Abstract
Deteriorating sleep quality and increased fatigue are common complaints of old age, and poor sleep is associated with decreased quality of life and increased mortality rates. To date, little attention has been given to the potential effects of physical activity on sleep quality and fatigue in aging. The purpose of this study was to examine the relationships between activity, sleep and fatigue across the adult lifespan. Sixty community-dwelling adults were studied; 22 younger (21–29 years), 16 middle-aged (36–64 years), and 22 older (65–81 years). Physical activity was measured by accelerometer. Sleep quality was assessed using the Pittsburg Sleep Quality Index. Self-reported fatigue was evaluated with the Patient-Reported Outcomes Measurement Information System (PROMIS). Regression analysis revealed a positive relationship between activity and sleep quality in the older (r2=0.18, p=0.05), but not the younger (r2=0.041, p=0.35) or middle-aged (r2=0.001, p=0.93) groups. This association was mainly established by the relationship between moderate-vigorous activity and sleep quality (r2=0.37, p=0.003) in older adults. No association was observed between physical activity and self-reported fatigue in any of the groups (r2≤0.14, p≥0.15). However, an inverse relationship was found between sleep quality and fatigue in the older (r2=0.29, p=0.05), but not the younger or middle-aged (r2≤0.13, p≥0.10) groups. These results support the hypothesis that physical activity may be associated with sleep quality in older adults, and suggest that improved sleep may mitigate self-reported fatigue in older adults in a manner that is independent of activity.
Keywords: aging, fatigability, physical function, accelerometry
INTRODUCTION
An estimated fifty percent of the population over the age of 65 years reports poor sleep quality or chronic fatigue, both of which are associated with decreased quality of life and increased rate of mortality in this population (Eldadah, 2010). According to a National Institute on Aging’s sample of 9,000 individuals >65 years, 42% reported difficulty both falling asleep and maintaining sleep (Foley et al., 1995). Further, the amount of time spent fully immersed in sleep each night has been shown to be approximately one hour longer in young adults compared with those over the age of 65 (Buysse et al., 1991). Older individuals often report greater time spent in bed but less time asleep, contributing to reduced sleep quality (Buysse et al., 1991).
In clinical populations, lower levels of physical activity (Valentine et al., 2009) and lower sleep quality (Cella et al., 2010, Valentine et al., 2009) have both been shown to be related to general feelings of fatigue. Although such self-reported fatigue is a common complaint in older individuals (Avlund, 2010), its relationship with physical activity has not been widely studied in this population. Structured physical activity interventions have been shown to improve sleep quality in older adults (King et al., 2008), however, little attention has been given to quantitative assessments of habitual physical activity and its relationship to sleep quality and self-reported fatigue. Further, to date, studies of sleep quality and fatigue in middle-aged adults are lacking and therefore little is known about potential progressive changes that occur across the lifespan.
Understanding the relationships among physical activity, quality of sleep, and self-reported fatigue across the lifespan will contribute to the development of effective strategies for reducing the use and risks of prescribed sleep medication, and improving quality of life into the later years. Therefore, the purpose of this study was to begin this evaluation by quantifying the relationships of physical activity with sleep quality and self-reported fatigue across the adult lifespan. We hypothesized that higher levels of habitual physical activity would be associated with greater sleep quality and lower self-reported fatigue.
METHODS
Participants
Sixty community-dwelling adults participated in the study, and were separated by age into three groups: young (21–29 years; n=22, 11 women), middle-aged (36–64 years; n=16, 10 women) and older (65–81 years; n=22, 11 women). The study was reviewed and approved by the University of Massachusetts Amherst Institutional Review Board and all participants provided written informed consent prior to enrollment. All participants reported good general health and were free of life-threatening illness, debilitating chronic disease, or diagnosed sleep disorders. All participants were relatively sedentary, reporting less than 30 minutes of structured physical activity per week, and reported sleeping an average of at least five hours per night, both of which were confirmed with activity logs.
Procedures
Participants visited the Muscle Physiology Laboratory at the University of Massachusetts Amherst on one occasion. During this visit, participants completed a detailed medical history form and questionnaires about sleep quality and general feelings of fatigue (described below). At the end of the visit, participants were provided with a physical activity monitor (Actigraph GT1M, Pensacola, FL) and a physical activity log, and were instructed in their use.
Physical Function Measures
To characterize our study cohort, physical function assessed by 400m walk, chair rises and stair ascent times. All participants completed the 400m walk using the same 10 laps of a 40m hallway course. Participants were asked to walk a fast but maintainable pace for the duration of the 400m. For timed chair rises, participants began seated in an armless chair with the arms folded across the chest. They were instructed to stand up and sit back down as fast as possible 10 times. Stair ascent times were measured on an 8-step staircase. Participants were instructed to ascend the stairs as fast as possible, without using the railings, while maintaining at least one foot in contact with the floor at all times and not skipping steps. For chair stands and stair climbs, 2 trials were performed and the shortest time was recorded for each measure. All of these measures are predictive of future functional limitations or mortality in older adults (Vestergaard et al., 2009, Tiedemann et al., 2008).
Physical Activity
Physical activity was measured by uni-axial accelerometry (ActiGraph GT1M, Pensacola, FL), as previously (Freedson et al., 1998) and according to best practice guidelines (Ward et al., 2005). The accelerometers measure vertical accelerations as activity counts that are averaged into 1-minute epochs. Accelerometers were distributed at the end of the laboratory visit and participants were asked to wear them around the waist during all waking hours for 10 consecutive days. Participants were instructed to carry out regular daily activities for an accurate assessment of habitual physical activity. In addition, participants were asked to complete an activity log for the corresponding 10 days, where activity, inactive times, sleep time, unusual activities and accelerometer wear time were recorded and used to confirm accelerometer data. A minimum of 7 days of representative physical activity data, where the participant wore the accelerometer for the full day and noted no unusual activity (e.g. participant was sick and stayed in bed most of the day) in the log, was required for a participant’s data to be included in the analysis.
Data from the accelerometers were analyzed using a custom-written MATLAB program to determine total physical activity counts and total activity minutes per day, which were averaged across days. Activity was also represented by the number of minutes spent in sedentary (1–99 counts), light (100 to 1951 counts), and moderate to vigorous (MVPA, ≥1952 counts) activity (Freedson et al., 1998). The same cut-points were used for all age groups. Although these cut-points were originally validated in young adults, they are currently the most widely-used cut-points for older adults (Gorman et al., 2014). As no consensus exists on validated age-specific cut-points, those employed here are suggested to be optimal for individuals aged 65 and over (Gorman et al., 2014).
Sleep Quality
The Pittsburg Sleep Quality Index (PSQI (Buysse et al., 1989)) was used to measure sleep quality. This 24-item questionnaire assesses habitual sleep over the past 30 days. Nineteen of the questions are self-rated, with 15 multiple-choice and 4 write-ins, while 5 of the questions refer to the opinion of a “sleeping partner.” As assessed by the PSQI, sleep quality is broken into 7 components: subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleep medications, and daytime dysfunction. Component scores, ranging from 0 to 3, were computed and summed to provide a global PSQI score out of 21, with lower scores indicating better overall quality of sleep (Buysse et al., 1991, Buysse et al., 1989).
Self-Reported Fatigue
Measures of self-reported fatigue were obtained from all young (n=22) and middle-aged (n=16) participants and from 13 of the 22 participants in the older age group. Nine of the older participants were enrolled in the study prior to the introduction of this measure. Self-reported fatigue was measured using the Patient-Reported Outcomes Measurement Information System (PROMIS; (Cella et al., 2010)) Short Form Fatigue Questionnaire. This form requires participants to answer 7 questions about how they have been feeling in the past 7 days. Participants rate questions on a 5-point scale from “never” to “always.” Scores from the 7 questions on the PROMIS short form were summed to provide a global PROMIS score, thus the total score ranges from 7 to 35, with lower scores indicating less fatigue.
Statistical Analysis
Two-factor (age group, sex) ANOVAs revealed no main effects of sex (p≥0.10) or age-by-sex interactions (p≥0.33) for any of the primary outcome variables. Therefore, data from men and women were combined and one-factor (age group) analysis of variance (ANOVA) was used to explore differences in physical activity, sleep quality, physical function, and self-reported fatigue. Linear regression analyses were performed within each age group to examine the relationship of physical activity with each of sleep quality and self-reported fatigue. Data are presented as mean±SD and significance was set at p≤0.05.
RESULTS
Group Characteristics
A summary of group characteristics is reported in Table 1. Height and body mass were similar in young, middle-aged and older groups (p≥0.34). The mean times for each group to complete the 400m walk, 10 chair rises, and 8-stair climbs are also presented in Table 1. The older group took longer to complete each of these timed physical function tasks compared with the middle-aged and younger groups (p≤0.03).
Table 1.
Descriptive Characteristics
| Young (n=22) |
Middle-aged (n=16) |
Older (n=22) |
|
|---|---|---|---|
| Age (years) | 23.0±2.3 | 53.5±9.2a | 73.9±6.1a,b |
| Height (m) | 1.7±0.1 | 1.7±0.1 | 1.7±0.1 |
| Mass (kg) | 65.4±14.1 | 74.8±11.2 | 74.6±12.2 |
| 400 m walk (s) | 280.9±38.0 | 268.3±130.8 | 306.1±51.1a,b |
| 10 chair rises (s) | 15.0±2.8 | 14.6±13.2 | 18.4±6.6a,b |
| Stair ascent (s) | 2.9±0.5 | 2.9±2.4 | 4.0±0.9a,b |
| PSQI (global) | 5.0±2.3 | 4.9±2.4 | 4.1±3.3 |
| PROMIS | 14.3±2.3 | 16.8±3.6a,b | 14.5±3.3 |
Data are presented as mean±SD.
PSQI = Pittsburgh Sleep Quality Index, lower value indicates better sleep quality; PROMIS = Patient-Reported Outcomes Measurement Information System Short Form Fatigue Questionnaire, lower values indicate less fatigue;
indicates different from young group (p≤0.02);
indicates different from older (p≤0.03)
PROMIS questionnaires were completed by 13 of the 22 individuals in the older group.
Physical Activity
The total physical activity counts per day and total activity minutes per day are reported in Table 2. Average daily activity counts were not different across groups (p=0.44; Table 2). However, the middle-aged and older groups had higher total minutes of physical activity per day than the younger group (p≤0.04; Table 2), indicating that the same number of activity counts was accumulated in a shorter amount of time in the young group. Supporting this result is the observation that the time spent in light activity was higher for the middle-aged and older groups than the younger group (p≤0.001), with no group differences in time spent in sedentary or MVPA (p=0.08; Table 2).
Table 2.
Physical Activity Variables
| Young (n=22) |
Middle-aged (n=16) |
Older (n=22) |
|
|---|---|---|---|
| Total (counts·day−1,000) | 207.7±65.2 | 227.6±67.2 | 193.4±109.3 |
| Total (min·day−1) | 362.8±123.4 | 478.0±76.8a | 432.4±87.2a |
| Sedentary (min·day−1) | 169.7±68.0 | 195.1±32.4 | 170.3±37.5 |
| Light (min·day−1) | 149.5±66.6 | 256.7±59.6a | 239.9±69.9a |
| MVPA (min·day−1) | 34.5±16.4 | 26.6±16.0 | 22.1±21.6 |
Data are presented as mean±SD.
MVPA = moderate-to-vigorous physical activity;
indicates different from young (p≤0.04)
Sleep Quality
Mean global scores on the PQSI were not different across age groups (p=0.61; Table 1). Previous research has identified a global score ≥5 as indicative of a significant sleep disturbance (Buysse et al., 1991). Applying this categorization, 56% of the younger participants, 44% of the middle-aged participants, and 45% of the older participants reported poor sleep quality.
Self-Reported Fatigue
Total PROMIS fatigue scores were higher for the middle-aged group than the younger or older participants (p≤0.05; Table 1). These self-reported fatigue ratings were not different between young and older adults (p=0.42).
Regression Analyses
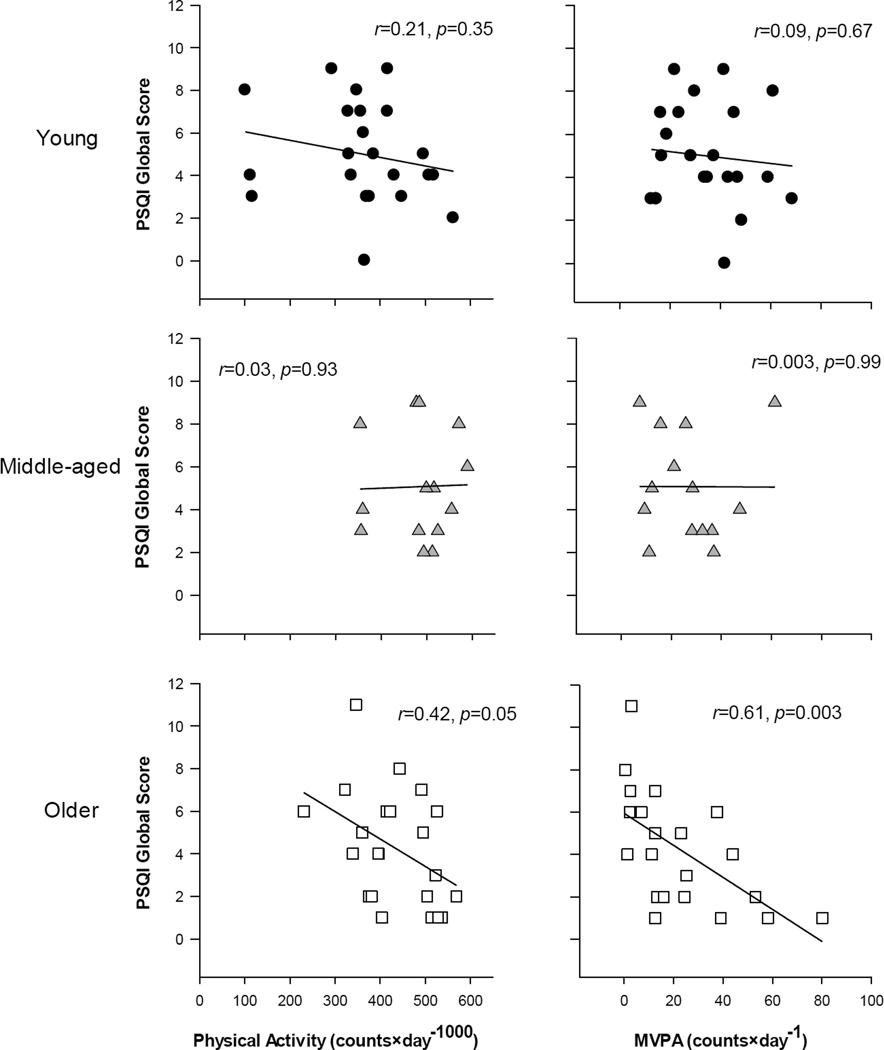
A significant association between total daily physical activity counts and PSQI scores was observed in the older (r2=0.18, p=0.05), but not in the younger (r2=0.04, p=0.35) or middle-aged participants (r2=0.001, p=0.93; Figure 1). A significant association between minutes of MVPA and PSQI score was also observed in the older (r2=0.37, p=0.003), but not in the younger (r2<0.001, p=0.67) or middle-aged participants (r2<0.001, p=0.99; Figure 1). Thus, older adults who averaged more physical activity per day also scored lower on the PSQI, indicating better sleep quality. No relationship was observed for any group between minutes of sedentary or light activity and PSQI scores (r2≤0.14, p≥0.10).
Figure 1.
Relationships between sleep quality and physical activity in young (top), middle-aged (middle) and older (bottom) adults. There was a significant association between the global PSQI score and daily physical activity counts (left column) in older adults only, indicating the more daily activity was associated with better sleep quality. Similarly, PSQI was significantly associated with minutes of moderate-vigorous physical activity (right column) in older adults only. PSQI = Pittsburgh Sleep Quality Index; MVPA = moderate-to-vigorous physical activity
No relationship was observed for any group between physical activity counts and the PROMIS measure of self-reported fatigue (r2≤0.13, p≥0.15). However, a significant association between PSQI and PROMIS scores (r2=0.29, p=0.05) was observed in the older, but not in the younger or middle-aged participants (r2≤0.13, p≥0.1). Thus, older adults who reported better sleep quality also reported less self-reported fatigue. These results support the concept that self-reported fatigue in older adults may be mediated by sleep quality; an effect that is not apparent in young and middle-aged adults.
DISCUSSION
This study evaluated the relationships between sleep quality, self-reported fatigue, and habitual physical activity across the adult lifespan. Physical activity was directly related to sleep quality in the older, but not the younger or middle-aged adults. Although no association was observed between physical activity and self-reported fatigue, sleep quality was inversely related to self-reported fatigue in older adults. These results highlight relationships between physical activity habits, sleep quality and feelings of fatigue that appear to be unique to older adults. While the precise nature of these variables and their interactions remain to be determined, these data provide novel and compelling impetus for further evaluation of the concept of “fatigability” in aging (Eldadah, 2010).
Physical Activity
Both total activity counts per day and time spent in MVPA for each of our age groups are in good agreement with data from a larger sample of 4,867 participants in the National Health and Nutrition Examination Survey (NHANES; (Troiano et al., 2008)). The cut-points for activity intensity used here are those most widely used for older adults (Gorman et al., 2014). However, depending on the question at hand, the validation of age-specific cut-offs and shorter epochs for collection (Edwardson and Gorely, 2010) may prove useful in the future. Additional studies of the relationships between physical activity, sleep quality, and self-reported fatigue should also include individuals with a larger range of physical activity levels.
Sleep Quality
The majority of our sample of 60 adults (55%) was classified as “good sleepers,” based on the global PSQI scores (Buysse et al., 1991), a value comparable to that observed in the general population (Loge et al., 1998). Somewhat surprisingly, PSQI scores were not different across the younger, middle-aged, or older age groups, demonstrating that sleep quality was not lower in old age, as predicted previously (Buysse et al., 1991). Our use of subjective measures of sleep quality may have underestimated the problem in our older cohort. The emerging evidence of the importance of sleep quality to cognitive function (Pace-Schott and Spencer, 2011), metabolic health (Valentine et al., 2009) and quality of life ratings (Avlund, 2010) has fostered the development of objective measures of sleep, including actigraphy-based assessments (Marino et al., 2013). Future studies designed to address questions related to sleep and aging should make good use of these new methodologies.
Self-reported Fatigue
The concept of “fatigue” is challenging to define and measure, contributing to mixed results regarding its prevalence among older adults (Avlund, 2010). However, reviews on the topic suggest evidence that self-reported fatigue is a significant issue for individuals over the age of 65 years (Poluri et al., 2005, Avlund, 2010). In our study sample, a greater proportion of middle-aged participants (68.8%) and younger participants (54.5%) than older participants (23.1%) had fatigue scores above the median for their respective age group, which is consistent with previous reports and can likely be attributed to lifestyle demands such as school, work and family (Junghaenel et al., 2011). However, this finding is contradictory to suggestions of greater fatigue in older adults (Avlund, 2010, Poluri et al., 2005), which may be due to our tightly-controlled recruitment of older individuals with no significant health or physical function complications, limiting the extension of our findings to individuals with clinical, or sub-clinical complications. It is therefore possible that higher self-reported fatigue in older adults may be related more to health status than to aging per se. This hypothesis awaits further investigation.
Relationships Among Sleep, Fatigue and Activity
A significant, positive relationship was observed between physical activity and sleep quality in the older, but not the younger or middle-aged participants. When physical activity was parsed into the varying intensities, it was apparent that the relationship was due in large part to minutes spent in MVPA each day (Figure 1, right). The older sample in our study demonstrated a larger range in MVPA than young, which may have led to the observation of a stronger relationship with sleep quality in this group. Previous research has shown that increasing fitness, while maintaining daily energy expenditure in older adults was not associated with changes in sleep quality (Oudegeest-Sander et al., 2013). Taken together with the results of the present study, it is suggested that habitual physical activity levels, rather than fitness, are associated with sleep quality in older adults. Further, such a relationship appears to be unique to our older population and warrants further research.
No relationship was observed between physical activity and self-reported fatigue in any of the age groups, suggesting that physical activity levels vary for the same level of fatigue. Many factors may contribute to the lack of association between physical activity and fatigue. One possibility is that in an attempt to avoid excessive fatigue, individuals reduce their physical activity, which could yield a weak association. Research focused on understanding the etiology and impact of self-reported fatigue in a variety of populations is a growing endeavor. While the PROMIS questionnaire was chosen for this study because of its strong validity (Castel et al., 2008), there are many other fatigue measures currently in use. As a result, fatigue analysis lacks a uniform protocol, making its relationships with other outcomes measures difficult to quantify.
A significant, positive association was observed between sleep quality and fatigue scores in the older, but not the younger or middle-aged participants. Such an association is consistent with previous reports in healthy (Stepanski et al., 1984, Goel et al., 2009) and clinical populations (Cella et al., 2010, Valentine et al., 2009). In the older group, we observed a relationship between physical activity and sleep quality and between sleep quality and fatigue but not between physical activity and fatigue. Thus, sleep quality and fatigue may be related in older individuals in a manner independent of physical activity. However, a cause and effect relationship cannot be established here and the contribution of factors such as stress, anxiety, or other sub-clinical disease processes cannot be ruled out.
All participants in this study were healthy, free from major disease or problems related to polypharmacy, and of average activity level for their age groups (Troiano et al., 2008). Despite these characteristics, our older adults had lower physical function than the young and middle-aged groups. It would be of value to determine whether the age-related interactions between sleep, activity and fatigue are more pronounced in older adults with more complex clinical presentation. The possibility that this latter portion of the aged population might benefit even more from increased daily physical activity remains to be determined.
Conclusion
To our knowledge, this is the first study to use an objective assessment of physical activity to examine the relationships among activity, sleep quality and feelings of fatigue across the adult lifespan. We have shown here that higher habitual physical activity, particularly MVPA, is associated with better sleep quality, which in turn is associated with lower self-reported fatigue in older adults. An important result to come from this work is the observation that these interactions between physical activity, sleep quality and fatigue appear to be unique to the population of adults over age 65 years. While these results lend support to the recommendation of physical activity to promote quality of sleep in older individuals, directionality of these relationships cannot be inferred from the current data. These results need to be confirmed in a larger study with experimental designs that allow for cause-and-effect testing. A better understanding relationships among physical activity, sleep quality and self-reported fatigue will lead to effective methods of mitigating fatigue of older adults, contributing to overall improvements in well-being.
Supplementary Material
Highlights.
Although sleep problems and fatigue are common complaints in old age, little information is available as to the possible role that habitual physical activity might play in alleviating these problems.
We measured physical activity, sleep quality and self-reported fatigue in healthy young, middle-aged and older adults, and examined the relationships among these variables.
Our results indicated that physical activity was associated with sleep quality only in older adults; likewise, poor sleep and fatigue also were related only in the older group. Somwhat surprisingly, there was no relationship between physical activity and fatigue in any age group.
These results suggest that physical activity may relieve sleep problems, and that in turn improved sleep may play a role in reducing self-reported fatigue in a manner that is unique to older adults. However, the directions of these relationships, and any potential causality, remain to be determined.
Acknowledgments
The authors thank Drs. Stephen Foulis and Rebecca Spencer for advice regarding the physical activity and sleep measures used in this study. We also thank Terri O’Brien for assistance with recruitment and scheduling, and the participants for their contributions to this work. This study was funded by NIH R01 AG21094 and K02 AG023582, as well as a University of Massachusetts, Amherst Commonwealth Honors College grant.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Avlund K. Fatigue in older adults: an early indicator of the aging process? Aging Clin Exp Res. 2010;22:100–115. doi: 10.1007/BF03324782. [DOI] [PubMed] [Google Scholar]
- Buysse DJ, Reynolds CF, 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. DOI: 0165-1781(89)90047-4 [pii] [DOI] [PubMed] [Google Scholar]
- Buysse DJ, Reynolds CF, 3rd, Monk TH, Hoch CC, Yeager AL, Kupfer DJ. Quantification of subjective sleep quality in healthy elderly men and women using the Pittsburgh Sleep Quality Index (PSQI) Sleep. 1991;14:331–338. [PubMed] [Google Scholar]
- Castel LD, Williams KA, Bosworth HB, Eisen SV, Hahn EA, Irwin DE, Kelly MA, Morse J, Stover A, DeWalt DA, DeVellis RF. Content validity in the PROMIS social-health domain: a qualitative analysis of focus-group data. Qual Life Res. 2008;17:737–749. doi: 10.1007/s11136-008-9352-3. [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cella D, Riley W, Stone A, Rothrock N, Reeve B, Yount S, Amtmann D, Bode R, Buysse D, Choi S, Cook K, Devellis R, DeWalt D, Fries JF, Gershon R, Hahn EA, Lai JS, Pilkonis P, Revicki D, Rose M, Weinfurt K, Hays R PROMIS Cooperative Group. The Patient-Reported Outcomes Measurement Information System (PROMIS) developed and tested its first wave of adult self-reported health outcome item banks: 2005–2008. J Clin Epidemiol. 2010;63:1179–1194. doi: 10.1016/j.jclinepi.2010.04.011. [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC) Adult participation in recommended levels of physical activity--United States, 2001 and 2003. MMWR Morb Mortal Wkly Rep. 2005;54:1208–1212. DOI: mm5447a3 [pii] [PubMed] [Google Scholar]
- Edwardson CL, Gorely T. Epoch length and its effect on physical activity intensity. Med Sci Sports Exerc. 2010;42:928–934. doi: 10.1249/MSS.0b013e3181c301f5. [doi] [DOI] [PubMed] [Google Scholar]
- Eldadah BA. Fatigue and fatigability in older adults. PM R. 2010;2:406–413. doi: 10.1016/j.pmrj.2010.03.022. [doi] [DOI] [PubMed] [Google Scholar]
- Foley DJ, Monjan AA, Brown SL, Simonsick EM, Wallace RB, Blazer DG. Sleep complaints among elderly persons: an epidemiologic study of three communities. Sleep. 1995;18:425–432. doi: 10.1093/sleep/18.6.425. [DOI] [PubMed] [Google Scholar]
- Freedson PS, Melanson E, Sirard J. Calibration of the Computer Science and Applications, Inc. accelerometer. Med Sci Sports Exerc. 1998;30:777–781. doi: 10.1097/00005768-199805000-00021. [DOI] [PubMed] [Google Scholar]
- Goel N, Rao H, Durmer JS, Dinges DF. Neurocognitive consequences of sleep deprivation. Semin Neurol. 2009;29:320–339. doi: 10.1055/s-0029-1237117. [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gorman E, Hanson HM, Yang PH, Khan KM, Liu-Ambrose T, Ashe MC. Accelerometry analysis of physical activity and sedentary behavior in older adults: a systematic review and data analysis. Eur Rev Aging Phys Act. 2014;11:35–49. doi: 10.1007/s11556-013-0132-x. [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Junghaenel DU, Christodoulou C, Lai JS, Stone AA. Demographic correlates of fatigue in the US general population: results from the patient-reported outcomes measurement information system (PROMIS) initiative. J Psychosom Res. 2011;71:117–123. doi: 10.1016/j.jpsychores.2011.04.007. [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- King AC, Pruitt LA, Woo S, Castro CM, Ahn DK, Vitiello MV, Woodward SH, Bliwise DL. Effects of moderate-intensity exercise on polysomnographic and subjective sleep quality in older adults with mild to moderate sleep complaints. J Gerontol A Biol Sci Med Sci. 2008;63:997–1004. doi: 10.1093/gerona/63.9.997. DOI: 63/9/997 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loge JH, Ekeberg O, Kaasa S. Fatigue in the general Norwegian population: normative data and associations. J Psychosom Res. 1998;45:53–65. doi: 10.1016/s0022-3999(97)00291-2. DOI: S0022-3999(97)00291-2 [pii] [DOI] [PubMed] [Google Scholar]
- Marino M, Li Y, Rueschman MN, Winkelman JW, Ellenbogen JM, Solet JM, Dulin H, Berkman LF, Buxton OM. Measuring sleep: accuracy, sensitivity, and specificity of wrist actigraphy compared to polysomnography. Sleep. 2013;36:1747–1755. doi: 10.5665/sleep.3142. [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oudegeest-Sander MH, Eijsvogels TH, Verheggen RJ, Poelkens F, Hopman MT, Jones H, Thijssen DH. Impact of physical fitness and daily energy expenditure on sleep efficiency in young and older humans. Gerontology. 2013;59:8–16. doi: 10.1159/000342213. [doi] [DOI] [PubMed] [Google Scholar]
- Pace-Schott EF, Spencer RM. Age-related changes in the cognitive function of sleep. Prog Brain Res. 2011;191:75–89. doi: 10.1016/B978-0-444-53752-2.00012-6. [doi] [DOI] [PubMed] [Google Scholar]
- Poluri A, Mores J, Cook DB, Findley TW, Cristian A. Fatigue in the elderly population. Phys Med Rehabil Clin N Am. 2005;16:91–108. doi: 10.1016/j.pmr.2004.06.006. DOI: S1047-9651(04)00059-2 [pii] [DOI] [PubMed] [Google Scholar]
- Stepanski E, Lamphere J, Badia P, Zorick F, Roth T. Sleep fragmentation and daytime sleepiness. Sleep. 1984;7:18–26. doi: 10.1093/sleep/7.1.18. [DOI] [PubMed] [Google Scholar]
- Tiedemann A, Shimada H, Sherrington C, Murray S, Lord S. The comparative ability of eight functional mobility tests for predicting falls in community-dwelling older people. Age Ageing. 2008;37:430–435. doi: 10.1093/ageing/afn100. [doi] [DOI] [PubMed] [Google Scholar]
- Troiano RP, Berrigan D, Dodd KW, Masse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40:181–188. doi: 10.1249/mss.0b013e31815a51b3. [doi] [DOI] [PubMed] [Google Scholar]
- Valentine RJ, McAuley E, Vieira VJ, Baynard T, Hu L, Evans EM, Woods JA. Sex differences in the relationship between obesity, C-reactive protein, physical activity, depression, sleep quality and fatigue in older adults. Brain Behav Immun. 2009;23:643–648. doi: 10.1016/j.bbi.2008.12.003. [doi] [DOI] [PubMed] [Google Scholar]
- Vestergaard S, Patel KV, Bandinelli S, Ferrucci L, Guralnik JM. Characteristics of 400-meter walk test performance and subsequent mortality in older adults. Rejuvenation Res. 2009;12:177–184. doi: 10.1089/rej.2009.0853. [doi] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ward DS, Evenson KR, Vaughn A, Rodgers AB, Troiano RP. Accelerometer use in physical activity: best practices and research recommendations. Med Sci Sports Exerc. 2005;37:S582–S588. doi: 10.1249/01.mss.0000185292.71933.91. DOI: 00005768-200511001-00011 [pii] [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.