Abstract
Background
Insomnia increases in prevalence with age, is strongly associated with depression, and has been identified as a risk factor for suicide in several studies. The aim of this study was to determine whether insomnia severity varies between those who have attempted suicide (n = 72), those who only contemplate suicide (n = 28), and those who are depressed but have no suicidal ideation or attempt history (n = 35).
Methods
Participants were middle-aged and older adults (Age 44–87, M = 66 years) with depression. Insomnia severity was measured as the sum of the early, middle, and late insomnia items from the Hamilton Rating Scale for Depression. General linear models examined relations between group status as the independent variable and insomnia severity as the dependent variable.
Results
The suicide attempt group suffered from more severe insomnia than the suicidal ideation and non-suicidal depressed groups (p < .05). Differences remained after adjusting for potential confounders including demographics, cognitive ability, alcohol dependence in the past month, severity of depressed mood, anxiety, and physical health burden. Moreover, greater insomnia severity in the suicide attempt group could not be explained by interpersonal difficulties, executive functioning, benzodiazepine use, or by the presence of post-traumatic stress disorder.
Conclusion
Our results suggest that insomnia may be more strongly associated with suicidal behavior than with the presence of suicidal thoughts alone. Accordingly, insomnia is a potential treatment target for reducing suicide risk in middle-aged and older adults.
Keywords: suicide attempt, suicidal ideation, insomnia symptoms, depression
Introduction
Despite legislative, clinical, and scientific efforts, suicide rates have gradually increased since the turn of the century, particularly among middle-aged and older adults. About 1 in 25 suicide attempts results in death, and suicide rates are more than 30% higher in middle-aged and older adults than in younger adults (Centers for Disease Control and Prevention, 2012). Identification of observable and modifiable risk factors of suicidal behavior in middle-aged and older adults is critical for suicide prevention efforts.
Depression is the most prevalent psychiatric condition in middle-aged and older adults who die by suicide. On the other hand, only 2–15% of patients with major depressive disorder engage in suicidal behavior (attempted suicide or death by suicide) during their lifetime (Bostwick and Pankratz, 2000). Thus, depression alone cannot explain the emergence of suicidal behavior. This presents a challenge for clinicians who need to assess suicide risk in patients with depression. To improve specificity, additional clinical markers are needed.
Insomnia, characterized by difficulty initiating or reinitiating sleep, is a readily identifiable and potentially modifiable condition associated with suicide (Bernert et al., 2014; Turvey et al., 2002) and suicide attempts (Li et al., 2010). Insomnia may confer a particularly high risk for suicidal behavior in individuals with depression (Bernert et al., 2014; Fawcett et al., 1990; McGirr et al., 2007). A better understanding of the insomnia-suicide relationship may be achieved by investigating insomnia differentially at the emergent (i.e., suicidal ideation and planning) and implementation (i.e., suicide attempt) stages of the suicidal process (Pigeon et al., 2012; Wojnar et al., 2009).
The question of whether insomnia is associated with suicidal behavior or more generally with suicidal ideation has not been answered conclusively. While insomnia has been linked to both suicide ideation and attempts (reviewed in Pigeon et al., 2012), previous studies have not consistently distinguished between the two. For example, when both behavior and ideation are assessed, 15–56% of participants in studies of insomnia and suicidal ideation may have a suicide attempt history (Bernert et al., 2005; McCall et al., 2013). Thus, correlations between suicidal ideation and insomnia may be driven by the direct association of suicidal ideation with suicidal behavior. Further, since suicidal ideation is much more common than suicidal behavior, selective markers of the latter have more utility in suicide prevention. Thus, the aim of the present study was to test for an association between insomnia and suicidal behavior above and beyond the association between insomnia and suicidal ideation.
Insomnia symptoms confer risk for suicidal behavior even when adjusting for depression (Malik et al., 2014), while insomnia’s association with suicidal ideation appears to be better explained by the presence of depression (Bernert et al., 2005; Nadorff et al., 2013; Richardson et al., 2014). Accordingly, we hypothesized that depressed adults with a history of a suicide attempt will have greater insomnia severity than either depressed adults with suicidal ideation and no attempt history, or depressed adults with neither suicidal ideation nor attempt history.
Methods
This paper reports data from an ongoing case-control study of cognitive mechanisms of late-life suicide. Methods for the parent project have been detailed previously (Szanto et al., 2014). Briefly, participants were recruited from the University of Pittsburgh Medical Center within two weeks of psychiatric inpatient admission or at the start of outpatient psychiatric treatment. The Clinical Interview for DSM-IV Axis I Disorders–Patient Edition (SCID-I/P) was used to confirm the presence of lifetime unipolar depression. Due to the rarity of suicidal behavior, a case-control design was used. Three groups of participants, all over age 40 with unipolar depression were recruited. The suicide attempt group was the group of interest and included individuals who had current suicidal ideation and a history of suicide attempt (n = 72). The suicidal ideation group included individuals with a specific, current suicide plan, but no history of acting on this plan by attempting suicide (n = 28). The non-suicidal group consisted of individuals with no lifetime history of suicide attempt or suicidal ideation (n = 35). The suicidal ideation and depressed non-suicidal groups were control groups. The total sample size was adequate to identify medium to large effect size group differences in insomnia severity with 80% power (G*Power 3). Suicide attempt was determined by consensus of the research team and defined as a history of a self-injurious act with intent to die. Current and lifetime history of suicidal behavior and ideation were assessed by clinical interview, medical record review, family reports, and questionnaires including the Suicide Intent Scale (Beck et al., 1974), the Scale for Suicidal Ideation (past week)(Beck et al., 1979), and the suicidality item on Hamilton Rating Scale for Depression (HAM-D; Hamilton, 1980). All cases were reviewed by a study psychiatrist (A.Y.D. or K.S.). Daily use and dose of benzodiazepines were determined from medical record review, pharmacy records, and self-report. The Mini-Mental State Examination, the Cumulative Illness Rating Scale for Geriatrics (CIRS-G), a measure of physical illness burden (Miller et al., 1992), the Inventory of Interpersonal Problems (IIP), a self-report measure of interpersonal difficulties (Horowitz et al., 1988), and the Executive Interview (EXIT), a 25-item screening measure of executive dysfunction (Royall et al., 1992) were also administered.
Exclusion criteria for this study were MMSE <24, severe psychiatric disorder other than depression (e.g., major depressive disorder with psychotic features, bipolar disorder, schizophrenia, schizoaffective disorder), electroconvulsive therapy in the previous 6 months, and neurological disorders (i.e., stroke, epilepsy, brain tumor, or brain injury). We excluded individuals whose suicidal intent was unclear (e.g., unintentional drug overdose) or where hospital records contradicted self-reported account of suicidal behavior. Individuals with suicidal ideation but no specific plan were also excluded from this study. Participants were not excluded for psychotropic medication use.
Sample characteristics are presented in Table 1. In brief, our sample was 47% female, and included middle-aged and older adults (M = 66 years old, 44–87) who were well-educated (M = 14 years of education). Groups were well-matched for age, gender, race, and education. All procedures were conducted in accordance with IRB approval.
Table 1.
Sample characteristics.
| Non-suicidal (n=35) |
Suicidal ideation (n=28) |
Suicidal attempt (n=72) |
χ2/F | df | p-Value | Post Hoc | |
|---|---|---|---|---|---|---|---|
| Age, yearsa | 68 | 64 | 63 | 4.3 | 2 | .11 | |
| Sex, % female | 46 | 43 | 50 | 0.5 | 2 | .79 | |
| Race, % Caucasian | 89 | 89 | 85 | 0.5 | 2 | .77 | |
| Education, yearsa | 13 | 15 | 13 | 5.1 | 2 | .08 | |
| SCID-I/P diagnosisb | |||||||
| GAD past month [lifetime] | 15[15] | 13[13] | 26[28] | 0.9 | 2 | .64 | |
| PTSD past month [lifetime] | 0[0] | 2[2] | 7[10] | 3.6 | 2 | .17 | |
| Panic past month [lifetime] | 6[6] | 3[8] | 10[20] | 1.6 | 2 | .46 | |
| Substance abuse [lifetime] | 1[2] | 1[4] | 3[5] | 0.1 | 2 | .94 | |
| Alcohol abuse [lifetime] | 1[3] | 1[3] | 4[11] | 0.4 | 2 | .79 | |
| Hamilton Rating Scale for Depressionc | 14.2(4.01) | 17(4.65) | 19(5.23) | F=13 | 2,132 | <.001*** | NS<SA |
| Inventory of Interpersonal Problemsa | 12 | 19 | 15 | 4.6 | 2 | .10 | |
| Duration of current depressive episode, days | 367.5(649.9) | 181.8(267.7) | 141.3(400.1) | 2.73 | 2,122 | .07 | |
| Adequacy of treatmenta | 4 | 4 | 4 | 2.5 | 2 | .29 | |
| Benzodiazepine use | 15 | 8 | 27 | 1.4 | 2 | .50 | |
| Physical illness burden (CIRS-G)a | 12 | 9 | 8 | 11 | 2 | .005** | NS<SI, SA |
| Mini-Mental Status Exama | 29 | 29 | 28 | 12 | 2 | .002** | NS,SI>SA |
| Executive Interviewa | 7 | 8 | 7 | 0.8 | 2 | .68 | |
Note:
p <.01,
p <.001.
Non-normally distributed variables values are reported as median.
Categorical variables are reported as a frequency or as a percentile.
Normally distributed variables are reported as mean (standard deviation).
Statistics for past month are reported, lifetime SCID diagnoses were not significantly different across groups.
GAD = generalized anxiety disorder.
PTSD = post-traumatic stress disorder.
Total Hamilton score did not include suicide item.
CIRS-G = Cumulative Illness Rating Scale for Geriatrics.
Analyses
Previously identified factors of the HAM-D (Fleck et al., 2004) were computed by summing each item within respective factors: depressed mood (depressed mood, feelings of guilt, and work and activities), anxiety (agitation, psychic anxiety, somatic anxiety, and hypochondriasis symptoms), and insomnia (onset, maintenance, and early morning symptoms). The insomnia items from the HAM-D have been linked to suicidality (Agargun et al., 2007). The reliability (Fleck et al., 2004) and clinical significance (Perico et al., 2005) of the insomnia factor have been demonstrated in previous work. Assumptions of normality (Kolmogorov-Smirnov >.05) were assessed for all continuous variables included in this study. Analysis of variance (ANOVA) using post-hoc t-tests, Kruskal Wallis tests using post hoc Mann Whitney tests, and chi-square tests were used to compare groups across demographic variables and health features (see Table 1). Bonferroni correction was applied to post hoc comparisons to control for family wise error.
A series of analyses of covariance (ANCOVA) was conducted to test whether groups differed in the severity of insomnia measured by the HAM-D. Variables that were different across the groups or that might be associated with insomnia based on the literature were included as covariates: age, gender, education, depressed mood and anxiety factors from the HAM-D, MMSE total score, alcohol dependence, and physical illness burden. Tukey HSD was used to test group differences post hoc. Variables that did not explain significant unique variance were removed to produce the final model. A subset of participants (n = 12) had a history of post-traumatic stress disorder (PTSD), a known risk factor for suicidality. We conducted a sensitivity analysis in which the final ANCOVA model did not include these patients to ensure that our findings were not entirely explained by PTSD.
Exploratory analyses were also conducted. Spearman correlations were used to determine whether insomnia severity was associated with suicidal ideation severity, recency of suicide attempt, number of suicide attempts, and lethality of suicide attempt. Previous studies have linked insomnia to cognitive difficulties, interpersonal problems, and benzodiazepine use (Roth and Ancoli-Israel, 1999). To explore whether an association between insomnia and suicidality might be explained by these variables, we also conducted exploratory correlation analyses in the total sample and within the suicide attempt group. Spearman correlations were used to investigate whether insomnia severity correlated with EXIT total score or IIP total score and an ANOVA was used to investigate if individuals who used benzodiazepines (n = 50) differed from those who did not use benzodiazepines (n = 85) in regards to insomnia severity. All analyses were conducted using IBM SPSS 22 (IBM 2014).
Results
Table 1 reports group characteristics. Groups were similar in terms of co-morbidities and exposure to antidepressant pharmacotherapy. They differed in current depressive severity, mental status, and physical health burden. Specifically, the non-suicidal group had higher CIRS-G scores than both suicidal groups and lower HAM-D total scores than the suicide attempt group. The groups differed significantly in MMSE score such that the suicide attempt group scored 1 point lower on average than the suicidal ideation and non-suicidal depressed groups.
Table 2 and Figure 1 report the group differences in insomnia severity. Insomnia severity scores ranged from 0–6. A basic ANOVA revealed that groups differed significantly in severity of insomnia, suicide attempt group (M = 3.49, SD = 1.82), suicidal ideation group (M = 2.32, SD = 1.72), non-suicidal depressed group (M = 2.34, SD = 1.71), F(2,132) = 7.12, p = .001, η2 = .097. Post hoc analyses with Bonferroni correction demonstrated that the suicide attempt group had significantly more severe insomnia than the suicidal ideation (p = .010) and non-suicidal depressed (p = .006) groups. The suicidal ideation group did not have more severe insomnia than the non-suicidal group. Covariates that were considered possible confounding variables were added in two steps. Step 1 included demographic variables: age, gender, and education. Step 2 included mental and physical health variables: depressed mood and anxiety factors from the HAM-D, MMSE, CIRS-G total score, and alcohol dependence in the past month. Covariates that were not significantly correlated with insomnia severity and did not contribute to the final model were removed for each step. No covariate was significantly associated with insomnia in any model. Nevertheless, because alcohol dependence in the past month and CIRS-G contributed to the overall model, they were retained in the final model. In all iterations of the model, group differences remained significant and post hoc Tukey HSD analyses confirmed the suicide attempt group had significantly more severe insomnia than the suicide ideation and non-suicidal groups (p < .05 for all). Results were robust to the exclusion of participants with lifetime history of PTSD, p < .05.
Table 2.
Steps for building final ANCOVA model for insomnia severity.
| F | df | p | η2 | Δη2 | |
|---|---|---|---|---|---|
| Basic ANOVA | 7.1 | 2,132 | .001*** | .10 | |
| Model 1-demographic variables added | .01 | ||||
| Age | 0.2 | 1,129 | .69 | .001 | |
| Gender | 1.0 | 1,129 | .32 | .008 | |
| Education | 0.1 | 1,129 | .81 | <.001 | |
| Group | 6.7 | 2,129 | .002** | .09 | |
| Model 2-health variables added | .03 | ||||
| Mini-Mental Status Exam | 0.1 | 1,126 | .77 | .001 | |
| Depressed mood (HAM-D factor) | 0.0 | 1,126 | .97 | <.001 | |
| Anxiety (HAM-D factor) | 0.5 | 1,126 | .47 | .004 | |
| Alcohol abuse in the past month (SCID-I/P) | 1.8 | 1,126 | .19 | .01 | |
| Physical illness burden (CIRS-G) | 2.3 | 1,126 | .13 | .02 | |
| Group | 5.1 | 2,126 | .008** | .07 | |
| Final model | .03 | ||||
| Physical illness burden (CIRS-G) | 2.4 | 1,129 | .12 | .02 | |
| Alcohol abuse in the past month (SCID-I/P) | 1.9 | 1,129 | .18 | .01 | |
| Group | 7.3 | 2,129 | .001** | .10 |
Note:
p <.05,
p <.01,
p <.001.
Δη2 = indicates difference compared to the basic ANOVA model, HAM-D=Hamilton Rating Score for Depression, SCID-I/P = The Clinical Interview for DSM-IV Axis I Disorders–Patient Edition, Version 2. CIRS-G = Cumulative Illness Rating Scale for Geriatrics.
Figure 1.
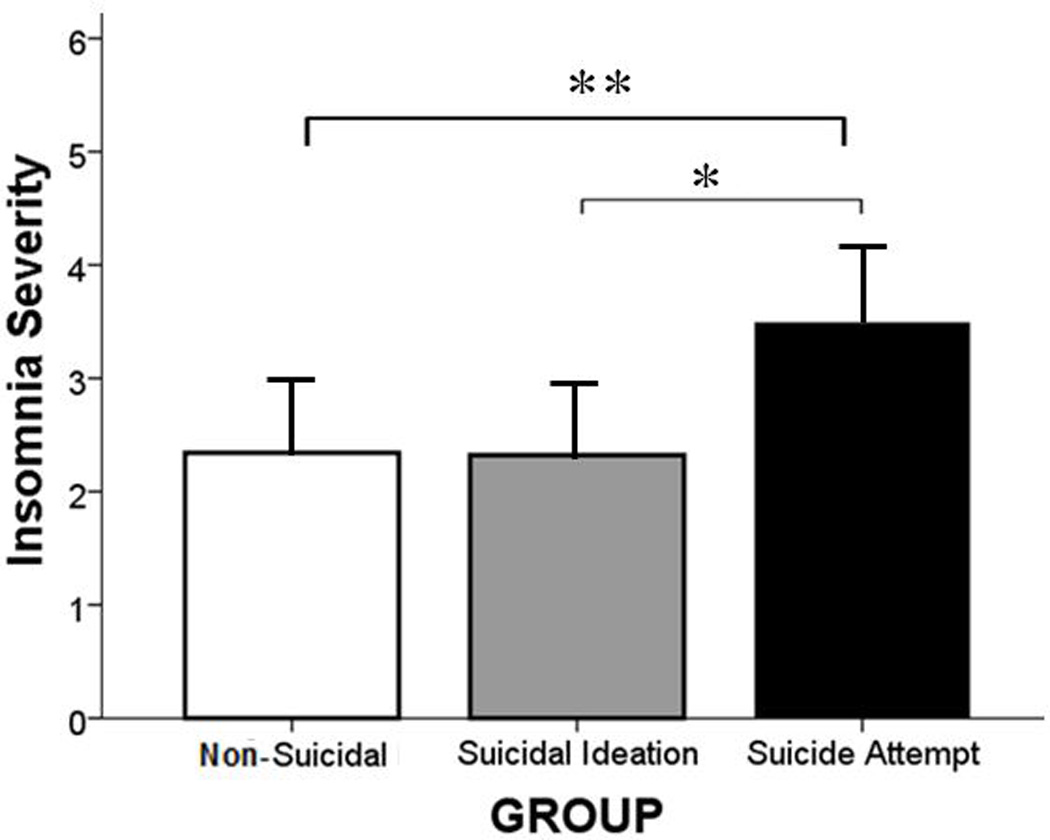
Among our sample individuals with a history of major depression, the suicide attempt group had significantly more severe symptoms of insomnia than the suicidal ideation or non- suicidal groups, *p < .05, **p < .01, respectively.
Exploratory analyses within the suicide attempt group revealed no significant correlations between insomnia and suicidal ideation severity, rs(72) = 0.19, p = 0.12, recency of suicide attempt, rs(72) = 0.03, p = 0.82, number of suicide attempts, rs(72) < −0.01, p = 0.98, lethality of suicide attempt, rs(72) = 0.09, p = 0.47, interpersonal difficulties, rs(135) < 0.01, p = 0.99, or executive functioning, rs(101) = 0.04, p = 0.71. Exploratory analysis in the total sample found no significant correlations between insomnia severity and interpersonal difficulties or executive functioning, (p > .10 for all). Exploratory ANOVAs found no significant differences in insomnia severity based on benzodiazepine use (yes vs. no) in the suicide attempt group, F(1,70) = 1.12, p = 0.29, or the total sample, F(1,133) = 0.53, p = 0.47.
Discussion
Our results support the hypothesis that insomnia severity is associated with suicidal behavior in individuals with depression. The observed associations remained after accounting for possible confounders (demographics, cognitive ability, alcohol dependence, severity of depressed mood, anxiety, and physical health burden). Individuals with a suicide attempt had on average one more symptom of insomnia (29% greater insomnia severity) than the non-attempt groups. Thus, the suicide attempt group tended to have more severe insomnia symptoms of a particular type (onset, maintenance, or early morning awakening) and on average had at least two different types of symptoms of insomnia. This study extends the results of a meta-analysis showing that symptoms of insomnia confer increased risk for suicidal behavior in patients with depression (Malik et al., 2014).
Results are consistent with a previous study that found that individuals with multiple sleep complaints have a particularly high risk for suicidal behavior (Wojnar et al., 2009). Also consistent with a previous study (Sjöström et al., 2007), we did not find a correlation between insomnia severity and other dimensions of suicidality (ideation, recency, frequency, or lethality) within the suicide attempt group. This study does not address whether insomnia is associcated with suicidal ideation severity in depressed individuals without a history of attempt. However, the majority of studies in the literature have failed to find an association between insomnia symptoms and suicidal ideation when controlling for depression (Bernert et al., 2005; Nadorff et al., 2011; 2013; Richardson et al., 2014).
Individuals with current suicidal ideation with a specific plan did not have more severe insomnia symptoms than non-suicidal individuals. This contradicts the findings of Wojnar and colleagues (Wojnar et al., 2009) who found that insomnia symptom severity was associated with suicide ideation or planning. In that study, however, the retrospective assessment window was limited to 12 months, lifetime history of suicide attempt was not assessed, and the temporal association between variables could not be determined. The added strength of the current study is its case-control design that carefully assessed lifetime history of suicidal behavior and allowed us to study a sample of individuals with suicidal ideation with a specific plan but no lifetime history of suicidal behavior. Our results suggest that insomnia severity may confer risk for suicidal behavior through mechanisms other than suicide planning.
Numerous hypotheses have been put forth to explain the association between insomnia and suicidal behavior (McCall and Black, 2013), including insomnia’s potential relationships with depression severity, cognitive deficits, or medications. Our results suggest that depression and anxiety severity do not explain the relationship between insomnia and suicidal behavior. Because the anxiety factor of the HAM-D included a measure of agitation, results of this study are not readily explained by general agitation associated with suicidal behavior. In addition, we found no evidence that interpersonal distress, lower-level executive functioning, distress associated psychical health, nor benzodiazepine use might explain the association between insomnia and suicidal behavior. Thus, there is a need to explore other behavioral and biological mechanisms through which insomnia may increase the risk for suicide including dysfunction in cognitive domains (i.e., autobiographical memory, problem solving, and working memory)(reviewed in Fortier-Brochu et a., 2012) and neural circuitries, including brain regions (i.e., prefrontal cortex, cingulate cortex, precuneus, and medial temporal cortex)(reviewed in Levenson et al., 2015) associated with insomnia.
This study is limited in that insomnia was only measured by the insomnia factor of the HAM-D; however, the items for this factor have been shown to correlate with suicidality in previous studies (Agargun et al., 2007). The results of this study need to be replicated in studies that use diagnostic criteria for insomnia and assess additional dimensions of insomnia. For example, chronicity of insomnia was not assessed by the HAM-D and is an important dimension of insomnia that may be related to suicidality. Although its cross-sectional design is another limitation of the present study, the relatively high prevalence of insomnia and rarity of suicidal behavior make it difficult to assess otherwise. Thus, these results cannot determine temporal or causal relationship between suicidal behavior and insomnia.
Assessing insomnia symptoms, as well as other markers of depression may improve risk assessment for suicidal behavior (Li et al., 2010; McGirr et al., 2007). Our findings support the notion that patients with depression who report having suicidal ideation and insomnia symptoms may have a higher risk for suicidal behavior than depressed individuals who do not have insomnia. Insomnia may also be a treatment target for reducing suicide risk. One study showed that insomnia treatment reduces suicidal ideation (Trockel et al., 2015). Thus, we recommend that clinicians who work with depressed individuals routinely assess and treat sleep disturbances. However, we acknowledge that this recommendation requires further assessment in prospective studies. Management of insomnia complaints in later-life has been reviewed in detail previously (McCrae et al., 2009). A referral for cognitive behavioral therapy for insomnia is the recommended front-line treatment.
Acknowledgments
This work was supported by the National Institute of Mental Health (R01 MH085651to K.S, K23 MH086620 and R01 MH100095 to A.Y.D); National Institutes of Health Heart Blood and Lung Institute (HL082610 to D.J.B., P60 MD000207, P30 MH090333, UL1RR024153, and UL1TR000005 to C.F.R.); and the UPMC Endowment in Geriatric Psychiatry (to C.F.R). We thank Joshua Feldmiller for data management.
Footnotes
This article has been accepted for publication and will appear in a revised form, subsequent to peer review and/or editorial input by Cambridge University Press, in International Psychogeriatrics published by Cambridge University Press. Copyright 2015, International Psychogeriatric Association.
Conflict of interest
None.
Description of authors’ roles
D. Kay conceptualized the study hypotheses, analyzed the data, and wrote the article. A. Dombrovski, D. Buysse, and Charles F. Reynolds III contributed to the conceptualization of the paper, statistical design, and writing the article. A. Begley assisted with statistical analyses. K. Szanto carried out the study, supervised data collection and contributed to the conceptualization, statistical design, and writing of the paper.
References
- Agargun MY, et al. Nightmares, suicide attempts, and melancholic features in patients with unipolar major depression. Journal of Affective Disorders. 2007;98:267–270. doi: 10.1016/j.jad.2006.08.005. [DOI] [PubMed] [Google Scholar]
- Beck AT, Kovacs M, Weissman A. Assessment of suicidal intention: the Scale for Suicide Ideation. Journal of Consulting and Clinical Psychology. 1979;47:343–352. doi: 10.1037//0022-006x.47.2.343. [DOI] [PubMed] [Google Scholar]
- Beck RW, Morris JB, Beck AT. Cross-validation of the Suicidal Intent Scale. Psychological Reports. 1974;34:445–446. doi: 10.2466/pr0.1974.34.2.445. [DOI] [PubMed] [Google Scholar]
- Bernert RA, Joiner TE, Jr, Cukrowicz KC, Schmidt NB, Krakow B. Suicidality and sleep disturbances. Sleep. 2005;28:1135–1141. doi: 10.1093/sleep/28.9.1135. [DOI] [PubMed] [Google Scholar]
- Bernert RA, Turvey CL, Conwell Y, Joiner TE., Jr Association of poor subjective sleep quality with risk for death by suicide during a 10-year period: a longitudinal, population-based study of late life. JAMA Psychiatry. 2014;71:1129–1137. doi: 10.1001/jamapsychiatry.2014.1126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bostwick JM, Pankratz VS. Affective disorders and suicide risk: a reexamination. American Journal of Psychiatry. 2000;157:1925–1932. doi: 10.1176/appi.ajp.157.12.1925. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Suicide: facts at a glance. 2012 Retreived 2015 Aug 12 from www.cdc.gov/ViolencePrevention/pdf/Suicide_DataSheet-a.pdf.html.
- Fawcett J, et al. Time-related predictors of suicide in major affective disorder. American Journal of Psychiatry. 1990;147:1189–1194. doi: 10.1176/ajp.147.9.1189. [DOI] [PubMed] [Google Scholar]
- Fleck MP, et al. Depression in France and Brazil: factorial structure of the 17-item Hamilton Depression Rating Scale in inpatients. The Journal of Nervous and Mental Disease. 2004;192:103–110. doi: 10.1097/01.nmd.0000110281.35970.33. [DOI] [PubMed] [Google Scholar]
- Fortier-Brochu E, Beaulieu-Bonneau S, Ivers H, Morin CM. Insomnia and daytime cognitive performance: a meta-analysis. Sleep Medicine Reviews. 2012;16:83–94. doi: 10.1016/j.smrv.2011.03.008. [DOI] [PubMed] [Google Scholar]
- Hamilton M. Rating depressive patients. Journal of Clinical Psychiatry. 1980;41:21–24. [PubMed] [Google Scholar]
- Horowitz LM, Rosenberg SE, Baer BA, Ureño G, Villaseñor VS. Inventory of interpersonal problems: psychometric properties and clinical applications. Journal of Consulting and Clinical Psychology. 1988;56:885–892. doi: 10.1037//0022-006x.56.6.885. [DOI] [PubMed] [Google Scholar]
- Levenson JC, Kay DB, Buysse DJ. The pathophysiology of insomnia. Chest. 2015;147:1179–1192. doi: 10.1378/chest.14-1617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li SX, Lam SP, Yu MWM, Zhang JH, Wing YK. Nocturnal sleep disturbances as a predictor of suicide attempts among psychiatric outpatients: a clinical, epidemiologic, prospective study. Journal of Clinical Psychiatry. 2010;71:1440–1446. doi: 10.4088/JCP.09m05661gry. [DOI] [PubMed] [Google Scholar]
- Malik S, et al. The association between sleep disturbances and suicidal behaviors in patients with psychiatric diagnoses: a systematic review and meta-analysis. Systematic Reviews. 2014;3:18. doi: 10.1186/2046-4053-3-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCall WV, et al. Nightmares and dysfunctional beliefs about sleep mediate the effect of insomnia symptoms on suicidal ideation. Journal of Clinical Sleep Medicine. 2013;9:135–140. doi: 10.5664/jcsm.2408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCall WV, Black CG. The link between suicide and insomnia: theoretical mechanisms. Current Psychiatry Reports. 2013;15:389. doi: 10.1007/s11920-013-0389-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCrae CS, Dzierzewski JM, Kay D. Treatment of late-life insomnia. Sleep Medicine Clinics. 2009;4:593–604. doi: 10.1016/j.jsmc.2009.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGirr A, et al. An examination of DSM-IV depressive symptoms and risk for suicide completion in major depressive disorder: a psychological autopsy study. Journal of Affective Disorders. 2007;97:203–209. doi: 10.1016/j.jad.2006.06.016. [DOI] [PubMed] [Google Scholar]
- Miller MD, et al. Rating chronic medical illness burden in geropsychiatric practice and research: application of the Cumulative Illness Rating Scale. Psychiatry Research. 1992;41:237–248. doi: 10.1016/0165-1781(92)90005-n. [DOI] [PubMed] [Google Scholar]
- Nadorff MR, Nazem S, Fiske A. Insomnia symptoms, nightmares, and suicidal ideation in a college student sample. Sleep. 2011;34:93–98. doi: 10.1093/sleep/34.1.93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nadorff MR, Fiske A, Sperry JA, Petts R, Gregg JJ. Insomnia symptoms, nightmares, and suicidal ideation in older adults. Journals of Gerontology, Series B: Psychological Sciences and Social Sciences. 2013;68:145–152. doi: 10.1093/geronb/gbs061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Périco CA-M, et al. Relationship between regional cerebral blood flow and separate symptom clusters of major depression: a single photon emission computed tomography study using statistical parametric mapping. Neuroscience Letters. 2005;384:265–270. doi: 10.1016/j.neulet.2005.04.088. [DOI] [PubMed] [Google Scholar]
- Pigeon WR, Pinquart M, Conner K. Meta-analysis of sleep disturbance and suicidal thoughts and behaviors. Journal of Clinical Psychiatry. 2012;73:e1160–e1167. doi: 10.4088/JCP.11r07586. [DOI] [PubMed] [Google Scholar]
- Richardson JD, Cyr KS, Nelson C, Elhai JD, Sareen J. Sleep disturbances and suicidal ideation in a sample of treatment-seeking Canadian Forces members and veterans. Psychiatry Research. 2014;218:118–123. doi: 10.1016/j.psychres.2014.04.008. [DOI] [PubMed] [Google Scholar]
- Roth T, Ancoli-Israel S. Daytime consequences and correlates of insomnia in the United States: Results of the 1991 National Sleep Foundation Survey II. Sleep. 1999;22:S354–S358. [PubMed] [Google Scholar]
- Royall DR, Mahurin RK, Gray KF. Bedside assessment of executive cognitive impairment: the Executive Interview. Journal of the American Geriatrics Society. 1992;40:1221–1226. doi: 10.1111/j.1532-5415.1992.tb03646.x. [DOI] [PubMed] [Google Scholar]
- Sjöström N, Waern M, Hetta J. Nightmares and sleep disturbances in relation to suicidality in suicide attempters. Sleep. 2007;30:91–95. doi: 10.1093/sleep/30.1.91. [DOI] [PubMed] [Google Scholar]
- Szanto K, et al. The cost of social punishment and high-lethality suicide attempts in the second half of fife. Psychology and Aging. 2014;29:84–94. doi: 10.1037/a0035339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trockel M, Karlin BE, Taylor CB, Brown GK, Manber R. Effects of cognitive behavioral therapy for insomnia on suicidal ideation in veterans. Sleep. 2015;38:259–265. doi: 10.5665/sleep.4410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turvey CL, et al. Risk factors for late-life suicide: a prospective, community-based study. American Journal of Geriatric Psychiatry. 2002;10:398–406. [PubMed] [Google Scholar]
- Wojnar M, et al. Sleep problems and suicidality in the National Comorbidity Survey Replication. Journal of Psychiatric Research. 2009;43:526–531. doi: 10.1016/j.jpsychires.2008.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]


