Abstract
Opioid use in pregnancy has increased dramatically over the past decade. Since prenatal opioid use is associated with numerous obstetrical and neonatal complications, this now has become a major public health problem. In particular, in utero opioid exposure can result in neonatal abstinence syndrome (NAS) which is a serious condition characterized by central nervous system hyperirritability and autonomic nervous system dysfunction. The present review seeks to define current practices regarding the approach to the pregnant mother and neonate with prenatal opiate exposure. Although the cornerstone of prenatal management of opioid dependence is opioid maintenance therapy, the ideal agent has yet to be definitively established. Pharmacologic management of NAS is also highly variable and may include an opioid, barbiturate, and/or α-agonist. Genetic factors appear to be associated with the incidence and severity of NAS. Establishing pharmacogenetic risk factors for the development of NAS has the potential for creating opportunities for “personalized genomic medicine” and novel, individualized therapeutic interventions.
Keywords: Newborn, opioids, pregnancy, neonatal abstinence syndrome
Prevalence of opiate use in pregnancy
Opiate use in the US has risen dramatically in recent years. In 2012, health care professionals dispensed an average of 82.5 opioid prescriptions per 100 persons, with significant variation observed between states (up to 143 prescriptions per 100 persons in some southern states).1 Women of reproductive age–have been particularly impacted, with approximately 28% of privately-insured and 39% of Medicaid enrolled women age 15–44 years filling a prescription for an opioid medication each year for five consecutive years.2 Illicit use of opioids (especially heroin) has also increased significantly over this same time period. Consistent with these national trends, maternal opiate use in pregnancy has also increased from 1.19 per 1000 births in 2000 to 5.63 in 2009, with 60% of these mothers insured through Medicaid.3 In parallel, the burden of NAS has increased from 7 to 27 per 1000 NICU admissions between 2004 and 2013.4 Factors associated with worse NAS outcomes include maternal use of cigarettes and other psychotropic medications such as benzodiazepines and selective serotonin re-uptake inhibitors (SSRIs).5–8 The impact of these drug-drug interactions on the fetus and how they might influence NAS have not been fully characterized.
Maternal agonist treatment for opiate-dependent pregnant women
Substance abuse use during pregnancy is associated with fetal death, intrauterine growth retardation, placental insufficiency, postpartum hemorrhage, pre-eclampsia, and premature rupture of membranes.9 Maternal opioid-substitution programs have been shown to improve pregnancy outcomes by minimizing the use of illicit drugs, reducing withdrawal and high risk behaviors, and improving compliance with prenatal care.10 The most common FDA approved agents are methadone and buprenorphine. The pharmacokinetics of methadone in pregnant women differ from the non-pregnant population and change significantly throughout pregnancy. For example, the half-life of methadone falls from an average of 23 hours in non-pregnant women to approximately 8 hours in pregnant women.11 The reduced half-life and increased volume of distribution in the pregnant woman often necessitates increased dosing as pregnancy progresses. Established drug-drug interactions exist between methadone and some anti-epileptics, rifampin, and several anti-retrovirals often used in the treatment of human immunodeficiency virus infection.
An alternative to methadone for maintenance therapy in pregnancy is buprenorphine, a partial mu-opioid agonist.12 Demonstrated advantages of buprenorphine over methadone include a diminished risk of overdose (due to low intrinsic receptor efficacy), less abrupt withdrawal, fewer drug-drug interactions, and prescriptions that are easier to obtain.13,14 In addition, buprenorphine has been associated with an overall reduction in the incidence and severity of NAS compared to methadone.15,16 Disadvantages of buprenorphine include increased dropout rates, more difficult initiation of treatment, potential risk of drug diversion, less social support and counseling compared to conventional methadone maintenance programs, and lack of long-term pregnancy and childhood safety data.17, 18
Neonatal Abstinence Syndrome
While opioid maintenance treatment during pregnancy improves maternal and infant outcomes, it does not prevent the development of NAS. In utero exposure to opioids in pregnancy is associated with a 60–80% risk of NAS requiring pharmacologic treatment.4 NAS is a highly variable condition characterized by central nervous system hyperirritability, autonomic nervous system dysfunction and gastrointestinal disturbances. Defining features include: excessive crying, irritability, poor sleep, increased muscle tone, tremors, excoriations of the skin from excessive movements, hyperthermia, loose stools, yawning, sweating, nasal stuffiness, and sneezing. In addition, seizures can occur in 2–11% of infants with NAS.19,20 The specific pathophysiology of neonatal opioid withdrawal and the factors that influence severity remain incompletely understood. However, altered levels of neurotransmitters such as norepinephrine, dopamine, and serotonin are believed to play a significant role.19, 21–23 Conceptually, every infant with in utero opioid exposure resides along the continuum of signs of withdrawal. While some have mild, clinically insignificant signs, others have more severe disease that significantly impacts growth and development without treatment. Thus, the diagnosis of NAS is not made by the need for pharmacologic treatment, but instead by the cardinal signs of neonatal withdrawal.
The most common approach to monitoring infants for NAS is the Finnegan scoring instrument. The scoring is performed in a serial manner to help determine: 1) which neonates require pharmacologic therapy; 2) how dosing should be escalated; and 3) when weaning should occur. The traditional Finnegan scoring system consists of a 31-item scale used to assess the presence and severity of various NAS-associated symptoms and is performed every 3–4 hours.19 Each evaluation should take into account behavior observed over the entire 3–4 hour period leading up to the assessment. A score of 7 on day 2 of life corresponds with the 95th percentile for non-exposed infants. A score of >8 is highly suggestive of NAS even in those denying opioid use during pregnancy.24 The Finnegan scoring system is primarily designed for term infants, making use in both preterm and older (>30 day) infants non-standardized. A significant limitation of the scoring system is the significant intra-observer variability that has been documented.16 Thus, continuous staff education and gold standard evaluations are a critical piece of optimal NAS care.
Maternal history taken in a neutral and non-judgmental fashion will identify the large majority of infants with in utero exposure. An adjunct to verbal history is typically provided via urine or meconium screening of the newborn. Hair and umbilical cord analyses have also been proposed, but their utility in medical management is limited.25 Urine screening has the advantage of being easily performed, but is limited by the identification of only recent exposures. Meconium testing has the advantage of screening for substance exposure extending back as far as 20 weeks gestation.
Treatment
The primary clinical concern for withdrawal is the impact upon growth and development. Secondary effects include impaired maternal bonding, infant discomfort, and seizures. The most effective treatment approaches are those that employ a systematic, multidisciplinary, and multimodal approach. Given the complexity of the disease and setting of treatment, a continuous process of quality improvement will lead to improved patient outcomes. Treatment is optimized when staff engage mothers with respect and acknowledge the struggles with substance abuse. Such mothers, who often experience other psychiatric and psychosocial comorbidities, are often sensitive to the perceived judgment of staff.
Non-Pharmacologic Treatment
All infants at risk for NAS should be managed with a non-pharmacologic approach that involves creating a quiet and soothing environment with the avoidance of excessive environmental stimulation. Frequent hypercaloric feeds minimize hunger and promote growth. Rooming-in may reduce the need for pharmacologic treatment and should be strongly encouraged if the situation permits. Maternal involvement in the infant’s care is an important component of non-pharmacologic management.19,26
In the absence of maternal HIV infection, illicit drug use, or other contraindications, both the American Congress of Obstetrics and Gynecology (ACOG) and the American Academy of Pediatrics (AAP) encourage breastfeeding in women in methadone or buprenorphine treatment programs.18,27 Breastfeeding has been associated with a decrease in the incidence and severity of NAS and should be encouraged.28 The amount of maternally transferred methadone or buprenorphine is low, but an additional therapeutic benefit is the physical contact and bonding. Multimodal institutional policies that promote safe breastfeeding are effective in increasing the very low rates of breast feeding among infants at risk for NAS. 29
Pharmacologic Therapy
Pharmacologic treatment is required in the 60–80% of infants who do not respond to non-pharmacologic therapy.20 Primary outcome measures in comparing treatments are duration of treatment, length of hospital stay, and need for adjunctive therapies. Despite a significant effort within the medical community to find the ideal drug and dosing regimen, the most important predictor of success in reducing total length of hospital stay and duration of pharmacologic treatment is the use of a standardized institutional protocol based on best practice (promoted by the Vermont-Oxford Neonatal Network). The use of a standardized approach is more important than the use of a specific drug (methadone or morphine) for pharmacologic treatment of NAS. In Central Ohio, a 50% decrease in length of stay (36 to 18 day) was achieved through the use of a Model for Improvement approach that involved standardized assessment and treatment protocols, educational outreach and assessment, and involvement of multiple stakeholders.30 Protocols developed in a multidisciplinary fashion have the highest potential for success [www.mededportal.org/icollaborative/resource/3920].
The AAP, multiple Cochrane reviews, and expert reviews identify opioid replacement as first line pharmacotherapy treatment for NAS.20,27,31–33 However, several treatment approaches are used and no universal standard of care for NAS exists. The most commonly used treatment approach initially uses an opioid. If there is inadequate response to a single agent at higher doses, a second line agent of phenobarbital or clonidine is used as an adjunct. However, there is significant heterogeneity in treatment approaches and the optimal treatment protocol has not been established in large, well-controlled studies.4,34–36 Variations include the initial use of phenobarbital monotherapy instead of an opioid, or initial dual therapy with an opioid and either phenobarbital or clonidine. In all cases, the approach involves rapid up-titration in dose to control symptoms, followed by a gradual weaning of typically 10% per day if signs of withdrawal allow.
Opioids
Morphine and Methadone
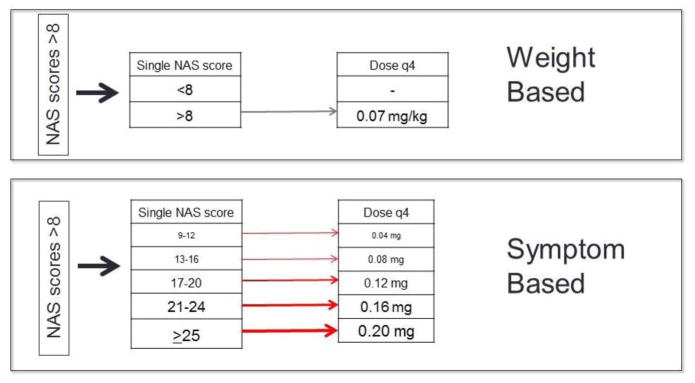
The two opioids used in practice are oral morphine and methadone. Morphine is the primary opioid used in the majority of centers, with methadone being used in 10–20% of hospitals.34 The pharmacokinetics of morphine in neonates are well established.37 Due to a short half-life, morphine is administered every 3–4 hours. The two approaches to dosing morphine are a fixed mg/kg dose or a fixed mg (non-weight based) dose depending upon severity of withdrawal signs/symptoms (Figure 1). These two approaches have not been directly compared in a clinical trial, with dosing protocols provided in Table 1. Comparisons between institutions using one or the other approach are not valid due to significant differences in patient population, robustness of institutional protocols, prenatal care, and other non-pharmacologic factors.
Figure 1.
Representative initiation doses for weight based compared to symptom based morphine dosing using the Finnegan score
Table 1.
Commonly Used Morphine Treatment Regimens (based on Finnegan Scoring every 4 h)
| Weight based | Symptom based16,19 ( doses are not based on body weight) RE-specify to avoid confusion or errors | |
|---|---|---|
|
| ||
Initial dose:
|
Initial dose ( not based on body weight? For first score >8, re-score in one hour to verify. If still elevated: | |
|
| ||
| Single NAS score | Dose q4h | |
|
| ||
| 9–12 | 0.04 mg | |
|
| ||
| 13–16 | 0.08 mg | |
|
| ||
| 17–20 | 0.12 mg | |
|
| ||
| 21–24 | 0.16 mg | |
|
| ||
| >25 | 0.20 mg | |
|
| ||
| Dose Increase: | ||
|
| ||
| Single NAS score | Increase Dose | |
|
| ||
| 0–9 | None | |
|
| ||
| 9–12 | 0.02 mg | |
|
| ||
| 13–16 | 0.04 mg | |
|
| ||
| 17–20 | 0.06 mg | |
|
| ||
Weaning Dose:
| ||
|
| ||
| Two NAS scores | Increase Dose | |
|
| ||
| 9–12 | 0.01 mg | |
|
| ||
| 13–16 | 0.02 mg | |
|
| ||
| 17–20 | 0.04 mg | |
|
| ||
| ||
|
Adjunctive treatment:
At dose of morphine 1.6 mg/day initiate second medication* | ||
phenobarbital loading dose of 20 mg/kg followed by 5 mg/kg/day OR clonidine
An alternative to morphine is methadone, which has a longer half-life, requiring less frequent administration and titration. The inter-individual pharmacokinetic variability in adults and children is high.38–40 A recently completed but unpublished clinical trial investigating oral methadone pharmacokinetics (NCT01754324) confirmed significant variability in response in NAS patients (Personal communication J Wiles). There are significant variations in dosing regimens used. Typically doses begin around 0.2 mg/kg/day in 2–6 divided doses a day. Some regimens employ a loading dose of 0.1 mg/kg.41 Modeling and simulation techniques to rationally craft a dosing regimen based upon emerging pharmacokinetic data are being pursued. Most formulations of methadone contain ethanol, though a stable ethanol-free methadone solution can be formulated using pure methadone powder. While the pharmacokinetic variability of methadone is of some concern in the outpatient setting, use has generally been safe. Similarly, no QT prolongation in methadone treated neonates has been noted nor has there has been documented morbidity in infants treated for NAS.40
There is no consensus as to the superiority of morphine or methadone. A retrospective review of administrative data from 14 children’s hospitals revealed a length of treatment 45% lower for methadone than morphine.34 This is in contrast to retrospective review of central Ohio patients in which outcomes were equal for both treatments.30 A 2015 single site clinical trial in 78 infants demonstrated a 14 day length of treatment with methadone compared to 21 days for morphine.42 A more definitive answer will be generated by the multi-center BABY trial currently underway (NCT01958476).
Buprenorphine
NAS treatment with sublingual buprenorphine has been investigated.31,43 While a phase 1 investigation suggested a 30% reduction in length of stay compared to morphine, a definitive randomized clinical trial will be completed in 2016 (NCT01452789). Like phenobarbital and most methadone formulations, buprenorphine contains a significant amount of ethanol. Despite widespread use in many medications as a preservative (e.g. extrinsic), the pharmacodynamic and safety profile of ethanol in neonates has not well defined.44 A pharmacokinetic model of buprenorphine in infants with NAS has been generated.45 This can serve as the basis of modeling and simulation to optimize dose and dose schedules that takes into account developmental ontogeny of metabolic processes and the natural history of symptom resolution in NAS.
Phenobarbital
Phenobarbital (phenobarbitone in the United Kingdom) is a barbiturate antiepileptic. Although it is often used as an adjunctive treatment once a maximum opioid dose is reached, it can be given as an initial adjunct in combination therapy with an opioid or as initial monotherapy.46–48 The half-life of phenobarbital in neonates is 115 hours at 1 week and declines to 67 hours after 4 weeks.49 This prolonged half-life means many standard doses (usually 5 mg/kg) are needed to reach steady state, and explains the improved outcome with a loading dose.50 The typical loading dose is 20 mg/kg, which leads to therapeutic concentrations for the majority of infants. It should be noted that the therapeutic range has been defined for treatment of seizures, but it does provide useful information about safety and appropriate dosing ranges. Phenobarbital appears to have particular utility in those infants with poly-drug exposure in utero, perhaps due to a more global CNS depressive effect. Phenobarbital causes increased breakdown of many drugs metabolized by the cytochrome P450 system. Despite widespread use in newborns (80% of all neonatal seizures, up to 30,000 infants receive this drug each year) the safety profile has not been fully established.51 Phenobarbital has been reported to be associated with cognitive deficits in children taking it for complicated febrile seizures and animal data is suggestive of disruptions to synaptic development.52 However, there is no evidence of neurodevelopmental effects at 36 months after antenatal exposure and no data on long term outcomes of infants treated for NAS.53 At the current time, short term efficacy and safety of phenobarbital has been established and it remains a viable option for treating NAS.
Clonidine
Clonidine is a centrally acting α agonist used for hypertension and adult withdrawal syndromes by way of reducing global sympathetic tone. Mechanistically, this counters the symptoms of NAS driven by the hyperadrenergic state induced by withdrawal. While clonidine is less efficacious in the management of withdrawal symptoms in adults, it has an advantage as a non-opioid adjunctive treatment.54 Safety concerns include hypotension during treatment and rebound hypertension or arrhythmia following cessation. Though non-clinically significant hemodynamic changes are seen with use in NAS, the safety profile for inpatient use has been favorable.55 Clonidine has been systematically investigated mostly as an adjunct or rescue medication, but has also been studied as a replacement for morphine in a small pilot trial (Table 2). The relative efficacy compared to phenobarbital has not been established, though one clinical trial suggested longer duration of therapy with clonidine.47
Table 2.
Randomized Controlled Trials employing Clonidine
| Year | Treatments | n | Clonidine dose (mcg/kg) | Outcome in Length of Stay (LOS) or Length of Treatment (LOT) |
|---|---|---|---|---|
| Agthe, 2009 (Agthe, Kim et al. 2009) | Morphine + clonidine vs Morphine + placebo | 40 | 1.0 Q4 hours | LOT 11 day (morphine and clonidine) vs. 15 day (morphine alone) |
| Suran (Surran, Visintainer et al. 2013) | Morphine + clonidine vs morphine + phenobarbital | 68 | 1–2 Q6 hours | LOT 18.2 days (Morphine +phenobarbital) vs 13.6 days (Morphine + clonidine) |
| Bada 2015 (Bada, Sithisarn et al. 2015) | Clonidine vs Morphine | 31 | 0.625 Q3 hours | LOT 39 days (morphine) vs 28 days (clonidine) |
Outpatient Treatment
Pharmacologic treatment for the great majority of infants occurs in an inpatient hospital setting. However, a combined inpatient/outpatient treatment approach can reduce the total length of stay by ~50% compared to inpatient only, but is associated with significantly longer lengths of treatment.28,42,56 Methadone is the most commonly employed agent due to a longer half-life, though phenobarbital and morphine have been used. It should be noted that these findings are all based upon retrospective reviews and not randomized, prospective investigations. It is likely that the ability to even be considered for outpatient treatment significantly impacted the length of stay in these studies. Additionally, there needs to be a comprehensive screening of the home environment to assess the suitability for outpatient treatment, as well as a robust infrastructure to track and manage outpatient treatment. Lastly, while shortened length of hospitalization is associated with less resource utilization, it is not clear that a shortened length of stay is beneficial for all infants. There may be individual mothers and infants for whom the inpatient stay allows for stabilization of medical, social, environmental, and/or psychiatric issues. A more vigorous expansion to the outpatient setting must be made with caution, especially given the significant variability of methadone pharmacokinetics in infants with NAS. Although reports of small numbers of infants suggest the practice is safe, sudden infant death attributed to bed sharing and unsafe sleep practice has been recently reported in a cohort of infants weaned at home using morphine.56
Long-term follow-up
Adverse neurodevelopmental outcomes have been described in infants and children exposed to opioids in utero. However, even though infants have been treated for NAS for over 30 years, there is relatively little data on long-term neurodevelopmental outcomes. This is primarily due to small studies that are unable to differentiate the effects of in utero exposures and postnatal treatments with confounding environmental influences. In general, opioid exposed children are more likely to have attention deficit disorders, disruptive behavior, and the need for comprehensive psychiatric referrals.57,58 Polydrug exposed children have smaller brains, thinner cortices, reduced cognitive ability and more behavioral problems.59 Studies of long term outcomes based upon short term exposure to drugs to treat NAS are extremely difficult to conduct. It is unlikely that the type of opioid used would have any impact on long term cognitive effects. An unmet need in long term follow-up is an examination of the role of phenobarbital.
Predictive factors
Factors that influence the onset and severity of NAS remain incompletely understood. Outcomes typically evaluated include treatment for NAS, peak NAS score, total dose required for treatment, duration of treatment, and length of hospitalization.
Maternal opiate dose
Many studies have attempted to define the correlation between maternal dose of methadone and NAS severity.26,60–62 A systematic review and meta-analysis suggest that maternal methadone or buprenorphine dose does not appear to correlate with the severity of NAS, a finding confirmed in the prospective, randomized Maternal Opioid Treatment: Human Experimental Research (MOTHER) trial.16,63 Low doses of methadone often lead to relapse or drug substitution to control symptoms. Higher methadone doses are associated with higher birth weight and head circumference. The prevailing approach in maternal management is to use the dose of methadone that best prevents maternal withdrawal. Optimizing maternal management will lead to better neonatal outcomes. These data in aggregate suggest that the appropriate maternal methadone dose will optimally ensure adherence and that dosing designed primarily to impact neonatal outcome will not be effective.
Maternal maintenance agent
Although methadone remains the most studied treatment for opiate dependence in pregnancy, initial studies have suggested that neonates exposed to buprenorphine in utero may be less likely to develop NAS compared to methadone.64 The MOTHER trial examined neonatal outcomes in pregnancies with exposure to buprenorphine versus methadone.16 Buprenorphine was associated with a significantly lower cumulative amount of morphine needed to treat NAS, shorter duration of treatment, and a 58% reduction in length of hospital stay. There were no differences between the buprenorphine and methadone groups with respect for the need for treatment, peak NAS score, or rate of serious maternal or neonatal adverse events. While the study suggested a less severe NAS course in neonates previously exposed to buprenorphine, a significantly higher dropout rate was observed in the buprenorphine group compared to the methadone group (33% vs 18%). In addition, entry criteria excluded mothers who were also receiving benzodiazepines which are known to influence NAS.
A recent Cochrane review indicated that existing data were inadequate to conclude whether methadone, buprenorphine, or other agents were superior for any relevant maternal or neonatal outcome.65 Relatively little information is available regarding the combined formulation of buprenorphine and naloxone compared to buprenorphine or methadone alone with respect to important NAS outcomes. However, some studies suggest less need for treatment, lower peak NAS scores, and shorter length of hospitalization in neonates exposed to the combined formulation.66, 67
Exposure to additional substances
Several studies have examined the combined effects of exposure to opiates and other substances on the incidence and severity of NAS. In a secondary analysis of the MOTHER study, Kaltenbach and colleagues found that greater nicotine use at delivery (defined by number of cigarettes smoked in the twenty-four hours prior to birth) was associated with higher rates of treatment for NAS as well as the total dose of medication required.61 However, maternal nicotine use did not correlate with higher peak NAS scores or duration of treatment. The same study also examined the relationship between SSRIs and the development of NAS. Although there was no correlation between maternal SSRI use and whether an infant received treatment for NAS, in infants who did require treatment, maternal SSRI use was associated with higher peak NAS scores and total dose of opioid replacement medication. This contrasted with the work of Seligman and colleagues who did not find an association between use of antidepressants and the incidence or severity of NAS.68 However, this study did find an association between concomitant exposure to benzodiazepines and longer length of treatment, which confirmed earlier work on the topic.28,69
Gestational age
Preterm neonates have a lower rate of NAS than term infants.68,70 This may be related to immaturity of the fetal brain and associated number of opiate receptors, lower cumulative drug exposure, less placental transfer, delayed hepatic and placental metabolism, and less drug deposition secondary to lower fat content. It is particularly important to note that assessment of NAS in preterm neonates is complicated by the lack of a validated scoring system specifically designed for this population who may have completely different autonomic responses.
Pharmacogenomics
Genetic factors are known to contribute to opiate addiction in adults.71 Specifically, single-nucleotide polymorphisms (SNPs) in the mu-opioid receptor (OPRM1), multidrug resistance (ABCB1), and catechol-O-methyltransferase (COMT) genes have been associated with adult opioid dependence.72–74 Initial studies in neonates with in utero opiate exposure demonstrated that SNPs in OPRM1 and COMT genes were associated with improved outcomes in infants with NAS.75 Infants with the OPRRM1 118A>G AG/GG genotype had shortened length of stay [β = −8.5 days (CI −14.9, −2.1), p=0.009] and were less likely to receive any treatment than AA infants [48 vs 72%; adjusted OR 0.76 (CI 0.63, 0.96), p=0.006]. The COMT 158A>G AG/GG genotype was associated with shortened length of stay [β = −10.8 days (CI −18.2, −3.4), p=0.005] and less treatment with >2 medications [18 vs 56%; adjusted OR 0.68 (CI 0.55, 0.85), p=0.001] than the AA genotype. SNPs in the maternal OPRM1 were also associated with improved outcome in the newborns. Associations with the ABCB1 SNPs were not significant. Microarray studies have demonstrated that SNPs in two additional opioid receptor genes in infants was associated with worse NAS outcomes.76 The presence of the PNOC rs732636 A allele (OR=3.8, p=0.004) was associated with the need for treatment with two medications and a longer hospital stay (5.8 days; p=0.01). The OPRK1 rs702764 C allele (OR=4.1, p=0.003) was also associated with the need for treatment with two medications. The OPRM1 rs1799971 G allele (β= −6.9 days, p=0.02) and COMT rs740603 A allele (β= −5.3 days, p=0.01) were associated with shorter length of stays. The OPRD1 rs204076 A allele in the mothers was associated with a longer length of stay by 6.6 days (p=0.008).
Epigenetic changes (methylation of DNA which does not change the sequence, but does alter the function of the protein) have also been studied in NAS.77 Hypermethylation of the OPRM1 promoter was seen at the −10 CpG in treated versus untreated infants [adjusted difference δ=3.2% (95% CI 0.3–6.0%), p=0.03; NS after multiple testing correction]. There was hypermethylation at the −14 [δ=4.9% (95% CI 1.8–8.1%), p=0.003], −10 [δ=5.0% (95% CI 2.3–7.7%), p=0.0005)], and +84 [δ=3.5% (95% CI 0.6–6.4), p=0.02] CpG sites in infants requiring treatment with two medications which remained significant for −14 and −10 after correction for multiple testing. While ongoing work in the field is needed to confirm these initial findings, these data do suggest that genetic and epigenetic changes are playing an important role in incidence and severity of NAS. Pharmacogenetic characterization of mothers and infants may eventually help to optimize duration of monitoring for NAS and to customize drug and dose to each individual infant. Additionally, it may allow for individualized prenatal management of mothers with opioid dependence to optimize neonatal outcomes.
Future Directions
The proliferation of electronic medical records and will lead to point-of-care clinical trials in which there is an initial randomization to a specific intervention or drug, followed by standard of care treatment outside of a rigid trial framework. In this way both inpatient and outpatient endpoints of interest can be collected in an efficient fashion. An example of this approach has been proposed to investigate the differential efficacy of buprenorphine compared to methadone78. Additionally, a number of large clinical trials investigating the use of commonly used agents are currently underway (NCT01958476, NCT01958476). Novel agents such ondansetron have been proposed prevent NAS, with a clinical trial examining ondansetron administered to pregnant women and their infants (up to age 5 days) currently enrolling (NCT01965704).79
Determination of current drug doses and regimens for the pharmacologic treatment of NAS has been empiric and extrapolated from other patient populations or limited to patient level data from infants with NAS. Pharmacokinetic modeling and simulation are techniques that allow a quantitative assessment that couples pharmacokinetic data with other covariates such as weight and age (gestational and postnatal). In addition, disease severity and pharmacogenetic factors which impact drug response or disposition can also be included in such models. The power of the models resides not only in the ability to characterize drug behavior with greater precision, but to predict and simulate optimal drug doses. This is a common and widespread technique used in other conditions, but has been increasingly applied to NAS.45,80 Such methods have the potential to increase the efficiency of clinical trials in neonatology by establishing drug doses and regimens that account for known sources of variability (likely closer to the optimal dose at the start of the trial). Thus, modeling and simulation can change a clinical trial from exploratory to confirmatory.81
Summary
As the number of infants with in utero opioid exposure continues to rise, work is urgently needed to address significant knowledge gaps regarding optimal prenatal and postnatal care. Specific areas of focus should include:
Reducing opioid exposure in women of child bearing age
Institutional-wide and multidisciplinary approaches to standardize and continuously assess/improve NAS care protocols
Use of big-data, outcomes methods and pragmatic clinical trials, as well as traditional randomized clinical trials to optimize treatment modalities in NAS
Expanding maternal treatment programs to reduce the incidence and severity of NAS
Better identifying and treating high-risk neonates through personalized genomic medicine
Use of modeling and simulation to optimize drug therapy
Increasing knowledge regarding the long-term effects of in utero opiate exposure and various neonatal treatment modalities
Clearly a multidisciplinary approach is needed with Obstetricians, Pediatricians, Nurses, Social Workers, Addiction Specialists, and Politicians all working together if we hope to significantly impact this important public health problem that is affecting this vulnerable population.
Acknowledgments
This work was supported in part by R01DA02976 (WKK) and R01DA032889-02 (JMD) from the National Institute on Drug Abuse.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Paulozzi LJMK, Hockenberry JM. Vital signs: Variation among states in prescribing opioid pain relievers and benzodiazepines - United States, 2012. MMWR. 2014;63:563–8. [PMC free article] [PubMed] [Google Scholar]
- 2.Ailes ECDA, Lind JN, Gilboa SM, Frey MT, Broussard CS, Honein MA. Opioid Prescription Claims Among Women of Reproductive Age United States, 2008–2012. MMWR. 2015;64:37–41. [PMC free article] [PubMed] [Google Scholar]
- 3.Patrick SW, Schumacher RE, Benneyworth BD, Krans EE, McAllister JM, Davis MM. Neonatal abstinence syndrome and associated health care expenditures: United States, 2000–2009. JAMA. 2012;307:1934–40. doi: 10.1001/jama.2012.3951. [DOI] [PubMed] [Google Scholar]
- 4.Tolia VN, Patrick SW, Bennett MM, et al. Increasing incidence of the neonatal abstinence syndrome in U.S. neonatal ICUs. New Engl J Med. 2015;372:2118–26. doi: 10.1056/NEJMsa1500439. [DOI] [PubMed] [Google Scholar]
- 5.Wachman EM, Newby PK, Vreeland J, et al. The relationship between maternal opioid agonists and psychiatric medications on length of hospitalization for neonatal abstinence syndrome. J Addict Med. 2011;5:293–9. doi: 10.1097/ADM.0b013e3182266a3a. [DOI] [PubMed] [Google Scholar]
- 6.Jones HE, Heil SH, Tuten M, et al. Cigarette smoking in opioid-dependent pregnant women: neonatal and maternal outcomes. Drug Alcohol Depend. 2013;131:271–7. doi: 10.1016/j.drugalcdep.2012.11.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Patrick SW, Dudley J, Martin PR, et al. Prescription opioid epidemic and infant outcomes. Pediatrics. 2015;135:842–50. doi: 10.1542/peds.2014-3299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Seligman NS, Salva N, Hayes EJ, Dysart KC, Pequignot EC, Baxter JK. Predicting length of treatment for neonatal abstinence syndrome in methadone-exposed neonates. Am J Obstet Gynecol. 2008;199:e391–7. doi: 10.1016/j.ajog.2008.06.088. [DOI] [PubMed] [Google Scholar]
- 9.Kennare R, Heard A, Chan A. Substance use during pregnancy: risk factors and obstetric and perinatal outcomes in South Australia. Australian New Zealand J OB-GYN. 2005;45:220–5. doi: 10.1111/j.1479-828X.2005.00379.x. [DOI] [PubMed] [Google Scholar]
- 10.Center for Substance Abuse Treatment: SAHMSA/CSAT treatment improvement protocols. Rockville (MD): Substance Abuse and Mental Health Services Administration; 2008. Medication-assisted treatment for opioid addiction during pregnancy. [PubMed] [Google Scholar]
- 11.Swift RM, Dudley M, DePetrillo P, Camara P, Griffiths W. Altered methadone pharmacokinetics in pregnancy: implications for dosing. J Substance Abuse. 1989;1:453–60. [PubMed] [Google Scholar]
- 12.Wiegand SL, Stringer EM, Stuebe AM, Jones H, Seashore C, Thorp J. Buprenorphine and naloxone compared with methadone treatment in pregnancy. Obstet Gynecol. 2015;125:363–8. doi: 10.1097/AOG.0000000000000640. [DOI] [PubMed] [Google Scholar]
- 13.Walsh SL, Preston KL, Stitzer ML, Cone EJ, Bigelow GE. Clinical pharmacology of buprenorphine: ceiling effects at high doses. Clin Pharmacol Therapeutics. 1994;55:569–80. doi: 10.1038/clpt.1994.71. [DOI] [PubMed] [Google Scholar]
- 14.Bell JR, Butler B, Lawrance A, Batey R, Salmelainen P. Comparing overdose mortality associated with methadone and buprenorphine treatment. Drug Alcohol Depend. 2009;104:73–7. doi: 10.1016/j.drugalcdep.2009.03.020. [DOI] [PubMed] [Google Scholar]
- 15.Jones HE, Heil SH, Baewert A, et al. Buprenorphine treatment of opioid-dependent pregnant women: a comprehensive review. Addiction. 2012;107(Suppl 1):5–27. doi: 10.1111/j.1360-0443.2012.04035.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jones HE, Kaltenbach K, Heil SH, et al. Neonatal abstinence syndrome after methadone or buprenorphine exposure. New Engl J Med. 2010;363:2320–31. doi: 10.1056/NEJMoa1005359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Johnson RE, Jones HE, Fischer G. Use of buprenorphine in pregnancy: patient management and effects on the neonate. Drug Acohol Depend. 2003;70:S87–101. doi: 10.1016/s0376-8716(03)00062-0. [DOI] [PubMed] [Google Scholar]
- 18.Women ACoHCfU, American Society of Addiction M. ACOG Committee Opinion No. 524: Opioid abuse, dependence, and addiction in pregnncy. Obstetr Gynecol. 2012;119:1070–6. doi: 10.1097/AOG.0b013e318256496e. [DOI] [PubMed] [Google Scholar]
- 19.Jansson LM, Velez M, Harrow C. The opioid-exposed newborn: assessment and pharmacologic management. J Opioid Manag. 2009;5:47–55. [PMC free article] [PubMed] [Google Scholar]
- 20.Kocherlakota P. Neonatal abstinence syndrome. Pediatrics. 2014;134:e547–61. doi: 10.1542/peds.2013-3524. [DOI] [PubMed] [Google Scholar]
- 21.Little PJ, Price RR, Hinton RK, Kuhn CM. Role of noradrenergic hyperactivity in neonatal opiate abstinence. Drug Alcohol Depend. 1996;41:47–54. doi: 10.1016/0376-8716(96)01236-7. [DOI] [PubMed] [Google Scholar]
- 22.Spiga S, Puddu MC, Pisano M, Diana M. Morphine withdrawal-induced morphological changes in the nucleus accumbens. European J Neuro. 2005;22:2332–40. doi: 10.1111/j.1460-9568.2005.04416.x. [DOI] [PubMed] [Google Scholar]
- 23.Lunden JW, Kirby LG. Opiate exposure and withdrawal dynamically regulate mRNA expression in the serotonergic dorsal raphe nucleus. Neuroscience. 2013;254:160–72. doi: 10.1016/j.neuroscience.2013.08.071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zimmerman-Baer U, Notzli U, Rentsch K, Bucher HU. Finnegan neonatal abstinence scoring system: normal values for first 3 days and weeks 5–6 in non-addicted infants. Addiction. 2010;105:524–8. doi: 10.1111/j.1360-0443.2009.02802.x. [DOI] [PubMed] [Google Scholar]
- 25.Concheiro M, González-Colmenero E, Lendoiro E, et al. Alternative matrices for cocaine, heroin, and methadone in utero drug exposure detection. Ther Drug Monit. 2013;35:702–9. doi: 10.1097/FTD.0b013e31828a6148. [DOI] [PubMed] [Google Scholar]
- 26.Velez ML, Jansson LM, Schroeder J, Williams E. Prenatal methadone exposure and neonatal neurobehavioral functioning. Pediatr Res. 2009;66:704–9. doi: 10.1203/PDR.0b013e3181bc035d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hudak ML, Tan RC Committee on Drugs, Committee on Fetus and Newborn, American Academy of Pediatrics. Neonatal drug withdrawal. Pediatrics. 2012;129:e540–60. doi: 10.1542/peds.2011-3212. [DOI] [PubMed] [Google Scholar]
- 28.Abdel-Latif ME, Pinner J, Clews S, Cooke F, Lui K, Oei J. Effects of breast milk on the severity and outcome of neonatal abstinence syndrome among infants of drug-dependent mothers. Pediatrics. 2006;117:e1163–9. doi: 10.1542/peds.2005-1561. [DOI] [PubMed] [Google Scholar]
- 29.Lind JN, Petersen EE, Lederer PA, et al. Infant and maternal characteristics in neonatal abstinence syndrome--selected hospitals in Florida, 2010–2011. MMWR. 2015;64:213–6. [PMC free article] [PubMed] [Google Scholar]
- 30.Hall ES, Wexeblatt SL, Crowley M, et al. A multicenter cohort study of treatments and hospital outcomes in neonatal abstinence syndrome. Pediatrics. 2014;134:e527–34. doi: 10.1542/peds.2013-4036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Osborn DA, Jeffrey HE, Cole MJ. Opiate treatment for opiate withdrawal in newborn infants. Cochrane Data Syst Rev. 2010;10:CD002059. doi: 10.1002/14651858.CD002059.pub3. [DOI] [PubMed] [Google Scholar]
- 32.Osborn DA, Jeffrey HE, Cole MJ. Sedatives for opiate withdrawal in newborn infants. Cochrane Data Syst Rev. 2010;10:CD002053. doi: 10.1002/14651858.CD002053.pub3. [DOI] [PubMed] [Google Scholar]
- 33.Jansson LM, Velez M. Neonatal abstinence syndrome. Current Opinion Pediatr. 2012;24:252–8. doi: 10.1097/MOP.0b013e32834fdc3a. [DOI] [PubMed] [Google Scholar]
- 34.Patrick SW, Kaplan HC, Passarella M, Davis MM, Lorch SA. Variation in treatment of neonatal abstinence syndrome in US children's hospitals, 2004–2011. J Perinatol. 2014;34:867–72. doi: 10.1038/jp.2014.114. [DOI] [PubMed] [Google Scholar]
- 35.O'Grady MJ, Hopewell J, White MJ. Management of neonatal abstinence syndrome: a national survey and review of practice. Arch Dis Child Fetal Neonat. 2009;94:F249–52. doi: 10.1136/adc.2008.152769. [DOI] [PubMed] [Google Scholar]
- 36.Sarkar S, Donn SM. Management of neonatal abstinence syndrome in neonatal intensive care units: a national survey. J Perinatol. 2006;26:15–7. doi: 10.1038/sj.jp.7211427. [DOI] [PubMed] [Google Scholar]
- 37.Boumeester NJ, Anderson BJ, Tibboel D, Holford NH. Developmental pharmacokinetics of morphine and its metabolites in neonates, infants and young children. British J Anaesth. 2004;92:208–17. doi: 10.1093/bja/aeh042. [DOI] [PubMed] [Google Scholar]
- 38.Ferrari A, Coccia CP, Bertolini A, Sternieri E. Methadone--metabolism, pharmacokinetics and interactions. Pharm Res. 2004;50:551–9. doi: 10.1016/j.phrs.2004.05.002. [DOI] [PubMed] [Google Scholar]
- 39.Yang F, Tong X, McCarver DG, Hines RN, Beard DA. Population-based analysis of methadone distribution and metabolism using an age-dependent physiologically based pharmacokinetic model. J Pharmacokin Pharmacodynam. 2006;33:485–518. doi: 10.1007/s10928-006-9018-0. [DOI] [PubMed] [Google Scholar]
- 40.Ward RM, Drover DR, Hammer GB, et al. The pharmacokinetics of methadone and its metabolites in neonates, infants, and children. Paediatr Anaesth. 2014;24:591–601. doi: 10.1111/pan.12385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lainwala S, Brown ER, Weinschenk NP, Blackwell MT, Hagadorn JI. A retrospective study of length of hospital stay in infants treated for neonatal abstinence syndrome with methadone versus oral morphine preparations. Adv Neonat Care. 2005;5:265–72. doi: 10.1016/j.adnc.2005.06.003. [DOI] [PubMed] [Google Scholar]
- 42.Brown MS, Hayes MJ, Thorton LM. Methadone versus morphine for treatment of neonatal abstinence syndrome: a prospective randomized clinical trial. J Perinatol. 2015;35:278–83. doi: 10.1038/jp.2014.194. [DOI] [PubMed] [Google Scholar]
- 43.Kraft WK, Dysart K, Greenspan JS, Gibson E, Kaltenbach K, Ehrlich ME. Revised dose schema of sublingual buprenorphine in the treatment of the neonatal opioid abstinence syndrome. Addiction. 2011;106:574–80. doi: 10.1111/j.1360-0443.2010.03170.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Marek E, Kraft WK. Ethanol pharmacokinetics in neonates and infants. Cur Ther Res Clin Exp. 2014;76:90–7. doi: 10.1016/j.curtheres.2014.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.NGCM, Dombrowsky E, Lin H, et al. Population pharmacokinetic model of sublingual buprenorphine in Neonatal Abstinence Syndrome. Pharmacotherapy. 2015;35:670–80. doi: 10.1002/phar.1610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Coyle MG, Ferguson A, Lagasse L, Oh W, Lester B. Diluted tincture of opium and phenobarbital versus DTO alone for neonatal opiate withdrawal in term infants. J Pediatr. 2002;140:561–4. doi: 10.1067/mpd.2002.123099. [DOI] [PubMed] [Google Scholar]
- 47.Surran B, Visitainer P, Chamberlin S, Kopcza K, Shah B, Singh R. Efficacy of clonidine versus phenobarbital in reducing neonatal morphine sulfate therapy days for neonatal abstinence syndrome. A prospective randomized clinical trial. J Perinatol. 2013;33:954–9. doi: 10.1038/jp.2013.95. [DOI] [PubMed] [Google Scholar]
- 48.Jackson L, Ting A, McKay S, Galea P, Skeoch C. A randomised controlled trial of morphine versus phenobarbitone for neonatal abstinence syndrome. Arch Dis Child Fet Neonat. 2004;89:F300–4. doi: 10.1136/adc.2003.033555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Pitlick W, Painter M, Pippenger C. Phenobarbital pharmacokinetics in neonates. Clin Pharm Ther. 1978;23:346–50. doi: 10.1002/cpt1978233346. [DOI] [PubMed] [Google Scholar]
- 50.Finnegan LP, Michael H, Leifer B. The use of phenobarbital in treating abstinence in newborns exposed in utero to psychoactive agents. NIDA Res Monograph. 1984;49:329. [PubMed] [Google Scholar]
- 51.Blume HK, Garrison MM, Christakis DA. Neonatal seizures: treatment and treatment variability in 31 United States pediatric hospitals. J Child Neurol. 2009;24:148–54. doi: 10.1177/0883073808321056. [DOI] [PubMed] [Google Scholar]
- 52.Forcelli PA, Janssen MJ, Vicini S, Gale K. Neonatal exposure to antiepileptic drugs disrupts striatal synaptic development. Ann Neurol. 2012;72:363–72. doi: 10.1002/ana.23600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Shankaran S, Papile LA, Wright LL, et al. Neurodevelopmental outcome of premature infants after antenatal phenobarbital exposure. Am J OB GYN. 2002;187:171–7. doi: 10.1067/mob.2002.122445. [DOI] [PubMed] [Google Scholar]
- 54.Gowing L, Farrell MF, Ali R, White JM. Alpha2-adrenergic agonists for the management of opioid withdrawal. Cochrane Data System Rev. 2014;3:CD002024. doi: 10.1002/14651858.CD002024.pub4. [DOI] [PubMed] [Google Scholar]
- 55.Agthe AG, Kim GR, Mathias KB, et al. Clonidine as an adjunct therapy to opioids for neonatal abstinence syndrome: a randomized, controlled trial. Pediatrics. 2009;123:e849–56. doi: 10.1542/peds.2008-0978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Kelly LE, Knoppert D, Roukema H, Rieder MJ, Koren G. Oral morphine weaning for neonatal abstinence syndrome at home compared with in-hospital: an observational cohort study. Paediatr Drugs. 2015;17:151–7. doi: 10.1007/s40272-014-0096-y. [DOI] [PubMed] [Google Scholar]
- 57.Ornoy A, Daka L, Goldzweig G, et al. Neurodevelopmental and psychological assessment of adolescents born to drug-addicted parents: effects of SES and adoption. Child Abuse Neglect. 2010;34:354–68. doi: 10.1016/j.chiabu.2009.09.012. [DOI] [PubMed] [Google Scholar]
- 58.Ornoy A. The impact of intrauterine exposure versus postnatal environment in neurodevelopmental toxicity: long-term neurobehavioral studies in children at risk for developmental disorders. Toxicol Letters. 2003;140:171–81. doi: 10.1016/s0378-4274(02)00505-2. [DOI] [PubMed] [Google Scholar]
- 59.Walhovd KB, Moe V, Slinning K, et al. Volumetric cerebral characteristics of children exposed to opiates and other substances in utero. NeuroImage. 2007;36:1331–44. doi: 10.1016/j.neuroimage.2007.03.070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Seligman NS, Almario CV, Hayes EJ, Dysart KC, Berghella V, Baxter JK. Relationship between maternal methadone dose at delivery and neonatal abstinence syndrome. J Pediatr. 2010;157:428–33. doi: 10.1016/j.jpeds.2010.03.033. [DOI] [PubMed] [Google Scholar]
- 61.Kaltenbach K, Holbrook AM, Coyle MG, et al. Predicting treatment for neonatal abstinence syndrome in infants born to women maintained on opioid agonist medication. Addiction. 2012;107(Suppl 1):45–52. doi: 10.1111/j.1360-0443.2012.04038.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Dashe JS, Sheffield JS, Olscher DA, Todd SJ, Jackson GL, Wendel GD. Relationship between maternal methadone dosage and neonatal withdrawal. Obstet Gynecol. 2002;100:1244–9. doi: 10.1016/s0029-7844(02)02387-6. [DOI] [PubMed] [Google Scholar]
- 63.Jones HE, Dengler E, Garrison A, et al. Neonatal outcomes and their relationship to maternal buprenorphine dose during pregnancy. Drug Alcohol Depend. 2014;134:414–7. doi: 10.1016/j.drugalcdep.2013.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Hytinantti T, Kahila H, Renlund M, Jarvenpaa AL, Halmesmaki E, Kivitie-Kallio S. Neonatal outcome of 58 infants exposed to maternal buprenorphine in utero. Acta Paediatr. 2008;97:1040–4. doi: 10.1111/j.1651-2227.2008.00838.x. [DOI] [PubMed] [Google Scholar]
- 65.Minozzi S, Amato L, Bellisario C, Ferri M, Davoli M. Maintenance agonist treatments for opiate-dependent pregnant women. Cochrane Syst Rev. 2013;12:CD006318. doi: 10.1002/14651858.CD006318.pub3. [DOI] [PubMed] [Google Scholar]
- 66.Debelak K, Morrone WR, O'Grady KE, Jones HE. Buprenorphine + naloxone in the treatment of opioid dependence during pregnancy-initial patient care and outcome data. Am J Addict. 2013;22:252–4. doi: 10.1111/j.1521-0391.2012.12005.x. [DOI] [PubMed] [Google Scholar]
- 67.Wiegand SL, Stringer EM, Stuebe AM, Jones H, Seashore C, Thorp J. Buprenorphine and naloxone compared with methadone treatment in pregnancy. Obstet Gynecol. 2015;125:363–8. doi: 10.1097/AOG.0000000000000640. [DOI] [PubMed] [Google Scholar]
- 68.Seligman NS, Salva N, Hayes EJ, Dysart KC, Pequignot EC, Baxter JK. Predicting length of treatment for neonatal abstinence syndrome in methadone-exposed neonates. Am J Obstet Gynecol. 2008;199:e391–7. doi: 10.1016/j.ajog.2008.06.088. [DOI] [PubMed] [Google Scholar]
- 69.Sutton LR, Hinderliter SA. Diazepam abuse in pregnant women on methadone maintenance. Implications for the neonate. Clin Pediatr. 1990;29:108–11. doi: 10.1177/000992289002900208. [DOI] [PubMed] [Google Scholar]
- 70.Doberczak TM, Kandall SR, Wilets I. Neonatal opiate abstinence syndrome in term and preterm infants. J Pediatr. 1991;118:933–7. doi: 10.1016/s0022-3476(05)82214-0. [DOI] [PubMed] [Google Scholar]
- 71.Kendler KS, Karkowski LM, Neale MC, Prescott CA. Illicit psychoactive substance use, heavy use, abuse, and dependence in a US population-based sample of male twins. Arch Gen Psych. 2000;57:261–9. doi: 10.1001/archpsyc.57.3.261. [DOI] [PubMed] [Google Scholar]
- 72.Mague SD, Blendy JA. OPRM1 SNP (A118G): involvement in disease development, treatment response, and animal models. Drug Alcohol Depend. 2010;108:172–82. doi: 10.1016/j.drugalcdep.2009.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Goldman D, Oroszi G, Ducci F. The genetics of addictions: uncovering the genes. Nature reviews Genetics. 2005;6:521–32. doi: 10.1038/nrg1635. [DOI] [PubMed] [Google Scholar]
- 74.Lotsch J, Skarke C, Liefhold J, Geisslinger G. Genetic predictors of the clinical response to opioid analgesics: clinical utility and future perspectives. Clin Pharmacokinetics. 2004;43:983–1013. doi: 10.2165/00003088-200443140-00003. [DOI] [PubMed] [Google Scholar]
- 75.Wachman EM, Hayes MJ, Brown MS, et al. Association of OPRM1 and COMT single-nucleotide polymorphisms with hospital length of stay and treatment of neonatal abstinence syndrome. JAMA. 2013;309:1821–7. doi: 10.1001/jama.2013.3411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Wachman EM, Hayes MJ, Sherva R, et al. Variations in opioid receptor genes in neonatal abstinence syndrome. Drug Alcohol Depend. 2015 doi: 10.1016/j.drugalcdep.2015.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Wachman EM, Hayes MJ, Lester BM, et al. Epigenetic variation in the mu-opioid receptor gene in infants with neonatal abstinence syndrome. J Pediatr. 2014;165:472–8. doi: 10.1016/j.jpeds.2014.05.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Winhusen T, Wilder C, Wexelblatt SL, et al. Design considerations for point-of-care clinical trials comparing methadone and buprenorphine treatment for opioid dependence in pregnancy and for neonatal abstinence syndrome. Contemp Clin Trials. 2014;39:158–65. doi: 10.1016/j.cct.2014.08.009. [DOI] [PubMed] [Google Scholar]
- 79.Elkomy MH, Sultan P, Carvalho B, et al. Ondansetron pharmacokinetics in pregnant women and neonates: towards a new treatment for neonatal abstinence syndrome. Clin Pharm Therapeutics. 2015;97:167–76. doi: 10.1002/cpt.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Xie HG, Cao YJ, Gauda EB, Agthe AG, Hendrix CW, Lee H. Clonidine clearance matures rapidly during the early postnatal period: a population pharmacokinetic analysis in newborns with neonatal abstinence syndrome. J Clin Pharm. 2011;51:502–11. doi: 10.1177/0091270010370587. [DOI] [PubMed] [Google Scholar]
- 81.Allegaert K, Van Den Anker J. Neonatal drug therapy: The first frontier of therapeutics for children. Clin Pharm Therapeutics. 2015;98:288–97. doi: 10.1002/cpt.166. [DOI] [PMC free article] [PubMed] [Google Scholar]