Abstract
The impact of Motivational Interviewing (MI) on risky behaviors of incarcerated adolescents and adults have been investigated with promising results. Findings suggest MI reduces substance use, improves motivation and confidence to reduce use, and decreases risky behaviors. The current study investigated the impact of MI on general, alcohol-related, and marijuana-related delinquent behaviors in incarcerated adolescents. Participants in the study were incarcerated adolescents in a state correctional facility in the Northeast region and were assessed as part of a larger randomized clinical trial. Adolescents were randomly assigned to receive MI or relaxation therapy (RT) (N=189) treatment. Delinquent behaviors and depressive symptomatology were measured using the Delinquent Activities Scale (DAS; Reavy, Stein, Paiva, Quina, & Rossi, 2012) and the Center for Epidemiological Studies-Depression scale (CES-D; Radloff, 1991) respectively. Findings indicate depression moderated treatment effects. Compared to RT, MI was better at reducing predatory aggression and alcohol-related predatory aggression 3 months post-release when depressive symptoms were low. Identifying an efficacious treatment for these adolescents may benefit society in that it may decrease crimes against persons (i.e., predatory aggression) post release.
1. Introduction
Juvenile offenders’ crimes are often connected to alcohol and drug use (Mulvey, Schubert, & Chassin, 2010; National Institute of Justice [NIJ], 1997; 2003), and lifetime prevalence of alcohol and marijuana use among juvenile offenders is 80% and 85% respectively, with 40% consuming alcohol and 57% using marijuana in the past 6 months (Mulvey et al., 2010). Additionally, greater use of substances is related to increased rates of offending, severity of the offense, and the duration of delinquent behaviors (Greenwood, 1992; Lipsey & Derzon, 1998; Sealock, Gottfredson, & Gallagher, 1997). Of particular concern is the relationship between substance use and violent crime that exists within this population (Mulvey et al., 2010). Among incarcerated juveniles, alcohol use is significantly and consistently associated with violent crime, including acts of predatory aggression (i.e., crimes against a person such as aggression involving a weapon) (Lennings, Copeland, & Howard, 2003).
Adolescents with substance use disorders commonly suffer from depression (Colder & Chassin, 1997; Myers, Aarons, Tomlinson, & Stein, 2003; Shoal & Giancola, 2003; Stice, Myers, & Brown, 1998). This comorbidity is associated with progression to problematic substance use (Rhode, Lewinsohn, & Seeley, 1996), failure in school, and increased risk of attempted suicide (Lewinsohn, Rhode, & Seeley, 1995). Adolescents involved in the juvenile justice system experience depression at a high rate (29.6%; Teplin, Abram, McClelland, Dulcan, & Mericle, 2002), and the comorbidity of depression and substance use is also high among these adolescents (Esposito-Smythers, Penn, Stein, Lacher-Katz, & Spirito, 2008; Turner, Larimer, Sarason, & Trupin, 2005), ranging from 21–73% (Abram, Teplin, McClelland, & Dulcan, 2003).
Riggs and colleagues (2008) reviewed three studies investigating the use of pharmacotherapy in adolescents with comorbid psychiatric disorders (including depression) and substance use disorders with results suggesting that some medications may be safe and effective for adolescents but are not likely to impact substance use without behavioral therapy (Geller et al., 1998; Riggs, Hall, Mikulich-Gilbertson, Lohman, & Kayser, 2004; Riggs, Mikulich-Gilbertson, Lohman, Klein, Stover, 2007). Similarly, Cornelius and colleagues (2005a, 2005b, 2009, 2011a, 2001b, 2013) found acute and long-term efficacy for Motivational Enhancement Therapy/Cognitive-Behavioral Therapy (MET/CBT) but not fluoxetine for treating depressive symptoms and alcohol use with substance-abusing youth. This body of work strongly suggests that behavioral intervention is an important aspect of treating depressive symptoms in substance abusing youth.
More recently, Hersh and colleagues (2014) reviewed the literature to investigate the impact of depression on adolescent substance abuse treatment retention and outcomes, and the findings were varied. Seven studies found a positive association with depression and retention or outcomes (Becker, Curry, & Yang, 2011; Deskovitz, Key, Hill, & Franklin, 2004; Hersh, Curry, & Becker, 2013; Pagnin, de Queiroz, & Saggese, 2005; Stein et al., 2011a; Stein et al., 2011b; Tapert et al., 2003) while five studies found a negative relationship with depression and retention or outcomes (Cornelius et al., 2004; Stein et al., 2011b; Tapert et al., 2003; Vourakis 2005; White et al., 2004), and yet six studies found that depression did not have any influence on retention or outcomes (Becker, Curry, & Yang, 2011; Crowley, Mikulich, MacDonald, Young, & Zerbe, 1998; deDios, 2007; Tapert et al.,2003; White et al.,2004; Whitmore, Mikulich, Ehlers, & Crowley, 2000; note: some studies reported interactions or multiple outcomes so they are identified in more than one category). Given the inconclusive findings regarding the relationship of depression and substance use treatment outcomes, Hersh and colleagues (2014) suggested this relationship be further examined.
Motivational Interviewing (MI) is a client centered approach directed at exploring and resolving ambivalence in making a behavior change (Miller and Rollnick, 2002), and several meta-analysis indicate a strong evidence base in the areas of addictive health behaviors (Burke, Arkowitz, Menchola, 2003; Hettema, Steele, Miller, 2005; Lundahl et al., 2013; Lundahl, & Burke, 2009; Lundahl, Kunz, Brownell, Tollefson, & Burke 2010). A recent review of evidence-based outpatient treatment for adolescent substance users (Hogue, Henderson, Ozechowski, & Robbins, 2014) found little support for MI-based stand-alone interventions (Baer, Garrett, Beadnell, Wells, & Peterson, 2007; Gmel, Venzin, Marmet, Danko, & Labhart, 2012; Walker et al., 2011; Walker, Roffman, Stephens, Berghuis, & Kim, 2006). However, some relatively recent meta-analyses of adolescent substance use outpatient treatment studies found support for MI-based interventions (Bender, Tripodi, Sarteschi, & Vaugn, 2011; Jensen, Cushing, Aylward, Craig, Sorell, & Steele, 2011; Tanner-Smith, Wilson, & Lipsey, 2013). Regarding justice-involved adolescents, MI-based interventions have been found to increase motivation and confidence to reduce substance use and risky behaviors, increase rates of retention and treatment, and decrease negative treatment engagement (McMurran, 2009; Osilla, Miles, Pedersen, Ortiz, Houck, & D’Amico, 2015; Sinha, Easton, Renee-Aubin, & Carroll, 2003; Slavet et al., 2005; Stein et al., 2006b; Stein & Lebeau-Craven, 2002). Importantly, among these youth, MI-based interventions have been found to decrease alcohol and other substance use (D’Amico, Hunter, Miles, Ewing, Osilla, 2013; Stein et al., 2011b) and risky behaviors related to alcohol and marijuana use (Schmiege, Broaddus, Levin, & Bryan, 2009; Stein et al., 2011a; Stein et al., 2006a).
Some findings also suggest MI-based interventions may work well with adolescents and adults with emotional dysregulation such as anger (Barrett, Slenick, Brody, Turner, & Peterson, 2001-adolescents; Karno & Longabaugh, 2004-adults) and depression (Colby et al., 1998; Connell & Dishion, 2008; Cornelius et al., 2013). Within a juvenile-justice population, MI reduced rates of alcohol and marijuana use at follow-up compared to relaxation training with evidence of moderating effects of depression; at low levels of depression, MI resulted in lower rates of use (Stein et al., 2011b) 3 months after release. Similarly, adolescents low in depressive symptoms that received MI had lower rates of risky behaviors (e.g., drinking and driving and risky sexual behaviors while using marijuana and alcohol) 3 months post release compared to those adolescents that received Relaxation Therapy (RT) (Rosengard et al., 2007; Stein et al., 2006b)
Giving these findings, it seems possible that mood may influence treatment response in incarcerated juveniles. The combination of incarceration and low depressive symptoms may assist in eliciting ambivalence about their behaviors associated with delinquency and incarceration (Stein et al., 2006b) while more severe depressive symptoms may hinder the capability to attend to the intervention or mobilize resources. Thus, the current study investigated potential moderation effects of depressed mood on treatment in reducing alcohol- and marijuana-related delinquent behaviors among incarcerated adolescents after release. Specifically, we hypothesized that compared to RT, MI will be better at reducing alcohol- and marijuana-related delinquent behaviors when depressive symptoms are low. This study adds to the literature and our own line of research in that the outcome of interest is involvement in crime. We know of no other studies examining this in incarcerated youth.
2. Methods
These data were collected as part of a parent study that examined the impact of MI on substance use (Stein et al., 2011b) and although the methodology for this study are described below, additional information can be found in Stein et al. (2011b).
2.1 Procedures
Adolescents were recruited from a state juvenile correctional facility in the Northeast over a five-year period. Immediately upon adjudication, adolescents were identified as potential participants, via record review, if they were 14 to 19 years of age and sentenced to the facility for 4 to 12 months. Next, adolescents were approached individually to determine eligibility based on meeting any of the following substance use criteria: 1) in the year prior to incarceration they 1a) used marijuana or drank at least monthly, or 1b) they binge-drank (≥5 standard drinks for boys, ≥4 for girls) at least once; 2) they used marijuana or drank in the 4 weeks before the offense for which they were incarcerated; or 3) they used marijuana or drank in the 4 weeks before they were incarcerated.
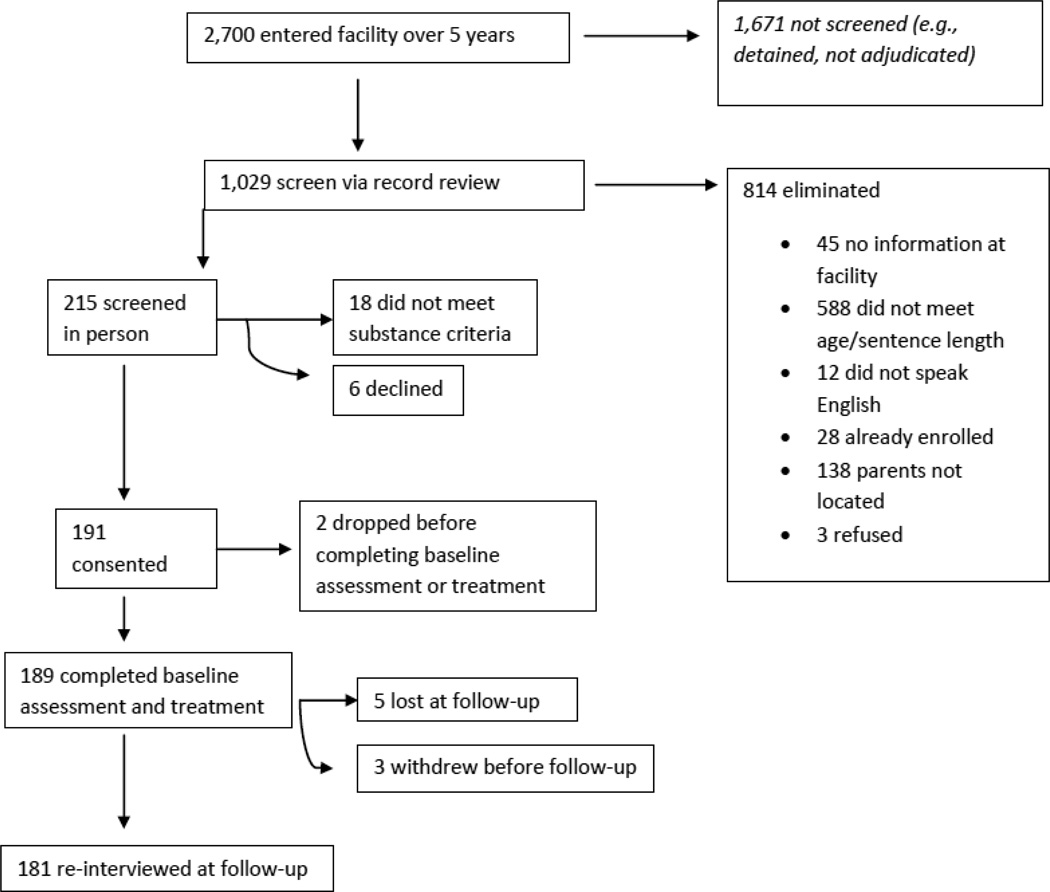
After guardian consent and adolescent assent (<18 years of age) were obtained, a baseline assessment was conducted, followed by random assignment to treatment (MI or RT), which occurred within about 4 days of the assessment. Adolescents then enrolled in the facility’s standard of care substance use programming (a detailed description of this programming can be found in Stein et al., 2011b). Approximately 2 weeks prior to release, participants received a booster intervention (MI or RT). Follow-up assessment occurred 3 months post-release. Average length of incarceration was approximately 6 months (M=188 days, SD=80), average length of time between baseline intervention and 3 month follow-up was approximately 8 months (M=244.64, SD=91.33), and average length of time from booster intervention to 3 month follow-up was approximately 4 months (M=122.51, SD=52.33). Institutional Review Board approval from Brown University was obtained. Figure 1 illustrates screening, recruitment, and retention (i.e., CONSORT diagram).
Figure 1.
CONSORT DIAGRAM
2.2 Participants
The participants were sentenced at the state’s sole juvenile correctional facility where charges range from truancy to murder. At baseline, 189 adolescents completed the assessment. At 3-month post-release follow-up, 181 were re-interviewed; five could not be located for follow-up and three withdrew from the study prior to follow-up (see CONSORT diagram). Almost 86% were boys, the mean age at baseline was 17.12 years (SD = 1.10), and participants identified with the following racial/ethnic backgrounds: 32.8% White, 29.1% Hispanic, 28.0% African American, 3.7% Native-American, 3.2% Asian-American, and 3.2% “other.” Almost 90% met criteria for a marijuana use disorder and 63% met criteria for an alcohol use disorder in the previous year.
2.3 Assessments
The baseline and 3 month follow-up assessment consisted of 60–90 minute interviews conducted by a trained bachelor’s or master’s-level research assistant. Research assistants received approximately 20 hours of training with 1 hour of individual and 1 hour of group supervision per week. In-vivo observations were conducted by a licensed psychologist and assessment data was reviewed by a licensed psychologist or master’s level project member. Participants received a $60 gift card at follow-up and a bonus $10 gift card if it was completed within one week of its scheduled date.
2.4. Interventions
After the baseline assessment (approximately 4 days later), adolescents were randomly assigned via random numbers table to one of two treatment conditions, MI (N=99) or RT (N=90), to prepare them for the facility standard care substance abuse treatment. Each intervention (either MI or RT) was delivered during one session (90 minutes) before entering standard care substance use programming and one follow up booster session (60 minutes) approximately 2 weeks prior to release. For both interventions (MI and RT), research counselors had about 56 hours of manualized training with two hours of group and one hour of individual supervision per week. Research counselors were two men and two women; all were Caucasian; one had an MA degree and three had BA/BS degrees. Each research counselor conducted intervention types, MI and RT.
The MI intervention was based on the basic principles of MI (Miller and Rollnick, 2002) and focused on four components: establishing rapport, assessing motivation to change alcohol and marijuana use, enhancing motivation to change, and establishing goals to assist in making changes. Elements of the MI included developing rapport, decisional balance, personalized assessment feedback, imagining the future with and without change, and establishing goals. The intervention targeted reducing alcohol and/or marijuana use and associated risky behaviors and related consequences (e.g., injuries while using alcohol and/or marijuana).
The RT intervention was designed to control for the effects of attending an individual intervention. Participants were instructed by research counselors in progressive muscle relaxation and use of imagery to produce a sense of calm. Research counselors maintained rapport and provided generalized advice to stop risky activities involving substances including alcohol and marijuana use. The rationale for RT provided to the adolescents was that these techniques can reduce the stress that often leads to substance use and may ultimately lead to reduced substance use and the associated delinquent behaviors.
2.5 Intervention fidelity
Counselors received manualized training, treatment manuals, regular supervision, regular file reviews, and random in-vivo observations by a licensed clinical psychologist to maintain intervention fidelity. The psychologist completed an observer fidelity measure (see O’Leary-Tevyaw and Monti, 2004 for additional details), and every session the counselor and adolescent independently and privately completed similar fidelity measures (see Stein et al., 2011b for a detailed description of these fidelity procedures and measures).
2.6 Measures
At baseline assessment, a background questionnaire was administered that included gender, age, ethnicity/race, and mother’s education level (a marker for socio-economic status).
The Center for Epidemiological Studies-Depression scale (CES-D; Radloff, 1991) was administered. Reliability coefficients on the CES-D for alcohol abusers range from .85–.90, and it is reliable and valid for use with adolescents (Radloff, 1991). Scores of 16 or greater indicate presence of significant depressive symptomatology (Radloff, 1977).
The Delinquent Activities Scale (DAS; Reavy et al., 2012) is a 37-item questionnaire based on the works of Dembo and colleagues (1992; 1993), Elliott and colleagues (1983), and on symptoms of conduct and antisocial personality disorders as found in the Diagnostic and Statistics Manual-IV-TR (American Psychiatric Association, 1994). At baseline, adolescents were asked the number of times each crime or misbehavior was committed over the 12 months prior to incarceration. These behaviors ranged from truancy to forced sexual activity. Adolescents were also asked the number of times each was committed while under the influence of alcohol or to obtain alcohol; this procedure was repeated for marijuana. Six scales assessed delinquent behaviors and included: Alcohol-related Predatory Aggression (i.e., crimes against a person such as aggression involving a weapon while under the influence of alcohol); alcohol-related Stealing/Delinquency (e.g., ran away from home overnight while under the influence of alcohol); marijuana-related Predatory Aggression (i.e., crimes against a person such as aggression involving a weapon while under the influence of marijuana); marijuana-related Stealing/Delinquency (e.g., ran away from home overnight while under the influence of marijuana); general Predatory Aggression (i.e., crimes against a person such as using a weapon); and general Stealing/Delinquency (e.g., ran away from home overnight). These scales evidence good concurrent and predictive validity and internal consistencies ranging from .422 to .843 (Reavy et al., 2012).
Substance abuse or dependence diagnoses were made using the criteria of the Structured Clinical Interview for DSM-IV Axis I Disorders - Patient Edition (First, Spitzer, Gibbon, & Williams, 1995), administered by trained research staff.
In an effort to enhance honesty about of self-reported alcohol/marijuana use and illegal activities, at the onset of the study participants were informed that records would be reviewed to verify self-report, and urinalysis was conducted at 3 month follow-up to assess marijuana and alcohol use.
2.7 Analyses
Moderation analyses to determine the impact of depressed mood on treatment to reduce predatory aggression and stealing/delinquency in general and associated with alcohol and marijuana use specifically followed (Edwards & Lambert, 2007; Preacher, Rucker, & Hayes 2007) using the PROCESS macro for SPSS (Hayes, 2012). The six MBQ scales at 3 month follow-up were the dependent variables in separate moderation models. Treatment group and the moderator were centered. The PROCESS model included the corresponding baseline measure of the MBQ scale DV, treatment group, CES-D, and the treatment by CES-D interaction. Following a significant moderator by treatment interaction, simple slopes analyses (Cohen, Cohen, West, & Aiken, 2003) examined effects of treatment on the dependent variables (predatory aggression and stealing/delinquency at follow-up) at low (−1SD below the mean), average (mean) and high (+ 1 SD from the mean) levels of depressed mood.
3. Results
3.1 Preliminary results
Almost 90% of participants met criteria for a marijuana use disorder and 63% met criteria for an alcohol use disorder in the previous year. Table 1 presents participant demographics and depression variables at baseline and substance use at baseline and 3 month follow-up. No significant differences were found between treatment groups on baseline variables including gender, age, ethnicity/race, or mother’s education level (a marker for socio-economic status).
Table 1.
Participant Characteristics and Substance Use. N=181
| Variable | Baseline Mean (SD) or % |
3-Month Follow- up Mean (SD) or % |
t (df) |
|---|---|---|---|
| Age in years | 17.11 (1.10) | ||
| Education (years) | 9.22 (1.26) | ||
| CES-D | 20.96 (10.28) | ||
| Race –white | 32.8% | ||
| Race – black | 28.0% | ||
| Race – Native American | 3.7% | ||
| Race – Asian American | 3.2% | ||
| Race – other | 3.2% | ||
| Hispanic | 29.1% | ||
| Male | 85.7% | ||
| % drinking days | 18.62 (23.64) | 8.48 (14.58) | 4.23 (161)* |
| % heavy drinking days | 13.91 (22.49) | 6.49 (13.84) | 5.22 (161)* |
| % marijuana use days | 69.32 (37.76) | 39.93 (41.02) | 8.89 (161)* |
CES-D = Center for Epidemiological Studies – Depression Scale
Baseline N=181
3-Month substance use N=162
p ≤ .001
A review of facility records found no discrepancy between self-reported-marijuana non-use and the chart and only 1% discrepancy for self-reported alcohol non-use and the chart. Over 20% of adolescents self-reported marijuana and alcohol use that was not found in the chart. Less than 5% of adolescents that indicated they did not use marijuana in the previous month had positive urine screens while about 8% self-reported marijuana use but had negative urine screens.
3.2 General delinquent behaviors
Table 2 presents results of the models assessing depressed mood as a moderator of treatment and general stealing/delinquency and predatory aggression. Models predicting general stealing/delinquency found no significant main effects for treatment or depression or treatment by depression interaction. Models predicting predatory aggression found no significant main effects for treatment or depression. The treatment by depressive symptoms interaction significantly predicted 3 month general predatory aggression. Predatory aggression differed for RT versus MI when depressive symptoms were below the mean, but not at the mean or above the mean. Compared to RT, MI is better at reducing predatory aggression when depressive symptoms are low.
Table 2.
Moderation model for predicting general, alcohol related, and marijuana related stealing/delinquency and predatory aggression at 3 month follow-up. N=181
| B | SE | 95% Confidence Interval |
t | p- value |
||
|---|---|---|---|---|---|---|
| General Stealing/Delinquency | ||||||
| Intercept | .23 | .13 | −.14 | 1.29 | ||
| Pretreatment Stealing/Delinquency | .17 | .04 | .21 | .42 | 4.69 | .001 |
| Treatment group | .18 | .15 | −.11 | .47 | 1.22 | .22 |
| CES-D | −.01 | .02 | −.03 | .01 | 1.55 | .12 |
| Treatment X CES-D | .01 | .01 | −.02 | .03 | .30 | .77 |
| General Predatory Aggression | ||||||
| Intercept | .57 | .36 | −.14 | 1.29 | ||
| Pretreatment predatory aggression | .31 | .05 | .21 | .42 | 5.85 | .001 |
| Treatment group | −.20 | .35 | −.89 | .50 | .57 | .57 |
| CES-D | −.03 | .02 | −.06 | .01 | 1.73 | .08 |
| Treatment X CES-D | .08 | .03 | .01 | .15 | 2.38 | .02 |
| Simple slopes tests of Treatment X CES-D: |
||||||
| Effect of treatment group at −1SD mean CES-D |
−1.04 | .51 | −2.05 | −.04 | 2.06 | .04 |
| Effect of treatment group at mean CES-D |
−.20 | .35 | −.89 | .50 | .57 | .57 |
| Effect of treatment group at +1SD mean CES-D |
.64 | .49 | −.32 | 1.61 | 1.31 | .19 |
| Alcohol Stealing/Delinquency | ||||||
| Intercept | .22 | .10 | .02 | .42 | ||
| Pretreatment alcohol stealing/delinquency |
.15 | .02 | .10 | .20 | 6.22 | .001 |
| Treatment group | −.01 | .15 | −.07 | .95 | .07 | .94 |
| CES-D | −.03 | .02 | −.03 | −.01 | 2.45 | .02 |
| Treatment X CES-D | .02 | .01 | −.01 | .05 | 1.34 | .18 |
| Alcohol Predatory Aggression | ||||||
| Intercept | .10 | .12 | −.15 | .34 | ||
| Pretreatment alcohol related predatory aggression |
.19 | .04 | .12 | .26 | 5.27 | .001 |
| Treatment group | −.31 | .19 | −.69 | .07 | 1.63 | .10 |
| CES-D | −.02 | .01 | −.04 | −.01 | 2.12 | .04 |
| Treatment X CES-D | .04 | .02 | .01 | .08 | 2.04 | .04 |
| Simple slopes tests of Treatment X CES-D: |
||||||
| Effect of treatment group at −1SD mean CES-D |
−.71 | .27 | −1.25 | −.17 | 2.58 | .01 |
| Effect of treatment group at mean CES-D |
−.31 | .19 | −.69 | .07 | 1.63 | .10 |
| Effect of treatment group at +1SD mean CES-D |
.08 | .27 | −.45 | .62 | .30 | .76 |
| Marijuana Stealing/Delinquency | ||||||
| Intercept | .32 | .12 | .09 | .54 | ||
| Pretreatment marijuana stealing/delinquency |
.12 | .03 | .06 | .18 | 3.97 | .001 |
| Treatment group | .01 | .03 | −.29 | .30 | .05 | .96 |
| CES-D | −.01 | .01 | −.03 | .01 | 1.74 | .08 |
| Treatment X CES-D | .02 | .01 | −.01 | .05 | 1.21 | .23 |
| Marijuana Predatory Aggression | ||||||
| Intercept | .25 | .11 | .04 | .47 | ||
| Pretreatment marijuana predatory aggression |
.15 | .04 | .06 | .23 | 3.26 | .001 |
| Treatment group | −.18 | .14 | −.45 | .09 | 1.32 | .19 |
| CES-D | −.02 | .01` | −.03 | −.01 | 2.33 | .02 |
| Treatment X CES-D | .01 | .01 | −.01 | .04 | 1.05 | .30 |
3.3 Delinquent behaviors under the influence of alcohol
Table 2 presents results of the models assessing depressed mood as a moderator of treatment and alcohol-related stealing/delinquency and alcohol-related predatory aggression. Models predicting alcohol-related stealing/delinquency found no significant main effects for treatment. The main effect for depression was significant such that higher depression was associated with less alcohol related stealing/delinquency. The interaction of treatment by depression was not significant. Models predicting alcohol-related predatory aggression found no significant main effect for treatment. The main effect for depression was significant such that higher depression was associated with less alcohol related stealing/delinquency. The treatment by depressive symptoms interaction was significant. Results indicate alcohol-related predatory aggression differed for RT versus MI when depressive symptoms were below the mean, but not at the mean or above the mean. Compared to RT, MI is better at reducing alcohol-related predatory aggression when depressive symptoms are low.
3.4 Delinquent behaviors under the influence of marijuana
Table 2 presents results of the models assessing depressed mood as a moderator of treatment and marijuana-related stealing/delinquency and marijuana-related predatory aggression. Models predicting marijuana-related stealing/delinquency found no significant main effects for treatment or depression or treatment by depression interaction. Models predicting marijuana-related predatory aggression found no significant effect for treatment or treatment by depressive symptoms interaction. There was a significant main effect for depression such that higher depression was associated with less marijuana related predatory aggression.
4. Discussion
Incarcerated adolescents who used alcohol and marijuana were recruited for this study. They received a baseline assessment that was followed by a brief intervention of either MI or RT. At 3 month follow-up, adolescents low in depressive symptoms who received MI exhibited significantly less predatory aggression compared to those that received RT; however, no differences were observed among adolescents with mean or high levels of depressive symptoms.
These findings are consistent with several recent findings on the positive effects of MI with adolescents (Jensen et al., 2011). The moderating effect of depression on treatment efficacy found in the present study extends our work and is consistent with previous findings from these data. MI reduced alcohol and marijuana use and risky behaviors, but only in adolescents low in depressive symptoms (Rosengard et al., 2007; Stein et al., 2011b). No treatment effects were found for adolescents high in depressive symptoms. Results from other studies support an association between depressive symptoms and poor substance use outcomes (Cinciripini et al., 2003; Subramaniam, Stitzer, Clemmey, Kolodner, & Fishman, 2007; Walker, Cole, & Logan, 2008; Kranzler, Del Boca, & Rounsaville, 1996). Furthermore, Chambers and colleagues (2008) suggest that certain cognitive factors may impact offenders’ responsiveness to treatment. These factors include self-esteem, self-efficacy, and an internal locus of control. Adolescent offenders reporting greater depressive symptoms may experience lower levels of these cognitive factors, thus impeding their ability to engage in treatment and initiate and sustain behavior change. Taken together, these findings may explain why adolescents in the present study who reported greater depressive symptomatology and received MI continued to demonstrate poorer alcohol-related outcomes, despite the efficacy MI has shown in reducing substance-related outcomes in other studies.
The current findings may have significant clinical and societal implications. To our knowledge, these are the first findings to suggest identifying adolescents’ level of depressive symptoms early in incarceration may inform which type of intervention to employ in order to reduce some delinquent behaviors post-release, as well as substance use post-release (Stein et al., 2011b). Furthermore, results suggest that assessing and treating depression prior to engagement in interventions (i.e., MI) designed to decrease delinquent behaviors and/or substance use may be necessary for more optimal outcome(s) post-release. This may have significant societal implications as it may result in lower rates of adolescent violent crimes against persons (i.e, predatory aggression).
The current study is not without its limitations. For example, the study sample was comprised of incarcerated adolescents, most of whom were male. This may limit the generalizability of the findings. Although reliance on self-report is often considered a limitation, there are findings that support the use and accuracy of this type of reporting (Babor, Webb, Burleson, & Kaminer, 2002), especially with adolescents. Interestingly, when self-report is compared to their urine screens, adolescents have been found to report more marijuana use. Similarly, they have also been found to self-report more problematic behaviors as compared to their parents’ reports of their behavior (Dennis et al., 2002). As indicated in our results section, a review of facility records found no discrepancy between self-reported-marijuana non-use and the chart and only 1% discrepancy for self-reported alcohol non-use and the chart. Over 20% of adolescents self-reported marijuana and alcohol use that was not found in the chart. Less than 5% of adolescents that indicated they did not use marijuana in the previous month had positive urine screens while about 8% self-reported marijuana use but had negative urine screens Additionally, the measure of depressive symptoms only assessed symptomology during the past week at baseline. High levels of depressive symptoms may reflect adolescents’ response to current stressors and/or more chronic depressive disorders. Also, depressive symptoms were not measured at follow-up, preventing any pre-post comparison. Further, this study examined behaviors associated with alcohol and did not measure consumption of alcohol. Interventions to reduce alcohol-related violence often reduce violence but does not impact drinking (Walton et al., 2010; Watt, Shepherd, & Newcombe, 2008). Lastly, the present study has a limited follow-up period of 3 months, although a brief follow-up is not unusual when initially establishing treatment effects. Future research may want to include replication with a larger sample, assessment of both lifetime and current major depressive disorder, and a follow-up of longer duration.
Highlights.
Depression moderated the effects of MI on delinquent behaviors 3 months after treatment.
Compared to meditation, MI is better at reducing predatory aggression when depressive symptoms are low.
Compared to meditation, MI is better at reducing alcohol-related predatory aggression when depressive symptoms are low.
Acknowledgments
This work was supported by grants from the National Institute on Drug Abuse, R01-13375 (PI, Stein) and the National Institute on Drug Abuse/ National Institute on Alcohol Abuse and Alcoholism R01-18851 (PI, Stein).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Abram KM, Teplin LA, McClelland GM, Dulcan MK. Comorbid psychiatric disorders in youth in juvenile detention. Archives of General Psychiatry. 2003;60:1097–1108. doi: 10.1001/archpsyc.60.11.1097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th. Washington, DC: N/Author; 1994. [Google Scholar]
- Babor TF, Webb C, Burleson JA, Kaminer Y. Subtypes of classifying adolescents with marijuana use disorders: Construct validity and clinical implications. Addiction. 2002;97:58–69. doi: 10.1046/j.1360-0443.97.s1.1.x. [DOI] [PubMed] [Google Scholar]
- Baer JS, Garrett SB, Beadnell B, Wells EA, Peterson PL. Brief motivational intervention with homeless adolescents: Evaluating effects on substance use and service utilization. Psychology of Addictive Behaviors. 2007;21:582–586. doi: 10.1037/0893-164X.21.4.582. [DOI] [PubMed] [Google Scholar]
- Barrett H, Slenick N, Brody JL, Turner CW, Peterson TR. Treatment outcomes for adolescent substance abuse at 4- and 7-month assessments. Journal of Consulting and Clinical Psychology. 2001;69:802–813. [PubMed] [Google Scholar]
- Becker SJ, Curry FJ, Yang C. Factors that influence trajectories of change in frequency of substance use and quality of life among adolescents receiving a brief intervention. Journal of Substance Abuse Treatment. 2011;41:294–304. doi: 10.1016/j.jsat.2011.04.004. [DOI] [PubMed] [Google Scholar]
- Bender K, Tripodi SJ, Sarteschi C, Vaughn MG. A meta-analysis of interventions to reduce adolescent cannabis use. Research on Social Work Practice. 2011;21:153–164. [Google Scholar]
- Burke BL, Arkowitz H, Menchola M. The efficacy of motivational interviewing: A meta-analysis of controlled clinical trials. Journal of Consulting and Clinical Psychology. 2003;71:843–861. doi: 10.1037/0022-006X.71.5.843. [DOI] [PubMed] [Google Scholar]
- Chambers J, Eccleston L, Day A, Ward T, Howells K. Treatment readiness in violent offenders: The influence of cognitive factors on engagement in violence programs. Aggression and Violent Behavior. 2008;13:276–284. [Google Scholar]
- Cinciripini PM, Wetter DW, Fouladi RT, Blalock JA, Carter BL, Cinciripini L, Baile WF. The effects of depressed mood on smoking cessation: Mediation by postcessation self-efficacy. Journal of Consulting and Clinical Psychology. 2003;71:292–301. doi: 10.1037/0022-006x.71.2.292. [DOI] [PubMed] [Google Scholar]
- Cohen J, Cohen PC, West SG, Aiken LS. Applied multiple regression/correlation analysis for the behavioral sciences. 3rd. Mahwah, NJ: Lawrence Erlbaum; 2003. [Google Scholar]
- Colby SM, Monti PM, Barnett NP, Rohsenhow DJ, Weissman K, Spirito A, …Lewander WJ. Brief motivational interviewing in a hospital setting for adolescent smoking: A preliminary study. Journal of Consulting and Clinical Psychology. 1998;66:574–578. doi: 10.1037//0022-006x.66.3.574. [DOI] [PubMed] [Google Scholar]
- Colder CR, Chassin L. Affectivity and impulsivity: Temperament risk for adolescent alcohol involvement. Psychology of Addictive Behaviors. 1997;17:179–192. [Google Scholar]
- Connell AM, Dishion TJ. Reducing depression among at-risk early adolescents: Three-year effects of a family-centered intervention embedded within schools. Journal of Family Psychology. 2008;22:574–585. doi: 10.1037/0893-3200.22.3.574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cornelius RJ, Bukstein GO, Wood SD, Kirisci L, Douaihy A, Clark BD. Double- blind placebo-controlled trial of fluoxetine in adolescents with comorbid major depression and an alcohol use disorder. Addictive Behaviors. 2009;34:905–909. doi: 10.1016/j.addbeh.2009.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cornelius RJ, Clark BD, Bukstein GO, Birmaher B, Kelly MT, Salloum IM, Wood DS. Fluoxetine in adolescents with comorbid major depression and an alcohol use disorder: a five-year follow-up study. Journal of Dual Diagnosis. 2005a;2:11–25. [Google Scholar]
- Cornelius RJ, Clark BD, Bukstein GO, Birmaher B, Salloum IM, Brown SA. Acute phase and five-year follow-up study of fluoxetine in adolescents with major depression and a comorbid substance use disorder: a review. Addictive Behaviors. 2005b;30:1824–1833. doi: 10.1016/j.addbeh.2005.07.007. [DOI] [PubMed] [Google Scholar]
- Cornelius RJ, Douaihy A, Bukstein BO, Daley DC, Wood SD, Kelly MT, Salloum Evaluation of cognitive behavioral therapy/motivational enhancement therapy CBT/MET in a treatment trial of comorbid MDD/AUD adolescents. Addictive Behaviors. 2011a;36:843–848. doi: 10.1016/j.addbeh.2011.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cornelius RJ, Douaihy A, Chung T, Kelly T, Daley DC, Hayes J, Clark D. Four-year follow-up of double-blind fluoxetine trial of comorbid MDD-AUD adolescents. Alcoholism: Clinical and Experimental Research. 2011b;(Suppl(35)) [Google Scholar]
- Cornelius RJ, Douaihy BA, Kirisci L, Daley DC. Longer-term effectiveness of CBT in treatment of comorbid AUD/MDD adolescents. International Journal of Medical and Biological Frontiers. 2013;19:1–10. [PMC free article] [PubMed] [Google Scholar]
- Cornelius JR, Maisto SA, Martin CS, Bukstein GO, Salloum IM, Daley DC, Clark BD. Major depression associated with earlier alcohol relapse in treated teens with AUD. Addictive Behaviors. 2004;29:1035–1038. doi: 10.1016/j.addbeh.2004.02.056. [DOI] [PubMed] [Google Scholar]
- Crowley TJ, Mikulich SK, MacDonald M, Young SE, Zerbe GO. Substance-dependent, conduct-disordered adolescent males: severity of diagnosis predicts 2-year outcome. Drug and Alcohol Dependence. 1998;49:225–237. doi: 10.1016/s0376-8716(98)00016-7. [DOI] [PubMed] [Google Scholar]
- D’Amico EJ, Hunter SB, Miles JNV, Ewing BA, Osilla K. A randomized controlled trial of a group motivational interviewing intervention for adolescents with a first time alcohol or drug offense. Journal of Substance Abuse Treatment. 2013;45:400–408. doi: 10.1016/j.jsat.2013.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- deDios MA. Depression, Conduct Problems, and Substance Abuse Treatment Outcomes Among Adolescents [unpublished doctoral dissertation] Miami, FL: University of Miami; 2007. [Google Scholar]
- Dembo R, Williams L, Schmeidler J, Berry E, Wothke W, Getreu A, Christensen C. A structural model examining the relationship between physical child abuse, sexual child victimization, and marijuana/hashish use in delinquent youth: A longitudinal study. Violence and Victims. 1992;7:41–62. [PubMed] [Google Scholar]
- Dembo R, Williams L, Schmeidler J, Wothke W. A longitudinal study of the predictors of the adverse effects of alcohol and marijuana/hashish use among a cohort of high risk youths. International Journal of the Addictions. 1993;28:1045–1083. doi: 10.3109/10826089309056243. [DOI] [PubMed] [Google Scholar]
- Dennis M, Titus JC, Diamond G, Donaldson J, Godley SH, Tims FM, Scott CK. The Cannabis Youth Treatment (CYT) experiment: Rationale, study design and analysis plans. Addiction. 2002;97(Suppl 1):16–34. doi: 10.1046/j.1360-0443.97.s01.2.x. [DOI] [PubMed] [Google Scholar]
- Deskovitz M, Key DE, Hill EM, Franklin JT. A long-term family-oriented treatment for adolescents with substance-related disorders: an outcome study. Child and Adolescent Social Work Journal. 2004;21:265–284. [Google Scholar]
- Edwards RJ, Lambert LS. Methods for integrating moderation and mediation: A general analytical framework using moderated path analysis. Psychological Methods. 2007;12:1–22. doi: 10.1037/1082-989X.12.1.1. [DOI] [PubMed] [Google Scholar]
- Elliot DS, Ageton SS, Huizinga D, Knowles BA, Canter RJ. The prevalence and incidence of delinquent behavior. Boulder, CO: Behavioral Research Institute; 1983. pp. 1976–1980. [Google Scholar]
- Esposito-Smythers C, Penn JV, Stein LAR, Lacher-Katz M, Spirito A. A test of problem behavior and self-medication theories in incarcerated adolescent males. Journal of Child and Adolescent Substance Abuse. 2008;17:41–56. doi: 10.1080/15470650802292731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders - Patient Edition (SCID-I/P, Version 2.0) New York, NY: Biometrics Research Department, New York State Psychiatric Institute; 1995. [Google Scholar]
- Geller B, Cooper TB, Sun K, Zimerman B, Frazier J, Williams M, Heath J. Double-blind and placebo-controlled study of lithium for adolescent bipolar disorders with secondary substance dependency. Journal of the American Academy of Child and Adolescent Psychiatry. 1998;37:171–178. doi: 10.1097/00004583-199802000-00009. [DOI] [PubMed] [Google Scholar]
- Gmel G, Venzin V, Marmet K, Danko G, Labhart F. A quasi-randomized group trial of a brief alcohol intervention on risky single occasion drinking among secondary school students. International Journal of Public Health. 2012;57:935–944. doi: 10.1007/s00038-012-0419-0. [DOI] [PubMed] [Google Scholar]
- Greenwood PW. Substance abuse problems among high-risk youth and potential intervention. Crime and Delinquency. 1992;38:444–458. [Google Scholar]
- Hayes AF. PROCESS: A versatile computational tool for observed variable mediation, moderation, and conditional process modeling [White paper] 2012 Retrieved from http://www.afhayes.com/public/process2012.pdf.
- Hersh J, Curry JF, Becker SJ. The influence of comorbid depression and conduct disorder on MET/CBT treatment outcome for adolescent substance use disorders. International Journal of Cognitive Psychotherapy. 2013;6:325–341. doi: 10.1521/ijct.2013.6.4.325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hersh J, Curry FJ, Kaminer Y. What is the impact of comorbid depression on adolescent substance abuse treatment? Substance Abuse. 2014;35:364–375. doi: 10.1080/08897077.2014.956164. [DOI] [PubMed] [Google Scholar]
- Hettema J, Steele J, Miller WR. Motivational Interviewing. Annual Review of Clinical Psychology. 2005;1:91–111. doi: 10.1146/annurev.clinpsy.1.102803.143833. [DOI] [PubMed] [Google Scholar]
- Houge A, Henderson EC, Ozechowski JT, Robbins SM. Evidence base on outpatient behavioral treatments for adolescent substance use: Updates and recommendations 2007–2013. Journal of Clinical Child & Adolescent Psychology. 2014;43:695–720. doi: 10.1080/15374416.2014.915550. [DOI] [PubMed] [Google Scholar]
- Jensen CD, Cushing CC, Aylward BS, Craig JT, Sorell DM, Steele RG. Effectiveness of motivational interviewing interventions for adolescent substance use behavior change: A meta-analytic review. Journal of Consulting and Clinical Psychology. 2011;79:433–440. doi: 10.1037/a0023992. [DOI] [PubMed] [Google Scholar]
- Karno MP, Longabaugh R. What do we know? Process analysis and the search for a better understanding of Project MATCH’s anger-by-treatment matching effect. Journal of Studies on Alcohol. 2004;65:501–512. doi: 10.15288/jsa.2004.65.501. [DOI] [PubMed] [Google Scholar]
- Kranzler HR, Del Boca FK, Rounsaville BJ. Comorbid psychiatric diagnosis predicts three-year outcomes in alcoholics: A posttreatment natural history study. Journal of Studies on Alcohol and Drugs. 1996;57:619–626. doi: 10.15288/jsa.1996.57.619. [DOI] [PubMed] [Google Scholar]
- Lennings CJ, Copeland J, Howard J. Substance use patterns of young offenders and violent crime. Aggressive Behavior. 2003;29:414–422. [Google Scholar]
- Lewinsohn PM, Rhode P, Seeley JR. Adolescent psychopathology: III. The clinical consequences of comorbidity. Journal of the American Academy of Child & Adolescent Psychiatry. 1995;34:510–519. doi: 10.1097/00004583-199504000-00018. [DOI] [PubMed] [Google Scholar]
- Lipsey MW, Derzon JH. Predictors of violent or serious delinquency in adolescence and early adulthood: A synthesis of longitudinal research. In: Loeber In R, Farrington DP., editors. Serious and Violent Offenders. Thousand Oaks, CA: Sage Publications, Inc; 1998. pp. 313–345. [Google Scholar]
- Lundahl B, Burke BL. The effectiveness and applicability of motivational interviewing: A practice-friendly review of four meta-analyses. Journal of Clinical Psychology. 2009;65:1232–1245. doi: 10.1002/jclp.20638. [DOI] [PubMed] [Google Scholar]
- Lundahl B, Kunz C, Brownell C, Tollefson D, Burke LB. A Meta-analysis of motivational interviewing: Twenty-five years of empirical studies. Research on Social Work Practice. 2010;20:137–160. [Google Scholar]
- Lundahl B, Moleni T, Burke BL, Butters R, Tollefson D, Butler C, Rollnick S. Motivational interviewing in medical care settings: A systematic review and meta-analysis of randomized controlled trials. Patient Education and Counseling. 2013;93:157–168. doi: 10.1016/j.pec.2013.07.012. [DOI] [PubMed] [Google Scholar]
- McMurran M. Motivational interviewing with offenders: A systematic review. Legal & Criminological Psychology. 2009;14:83–100. [Google Scholar]
- Miller WR, Rollnick S. Motivational interviewing: Preparing people for change. 2nd. New York: The Guildord Press; 2002. [Google Scholar]
- Mulvey EP, Schubert CA, Chassin L. Substance use and delinquent behavior among serious adolescent offenders. Washington, D.C.: U.S: Department of Justice; 2010. Juvenile Justice Bulletin. [Google Scholar]
- Myers MG, Aarons GA, Tomlinson K, Stein MB. Social anxiety, negative affectivity, and substance use among high school students. Psychology of Addictive Behaviors. 2003;17:277–283. doi: 10.1037/0893-164X.17.4.277. [DOI] [PubMed] [Google Scholar]
- National Institute of Justice. 1997 annual report on adult and juvenile arrestees. Washington, DC: U.S. Department of Justice; 1997. [Google Scholar]
- National Institute of Justice. 2000 arrestee drug abuse monitoring: Annual report. Washington, DC: U.S. Department of Justice; 2003. (NCJ 193013) [Google Scholar]
- O’Leary-Tevyaw T, Monti PM. Motivational enhancement and other brief interventions for adolescent substance abuse: Foundations, applications and evaluations. Addiction. 2004;99:63–75. doi: 10.1111/j.1360-0443.2004.00855.x. [DOI] [PubMed] [Google Scholar]
- Osilla KC, Ortiz JA, Miles JNV, Pedersen ER, Houck JM, D’Amico EJ. How group factors affect adolescent change talk and substance use outcomes: Implications for motivational interviewing training. Journal of Counseling Psychology. 2015;62:79–86. doi: 10.1037/cou0000049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pagnin D, de Queiroz V, Saggese EG. Predictors of attrition from day treatment of adolescents with substance-related disorders. Addictive Behaviors. 2005;30:1065–1069. doi: 10.1016/j.addbeh.2004.09.013. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Rucker DD, Hayes AF. Assessing moderated mediation hypotheses: Theory, methods, and prescriptions. Multivariate Behavioral Research. 2007;42:185–227. doi: 10.1080/00273170701341316. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The use of the Center for Epidemiologic Studies Depression Scale in adolescents and young adults. Journal of Youth and Adolescence. 1991;20:149–166. doi: 10.1007/BF01537606. [DOI] [PubMed] [Google Scholar]
- Radloff LS. CES-D scale: A self-report depression scale for research on the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Reavy R, Stein LAR, Paiva A, Quina K, Rossi JS. Validation of the delinquent activities scale for incarcerated adolescents. Addictive Behaviors. 2012;37:875–879. doi: 10.1016/j.addbeh.2012.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhode P, Lewinsohn PM, Seeley JR. Psychiatric comorbidity with problematic alcohol use in high school students. Journal of the American Academy of Child & Adolescent Psychiatry. 1996;35:101–109. doi: 10.1097/00004583-199601000-00018. [DOI] [PubMed] [Google Scholar]
- Riggs PD, Hall SK, Mikulich-Gilbertson SK, Lohman M, Kayser A. A randomized controlled trial of pemoline for ADHD for substance abusing adolescents. Journal of the American Academy of Child & Adolescent Psychiatry. 2004;43:420–429. doi: 10.1097/00004583-200404000-00008. [DOI] [PubMed] [Google Scholar]
- Riggs P, Levin F, Green IA, Vocci F. Comorbid psychiatric and substance abuse disorders: Recent treatment research. Substance Abuse. 2008;29:51–61. doi: 10.1080/08897070802218794. [DOI] [PubMed] [Google Scholar]
- Riggs P, Mikulich-Gilbertson S, Lohman M, Klein C, Stover S. A randomized controlled trial of fluoxetine and cognitive behavioral therapy in adolescents with major depression, behavior problems, and substance use disorders. Archives of Pediatric and Adolescent Medicine. 2007;161:1026–1034. doi: 10.1001/archpedi.161.11.1026. [DOI] [PubMed] [Google Scholar]
- Rosengard C, Stein LAR, Barnett NP, Monti PM, Golembeske C, Lebeau-Craven R, Miranda R. Randomized clinical trial of motivational enhancement of substance use treatment among incarcerated adolescents: Post-release condom non-use. Journal of HIV/AIDS Prevention in Children & Youth. 2007;8:45–64. doi: 10.1300/J499v08n02_04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmiege SJ, Broaddus MR, Levin M, Bryan AD. Randomized trial of group interventions to reduce HIV/STD risk and change theoretical mediators among detained adolescents. Journal of Consulting and Clinical Psychology. 2009;77:38–50. doi: 10.1037/a0014513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sealock MD, Gottfredson DC, Gallagher CA. Drug treatment for juvenile offenders: Some good and bad news. Journal of Research in Crime and Delinquency. 1997;34:210–236. [Google Scholar]
- Shoal GD, Giancola PR. Negative affectivity and drug use in adolescent boys: Moderating and mediating mechanisms. Journal of Personality and Social Psychology. 2003;84:221–223. [PubMed] [Google Scholar]
- Sinha R, Easton C, Renee-Aubin L, Carroll KM. Engaging young probation-referred marijuana-abusing individuals in treatment: A pilot trial. American Journal on Addictions. 2003;12:314–323. [PubMed] [Google Scholar]
- Slavet JD, Stein LAR, Klein J, Colby SM, Barnett NP, Monti PM. Piloting the family check up with incarcerated adolescents and their parents. Psychological Services. 2005;2:123–132. doi: 10.1037/1541-1559.2.2.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein LAR, Clair M, Lebeau R, Colby S, Barnett NP, Golembeske C, Monti P. Motivational interviewing to reduce substance-related consequences: Effects for incarcerated adolescents with depressed mood. Drug and Alcohol Dependence. 2011a;118:475–478. doi: 10.1016/j.drugalcdep.2011.03.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein LAR, Colby SM, Barnett NP, Monti PM, Golembeske C, Lebeau-Craven R. Effects of motivational interviewing for incarcerated adolescents on driving under the influence after release. The American Journal on Additions. 2006a;15:50–57. doi: 10.1080/10550490601003680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein LAR, Lebeau-Craven R. Motivational interviews & relapse prevention for DWI: A pilot study. Journal of Drug Issues. 2002;32:1051–1070. doi: 10.1177/002204260203200403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein LAR, Lebeau R, Colby S, Barnett NP, Golembeske C, Monti PM. Motivational interviewing for incarcerated adolescents: Effects of depressive symptoms on reducing alcohol and marijuana use after release. Journal of Studies on Alcohol and Drugs. 2011b;72:497–506. doi: 10.15288/jsad.2011.72.497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein LAR, Monti PM, Colby SM, Barnett NP, Golembeske C, Lebeau-Craven R, Miranda R. Enhancing substance abuse treatment engagement in incarcerated adolescents. Psychological Services. 2006b;3:25–34. doi: 10.1037/1541-1559.3.1.0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Myers MG, Brown SA. A longitudinal grouping analysis of adolescent substance use escalation and de-escalation. Psychology of Addictive Behaviors. 1998;12:14–27. [Google Scholar]
- Subramaniam GA, Stitzer MA, Clemmey P, Kolodner K, Fishman MJ. Baseline depressive symptoms predict poor substance use outcome following adolescent residential treatment. Journal of the American Academy of Child and Adolescence Psychiatry. 2007;46:1062–1069. doi: 10.1097/chi.0b013e31806c7ad0. [DOI] [PubMed] [Google Scholar]
- Tanner-Smith EE, Wilson SJ, Lipsey MW. The comparative effectiveness of outpatient treatment for adolescent substance abuse: A meta-analysis. Journal of Substance Abuse Treatment. 2013;44:145–158. doi: 10.1016/j.jsat.2012.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tapert SJ, Colby SM, Barnett NP, Spirito A, Rohsenow DJ, Myers MG, Monti Peter M. Depressed mood, gender, and problem drinking in youth. Journal of Child and Adolescent Substance Abuse. 2003;12:55–68. [Google Scholar]
- Teplin LA, Abram KM, McClelland GM, Dulcan MK, Mericle AA. Psychiatric disorders in youth in juvenile detention. Archives of General Psychiatry. 2002;59:1133–1143. doi: 10.1001/archpsyc.59.12.1133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner AP, Larimer ME, Sarason IG, Trupin EW. Identifying a negative mood subtype in incarcerated adolescents: Relationship to substance use. Addictive Behaviors. 2005;30:1442–1448. doi: 10.1016/j.addbeh.2005.01.009. [DOI] [PubMed] [Google Scholar]
- Vourakis C. Admission variables as predictors of completion in an adolescent residential drug treatment program. Journal of Child Adolescent Psychiatric Nursing. 2005;18:161–170. doi: 10.1111/j.1744-6171.2005.00031.x. [DOI] [PubMed] [Google Scholar]
- Walker R, Cole J, Logan TK. Identifying client-level indicators of recovery among DUI, criminal-justice, and non-criminal justice treatment referrals. Substance Use and Misuse. 2008;43:1785–1801. doi: 10.1080/10826080802297484. [DOI] [PubMed] [Google Scholar]
- Walker DD, Roffman RA, Stephens RS, Berghuis J, Kim W. Motivational enhancement therapy for adolescent marijuana users. A preliminary randomized controlled trial. Journal of Consulting and Clinical Psychology. 2006;74:628–632. doi: 10.1037/0022-006X.74.3.628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker DD, Stephens R, Roffman R, Demarce J, Lozano B, Towe S, Berg B. A randomized controlled trial of motivational enhancement therapy with non-treatment-seeking adolescent cannabis users: A further test of the Teen Marijuana Check-Up. Psychology of Addictive Behaviors. 2011;25:474–484. doi: 10.1037/a0024076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walton MA, Chermack ST, Shope JT, Bingham CR, Zimmerman MA, Blow FC, Cunningham RM. Effects of a brief intervention for reducing violence and alcohol misuse among adolescents: A randomized controlled trial. Journal of the American Medical Association. 2010;304:527–535. doi: 10.1001/jama.2010.1066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watt K, Shepherd J, Newcombe R. Drunk and dangerous: A randomised controlled trial of alcohol brief intervention for violent offenders. Journal of Experimental Criminology. 2008;4:1–19. [Google Scholar]
- White AM, Jordan JD, Schroeder KM, Acheson SK, Georgi BD, Sauls G, Swartzwelder HS. Predictors of relapse during treatment and treatment completion among marijuana-dependent adolescents in an intensive outpatient substance abuse program. Substance Abuse. 2004;25:53–59. doi: 10.1300/J465v25n01_08. [DOI] [PubMed] [Google Scholar]
- Whitmore EA, Mikulich SK, Ehlers KM, Crowley TJ. One-year outcome of adolescent females referred for conduct disorder and substance abuse/dependence. Drug Alcohol Depend. 2000;59:131–141. doi: 10.1016/s0376-8716(99)00112-x. [DOI] [PubMed] [Google Scholar]