic leukemia: correlations with In vitro and In vivo chemoresponses. Blood. 1998;91:3379–3389. [PubMed] [Google Scholar]
- 189.Nita ME, Nagawa H, Tominaga O, Tsuno N, Fujii S, Sasaki S, Fu CG, Takenoue T, Tsuruo T, Muto T. 5-Fluorouracil induces apoptosis in human colon cancer cell lines with modulation of Bcl-2 family proteins. Br J Cancer. 1998;78:986–992. doi: 10.1038/bjc.1998.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Wang D, Xiang DB, Yang XQ, Chen LS, Li MX, Zhong ZY, Zhang YS. APE1 overexpression is associated with cisplatin resistance in non-small cell lung cancer and targeted inhibition of APE1 enhances the activity of cisplatin in A549 cells. Lung Cancer. 2009;66:298–304. doi: 10.1016/j.lungcan.2009.02.019. [DOI] [PubMed] [Google Scholar]
- 191.Alvero AB, Montagna MK, Chen R, Kim KH, Kyungjin K, Visintin I, Fu HH, Brown D, Mor G. NV-128, a novel isoflavone derivative, induces caspase-independent cell death through the Akt/mammalian target of rapamycin pathway. Cancer. 2009;115:3204–3216. doi: 10.1002/cncr.24397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Ng KP, Hillmer AM, Chuah CT, Juan WC, Ko TK, Teo AS, Ariyaratne PN, Takahashi N, Sawada K, Fei Y, Soh S, Lee WH, Huang JW, Allen JC, Jr, Woo XY, Nagarajan N, Kumar V, Thalamuthu A, Poh WT, Ang AL, Mya HT, How GF, Yang LY, Koh LP, Chowbay B, Chang CT, Nadarajan VS, Chng WJ, Than H, Lim LC, Goh YT, Zhang S, Poh D, Tan P, Seet JE, Ang MK, Chau NM, Ng QS, Tan DS, Soda M, Isobe K, Nothen MM, Wong TY, Shahab A, Ruan X, Cacheux-Rataboul V, Sung WK, Tan EH, Yatabe Y, Mano H, et al. A common BIM deletion polymorphism mediates intrinsic resistance and inferior responses to tyrosine kinase inhibitors in cancer. Nat Med. 2012;18:521–528. doi: 10.1038/nm.2713. [DOI] [PubMed] [Google Scholar]
- 193.Costa DB, Halmos B, Kumar A, Schumer ST, Huberman MS, Boggon TJ, Tenen DG, Kobayashi S. BIM mediates EGFR tyrosine kinase inhibitor-induced apoptosis in lung cancers with oncogenic EGFR mutations. PLoS Med. 2007;4:1669–1679. doi: 10.1371/journal.pmed.0040315. discussion 1680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Kuribara R, Honda H, Matsui H, Shinjyo T, Inukai T, Sugita K, Nakazawa S, Hirai H, Ozawa K, Inaba T. Roles of Bim in apoptosis of normal and Bcr-Abl-expressing hematopoietic progenitors. Mol Cell Biol. 2004;24:6172–6183. doi: 10.1128/MCB.24.14.6172-6183.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Blower PE, Verducci JS, Lin S, Zhou J, Chung JH, Dai Z, Liu CG, Reinhold W, Lorenzi PL, Kaldjian EP, Croce CM, Weinstein JN, Sadee W. MicroRNA expression profiles for the NCI-60 cancer cell panel. Mol Cancer Ther. 2007;6:1483–1491. doi: 10.1158/1535-7163.MCT-07-0009. [DOI] [PubMed] [Google Scholar]
- 196.Faber AC, Corcoran RB, Ebi H, Sequist LV, Waltman BA, Chung E, Incio J, Digumarthy SR, Pollack SF, Song Y, Muzikansky A, Lifshits E, Roberge S, Coffman EJ, Benes CH, Gomez HL, Baselga J, Arteaga CL, Rivera MN, Dias-Santagata D, Jain RK, Engelman JA. BIM expression in treatment-naive cancers predicts responsiveness to kinase inhibitors. Cancer Discov. 2011;1:352–365. doi: 10.1158/2159-8290.CD-11-0106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Ni Chonghaile T, Sarosiek KA, Vo TT, Ryan JA, Tammareddi A, del Moore VG, Deng J, Anderson KC, Richardson P, Tai YT, Mitsiades CS, Matulonis UA, Drapkin R, Stone R, Deangelo DJ, McConkey DJ, Sallan SE, Silverman L, Hirsch MS, Carrasco DR, Letai A. Pretreatment mitochondrial priming correlates with clinical response to cytotoxic chemotherapy. Science. 2011;334:1129–1133. doi: 10.1126/science.1206727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Capper D, Gaiser T, Hartmann C, Habel A, Mueller W, Herold-Mende C, von Deimling A, Siegelin MD. Stem-cell-like glioma cells are resistant to TRAIL/Apo2L and exhibit down-regulation of caspase-8 by promoter methylation. Acta Neuropathol. 2009;117:445–456. doi: 10.1007/s00401-009-0494-3. [DOI] [PubMed] [Google Scholar]
- 199.Tagscherer KE, Fassl A, Campos B, Farhadi M, Kraemer A, Bock BC, Macher-Goeppinger S, Radlwimmer B, Wiestler OD, Herold-Mende C, Roth W. Apoptosis-based treatment of glioblastomas with ABT-737, a novel small molecule inhibitor of Bcl-2 family proteins. Oncogene. 2008;27:6646–6656. doi: 10.1038/onc.2008.259. [DOI] [PubMed] [Google Scholar]
- 200.Piggott L, Omidvar N, Marti Perez S, Eberl M, Clarkson RW. Suppression of apoptosis inhibitor c-FLIP selectively eliminates breast cancer stem cell activity in response to the anti-cancer agent, TRAIL. Breast Cancer Res. 2011;13:R88. doi: 10.1186/bcr2945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Yin S, Xu L, Bandyopadhyay S, Sethi S, Reddy KB. Cisplatin and TRAIL enhance breast cancer stem cell death. Int J Oncol. 2011;39:891–898. doi: 10.3892/ijo.2011.1085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Tang SN, Singh C, Nall D, Meeker D, Shankar S, Srivastava RK. The dietary bioflavonoid quercetin synergizes with epigallocathechin gallate (EGCG) to inhibit prostate cancer stem cell characteristics, invasion, migration and epithelial-mesenchymal transition. J Mol Signal. 2010;5:14. doi: 10.1186/1750-2187-5-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Nanta R, Kumar D, Meeker D, Rodova M, Van Veldhuizen PJ, Shankar S, Srivastava RK. NVP-LDE-225 (Erismodegib) inhibits epithelial-mesenchymal transition and human prostate cancer stem cell growth in NOD/SCID IL2Rgamma null mice by regulating Bmi-1 and microRNA-128. Oncogenesis. 2013;2:e42. doi: 10.1038/oncsis.2013.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Pavet V, Portal MM, Moulin JC, Herbrecht R, Gronemeyer H. Towards novel paradigms for cancer therapy. Oncogene. 2011;30:1–20. doi: 10.1038/onc.2010.460. [DOI] [PubMed] [Google Scholar]
- 205.Guttilla IK, Phoenix KN, Hong X, Tirnauer JS, Claffey KP, White BA. Prolonged mammosphere culture of MCF-7 cells induces an EMT and repression of the estrogen receptor by microRNAs. Breast Cancer Res Treat. 2012;132:75–85. doi: 10.1007/s10549-011-1534-y. [DOI] [PubMed] [Google Scholar]
- 206.Gibbons DL, Lin W, Creighton CJ, Rizvi ZH, Gregory PA, Goodall GJ, Thilaganathan N, Du L, Zhang Y, Pertsemlidis A, Kurie JM. Contextual extracellular cues promote tumor cell EMT and metastasis by regulating miR-200 family expression. Genes Dev. 2009;23:2140–2151. doi: 10.1101/gad.1820209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Gregory PA, Bracken CP, Bert AG, Goodall GJ. MicroRNAs as regulators of epithelial-mesenchymal transition. Cell Cycle. 2008;7:3112–3118. doi: 10.4161/cc.7.20.6851. [DOI] [PubMed] [Google Scholar]
- 208.Bracken CP, Gregory PA, Khew-Goodall Y, Goodall GJ. The role of microRNAs in metastasis and epithelial-mesenchymal transition. Cell Mol Life Sci. 2009;66:1682–1699. doi: 10.1007/s00018-009-8750-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Gregory PA, Bert AG, Paterson EL, Barry SC, Tsykin A, Farshid G, Vadas MA, Khew-Goodall Y, Goodall GJ. The miR-200 family and miR-205 regulate epithelial to mesenchymal transition by targeting ZEB1 and SIP1. Nat Cell Biol. 2008;10:593–601. doi: 10.1038/ncb1722. [DOI] [PubMed] [Google Scholar]
- 210.Korpal M, Lee ES, Hu G, Kang Y. The miR-200 family inhibits epithelial-mesenchymal transition and cancer cell migration by direct targeting of E-cadherin transcriptional repressors ZEB1 and ZEB2. J Biol Chem. 2008;283:14910–14914. doi: 10.1074/jbc.C800074200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Park SM, Gaur AB, Lengyel E, Peter ME. The miR-200 family determines the epithelial phenotype of cancer cells by targeting the E-cadherin repressors ZEB1 and ZEB2. Genes Dev. 2008;22:894–907. doi: 10.1101/gad.1640608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Li Y, VandenBoom TG, 2nd, Kong D, Wang Z, Ali S, Philip PA, Sarkar FH. Up-regulation of miR-200 and let-7 by natural agents leads to the reversal of epithelial-to-mesenchymal transition in gemcitabine-resistant pancreatic cancer cells. Cancer Res. 2009;69:6704–6712. doi: 10.1158/0008-5472.CAN-09-1298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Wellner U, Schubert J, Burk UC, Schmalhofer O, Zhu F, Sonntag A, Waldvogel B, Vannier C, Darling D, zur Hausen A, Brunton VG, Morton J, Sansom O, Schuler J, Stemmler MP, Herzberger C, Hopt U, Keck T, Brabletz S, Brabletz T. The EMT-activator ZEB1 promotes tumorigenicity by repressing stemness-inhibiting microRNAs. Nat Cell Biol. 2009;11:1487–1495. doi: 10.1038/ncb1998. [DOI] [PubMed] [Google Scholar]
- 214.Wang X, Lu H, Li T, Yu L, Liu G, Peng X, Zhao J. Kruppel-like factor 8 promotes tumorigenic mammary stem cell induction by targeting miR-146a. Am J Cancer Res. 2013;3:356–373. [PMC free article] [PubMed] [Google Scholar]
- 215.Hwang WL, Jiang JK, Yang SH, Huang TS, Lan HY, Teng HW, Yang CY, Tsai YP, Lin CH, Wang HW, Yang MH. MicroRNA-146a directs the symmetric division of Snail-dominant colorectal cancer stem cells. Nat Cell Biol. 2014;16:268–280. doi: 10.1038/ncb2910. [DOI] [PubMed] [Google Scholar]
- 216.Li T, Lu H, Mukherjee D, Lahiri SK, Shen C, Yu L, Zhao J. Identification of epidermal growth factor receptor and its inhibitory microRNA141 as novel targets of Kruppel-like factor 8 in breast cancer. Oncotarget. 2015;6:21428–21442. doi: 10.18632/oncotarget.4077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Wang Z, Li Y, Ahmad A, Azmi AS, Kong D, Banerjee S, Sarkar FH. Targeting miRNAs involved in cancer stem cell and EMT regulation: An emerging concept in overcoming drug resistance. Drug Resist Updat. 2010;13:109–118. doi: 10.1016/j.drup.2010.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Thiery JP, Sleeman JP. Complex networks orchestrate epithelial-mesenchymal transitions. Nat Rev Mol Cell Biol. 2006;7:131–142. doi: 10.1038/nrm1835. [DOI] [PubMed] [Google Scholar]
- 219.Morel AP, Hinkal GW, Thomas C, Fauvet F, Courtois-Cox S, Wierinckx A, Devouassoux-Shisheboran M, Treilleux I, Tissier A, Gras B, Pourchet J, Puisieux I, Browne GJ, Spicer DB, Lachuer J, Ansieau S, Puisieux A. EMT inducers catalyze malignant transformation of mammary epithelial cells and drive tumorigenesis towards claudin-low tumors in transgenic mice. PLoS Genet. 2012;8:e1002723. doi: 10.1371/journal.pgen.1002723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Morel AP, Lievre M, Thomas C, Hinkal G, Ansieau S, Puisieux A. Generation of breast cancer stem cells through epithelial-mesenchymal transition. PLoS One. 2008;3:e2888. doi: 10.1371/journal.pone.0002888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Masui T, Ota I, Yook JI, Mikami S, Yane K, Yamanaka T, Hosoi H. Snail-induced epithelial-mesenchymal transition promotes cancer stem cell-like phenotype in head and neck cancer cells. Int J Oncol. 2014;44:693–699. doi: 10.3892/ijo.2013.2225. [DOI] [PubMed] [Google Scholar]
- 222.Radisky DC, LaBarge MA. Epithelial-mesenchymal transition and the stem cell phenotype. Cell Stem Cell. 2008;2:511–512. doi: 10.1016/j.stem.2008.05.007. [DOI] [PubMed] [Google Scholar]
- 223.DiMeo TA, Anderson K, Phadke P, Fan C, Perou CM, Naber S, Kuperwasser C. A novel lung metastasis signature links Wnt signaling with cancer cell self-renewal and epithelial-mesenchymal transition in basal-like breast cancer. Cancer Res. 2009;69:5364–5373. doi: 10.1158/0008-5472.CAN-08-4135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Brabletz T, Jung A, Spaderna S, Hlubek F, Kirchner T. Opinion: migrating cancer stem cells - an integrated concept of malignant tumour progression. Nat Rev Cancer. 2005;5:744–749. doi: 10.1038/nrc1694. [DOI] [PubMed] [Google Scholar]
- 225.Blick T, Hugo H, Widodo E, Waltham M, Pinto C, Mani SA, Weinberg RA, Neve RM, Lenburg ME, Thompson EW. Epithelial mesenchymal transition traits in human breast cancer cell lines parallel the CD44(hi/)CD24 (lo/-) stem cell phenotype in human breast cancer. J Mammary Gland Biol Neoplasia. 2010;15:235–252. doi: 10.1007/s10911-010-9175-z. [DOI] [PubMed] [Google Scholar]
- 226.Hollier BG, Evans K, Mani SA. The epithelial-to-mesenchymal transition and cancer stem cells: a coalition against cancer therapies. J Mammary Gland Biol Neoplasia. 2009;14:29–43. doi: 10.1007/s10911-009-9110-3. [DOI] [PubMed] [Google Scholar]
- 227.Yauch RL, Januario T, Eberhard DA, Cavet G, Zhu W, Fu L, Pham TQ, Soriano R, Stinson J, Seshagiri S, Modrusan Z, Lin CY, O’Neill V, Amler LC. Epithelial versus mesenchymal phenotype determines in vitro sensitivity and predicts clinical activity of erlotinib in lung cancer patients. Clin Cancer Res. 2005;11:8686–8698. doi: 10.1158/1078-0432.CCR-05-1492. [DOI] [PubMed] [Google Scholar]
- 228.Rho JK, Choi YJ, Lee JK, Ryoo BY, Na II, Yang SH, Kim CH, Lee JC. Epithelial to mesenchymal transition derived from repeated exposure to gefitinib determines the sensitivity to EGFR inhibitors in A549, a non-small cell lung cancer cell line. Lung Cancer. 2009;63:219–226. doi: 10.1016/j.lungcan.2008.05.017. [DOI] [PubMed] [Google Scholar]
- 229.Frederick BA, Helfrich BA, Coldren CD, Zheng D, Chan D, Bunn PA, Jr, Raben D. Epithelial to mesenchymal transition predicts gefitinib resistance in cell lines of head and neck squamous cell carcinoma and non-small cell lung carcinoma. Mol Cancer Ther. 2007;6:1683–1691. doi: 10.1158/1535-7163.MCT-07-0138. [DOI] [PubMed] [Google Scholar]
- 230.Fuchs BC, Fujii T, Dorfman JD, Goodwin JM, Zhu AX, Lanuti M, Tanabe KK. Epithelial-to-mesenchymal transition and integrin-linked kinase mediate sensitivity to epidermal growth factor receptor inhibition in human hepatoma cells. Cancer Res. 2008;68:2391–2399. doi: 10.1158/0008-5472.CAN-07-2460. [DOI] [PubMed] [Google Scholar]
- 231.Shah AN, Summy JM, Zhang J, Park SI, Parikh NU, Gallick GE. Development and characterization of gemcitabine-resistant pancreatic tumor cells. Ann Surg Oncol. 2007;14:3629–3637. doi: 10.1245/s10434-007-9583-5. [DOI] [PubMed] [Google Scholar]
- 232.Wang Z, Li Y, Ahmad A, Banerjee S, Azmi AS, Kong D, Sarkar FH. Pancreatic cancer: understanding and overcoming chemoresistance. Nat Rev Gastroenterol Hepatol. 2011;8:27–33. doi: 10.1038/nrgastro.2010.188. [DOI] [PubMed] [Google Scholar]
- 233.Sabbah M, Emami S, Redeuilh G, Julien S, Prevost G, Zimber A, Ouelaa R, Bracke M, De Wever O, Gespach C. Molecular signature and therapeutic perspective of the epithelial-to-mesenchymal transitions in epithelial cancers. Drug Resist Updat. 2008;11:123–151. doi: 10.1016/j.drup.2008.07.001. [DOI] [PubMed] [Google Scholar]
- 234.Arumugam T, Ramachandran V, Fournier KF, Wang H, Marquis L, Abbruzzese JL, Gallick GE, Logsdon CD, McConkey DJ, Choi W. Epithelial to mesenchymal transition contributes to drug resistance in pancreatic cancer. Cancer Res. 2009;69:5820–5828. doi: 10.1158/0008-5472.CAN-08-2819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Kajiyama H, Shibata K, Terauchi M, Yamashita M, Ino K, Nawa A, Kikkawa F. Chemoresistance to paclitaxel induces epithelial-mesenchymal transition and enhances metastatic potential for epithelial ovarian carcinoma cells. Int J Oncol. 2007;31:277–283. [PubMed] [Google Scholar]
- 236.Konecny GE, Venkatesan N, Yang G, Dering J, Ginther C, Finn R, Rahmeh M, Fejzo MS, Toft D, Jiang SW, Slamon DJ, Podratz KC. Activity of lapatinib a novel HER2 and EGFR dual kinase inhibitor in human endometrial cancer cells. Br J Cancer. 2008;98:1076–1084. doi: 10.1038/sj.bjc.6604278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Hiscox S, Jiang WG, Obermeier K, Taylor K, Morgan L, Burmi R, Barrow D, Nicholson RI. Tamoxifen resistance in MCF7 cells promotes EMT-like behaviour and involves modulation of beta-catenin phosphorylation. Int J Cancer. 2006;118:290–301. doi: 10.1002/ijc.21355. [DOI] [PubMed] [Google Scholar]
- 238.Kim MR, Choi HK, Cho KB, Kim HS, Kang KW. Involvement of Pin1 induction in epithelial-mesenchymal transition of tamoxifen-resistant breast cancer cells. Cancer Sci. 2009;100:1834–1841. doi: 10.1111/j.1349-7006.2009.01260.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Yang AD, Fan F, Camp ER, van Buren G, Liu W, Somcio R, Gray MJ, Cheng H, Hoff PM, Ellis LM. Chronic oxaliplatin resistance induces epithelial-to-mesenchymal transition in colorectal cancer cell lines. Clin Cancer Res. 2006;12:4147–4153. doi: 10.1158/1078-0432.CCR-06-0038. [DOI] [PubMed] [Google Scholar]
- 240.Carey LA, Dees EC, Sawyer L, Gatti L, Moore DT, Collichio F, Ollila DW, Sartor CI, Graham ML, Perou CM. The triple negative paradox: primary tumor chemosensitivity of breast cancer subtypes. Clin Cancer Res. 2007;13:2329–2334. doi: 10.1158/1078-0432.CCR-06-1109. [DOI] [PubMed] [Google Scholar]
- 241.Liedtke C, Mazouni C, Hess KR, Andre F, Tordai A, Mejia JA, Symmans WF, Gonzalez-Angulo AM, Hennessy B, Green M, Cristofanilli M, Hortobagyi GN, Pusztai L. Response to neoadjuvant therapy and long-term survival in patients with triple-negative breast cancer. J Clin Oncol. 2008;26:1275–1281. doi: 10.1200/JCO.2007.14.4147. [DOI] [PubMed] [Google Scholar]
- 242.Paik S, Tang G, Shak S, Kim C, Baker J, Kim W, Cronin M, Baehner FL, Watson D, Bryant J, Costantino JP, Geyer CE, Jr, Wickerham DL, Wolmark N. Gene expression and benefit of chemotherapy in women with node-negative, estrogen receptor-positive breast cancer. J Clin Oncol. 2006;24:3726–3734. doi: 10.1200/JCO.2005.04.7985. [DOI] [PubMed] [Google Scholar]
- 243.Wang Z, Li Y, Kong D, Banerjee S, Ahmad A, Azmi AS, Ali S, Abbruzzese JL, Gallick GE, Sarkar FH. Acquisition of epithelial-mesenchymal transition phenotype of gemcitabine-resistant pancreatic cancer cells is linked with activation of the notch signaling pathway. Cancer Res. 2009;69:2400–2407. doi: 10.1158/0008-5472.CAN-08-4312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Takahashi K, Yamanaka S. Induction of pluripotent stem cells from mouse embryonic and adult fibroblast cultures by defined factors. Cell. 2006;126:663–676. doi: 10.1016/j.cell.2006.07.024. [DOI] [PubMed] [Google Scholar]
- 245.Izpisua Belmonte JC, Ellis J, Hochedlinger K, Yamanaka S. Induced pluripotent stem cells and reprogramming: seeing the science through the hype. Nat Rev Genet. 2009;10:878–883. doi: 10.1038/nrg2700. [DOI] [PubMed] [Google Scholar]
- 246.Yu J, Vodyanik MA, Smuga-Otto K, Antosiewicz-Bourget J, Frane JL, Tian S, Nie J, Jonsdottir GA, Ruotti V, Stewart R, Slukvin II, Thomson JA. Induced pluripotent stem cell lines derived from human somatic cells. Science. 2007;318:1917–1920. doi: 10.1126/science.1151526. [DOI] [PubMed] [Google Scholar]
- 247.Takahashi K, Tanabe K, Ohnuki M, Narita M, Ichisaka T, Tomoda K, Yamanaka S. Induction of pluripotent stem cells from adult human fibroblasts by defined factors. Cell. 2007;131:861–872. doi: 10.1016/j.cell.2007.11.019. [DOI] [PubMed] [Google Scholar]
- 248.Islam F, Qiao B, Smith RA, Gopalan V, Lam AK. Cancer stem cell: fundamental experimental pathological concepts and updates. Exp Mol Pathol. 2015;98:184–191. doi: 10.1016/j.yexmp.2015.02.002. [DOI] [PubMed] [Google Scholar]
- 249.Blau HM, Brazelton TR, Weimann JM. The evolving concept of a stem cell: entity or function? Cell. 2001;105:829–841. doi: 10.1016/s0092-8674(01)00409-3. [DOI] [PubMed] [Google Scholar]
- 250.Zipori D. The nature of stem cells: state rather than entity. Nat Rev Genet. 2004;5:873–878. doi: 10.1038/nrg1475. [DOI] [PubMed] [Google Scholar]
- 251.Miyabayashi T, Teo JL, Yamamoto M, McMillan M, Nguyen C, Kahn M. Wnt/beta-catenin/CBP signaling maintains long-term murine embryonic stem cell pluripotency. Proc Natl Acad Sci U S A. 2007;104:5668–5673. doi: 10.1073/pnas.0701331104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.Pawlik TM, Keyomarsi K. Role of cell cycle in mediating sensitivity to radiotherapy. Int J Radiat Oncol Biol Phys. 2004;59:928–942. doi: 10.1016/j.ijrobp.2004.03.005. [DOI] [PubMed] [Google Scholar]
- 253.Horta S, Agostinho AL, Mateus R, Pereira L, Pereira C, Capinha L, Doktorovova S, Brito A, Videira M. Looking out for cancer stem cells’ properties: the value-driving role of CD44 for personalized medicines. Curr Cancer Drug Targets. 2015;14:832–849. doi: 10.2174/1568009614666141111154713. [DOI] [PubMed] [Google Scholar]
- 254.Ghosh SC, Neslihan Alpay S, Klostergaard J. CD44: a validated target for improved delivery of cancer therapeutics. Expert Opin Ther Targets. 2012;16:635–650. doi: 10.1517/14728222.2012.687374. [DOI] [PubMed] [Google Scholar]
- 255.Leizer AL, Alvero AB, Fu HH, Holmberg JC, Cheng YC, Silasi DA, Rutherford T, Mor G. Regulation of inflammation by the NF-kappaB pathway in ovarian cancer stem cells. Am J Reprod Immunol. 2011;65:438–447. doi: 10.1111/j.1600-0897.2010.00914.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256.Chefetz I, Holmberg JC, Alvero AB, Visintin I, Mor G. Inhibition of Aurora-A kinase induces cell cycle arrest in epithelial ovarian cancer stem cells by affecting NFkB pathway. Cell Cycle. 2011;10:2206–2214. doi: 10.4161/cc.10.13.16348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 257.Wang L, Guo H, Yang L, Dong L, Lin C, Zhang J, Lin P, Wang X. Morusin inhibits human cervical cancer stem cell growth and migration through attenuation of NF-kappaB activity and apoptosis induction. Mol Cell Biochem. 2013;379:7–18. doi: 10.1007/s11010-013-1621-y. [DOI] [PubMed] [Google Scholar]
- 258.Gunn EJ, Williams JT, Huynh DT, Iannotti MJ, Han C, Barrios FJ, Kendall S, Glackin CA, Colby DA, Kirshner J. The natural products parthenolide and andrographolide exhibit anti-cancer stem cell activity in multiple myeloma. Leuk Lymphoma. 2011;52:1085–1097. doi: 10.3109/10428194.2011.555891. [DOI] [PubMed] [Google Scholar]
- 259.Hellsten R, Johansson M, Dahlman A, Sterner O, Bjartell A. Galiellalactone inhibits stem cell-like ALDH-positive prostate cancer cells. PLoS One. 2011;6:e22118. doi: 10.1371/journal.pone.0022118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Ashizawa T, Miyata H, Iizuka A, Komiyama M, Oshita C, Kume A, Nogami M, Yagoto M, Ito I, Oishi T, Watanabe R, Mitsuya K, Matsuno K, Furuya T, Okawara T, Otsuka M, Ogo N, Asai A, Nakasu Y, Yamaguchi K, Akiyama Y. Effect of the STAT3 inhibitor STX-0119 on the proliferation of cancer stem-like cells derived from recurrent glioblastoma. Int J Oncol. 2013;43:219–227. doi: 10.3892/ijo.2013.1916. [DOI] [PubMed] [Google Scholar]
- 261.Lin C, Wang L, Wang H, Yang L, Guo H, Wang X. Tanshinone IIA inhibits breast cancer stem cells growth in vitro and in vivo through attenuation of IL-6/STAT3/NF-kB signaling pathways. J Cell Biochem. 2013;114:2061–2070. doi: 10.1002/jcb.24553. [DOI] [PubMed] [Google Scholar]
- 262.Sai K, Wang S, Balasubramaniyan V, Conrad C, Lang FF, Aldape K, Szymanski S, Fokt I, Dasgupta A, Madden T, Guan S, Chen Z, Alfred Yung WK, Priebe W, Colman H. Induction of cell-cycle arrest and apoptosis in glioblastoma stem-like cells by WP1193, a novel small molecule inhibitor of the JAK2/STAT3 pathway. J Neurooncol. 2012;107:487–501. doi: 10.1007/s11060-011-0786-z. [DOI] [PubMed] [Google Scholar]
- 263.Singh BN, Kumar D, Shankar S, Srivastava RK. Rottlerin induces autophagy which leads to apoptotic cell death through inhibition of PI3K/Akt/mTOR pathway in human pancreatic cancer stem cells. Biochem Pharmacol. 2012;84:1154–1163. doi: 10.1016/j.bcp.2012.08.007. [DOI] [PubMed] [Google Scholar]
- 264.Carra E, Barbieri F, Marubbi D, Pattarozzi A, Favoni RE, Florio T, Daga A. Sorafenib selectively depletes human glioblastoma tumor-initiating cells from primary cultures. Cell Cycle. 2013;12:491–500. doi: 10.4161/cc.23372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265.Pollock CB, Koltai H, Kapulnik Y, Prandi C, Yarden RI. Strigolactones: a novel class of phytohormones that inhibit the growth and survival of breast cancer cells and breast cancer stem-like enriched mammosphere cells. Breast Cancer Res Treat. 2012;134:1041–1055. doi: 10.1007/s10549-012-1992-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 266.Liu H, Han D, Liu Y, Hou X, Wu J, Li H, Yang J, Shen C, Yang G, Fu C, Li X, Che H, Ai J, Zhao S. Harmine hydrochloride inhibits Akt phosphorylation and depletes the pool of cancer stem-like cells of glioblastoma. J Neurooncol. 2013;112:39–48. doi: 10.1007/s11060-012-1034-x. [DOI] [PubMed] [Google Scholar]
- 267.Yo YT, Lin YW, Wang YC, Balch C, Huang RL, Chan MW, Sytwu HK, Chen CK, Chang CC, Nephew KP, Huang T, Yu MH, Lai HC. Growth inhibition of ovarian tumor-initiating cells by niclosamide. Mol Cancer Ther. 2012;11:1703–1712. doi: 10.1158/1535-7163.MCT-12-0002. [DOI] [PubMed] [Google Scholar]
- 268.Isayev O, Rausch V, Bauer N, Liu L, Fan P, Zhang Y, Gladkich J, Nwaeburu CC, Mattern J, Mollenhauer M, Ruckert F, Zach S, Haberkorn U, Gross W, Schonsiegel F, Bazhin AV, Herr I. Inhibition of glucose turnover by 3-bromopyruvate counteracts pancreatic cancer stem cell features and sensitizes cells to gemcitabine. Oncotarget. 2014;5:5177–5189. doi: 10.18632/oncotarget.2120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 269.Ciavardelli D, Rossi C, Barcaroli D, Volpe S, Consalvo A, Zucchelli M, De Cola A, Scavo E, Carollo R, D’Agostino D, Forli F, D’Aguanno S, Todaro M, Stassi G, Di Ilio C, De Laurenzi V, Urbani A. Breast cancer stem cells rely on fermentative glycolysis and are sensitive to 2-deoxyglucose treatment. Cell Death Dis. 2014;5:e1336. doi: 10.1038/cddis.2014.285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 270.Guo Y, Zhang X, Meng J, Wang ZY. An anticancer agent icaritin induces sustained activation of the extracellular signal-regulated kinase (ERK) pathway and inhibits growth of breast cancer cells. Eur J Pharmacol. 2011;658:114–122. doi: 10.1016/j.ejphar.2011.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271.Dong Y, Han Q, Zou Y, Deng Z, Lu X, Wang X, Zhang W, Jin H, Su J, Jiang T, Ren H. Long-term exposure to imatinib reduced cancer stem cell ability through induction of cell differentiation via activation of MAPK signaling in glioblastoma cells. Mol Cell Biochem. 2012;370:89–102. doi: 10.1007/s11010-012-1401-0. [DOI] [PubMed] [Google Scholar]
- 272.Guvenc H, Pavlyukov MS, Joshi K, Kurt H, Banasavadi-Siddegowda YK, Mao P, Hong C, Yamada R, Kwon CH, Bhasin D, Chettiar S, Kitange G, Park IH, Sarkaria JN, Li C, Shakhparonov MI, Nakano I. Impairment of glioma stem cell survival and growth by a novel inhibitor for Survivin-Ran protein complex. Clin Cancer Res. 2013;19:631–642. doi: 10.1158/1078-0432.CCR-12-0647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 273.Rentala S, Chintala R, Guda M, Chintala M, Komarraju AL, Mangamoori LN. Atorvastatin inhibited Rho-associated kinase 1 (ROCK1) and focal adhesion kinase (FAK) mediated adhesion and differentiation of CD133+CD44+ prostate cancer stem cells. Biochem Biophys Res Commun. 2013;441:586–592. doi: 10.1016/j.bbrc.2013.10.112. [DOI] [PubMed] [Google Scholar]
- 274.Lonardo E, Cioffi M, Sancho P, Sanchez-Ripoll Y, Trabulo SM, Dorado J, Balic A, Hidalgo M, Heeschen C. Metformin targets the metabolic achilles heel of human pancreatic cancer stem cells. PLoS One. 2013;8:e76518. doi: 10.1371/journal.pone.0076518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 275.Serrano D, Bleau AM, Fernandez-Garcia I, Fernandez-Marcelo T, Iniesta P, Ortiz-de-Solorzano C, Calvo A. Inhibition of telomerase activity preferentially targets aldehyde dehydrogenase-positive cancer stem-like cells in lung cancer. Mol Cancer. 2011;10:96. doi: 10.1186/1476-4598-10-96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 276.Allan EK, Holyoake TL, Craig AR, Jorgensen HG. Omacetaxine may have a role in chronic myeloid leukaemia eradication through downregulation of Mcl-1 and induction of apoptosis in stem/progenitor cells. Leukemia. 2011;25:985–994. doi: 10.1038/leu.2011.55. [DOI] [PubMed] [Google Scholar]
- 277.Zhu C, Cheng KW, Ouyang N, Huang L, Sun Y, Constantinides P, Rigas B. Phosphosulindac (OXT-328) selectively targets breast cancer stem cells in vitro and in human breast cancer xenografts. Stem Cells. 2012;30:2065–2075. doi: 10.1002/stem.1139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 278.Kusunoki S, Kato K, Tabu K, Inagaki T, Okabe H, Kaneda H, Suga S, Terao Y, Taga T, Takeda S. The inhibitory effect of salinomycin on the proliferation, migration and invasion of human endometrial cancer stem-like cells. Gynecol Oncol. 2013;129:598–605. doi: 10.1016/j.ygyno.2013.03.005. [DOI] [PubMed] [Google Scholar]
- 279.Fuchs D, Daniel V, Sadeghi M, Opelz G, Naujokat C. Salinomycin overcomes ABC transporter-mediated multidrug and apoptosis resistance in human leukemia stem cell-like KG-1a cells. Biochem Biophys Res Commun. 2010;394:1098–1104. doi: 10.1016/j.bbrc.2010.03.138. [DOI] [PubMed] [Google Scholar]
- 280.Ketola K, Hilvo M, Hyotylainen T, Vuoristo A, Ruskeepaa AL, Oresic M, Kallioniemi O, Iljin K. Salinomycin inhibits prostate cancer growth and migration via induction of oxidative stress. Br J Cancer. 2012;106:99–106. doi: 10.1038/bjc.2011.530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 281.Gupta PB, Onder TT, Jiang G, Tao K, Kuperwasser C, Weinberg RA, Lander ES. Identification of selective inhibitors of cancer stem cells by high-throughput screening. Cell. 2009;138:645–659. doi: 10.1016/j.cell.2009.06.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 282.Takehara M, Hoshino T, Namba T, Yamakawa N, Mizushima T. Acetaminophen-induced differentiation of human breast cancer stem cells and inhibition of tumor xenograft growth in mice. Biochem Pharmacol. 2011;81:1124–1135. doi: 10.1016/j.bcp.2011.02.012. [DOI] [PubMed] [Google Scholar]
- 283.Deng Y, Su Q, Mo J, Fu X, Zhang Y, Lin EH. Celecoxib downregulates CD133 expression through inhibition of the Wnt signaling pathway in colon cancer cells. Cancer Invest. 2013;31:97–102. doi: 10.3109/07357907.2012.754458. [DOI] [PubMed] [Google Scholar]
- 284.Farhana L, Dawson MI, Das JK, Murshed F, Xia Z, Hadden TJ, Hatfield J, Fontana JA. Adamantyl Retinoid-Related Molecules Induce Apoptosis in Pancreatic Cancer Cells by Inhibiting IGF-1R and Wnt/beta-Catenin Pathways. J Oncol. 2012;2012:796729. doi: 10.1155/2012/796729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 285.Zhang Y, Piao B, Zhang Y, Hua B, Hou W, Xu W, Qi X, Zhu X, Pei Y, Lin H. Oxymatrine diminishes the side population and inhibits the expression of beta-catenin in MCF-7 breast cancer cells. Med Oncol. 2011;28(Suppl 1):S99–107. doi: 10.1007/s12032-010-9721-y. [DOI] [PubMed] [Google Scholar]
- 286.Li Y, Zhang T, Korkaya H, Liu S, Lee HF, Newman B, Yu Y, Clouthier SG, Schwartz SJ, Wicha MS, Sun D. Sulforaphane, a dietary component of broccoli/broccoli sprouts, inhibits breast cancer stem cells. Clin Cancer Res. 2010;16:2580–2590. doi: 10.1158/1078-0432.CCR-09-2937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 287.Li SH, Fu J, Watkins DN, Srivastava RK, Shankar S. Sulforaphane regulates self-renewal of pancreatic cancer stem cells through the modulation of Sonic hedgehog-GLI pathway. Mol Cell Biochem. 2013;373:217–227. doi: 10.1007/s11010-012-1493-6. [DOI] [PubMed] [Google Scholar]
- 288.Rodova M, Fu J, Watkins DN, Srivastava RK, Shankar S. Sonic hedgehog signaling inhibition provides opportunities for targeted therapy by sulforaphane in regulating pancreatic cancer stem cell self-renewal. PLoS One. 2012;7:e46083. doi: 10.1371/journal.pone.0046083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 289.Singh BN, Fu J, Srivastava RK, Shankar S. Hedgehog signaling antagonist GDC-0449 (Vismodegib) inhibits pancreatic cancer stem cell characteristics: molecular mechanisms. PLoS One. 2011;6:e27306. doi: 10.1371/journal.pone.0027306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 290.Fu J, Rodova M, Roy SK, Sharma J, Singh KP, Srivastava RK, Shankar S. GANT-61 inhibits pancreatic cancer stem cell growth in vitro and in NOD/SCID/IL2R gamma null mice xenograft. Cancer Lett. 2013;330:22–32. doi: 10.1016/j.canlet.2012.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 291.Jiang LY, Zhang XL, Du P, Zheng JH. gamma-Secretase Inhibitor, DAPT Inhibits Self-renewal and Stemness Maintenance of Ovarian Cancer Stem-like Cells In Vitro. Chin J Cancer Res. 2011;23:140–146. doi: 10.1007/s11670-011-0140-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 292.Kondratyev M, Kreso A, Hallett RM, Girgis-Gabardo A, Barcelon ME, Ilieva D, Ware C, Majumder PK, Hassell JA. Gamma-secretase inhibitors target tumor-initiating cells in a mouse model of ERBB2 breast cancer. Oncogene. 2012;31:93–103. doi: 10.1038/onc.2011.212. [DOI] [PubMed] [Google Scholar]
- 293.Campos B, Wan F, Farhadi M, Ernst A, Zeppernick F, Tagscherer KE, Ahmadi R, Lohr J, Dictus C, Gdynia G, Combs SE, Goidts V, Helmke BM, Eckstein V, Roth W, Beckhove P, Lichter P, Unterberg A, Radlwimmer B, Herold-Mende C. Differentiation therapy exerts antitumor effects on stem-like glioma cells. Clin Cancer Res. 2010;16:2715–2728. doi: 10.1158/1078-0432.CCR-09-1800. [DOI] [PubMed] [Google Scholar]
- 294.Ying M, Wang S, Sang Y, Sun P, Lal B, Goodwin CR, Guerrero-Cazares H, Quinones-Hinojosa A, Laterra J, Xia S. Regulation of glioblastoma stem cells by retinoic acid: role for Notch pathway inhibition. Oncogene. 2011;30:3454–3467. doi: 10.1038/onc.2011.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 295.Huynh C, Poliseno L, Segura MF, Medicherla R, Haimovic A, Menendez S, Shang S, Pavlick A, Shao Y, Darvishian F, Boylan JF, Osman I, Hernando E. The novel gamma secretase inhibitor RO4929097 reduces the tumor initiating potential of melanoma. PLoS One. 2011;6:e25264. doi: 10.1371/journal.pone.0025264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 296.Hage C, Rausch V, Giese N, Giese T, Schonsiegel F, Labsch S, Nwaeburu C, Mattern J, Gladkich J, Herr I. The novel c-Met inhibitor cabozantinib overcomes gemcitabine resistance and stem cell signaling in pancreatic cancer. Cell Death Dis. 2013;4:e627. doi: 10.1038/cddis.2013.158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 297.Kanwar SS, Yu Y, Nautiyal J, Patel BB, Padhye S, Sarkar FH, Majumdar AP. Difluorinated-curcumin (CDF): a novel curcumin analog is a potent inhibitor of colon cancer stem-like cells. Pharm Res. 2011;28:827–838. doi: 10.1007/s11095-010-0336-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 298.Brendel C, Scharenberg C, Dohse M, Robey RW, Bates SE, Shukla S, Ambudkar SV, Wang Y, Wennemuth G, Burchert A, Boudriot U, Neubauer A. Imatinib mesylate and nilotinib (AMN107) exhibit high-affinity interaction with ABCG2 on primitive hematopoietic stem cells. Leukemia. 2007;21:1267–1275. doi: 10.1038/sj.leu.2404638. [DOI] [PubMed] [Google Scholar]
- 299.Miyazaki T, Pan Y, Joshi K, Purohit D, Hu B, Demir H, Mazumder S, Okabe S, Yamori T, Viapiano M, Shin-ya K, Seimiya H, Nakano I. Telomestatin impairs glioma stem cell survival and growth through the disruption of telomeric G-quadruplex and inhibition of the proto-oncogene, c-Myb. Clin Cancer Res. 2012;18:1268–1280. doi: 10.1158/1078-0432.CCR-11-1795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 300.Sabisz M, Skladanowski A. Cancer stem cells and escape from drug-induced premature senescence in human lung tumor cells: implications for drug resistance and in vitro drug screening models. Cell Cycle. 2009;8:3208–3217. doi: 10.4161/cc.8.19.9758. [DOI] [PubMed] [Google Scholar]
- 301.Lee YR, Yu DS, Liang YC, Huang KF, Chou SJ, Chen TC, Lee CC, Chen CL, Chiou SH, Huang HS. New approaches of PARP-1 inhibitors in human lung cancer cells and cancer stem-like cells by some selected anthraquinone-derived small molecules. PLoS One. 2013;8:e56284. doi: 10.1371/journal.pone.0056284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 302.Newman B, Liu Y, Lee HF, Sun D, Wang Y. HSP90 inhibitor 17-AAG selectively eradicates lymphoma stem cells. Cancer Res. 2012;72:4551–4561. doi: 10.1158/0008-5472.CAN-11-3600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 303.Patel NJ, Karuturi R, Al-Horani RA, Baranwal S, Patel J, Desai UR, Patel BB. Synthetic, Non-saccharide, Glycosaminoglycan Mimetics Selectively Target Colon Cancer Stem Cells. ACS Chem Biol. 2014;9:1826–1833. doi: 10.1021/cb500402f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 304.Shankar S, Nall D, Tang SN, Meeker D, Passarini J, Sharma J, Srivastava RK. Resveratrol inhibits pancreatic cancer stem cell characteristics in human and KrasG12D transgenic mice by inhibiting pluripotency maintaining factors and epithelial-mesenchymal transition. PLoS One. 2011;6:e16530. doi: 10.1371/journal.pone.0016530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 305.Lee TK, Poon RT, Wo JY, Ma S, Guan XY, Myers JN, Altevogt P, Yuen AP. Lupeol suppresses cisplatin-induced nuclear factor-kappaB activation in head and neck squamous cell carcinoma and inhibits local invasion and nodal metastasis in an orthotopic nude mouse model. Cancer Res. 2007;67:8800–8809. doi: 10.1158/0008-5472.CAN-07-0801. [DOI] [PubMed] [Google Scholar]
- 306.Sokol JP, Neil JR, Schiemann BJ, Schiemann WP. The use of cystatin C to inhibit epithelial-mesenchymal transition and morphological transformation stimulated by transforming growth factor-beta. Breast Cancer Res. 2005;7:R844–853. doi: 10.1186/bcr1312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 307.Finn RS, Dering J, Ginther C, Wilson CA, Glaspy P, Tchekmedyian N, Slamon DJ. Dasatinib, an orally active small molecule inhibitor of both the src and abl kinases, selectively inhibits growth of basal-type/”triple-negative” breast cancer cell lines growing in vitro. Breast Cancer Res Treat. 2007;105:319–326. doi: 10.1007/s10549-006-9463-x. [DOI] [PubMed] [Google Scholar]
- 308.Prud’homme GJ, Glinka Y, Toulina A, Ace O, Subramaniam V, Jothy S. Breast cancer stem-like cells are inhibited by a non-toxic aryl hydrocarbon receptor agonist. PLoS One. 2010;5:e13831. doi: 10.1371/journal.pone.0013831. [DOI] [PMC free article] [PubMed] [Google Scholar]