Abstract
Rationale and Objectives
Anatomy is an essential component of medical education as it is critical for the accurate diagnosis in organs and human systems. The mental representation of the shape and organization of different anatomical structures is a crucial step in the learning process. The purpose of this pilot study is to demonstrate the feasibility and benefits of developing innovative teaching modules for anatomy education of first-year medical students based on 3D reconstructions from actual patient data.
Materials and Methods
A total of 196 models of anatomical structures from 16 anonymized CT datasets were generated using the 3D Slicer open-source software platform. The models focused on three anatomical areas: the mediastinum, the upper abdomen and the pelvis. Online optional quizzes were offered to first-year medical students to assess their comprehension in the areas of interest. Specific tasks were designed for students to complete using the 3D models.
Results
Scores of the quizzes confirmed a lack of understanding of 3D spatial relationships of anatomical structures despite standard instruction including dissection. Written task material and qualitative review by students suggested that interaction with 3D models led to a better understanding of the shape and spatial relationships among structures, and helped illustrate anatomical variations from one body to another.
Conclusion
The study demonstrates the feasibility of one possible approach to the generation of 3D models of the anatomy from actual patient data. The educational materials developed have the potential to supplement the teaching of complex anatomical regions and help demonstrate the anatomic variation among patients.
Keywords: 3D visualization, open-source software, anatomy
Introduction
The teaching of anatomy is in crisis, as the discipline is disappearing from many academic institutions, being subsumed by disciplines such as cell biology (1). However anatomy remains a vital element of any medical educational curriculum. Accurate diagnosis of alterations in organs or human systems requires a deep knowledge of anatomy. Radiology can play a critical role in helping medical students to recognize gross anatomic structures and their relationships to one another. The rapid development and application of imaging in medicine over the past twenty years has led to a better assessment and understanding of organ function in health and disease. In parallel, the emergence of increasingly sophisticated mathematical models, image processing and visualization tools in the field of biomedical imaging research have enabled sophisticated three-dimensional (3D) representation of anatomical structures (2). The Visible Human Project (VHP) of the National Library of Medicine pioneered the development of digital image libraries of volumetric data to serve as a common reference point for the study of human anatomy. The VHP was initiated to attempt to provide rich datasets from Computed Tomography (CT), Magnetic Resonance Imaging (MRI) and cryosection of representative male and female cadavers at an average of one millimeter intervals (3). Detailed animations and interactive 3D models of the human body such as the Visible Human 3D Anatomical Structure Viewer have been developed using the VHP data to facilitate learning of anatomy, radiological and surgical procedures (4–7). By offering the possibility to add or remove anatomical structures and to observe an organ from different angles, 3D computer-aided visualization can enhance teaching of complex anatomical areas. A wealth of innovative anatomy education resources have been developed including tools such as Anatomy TV (8) and the Visible Body (9), as well as digital atlases generated from cadaver and clinical imaging data such as the Visible Ear (10), the Digital Anatomist project (11) and RadStax (12). While these resources provide a very rich set of tools for radiological anatomy education, one of the most essential aspects of anatomy education is for students to realize the often dramatic degree of variation from one body to another. With the advent and wide availability of multi-detector CT scanners, it is now routine to obtain data in living patients that can be reconstructed at 1 mm or smaller increments. We propose to use this volume of data to demonstrate the degree of anatomic variation between patients for medical education purpose. This paper present the results of our pilot study to assess the feasibility of the development of teaching modules for anatomy education of first-year medical students based on 3D reconstructions from actual patient data. We chose three of the most complicated regions of the body for this project, and recruited fourth-year medical students to participate in building models. In this way, we used senior students in a manner analogous to a traditional approach, where senior students could serve as preceptors for junior students, sometimes preparing prosections for anatomic study. Our students prepared ‘digital prosections’, learning the anatomy of these regions themselves in the process. Our goal was to determine the feasibility of this method of teaching, and to elicit feedback from first-year anatomy students on whether they felt that the use of 3D models helped them gain a deeper understanding of the shape and spatial organization of anatomical structures, as well as an appreciation of anatomical variation among patients that is so important in actual clinical practice.
Needs Assessment
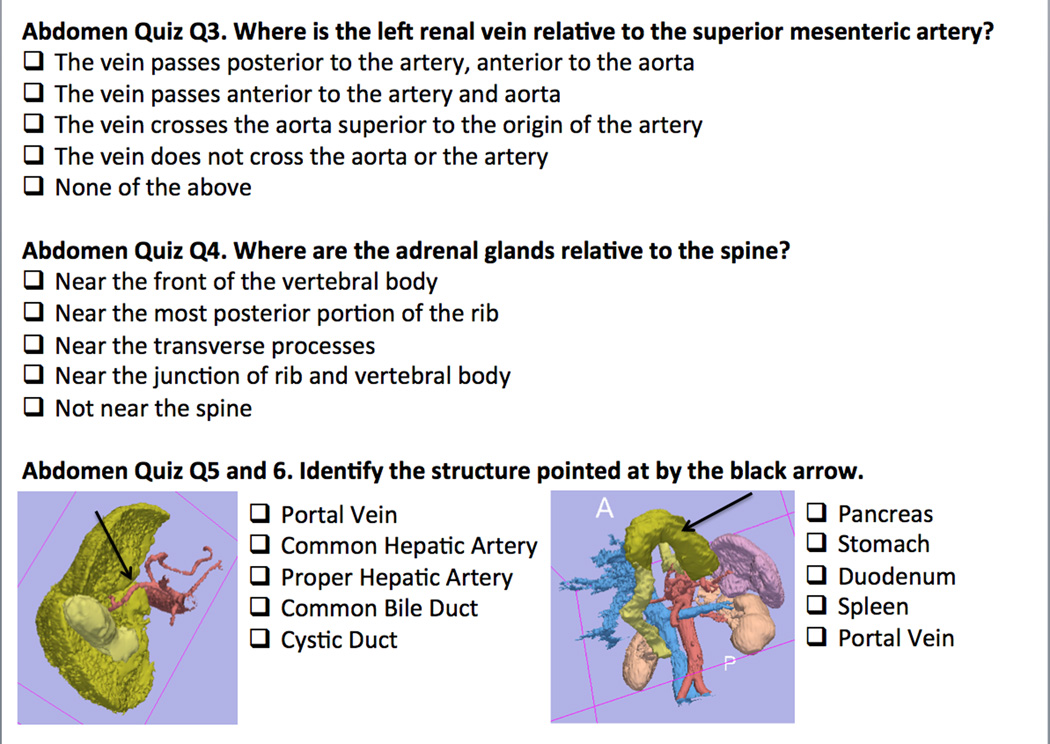
Medical school institutional review board approval was obtained for use of anonymous student feedback and anonymous optional test results. Two anonymous optional online quizzes consisting of 13 questions each were offered to students in a first-year medical anatomy course. Students were informed that quiz results would have no affect on their course grade and that quiz material would not be used in the final exam for the course. The first quiz covered structures in the upper abdomen and the second quiz covered structures in the pelvis. A quiz for mediastinal structures was also developed but was not administered due to technical difficulties. Questions in the quizzes were designed to assess both student ability to recognize structures in 3D representations in various orientations, as well as to demonstrate their understanding of spatial relationships between structures. Figure 1 shows a set of representative quiz questions for the upper abdomen.
Figure 1.
Abdomen quiz. The figure shows examples of questions from the online abdomen quiz that was offered to first-year medical students to assess their comprehension in the areas of interest. The associated screenshots show 3D models of the abdominal structures of two different cases: Q5 : abdominal aorta and its branches (red), liver (dark yellow) and gallbladder (light yellow) ; Q6 : stomach (dark yellow), duodenum (light yellow), abdominal aorta and its branches (red), inferior vena cava (blue), hepatic vein (blue), kidney (light pink), and spleen (light purple).
3D Modeling of Anatomy
Anonymized CT datasets from 16 patients were collected, including imaging of the mediastinum (five datasets), the abdomen (six datasets) and the pelvis (three female datasets and two male datasets). IRB exemption was obtained from the hospital of origin of the cases for use of anonymized clinical images for teaching purpose. Cases were selected for their optimal demonstration of normal anatomy as well as for variation in anatomy. Some cases included minor abnormalities or anomalies for comparison to normals. Images were acquired on a multi-detector CT Scanner (Somatom Sensation 16-slice CT scanner, Siemens, Erlangen, Germany), resulting in 18 series of 200 slices with a slice thickness of 1.5 mm, and pixel dimension of 1.4 × 1.4 mm. We used an open-source Digital Imaging and Communication in Medicine (DICOM) management program, Osirix (13), to transfer and anonymize the clinical datasets. The images were loaded on a standard computer (IBM Think Pad T42p PC, 1GB Ram, 60 GB Hard drive, ATI Mobi Fire GLT2 128 MB, Armonk, NY) for post-processing. 3D surface modeling of the anatomical structures was performed using the 3D Slicer open-source software platform (14). 3D Slicer or simply 'Slicer' is a medical image computing platform used in clinical research worldwide. The platform is majoritarily funded by the U.S. National Institutes of Health through a multi-institutional effort of large scale biomedical research consortia that include the National Alliance for Medical Image Computing, the Neuroimage Analysis Center and the National Center for Image-Guided Therapy.
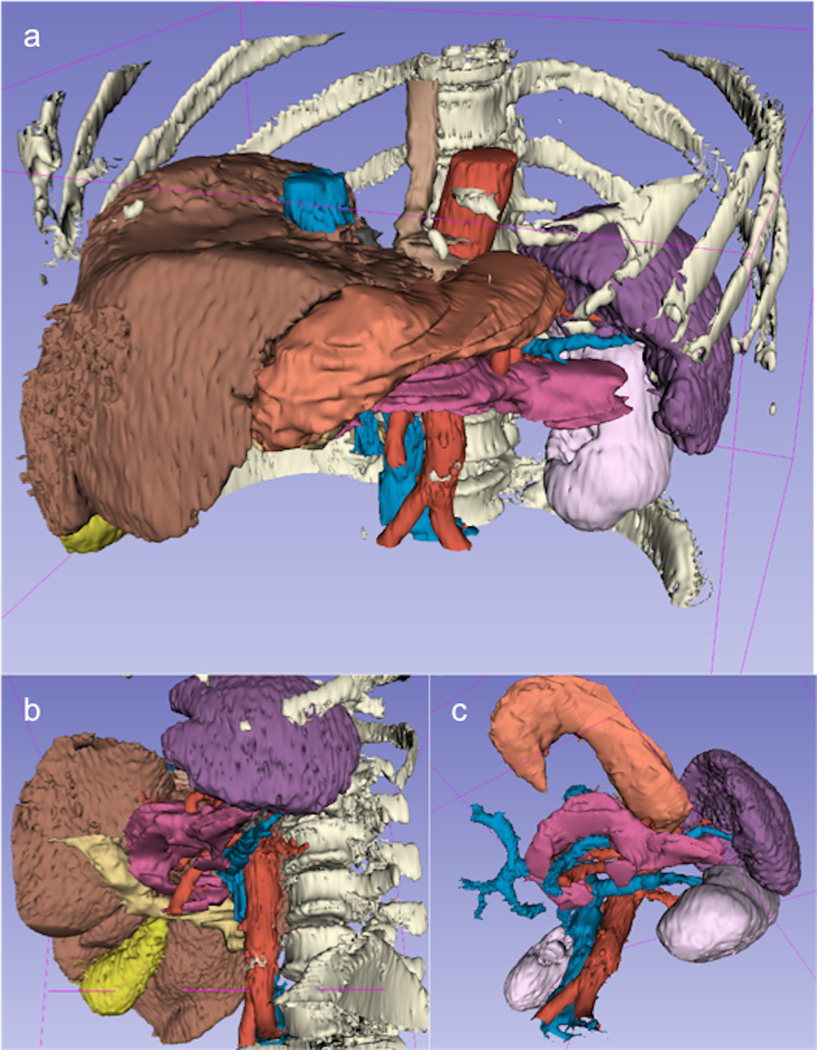
Initial modeling of mediastinal structures was performed by the senior radiologist (over 15 years experience in thoracic imaging and medical student education) and a programmer with expertise in the use of the modeling software. The generation consisted of three steps: first, each volume was resampled using tri-linear interpolation, second, the anatomical structures were segmented from the images, and third, the models were generated using the marching cubes algorithm (15). Figure 2 shows an example of 3D anatomical models of the mediastinal structures. Two fourth-year medical students were recruited to assist in preparation of additional models, and received a brief introduction to the use of the software from the programmer. To enhance the demonstration of the spatial position and orientation of the different anatomical structures, a hierarchy based on four different categories - organs, arteries, veins and bones - was generated for each patient case. Each model was assigned a position within this hierarchy, as shown in Tables 1–3. The fourth-year students used semi-automated segmentation to outline the contours of the anatomical structures of interest, and performed manual adjustments to improve the accuracy of the segmentation. Initial models were reviewed with the senior radiologist for assessment of quality and accuracy. Any necessary manual corrections were then made prior to use of the models in the teaching sessions. Figure 3 shows an example of 3D anatomical models reconstructed by the students for the upper abdomen. There was no attempt to produce completely smooth models, as the emphasis was on rapid production that would allow modeling of numerous structures in several patient datasets in a reasonable length of time. Students recorded approximately how long they spent working on each model from start to completion.
Figure 2.
3D anatomical models of the mediastinum. The figure displays the airways (blue), the pulmonary artery (pink) and the esophagus (yellow). The opacity of the aorta (red) has been lowered in order to facilitate the visualization of posterior structures. These models were created by the senior radiologist and programmer over several weeks.
Table 1.
Anatomical models of the mediastinum
| Organs | Vessels | Bones |
|---|---|---|
| Heart | Arteries | Thoracic spine |
| Left atrium | Ascending aorta | Ribs |
| Left ventricle | Aortic arch | Sternum |
| Right atrium | Descending aorta | |
| Right ventricle | Pulmonary artery | |
| Esophagus | Veins | |
| Thymus | Superior vena cava | |
| Inferior vena cava | ||
| Azygos vein |
Table 3.
Anatomical Models of the Pelvis.
| Organs | Vessels | Bones | Muscles |
|---|---|---|---|
| Urinary | Arteries | Pelvis | Pelvic |
| Bladder | Common Iliac | Sacrum | Coccygeus |
| Urethra | Internal Iliac | Femur | External anal sphincter |
| Gastrointestinal | External Iliac | Levator ani | |
| Sigmoid colon | Veins | Thigh | |
| Anus | Common Iliac | Quadratus femoris | |
| Genital (male) | Internal Iliac | Obturator externus | |
| Internal genital | External Iliac | Obturator internus | |
| Prostate | Piriformis | ||
| Vas deferens | Pectineus | ||
| Testes | Adductor brevis | ||
| External Genital | |||
| Cura of penis | |||
| Bulb of penis | |||
| Genital (female) | |||
| Internal Genital | |||
| Uterus | |||
| Cervix | |||
| Vagina | |||
| Ovaries | |||
| External Genital | |||
| Crura of clitoris | |||
| Bulb of vestibule | |||
| Bartholin's glands |
Figure 3.
3D anatomical models of the upper abdomen. The figure displays the liver (dark yellow), stomach (brown), esophagus (light yellow), spleen (light purple), pancreas (dark pink) and air-filled bowel (cyan), along with the aorta (red), inferior vena cava (blue) and portal vein (blue). The opacity of the bowel has been lowered to allow deeper structures to become visible. These models were created by two fourth-year medical students.
Computer-Assisted Teaching of Radiological Anatomy
Teaching modules were prepared covering three different regions of anatomy: the mediastinum, the upper abdomen and the pelvis. These regions were chosen because they are each difficult areas for students to understand, and contain many complex structures of clinical importance. There were 171 students in the first-year anatomy course in year 1 of the project, 172 first-year students in year 2 and 178 first-year students in year 3. Students were invited to participate in optional 3D workshops during their anatomy course via online announcements on the course website.
In year 1 of the project, 3D Slicer was loaded onto approximately 20 computers in one of four student labs. Students who chose to participate were given access to the mediastinal datasets. Ability of the students to use the software and the quality of their interactions with the models was assessed with direct observation by faculty.
In year 2 of the project, first-year students were offered two optional workshops on mediastinum and two workshops on upper abdomen. Each workshop began with a didactic introduction on the 3D Slicer software, including a short hands-on training session on how to manipulate and rotate the models, in order to provide students the necessary instruction on the use of the 3D visualization program prior to the educational session. Students were then given a list of tasks to be completed using the models for the particular anatomic area under discussion. Students were requested to save and provide screen shots of the images that they obtained using 3D Slicer to complete each task. Students were then asked to fill out an optional anonymous online survey on their assessment of the educational value of their experience at the end of each session. Supplementary Table S1 and Supplementary Figure S1 provide examples of the mediastinum tasks and survey, respectively.
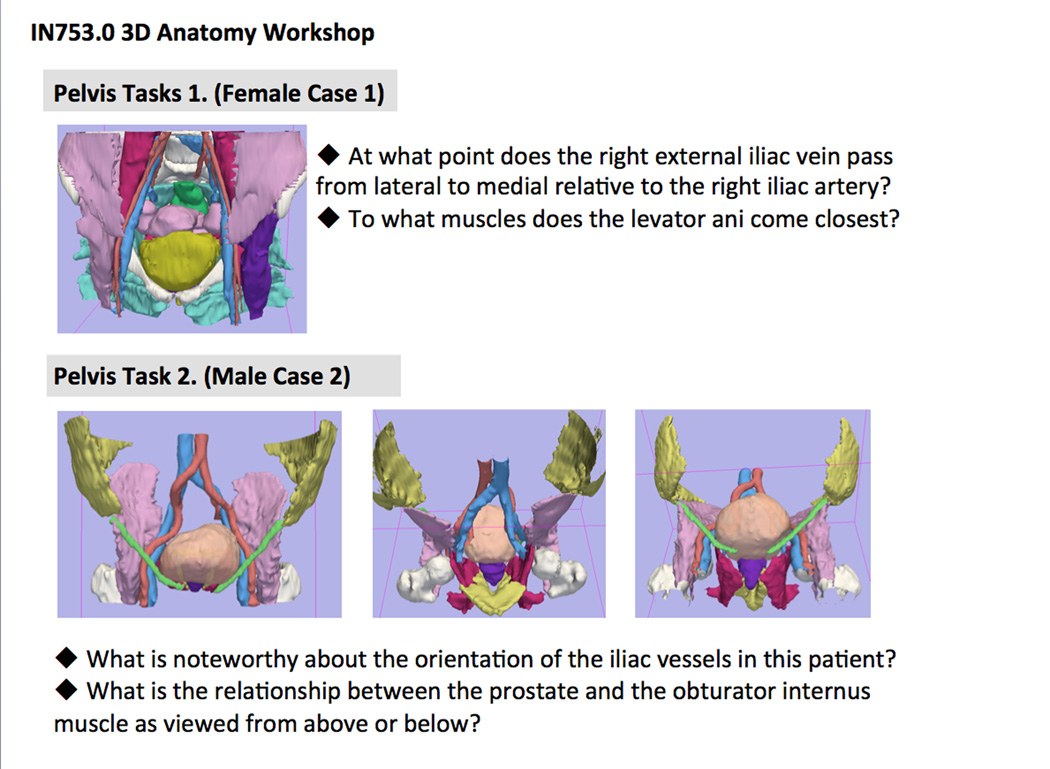
In year 3 of the project, first-year students were offered either of two optional 3D workshops in each of three areas: mediastinum, upper abdomen and pelvis. The workshops each began with a didactic introduction to use of the software, followed by distribution of a list of tasks to be completed. Tasks were designed to require students to use all of the features of 3D Slicer while working with models, including adjustment of model transparency, selection of which models to view and which to hide, and rotation of models to best demonstrate anatomic relationships. Figure 4 shows an example of tasks from the pelvis workshops, along with screenshots of the corresponding 3D models. Students in year 3 were asked to work in groups, to turn in a written account of their conclusions based on the assigned tasks, and were again asked to fill out an optional online survey regarding their qualitative assessment of the educational value of the workshop.
Figure 4.
Pelvis workshop tasks. The figure shows a set of representative tasks for first-year students from the pelvis workshop. The associated screenshots show 3D models of corresponding anatomical structures in a female case and in a male case.
Results
Generation of 3D Models
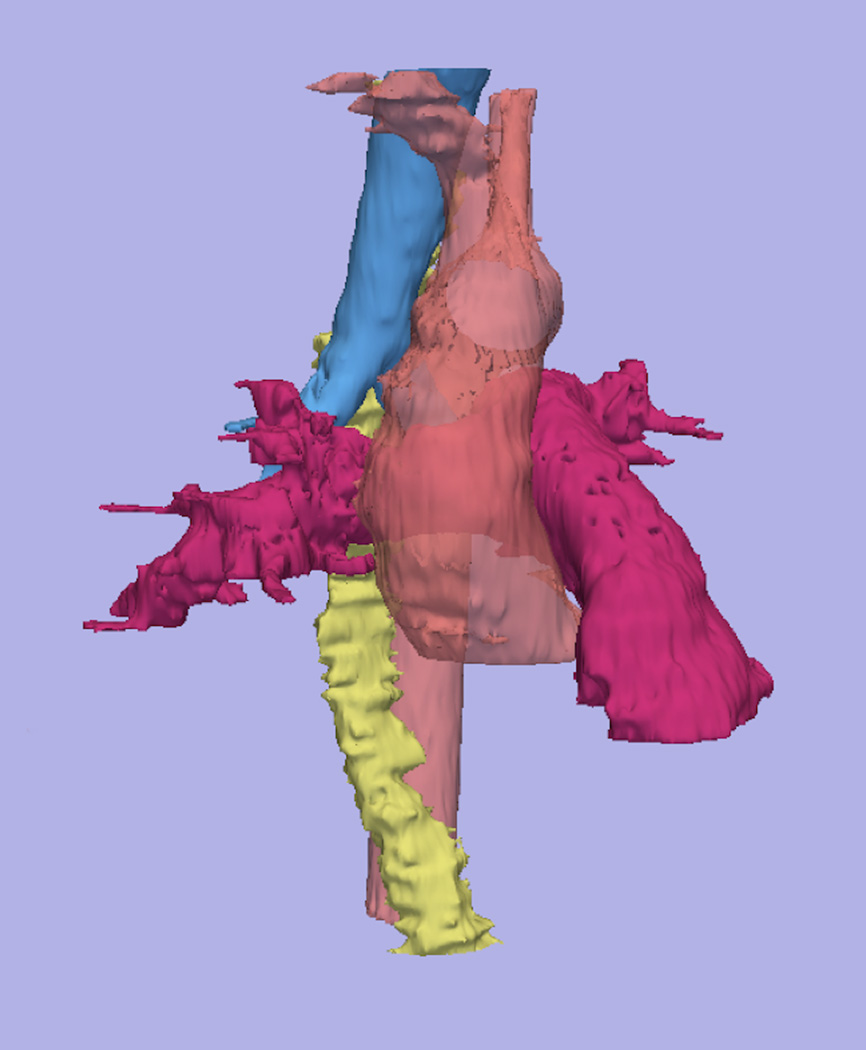
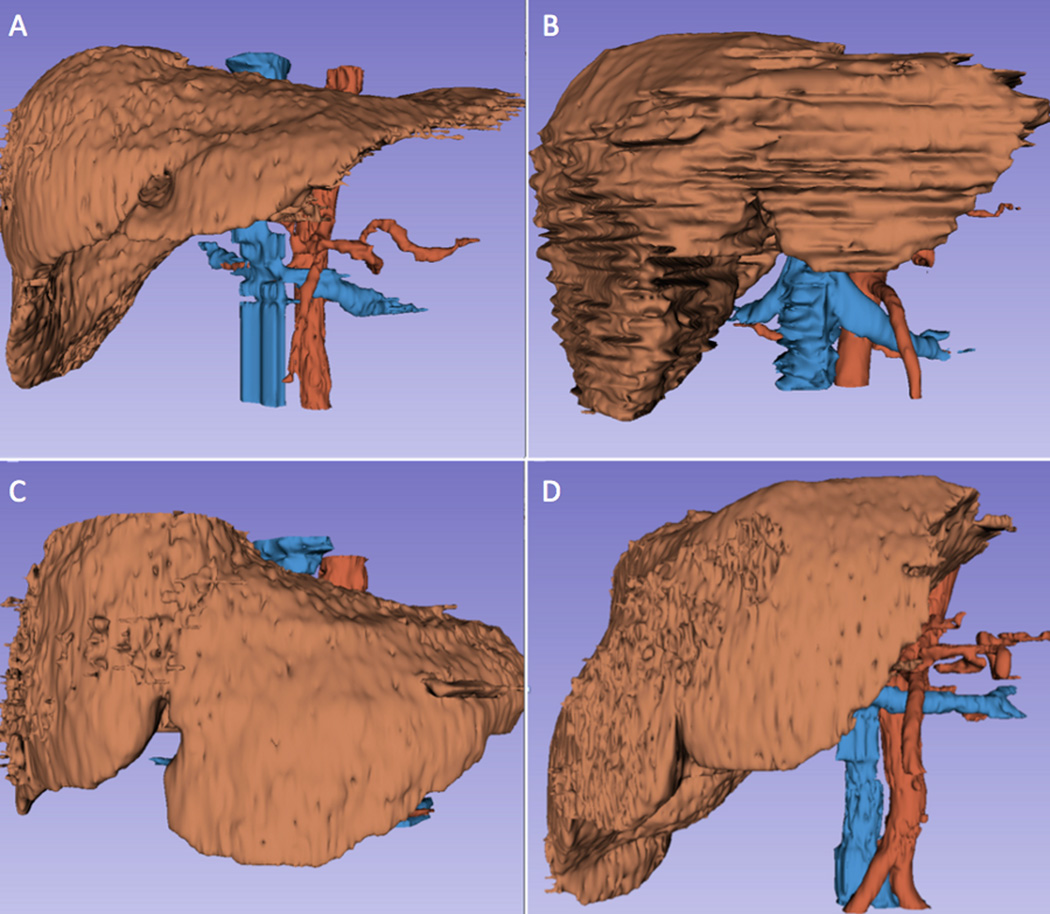
Initial time to generate models by the programmer and senior radiologist ranged from 10 to 90 minutes per structure, depending on the success of the semi-automated component of the segmentation and how much manual segmentation was needed. The anatomical models of the mediastinum, abdomen and pelvis that were generated are listed in Table 1, 2 and 3 respectively. For vascular structures, such as the aorta, that demonstrated adequate contrast with surrounding structures, automated segmentation required little modification. For structures such as the esophagus with less contrast relative to surrounding tissues, extensive manual segmentation was required. The models for the mediastinum included normal cases and slightly abnormal cases of an aortic aneurysm, a thick left ventricle, a dilated esophagus and a right arch aorta. The models of the abdomen illustrated the major structures of the digestive system and liver (Figure 5). The models of the pelvis described anatomical structures of two male patients and three female patients. Supplementary Figure S2 and Figure S3 show examples of the structures reconstructed in a male patient and in a female patient, respectively. Datasets for the abdomen were selected to show normal variation in liver anatomy, and the degree of variation in final models is illustrated in Table 4 and Figure 6.
Table 2.
Anatomical models of the upper abdomen
| Organs | Vessels | Muscles |
|---|---|---|
| Adrenal glands | Arteries | External Obliques |
| Duodenum | Common Iliac | Internal Obliques |
| Esophagus | Internal Iliac | Rectus abdominis |
| Gall bladder | External Iliac | Iliacus |
| Liver | Veins | Psoas |
| Kidneys | Common Iliac | |
| Pancreas | Internal Iliac | |
| Spleen | External Iliac | |
| Stomach |
Figure 5.
3D models of the abdomen. The figure displays the liver (brown), stomach (orange), gall-bladder (yellow), spleen (dark purple), kidney (light purple) and pancreas (pink) together with major vessels and bones. (5a) Examples of 3D views (5b and 5c) of these structures that were generated by rotating the models with the 3D Slicer software platform. The models were created by a fourth year medical student over the course of an elective month in radiology.
Table 4.
Dimensions and volume of the liver in three anatomical directions (I-S: Inferior-Superior; R-L: Right-Left; A-P: Anterior-Posterior)
| Case A | Case B | Case C | CaseD | |
|---|---|---|---|---|
| I-S (mm) | 159 | 165 | 130 | 185 |
| R-L (mm) | 251 | 234 | 323 | 207 |
| A-P (mm) | 199 | 225 | 190 | 226 |
| Volume (ml) | 1,302 | 2,322 | 1,380 | 2,184 |
Figure 6.
3D models of the liver. The figure shows the anatomical shape variations of the liver (brown) among four different patients. The aorta (red) and inferior vena cava (blue) are displayed for anatomical reference.
Two fourth-year medical students were recruited to assist in development of additional models from among all students with an expressed interest in radiology. One student went on to match in a radiology residency and the other chose emergency medicine. One senior student created models for the pelvis and the other created models for the upper abdomen as well as adding more structures to the existing mediastinal datasets. All models generated by the two senior students were reviewed by the senior radiologist upon completion for accuracy. Both senior students were able to begin making models after minimal training by the programmer, and rapidly became adept. Neither had used 3D Slicer prior to the project. Typical time required to generate a simple model by the senior students was approximately 10 minutes. For more complex structures or for structures requiring considerable manual segmentation, typical time for completion of each model was approximately 45 minutes. Both senior students felt that they learned the anatomy of their region in considerable depth through generation of models, and this was evident in sessions with the senior radiologist to fine-tune models and eliminate incorrect segmentation. Total numbers of models created by the two senior students were 104 models for the liver anatomy and 88 for the pelvis anatomy.
Results of Upper Abdomen and Pelvis Quiz
A total of 23 first-year students completed the upper abdomen quiz, and 51 first-year students completed the pelvis quiz. Online quizzes prior to completion of 3D modeling sessions showed considerable confusion among students regarding spatial relationships in the areas considered. The average score of the students was 8.1±2.0 and 7.1±1.7 (on a 13.0 scale) for the abdomen quiz and pelvis quiz, respectively.
3D Anatomy Workshops
521 first-year medical students attended the 3D anatomy workshops in study years 1, 2 and 3. Students at all sessions were able to use the software in less than 10 minutes after the initial didactic introduction and a short hands-on guided use of the program at computer workstations. Observation of first-year students using the models in year 1 showed that they were quickly able to learn to manipulate and rotate models but students expressed confusion as to what they should be doing, as well as a desire for more models for each case. Most students did not stay for the entire assigned time of the workshop in study year 1. In year 2 and 3 of the study, with defined tasks, first-year students demonstrated more enthusiasm while working with the models, and asked more sophisticated questions to the session observers. Most students stayed for the entire time assigned and most expressed considerable interest in pursuing more opportunities to work with 3D models in study years 2 and 3. Students in study year 2 found the saving of screenshots to be cumbersome and difficult. Use of paper forms to record task completion in study year 3 was easier for students.
Task Forms
A total of 8 completed task forms were available from the pelvis workshops and a total of 11 complete or partially complete task forms were available from the abdomen workshops in year 3 of the project. Because of technical difficulties, no task forms were available from the mediastinum workshops.
Tasks for abdomen and pelvis began with identification of all unlabeled structures in the model hierarchy of the first case. The majority of returned forms showed accurate identification of all structures. Review of task forms demonstrated that the majority of students were able to recognize important anatomic relationships such as the orientation of the adrenals relative to the kidneys in the anterioposterior plane, the location of the splenic artery vs. splenic vein relative to the pancreas, and the attachment points of various muscles of the pelvis.
Students were able to describe relationships, such as the orientation of the body of the uterus to the vaginal canal in a patient with a markedly anteverted uterus. Students were able to recognize structures when viewed from unusual angles, such as the prostate and seminal vesicles viewed from above or the liver viewed from below. They were also able to describe the relationships between bony landmarks and underlying vascular structures/organs and to identify structures that pass from one region of the body to another, as in the thigh and pelvis. Since the tasks were not designed as a test, and students worked in groups on the tasks, no scoring of these forms was performed.
Qualitative Feedback
In year 2 and 3, there were 26 completed online surveys regarding the 3D anatomy workshops. Overall response rate was 75%. Eleven students provided comments on the mediastinum workshop, seven on the abdomen workshop, and the remainder did not indicate which workshop they had attended. Students reported spending an average of 60 minutes working with models during the session (range 15 minutes to 120 minutes). On a scale of 1 (expert) to 5 (computer illiterate) regarding their proficiency with computers, student average self-rating was 1.8. Eighteen of the students rated the introductory session on use of 3D Slicer as 1 (excellent) while the remaining 8 rated the introductory session as 2 on a scale of 1–5.
Fourteen of the students indicated that the workshop gave them a better understanding of 3D relationships while 16 students indicated that the session gave them a chance to review what they had learned in gross lab. Four students noted that the session demonstrated the range of normal anatomic variation. Nine students indicated that the session was appealing because it was innovative and novel and 13 indicated that the session enhanced their understanding of how 3D structures appear on cross sections. Overall, there were 68 positive comments selected by the students regarding the session.
Two students indicated that the program did not run properly, one student could not find the program and 5 stated that they did not have enough guidance in use of the program while 3 indicated that the program was too hard to use. Two students indicated that they did not understand what they were supposed to do with the program, one indicated that the session was just fun and not educational, 5 indicated that they would have preferred more explanatory text, and one stated that the models were too obvious and that the 3D aspects did not add anything. Two students stated that the process took too long. Overall, there were 24 negative comments selected by the students.
Most suggestions from students indicated a need for more models per patient and a desire for similar sessions for other complex anatomical areas, such as the pelvis in which surrounding bony structures limit visualization of organs and muscle. These comments were submitted prior to the pelvis sessions. Several students expressed a desire for more detailed models and several mentioned the slowness of the computers that were used for the session. Several students stated that they found the program complex to use and had to spend most of the time during the workshop learning how to operate it rather than manipulating the models. One student indicated that the quality of the models was insufficient to demonstrate the anatomy. Other student text comments included:
“The 3D imaging was really helpful in visualizing areas of the body that we could not see clearly in lab. Because the spatial relationships and surface anatomy are so important for clinical practice, the 3D imaging is such a useful learning tool, and I hope that all of the areas of the body can be studied this way (especially the pelvis!).”
“Bravo! I think this should replace cadaver study.”
“I found the comparison of the model with CT images to be the most helpful aspect of this program.”
“Visualizing 3D objects in 2D images (such as in CT, MR, and US) is really difficult, and I think Slicer is an invaluable tool to help us to do that!”
“It would be nice to be able to easily compare images on Slicer from different cases, in particular to view various anatomical variations or to compare a variation to the normal structure.”
“I think it would be a useful tool in radiology lab to use alongside the current online modules.”
“This session was fantastic! I gained a new appreciation of being to see the body in 3D terms. Initially I got a little frustrated trying to figure the program out -- but, in time I was able to use it sufficiently well to learn from the program. I only wish that Slicer could be installed on all of the computers in the other skills areas so more students could use it.”
“This is something that is very useful if you have a hard time seeing things in dissection, plus it really helped my visualize CT scans. I also worked in a small group which I also thought was very beneficial.”
“As long as it's complete, I think it will be a fantastic learning tool.”
Regarding specific program features that students used during the session, 15 students noted the ability to add/remove structures, 11 noted freehand rotation, 10 noted automated rotation, 15 noted ability to superimpose CT images on models, and 11 noted ability to change transparency as particularly helpful. Eight students indicated that they planned to install Slicer on their own computer for future use. Regarding the overall experience of using this program to explore anatomy, the average rating by students was 1.5 on a scale from 1 (excellent) to 5 (poor). Fourteen students indicated that they would recommend this session as a learning tool for other students. Structures that students suggested as potential additions for future workshops included nerves, more cardiovascular structures, heart chambers, collateral pathways for veins, and neck structures.
Conclusion
Understanding of gross anatomic structures requires a grasp of complex spatial relationships. The mental representation of the shape and organization of different structures is a crucial step in the learning process of anatomy. A thorough understanding of 3D anatomic relationships is vital in interpretation of most types of imaging studies, in surgical approaches to treatment of disease, and in physical diagnosis of most parts of the body other than the skin.
Traditionally, the gross lab has been the venue for students to gain such understanding, through actual visualization and manipulation of the 3D objects in their cadavers. However, many forces are at work to curtail the time available for students to experience this valuable learning method. With the decrease in time in the basic science curriculum and the decrease in funding for cadavers, other methods must be sought that can provide students with a deep understanding of the shape, orientation and relationship of important structures in the body. Modern imaging methods offer the potential to supplement traditional teaching methods for anatomy.
One possible approach to digital presentation of anatomy has been demonstrated by the Visible Human Project, where a robust anatomic dataset has been generated from a few donated bodies. This data has been used to generate a ‘virtual reality’ view of human anatomy, with models that have been rendered using extremely sophisticated graphic and animation software representing years of work by a large number of programmers and graphic designers. This data clearly has great value in the teaching of anatomy, and can be thought of as an extremely complete 3D atlas of anatomy.
With the advent of multi-detector CT scanners, it is now a routine to obtain 1 mm or thinner datasets on studies of living patients. This volume of data offers the opportunity to produce teaching models that may actually demonstrate some aspects of anatomy even better than in the cadaver. It is very hard to gain an appreciation of the internal structure of the liver vasculature and lobar anatomy in most cadavers, but using 3D CT data, this can be clearly represented. In addition, digital teaching of anatomy allows depiction of structures that might be damaged or destroyed during dissection. The position of organs in CT data is probably a closer representation of what might be encountered in the operating room than the fixed and sometimes contracted tissue of the cadaver. The limitations of the Visible Human approach are mainly related to the small number of bodies used and the expense of creating such elaborate renderings.
Our project attempted to approach digital teaching of anatomy in a very different way, providing quick ‘sketches’ of structures showing the range of normal from several different patients. Using 3D Slicer, which is a free open-source software package, anatomic models can be generated relatively quickly with some initial time required for training in the use of the software. The only requirements are a computer lab, which is commonly available in many medical schools, and sufficient training time for faculty to learn to use the software. In this way, dissection can be supplemented with another teaching method that also emphasizes three-dimensional representation of anatomic structures and their relationships. The ability to rotate, remove, and otherwise manipulate models by learners allows to demonstrate these relationships, including some that are difficult to display with dissection, as previously noted. Such an approach could help compensate for continued decreases in curricular time devoted to dissection. While this method cannot replace dissection, it can supplement it and offers students one more way to explore anatomy, both in class and on their own without requiring additional lab time.
The anatomical models were mostly created by senior students for use by junior students. In this way, we were continuing a long tradition of using senior students as gross lab preceptors, now asking them to produce ‘digital prosections’ of anatomic structures for the teaching of their junior colleagues. This is a win-win situation, with the senior students learning the anatomy of their area of interest in great detail from building models through repetition while the junior students have a larger variety of specimens to examine. While we specifically invited senior students who were interested in radiology to participate as ‘digital prosectors’, any student who is interested in learning anatomy in more detail would likely benefit from such an experience. Students interested in obstetrics or general surgery might all be likely prospects for this task. The younger generation of students is very facile in using computer programs and most students learned the Slicer interface quickly. However, in generating models, students definitely needed guidance from a radiologist in outlining normal structures, just as students in the dissection lab need guidance from anatomists in locating and defining structures. This guidance could be provided by a faculty member in radiology, as was done in our study, but since the structures are generally normal, even a motivated radiology resident could provide this assistance. The list of tasks for fourth-year ‘digital prosectors’ were initially provided by the senior radiologist, but students could be encouraged to participate in deciding what structures to include.
By use of many different patient datasets, anatomic variation can be clearly illustrated. One of the things that is always a surprise to students in the first year is when they discover that the cadaver of the anatomy laboratory does not look like the illustrations in their textbooks. It is very important for students to understand from the beginning of their training that every person is unique and every anatomical structure is a slightly different shape. By producing a large number of quick and crude models from a large number of actual living patients, this concept can be made graphically apparent to students.
An important lesson was learned in year 1 of the project, which is that students will not benefit from even very elaborate models if they are not given something concrete to do with them. Simply providing the images is not enough. Students did rotate the models in year 1, and were intrigued for the first 15 minutes of the workshop, but without specific goals, they did not feel compelled to truly explore the models or use all of the software tools for variable transparency and visualization. In order for 3D models to really be of educational value, students must be given tasks to perform that will force them to manipulate the data and explore the information before them. In years 3 and 4 of the project, the level of student engagement was much higher, and students stayed for the entire allotted time, expressing considerable enthusiasm for the process. In addition to the online feedback forms, five students specifically commented in their final course evaluations for anatomy regarding the educational value of the 3D modeling workshops.
The 3D models could be freely oriented to provide the best working view for each student. In observing students using the models, it was evident that this functionality was key for the understanding of complex anatomical structures. Student groups would frequently express dramatic enthusiasm as the answers to the assigned tasks became clear to them through rotation, careful selection of which models to view, and variation in transparency of structures. The ability to move the models gave students a graphic understanding of the complex shapes and surfaces, even though the models were not smoothly rendered or life-like in appearance. Additional optional tasks could be designed to encourage students to continue to work on their own after the initial teaching workshop. Since 3D Slicer is freely available, each interested student could download it to their own laptop and be given datasets to explore on their own.
Our study has a number of limitations. The number of students who volunteered to participate was small. Although written questionnaires showed generally positive feedback from the students, this is by no means a quantitative evaluation of learning, which remains a challenging problem in assessment. No direct comparison of this teaching method with dissection or other teaching methods was possible, since all students in the course were also actively involved in dissection as their primary learning method. The students who attended the 3D modeling sessions had access to all additional resources for the course, so we were not able to assess the benefits from the use of 3D modeling in isolation from the use of textbooks, dissection and course notes.
As this study was designed primarily to assess the practicality of generation of models by radiologists and senior students, as well as initial response of junior students to the teaching methods, we feel that our goals were accomplished in spite of the small number of students involved and the lack of quantitative assessment. A subjective indicator of how much students learned during the 3D workshops was gained by reviewing questions generated by the students during the sessions, which showed a sophisticated understanding of relationships that was not evident in their responses to the initial online quizzes.
Another limitation of our study is related to the fact that our 3D modeling sessions were optional, which likely led to biases in various directions with respect to which students chose to attend the sessions. Students who were particularly interested in computers or radiology might have been attracted to the 3D workshops, while at the same time students who were struggling with the course material might have chosen to attend to obtain additional help. Not all students are equally comfortable using digital learning methods. In an ideal teaching setting, many different teaching methods should be offered to appeal to all possible student learning styles. The younger generations of students generally are more and more comfortable with computers, but this is not universal. The degree of computer skill needed to participate in the first-year sessions was not high, and particularly if students work in groups, the members with the most comfort with computers can take on the assignment to run the program, while other group members can participate in other ways, such as identifying structures, suggesting manipulations to try, and proposing answers to task questions.
In a similar way, the two students who volunteered to build models are not representative of the entire student body, and were both at interested in careers in radiology, which biased this sample toward an aptitude for working with computers that may be higher than the average student. In the same way that students who volunteer to become anatomy prosectors are likely to be those with particular interests and skills in this area, students who choose to become ‘digital prosectors’ are also likely to be those with the most interest in anatomy and the most comfort with digital methods. The degree of time commitment for the ‘digital prosection’ portion of the project is much higher than for those who merely participated in workshops and learned to use the display functions of 3D Slicer. Only a motivated student would be likely to devote the time to the project of developing models, but an average student can quickly learn to view and manipulate existing models.
In summary, our study demonstrates the feasibility of one possible approach to the generation of 3D models to supplement anatomic teaching, and describes a practical and inexpensive method of 3D visualization of anatomy from actual patient cases. The design of interactive tasks using 3D models can provide students with a personal approach to the identification of regions of interest, and the ability to interactively manipulate the models gives students a graphic mental picture of shapes and relationships that may be more useful than 2D drawings or atlases. Future work could include the generation of 3D models of more complex structures, such as the segments of the liver for use by higher-level trainees such as radiology residents, as well as larger scale and more quantitative comparisons of this teaching method with more traditional methods such as dissection. Education in radiological anatomy plays an important role in the training of those who will ultimately interpret patient data, and this pilot study demonstrates the potential benefits of a transfer of advanced image analysis techniques to medical education.
Supplementary Material
Supplementary Figure S1. Mediastinum module survey. The figure shows the on-line evaluation questionnaire that was distributed to the students following the 3D anatomy educational session on the mediastinum.
Supplementary Figure S2. 3D models of the male pelvis. The figure displays a tilted anterior view demonstrating the position of the inguinal ligament (green), the thigh muscles (pink), the prostate (dark purple) and the bladder (light orange). Iliacus muscles (light purple), pelvic muscles (yellow) are also shown along with proximal femurs (white). These models were created by a fourth year medical student during an elective month in radiology.
Supplementary Figure S3. 3D models of the female pelvis. The figure displays a tilted anterior view of the following structures : sacrum and iliac bone (white), iliac arteries (red), iliac veins (blue), uterus (light purple), ovaries (dark purple), anus (dark green), bladder (light yellow) and sciatic nerve (bright yellow). The figure also shows the following muscles : piriformis (bright yellow), pectineus (light green), psoas (dark pink), quadratus femoris (light orange), obturator externus (cyan) and obturator internus (dark blue). The opacity of the abdominal muscles has been lowered to enhance visualization of internal structures. These models were generated by the same fourth year medical student as the models in Supplementary Figure 2.
Acknowledgments
The authors are grateful to the Radiological Society of North America (RSNA), the Association of University Radiologists (AUR), the Association of Program Directors in Radiology (APDR), and the Society of Chairmen of Academic Radiology Departments (SCARD) for funding this project through the RSNA/AUR/APDR/SCARD Radiology Educational Research Development Grant ERD0501. S.P. and R.K. were supported in part by the Neuroimage Analysis Center (NIH P41EB015902), the National Center for Image-Guided Therapy (NIH P41EB015898), and the National Alliance for Medical Image Computing (NIH U54EB5149).
Abbreviations
- 3D
Three Dimensional
- VHP
Visible Human Project
- CT
Computed Tomography
- MRI
Magnetic Resonance Imaging
- DICOM
Digital Imaging and Communication in Medicine
Contributor Information
Sonia Pujol,
Michael Baldwin,
Joshua Nassiri,
Ron Kikinis,
Kitt Shaffer,
References
- 1.Vazquez R, Riesco JM, Carretero J. Reflections and Challenges in the teaching of human anatomy at the beginning of the 21st century. Eur J Anat. 2005;9(2):111–115. [Google Scholar]
- 2.Duncan JS, Ayache N. Medical image analysis: progress over two decades and the challenges ahead. IEEE Trans Pattern Anal Machine Intell. 2000;22:85–105. [Google Scholar]
- 3.Spitzer VM, Ackerman MJ, Scherzinger AL, Whitlock DG. The Visible Human Male: a technical report. J Am Med Inform Assoc. 1996;3:118–130. doi: 10.1136/jamia.1996.96236280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pommert A, Hohne KH, Plesser B, et al. Creating a high-resolution spatial/symbolic model of the inner organs based on the Visible Human. Med Image Anal. 2001;5:221–228. doi: 10.1016/s1361-8415(01)00044-5. [DOI] [PubMed] [Google Scholar]
- 5.Gehrmann S, Hohne KH, Linhart W, Pommert A, Tiede U, Yarar S. A detailed 3D model of the human hand. J Visualization. 2004;7:221. [Google Scholar]
- 6.Burmester E, Leineweber T, Hacker S, Tiede I, Hutteroth H, Hohne KH. EUS meets Voxel-man: three-dimensional anatomical animation of linear-array endoscopic ultrasound images. Endoscopy. 2004;36:726–730. doi: 10.1055/s-2004-825669. [DOI] [PubMed] [Google Scholar]
- 7.Pommert A, Hohne KH, Burmester E, Gehrmann S, Leuwer R, Petersik A, Pflesser B, Tiede U. Computer-based anatomy: a prerequisite for computer-assisted radiology and surgery. Acad Radiol. 2006;13:104–112. doi: 10.1016/j.acra.2005.08.034. [DOI] [PubMed] [Google Scholar]
- 8.Visible Body. Newton, MA: Argosy Publishing Inc.; 2012. [Accessed August 26, 2015]. Available at: http://www.visiblebody.com. [Google Scholar]
- 9.Anatomy.tv. London, UK: Primal Pictures Ltd.; 2006. [Accessed August 26, 2015]. Available at: http://www.anatomy.tv. [Google Scholar]
- 10.Wang H, Merchant SN, Sorensen MS. A downloadable three-dimensional virtual model of the Visible Ear. [Accessed August 26, 2015];ORL J Otorhinolaryngol Relat Spec. 2007 69(2):63–67. doi: 10.1159/000097369. Available at: http://research.meei.harvard.edu/Otopathology/3dmodels/visible_ear.html. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brinkley JF, Bradley SW, Sundsten JW, Rosse C. The digital anatomist information system and its use in the generation and delivery of web-based anatomy atlases. [Accessed August 26, 2015];Comput Biomed Res. 1997 30(6):472–503. doi: 10.1006/cbmr.1997.1461. Available at: http://www9.biostr.washington.edu/da.html. [DOI] [PubMed] [Google Scholar]
- 12.Colucci PG, Kostandy P, Shrauner WR, Arleo E, Fuortes M, Griffin AS, Huang YH, Juluru K, Tsiouris AJ. Development and utilization of a web-based application as a robust radiology teaching tool (RadStax) for medical student anatomy teaching. Acad Radiol. 2015 Feb;22(2):247–255. doi: 10.1016/j.acra.2014.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.OsiriX: An open-source software for navigating in multidimensional DICOM images. J Digit Imaging. 2004 Sep;17(3):205–216. doi: 10.1007/s10278-004-1014-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pieper S, Halle M, Kikinis R. 3D Slicer. Proceedings of the IEEE Symposium on Biomedical Imaging; April 15–18, 2004; Arlington, Virginia, USA. pp. 632–635. [Google Scholar]
- 15.Lorensen WE, Cline HE. Marching Cubes: a high resolution 3D surface construction algorithm. Proceedings of the 14th annual conference on Computer Graphics and Interactive Techniques, SIGGRAPH’87; July 27–31, 1987; Anaheim, California, USA. pp. 163–169. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Figure S1. Mediastinum module survey. The figure shows the on-line evaluation questionnaire that was distributed to the students following the 3D anatomy educational session on the mediastinum.
Supplementary Figure S2. 3D models of the male pelvis. The figure displays a tilted anterior view demonstrating the position of the inguinal ligament (green), the thigh muscles (pink), the prostate (dark purple) and the bladder (light orange). Iliacus muscles (light purple), pelvic muscles (yellow) are also shown along with proximal femurs (white). These models were created by a fourth year medical student during an elective month in radiology.
Supplementary Figure S3. 3D models of the female pelvis. The figure displays a tilted anterior view of the following structures : sacrum and iliac bone (white), iliac arteries (red), iliac veins (blue), uterus (light purple), ovaries (dark purple), anus (dark green), bladder (light yellow) and sciatic nerve (bright yellow). The figure also shows the following muscles : piriformis (bright yellow), pectineus (light green), psoas (dark pink), quadratus femoris (light orange), obturator externus (cyan) and obturator internus (dark blue). The opacity of the abdominal muscles has been lowered to enhance visualization of internal structures. These models were generated by the same fourth year medical student as the models in Supplementary Figure 2.