Abstract
Communication with healthcare providers, family, and friends is associated with increased mammography use. Less is known about the abnormal mammogram experience, especially in terms of the interval between screening and follow-up appointments (time to follow-up) and psychological distress. The impact of communication may vary across ethnicity, depending on cultural emphases placed on interpersonal relationships. The current study’s objectives were to a) explore the role of family/friend and provider communication with regard to time to follow-up and distress; and b) examine if family/friend and provider communication moderates associations between ethnicity and these outcomes. A convenience-based sample of 41 Latina and 41 non-Latina White (NLW) women who had received an abnormal mammogram result was recruited from Washington State. Women who discussed results with providers had a shorter time to follow-up, although this was not significant when including health insurance. A significant interaction between conversations with family/friends and ethnicity was found: Latinas who did not have conversations with family/friends had particularly elevated psychological distress relative to NLW women and slightly more than other Latinas. This exploratory study suggests health communication with providers and family/friends are important for timely receipt of follow-up care and reduced distress among women who receive an abnormal mammogram result, which has implications for cancer education intervention development and adaptation. Larger, population-based research is necessary to confirm these findings.
Keywords: Latina, mammogram, distress, support, provider, family
Introduction
To maximize the promise of screening for early detection of breast cancer and patient well-being, there is a need for cancer education interventions to identify and address protective factors following an abnormal screening result, including those characteristics that reduce time to follow-up, defined as the number of days between screening and follow-up appointments, and psychological distress, defined as non-specific distress associated with abnormal mammogram results. Another major priority in cancer prevention and treatment is the reduction and elimination of racial/ethnic disparities, including the delayed adherence and worse psychological distress Latinas experience after an abnormal mammogram relative to their non-Latina White counterparts (NLW) [1, 2]. Social factors can be protective across the cancer continuum and have been implemented in cancer educational interventions [3]; nonetheless, efforts are ongoing to develop methodologies to measure and accurately capture them and their influence across cultural groups. Previous research has focused on social network characteristics, especially the number of family and friends, as a proxy for social resources [4]. The influence of social factors may, however, vary across different members of one’s social network and ethnic lines [5]. Research utilizing social network methods in the context of ethnic differences following an abnormal mammogram will be greatly enhanced by pilot data identifying which social factors are relevant to timely adherence and reduced distress for a given social or cultural group. The current study serves to address existing gaps in the literature by identifying functional characteristics of one’s social network related to time to follow-up and psychological distress and examining the moderating influence of these characteristics on ethnic differences in time to follow-up and psychological distress.
There are a number of ways to characterize social networks within the breast cancer continuum [6, 7], including structural (e.g., number of social ties) and functional characteristics (e.g., frequency of social contacts). Both types of characteristics of networks appear to be particularly relevant for cancer screening intentions and practices, including social network size [8], frequency of conversations with healthcare providers [9], and frequency of conversations with family/friends [10]. In comparison, the majority of research concerning the role of social factors following an abnormal mammogram result on timely follow-up has been qualitative or has not focused on social network characteristics [11, 12]. To date, only one study has quantified differences across the absence/presence of conversations about results: authors found women who do not discuss results with providers are less likely to have shorter time to follow-up [13]. Little is further known about how structural and functional characteristics are associated with psychological distress in screening or diagnostic stages of the continuum. Assessment of functional characteristics on time to follow-up and psychological distress is warranted, as recent research indicates that many women (23%) do not speak with a healthcare providers about these results [14] and little to nothing is known about the influence of conversations with family/friends. Such information on these potentially protective factors is essential to assessing the potential effectiveness of educational interventions to help women during this stressful time through promotion of communication with providers and family/friends.
Understanding the differential effects of healthcare provider versus family/friend communication may be particularly helpful in planning and designing programs that serve vulnerable populations. Interpersonal relationships are highly valued in Latin American culture [15] and so conversations with providers and family/friends may be particularly helpful for Latinas. Specifically, given the strong cultural emphasis Latinos place on interpersonal relationships, conversations about results may serve as moderators in disparities, in that ethnic differences may vary depending on the presence or absence of such conversations. Latinas who do not have conversations with providers and family/friends may have longer time to follow-up and greater psychological distress relative to NLWs who have not had conversations, due to the lack of social resources to address barriers such as patient comprehension and socioeconomic disadvantage [16, 17]. Latinas who discuss results with providers and family/friends may be more similar to or have even greater added benefits of conversations relative to NLW counterparts, given cultural emphases on interpersonal relationships and access to support to overcome barriers described above. Given this, greater delay in time to follow-up and distress among Latinas may be pronounced among women who have not discussed their abnormal results, whereas ethnic differences in time to follow-up and psychological distress may be diminished or Latinas who have these conversations may even have reduced time to follow-up and diminished distress due to access to resources that are particularly important for this group. Nonetheless, the majority of extant literature concerning associations among social factors, time to follow-up, and psychological distress after an abnormal mammogram result has focused on NLW samples or not directly addressed racial/ethnic differences [17, 18].
Purpose of current study
This exploratory study attempts to address several gaps in existing literature concerning social network functional characteristics in relation to the abnormal mammogram experience. We first take a step toward understanding the role of conversations with providers and family/friends in relation to the time to follow-up and psychological distress. We hypothesize women who communicate with providers and family/friends will have fewer days to follow-up and lower psychological distress. Next, we use analyses guided by research concerning the cultural importance placed on strong interpersonal relationships among Latinas to explore if ethnic differences in time to follow-up and psychological distress vary across levels of functional characteristics. We predict Latinas who do not discuss results may have longer time to follow-up and greater psychological distress relative to NLW counterparts. Conversely, there may be few differences in time to follow-up or psychological distress among Latinas and NLWs who discuss results or Latinas may have reduced time to follow-up and distress.
Methods
Procedures
Recruitment
The current study utilizes baseline questionnaire and electronic medical record data from a larger longitudinal project addressing ethnic differences in stress and coping after an abnormal mammogram result among Latina and NLW women living in in eastern and western regions of Washington State (BLINDED FOR REVIEW). Our convenience sample was composed of women who received a BI-RADS (Breast Imaging Reporting and Data System) Category 0 result. Participating clinics included two mobile mammography services and a community hospital. A two-step recruitment process was used in order to maximize recruitment and enrollment. Women were first approached and received information about the study by clinic staff during their initial mammography appointment. Women who indicated interest and received an abnormal screening result were contacted by staff within a week of receipt of their results. Second, all women with an abnormal mammogram received study materials (e.g., letter of approach, brochure) shortly after receiving their results. Preliminary analyses revealed no significant differences in study variables of interest by clinic or recruitment strategy (data not shown).
Interested women contacted research staff for further information and screening. Inclusion criteria were as follows: identification as Hispanic/Latina/ Chicana or as European American/White/Caucasian; age of 40–74 years old; receipt of an abnormal mammogram result within the last month; and no personal history of breast cancer. Subsequent baseline surveys were administered by a bicultural, bilingual interviewer via telephone, in person, or by mail. All study materials were available in English and Spanish. Informed consent was obtained from all individual participants included in the study.
Measures
Socio-demographic variables
We administered standard and census demographic questions concerning ethnicity, age, education, personal annual income, insurance status, and nationality. Preliminary analyses suggested personal annual income, education, and insurance status were strongly associated; given this, a socioeconomic position composite score was calculated based on loadings from a factor analysis (range: 0 to 4.16). Larger values for this variable indicate greater socioeconomic advantage.
Conversations concerning results
To examine interpersonal interactions, we asked women if they had spoken with healthcare providers, outside of the initial notification of results (No = 0, Yes = 1), and if they had spoken with family/friends (No = 0, Yes = 1) about their abnormal mammogram results before they scheduled their follow-up appointment.
Time to follow-up
The interval between screening and follow-up appointments was drawn from electronic medical record data for women who completed HIPAA forms (n = 63) and from self-report data for women who reported specific days during the interview, but did not complete HIPAA forms (n = 18). The difference in days between the first follow-up appointment and the initial screening appointment was calculated.
Psychological distress
To measure psychological distress, we administered two sub-scales of the Impact of Events Scale-Revised instrument, which have been validated in English and Spanish [19, 20]. Sample items of the 15-item Avoidance and Intrusion sub-scales are respectively, “I am aware that I have a lot of feelings about my results, but I haven’t dealt with them” and “I have had waves of strong feelings about my results.” The Avoidance and Intrusion subscales have been suggested to be relevant across different traumatic events of varying severity, in contrast to the Hyperarousal subscale [21]. Given this and to minimize patient burden, we only administered the Avoidance and Intrusion sub-scales. Participants chose from 0 = Not at all, 1 = A little bit, 2 = Moderately, 3 = Quite a bit, and 5 = Extremely. We followed the standard scoring techniques for this instrument, by calculating means of all items for both sub-scales and summing these means to create an overall score. Cronbach’s alpha for this sample was 0.90.
Analysis plan
We first provide descriptive information concerning differences among women who did and did not report conversations with providers and family/friends about their results. For our first question, we conducted two linear regression models to examine the effect of conversations on time between time to follow-up and psychological distress. For our second research question, we assessed interactions between ethnicity and conversations with healthcare providers and family/friends through multivariable regression models. Main effects were not required to be significant before testing for interaction/moderation, as moderation was the hypothesis ab initio [22]. It is acknowledged that the study is underpowered to detect small interaction effects, but is designed to provide estimates that will inform future analyses on larger, population-based samples. Assumptions of homogeneous variance were met across the categorical variables for psychological distress, but not for time to follow-up. Given this, moderation models were not conducted for time to follow-up [22]. Unstandardized coefficients are presented and used for data interpretation. If significant, simple slopes were compared, to estimate the relationships between the predictor (ethnicity) and outcome (psychological distress) across different levels of moderators (conversations about results). Notably, insurance status may be more strongly associated with provider-patient interactions than other indicators of socioeconomic position, as access facilitates utilization (i.e., initiating conversations with providers about abnormal results). Given this, secondary analyses concerning provider communication were also conducted that included only insurance status.
Results
There were no missing data with regard to conversations concerning results and survey instruments, as all women completed baseline questionnaires. With regard to time to follow-up, we report analyses using electronic medical record and self-report data (EMR+SR; n = 81) as well as a only electronic medical record data (EMR; n = 63).
Table 1 provides socio-demographic variables for our sample of women across conversations with providers or family/friends, including 41 Latinas and 40 NLWs. The overall age of women in our sample was 49.49 years (SD = 6.69). Regarding socio-economic indicators, the median individual income was $10–19,999, 38% of participants had completed no formal education beyond high school, and 48% had no insurance at the baseline interview. No significant socio-demographic differences were observed between women who did and did not discuss their results with health care providers, although there was a non-significant association with insurance status (p = .08). However, women who had not discussed their results with family/friends had lower income than women who spoke with family/friends, F(1,76) = 4.35, p = .04. Given these findings, the composite variable socioeconomic position was entered as a covariate and, as described above, secondary analyses for provider communication included models with insurance status alone as a covariate.
Table 1.
Descriptive information comparing women who did and did not have conversations about their results with healthcare providers or family/friends
| Variable | Healthcare Providers | Family/Friends | ||
|---|---|---|---|---|
| Had conversation (n = 54) |
Did not have conversation (n = 27) |
Had conversation (n = 68) |
Did not have conversation (n =13) |
|
| % (n) | % (n) | % (n) | % (n) | |
| % Latina | 48% (26) | 56% (15) | 50% (34) | 54% (7) |
| % Insured | 44% (18) | 58% (11) | 51% (25) | 36% (2) |
| Education1 | 44% (12) | 34% (18) | 39% (26) | 31% (4) |
| Income (≤$10–19,999)1* | 56% (15) | 57% (30) | 51% (34) | 85% (11) |
| M (SD) | M (SD) | M (SD) | M (SD) | |
| Age (years) | 48.22 (6.76) | 50.45 (6.62) | 49.43 (0.89) | 49.39 (1.93) |
| Socioeconomic position2 | 1.48 (0.96) | 1.58 (1.04) | 1.60 (1.05) | 1.26 (0.70) |
Notes.
Education and income were analyzed as continuous variables for analyses, but are presented dichotomously (≤HS or >HS; (≤$10–19,999 or >$10–19,999) for ease of readability in this table.
Socioeconomic position was a composite score from factor analysis loadings. Greater values indicate greater socioeconomic advantage.
p ≤ .05
Conversations about results, time to follow-up, and psychological distress
Table 2 depicts information for time to follow-up and psychological distress across conversations with providers and conversations with family/friends, after adjusting for socioeconomic position. We first conducted two linear regression models to assess the effects of conversations with providers and conversations with family/friends on time to follow-up, emotional support, and psychological distress, after adjusting for socioeconomic position. Women who had conversations with healthcare providers had less time to follow-up than women who had not, EMR: B = −2.13, 95%CI [−17.37, −0.56], p = .04; EMR+SR: B = −10.18, 95%CI [−19.36, −1.00], p = .03. Interestingly, the relationship between provider conversations and time to follow-up was not significant in models that examined insurance status as a separate variable (ps = 0.74–0.85). There was no significant relationship between time to follow-up and conversations with family/friends (ps = .10–.46). Neither conversations with providers nor conversations with family/friends were associated with psychological distress (ps = .85–.97).
Table 2.
Differences in time to follow-up care and psychological distress by whether results were discussed with healthcare providers or family/friends, after adjusting for socioeconomic position
| Variable | Healthcare Providers | Family/Friends | ||
|---|---|---|---|---|
| Had conversation (n = 27) |
Did not have conversation (n = 54) |
Had conversation (n = 68) |
Did not have conversation (n =13) |
|
| M (SE) | M (SE) | M (SE) | M (SE) | |
| Time to follow-up1 | 23.99 (4.50) | 34.17 (3.15) | 24.14 (2.41) | 34.02 (5.62) |
| Psychological distress2 | 2.57 (0.36) | 2.50 (0.25) | 2.53 (0.19) | 2.55 (0.44) |
Time to follow-up was calculated as the number of days between date of the initial screening appointment and the first follow-up appointment. Data were largely abstracted from electronic medical records; self-report data were used for cases wherein HIPAA forms were not completed. Findings did not vary depending on inclusion or exclusion of self-report data.
Range for summary scores from the Impact of Events-Revised Scale subscales was 0 to 6.
p≤.05,
p<.01,
p<.001
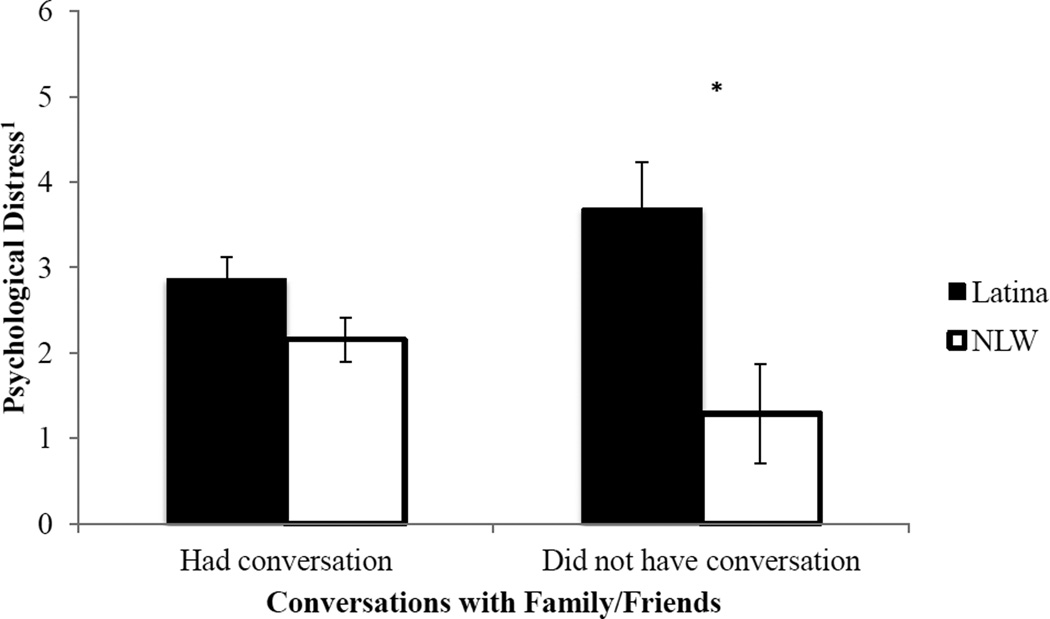
Ethnic differences in psychological distress across levels of conversations about results
Two regression models were fit to assess potential interactions between ethnicity and each conversation variable (with healthcare providers, with family/friends) on psychological distress. There was no interaction between ethnicity and conversation with providers on psychological distress, when including the composite socioeconomic position variable (p = .17) or insurance status separately (p = .22). There was however a significant interaction of ethnicity and presence of conversation with family/friends on psychological distress, B = −1.69, 95%CI [−3.42, −0.03], p = .05. Given this, we compared the simple slopes for ethnicity on psychological distress across the two levels of conversations with family/friends: presence (34 NLW, 34 Latina) and absence (6 NLW, 7 Latina; Figure 1). Among women who did have conversations with family/friends, there was no significant association between ethnicity and psychological distress, B = 0.65, 95%CI [−0.13, 1.4], p = .10. There were, however, ethnic differences among women who did not discuss results with their family/friends, B = 2.74, 95%CI [0.80, 4.69], p = .01. Latinas who did not discuss with family/friends reported greater psychological distress than non-Latina White counterparts (Figure 1).
Figure 1.
Ethnic differences in psychological distress among women who did and did not have conversations with their family and friends about their abnormal mammogram result.
1Range for summary scores from the Impact of Events-Revised Scale subscales was 0 to 6. *p < .05 *
Discussion
This exploratory study provides pilot data to support further investigation into the role of social networks’ functional characteristics on ethnic disparities following an abnormal mammogram result. Similar to previous research, we found that conversations with providers were associated with fewer days to follow-up [13]. Our work further suggests that conversations with family/friends may be especially important to Latinas with regard to the psychological distress they experience related to an abnormal mammogram finding. Despite the small sample size, our study coincides with extant literature, demonstrating the importance of both provider and family/friend communications in the context of cancer screening and early detection practices [10, 23]. It also contributes to existing theories on social network characteristics and social context by focusing on the functional aspects of these constructs. Overall, these pilot data suggest a need for larger studies assessing the role of family/friend interactions for ethnically diverse populations of women who receive an abnormal mammogram result.
Our preliminary findings offer several venues for social network research to promote cancer education about the abnormal mammogram experience. The main effect of conversations with providers on time to follow-up is consistent with a robust body of literature that indicates the importance of provider communication for breast cancer screening [23]. Our work furthermore adds to existing literature concerning the role of functional characteristics of social networks for receipt of follow-up care after an abnormal mammogram result and suggests the importance of conversations with providers about results [13]. It should be noted that models that incorporated insurance status attenuated this effect. This attenuation likely speaks to underlying associations between healthcare access and types of interactions patients have with providers. Another component of healthcare access that could influence time to follow-up is regular source of care, which was not assessed for the current study. Relatedly, the current study did not discern between different types of healthcare providers; thus it is unclear if women discussed their results with primary care providers and/or with staff from mobile mammography services before scheduling their appointment. Future research should elucidate the nuanced relationships of different, interrelated, components of healthcare, including access, regular source of care, as well as communication with different providers.
Interpersonal interactions, such as conversations with different members of one’s social network, may influence individuals’ health behaviors through perceptions of social norms and resources, and these social norms can be expected to vary across groups [25]. For example, social withdrawal from family, including a lack of conversation about results, may be particularly adverse for Latina populations, given the importance placed on family in Latin American culture [15]. In line with these hypotheses, our work suggests that Latinas who do not disclose results with family/friends appear to have elevated psychological distress relative to NLW counterparts. This research has important implications, as Latinas who receive an abnormal mammogram result experience elevated social withdrawal relative to NLW counterparts [2]. Conversely, Latinas who discuss results with family/friends appear to have comparable levels of distress relative to NLWs. This preliminary study thus offers important evidence concerning the need to understand and address ethnic disparities in the context of modifiable, social network functional characteristics.
Limitations
This study had several limitations. First, the current study is cross-sectional in nature, and thus causal relationships should not be inferred. Second, our small samples of Latina and non-Latina White women were recruited through convenience sampling. These findings are not likely to be representative of broader Latina and NLW samples. The majority of women from our sample were also recruited from mobile mammography services, which may have influenced the generalizability of our findings. Furthermore, we had particularly few women who did not disclose their results with family/friends and a small sample size in general. Relatively large sample sizes that are needed to test interactive effects: our moderation models provide estimated effects that may inform sample size calculations for larger population-based studies that are necessary to confirm our findings. These data suggest the need to further examine the relationship between functional characteristics of social networks and outcomes associated with receipt of an abnormal mammogram. We measured whether women disclosed their results to healthcare providers as well as family/friends, but did not collect data on the content of these conversations nor specified which specific family, friend, and healthcare providers were notified of results. Finally, it is important to note communication within the cancer continuum is a multi-faceted construct. Future research is needed to discern how communication impacts time to follow-up and psychologically distress after an abnormal mammogram result, especially among Latinas, in terms of to whom results are communicated, how much is communicated, and the valence of the communication.
Conclusions
Our study offers necessary pilot data for future studies interested in the role of social network characteristics in time to follow-up and psychological distress following an abnormal mammogram. In this study, we addressed the experiences of women who disclosed their results with healthcare providers as well as family/friends in relation to timely receipt of follow-up care and psychological distress. Conversations with providers were associated with fewer days to follow-up after an abnormal screening result. Latinas who do not discuss results with family/friends had particularly elevated distress. Altogether, such information demonstrates a need to examine social factors in relation to ethnic disparities following an abnormal mammogram result in order to develop evidence-based interventions to improve time to follow-up and reduce psychological distress.
Implications for cancer education research
Overall, our findings offer several potential venues for future cancer education research to characterize the psychological health of Latinas who receive an abnormal screening result and do not disclose results with family/friends. One focus of the current study was to examine the relationship of functional characteristics of social networks on time to follow-up and psychological distress. This is in part due to previous research, which has indicated structural characteristics such as network size are not associated with early cancer detection practices [24]. Functional characteristics, such as the number of individuals with whom women have conversations about cancer specifically, as well as who they are (e.g., family, friend, provider) and the strength of that relationship, may be more related to subsequent behaviors and outcomes than overall social network size. In line with this postulation, our preliminary findings suggest conversations with different members of one’s social network have different implications for time to follow-up and psychological distress. Future research should thus include data concerning the frequency and number of individuals with whom women discuss results in order to acquire a clearer, more comprehensive picture of the role of social networks in the context of the abnormal mammogram experience. These findings, if replicated, may inform future family-based interventions for women who receive abnormal screening results.
In addition to future social network analysis, more qualitative research is warranted to explore different types of social resources and support specifically in the context of the abnormal mammogram experience. Different healthcare providers as well as family/friends likely represent different social networks and may offer different forms of support to women. Future qualitative research is further warranted to examine decisions to disclose and subsequent psychosocial consequences across different cultural groups. Future research may further expand our findings by assessing the role of interpersonal communication among ethnic and cultural groups that have a similar emphasis on family and one’s social network.
Finally, another important venue to consider is future research that addresses the potential role language plays in associations between social factors, time to follow-up and psychological distress. Indeed, that may be substantial heterogeneity in access to and effects of communication with providers, family and friends within Latinas relative to Whites, given the wide breadth in English proficiency levels. On the one hand, Latinas with limited English proficiency have lower access to communication with providers and the healthcare system overall [26–28]. Simultaneously, these Latinas have been generally conceptualized as less acculturated [29] and thus be particularly responsive to communication with providers, family, and friends, due to cultural norms and values rooted within Latin America. Unfortunately, the proportion of Latinas within this sample with sufficient English was small (n = 17), and we are unable to assess the differences in associations between social factors and abnormal mammogram-related outcomes by both ethnicity and language. Nonetheless, our work provides an important springboard from which larger studies with greater samples of Latinas varying in English proficiency can test these hypotheses and provide evidence regarding the wide variation in healthcare experiences and outcomes among U.S.-based Latina populations.
Implications for cancer education interventions in practice
Our work suggests the importance of interpersonal communication for women who receive abnormal mammogram results, especially among patients and clinicians. Communication with providers may facilitate timely adherence to recommended early detection guidelines. In addition, providers may encourage Latinas who receive abnormal screening results to discuss the experience with their family and friends in order to mitigate distress. The current study thus highlights potential targets for educational interventions, including provider training with regard to communication with ethnically diverse populations and family-based patient counseling and education to promote access to social support resources.
Acknowledgements
The authors would like to thank Noah Espinoza for technical support. The current project was funded in part by multiple National Institutes of Health/National Cancer Institute grants (P50CA148143, R25CA92408) and Fred Hutchinson Cancer Research Center Faculty Development Funds. The opinions or assertions contained herein are the private ones of the authors and are not considered as official or reflecting the views of the National Institutes of Health.
Contributor Information
Yamile Molina, University of Illinois-Chicago, Fred Hutchinson Cancer Research Center.
Shirley A.A. Beresford, University of Washington, Fred Hutchinson Cancer Research Center
Tara Hayes-Constant, University of Washington, Fred Hutchinson Cancer Research Center.
Beti Thompson, Fred Hutchinson Cancer Research Center, University of Washington.
References
- 1.Ramirez AG, Pérez-Stable EJ, Penedo FJ, Talavera GA, Carrillo JE, Fernandez ME, Holden AEC, Munoz E, San Miguel S, Gallion K. Navigating Latinas with breast screen abnormalities to diagnosis. Cancer. 2013;119(7):1298–1305. doi: 10.1002/cncr.27912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Molina Y, Beresford SAA, Espinoza N, Thompson B. Psychological distress, social withdrawal, and coping following receipt of an abnormal mammogram among Latina and non-Latina White women: A mediation model. Oncol Nurs Forum. 2014;41:525–532. doi: 10.1188/14.ONF.523-532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Molina Y, Yi JC, Martinez-Gutierrez J, Yi-Frazier J, Redding K, Rosenberg AR. Resilience among patients across the cancer continuum: diverse perspectives. Clinical Journal of Oncological Nursing. 2014;18:93–101. doi: 10.1188/14.CJON.93-101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Berkman LF, Glass T. Social integration, social networks, social support, and health. In: Berkman LF, Kawachi I, editors. Social Epidemiology. New York: Oxford University Press; 2000. pp. 137–173. [Google Scholar]
- 5.Chen JM, Kim HS, Mojaverian T, Morling B. Culture and social support provision: Who gives what and why. Personaltiy and Social Psychology Bulletin. 2012;38:3–13. doi: 10.1177/0146167211427309. [DOI] [PubMed] [Google Scholar]
- 6.Heaney CA, Israel BA. Social networks and social support. In: Glanz K, Rimer BK, Viswanath K, editors. Health behavior and health education. San Francisco, CA: Jossey-Bass; 2008. [Google Scholar]
- 7.Kroenke CH, Kwan ML, Neugut AI, Ergas IJ, Wright JD, Caan BJ, Hershman DL, Kushi LH. Social networks, social support mechanisms, and quality of life after breast cancer diagnosis. Breast Cancer Research and Treatment. 2013;139:515–527. doi: 10.1007/s10549-013-2477-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Katapodi MC, Facione NC, Dodd MJ, Waters C. The influence of social support on breast cancer screening in a multicultural community sample. Oncological Nursing Forum. 2002;29:845–852. doi: 10.1188/02.ONF.845-852. [DOI] [PubMed] [Google Scholar]
- 9.Gonzalez P, Borrayo EA. Role of physician involvement on Latinas' mammography screening adherence. Women's Heatlh Issues. 2011;21:165–170. doi: 10.1016/j.whi.2010.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Molina Y, Martinez-Gutierrez J, Puschel K, Thompson B. Mammography use in Chile: The role of self-efficacy and provider, family, and friend recommendations. Health Education Research. 2013;28:784–792. doi: 10.1093/her/cyt047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lown BA, Roy E, Gorman P, Sasson JP. Women's and residents’ experiences of communication in the diagnostic mammography suite. Patient Education and Counseling. 2009;77(3):328–337. doi: 10.1016/j.pec.2009.09.019. [DOI] [PubMed] [Google Scholar]
- 12.Perez-Stable EJ, Afable-Munsuz A, Kaplan CP, Pace L, Samayoa C, Somkin CP, Nickleach D, et al. Factors influencing time to diagnosis after abnormal mammography in diverse women. Journal of Women's Health. 2013;22:159–166. doi: 10.1089/jwh.2012.3646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Poon EG, Haas JS, Puopolo AL, Gandhi TK, Burdick E, Bates DW, Brennan TA. Communication Factors in the Follow-up of Abnormal Mammograms. Journal of General Internal Medicine. 2004;19(4):316–323. doi: 10.1111/j.1525-1497.2004.30357.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Carney PA, Kettler M, Cook AJ, Geller BM, Karliner LS, Miglioretti DL, Bowles EA, Buist DS, Gallagher TH, Elmore JG. An assessment of the likelihood, frequency, and content of verbal communication between radiologists and women receiving screening and diagnostic mammography. Academic Radiology. 2009;16:1056–1063. doi: 10.1016/j.acra.2009.02.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Marin G, VanOss Marin B. Research with Hispanic populations. Newbury Park, CA: Sage Publications; 1991. [Google Scholar]
- 16.Tejeda S, Darnell JS, Cho YI, Stolley MR, Markossian TW, Calhoun EA. Patient barriers to follow-up care for breast and cervical cancer abnormalities. Journal of Women's Health. 2013;22:507–518. doi: 10.1089/jwh.2012.3590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Allen JD, Shelton RC, Harden E, Goldman RE. Follow-up of abnormal screening mammograms among low-income ethnically diverse women: Findings from a qualitative study. Patient Education and Counseling. 2008;72:283–292. doi: 10.1016/j.pec.2008.03.024. [DOI] [PubMed] [Google Scholar]
- 18.Ferrante JM, Chen P-H, Kim S. The effect of patient navigation on time to diagnosis, anxiety, and satisfaction in urban minority women with abnormal mammograms: A randomized controlled trial. Journal of Urban Health. 2007;85:114–125. doi: 10.1007/s11524-007-9228-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Weiss DS. The Impact of Event Scale: Revised. In: Wilson JP, So-kum Tang C, editors. Cross-Cultural Assessment of Psychological Trauma and PTSD. Springer US: International and Cultural Psychology Series; 2007. pp. 219–238. [Google Scholar]
- 20.Moncayo FL, Requena GC. Propiedades psicométricas de la escala revisada del impacto del evento estresante (IES-R) en una muestra española de pacientes con cáncer. Análisis y modificación de conducta. 2007;33(149):5. [Google Scholar]
- 21.Sundin Eva C, Horowitz Mardi J. Impact of Event Scale: psychometric properties. The British Journal of Psychiatry. 2002;180(3):205–209. doi: 10.1192/bjp.180.3.205. [DOI] [PubMed] [Google Scholar]
- 22.Frazier PA, Tix AP, Baron KE. Testing moderator and mediator effects in counseling psychology research. Journal of Counseling Psychology. 2004;51:115–134. [Google Scholar]
- 23.Austin LT, Ahmad F, McNally M-J, Stewart DE. Breast and cervical screening in Hispanic women: A literature review using the Health Belief Model. Women's Health Issues. 2002;12:122–129. doi: 10.1016/s1049-3867(02)00132-9. [DOI] [PubMed] [Google Scholar]
- 24.Keating NL, O'Malley JA, Murabito JM, Smith KP, Christakis NA. Minimal social network effects evident in cancer screening behavior. Cancer. 2011;1117:3045–3052. doi: 10.1002/cncr.25849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Burke NJ, Joseph G, Pasick RJ, Barker JC. Theorizing social context: Rethinking behavioral theory. Health Education Behavior. 2009;36:55S–70S. doi: 10.1177/1090198109335338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Karliner LS, Ma L, Hofman M, Kerlikowske K. Language barriers, location of care, and delays in follow-up of abnormal mammograms. Med Care. 2012;50:171–178. doi: 10.1097/MLR.0b013e31822dcf2d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Karliner LS, Kaplan CP, Juarbe T, Pasick R, Pérez-Stable EJ. Poor patient comprehension of abnormal mammography results. Journal of General Internal Medicine. 2005;20(5):432–437. doi: 10.1111/j.1525-1497.2005.40281.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Arnsberger P, Fox P, Ryder P, Nussey B, Zhang X, Otero-Sabogal R. Timely Follow-up Among Multicultural Women With Abnormal Mammograms. American Journal of Health Behavior. 2006;30(1):51–61. doi: 10.5555/ajhb.2006.30.1.51. [DOI] [PubMed] [Google Scholar]
- 29.Lara M, Gamboa C, Kahramanian MI, Morales LS, Bautista DEH. Acculturation and Latino health in the United states: A review of the literature and its sociopolitical context. Annual Reviews of Public Health. 2005;26:367–397. doi: 10.1146/annurev.publhealth.26.021304.144615. [DOI] [PMC free article] [PubMed] [Google Scholar]