Abstract
Objective
To determine range of bottle sizes used and examine the relationship between bottle size and total daily consumption of formula.
Methods
Cross-sectional analysis of baseline data collected as part of Greenlight, a cluster randomized trial to prevent childhood obesity at 4 pediatric resident clinics. The Greenlight study included healthy, term infants. For our analysis, parents of exclusively formula-fed infants reported volume per feed, number of feeds per day, and bottle size, which was dichotomized into “small” (< 6 ounces) or “large” (≥ 6 ounces). We identified determinants of bottle size, and then examined relationships between bottle size and volume fed with log-transformed OLS regression, adjusting for infant age, sex, birth weight, current weight, race/ethnicity, and enrollment in WIC.
Results
Of 865 participants in the Greenlight study, forty-four percent (n=378; 21.8% white, 40.6% black, 35.3% Hispanic, 2.4% other) of infants were exclusively formula-fed at 2 months. Median volume per day was 30 ounces (IQR 12) and 46.0% of infants used large bottles. Adjusted for covariates, parents using larger bottles reported feeding 4 ounces more formula per day (34.2 ounces, 95% CI: 33.5-34.9 vs. 29.7 ounces, 95% CI: 29.2-30.3, p=0.03).
Conclusions
Among exclusively formula-fed infants, use of a larger bottle is associated with parental report of more formula intake when compared with infants fed with smaller bottles. If infants fed with larger bottles receive more formula, these infants may be overfed, and, consequently, at risk for obesity.
Keywords: infant growth, bottle size, formula feeding
Introduction
Rapid weight gain in the first year of life has been associated with later obesity and cardiovascular risk, even after adjusting for birth weight, breastfeeding, gestational weight gain, maternal BMI, and maternal smoking.1-9 Risk of rapid infant weight gain may be influenced by birth weight, discordance between the infant's feeding cues and the parents' feeding behavior, early introduction of complementary foods, increased protein content of formula, and other factors.10-12 Breastfed infants demonstrate weight gain trajectories distinct from infants who are primarily bottle-fed13,14 and exclusive breastfeeding may be protective against obesity.15-17 Infant weight gain may depend on the mode of feeding (breast or bottle) rather than the type of milk given, and evidence suggests growth patterns of infants fed expressed breastmilk via bottle may be similar to infants fed formula.18 The rate and volume of intake during bottle-feeding is inherently more parent-directed and may promote overfeeding, leading to rapid weight gain and increasing the risk of obesity.19,20 Despite this potential risk, little is known regarding feeding behaviors among infants who are exclusively bottle-fed.
An emerging body of literature relates food container size to volume consumed in both adults and children.21-24 A group of low income, ethnically diverse children requested and consumed more cereal when served with a large bowl compared with a small bowl.21 A similar mechanism linking container size with volume may also exist among infants fed with bottles, yet despite marketing of bottle sizes from two ounces to over ten ounces, there is no consistent guidance available from clinicians as to appropriate size. Little is known about the relationship between bottle size and infant feeding, but using a bottle may encourage parents to finish a feed despite infant satiety, and using a larger bottle may encourage preparation of feeds that are larger in volume.
If bottle size relates to the amount of formula fed to infants, adjusting bottle size may be a way to decrease overfeeding and waste and prevent rapid infant weight gain and obesity. To our knowledge, no prior studies have evaluated the relationships between bottle size, volume of intake, and growth patterns in bottle-fed infants. We aimed to describe bottle size used at the 2-month well child visit in exclusively formula fed infants in a large cohort study and examine if there was an association between bottle size and volume of formula intake. We hypothesized that caregivers who used larger bottles would feed their infants more formula per day.
Methods
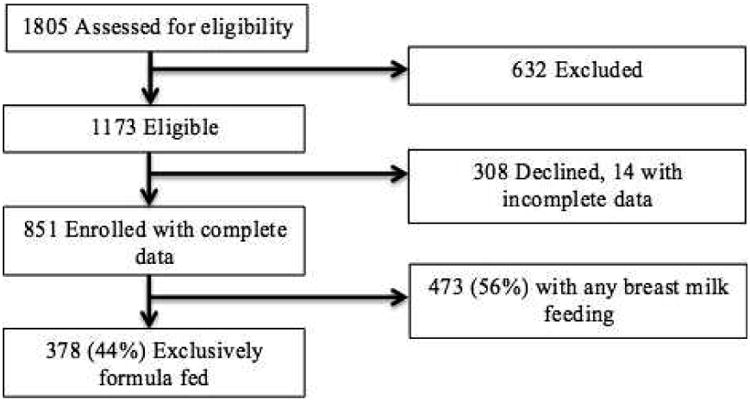
We performed a cross-sectional analysis of survey data from the Greenlight Intervention Study. The Greenlight Study is a previously described cluster randomized trial of an obesity prevention intervention targeting children during their first 2 years of life.25 Four university-affiliated pediatric clinics were randomized to either obesity prevention or injury prevention as an active control. Parent-infant dyads were followed from 2 months of age through 2 years of age, starting December 2009 and ending June 2014. Children were included in the Greenlight study if they presented for their 2 month well visit between 6 and 16 weeks of age and if caregivers spoke English or Spanish and agreed to participate until the child reached 2 years of age. Of the 1805 dyads assessed for eligibility, 632 were excluded, mainly for caregiver age, language (not English/Spanish), or plans to move outside the study area. (Figure 1) We obtained written and verbal consent from parents according to the institutional review board procedures of each of the four sites. Data were managed through secure Research Electronic Data Capture (REDCap)26 hosted at Vanderbilt University.
Figure 1. Eligibility and Enrollment Flow.
For this analysis, we used responses from a questionnaire of caregivers reporting on feeding and physical activity. Exposure and outcome variables were part of a previously reported questionnaire developed through synthesis of the literature and iterative review by content experts in measurement and in pediatric obesity. The instruments were translated by an advisory committee composed of 4 native Spanish-speaking members representing 4 nations in Latin America, who reached consensus on the appropriate terminology.27 The survey was administered in English or Spanish, at the time of the child's two-month well child check, once each clinic had been randomized, but prior to any intervention. Parents answered “What type of milk does your child drink now?” with “formula only,” “mostly formula and some breast milk,” “mostly breast milk, but some formula,” “breast milk only,” or “both equally” as options. We limited our sample to include only infants whose caregivers responded “formula only.” Infants who were currently fed from the breast in any amount were excluded because total volume could not be measured, and although infants fed expressed breast milk via bottle may exhibit similar feeding characteristics, we did not collect specific information regarding this subgroup.
Our main outcome was reported total amount of formula fed each day, which was calculated by taking the product of caregivers' responses to two questions: “In the past 24 hours, how many times was your child fed infant formula?”; “How much formula do you usually give your child at each feeding? Our main exposure measure was bottle size. At the time of measurement, we asked parents if they had a bottle that represented the bottle they typically use to feed their child. If parents did not bring their bottles to the clinic (2% of sample), they chose a sample bottle of four, six, or eight ounces as “most like the one” used to feed the infant. For analysis, we dichotomized bottle size into large (greater than or equal to six ounces) and small (less than 6 ounce) bottles, as a two month old infant of average size would be expected to take no more than 6 ounces every 3 to 4 hours.28
To assess for confounding, we examined the infant's birth weight, sex, and age in weeks, caregiver's race/ethnicity, household income, and enrollment in the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC). We examined WIC enrollment as a dichotomous variable, with enrollment defined as the infant having received WIC formula or food within the past month. We created a combined race/ethnicity variable from separate questions about race and Hispanic/Latino ethnicity, resulting in four categories: Hispanic, black non-Hispanic, other non-Hispanic, or white non-Hispanic. Annual household income was reported in five categories: less than $10,000; $10,000-19,999; $20,000-39,999; $40,000-59,999; and $60,000 and more.
We examined bivariate relationships between bottle size and potential confounders, number of feeds per day, volume per feed, and total volume per day with t-tests, Chi-square and Wilcoxon rank sum tests as appropriate, and results from nonparametric tests were not significantly different that results from parametric tests. To identify characteristics associated with size of bottle used, we used logistic regression models to examine relationships between bottle size and potential confounding variables, including race, age, sex, birth weight, household income, and WIC enrollment. In order to examine the effect of bottle size on total volume, we used an ordinary least squares regression model, adjusting for caregiver race/ethnicity, infant birth weight, age in weeks, sex, and WIC enrollment. Because of the non-normal distribution of total volume, we regressed bottle size and covariates onto log-transformed total volume. In order to ease interpretation of the log-transformed models, we report predicted total volume per day by bottle size. Retransformed predicted values are adjusted using Duan's smearing factor to correct for retransformation bias. We conducted all analyses using Stata version 13.0 (College Station, TX).
Results
In the study sample 851 infants with complete data and with a mean age of 9.3 weeks presenting for their 2-month well child visit, 44.4% (n=378) were fed exclusively with formula (Figure 1). Of these, 75.6% were black or Hispanic (Table 1). Over half of households had an annual income below $20,000, and 85.8% of infants received assistance from WIC. Overall, 54% of caregivers used a smaller (<6 ounce) bottle. The number of feeds per day ranged from 2 to 20 (mean 7.3, SD 2.6) and the number of ounces per feed ranged from 2 to 10 (mean 4.4, SD 1.3). The median (interquartile range) total volume of formula intake was 30 ounces (12).
Table 1. Characteristics of Population by Bottle Size.
| Total (N=367) | Small bottle (N=198) | Large bottle (N=169) | p | |
|---|---|---|---|---|
|
| ||||
| Mean (SD) age in weeks | 9.3 (1.8) | 9.1 (1.9) | 9.5 (1.8) | 0.03 |
|
| ||||
| Mean (SD) birth weight in kg | 3.2 (0.6) | 3.2 (0.5) | 3.3 (0.6) | 0.10 |
|
| ||||
| Mean (SD) weight-for-length z-score at birth | -0.5 (1.1) | -0.5 (1.1) | -0.4 (1.2) | 0.45 |
|
| ||||
| Current weight (SD) in kg | 5.3 (0.8) | 5.1 (0.7) | 5.4 (0.8) | 0.001 |
|
| ||||
| Current mean (SD) weight-for-length z-score | 0.2 (1.0) | 0.1 (1.0) | 0.3 (1.1) | 0.07 |
|
| ||||
| Female, % | 52.4 | 57.1 | 47.9 | 0.08 |
|
| ||||
| Race/Ethnicity, % | ||||
| Black | 41.0 | 35.9 | 47.0 | |
| Hispanic | 34.6 | 42.4 | 26.2 | 0.01 |
| White | 22.0 | 20.7 | 23.8 | |
| Other | 2.4 | 1.0 | 3.0 | |
|
| ||||
| Household income, % | ||||
| <$10,000 | 35.0 | 33.0 | 37.7 | |
| $10,000-19,999 | 26.3 | 25.5 | 27.0 | |
| $20,000-39,999 | 26.6 | 29.3 | 23.3 | 0.66 |
| $40,000-59,999 | 7.9 | 8.5 | 6.9 | |
| >$60,000 | 4.2 | 3.7 | 5.0 | |
|
| ||||
| Only child, % | 39.0 | 38.1 | 40.7 | 0.61 |
|
| ||||
| Infant WIC enrollment, % | 85.8 | 86.4 | 85.2 | 0.75 |
There were no statistically significant differences in bottle size used and birth weight, z-scores for weight-for-length at birth or 2 months, whether the infant had siblings, sex, household income or enrollment in WIC. When examining bottle size and potential confounding variables, we found older age of the infant at the visit (OR 1.1, CI: 1.0-1.3) and greater weight of the infant at this visit (OR 1.6, CI: 1.2-2.1) were significantly associated with higher odds of parents using a larger bottle. Hispanic infants had approximately half the odds of using a larger bottle when compared to white infants (OR 0.5, CI: 0.3-0.9) and when compared to black non-Hispanic infants (OR 0.5, CI: 0.3-0.8).
Feeding characteristics were significantly different between groups using a small or large bottle (Table 2). Infants using a large bottle received fewer feeds per day, but received more volume of formula with each feed, contributing to a 4-ounce difference in volume per day between those infants using a small and large bottle (29.8 vs. 33.3 ounces). Although our main analysis included a dichotomous exposure variable, when we examined bottle size in 3 categories (four, six, or eight ounces), there was a stepwise positive correlation between bottle size and both volume per feed and volume per day. The median (interquartile range) for total volume per day was similar: 30 (12) ounces. When adjusted for the infant's age, sex, birth weight, current weight, weight-for-length z-scores at birth and 2 months, race/ethnicity, enrollment in WIC, and whether the infant was an only child, there remained a meaningful and significant difference of 4 ounces in total volume of formula fed per day (Table 3).
Table 2. Feeding Characteristics by Bottle Size.
| Overall – n=371 | Small – n=201 | Large – n=170 | p | |
|---|---|---|---|---|
| Mean (SD) number of feeds per day, oz | 7.3 (2.6) | 7.6 (2.6) | 6.9 (2.4) | 0.01 |
| Mean (SD) volume per feed, oz | 4.4 (1.3) | 4.0 (1.1) | 4.8 (1.3) | <0.001 |
| Mean (SD) volume per day, oz | 31.4 (13.4) | 29.8 (12.9) | 33.3 (13.8) | 0.01 |
| Median (IQR) volume per day, oz | 30 (12) | 28 (12) | 32 (15) | 0.006* |
Wilcoxon rank-sum test
Table 3. Unadjusted and Adjusted Volume of Intake per Day.
| Small bottle | Large bottle | p | |
|---|---|---|---|
| Unadjusted, oz (95% CI) | 29.8 (28.0 – 31.7) | 33.3 (31.2 – 35.4) | 0.01 |
| Adjusted, oz (95% CI)* | 29.7 (29.2 – 30.3) | 34.2 (33.5 – 34.9) | 0.03 |
Adjusted for infant's age, sex, birth weight, current weight, weight-for-length z-score at birth and 2 months, race/ethnicity, enrollment in WIC, and whether the infant was an only child
Discussion
In this cross-sectional analysis of baseline data from a large, multi-center, cluster randomized controlled trial among infants from safety net clinics in four states, we found that bottle size at 2 months is associated with greater volume of formula intake per day, even when controlling for race/ethnicity, birth weight, sex, current weight, current age and WIC use. Infants using bottles greater than or equal to 6 ounces consume about 4 ounces more formula intake per day than infants using bottles smaller than 6 ounces, which is equivalent to an additional 80 kcal per day. In a 2 month old infant of average weight, assuming all formula is consumed and no additional caloric content is added to the bottle, this additional formula is approximately 15 kcal per kg per day. Although no previous study has examined the influence of container size on intake during infancy, our findings of a positive relationship between intake and container size are consistent with studies done in older children and adults.21,29
Past research linking bottle feeding to rapid infant weight gain has included largely white, educated families.7,18,30 Our study relates bottle size and feeding volume for infants in a low-income, ethnically diverse population who are at increased risk of developing obesity in early childhood. At this stage in their child's development, mothers are unlikely to initiate or resume breastfeeding, and these results suggest that if parents regularly use a large bottle, they may promote overfeeding. A range of 140 to 200ml/kg/day is recommended for infants less than 3 months of age,28 and although the median intake in our study population (30 ounces per day) matches the expected 170ml/kg/day for an average weight 2 month old, the range of reported intake is wide, with the 5th percentile of volume approximating 85ml/kg/day and the 95th percentile approximating 240ml/kg/day. Given a range of smallest (3.3 kg) to largest (8.5 kg) infants in our study, an extra 4 ounces per day would result in a 5 to 20% increase in daily caloric intake. Although our study is limited to infants fed exclusively with formula, the association between bottle size and volume per day may be independent of type of milk, and so infants fed breast milk by bottle may also receive additional volume. There are several reasons why infants may feed with breast milk from a bottle,31 and prospective study of infants fed breast milk via bottle may provide insight into the impact of container size vs. milk type on infant weight gain.
There are several limitations to our findings. We cannot assess causation and directionality with this cross-sectional analysis, and some infants may demand more intake, prompting parents to use a larger bottle early in life. Our data were analyzed from caregiver-reported measures based on their best estimate of feeding pattern from the most recent 24-hour period and from their most commonly used bottle size, however, additional considerations, such as the size and flow of the nipple on the bottle (not assessed in our study) may independently effect both bottle size, rate and volume of intake, and subsequent weight gain. Infant growth during this period of development is dynamic, and 24-hour recall may not be sufficient for assessing patterns in intake, because while we asked for a typical feeding volume, most infants will not consume the same volume at each feeding. Study personnel attempted to collect accurate information, yet recall of the last 24 hours is subject to bias. Although measurement of intake in this fashion fails to account for spitting up or the addition of extra calories, such as rice cereal to the bottle (only 12% percent of infants in our study), we believed that 24-hour recall would represent a generally and clinically relevant measure. Parents are likely to use multiple sizes of bottles throughout infancy, and we simply asked about the size most frequently used at the 2-month well child check. Limiting analysis to infants who are exclusively fed formula may limit external validity, but approximately 40% of breastfed infants receive some formula supplementation before they are 3 months old,32 and 44% of our original sample was exclusively formula feeding at the 2 month, baseline measurement.27
Further investigation into the influences on bottle selection and bottle-feeding behaviors is needed. Influences such as cost, food insecurity and considerations of waste, parental perception of infant weight and infant appetite, and the role of parental feeding styles must be considered to gain a full perspective of the relationship between bottle-feeding and weight gain. Particular attention should be given to the directionality of the relationship between bottle size used and an infant's weight and weight-for-length. It is possible that families select bottles dependent on the infant's age or weight, variables that we found to differ significantly by bottle size. Additionally, the perception of hunger cues and caloric needs may differ by culture, and the perception of infant appetite may be a strong influence on parental feeding styles, resulting in changes to bottle-feeding behaviors or bottle sizes used throughout infancy.
Most infants in the United States will be fed with a bottle, and understanding the feeding behaviors related to different size bottles can therefore be useful for the majority of infants and children. Although there is little data on where and how families select bottles for infant feeding, a wide variety of bottles are marketed. Bottles larger than 6 ounces may not be necessary to feed 2 month-old infants, but it is possible that many families prefer to buy a large bottle once as opposed to buying multiple bottles as their child “outgrows” his or her first bottle. Some families may purchase bottles in bulk or from stores where larger bottles are either less expensive or more prominently displayed. It is also possible these families are reusing bottles from prior older siblings. It is important to note that although educational interventions that encourage recognition of hunger and satiety cues may promote more infant-directed bottle feeding,33 simply intervening at the moment the bottle is purchased or provided may decrease overfeeding by caregivers. Similar interventions to alter environmental influences on portion size are being studied in children and adults,34 and our findings provide the first step to extend this approach and modify risk in the first year of life. Our study should encourage future studies to assess bottle size's impact on consumption and weight gain through prospective and experimental methods.
Conclusion
We found that a number of caregivers use larger bottles to feed their 2 month old infants and that the volume of formula fed per day increases as bottle size increases, adjusting for confounders. In order to understand healthy growth in infants who are fed by bottle, further research is needed to determine whether use of larger bottles predicts infant obesity or rapid weight gain, and whether providing a smaller bottle would prevent excessive weight gain in infancy. This research may also have implications for community-based interventions, including partnerships with WIC and with private vendors of infant bottles, to prevent childhood obesity. Although clinicians should always encourage exclusive breastfeeding in the first six months of life, if families choose to feed with a bottle, encouraging use of a smaller bottle may help promote healthier growth that more closely resembles the breastfed infant.
What's New.
Larger bottle size is associated with more reported formula intake over a 24-hour period. If infants using larger bottles are prone to be overfed and thus at risk for obesity, reducing bottle size may be an intervention to prevent obesity.
Acknowledgments
Funding: The study was supported by NIH/NICHD (R01HD059794) supplemented by with CDC (04S1 and 04S2). Additional support was provided by NIH CTSA grants UL1TR001111, UL1TR000445 and by NIH/NCRR U54RR023499, UL1RR025747, UL1TR000038. Dr. Yin was supported in part by a grant under the Robert Wood Johnson Foundation Physician Faculty Scholars Program, and Dr. Wood is supported by the University of North Carolina Primary Care Research Fellowship (HRSA 5T32HP014001).
Footnotes
Disclosure: The authors have no conflicts of interest to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Asheley C. Skinner, Email: asheley@unc.edu.
H. Shonna Yin, Email: hsiang.yin@nyumc.org.
Russell L. Rothman, Email: Russell.rothman@vanderbilt.edu.
Lee M. Sanders, Email: leesanders@stanford.edu.
Alan Delamater, Email: adelamater@med.miami.edu.
Sophie N. Ravanbakht, Email: snravan@live.unc.edu.
Eliana M. Perrin, Email: eliana_perrin@med.unc.edu.
References
- 1.Ong KK, Loos RJ. Rapid infancy weight gain and subsequent obesity: systematic reviews and hopeful suggestions. Acta paediatrica (Oslo, Norway : 1992) 2006 Aug;95(8):904–908. doi: 10.1080/08035250600719754. [DOI] [PubMed] [Google Scholar]
- 2.Stettler N, Zemel BS, Kumanyika S, Stallings VA. Infant weight gain and childhood overweight status in a multicenter, cohort study. Pediatrics. 2002 Feb;109(2):194–199. doi: 10.1542/peds.109.2.194. [DOI] [PubMed] [Google Scholar]
- 3.Eid EE. Follow-up study of physical growth of children who had excessive weight gain in first six months of life. British medical journal. 1970 Apr 11;2(5701):74–76. doi: 10.1136/bmj.2.5701.74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Baird J, Fisher D, Lucas P, Kleijnen J, Roberts H, Law C. Being big or growing fast: systematic review of size and growth in infancy and later obesity. BMJ (Clinical research ed) 2005 Oct 22;331(7522):929. doi: 10.1136/bmj.38586.411273.E0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Druet C, Stettler N, Sharp S, et al. Prediction of childhood obesity by infancy weight gain: an individual-level meta-analysis. Paediatric and perinatal epidemiology. 2012 Jan;26(1):19–26. doi: 10.1111/j.1365-3016.2011.01213.x. [DOI] [PubMed] [Google Scholar]
- 6.Skilton MR, Marks GB, Ayer JG, et al. Weight gain in infancy and vascular risk factors in later childhood. Pediatrics. 2013 Jun;131(6):e1821–1828. doi: 10.1542/peds.2012-2789. [DOI] [PubMed] [Google Scholar]
- 7.Taveras EM, Rifas-Shiman SL, Sherry B, et al. Crossing growth percentiles in infancy and risk of obesity in childhood. Archives of pediatrics & adolescent medicine. 2011 Nov;165(11):993–998. doi: 10.1001/archpediatrics.2011.167. [DOI] [PubMed] [Google Scholar]
- 8.Taveras EM, Rifas-Shiman SL, Belfort MB, Kleinman KP, Oken E, Gillman MW. Weight status in the first 6 months of life and obesity at 3 years of age. Pediatrics. 2009 Apr;123(4):1177–1183. doi: 10.1542/peds.2008-1149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dennison BA, Edmunds LS, Stratton HH, Pruzek RM. Rapid infant weight gain predicts childhood overweight. Obesity (Silver Spring, Md) 2006 Mar;14(3):491–499. doi: 10.1038/oby.2006.64. [DOI] [PubMed] [Google Scholar]
- 10.Escribano J, Luque V, Ferre N, et al. Effect of protein intake and weight gain velocity on body fat mass at 6 months of age: the EU Childhood Obesity Programme. International journal of obesity (2005) 2012 Apr;36(4):548–553. doi: 10.1038/ijo.2011.276. [DOI] [PubMed] [Google Scholar]
- 11.Wright CM, Cox KM, Sherriff A, Franco-Villoria M, Pearce MS, Adamson AJ. To what extent do weight gain and eating avidity during infancy predict later adiposity? Public health nutrition. 2012 Apr;15(4):656–662. doi: 10.1017/S1368980011002096. [DOI] [PubMed] [Google Scholar]
- 12.Mihrshahi S, Battistutta D, Magarey A, Daniels LA. Determinants of rapid weight gain during infancy: baseline results from the NOURISH randomised controlled trial. BMC pediatrics. 2011;11:99. doi: 10.1186/1471-2431-11-99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.van Dijk CE, Innis SM. Growth-curve standards and the assessment of early excess weight gain in infancy. Pediatrics. 2009 Jan;123(1):102–108. doi: 10.1542/peds.2007-3382. [DOI] [PubMed] [Google Scholar]
- 14.de Onis M, Garza C, Onyango AW, Borghi E. Comparison of the WHO child growth standards and the CDC 2000 growth charts. The Journal of nutrition. 2007 Jan;137(1):144–148. doi: 10.1093/jn/137.1.144. [DOI] [PubMed] [Google Scholar]
- 15.Owen CG, Martin RM, Whincup PH, Smith GD, Cook DG. Effect of infant feeding on the risk of obesity across the life course: a quantitative review of published evidence. Pediatrics. 2005 May;115(5):1367–1377. doi: 10.1542/peds.2004-1176. [DOI] [PubMed] [Google Scholar]
- 16.Owen CG, Martin RM, Whincup PH, Davey-Smith G, Gillman MW, Cook DG. The effect of breastfeeding on mean body mass index throughout life: a quantitative review of published and unpublished observational evidence. The American journal of clinical nutrition. 2005 Dec;82(6):1298–1307. doi: 10.1093/ajcn/82.6.1298. [DOI] [PubMed] [Google Scholar]
- 17.Disantis KI, Collins BN, Fisher JO, Davey A. Do infants fed directly from the breast have improved appetite regulation and slower growth during early childhood compared with infants fed from a bottle? The international journal of behavioral nutrition and physical activity. 2011;8:89. doi: 10.1186/1479-5868-8-89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Li R, Magadia J, Fein SB, Grummer-Strawn LM. Risk of bottle-feeding for rapid weight gain during the first year of life. Archives of pediatrics & adolescent medicine. 2012 May;166(5):431–436. doi: 10.1001/archpediatrics.2011.1665. [DOI] [PubMed] [Google Scholar]
- 19.Butte NF, Wong WW, Hopkinson JM, Smith EO, Ellis KJ. Infant feeding mode affects early growth and body composition. Pediatrics. 2000 Dec;106(6):1355–1366. doi: 10.1542/peds.106.6.1355. [DOI] [PubMed] [Google Scholar]
- 20.Dewey KG, Heinig MJ, Nommsen LA, Peerson JM, Lonnerdal B. Breast-fed infants are leaner than formula-fed infants at 1 y of age: the DARLING study. The American journal of clinical nutrition. 1993 Feb;57(2):140–145. doi: 10.1093/ajcn/57.2.140. [DOI] [PubMed] [Google Scholar]
- 21.Wansink B, van Ittersum K, Payne CR. Larger Bowl Size Increases the Amount of Cereal Children Request, Consume, and Waste. The Journal of pediatrics. 2013 Nov 16; doi: 10.1016/j.jpeds.2013.09.036. [DOI] [PubMed] [Google Scholar]
- 22.Wansink B. Environmental factors that increase the food intake and consumption volume of unknowing consumers. Annual review of nutrition. 2004;24:455–479. doi: 10.1146/annurev.nutr.24.012003.132140. [DOI] [PubMed] [Google Scholar]
- 23.DiSantis KI, Birch LL, Davey A, et al. Plate size and children's appetite: effects of larger dishware on self-served portions and intake. Pediatrics. 2013 May;131(5):e1451–1458. doi: 10.1542/peds.2012-2330. [DOI] [PubMed] [Google Scholar]
- 24.Wansink B, van Ittersum K, Painter JE. Ice cream illusions bowls, spoons, and self-served portion sizes. American journal of preventive medicine. 2006 Sep;31(3):240–243. doi: 10.1016/j.amepre.2006.04.003. [DOI] [PubMed] [Google Scholar]
- 25.Sanders LM, Perrin EM, Yin HS, Bronaugh A, Rothman RL. “Greenlight study”: a controlled trial of low-literacy, early childhood obesity prevention. Pediatrics. 2014 Jun;133(6):e1724–1737. doi: 10.1542/peds.2013-3867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. Journal of biomedical informatics. 2009 Apr;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Perrin EM, Rothman RL, Sanders LM, et al. Racial and Ethnic Differences Associated With Feeding- and Activity-Related Behaviors in Infants. Pediatrics. 2014 Mar 17; doi: 10.1542/peds.2013-1326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nutrition ACo. Pediatric Nutrition Handbook. Sixth. Elk Grove Village, IL: American Academy of Pediatrics; 2008. [Google Scholar]
- 29.Wansink B, Cheney MM. Super Bowls: serving bowl size and food consumption. JAMA : the journal of the American Medical Association. 2005 Apr 13;293(14):1727–1728. doi: 10.1001/jama.293.14.1727. [DOI] [PubMed] [Google Scholar]
- 30.Taveras EM, Gillman MW, Kleinman KP, Rich-Edwards JW, Rifas-Shiman SL. Reducing racial/ethnic disparities in childhood obesity: the role of early life risk factors. JAMA pediatrics. 2013 Aug 1;167(8):731–738. doi: 10.1001/jamapediatrics.2013.85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Whitaker RC, Wright JA. Why feed breast milk from a bottle? Archives of pediatrics & adolescent medicine. 2012 May;166(5):483–484. doi: 10.1001/archpediatrics.2012.275. [DOI] [PubMed] [Google Scholar]
- 32.CDC. Breastfeeding Among U.S. Children Born 2000-2010, CDC National Immunization Survey. [Accessed March 22, 2014];2013 http://www.cdc.gov.libproxy.lib.unc.edu/breastfeeding/data/nis_data/
- 33.Kavanagh KF, Cohen RJ, Heinig MJ, Dewey KG. Educational intervention to modify bottle-feeding behaviors among formula-feeding mothers in the WIC program: impact on infant formula intake and weight gain. Journal of nutrition education and behavior. 2008 Jul-Aug;40(4):244–250. doi: 10.1016/j.jneb.2007.01.002. [DOI] [PubMed] [Google Scholar]
- 34.Robinson TN, Matheson D, Desai M, et al. Family, community and clinic collaboration to treat overweight and obese children: Stanford GOALS-A randomized controlled trial of a three-year, multi-component, multi-level, multi-setting intervention. Contemporary clinical trials. 2013 Nov;36(2):421–435. doi: 10.1016/j.cct.2013.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]


