SUMMARY
Standard precaution (SP) adherence is universally suboptimal, despite being a core component of healthcare-associated infection (HCAI) prevention and healthcare worker (HCW) safety. Emerging evidence suggests that patient safety climate (PSC) factors may improve HCW behaviours. Our aim was to examine the relationship between PSC and SP adherence by HCWs in acute care hospitals. A systematic review was conducted as guided by the Preferred Reporting Items for Systematic Reviews and Meta-Analysis. Three electronic databases were comprehensively searched for literature published or available in English between 2000 and 2014. Seven of 888 articles identified were eligible for final inclusion in the review. Two reviewers independently assessed study quality using a validated quality tool. The seven articles were assigned quality scores ranging from 7 to 10 of 10 possible points. Five measured all aspects of SP and two solely measured needlestick and sharps handling. Three included a secondary outcome of HCW exposure; none included HCAIs. All reported a statistically significant relationship between better PSC and greater SP adherence and used data from self-report surveys including validated PSC measures or measures of management support and leadership. Although limited in number, studies were of high quality and confirmed that PSC and SP adherence were correlated, suggesting that efforts to improve PSC may enhance adherence to a core component of HCAI prevention and HCW safety. More clearly evident is the need for additional high-quality research.
Keywords: Healthcare-associated infection, Infection prevention, Safety climate, Standard precautions
Introduction
Healthcare-associated infections (HCAIs) – largely preventable adverse events – are a global patient safety problem.1 Over the past decade literature continues to conclude that HCAIs are frequent, catastrophic, and costly.2–6 Despite estimates that 10–70% of HCAIs are preventable, the burden is staggering in developed and developing nations.1,7 In the USA 5–10% of acute care patients acquire one or more HCAIs; in lives directly affected this indicates that approximately two million US patients suffer an HCAI, resulting in an estimated 99,000 deaths annually.1,4,5,8 In European countries these statistics are similar with prevalence estimates of 6%, or 3.2 million patients per year with at least one HCAI.9,10 On any given day 80,000, or one in 18, patients in a European hospital have at least one HCAI, resulting in an estimated 37,000 attributable deaths annually.9,10 The estimates are more striking in developing countries where pooled prevalence estimates range between 10.1% and 15.5%.11,12 HCAI densities in intensive care units are up to three times greater than in developed countries at 47.9 per 1000 patient-days, with excess mortality attributed to HCAI at 18.5–29.3%.11,12 Moreover, the annual attributable direct costs of HCAI are $9.8 billion in the USA and €7 billion in Europe, and are estimated to be high also in developing countries.12–14 In sum, the prevention of HCAI is of significant and current importance, affecting all healthcare consumers with real direct and indirect consequences.2,7,9
Nearly 30 years ago the US Centers for Disease Control and Prevention (CDC) introduced universal precautions as a core component of HCAI prevention, deemed applicable to all healthcare workers (HCWs) in contact with all patients in all settings, regardless of the suspected or confirmed presence of an infectious agent.15 In 1996, CDC universal precautions guidelines were updated and termed ‘standard precautions’ (SPs). Specific components of SP include hand hygiene, use of appropriate personal protective equipment (PPE), safe use and disposal of sharps, decontamination of environment and equipment, patient placement and linen and waste management.16 These standards have been adopted internationally by European and other countries and are considered a common national-level guideline, in contradistinction to recommendations for prevention of specific types of HCAI, such as targeted device-related prevention bundles, surgical site infection procedures, or pharmacologic measures.13,16 The World Health Organization has declared it imperative that standard precautions be established prior to implementation of any specific measure or practice ‘bundle’ or targeted intervention.12 Thus, a longstanding and broad-reaching approach and primary strategy to prevent HCAI is adherence to SPs by HCWs.16
Over a decade of literature has demonstrated that HCW adherence to basic preventive practices such as SPs remains suboptimal, adhered to less than 50% of the time.17–19 A body of literature has also explored the relationships among individual-level factors such as intent, knowledge, attitudes, and experience and adherence to components of SP.20–24 Mixed findings from these studies demonstrate the complex and multidimensional nature of infection prevention behaviours, suggesting that important antecedents to SP adherence may also include organizational level characteristics in which the HCW performs.
Over a decade ago the Institute of Medicine’s To err is human landmark report recognized the importance of the safety culture of healthcare organizations in improved provider performance and adverse event reduction, and implored organizations to create a safety culture.25 Safety culture is considered broadly the managerial and HCW attitudes and values as they relate to the perception of risk and safety. Teamwork, leadership support, communication, non-punitive response to errors, perception of organizational commitment, work design, staffing and workload, resources, and emphasis on quality have been identified as important and common attributes of a positive safety culture in the literature.26–28 Patient safety climate (PSC), a related concept, has also been identified as an important antecedent of HCW behaviour.29–31 Although the terminology overlaps in the literature, one conceptual distinction is that safety culture is described as the overarching values, norms, and assumptions of the organization that drive the quality of care, and that safety climate is the collective reflection of the perception, attitudes, and shared experiences of the culture.26,32 Succinctly, safety climate comprises the group-level experiences of the overarching organization-level culture of safety.
Several studies have demonstrated that safety climate factors are a significant predictor of safe work behaviours. Findings by DeJoy et al. indicate that a positive PSC may facilitate the creation of a work environment that will enable, support, and reinforce HCWs to comply with safe practices.33 These findings are supported in a review that examined the relationship between PSC and nurses’ health and safety behaviours and outcomes.34 Similarly, Gershon et al. demonstrated that SP compliance was strongly correlated with organizational commitment to safety.21 Advancing this knowledge, DeJoy et al. found that a negative safety climate was the strongest predictor of job hindrances, which in turn were the strongest predicators of lower SP adherence.35 Most recently, support for the PSC antecedent of SP adherence was demonstrated by Nichol et al., and also by Brevidelli and Cianciarullo who identified that factors of management support for ‘safe work practices’ and ‘safety performance feedback’ were correlated with SP adherence.36,37
Despite the significant burden of HCAI, persistent evidence of suboptimal SP adherence, and the growing body of evidence of the importance of PSC factors to HCW behaviours such as SP adherence, there has been no systematic review specifically examining the relationship between PSC and SP adherence. A systematic review is required to summarize this research evidence, thereby accelerating the translation of evidence into practice and guiding future research as appropriate. There is an urgent need to systematically identify and appraise this body of research and information, synthesize the results, and provide an assessment of the evidence that may support decision-making and guide allocation of scarce resources. To address this gap a systematic review was conducted to identify, critically review and synthesize literature regarding the evidence of a relationship between PSC and SP adherence in acute care hospitals.
Methods
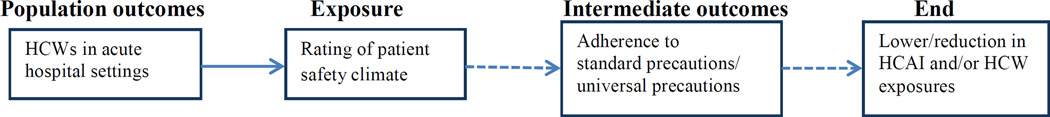
This systematic review addressed the question: ‘What is the relationship between PSC and SP adherence in healthcare professionals working in acute care hospital settings?’ The analytic framework is presented in Figure 1. The primary outcome of interest is adherence to SP protocols; the secondary outcome of interest is the occurrence of HCAI and HCW exposures. The Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) statement and 27-item checklist guided this review.38
Figure 1.
Analytic Framework for Patient Safety Climate and Standard Precaution Adherence. Boxes represent the population, exposure, and outcomes examined to address the question: ‘Do healthcare workers in acute hospital settings with a high rating of patient safety climate adhere more to standard precautions than healthcare professionals in acute hospital settings with a low rating of patient safety climate?’ HCW, healthcare worker; HCAI, healthcare-associated infection.
Search strategy and selection criteria
All eligible studies had to meet the following inclusion criteria: a quantitative study that examines the relationship between PSC dimensions and adherence to components of SP by HCWs in acute care hospital settings, published between January 2000 and September 2014, and available in English language. This 14-year time frame was selected as it encompasses the recent literature following the 1999 Institute of Medicine landmark report and the subsequent focus of safety culture and climate in healthcare settings.25 HCWs must include direct care providers who work in the setting to represent those whose behaviours have an impact on patient outcomes and who are adequately assimilated in the environment to rate the PSC. Studies solely including students or trainees or laboratory workers are excluded. Studies that included outcomes of HCAI and HCW exposure injury were of particular interest as a secondary outcome. The study had to explicitly use a PSC scale or measure leadership, peer support, or teamwork to more fully capture the breadth of the PSC construct in contradistinction to articles that focused solely on need for resources, patient equipment availability, education, or training. Quality improvement and studies that included an intervention such as education were excluded to isolate the specific relationship of interest between PSC and SP adherence. Whereas these studies indicated an organizational interest, the focus of this review was the relationship between measured features of the PSC and SP, not the intervention effect. Therefore these studies were excluded to allow for a more rigorous and focused review addressing the study question. Qualitative studies, reviews, letters and articles that did not report primary data were excluded, as were studies that were not conducted in acute care hospitals.
Three databases explicitly selected that include primary biomedical research were searched: PubMed, CINAHL, and Embase. The search strategy was developed following consultation with an information specialist in an iterative process. Initially, titles and abstracts were searched for key terminology. Search terms included Medical Subject Headings (MeSH), related text word, entry terms or major headings as appropriate for each database structure (Appendix A). Search terminology was broad and specifically selected to capture the evolving terminology in fields of infection prevention and patient safety. These included ‘universal precautions’, and ‘universal precaution’ (this was selected as there is no MeSH term for standard precautions – the terminology recommend by the CDC in 1996), and ‘safety climate’, ‘patient safety culture’, ‘patient safety’ (introduced in MeSH in 2012). Search terminology from both safety culture and climate literature were included to ensure an exhaustive review, though the inclusion criteria for abstract selection and final review was that articles include the PSC factors of HCW perceptions, attitudes, or shared experiences of the organizational features of the work environment. That is, the key discerning factor for inclusion was the HCW view of elements of the safety culture. Additionally, several terms to capture the population of all HCWs were selected including ‘healthcare worker’, ‘healthcare professional,’ ‘nurse,’ and ‘physician’. The terminology search yielded a total of 2,147,731 titles and abstracts that contained any one of the population, exposure, or outcome terms of interest (Appendix A). The search strategy was then applied to yield only articles that included all three (population, exposure and outcomes) components. This search yield was then de-duplicated and abstracts and titles were screened for inclusion and exclusion criteria. Disagreements were resolved by consensus (A.H. and E.L.L.).
Data extraction
A summary of select study characteristics was created and completed (Table I). Two reviewers (A.H. and E.L.L.) independently assessed study quality using a modified Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) tool.45 This 22-item validated measure guides the reviewer to assess the quality of the study title and abstract, introductions, methods, results, discussion and other information. This was modified to retain 10 items in four categories: introduction (one item); methods (five items); results (two items); and discussion (two items) (Table II). Items relevant to this review included: background and rationale, setting, variables, data sources, measurement, statistical methods, main results and results summary, discussion strengths and limitations, and interpretation. Each item was scored one point if sufficiently reported; thus each study was assigned a score ranging from 0 to 10 by each reviewer. Inter-rater reliability was then established by discussion of the scoring assigned. Quality scores were considered in agreement if they were within two points of each other based on prior use of the tool. In this review, the two raters reached consensus as all studies were scored within one point of each other.
Table I.
Summary of select study characteristics
| Source | Objective | Study design |
Sample | Setting | PSC measure: components, type of measure, psychometric properties |
Primary outcome: SP adherence components, type of measure, psychometric properties |
Secondary outcomes: HCAI or HCW exposure |
Results | Quality rating |
|---|---|---|---|---|---|---|---|---|---|
| Anderson et al.39 |
Evaluate the validity and reliability of a measure of organizational safety climate in association with HCW compliance with SP. |
Secondary analysis of cross- sectional data. |
1746 HCWs (four categories: RN, MD, laboratory and miscellaneous) with direct patient contact or specimen contact. |
Three large acute care hospitals in the Mid- Atlantic, Southwest and Midwest USA. |
Survey, nine-item 4-point Likert scale measuring leadership, management, non- punitive environment, organizational structure, summated as mean score across all items. Five-item 5- point Likert survey on availability of PPE. Cronbach’s alpha = 0.85, construct validity established by hypothesis testing of relationships between variables. |
Survey (Gershon et al.21), measured frequency of 11 behaviours using 5-point Likert scale. Includes PPE, HH, sharps environmental cleaning and food in work area. Mean of items comprised a SP score. Content validity reported, derived from CDC guidelines and Gershon et al. 21 tool. |
Neither | Statistically significant relationship between PSC and SP adherence. Measure of PSC found reliable and valid. |
10 |
| Brevidelli et al.37 |
To analyse the influence of psychosocial and organizational factors on compliance with SP for preventing exposure to biologic materials. |
Cross- sectional survey |
Random sampling, 270 HCWs (213 nurses and 57 MDs). 370 sample aim. |
University hospital in São Paulo, Brazil. |
65-item survey, adapted from Gershon et al.21 and DeJoy et al.40 transculturally adapted and includes psychosocial and organizational factors: management support, knowledge about risk of transmission, risk- taking personality, organizational barriers, availability of equipment, workload and training. Cronbach’s alpha between 0.67 and 0.82 for scales, construct validity established by exploratory factor analysis. |
13-item survey, ‘standard precaution compliance’ composed as a global index and grouped by adherence to PPE or disposal of sharps. Content validity reported as derived from Gershon et al. (1995)21 and DeJoy et al.40 tools. |
Neither. | Safety climate scale statistically significant between management support for safe work practices and safety performance feedback and SP adherence. As single dimensional construct statistically significant relationship between training, less perceived barriers, feedback and support for safe practices and SP adherence. |
8 |
| Clarke et al.41 |
To examine relationships between nurse characteristics , types of protective equipment, organizational climate, and risk of needlestick injuries and near misses. |
Cross- sectional study |
2287 RNs with direct care responsibility who worked at least 16 h per week on medical surgical units and surveys from management, infection control and purchasing officials. |
22 US hospitals described as Magnet certified or reputations for excellence |
Questionnaire of safety officials at hospitals regarding presence and availability of safety intravenous insertion equipment. Five- item scale, items from the 49-item Nursing Work Index Revised survey of nurses using a 4-point Likert scale to rate the presence of administrative and management support, leadership and responsiveness. Cronbach’s alpha = 0.85. |
Questionnaire survey that asked frequency of wearing gloves when performing venepuncture and other procedures with a risk of contact with body fluids. No psychometrics properties reported. |
HCW outcome: needlestick injuries of nurses. |
Statistically significant relationship between poor safety climate and needlestick injuries. Nurse self-report compliance with SPs was analysed separately descriptively. |
7 |
| DeJoy et al.35 |
To examine the individual, job-task and environment organizational factors related to SP compliance. |
Cross- sectional analysis of data from a larger study examining nurses. |
889 nurses. |
Three large (~1000 beds) regionally distinct acute care hospitals in the USA |
17 items from a larger survey measuring safety climate dimensions: priority assigned to safety, formal and informal feedback, management actions and commitment to safety. Cronbach’s alpha range 0.57–0.84 for scales. Construct validity established by confirmatory factor analysis. |
11-item survey measuring compliance with sharps and waste disposal, needle recapping, hand hygiene, cleaning spills and use of PPE/barriers. Cronbach’s alpha = 0.73 for compliance with PPE (three items) and 0.53 for general compliance (8 items). Construct validity established by exploratory factor analysis. |
HCW exposure analysed as predict or: exposure to blood or body fluids including splashes, needlesticks, cuts with sharp objects and contact with open wounds. |
Statistically significant relationships between knowledge of transmission risks, absence of job hindrances, formal and informal feedback, availability of supplies, and priority assigned to safety with compliance with PPE and general compliance. |
7 |
| Gershon et al.42 |
To develop a measure of safety climate that is specific for bloodborne pathogen management, and assesses relationship with safe behaviour and workplace exposures. |
Cross- sectional design. |
Stratified sample of those considered highest risk for blood and body fluid exposure; 789 nurses, physicians and technicians. |
One urban, 1000-bed research medical centre. |
46-item 5-point Likert survey measuring presence of safety climate dimensions: senior management support, absence of workplace barriers, worksite cleanliness and orderliness, minimal conflict and good communication, frequent safety monitoring feedback and training and availability of engineering controls. Original 46-item tool psychometric properties referenced but not reported. Construct validity and reliability established through factor analysis in 6 factors (20 items). Cronbach’s alpha range 0.71–0.84 for scales. |
14-item survey of SP compliance using 5-point Likert scale ‘strict compliance’ defined as score above ≥80%). Prior tool development and testing referenced though psychometric properties not reported. |
HCW outcome: workplace exposures to blood and body fluids over preceding 6 months. |
Statistically significant relationship between senior management support, absence of workplace barriers, and worksite cleanliness and orderliness and SP adherence. Senior management support and frequent safety monitoring feedback and training were significantly related with workplace exposures. |
10 |
| Kermode et al.43 |
Describe the knowledge and understanding of SPs and predictors of compliance among HCWs in rural north India. Assess extent of occupational exposure, identify factors associated with exposure, quantify the risk of bloodborne pathogens, assess compliance with SPs and identify factors associated with non-compliance. |
Cross- sectional survey of HCWs. |
266 HCWs including nurses, midwives, student nurses, laboratory workers, doctors dentists and others. |
Seven hospitals in rural north India. |
13-item, 5-point Likert scale of items related to patient safety climate including availability of PPE, cleanliness of environment, management support and leadership, organizational commitment to patient safety and training. Nine-item 5-point Likert scale used to measure barriers was a separate scale. Tool reliability and validity testing referenced to Gershon et al.21, though psychometric properties not reported. |
12 item, 5- point Likert scale measures behaviours related to SP. An overall compliance score calculated by summing the scores across participants. Tool reliability and validity testing referenced to Gershon et al.21, though psychometric properties not reported. |
HCW outcome: occupational blood exposure. No patient outcome. |
Statistically significant relationship between PSC and SP compliance and perceived barriers and SP compliance. |
9 |
| Vaughn et al.44 |
To examine organizational factors and occupational characteristics associated with adherence to occupational safety guidelines to avoid needle recapping. |
A cross- sectional study linking three data sources |
The sample comprised 1454 physicians, nurses and laboratory workers who self- identified as likely to routinely handle needles and 99 IPs from 99 hospitals. |
Analytic sample included nurses and IPs from 84 hospitals drawn from a stratified random sample to represent each county in Iowa. |
17 items drawn from HCW survey (management support, job demands, feedback, and availability of PPE) and IP survey (structural support, key leadership support and equipment availability). Construct validity and reliability established through factor analysis in four factors (17 items). Cronbach’s alpha range 0.70–0.90 for scales. |
One-item survey measure using a visual scale to mark respondents’ level of compliance between 0 and 100% and then treated as a dichotomous measure of never recapping or ever recapping a needle. Psychometric properties not reported. |
Neither. | Statistically significant relationships were found between organizational IP staffing, HCW education, availability of PPE, management support for safety, and consistent adherence to needle recapping guidance. |
9 |
PSC, patient safety climate; SP, standard precaution; HCAI, healthcare-associated infection; HCW, healthcare worker; RN, registered nurse; MD, medical doctor; PPE, personal protective equipment; HH, hand hygiene; IP, infection prevention.
Table II.
Quality Assessment Tool: Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Modified
| Section | Points | Evaluation |
|---|---|---|
| Introduction | ||
| Background/rationale | 1 | Explain the scientific background and rationale for the investigation being reported and state specific objectives/aims, including any pre-specified hypotheses. |
| Methods | ||
| Setting | 1 | Describe the setting, locations, and relevant dates, including periods of recruitment, exposure, follow-up, and data collection. |
| Variables | 1 | Clearly define all outcomes, exposures, predictors, potential confounders, and effect modifiers. Give diagnostic criteria, if applicable. |
| Data sources | 1 | For each variable of interest, give sources of data and details |
| Measurement | 1 | What are the methods of assessment (measurement) and are the measures validated? |
| Statistical methods | 1 | Describe all statistical methods, including those used to control for confounding. Describe any relative sensitivity analyses when applicable. Give unadjusted estimates and, if applicable, confounder-adjusted estimates and their precision (e.g. 95% confidence interval). Make clear which confounders were adjusted for and why they were included. |
| Results | ||
| Main results | 1 | Report results for each specified objective/aim in introduction. |
| Result summary | 1 | Results clearly summarized with appropriate graphics. |
| Discussion | ||
| Strengths and limitations | 1 | Discuss limitations of the study, taking into account sources of potential bias or imprecision. Discuss both direction and magnitude of any potential bias. Discuss the generalizability (external validity) of the study results. |
| Interpretation | 1 | Give a cautious overall interpretation of results considering objectives, limitations, multiplicity of analyses, results from similar studies, and other relevant evidence. |
| Total points | 10 |
Results
Study selection
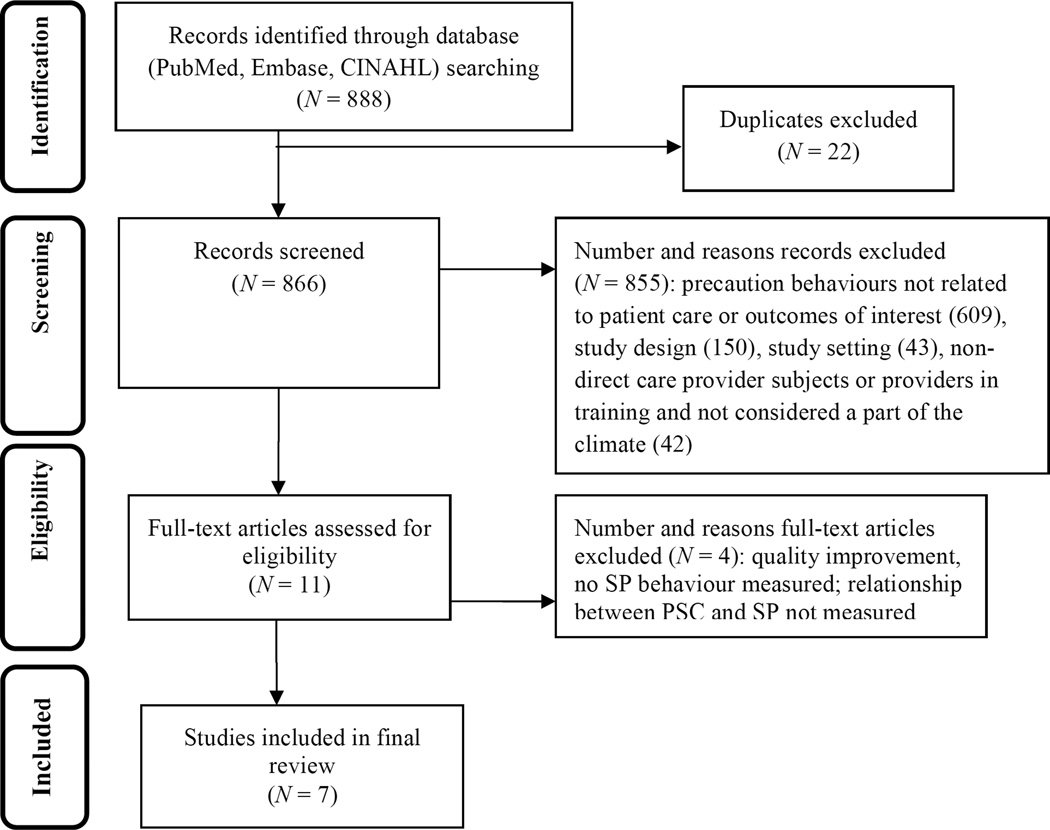
The search yielded 888 articles; of these, 22 articles were duplicates and excluded, yielding 866 that were screened for eligibility. Following title screening and abstract review 855 were excluded, yielding 11 articles retrieved for full review and data extraction. The main reasons for excluding studies was precaution behaviours not related to patient care or outcomes of interest (609), study design (150), study setting (43), or non-direct care provider subjects or providers in training and not considered a part of the climate (42) (e.g. laboratory workers, nursing students, dentists, rural settings, tobacco exposure, handling of chemotoxic agents). During full review four articles were excluded from data extraction as they did not meet the inclusion criteria. One was a quality improvement intervention study two did not include SP behaviour, and one described SP adherence and features of the organizational climate but did not measure the relationship between the variables.46–49 Seven articles were included in the final review (Figure 2).
Figure 2.
PRISMA flow diagram: relationship between patient safety climate (PSC) and standard precautions (SPs). Boxes on the left represent each stage of search strategy; boxes on the right represent the number of articles retained and excluded by stage of analysis. Records identified through database
Study characteristics
All seven studies were cross-sectional surveys conducted in acute care hospitals. Sample sizes ranged from 266 to 2287. All studies included nurses; two included nurses only, and five included physicians, technicians, laboratory workers and other HCWs with direct patient or specimen contact. Five studies were conducted in geographically distinct regions of the USA, one was conducted in an urban location in Brazil and one in rural north India. Two were single site studies, the remaining five were multi-site. Multi-site studies were conducted at three, seven, 22, or 84 hospitals. Hospital settings were heterogeneous, and included large (~1000 beds) and small (<100 beds), teaching and non-teaching hospitals, research hospitals, those with and without specialty certification such as The Joint Commission Accreditation or Magnet Designation, and private and public hospitals.
Relationship between PSC and SP adherence
All of the studies reported statistically significant results in support of a relationship between features of the PSC and SP adherence (Table I). Overall, better PSC was related to greater SP adherence in heterogeneous hospital settings. Five of the studies measured items in all categories of SP adherence; these studies, however, analytically examined SP adherence as a global construct and did not discern between types of behaviours. The remaining two studies measured a single component of SP adherence: one measured the use of gloves when performing needlestick procedures and the other measured recapping needles when using sharps equipment. There was no standardized measure of PSC used in all studies, although three studies did employ an adaptation of the Gershon tool.21 All studies minimally measured features of management support and leadership as specified in the inclusion criteria. Other factors measured included job demands and feedback, equipment availability, commitment to safety and training, physical environment, transmission knowledge, risk-taking personality and non-punitive environment.29,35,37,41,42,44,48 Three of the seven studies examined the relationship between secondary outcomes of HCW (occupational) outcomes. Of note, one study examined HCWs’ prior exposure to blood and body fluids as a reinforcing factor or independent variable as opposed to an outcome. No study included patients’ HCAI outcomes.
Quality of studies
The scored quality of the studies ranged from 7 to 10 of 10 possible points; four were at or above the median of nine (Table I). Because the STROBE scoring system assigns the same weight to each criterion, the specific reason points were not assigned for each of the seven studies, detailed by category and item as follows. All studies sufficiently reported the introduction section as rated by the background/rationale; the results section, as rated by the adequacy of reporting main results for each specified objective/aim in the introduction; and the discussion section, as rated by sufficiently reporting the interpretation of the results. Studies by Clarke et al.41 and DeJoy et al. were not assigned a setting point for sufficiently describing the setting locations, and relevant dates, including periods of recruitment, exposure, follow-up, and data collection.35,41 Studies by Brevidelli and Cianciarullo and by DeJoy et al. were not assigned a data sources point for sufficiently reporting sources of data and details for each variable of interest.35,37 Clarke et al.’s study was not assigned a point for measurement, indicating that methods of assessment (measurement) and description of measure validation were insufficiently reported.41 Clarke et al.’s study was not assigned a point for statistical methods, including a description of methods to control for confounding, confounders included, and rationale.41 Brevidelli and Cianciarullo’s study was not assigned a results point for clearly summarizing and presenting results with appropriate graphics.37 Finally, Anderson et al.39 and Dejoy et al.’s studies were not assigned a discussion point for strengths and limitations including discussion of any potential bias, and direction and magnitude of any bias, and external validity.35,37,39
Discussion
CDC guidelines exist for HCWs to adhere to SPs in all settings, for all patients, all the time, as a primary strategy to prevent HCAI and HCW injuries and exposures. However, these guidelines are not embedded in practice, and reports of suboptimal adherence persist in the literature. An emerging body of evidence suggests that PSC factors are important to improve HCW behaviours. This focused systematic review was conducted to elucidate the relationship between PSC and SP adherence in healthcare professionals working in acute care hospital settings. Fourteen years of research was synthesized and important gaps in our knowledge were identified. These gaps are perhaps unsurprising given the dearth of research that has been conducted on this topic. Of the nearly 1000 articles identified through an exhaustive search, fewer than ten studies have been published that aim to address this important topic in whole or in part. Notably, no studies contained HCAI outcomes which would justify efforts to link PSC with SPs and patient outcomes.
The interest in PSC is evident; PSC has been identified as an important antecedent of HCW behaviour in general, and appears extensively in the infection prevention literature, typically in context of secondary strategies such as ‘bundled’ or targeted interventions to prevent device-related or surgical site infections.26–28,50,51 This was exemplified in our systematic review; the search strategy yielded 175,185 articles on PSC, more than three times the number (53,369) published that included SPs. Hence, an important gap identified in this review is the examination of the relationship between shared core values (PSC) and core practices (SPs).
Although limited in number, the studies identified were of high quality and therefore some critical insight into these relationships can be gained from this review, specifically the consistent correlation reported between better PSC and greater SP adherence in heterogeneous hospital settings. However, these studies largely focused on nurses, used a variety of self-report measures, and a limited number included HCW outcomes. Notably, none included patient outcomes; therefore the potential preventability of HCAIs by adherence to SPs, or the value of SPs, is not evident. Additionally, the majority of studies measured SPs as a global construct even though there may be different antecedent barriers and facilitators for different behavioural actions of SPs. For example, equipment availability may not be a barrier to performing hand hygiene but is a barrier to appropriate gown and glove use.
Identifying the modifiable features of the PSC that improve practices such as SPs will likely support the provision of more efficient and effective patient care. Notwithstanding the strengths of the identified studies, the gaps revealed by the lack of studies identified in this systematic review in and of itself points to the need for standardized, psychometrically sound measures and for more research that specifically examines the relationship between PSC and SP in acute care settings.
Limitations
This study used three databases: PubMed, CINAHL, and EMBASE, and focused on terms used to capture complex concepts and practices such as PSC and SP. Searching additional databases or using additional search terms may have identified more publications. The search strategy, however, was comprehensive and identified more than two million articles that included a population, exposure, or outcome of interest, and 866 that included all concepts of interest. The criteria that the article be written or available in the English language may also have led to omissions of studies published in other languages, particularly since studies that were screened and included were international. Additionally, PSC and SPs were operationalized differently across studies, making it impossible to conduct a meta-analysis. The final sample of seven studies limits the external validity of the study results. Finally, publication bias is a possible limitation; studies are less likely to be published if the findings are negative. For these reasons, and despite the high quality ratings of all studies, there are limits to our confidence in the correlation between PSC and SPs.
Conclusion
Despite decades of discordance between SP guidelines and practice, little attention has been paid, and subsequently little progress made, to close that gap. The importance of the organizational culture and climate has been suggested as an important variable in patient safety and HCW behaviour for nearly 15 years, but to our knowledge this is the first review to examine the specific relationship between PSC and SP adherence. Although limited in number, the seven studies identified were of high quality and confirmed that PSC and adherence to SP were correlated. Implications of this systematic review for administrators and clinical practice suggest that efforts to improve PSC may enhance adherence to a core component of HCAI prevention and HCW safety. Implications for researchers are indisputably evident; more high-quality studies are needed.
Acknowledgements
The authors would like to acknowledge L. Falzon, Information Specialist at Columbia University Libraries, for consultation in developing the search strategy and the Columbia University School of Nursing Writing Workshop Initiative members in refining this manuscript.
Funding sources
The corresponding author was supported as a postdoctoral trainee by the National Institute of Nursing Research, National Institutes of Health (Training in Interdisciplinary Research to Prevent Infections, T32 NR013454). The funder of the study had no role in the study design, data collection, analysis, interpretation of data, or writing of the report.
Appendix A. Standard precautions and safety climate search strategy
Summary
Total articles identified in PubMed, Embase, and CINAHL, N = 888
Articles excluded based on removal of duplicates, N = 22
Abstracts screened for eligibility, N = 866
Articles excluded following title screening and abstract review, N = 855
Full-text articles retrieved for full review, N = 11
Sources
-
PubMed
Limit: English, dates January 1st, 2000 to September 30th, 2014, abstract
Standard precautions:- Search standard precaution*[tw: Text Word], 285
- Search universal precaution*[tw], 613
-
Search Universal precautions[mesh: MeSH Terms], 345Combine #1 or #2 or #3 = 841
Safety culture:- patient safety[tw], 13,774
- hospital cultur*[tw], 68
- corporate cultur*[tw], 75
- ((Organization* OR organisation*) AND cultur*[tw]), 26,890
- safety environment[tw], 19
- safety climate[tw], 405
- safety culture[tw], 730
- Safety Management[MeSH], 7882
- Patient safety[MeSH], 3336
- Organizational culture[MeSH], 6467
Combine 1–10 with “OR”, N = 44,689
Final search: Combine SP and Climate with “AND”, N = 28
-
Embase
Quick limits: with abstract, only in English, pub type is article, years 2000 to 2014, search as broadly as possible
Climate:- Organizational culture (1603)
- Patient safety (29,581)
- Safety management (45,564)
- Safety culture (11,064)
- Safety climate (1256)
- Safety environment (13,538)
- Work environment (29,102)
- Search #1 or #2 or #3 or #4 or #5 or #6 or #7 with limits = 111,314
Standard precautions:- Universal precautions (21,432)
- Standard precautions (664)
- Universal precaution (41)
- Standard precaution (89)
- Occupational exposure (32,068)
- Search #1 or #2 or #3 or #4 or #5 with limits = 52,528
- Search climate and SP = (combine 18 and 12) = 5470
Personnel and setting:- Personnel hospital (17,053)
- Healthcare workers (16,583)
- Nurses (55,042)
- Doctors (30,907)
- Combine 1 or 2 or 3 or 4 = 110,254
- Hospital (1,776,550)
- Acute care (77,993)
Combine 1 or 2 = 1,803,163
Final search: Climate and SP and personnel and setting = 508
-
EBSCO/CINAHL
Limits: abstract available, peer reviewed, January 2000 to September 2014, search for term in abstract, English language
Culture:- Organizational culture (AB: abstract), 461
- Patient safety (AB), 4697
- Safety management (AB), 353
- Safety culture (AB), 321
- Safety climate (AB), 148
- Hospital culture (AB), 154
- Work environment (AB), 1946
- Organizational culture (MJ: major subject heading), 1167
- Patient safety (MJ), 3394
- Safety management (MJ), 0
- Safety culture (MJ), 0
- Safety climate (MJ), 0
- Work environment (MJ), 2378
- Attitude of health personnel (MJ), 3976
- Safety (MJ), 7376
- Hospital culture (MJ), 0
- Search #1 or #2 or #3 or #4 or #5 or #6 or #7 or #8 or #9 or #13 or #14 or #15 with limits = (S39) 19,182
Precautions:- Universal precautions (AB), 148
- Universal precautions (MJ), 73
- Universal precautions (TX: text word), 327
- Universal precaution (AB), 11
- Universal precaution (MJ), 0
- Universal precaution (TX), 12
- Standard precautions (AB), 158
- Standard precautions (MJ), 0
- Standard precautions (TX), 159
- Standard precautions (AB), 5
- Standard precautions (MJ), 0
- Standard precautions (TX), 5
- Occupational exposure (AB), 1086
- Occupational exposure (MJ), 2579
- Search #1 or #2 or #3 or #4 or #6 or #7 or #9 or #10 or #12 or #13 or #14 with limits = (S76) 3460
Adherence:- Guideline adherence (AB), 168
- Guideline adherence (TX), 2087
- Guideline adherence (MJ), 861
- Policy compliance (AB), 36
- Policy compliance (TX), 40
- Policy compliance (MJ), 0
- Compliance, protocol (MJ), 0
- Compliance, protocol (TX), 89
- Compliance, protocol (AB), 85
- Compliance, policy (MJ), 0
- Compliance, policy (TX), 57
- Compliance, policy (AB), 51
- Adherence, guideline (TX), 108
- Adherence, guideline (AB), 100
- Search #1 or #2 or #3 or #4 or #6 or #7 or #9 or #10 or #12 or #13 or #14 with limits = (S154), 2300
Final search: combine S76 and S39 = 352
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of interest statement
None declared.
References
- 1.Harbarth S, Sax H, Gastmeier P. The preventable proportion of nosocomial infections: an overview of published reports. J Hosp Infect. 2003;54:258–266. doi: 10.1016/s0195-6701(03)00150-6. quiz 321. [DOI] [PubMed] [Google Scholar]
- 2.Burke JP. Infection control – a problem for patient safety. N Engl J Med. 2003;348:651–656. doi: 10.1056/NEJMhpr020557. [DOI] [PubMed] [Google Scholar]
- 3.Gerberding JL. Hospital-onset infections: a patient safety issue. Ann Intern Med. 2002;137:665–670. doi: 10.7326/0003-4819-137-8-200210150-00011. [DOI] [PubMed] [Google Scholar]
- 4.Krein SL, Olmsted RN, Hofer TP, et al. Translating infection prevention evidence into practice using quantitative and qualitative research. Am J Infect Control. 2006;34:507–512. doi: 10.1016/j.ajic.2005.05.017. [DOI] [PubMed] [Google Scholar]
- 5.Saint S, Kowalski CP, Banaszak-Holl J, Forman J, Damschroder L, Krein SL. How active resisters and organizational constipators affect health care-acquired infection prevention efforts. Jt Comm J Qual Patient Saf. 2009;35:239–246. doi: 10.1016/s1553-7250(09)35032-1. [DOI] [PubMed] [Google Scholar]
- 6.Jeeva RR, Wright D. Healthcare-associated infections: a national patient safety problem and the coordinated response. Med Care. 2014;52:S4–S8. doi: 10.1097/MLR.0b013e3182a54581. [DOI] [PubMed] [Google Scholar]
- 7.US Department of Health and Human Services (DHHS) Office of Inspector General. [last accessed July 2015];Adverse events in hospitals: national incidence among Medicare beneficiaries. 2010 OEI Publication No, 06-09-00090; Available at: http://oig.hhs.gov/oei/reports/oei-06-09-00090.pdf.
- 8.Brown J, Doloresco F, Mylotte JM. “Never events”: not every hospital-acquired infection is preventable. Clin Infect Dis. 2009;49:743–746. doi: 10.1086/604719. [DOI] [PubMed] [Google Scholar]
- 9.Point prevalence survey of healthcare associated infections and antimicrobial use in European acute care hospitals. Stockholm: ECDC; 2013. [last accessed February 2015]. European Centre for Disease Prevention and Control. Available at: http://www.ecdc.europa.eu/en/healthtopics/healthcare-associated_infections/point-prevalence-survey/pages/point-prevalence-survey.aspx. [Google Scholar]
- 10.Zingg W, Holmes A, Dettenkofer M, et al. Hospital organisation, management, and structure for prevention of health-care-associated infection: a systematic review and expert consensus. Lancet Infect Dis. 2015;15:212–224. doi: 10.1016/S1473-3099(14)70854-0. [DOI] [PubMed] [Google Scholar]
- 11.Allegranzi B, Bagheri Nejad S, Combescure C, et al. Burden of endemic health-care-associated infection in developing countries: systematic review and meta-analysis. Lancet. 2011;377:228–241. doi: 10.1016/S0140-6736(10)61458-4. [DOI] [PubMed] [Google Scholar]
- 12.World Health Organization. [last accessed February 2015];Report on the burden of endemic health care-associated infection worldwide. 2011 Available at: http://apps.who.int/iris/bitstream/10665/80135/1/9789241501507_eng.pdf.
- 13.Zimlichman E, Henderson D, Tamir O, et al. Health care-associated infections: a meta-analysis of costs and financial impact on the US health care system. JAMA Intern Med. 2013;173:2039–2046. doi: 10.1001/jamainternmed.2013.9763. [DOI] [PubMed] [Google Scholar]
- 14.European Centre for Disease Prevention and Control. Annual epidemiological report on communicable diseases in Europe 2008. Stockholm: European Centre for Disease Prevention and Control; 2008. [last accessed February 2015]. Available at: http://www.ecdc.europa.eu/en/healthtopics/healthcare-associated_infections/point-prevalence-survey/pages/point-prevalence-survey.aspx. [Google Scholar]
- 15.Anonymous. Update: universal precautions for prevention of transmission of human immunodeficiency virus, hepatitis B virus, and other bloodborne pathogens in health-care settings. Morb Mortal Wkly Rev. 1988;37:377–382. 87–88. [PubMed] [Google Scholar]
- 16.Siegel JD, Rhinehart E, Jackson M, Chiarello L Committee HCICPA. 2007 guideline for isolation precautions: preventing transmission of infectious agents in health care settings. Am J Infect Control. 2007;35:S65–S164. doi: 10.1016/j.ajic.2007.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Erasmus V, Daha TJ, Brug H, et al. Systematic review of studies on compliance with hand hygiene guidelines in hospital care. Infect Control Hosp Epidemiol. 2010;31:283–294. doi: 10.1086/650451. [DOI] [PubMed] [Google Scholar]
- 18.Gammon J, Morgan-Samuel H, Gould D. A review of the evidence for suboptimal compliance of healthcare practitioners to standard/universal infection control precautions. J Clin Nurs. 2008;17:157–167. doi: 10.1111/j.1365-2702.2006.01852.x. [DOI] [PubMed] [Google Scholar]
- 19.Kretzer EK, Larson EL. Behavioral interventions to improve infection control practices. Am J Infect Control. 1998;26:245–253. doi: 10.1016/s0196-6553(98)80008-4. [DOI] [PubMed] [Google Scholar]
- 20.Efstathiou G, Papastavrou E, Raftopoulos V, Merkouris A. Compliance of Cypriot nurses with standard precautions to avoid exposure to pathogens. Nurs Health Sci. 2011;13:53–59. doi: 10.1111/j.1442-2018.2011.00576.x. [DOI] [PubMed] [Google Scholar]
- 21.Gershon RR, Vlahov D, Felknor SA, et al. Compliance with universal precautions among health care workers at three regional hospitals. Am J Infect Control. 1995;23:225–236. doi: 10.1016/0196-6553(95)90067-5. [DOI] [PubMed] [Google Scholar]
- 22.Godin G, Naccache H, Morel S, Ébacher M-F. Determinants of nurses’ adherence to universal precautions for venipunctures. Am J Infect Control. 2000;28:359–364. doi: 10.1067/mic.2000.107594. [DOI] [PubMed] [Google Scholar]
- 23.Mahat G, Eller LS. HIV/AIDS and universal precautions: knowledge and attitudes of Nepalese nursing students. J Adv Nurs. 2009;65:1907–1915. doi: 10.1111/j.1365-2648.2009.05070.x. [DOI] [PubMed] [Google Scholar]
- 24.Whitby M, McLaws M-L, Ross MW. Why healthcare workers don’t wash their hands: a behavioral explanation. Infect Control Hosp Epidemiol. 2006;27:484–492. doi: 10.1086/503335. [DOI] [PubMed] [Google Scholar]
- 25.Kohn LT, Corrigan JM, Donaldson MS, editors. Institute of Medicine (IOM) To err is human: building a safer health system. Washington, DC: National Academies Press; 2000. [PubMed] [Google Scholar]
- 26.Gershon RR, Stone PW, Bakken S, Larson E. Measurement of organizational culture and climate in healthcare. J Nur Admin. 2004;34:33–40. doi: 10.1097/00005110-200401000-00008. [DOI] [PubMed] [Google Scholar]
- 27.Nieva V, Sorra J. Safety culture assessment: a tool for improving patient safety in healthcare organizations. Qual Saf Health Care. 2003;12(Suppl 2):ii17–ii23. doi: 10.1136/qhc.12.suppl_2.ii17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Stone PW, Mooney-Kane C, Larson EL, et al. Nurse working conditions and patient safety outcomes. Med Care. 2007;45:571–578. doi: 10.1097/MLR.0b013e3180383667. [DOI] [PubMed] [Google Scholar]
- 29.Feng X, Bobay K, Weiss M. Patient safety culture in nursing: a dimensional concept analysis. J Adv Nur. 2008;63:310–319. doi: 10.1111/j.1365-2648.2008.04728.x. [DOI] [PubMed] [Google Scholar]
- 30.Hofmann DA, Mark B. An investigation of the relationship between safety climate and medication errors as well as other nurse and patient outcomes. Pers Psychol. 2006;59:847–869. [Google Scholar]
- 31.Sleutel MR. Climate, culture, context, or work environment? Organizational factors that influence nursing practice. J Nur Admin. 2000;30:53–58. doi: 10.1097/00005110-200002000-00002. [DOI] [PubMed] [Google Scholar]
- 32.Nelson S, Stone PW, Jordan S, et al. Patient safety climate: variation in perceptions by infection preventionists and quality directors. Interdiscipl Perspect Infect Dis. 2011:7. doi: 10.1155/2011/357121. 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.DeJoy DM, Gershon RR, Schaffer BS. Safety research – safety climate: assessing management and organizational influences on safety. Prof Saf. 2004;49:50–57. [Google Scholar]
- 34.Geiger-Brown J, Lipscomb J. The health care work environment and adverse health and safety consequences for nurses. Ann Rev Nurs Res. 2010;28:191–231. doi: 10.1891/0739-6686.28.191. [DOI] [PubMed] [Google Scholar]
- 35.DeJoy DM, Searcy CA, Murphy LR, Gershon RR. Behavior diagnostic analysis of compliance with universal precautions among nurses. J Occup Health Psychol. 2000;5:127. doi: 10.1037//1076-8998.5.1.127. [DOI] [PubMed] [Google Scholar]
- 36.Nichol K, Bigelow P, O’Brien-Pallas L, McGeer A, Manno M, Holness DL. The individual, environmental, and organizational factors that influence nurses’ use of facial protection to prevent occupational transmission of communicable respiratory illness in acute care hospitals. Am J Infect Control. 2008;36:481–487. doi: 10.1016/j.ajic.2007.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Brevidelli MM, Cianciarullo TI. Psychosocial and organizational factors relating to adherence to standard precautions. Rev Saúde Pública. 2009;43:10. doi: 10.1590/s0034-89102009010700001. [DOI] [PubMed] [Google Scholar]
- 38.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol. 2009;62:1006–1012. doi: 10.1016/j.jclinepi.2009.06.005. [DOI] [PubMed] [Google Scholar]
- 39.Anderson E, McGovern PM, Kochevar L, Vesley D, Gershon R. Testing the reliability and validity of a measure of safety climate. J Healthc Qual. 2000;22:19–24. doi: 10.1111/j.1945-1474.2000.tb00111.x. [DOI] [PubMed] [Google Scholar]
- 40.Dejoy DM, Murphy LR, Gershon RM. The influence of employee, job/task, and organizational factors on adherence to universal precautions among nurses. Int J Industr Ergonom. 1995;16:43–55. [Google Scholar]
- 41.Clarke SP, Rockett JL, Sloane DM, Aiken LH. Organizational climate, staffing, and safety equipment as predictors of needlestick injuries and near-misses in hospital nurses. Am J Infect Control. 2002;30:207–216. doi: 10.1067/mic.2002.123392. [DOI] [PubMed] [Google Scholar]
- 42.Gershon RR, Karkashian CD, Grosch JW, et al. Hospital safety climate and its relationship with safe work practices and workplace exposure incidents. Am J Infect Control. 2000;28:211–221. doi: 10.1067/mic.2000.105288. [DOI] [PubMed] [Google Scholar]
- 43.Kermode M, Jolley D, Langkham B, Thomas MS, Holmes W, Gifford SM. Compliance with universal/standard precautions among health care workers in rural north India. Am J Infect Control. 2005;33:27–33. doi: 10.1016/j.ajic.2004.07.014. [DOI] [PubMed] [Google Scholar]
- 44.Vaughn TE, McCoy KD, Beekmann SE, Woolson RE, Torner JC, Doebbeling BN. Factors promoting consistent adherence to safe needle precautions among hospital workers. Infect Control Hospl Epidemiol. 2004;25:548–555. doi: 10.1086/502438. [DOI] [PubMed] [Google Scholar]
- 45.Noah N. The STROBE Initiative STrengthening the Reporting of OBservational studies in Epidemiology (STROBE) Epidemiol Infect. 2008;136:865. doi: 10.1017/S0950268808000733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Cumbler E, Castillo L, Satorie L, et al. Culture change in infection control: applying psychological principles to improve hand hygiene. J Nurs Care Qual. 2013;28:304–311. doi: 10.1097/NCQ.0b013e31829786be. [DOI] [PubMed] [Google Scholar]
- 47.Turnberg W, Daniell W. Evaluation of a healthcare safety climate measurement tool. J Safety Res. 2008;39:563–568. doi: 10.1016/j.jsr.2008.09.004. [DOI] [PubMed] [Google Scholar]
- 48.Marziale MH1, Rocha FL, Robazzi ML, Cenzi CM, dos Santos HE, Trovó ME. Organizational influence on the occurrence of work accidents involving exposure to biological material. Revista Latino-Americana de Enfermagem. 2013;21(Special number):199–206. doi: 10.1590/s0104-11692013000700025. [DOI] [PubMed] [Google Scholar]
- 49.van Gemert-Pijnen J, Hendrix MGR, Van der Palen J, Schellens PJ. Effectiveness of protocols for preventing occupational exposure to blood and body fluids in Dutch hospitals. J Hosp Infect. 2006;62:166–173. doi: 10.1016/j.jhin.2005.07.010. [DOI] [PubMed] [Google Scholar]
- 50.Agnew C, Flin R, Mearns K. Patient safety climate and worker safety behaviours in acute hospitals in Scotland. J Safety Res. 2013;45:95–101. doi: 10.1016/j.jsr.2013.01.008. [DOI] [PubMed] [Google Scholar]
- 51.Sakamoto F, Sakihama T, Saint S, Greene MT, Ratz D, Tokuda Y. Health care-associated infection prevention in Japan: the role of safety culture. Am J Infect Control. 2014;42:888–893. doi: 10.1016/j.ajic.2014.05.018. [DOI] [PubMed] [Google Scholar]