Abstract
Yersinia pestis causes bubonic plague, a fulminant disease where host immune responses are abrogated. Recently developed in vivo models of plague have resulted in new ideas regarding bacterial spread in the body. Deciphering bacterial spread is key to understanding Y. pestis and the immune responses it encounters during infection.
Keywords: Yersinia pestis, bubonic plague, dissemination
Evolving Portrait of a Deadly Pathogen
Yersinia pestis is arguably the most feared pathogen of the bacterial world. The bacterium causes plague, a reemerging infectious disease that can kill a host (including humans) in less than a week. The bacterium survives in sylvatic animal reservoirs, mainly in rodents. These animal reservoirs are the source of modern plague outbreaks.
The field of plague pathogenesis focuses on how Y. pestis infects a host, and how infection results in disease and death. Much progress has been made in the identification of genes the bacterium might use during infection. The plasmid pCD1, the most studied genetic determinant of Y. pestis, is essential for infection. pCD1 encodes proteins of the Yersinia type III secretion system, a syringe-like molecular apparatus responsible for secretion of proteins that interfere with host cellular functions. Other genetic determinants have been regarded as essential for Y. pestis infection but most of them have been tested only in vitro. By far, the biggest challenge in the field is the widespread use of in vitro approaches to build a picture of what occurs during infection. Addressing infection with in vivo models and fully virulent strains is challenging, but this is a challenge the field needs to embrace to advance.
Bubonic plague develops after Y. pestis enters the body via the skin, typically through the bite of an infectious flea. During infection the bacterium disseminates from the dermis to draining lymph nodes (dLNs), and from dLNs to systemic circulation [1, 2]. Notably, movement from tissue to tissue is not directly dependent on the bacterium as Y. pestis is nonmotile (i.e. lacks flagella).
How Y. pestis disseminates inside the body during bubonic plague and what host-pathogen interactions accompany this process are two prominent questions in the field. Here, we address these questions by paying particular, if not exclusive, attention to work done in vivo (i.e. using animal models) and with fully virulent Y. pestis strains.
Escape from the Skin and Initiation of Infection
Before entering the host, Y. pestis survives in the digestive tract of a flea. Infected fleas deposit bacteria in the dermal layer of the skin while obtaining a blood meal [3]. The bacterial population inoculated in the dermis can be divided into two: a large population that remains in the skin, and a very small population that leaves this tissue [4]. The bacteria that remain in the skin trigger the recruitment of neutrophils [4–6], which can be seen in close proximity to the bacteria or engulfing them. Neutrophils arrest bacterial proliferation in the skin but are unable to clear infection in this tissue [3, 4]. Accordingly, Y. pestis must interfere, at least to some extent, with the normal function of neutrophils. pCD1 has been implicated as a key player in this process [5].
We propose the bacterial population in the skin and the host-pathogen interactions at this site are not crucial in the development of disease. Instead, we hypothesize the bacteria that escape from the skin are responsible for host colonization and disease. The bacterial population that escapes from the skin travels to the dLN through lymphatic vessels and most-likely, contrary to prevailing models [7, 8], without the need of a phagocyte [i.e. macrophage, dendritic cell (DC), or neutrophil] [4]. Because the latter statement goes against long-lasting dogma it is important to review the most relevant evidence that supports it (Box 1).
Box 1. In or Out?
Y. pestis traditionally has been thought to require an intracellular stage to disseminate from skin to dLN [7, 8]. However, the points listed below argue against this hypothesis.
Y. pestis is detected in the dLN minutes after ID inoculation [4, 12]. Phagocytes reach LNs in hours, not minutes.
Macrophages are in general regarded as poor migratory cells. In addition, macrophage recruitment to the skin is very low after Y. pestis inoculation [5].
Neutrophil depletion does not affect Y. pestis loads in the dLN [4, 5].
DC recruitment in the skin is very low after Y. pestis inoculation and bacterial loads in the dLN are not affected in a model where DC trafficking to dLNs is abrogated [5].
Y. pestis that associate with skin lymphatic vessels immediately after inoculation are not associated with phagocytic cells [4].
Colonization of the dLN by Y. pestis begins in its periphery and not in the cortex, where trafficking phagocytes bring engulfed antigen [1].
Y. pestis is observed extracellularly during early stages of LN colonization [1].
Nevertheless, an intracellular phase might be required beyond early stages of infection (late disseminators). This idea has not been addressed experimentally with fully virulent strains.
The mechanisms behind phagocyte-independent transport to dLNs are unknown, however, it is likely that transport is driven by lymph flow. We propose that movement from the skin into the dLN is the key step for Y. pestis to successfully colonize the host and that this process depends almost exclusively on the fluidics of lymph.
The Lymph Node (LN), a Killer’s Heaven
When traceable, genetically tagged Y. pestis are inoculated intradermally (ID) (~20 CFU/tag) into the skin, only a few of the tags are detected in the dLN, while most of them persist in the skin [4]. This bottleneck in bacterial dissemination from skin to dLN might form in part because only a fraction of the bacteria are dissemination competent (i.e. are free to enter lymphatic vessels). Bacterial killing in the LN early after arrival also may contribute to bottleneck formation. This hypothesis predicts that any process contributing to bacterial escape from the skin (e.g. reduced bacterial adhesion) or bacterial survival would result in a weaker bottleneck.
The very few individual bacteria that pass the bottleneck colonize the LN at remarkably high rates. Approximately 104–105 colony forming units (CFU)/LN can be detected 24 hours after ID inoculation of ~200 CFU [3]. This number increases to ~108 CFU/LN around 48 hours after inoculation. As opposed to the skin, the LN environment might represent a ‘special niche’ that favors proliferation by triggering replication and/or the synthesis of proteins to fight host defenses. One of these proteins might be the protease Pla, regarded as critical for Y. pestis proliferation in the dLN [9].
The LN is the organ most associated with Y. pestis and bubonic plague. We propose that it is in this tissue (and not in the skin) where the fate of an infected individual is defined. For this reason, we propose that elucidating LN colonization is a high priority for the field.
Escaping Heaven to Cause Havoc
Y. pestis must escape the LN and enter systemic circulation as only then can a naïve flea acquire the bacterium and transmit it to a new host [10]. How Y. pestis escapes the dLN is unknown. However, two possible mechanisms are (i) escape through efferent lymphatic vessels, to eventually drain into the subclavian vein, and (ii) escape through the LN vasculature, ruptured as a result of LN colonization. The use of genetically tagged bacteria revealed a reduction in the number of tags in the spleen (used to assess systemic dissemination) in comparison with tags in the LN [3]. This second bottleneck is a barrier the bacteria pass to reach the bloodstream. Bacterial dissemination into blood results in sepsis, a systemic inflammatory response that can lead to septic shock and death.
In one of the very few studies reporting on septicemic stages of bubonic plague intravenous injections confirmed pCD1 is essential for bacterial proliferation in blood [11]. Other studies have implicated additional Y. pestis genetic determinants to be important as well, but their methods cannot exclude the possibility of effects on earlier stages of infection (e.g. LN colonization) rather than a specific effect in the blood.
The study of Y. pestis in the bloodstream is probably the area of plague pathogenesis where research has invested the least. This is paradoxical as severe disease and death from bubonic plague directly derive from bacterial systemic colonization.
Concluding Remarks
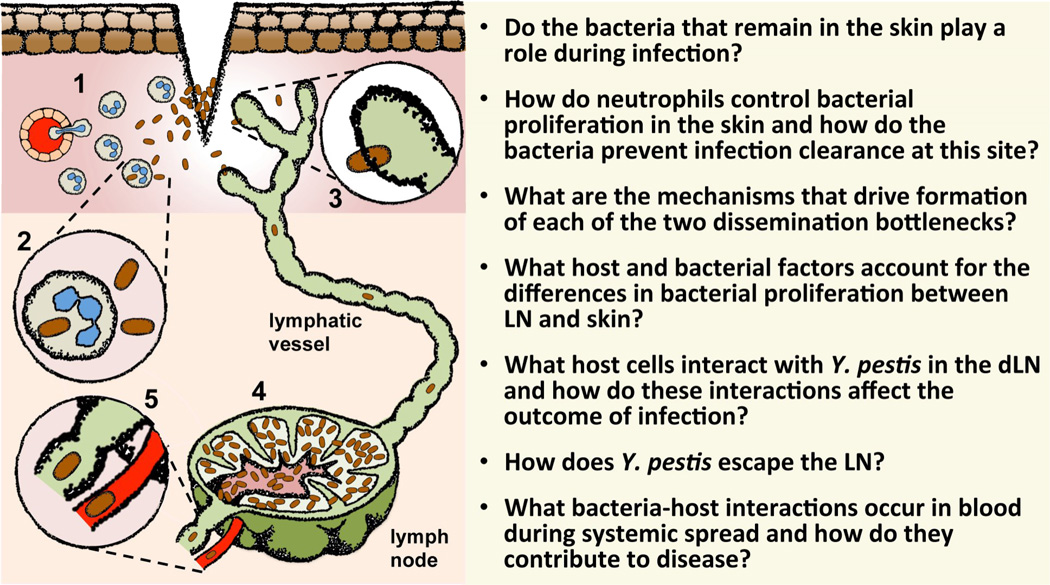
Much remains to be uncovered to paint a clear portrait of Y. pestis dissemination in the body and effective transmission to a new flea. The questions presented with the model in Figure 1 remain unanswered and are key to characterizing the events that define Y. pestis success. Notably, these questions are all related to an even greater question: Why is the immune system defenseless overall when encountering Y. pestis? Any efforts towards answering this question will not only contribute to the understanding of this fascinating bacterium but also of the biology of the immune system.
Figure 1. Dissemination of Y. pestis in the Body During Bubonic Plague.
(1) Inoculation of Y. pestis (brown rods) into the dermal layer of the skin triggers the recruitment of neutrophils (light green cells with blue nuclei). The dermis (pink) appears bellow the epidermis (brown cuboidal cells). (2) In the dermis, Y. pestis interacts mostly with neutrophils. These cells control Y. pestis proliferation in the dermis but are unable to eliminate infection. (3) Dissemination competent bacteria escape from the skin immediately after inoculation via lymphatic vessels (green) to reach the draining lymph node. (4) Y. pestis colonizes the lymph node at very high rates. (5) The bacteria escape the lymph node compartment into systemic circulation through efferent lymphatic vessels or via blood vessels (red). The questions at the right of the figure summarize areas of the field that need to be explored to obtain a more detailed picture of how Y. pestis disseminates in the body.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Sebbane F, et al. Kinetics of disease progression and host response in a rat model of bubonic plague. Am J Pathol. 2005;166:1427–1439. doi: 10.1016/S0002-9440(10)62360-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gonzalez RJ, et al. Bioluminescence imaging to track bacterial dissemination of Yersinia pestis using different routes of infection in mice. BMC Microbiol. 2012;12:147. doi: 10.1186/1471-2180-12-147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gonzalez RJ, et al. Comparison of models for bubonic plague reveals unique pathogen adaptations to the dermis. Infect Immun. 2015 doi: 10.1128/IAI.00140-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gonzalez RJ, et al. Dissemination of a highly virulent pathogen: tracking the early events that define infection. PLoS Pathog. 2015;11:e1004587. doi: 10.1371/journal.ppat.1004587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shannon JG, et al. Yersinia pestis subverts the dermal neutrophil response in a mouse model of bubonic plague. MBio. 2013;4:e00170-13. doi: 10.1128/mBio.00170-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bosio CF, et al. Kinetics of innate immune response to Yersinia pestis after intradermal infection in a mouse model. Infect Immun. 2012;80:4034–4045. doi: 10.1128/IAI.00606-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pujol C, Bliska JB. The ability to replicate in macrophages is conserved between Yersinia pestis and Yersinia pseudotuberculosis. Infect Immun. 2003;71:5892–5899. doi: 10.1128/IAI.71.10.5892-5899.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Titball RW, et al. Yersinia pestis and plague. Biochem. Soc. Trans. 2003;31:104–107. doi: 10.1042/bst0310104. [DOI] [PubMed] [Google Scholar]
- 9.Guinet F, et al. Dissociation of Tissue Destruction and Bacterial Expansion during Bubonic Plague. PLoS Pathog. 2015;11:e1005222. doi: 10.1371/journal.ppat.1005222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lorange EA, et al. Poor vector competence of fleas and the evolution of hypervirulence in Yersinia pestis. J Infect Dis. 2005;191:1907–1912. doi: 10.1086/429931. [DOI] [PubMed] [Google Scholar]
- 11.Brubaker R. Yersinia pestis and bubonic plague. Prokaryotes. 2006;6:399–442. [Google Scholar]
- 12.Shannon JG, et al. Dermal neutrophil, macrophage and dendritic cell responses to Yersinia pestis transmitted by fleas. PLoS Pathog. 2015;11:e1004734. doi: 10.1371/journal.ppat.1004734. [DOI] [PMC free article] [PubMed] [Google Scholar]